Abstract
Background:
Interdental areas are more prone to plaque accumulation, thereby increasing the susceptibility for periodontal diseases. Proper method of interdental hygiene assessment and motivation to use interdental aids can potentially reduce the burden of periodontal diseases.
Materials and Methods:
Fifty consecutive volunteer participants who presented with gingival inflammation were recruited based on the set of inclusion criteria. Further, proposed interdental hygiene index (IDHI) and gingival index were recorded by the examiner. Patient-reported outcome measures (PROMs) were recorded on the baseline and 4-week follow-up visits. Descriptive statistics and correlation analysis were performed.
Results:
The study comprised 50 participants with 22 male and 23 female participants. At baseline, the mean/standard deviation of IDHI was 1.32 ± 0.10 and 0.62 ± 0.21 on follow–up, respectively. For Gingival Index (GI) at baseline, the mean/standard deviation was 1.61 ± 0.15 and 0.70 ± 0.24 on follow–up, respectively. Correlation analysis revealed a significant correlation between IDHI and GI at baseline and follow-up. Majority of the participants scored 0 on the Visual Analogue Scale (VAS) for pain, rated “Good” for acceptability of procedure and perceived efficacy of interdental brush. Participants reported to have acquired “High level of motivation” to use an interdental brush.
Conclusion:
IDHI is a simple and reliable tool to assess the interdental areas of the patient and motivate to use interdental brush for the maintenance of good oral hygiene. PROMs also revealed positive responses from participants.
Keywords: Dental hygiene, gingivitis, index, interdental access probe, interdental brushes, interproximal cleaning, preventive dentistry
INTRODUCTION
A shift in the health–disease equilibrium occurs due to the accumulation and maturation of the oral biofilm. It results in proliferation of periodontopathogens and the host responds with inflammatory processes which results in the destruction of periodontium.[1] To disrupt the oral biofilm, mechanical method remains the cornerstone of plaque control, especially from the interproximal areas.[2] In a recent systematic review and meta-analysis, it is reported that the use of either a power or manual toothbrush can be advised for patients for periodontal maintenance. It is also recommended that interdental brushes (IDBs) are the device of choice for interdental cleaning.[3]
Indices are important tools to measure quantify and treat periodontitis both in epidemiological and clinical situations.[4] Over the years, several indices and their modifications have been reported and are being used. Gingival bleeding is an easily assessed sign of inflammation and it is associated with several periodontal diseases. To assess gingival bleeding, dichotomous indices are commonly used.[5] The dichotomous Eastman Interdental Bleeding Index (EIBI) was proposed in 1984, which involves horizontal insertion of a wooden interdental cleaner to stimulate the interproximal gingival tissues and the presence or absence of bleeding within 15 s is recorded.[6] Clinical effectiveness of different interdental aids in reducing interdental bleeding sites is established and it is reported that the interdental bleeding index method is a simplified way to assess interproximal gingival inflammation.[7] Although this index produces promising results, concern on trauma to the papilla has to be considered. To address this concern, IDBs instead of wooden sticks for the assessment; conical IDBs were used and authors have reported a significant correlation with the EIBI.[5,8]
Till date, the focus has been on assessment of bleeding on probing, bleeding on use of wooden, plastic interdental cleaner, and interdental brushing. There are no indices to assess the debris status of interdental regions. Although Approximal Plaque Index (API) is meant to assess the plaque in interproximal spaces, it lacks clarity on interdental situations.[5] Our proposal includes addition of debris component to the given bleeding on brushing index (BOB). To minimize trauma, our method includes the use of a color-coded interdental access probe (IAP) that determines the size of IDB to be used. The primary objective of the present study was to introduce a simple and reliable tool for assessment of interdental hygiene status, which can serve to motivate and educate patients in maintenance of overall oral hygiene. The secondary objective was to assess the patient-reported outcome measures (PROMs) like acceptability of the procedure, perceived level of efficacy of IDB, and the acquired level of motivation to use IDB through the process.
MATERIALS AND METHODS
This single-center, clinical study was conducted between December 2019 and February 2020. The study protocol was reviewed and approved by Institute Ethical Committee. Written informed consent was obtained from all participants after a thorough explanation of the nature of risks and benefits of the clinical investigation and associated procedures. While conducting the study, ethical principles outlined in the Declaration of Helsinki for research involving human subjects as revised in 2013 were followed.
A minimum sample size of 42 was estimated based on our pilot study to obtain a power of 80% and at 95% confidence interval (standard deviation: 0.7) using online software (OpenEpi) Open Source Epidemiologic Statistics for Public Health, Version 3.01. However, 50 consecutive volunteer participants who presented with gingivitis (as per the 2017 World Workshop Classification) were recruited for the study. The inclusion criteria were as follows: ≥18 years of age and <50 years and ≥20 teeth with adjacent teeth present, systemically healthy individuals. Exclusion criteria were periodontal pocket depth >4 mm, smoking, and pregnancy.
The IAP probe (CURAPROX™) is a color-coded graduated conical instrument with a rounded tip. The working part comprises colored bands from the point to the base corresponding to IDBs by increasing diameter. The largest section of each colored band corresponds to the cleaning efficiency diameter of the relevant brush. The nonworking part has a click-fastening joint for the attachment of a handle for easier use and access to the interproximal spaces at the back of the mouth. Straight handle or right-angled handle can be used based on the clinical situation and access to the interdental site. The procedure to use the IAP probe consists of introducing the probe into the interdental space, gently until resistance is met, and then noting the color that ends. This corresponds to the color code of the interdental brush most suitable for the space in question.[9] Before the start of the study, intra-examiner calibration for use of IAP, thereby determination of the size of IDB, and for Gingival Index was performed. This was achieved by examination of 30 sites twice, 24 h apart. Calibration was accepted if measurements at baseline and 24 h were similar. To avoid any bias, the calibration procedure was verified by a gold standard examiner[10,11] (a well-experienced examiner) who was not the part of the study.
On the day of screening, participants were explained about the study protocols and consent was obtained. In the same visit, they were assessed for inclusion criteria and interdental hygiene index (IDHI) and gingival index (GI, Löe and Silness, 1963) were recorded by the examiner. All the participants underwent scaling/root planing. After 4 weeks, participants were recalled; IDHI and gingival index (GI, Löe and Silness, 1963) were recorded. All the clinical examination were performed by a single examiner which was verified by a gold standard examiner.
The proposed interdental hygiene index
Armamentarium needed are mouth mirror, Color-coded IAP (IAP Curaprox™, Curaden International AG, Kriens, Switzerland), and IDBs – sizes: 0.6 mm, 0.7 mm, 0.8 mm, 0.9 mm, and 1.1 mm (Curaprox CPS Prime™; Curaden AG, Kriens, Switzerland).
IAP is used to measure the size of the interproximal area. It is gently inserted just above the papilla in the interproximal area until resistance is felt. As the IAP penetration stops, color on the probe is noted on the chart. A chart is prepared to record the readings of IAP. Based on the reading in the color-coded IAP, a corresponding interdental brush is chosen. Color coding corresponds to different sizes of the interdental brush. Color coding is as follows: blue – 0.6 mm, red – 0.7 mm, pink – 0.8 mm, yellow – 0.9 mm, and green – 1.1 mm [Figure 1]. The chosen interdental brush is gently inserted just under the contact point and guided between the teeth taking care not to exert force. If the brush met any resistance, a smaller brush was substituted and the insertion procedure is repeated.[8] Illustration of use of IAP and corresponding IDB is shown in Figure 2. Interdental brush is observed for the presence of debris and/or bleeding. Care has to be taken not to use wrong size of interdental brush to avoid any irritation or trauma to the papilla. Those teeth with an interproximal area wider than 1.1 mm and missing proximal teeth are excluded. Scoring criteria are given below. The chart to mark the selection of interdental brush and score of index is given in Figure 3.
Figure 1.

Interdental brush and interdental access probe, IDB - Interdental brush: IAP - Interdental Access Probe
Figure 2.
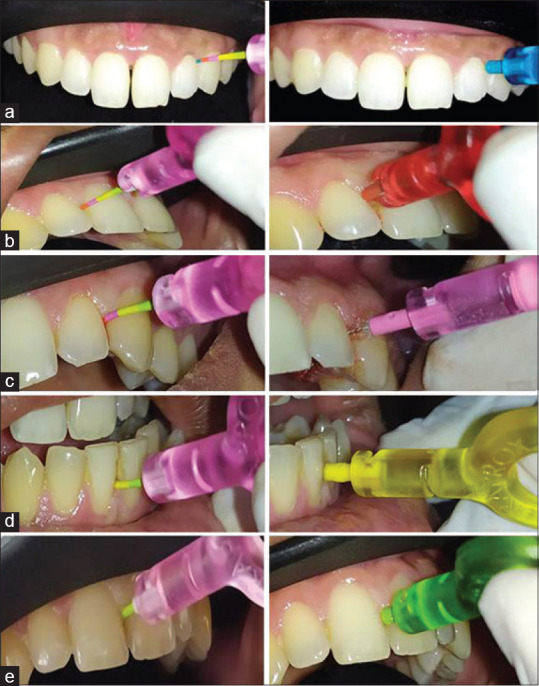
Illustration of use of interdental access probe and interdental brush. (a) (Left) interdental access probe indicates – Blue (0.6mm) and corresponding interdental brush is used. (Right); (b) (Left) interdental access probe indicates – Red (0.7mm) and corresponding interdental brush is used. (Right); (c) (Left) interdental access probe indicates – Pink (0.8mm) and corresponding interdental brush is used. (right); (d) (Left) interdental access probe indicates – Yellow (0.9mm) and corresponding interdental brush is used. (Right); (e) (Left) interdental access probe indicates – Yellow (1.1mm) and corresponding interdental brush is used. (Right)
Figure 3.
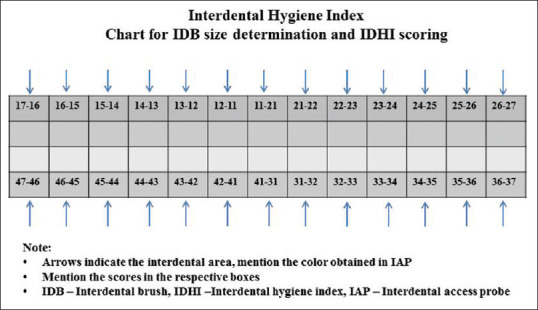
Chart for Interdental brush size determination and recording of interdental hygiene index. Arrows indicate the interdental area, mention the color obtained in interdental access probe. Mention the Interdental hygiene scores in the respective boxes
Scoring criteria
Score 0 = No debris and no bleeding on interdental brushing
Score 1 = Only debris on interdental brushing
Score 2 = Bleeding on interdental brushing.
Calculation of the index
IDHI = Total score/number of sites examined additional data that can be obtained
Number of interdental sites with no debris and bleeding
Number of interdental sites with debris
Number of interdental sites with bleeding.
Interpretation of overall score
-
Range of IDHI is 0–2
Average IDHI and interpretation: <0.1 = good, 0.1–1 = fair, and 1.1–2 = poor [Sample illustrated in Figure 4]
More than 30% sites with interdental bleeding (i.e., with Score 2) – Oral prophylaxis and regular use of interdental brush.
Figure 4.
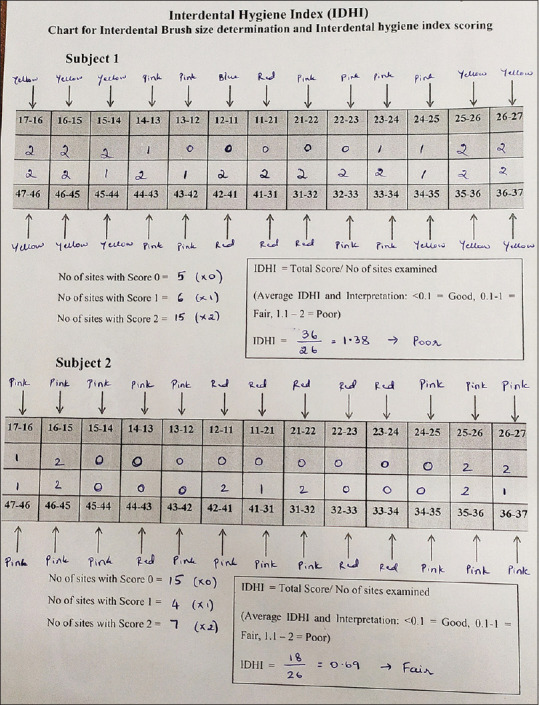
Illustration of scoring data and calculation of interdental hygiene index – interdental hygiene index
Rules for scoring
Tooth with no proximal tooth has to be excluded
All the third molars are excluded
In case of presence of crowded teeth and when the use of smallest size of interdental brush is not possible, those sites can be excluded
When debris and bleeding are present simultaneously, the score has to be considered for score 2.
The IDBs used to assess the index were given to the participants and method to use was demonstrated using touch to teach (T2T) concept.[12] T2T concept involves direct hands-on training of subjects to use the oral hygiene aids in their mouth itself. A maximum of three interdental brush sizes were chosen per subject to simplify the usage for the subjects. When more than three brush sizes were required, a smaller already identified diameter was used for that site. Once patient compliance was achieved, in further appointments, interdental sites were recalibrated and appropriate-sized IDBs were given. Participants were advised to brush twice daily and use the given interdental brush once a day. Further, to check the compliance, the participants had to make a note of the date and the time they brushed their teeth in a given form as described in the previous study. At the end of 4 weeks, safety evaluation was done by the examiner to check for any gingival abrasions.
All the participants were given a questionnaire and visual analog scale (VAS)[13] to assess the PROMS. Acceptability of the procedure was asked to be rated on a 3-point Likert scale[14] (good, fair, and poor) and VAS was recorded for pain/discomfort (0 – no pain/discomfort, 5 – moderate pain/discomfort, 10 – worst pain/discomfort). After 4 weeks of recall appointment, participants were asked to rate the following parameters on a 3-point Likert scale: perceived efficacy of interdental brush (good, fair, and poor) and motivation to use IDB (highly motivated, fairly motivated, and not motivated).
Data analysis used the Statistical Package for the Social Sciences (SPSS) IBM SPSS® version 22. Descriptive statistics were calculated. Comparison between baseline and 4-week follow-up recording of IDHI and Gingival Index (GI) was performed using paired t-test. Pearson's correlation coefficients were calculated between IDHI and GI indices for both baseline and follow-up visits.
RESULTS
The study comprised 50 participants, with 22 male and 23 female participants who belonged to 18–50 years' age group. All the participants had 26 interdental sites that were probed with color-coded IAP and corresponding sized brushed were used. The mean and standard deviation of the indices data and tests of significance are summarized in Table 1. PROMs are summarized in Table 2.
Table 1.
Results of interdental hygiene index and gingival index
| Mean±SD | P | |
|---|---|---|
| IDHI | ||
| Baseline | 1.32±0.10 | 0.001* |
| Follow-up | 0.62±0.21 | |
| GI | ||
| Baseline | 1.61±0.15 | 0.001* |
| Follow-up | 0.70±0.24 |
*P<0.05 is considered statistically significant. SD Standard deviation; IDHI – Interdental hygiene index; GI – Gingival index; p - p-value
Table 2.
Patient-reported outcome measures
| Patient reported outcome measures | %, n |
|---|---|
| Pain - VAS | 92% (n=42) |
| No pain (0) | 8% (n=4) |
| Moderate pain (5) | |
| Worst pain (10) | - |
| Acceptability | |
| Good | 100% (n=50) |
| Fair | - |
| Poor | - |
| Perceived efficacy | |
| Good | 100% (n=50) |
| Fair | |
| Poor | |
| Level of motivation | |
| Highly motivated | 74% (n=37) |
| Fairly motivated | 26% (n=13) |
| Not motivated | - |
VAS – Visual analog scale; n – Numbers
It was observed that there was a statistically significant correlation between IDHI and GI. At baseline, correlation coefficient between IDHI and GI was 0.97 with P value of 0.001*. At a follow-up visit, correlation coefficient between IDHI and GI was noted to be 0.97 with P value of 0.001*. (P < 0.05 is considered as statistically significant).
DISCUSSION
The aim of the present study was to propose a novel, simple, and reliable IDHI to assess and motivate the patients and assess the PROMs. Interdental areas, which are prone to caries and periodontal diseases, are less accessible for standard hygiene devices.[15] In recent systematic reviews, it has been reported that IDBs are best among other interdental aids for maintenance of interdental hygiene.[3,16] The proposed index utilizes an interdental brush as a tool for assessment and will serve to motivate the patient to use interdental brush regularly.
So far, several indices have been proposed and are being used in dental practice. EIBI, API, and BOB index are a few indices that focus on interdental areas. EIBI employs a wood stick slid horizontally between the teeth, apical to the contact area. It has been reported that by virtue of the shape and rigidity of the wood sticks employed, they have an inherent potential to cause trauma to the papilla.[8] To overcome this, a conical interdental brush (the BOB-probe) was used to assess the BOB index.[5] The goal of achieving a high degree of interdental hygiene with no/minimal damage is of utmost importance and priority while evaluating and selecting an interdental brush.[9] Use of a graduated color coded IAP to determine the size of interdental brush has been utilized and the authors have reported promising results.[17,18,19] Hence, a graduated color-coded probe is utilized to determine the right size of interdental brush which will aid in atraumatic use of interdental brush. VAS scores obtained in the current study (92% of participants – score 0, no pain) reveal that the procedure of IDHI is atraumatic and acceptable. The current study also assessed for any gingival abrasions due to the use of interdental brush and found that there were no gingival abrasions in any of the participants. This indicates the favorable nature of use of prescribed interdental brush in terms of safety. It can be attributed to the specific size of interdental brush used based on IAP reading, T2T method of instruction, and the nature of interdental brush per se.
API is a dichotomous index with quite strict criteria. In addtion, interdental condition is not described adequately. With this index, patients with good oral hygiene also could not achieve a lower API value, which makes it not a suitable tool for patient motivation.[5] As there are no other indices that evaluate plaque or debris at interdental areas, the proposed IDHI introduces debris component in the current index. Visible debris on IDB will help to make the patient realize that accumulation of debris can progress to gingival inflammation and if not checked may also proceed to periodontal diseases.
Previously introduced BOB index evaluates the interdental situation with regard to bleeding, which is one of the main signs of gingival inflammation. The proposed IDHI is similar to the BOB index in terms of bleeding component. IDHI has a debris score as an additional component when compared to the BOB index. Studies have compared and correlated the BOB index with previously established indices like modified sulcus bleeding index and bleeding on marginal bleeding and have found a significant correlation.[5,8]
The criterion for the quality of measurement method is its validity. One of the methods used is convergent validity, i.e., its correlation with another index which is already well established and considered to be a standard.[20] Thus, the current study assessed IDHI and GI and they were subjected to correlation analysis. It was noted that there was a statistically significant correlation between the two indices. Although criteria for IDHI and GI are different, IDHI has debris and bleeding components which are known to be part of gingivitis. Accumulation of debris and further plaque can lead to gingivitis.[21,22,23] Considering the above fact, the present study included GI measurement for correlation.
The present study assessed the PROMs. Majority of the participants rated “good” for acceptability and “good” for perceived level of efficacy of IDB. Furthermore, participants have reported to be “highly motivated” to use IDB through the process of assessment of IDHI.
The advantages of the proposed IDHI are: (a) visible debris and/or bleeding from interdental area can be shown to the patient and thereby motivated to maintain good oral hygiene; (b) A patient gets oriented toward the use of interdental brush for oral hygiene maintenance; (c) improvement in IDHI score if any, in follow-up visit, may further motivate the patient to comply with the use of interdental brush; (d) use of color-coded IAP to determine the correct size of interdental brush ensures atraumatic experience during the recording of index and also on the use of interdental brush in patient's routine. The limitation of the study is the smaller sample size. There is further scope to utilize the proposed IDHI index in a larger sample group.
CONCLUSION
IDHI is a simple and reliable tool to assess the interdental areas of the patient and motivate to use interdental brush for maintenance of good oral hygiene. PROMs also reveal that procedure is acceptable, perceived efficacy of interdental brush is good, and participants were highly motivated to use interdental brush.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors acknowledge the contribution of Dr. Amith Thakur, Senior Resident, PGI Chandigarh, in statistical analysis.
REFERENCES
- 1.Dalwai F, Spratt DA, Pratten J. Modeling shifts in microbial populations associated with health or disease. Appl Environ Microbiol. 2006;72:3678–3684. doi: 10.1128/AEM.72.5.3678-3684.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chandki R, Banthia P, Banthia R. Biofilms: A microbial home. J Indian Soc Periodontol. 2011;15:111–4. doi: 10.4103/0972-124X.84377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slot DE, Dörfer CE, Van der Weijden GA. The efficacy of interdental brushes on plaque and parameters of periodontal inflammation: A systematic review. Int J Dent Hyg. 2008;6:253–64. doi: 10.1111/j.1601-5037.2008.00330.x. [DOI] [PubMed] [Google Scholar]
- 4.Dhingra K, Vandana KL. Indices for measuring periodontitis: A literature review. Int Dent J. 2011;61:76–84. doi: 10.1111/j.1875-595X.2011.00018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenauer T, Wagenschwanz C, Kuhn M, Kensche A, Stiehl S, Hannig C. The Bleeding on Brushing Index: A novel index in preventive dentistry. Int Dent J. 2017;67:299–307. doi: 10.1111/idj.12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrams K, Caton J, Polson A. Histologic comparisons of interproximal gingival tissues related to the presence or absence of bleeding. J Periodontol. 1984;55:629–32. doi: 10.1902/jop.1984.55.11.629. [DOI] [PubMed] [Google Scholar]
- 7.Graves RC, Disney JA, Stamm JW. Comparative effectiveness of flossing and brushing in reducing interproximal bleeding. J Periodontol. 1989;60:243–7. doi: 10.1902/jop.1989.60.5.243. [DOI] [PubMed] [Google Scholar]
- 8.Hofer D, Sahrmann P, Attin T, Schmidlin PR. Comparison of marginal bleeding using a periodontal probe or an interdental brush as indicators of gingivitis. Int J Dent Hyg. 2011;9:211–5. doi: 10.1111/j.1601-5037.2010.00483.x. [DOI] [PubMed] [Google Scholar]
- 9.Bourgeois D, Carrouel F, Llodra JC, Bravo M, Viennot S. A colorimetric interdental probe as a standard method to evaluate interdental efficiency of interdental brush. Open Dent J. 2015;9:431–7. doi: 10.2174/1874210601509010431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hefti AF, Preshaw PM. Examiner alignment and assessment in clinical periodontal research. Periodontol 2000. 2012;59:41–60. doi: 10.1111/j.1600-0757.2011.00436.x. [DOI] [PubMed] [Google Scholar]
- 11.Hasturk H, Cugini M. Examiner standardization and calibration for oral and periodontal regenerative studies. In: Giannobile WV, Lang NP, Tonetti MS, editors. Osteology Guidelines for Oral and Maxillofacial Regeneration: Clinical Research. Batavia: Quintessence Publishing Co Inc; 2014. pp. 97–120. [Google Scholar]
- 12.Philosophy | iTop. [[Last accessed on 2020May 24]]. Available from: https://www.itop-dental.com/en/philosophy .
- 13.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Avula H. Periodontal research: Basics and beyond – Part III (Data presentation, statistical testing, interpretation and writing of a report) J Indian Soc Periodontol. 2013;17:577–82. doi: 10.4103/0972-124X.119293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Demirci M, Tuncer S, Yuceokur AA. Prevalence of caries on individual tooth surfaces and its distribution by age and gender in university clinic patients. Eur J Dent. 2010;4:270–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Kotsakis GA, Lian Q, Ioannou AL, Michalowicz BS, John MT, Chu H. A network meta-analysis of interproximal oral hygiene methods in the reduction of clinical indices of inflammation. J Periodontol. 2018;89:558–70. doi: 10.1002/JPER.17-0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carrouel F, Llodra JC, Viennot S, Santamaria J, Bravo M, Bourgeois D. Access to interdental brushing in periodontal healthy young adults: A cross-sectional study. PLoS One. 2016;11:e0155467. doi: 10.1371/journal.pone.0155467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourgeois D, Saliasi I, Llodra JC, Bravo M, Viennot S, Carrouel F. Efficacy of interdental calibrated brushes on bleeding reduction in adults: A 3-month randomized controlled clinical trial. Eur J Oral Sci. 2016;124:566–71. doi: 10.1111/eos.12302. [DOI] [PubMed] [Google Scholar]
- 19.Imai PH, Hatzimanolakis PC. Interdental brush in type I embrasures: Examiner blinded randomized clinical trial of bleeding and plaque efficacy. Can J Dent Hyg. 2011;45:25–32. [Google Scholar]
- 20.Deinzer R, Jahns S, Harnacke D. Establishment of a new marginal plaque index with high sensitivity for changes in oral hygiene. J Periodontol. 2014;85:1730–8. doi: 10.1902/jop.2014.140285. [DOI] [PubMed] [Google Scholar]
- 21.Periodontal Disease – StatPearls – NCBI Bookshelf. [[Last accessed on 2020 Nov 11]]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554590/
- 22.Kimball GC. The relationship of Materia Alba and dental plaque to periodontal disease. J Periodontol. 1952;23:164–9. [Google Scholar]
- 23.Intan Suhana MA, Farha A, Hassan BM. Inflammation of the gums. Malays Fam Physician. 2020;15:71–3. [PMC free article] [PubMed] [Google Scholar]


