Abstract
Background
The use of rural rotations within urban-based postgraduate programs is the predominant response of medical education to the health needs of underserved rural populations. The broader impact on rural physicians who teach has not been reported.
Methods
This study examined the personal, professional, and financial impact of a rural rotations for urban-based family medicine (UBFM) residents on Canadian rural teaching physicians. A survey was created and reviewed by community and academic rural physicians and a cohort of Canadian rural family physicians teaching UBFM residents was sampled. Survey data and free-text responses were assessed using quantitative and qualitative analyses.
Results
Participants with rural residency backgrounds perceived a negative impact of teaching UBFM (p = 0.02 personal and professional) and those in a primary rural environment (as defined below) perceived impact as positive (p < 0.001). Rural preceptors often held contrasting attitudes towards learners with negative judgements counter-balanced by positive thoughts. Duration in practice and of teaching experience did not have a significant impact on ratings.
Conclusion
Being a rural preceptor of UBFM residents is rewarding but also stressful. The preceptor location of training and scope of practice appears to influence the impact of UBFM residents.
Abstract
Contexte
L’introduction de stages en milieu rural pour les résidents qui effectuent leur formation postdoctorale dans un centre urbain constitue la solution principale adoptée en matière d’éducation médicale pour répondre aux besoins des populations rurales mal desservies. L’impact plus large de ces stages sur les médecins enseignants en milieu rural n’a pas été documenté.
Méthodes
Cette étude examine les répercussions personnelles, professionnelles et financières du stage réalisé en milieu rural par les résidents de médecine familiale en milieu urbain (MFMU) sur les médecins enseignants en milieu rural au Canada. Un sondage a été créé et revu par des médecins universitaires et communautaires en milieu rural et une cohorte de médecins de famille ruraux enseignant à des résidents de médecine familiale en milieu urbain a été échantillonnée. Les données du sondage et les réponses ouvertes obtenues ont fait l’objet d’analyses quantitative et qualitative.
Résultats
Tandis que les participants possédant une expérience de résidence en milieu rural ont perçu l’effet négatif du fait d’enseigner aux résidents de MFMU (p = 0,02 personnel et professionnel), ceux qui exercent dans un environnement rural primaire (tel que défini ci-dessous) en ont une perception positive (p<0,001). Les superviseurs en milieu rural avaient souvent des attitudes contrastées envers les apprenants, des aspects positifs compensant certains jugements négatifs. La durée d’exercice et l’expérience en l’enseignement n’ont pas eu d’impact significatif sur les évaluations.
Conclusion
Être un superviseur en milieu rural de résidents en MFMU est gratifiant, mais aussi stressant. Le lieu de formation et le champ d’exercice du superviseur semblent déterminer l’effet qu’ont les stages de résidents de MFMU sur ces superviseurs.
Introduction
There is an ongoing international crisis of health care delivery in underserved rural populations.1,2,3,4,5,6 Medical education has commonly been proposed as a solution to this crisis, specifically with the goal of increasing the number of rural health care workers and physicians.5,7,8 Before the widespread development of rural Family Medicine (FM) training programs, institutions often mandated rural experiences within urban-based postgraduate training programs. Similar to other jurisdictions, the Canadian College of Family Physicians implemented this recommendation in 1999.9 The “rural rotation” in urban-based postgraduate training programs has largely remained unchanged since that time. While there is no required duration, the majority of rural rotations consist of eight weeks during which the resident is expected to achieve a program-specific list of learning objectives. The rotation is typically scheduled in the second year of the program. Rural preceptors, especially in smaller centres, usually have an intense daily, one-on-one, supervisory role in these rotations. Within the Canadian context, as urban-based programs have grown, there has been more pressure on rural communities to accommodate urban learners. This has resulted in a substantial increase in the number of rural training sites.10 Therefore, Canadian rural communities form an integral and essential part of the training of urban-based postgraduate learners.
Despite the widespread implementation of rural rotations in urban-based postgraduate training programs, systematic evaluations of their impact are scarce. A recent literature review examining how these rotations influenced learners found they were associated with an increased likelihood of future rural practice.11 The outcome of “practice location” has remained the primary measure of success in the evaluation of the rural training experience. However, while the intent of rural rotations may have been to increase the profile and desirability of a rural practice in the mind of the postgraduate learner, other potential impacts remain unstudied, and therefore unidentified.
One area that has not been adequately explored in the published literature is the impact of rural rotations of urban-based postgraduate family medicine (UBFM) residents on rural preceptors. To our knowledge, the majority of prior studies12,13.14,15,16 have examined the impact of undergraduate medical learners on rural preceptors with very few17 having focused on the impact of postgraduate learners. Although ample anecdotal evidence exists from rural doctors, a systematic documentation of this cohort’s experiences (including outcomes, barriers, and facilitators) is important for both recruiting new preceptors and supporting the existing teaching physicians.
The current study was designed to address the gap in the literature by grounding commonly voiced beliefs in empirical evidence. Specifically, we sought to understand the variety of ways in which rural rotations of UBFM residents may impact the rural preceptor.
Methods
The research team consisted of three clinicians (DM, MWB, JO) and a PhD researcher (RM). The lead author formulated the initial question. Two of the clinicians had experience in working in rural and regional teaching communities (MWB, DM), the third brought quantitative expertise to the team (JO) and qualitative expertise was brought by RM. All members participated in the final submission and none of the team members had direct responsibility or accountability to the rural program at the University of Calgary at the time of the project. An expert in evaluation at the University of Calgary assisted in the survey design.
An online survey collected quantitative and free-text data. The proposed survey was presented to a focus group for assessment. The focus group consisted of a selected sample of four experienced family medicine rural preceptors. Each preceptor had a minimum of five years teaching experience, was currently in practice, and had an academic appointment. Based on their feedback, the survey, including the categorization of rural teaching hospitals into two scopes of practice, was revised and beta tested on the same group to ensure accuracy of language, interpretation of the questions and flow. The final survey is shown in Appendix A.
The University of Calgary Department of Family Medicine teaching preceptor data base was used to determine potential participants. We searched the database for rural FM preceptors who had been assigned UBFM residents from the Department of Family Medicine training program. With the exception of the previous academic year, there had been no change in the database for the previous five years. Therefore, contact information for the previous two academic years (2017-18, 2018-19) was used. The survey and an introductory letter were electronically mailed to this cohort, seeking their consent to participate in the study.
The survey collected demographic data related to the teaching preceptor such as duration of teaching appointment, the preceptor’s own FM training location (rural/urban), location of practice and the scope of practice in their community. While all smaller communities had an active hospital, there was a wide range of services that could be available locally. Communities were therefore categorized both with regards to size as well as scope of practice in order to move beyond size and distance from a major centre as being markers of rurality. The presence of full-time specialists was distinct, and the presence of a functioning obstetrical unit was a marker for anesthesia and surgical services. Rural hospitals where care was provided solely by family physicians and there were no obstetrical services were categorized as primary rural with all others secondary. Regional centers had dedicated ICU’s and were also defined by population size.
The survey included two questions about the preceptors’ participation in Faculty Development (FD). We speculated that attendance at institution-sponsored events might be a factor in the preceptor teaching experience through skill enhancement or facilitated engagement with the teaching community.
Participants were asked to rate the impact of teaching UBFM residents on a 5-point Likert scale (significantly negative to significantly positive) across three domains: personal, professional, and financial. Microsoft Excel was used to organize responses and for data entry into Stata 14. Ordinal logistic regression was used to analyze whether impact ratings varied with participant factors. Subcategories were combined to perform binomial logistic regression where data were insufficient for ordinal logistic regression. Binomial regression was performed for the following variables: residency program (rural compared to urban), whether participants discussed teaching challenges in administrative or social networks, and whether participants attended faculty development events. Odds ratios with 95% confidence intervals were calculated with corresponding p values of < 0.05 considered significant.
Participants were also able to elaborate on their ratings by providing free-text comments within the personal, professional and financial spheres of impact. Although these spheres were deductive, the written comments were analyzed qualitatively using a structured, inductive approach based on thematic analysis.18 Preceptor responses were first imported to three tables in Microsoft Word, one for each sphere of impact. Coding was performed independently by RM and MWB. Data were initially coded within each table. Comments with multiple concepts could be assigned to more than one code.
After the coding step, we amalgamated the data across the three spheres of impact. The method of constant comparison was used to systematically categorize, compare, and evaluate the data.19 Emerging themes were discussed during regular meetings with team members until consensus was reached. This study was approved by the University of Calgary REB19-1258.
Results (quantitative)
Demographics of respondents
There was a 46% response rate with 28 of 61 physicians surveyed providing responses to some or all of the survey questions. Most respondents (89%) were from communities of less than 20, 000 people and although the scope of practice varied, approximately 57% practiced in secondary rural communities. Most participants had been in practice for more than five years (89%) with the majority in practice for more than 10 years (61%). Participant demographics are further detailed in Table 1.
Table 1.
Participant demographics (N = 28)
| Demographics | Subcategory | n | % |
|---|---|---|---|
| Age | < 30 years | 1 | 3.6 |
| 31-40 years | 11 | 39.3 | |
| 41-50 years | 9 | 32.1 | |
| 51-60 years | 2 | 7.1 | |
| > 60 years | 5 | 17.9 | |
| Gender | Male | 21 | 75.0 |
| Female | 7 | 25.0 | |
| Years in Practice | < 5 years | 3 | 10.7 |
| 6-10 years | 8 | 28.6 | |
| 11-20 years | 6 | 21.4 | |
| 21-30 years | 6 | 21.4 | |
| > 30 years | 5 | 17.9 | |
| Community size | Remote: 20,000-500,000 people AND > 300 km from metro centre | 2 | 7.1 |
| Small rural: population < 5,000 people | 5 | 17.9 | |
| Rural: population 5,000-10,000 people | 11 | 39.3 | |
| Large rural: population 11,000-20,000 people | 9 | 32.1 | |
| Regional: population 20,000-500,000 people | 1 | 3.6 | |
| Scope of practice | Primary rural community (Family physicians, no obstetrical deliveries, no/only visiting specialists) | 10 | 35.7 |
| Secondary rural with no OR (Family physicians and on-site specialists, obstetrical deliveries) | 1 | 3.6 | |
| Secondary rural (Family physicians and on-site specialists, obstetrical deliveries with OR) | 16 | 57.1 | |
| Regional centre (Hospital primarily specialist based, onsite advanced imaging, full time OR and ICU) | 1 | 3.6 | |
| Residency program attended by participant | Urban-based residency program (Canadian and International) | 16 | 57.1 |
| Rural-based residency program (Canadian and International) | 12 | 42.9 |
Teaching experience data are shown in Table 2. Most participants had between 6-10 (29%) or 11-20 (32%) years of teaching overall, with a majority of respondents (61%) having less than 10 years of experience specifically teaching UBFM. Half of the respondents taught UBFM residents more than two but less than six months of the year. When preceptors had issues with teaching UBFM residents, most discussed their challenges within their social network (89%). Further characteristics of engagement in teaching supports can be found in Table 3.
Table 2.
Participant teaching experience
| Demographics | Subcategory | n | % |
|---|---|---|---|
| Years teaching any learner | < 5 years | 5 | 17.9 |
| 6-10 years | 8 | 28.6 | |
| 11-20 years | 9 | 32.1 | |
| 21-30 years | 2 | 7.1 | |
| > 30 years | 4 | 14.3 | |
| Years teaching UBFM residents | < 5 years | 8 | 28.6 |
| 6-10 years | 9 | 32.1 | |
| 11-20 years | 6 | 21.4 | |
| 21-30 years | 2 | 7.1 | |
| > 30 years | 3 | 10.7 | |
| Months per year teaching UBFM residents | < 2 months/year | 3 | 10.7 |
| > 2 but < 6 months/year | 14 | 50.0 | |
| > 6 months/year | 11 | 39.3 |
Table 3.
Participant engagement in teaching supports
| Response | n | % | |
|---|---|---|---|
| If challenges teaching UBFM residents - discuss in social network? | Yes | 25 | 89.3 |
| No | 2 | 7.1 | |
| No response | 1 | 3.6 | |
| If challenges teaching UBFM residents – discuss in formal administrative network? | Yes | 19 | 67.9 |
| No | 7 | 25.0 | |
| No response | 2 | 7.1 | |
| Attend faculty development events? | Yes | 18 | 64.3 |
| No | 8 | 28.6 | |
| No response | 2 | 7.1 |
Ratings of personal, professional and financial impact
Overall, participant age, gender, and community size were not associated with statistically significant differences in personal, professional, or financial impact ratings (Figure 1). Years teaching any learner also did not seem to significantly influence the ratings.
Figure 1.
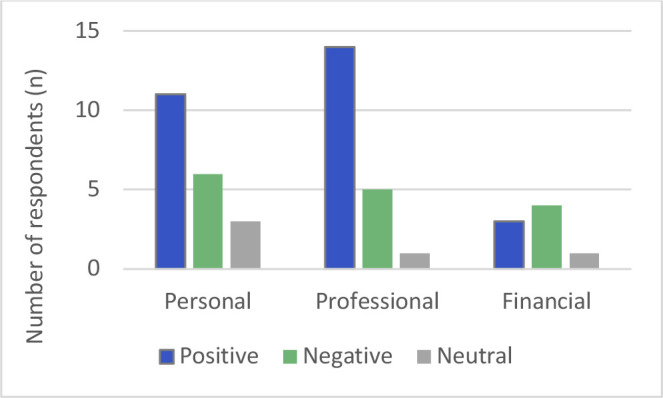
Participant-rated impact of teaching UBFM residents
The majority of respondents (20/28) provided Likert scale ratings for personal and professional impact of teaching UBFM residents. Only eight of 28 physicians provided ratings for financial impact.
The location of the FM residency program (urban vs. rural) attended by respondents was the factor that most consistently influenced impact ratings. While participants with FM rural residency backgrounds were more likely to rate personal and professional impact negatively, those with FM urban residency training rated the same impact as favorable (p = 0.02 personal, p = 0.02 professional). Similarly, there were divergent ratings depending on the environments where the respondents practiced. If the respondent practiced in a primary rural environment (i.e. no obstetrical deliveries and no access to on-site specialists), the personal impact was perceived as overwhelmingly positive (p < 0.001)) compared to those practicing in rural communities with a broader scope of practice.
Almost all of the participants reported that they discussed the challenges of teaching UBFM residents within their social networks. Of those who provided personal impact ratings, half rated the impact positively, a third rated the impact negatively, with the remaining participants providing a neutral rating.
Participants who discussed UBFM teaching challenges in social networks rated personal impact more negatively than those who did not (p = 0.04). Similarly, those who attended faculty development events were more likely to rate professional impact negatively (p = 0.01).
The results of attendance at FD events showed a statistically significant trend (p = 0.00) towards a more negative professional impact rating for participants with more years of experience teaching UBFM residents. However, the free-text responses suggest that the preceptors do not link their own teaching skill to the experience of having an UBFM learner in their practice and do not think that FD can address the problems of the learners lacking the necessary skills and motivation to work in rural communities. One preceptor stated, “The issue is not faculty development, [it] is getting them more up to speed before they get to us” (P6). Another respondent commented, “Don't ask me how I could better accommodate unwilling participants. I'm happy to have keen urban residents” (P18). According to another individual, one role of FD is to inform the preceptor of the urban program structure: “Know limitations of urban program in providing independence and experience” (P16).
Results (qualitative)
In conjunction with the quantitative evaluation of the impact of UBFM residents in the personal, professional, and financial spheres, rural preceptors were also asked to elaborate in free-form comments on these impacts. Some respondents wrote in substantial detail. In general, preceptors described more personal and professional impacts than financial impacts. In this analysis, we have combined similar themes across the three broad impact categories.
Being a preceptor is rewarding
Most of the respondents described various intangible, intrinsic rewards associated with being a preceptor. Several preceptors mentioned their enjoyment of teaching and being able to share their knowledge and experiences. They also expressed personal and professional satisfaction from having learners at their sites, especially when the residents were highly motivated. For example, one preceptor noted, “The residents are very eager to learn and so there is better job satisfaction when you can really help them to learn about rural medicine and all that comprehensive family medicine can offer” (P17).
Several preceptors took pride in being able to contribute to the development of a new physician: “…It provides job satisfaction knowing that one can be a part of their learning and helping them in their career” (P7). One respondent stated that being a preceptor is a way of “giving back” to the medical community (P23). As well as providing residents with the required clinical skills, preceptors also bolstered learner confidence and acted as role models. In some cases, there can be an unexpected long-term professional benefit: “Some [learners] have become colleagues at our site or others, which although against the norm, is heartwarming to see” (P9).
Preceptors stressed that learning was a continuous and two-way process. Having residents gave rural physicians the opportunity to maintain and update their own skills. One survey respondent said, “I continuously learn new things when I have residents. The questions they ask usually result in a few new learning topics each day” (P11). Preceptors also noted that it was exciting to work with a diverse group of people: “… The exposure to the youthful enthusiasm, academic freshness and ethnic diversity of the residents is often very stimulating for the practice” (P16). In addition, the presence of learners motivated preceptors to “model positive professional behaviour” (P5).
Although the majority of the benefits of being a preceptor are intrinsic, a few respondents did mention some extrinsic rewards as well. Well-trained residents can contribute to the practice by freeing up the preceptor’s time during clinic hours and helping at busy times in the hospital. One preceptor stated, “It allows us to spend time more with patients as two vs one. Often easy to stay on time. Allows me to do things like call specialists, patients, referrals, etc. around the office sometimes as well which can be very nice. At urgent care they help significantly with ED flow” (P23). Experienced learners can also take on some of the workload for their supervisors during weekend and night shifts: “… If I have a stable patient on the ward, they can round for me on the weekend (which is a huge time save and I just check in by phone). Once I have them up and running, they also make night shifts much more pleasant, and usually buy me at least two more hours of sleep” (P20).
Being a preceptor is stressful
Preceptors frequently noted that, in general, supervising urban-based residents is a time-intensive process that affects their personal and professional lives. One respondent said, “It does create longer days as reviewing and teaching during the day as well as managing a busy schedule with a learner takes more time than it would if I were working on my own” (P2). Participants also clarified that while residents usually required more of the preceptor’s time in the initial stages of the rotation, learners generally required fewer resources once they became more skilled and comfortable in the clinical or hospital environment: “[It] does become positive after the first few weeks” (P25).
Several preceptors described UBFM residents as having fewer clinical skills than rural residents, thus requiring more supervision: “Most urban residents come out at a level more typical of a medical student in independence and represent a significant work load to try and move them forward to their goals of a well-rounded generalist” (P6) and “urban residents are mostly not comfortable in ER settings. The urban residents are not as comfortable doing office procedures compared to rural residents” (P24). A learner with lower skill levels may have difficulties during their rotation and even face remediation – outcomes that place additional burden on their preceptor: “The main problem is the impact of a struggling learner. This seems to occur more often in the urban pool, and it absolutely drains time and energy from the professional side of our lives” (P16).
A consequence of having learners in a clinical practice is the inevitable contact with patients. Two preceptors described patients as “happy to see learners” (P2), while one preceptor said the opposite, “Some patients don't like to see a resident” (P20). Patient-resident interactions can cause additional stress for the supervisor. The resident’s lack of experience means that the preceptor must check their findings, therefore slowing the clinic flow: “Less experienced outside of clinic - more often than not performing at clinical clerk level - therefore not entrustable to work in those environments without close (usually direct) supervision. This acts as an anchor on my efficiency in those environments and often causes longer patient waits thereby affecting access” (P26). Preceptors are also intensely aware that they are ultimately responsible for any patient diagnosis (and any errors): “I did have one particularly bad resident who missed an ectopic pregnancy and an ischemic limb; and so I do worry at times that I am putting my name on someone else's work” (P20).
There appears to be an emotional toll on preceptors when they are asked to supervise learners who have little intention of establishing a rural practice at a future date. UBFM residents who are mandated to do rotations in rural communities may lack commitment or interest in those placements and often do not integrate into the community. Several preceptors used words like “exhausting,” “tiring,” “disappointed,” “fatiguing,” “frustrating,” “resentment,” and “challenging” to describe their own emotions in dealing with these learners. As one respondent noted,
I often find that the rural rotation experience is not valued by the urban residents; this is of course not universally the case, but many choose to return to their urban homes on as many weekends as possible, take as much vacation and flex time as possible and generally are not interested in gaining skills in the full scope practice that rural is…. Rural preceptors accept learners from all over; the ones that exhaust my teaching energy the most are the disinterested ones (P4).
In such situations, the intrinsic rewards appear to decrease and preceptors may lose their motivation to teach. Some respondents suggested that rural rotations should only be offered to interested urban residents: “Low job satisfaction in teaching those who are disengaged with their rural experience. This is not applicable to all urban learners, but at least 50%... Would rather have voluntary urban learners come to rural locations” (P18).
Rural preceptors report being challenged because UBFM residents may have differing goals or expectations about the placement. Some preceptors are surprised at the learners’ lack of interest in skills which would be valuable even in a future urban family medicine practice. One preceptor stated, “They are usually polite and keen to learn in our environment. I am usually disappointed however that not only are they not going to practice rurally, they generally do not embrace generalist philosophy of practice even in their eventual urban environment (i.e. don't do OB, ED, hospital medicine, etc.)” (P9). Another preceptor described mixed feelings about their learners: “By far positive, but some resentment on my part, given that urban residents seem to be less motivated to practice hospital-based medicine, which I think is important for urban family medicine” (P5). Amending a learner’s beliefs about rural medicine or scope of practice can be very satisfying for their preceptor: “On the positive side, I find I'm really able to impact the urban residents’ beliefs about what their scope of practice could entail” (P14).
Counter-balancing narratives
In their comments, respondents sometimes mentioned one positive or negative impact that was immediately followed by a contrasting statement. This juxtaposition was used to explain why they had recorded the overall impact of having urban residents as “neutral.” For example, one preceptor followed up their statement of “neutral professional impact” with both positive and negative impacts: “Sometimes a resident may help to see more volume, but often times the urban residents are functioning below the level of independence of a matched stage rural resident” (P4). Similarly, another preceptor explained their rating of “neutral overall” with a negative impact statement (“longer days, occasionally dealing with unprofessional behaviours”) counter-balanced with a positive impact (“better job satisfaction and ability to accommodate more appointments to service our panel.”) (P21)
Counter-balancing narratives were also demonstrated when respondents discussed the financial impact of teaching UBFM residents. Almost half of the preceptors (12/28) reported no financial impact, or that it was revenue neutral. Two others were unsure about the financial aspect. In general, the respondents noted that the slight increase in revenue was offset by spending more time at work, especially early in the placement. For example, one preceptor noted that the positive aspect of the teaching stipend and the learner seeing his own patients, “When [the learner] sees patients on my list it slows me down and has a slight negative effect” (P21). Another preceptor described the potential negative effect of supervising learners on revenue: “I end up spending more time overall dealing with patients, but less time with the patients which impacts my billing negatively. The stipend does not come close to making up for the lost billing. I do not book extra patients for residents to see, as I feel that is a misuse of their time. They do more work, but overall learn less” (P11).
Synthesis
There was no reported significant overall impact on finances based in both the qualitative and quantitative components of the survey. Despite the individual challenges, there appears to be a general belief that teaching urban-based residents remains rewarding. Somewhat surprisingly, the duration in practice and the duration of teaching did not significantly impact the perceptions of these teaching physicians.
Discussion
This study provides an initial exploration of an under-studied area in medical education: how and to what extent are rural preceptors impacted by the rural rotations of urban-based postgraduate Family Medicine learners. As far as we have been able to determine, it is the first study of its kind and will naturally raise many questions for verification or further exploration.
Respondents were generally an experienced group of teachers, not limited to supervising UBFM residents, and reported teaching across the educational spectrum. Overall, the impact of teaching UBFM learners was positive within the personal and professional spheres and neutral in the financial sphere. However, individual responses suggest that preceptors weigh the positives and negatives within each of these domains. Doctors reported feeling intrinsically rewarded by acting as a preceptor even while they detailed the emotional stress and frustration of working with some residents. As such, negative personal impacts appeared to be offset by other personal experiences or perceived increased professional benefits. Interestingly, the oft-quoted anecdote of negative financial impact of teaching these learners was not upheld within our sample.
The factor that influenced ratings most significantly was the location (rural vs urban) of the residency program attended by the teaching preceptor. Preceptors who completed a rural residency were less likely to rate a positive personal or professional impact of teaching UBFM learners than those who completed an urban residency training program. The preceptors’ lived experience in residency may contribute to the expectations they have of incoming residents on a rural rotation. Assuming that it would be unlikely for the majority of UBFM learners to be performing below expectations during their urban rotations, comments calling into question the generalist skill set of UBFM resident imply that there may be a disconnect between rural preceptors’ expectations for the rotation compared to the curricular expectations of either the program or the learner. This potential incongruence could be the underlying factor in negative perceptions of the impact of teaching UBFM learners on rural preceptors and deserves to be further explored. Seeking an understanding of the impact on the rural preceptor raises the question of how other professionals who are both serving and teaching in under-resourced populations, are being asked for their input into curricular change. A deeper understanding of these complexities could lead to institutional program evolution.
We speculate that discrepancies between preceptor, learner, and program expectations could emerge as unforeseen consequences of rapid urban program expansion. With expansion has come an increased demand for mandated rural rotations, and in a resource limited community, this increase may have caused the experience to have strayed from its original objective of physician recruitment. Over time, as programs have grown and family medicine training opportunities and skill sets in large urban areas have changed, rural experiences have likely evolved from a singular recruitment purpose based on the learning relationship, to rotations where core procedural and diagnostic skills are taught. Given the generalist tradition of rural practice, and the limited ability to gain independence and broad skills in the urban environment, learners may arrive with the needed theoretical knowledge but without the clinical experience to perform the required skills. Preceptor comments suggest that important teaching about family medicine competencies - beyond those traditionally explored in urban clinics - take place during the rural rotation. The rural rotation, therefore, serves a critical role in training UBFM learners, particularly in the fields of acute care and procedural medicine.
The importance of the quality of the teaching relationship between the rural preceptor and the UBFM resident is highlighted by respondents. Many preceptors described growth in the residents they taught and a personal sense of satisfaction as they spent more time with the learner. Previously, Hecker and Violato20 have emphasized the importance of the learner-teacher relationship, and Chong and Kiroff21 specifically reported that the quality of the educational relationship is a determinant in rural recruitment. The concept of total accumulated time in a rural teaching site may more accurately reflect this relationship-based teaching.22
Strengths and limitations of study
A strength of the study is the survey that was designed and modified by rural teaching physicians. The unique scale of community categorization was created in an attempt to remove the often-quoted population size and distance from tertiary care as the predominant markers for rurality. It was posited that the focus on scope of practice, as a recognized driving force for rural physician recruitment, might also be a driver for perception of impact of the urban-based learner on the rural teacher. This was supported by our findings.
The major weakness of the study is the small sample size of currently teaching rural physicians from a single university program in Western Canada. However, the small sample size was counter-balanced by the inclusion of all rural teaching preceptors within the program. As preceptors dissatisfied with the teaching experience may have already left the preceptor roster, their voices are not captured giving more weight to the perspectives of those remaining. As previously noted, the small sample size necessitated the pooling of data across three subcategories.
Future studies should expand the sample set and include a larger geographic area. The impact of the rural rotation on patients and the urban-based learner, as well as the potentially incongruent expectations of urban-based learners, rural preceptors and host programs with regards to the objectives of the rural family medicine rotation, are all areas ripe for investigation. The counter-intuitive results of the relationship of Faculty Development to the preceptor experience also requires further exploration.
Conclusion
Our results suggest that preceptors balance differing narratives between personal and professional impacts with the benefits of intrinsic rewards compensating for some of the stressors. Overall, teaching family medicine residents was reported to have neither a positive nor negative financial impact. Our results do suggest that the location of preceptor postgraduate training as well as their scope of practice, are linked to their perception of urban-based postgraduate family medicine learners.
There appears to be a possible incongruence between the expectations of rural teaching physicians and UBFM residents, which may fuel preceptor discontent. Future research into both preceptor and learner expectations for the rural postgraduate family medicine rotation may further elucidate whether policy changes or clarification about the purpose of the rotation may be helpful to better serve those involved.
Appendix A. Complete survey.
The Impact of Impact of Urban-based Family Medicine Postgraduate Rotations on Rural Preceptors/Teachers (IMPORT)
(REB19-1258)
Demographics
-
Age group
- <30 Years
- 31-40 Years
- 41-50Years
- 51-60 Years
- >60 Years
-
Gender
- Male
- Female
- Prefer not to say
- Prefer to self-describe
-
Total years in practice
- <5 years
- 6 -10 years
- 11 - 20 years
- 21 - 30 years
- >30 years
-
Size of community you practice in
- Small Rural - population <5,000
- Rural - population 5,000 – 10,000
- Large Rural - population 11,000 – 20,000
- Regional - population 20,000 - 500,000
- Remote - population > 20,000 but < 500,000 AND > 300 km from metropolitan centre
-
Scope of practice in the community
- Primary rural community (Family Practitioners, no obstetrical deliveries, no or only visiting specialists)
- Secondary rural (Family Practitioners and on-site specialists, obstetrical deliveries with OR)
- Regional centre (Hospital primarily specialist based, onsite advanced imaging, full time OR and ICU)
-
Total years teaching any medical learner
- <5 years
- 6-10 years
- 11-20 years
- 21-30 years
- >30 years
-
Total years teaching assigned urban-based Family Medicine residents
- <5 years
- 6-10 years
- 11-20 years
- 21-30 years
- >30 years
-
How many months in the year are you scheduled to supervise an urban FM resident?
- <2 months
- >2 and <6 months
- >6 months
-
Where did you complete your residency?
- Canadian URBAN residency program <=2 months rural exposure
- Canadian URBAN residency program >3 months rural exposure
- Canadian RURAL residency program
- International URBAN residency program
- International RURAL residency program
Survey Questions
Consider the urban based family medicine residents that you have worked with: the most enjoyable as well as the most challenging. Please answer the following questions with a perspective of your overall experience in teaching urban based family medicine residents.
-
What kinds of impact (positive or negative) have you experienced by having urban based family medicine residents in your practice?
-
Please describe any experienced PERSONAL impact? (eg. family, health)

-
Magnitude of Personal Impact
-
Please describe any experienced PROFESSIONAL impact? (eg. work relationships, time, job satisfaction, bookings)
-
Magnitude of Professional Impact
-
Please describe any experienced FINANCIAL impact ?

-
Magnitude of Financial Impact
-
-
If you have challenges or difficulties teaching urban based FM residents, do you discuss your challenges or difficulties in a social support network? (eg. partner/spouse, medical colleagues)
- Yes: on an ongoing regular basis
- Yes: as the need arises
- No
-
If you have challenges or difficulties teaching urban based FM residents, do you discuss your challenges or difficulties in a formal administrative network? (eg. program admin, rural director, formal preceptor meeting)
- Yes: on an ongoing regular basis
- Yes: as the need arises
- No
-
Do you attend formal faculty development events?
- Used to but not now
- Yes: on an ongoing regular basis
- Yes: irregularly
- No
-
How do you think faculty development could help rural preceptors accommodate urban based residents into their practices?

Conflicts of Interest
The authors have no conflicts of interest to declare with respect to this study.
Funding
This was an unfunded study.
References
- 1.Brooks RG, Walsh M, Mardon RE, Lewis M, Clawson A. The roles of nature and nurture in the recruitment and retention of primary care physicians in rural areas: a review of the literature. Acad Med. 2002; 77(8):790-798. 10.1097/00001888-200208000-00008 [DOI] [PubMed] [Google Scholar]
- 2.Australian Institute of Health and WelfareMedical Labour Force 2001. Canberra: Australian Institute of Health and Welfare. 2003; Available at https://www.aihw.gov.au/reports/workforce/medical-labour-force-2001/contents/table-of-contents [Accessed Aug 26, 2020]. [Google Scholar]
- 3.Whitcomb ME. The challenge of providing doctors for rural America. Acad Med.2005; 80(8):715-716. 10.1097/00001888-200508000-00001 [DOI] [PubMed] [Google Scholar]
- 4.Hogenbirk JC, Mian O, Pong RW. Postgraduate specialty training in northeastern Ontario and subsequent practice location. Rural Remote Health. 2011; 11(2):1603. 10.22605/RRH1603 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization How to conduct a discrete choice experiment for health workforce recruitment and retention in remote and rural areas: a user guide with case studies. Geneva: World Health Organization. 2012; Available at https://www.who.int/hrh/resources/dceguide/en/ [Accessed Aug 26, 2020]. [Google Scholar]
- 6.Schmidt S, Gresser U. Development and consequences of physician shortages in Bavaria. Versicherungsmedizin. 2014; 66(1):25-29. [PubMed] [Google Scholar]
- 7.Pathman DE, Steiner BD, Jones BD, Konrad TR. Preparing and retaining rural physicians through medical education. Acad Med. 1999; 74(7):810-820. 10.1097/00001888-199907000-00016 [DOI] [PubMed] [Google Scholar]
- 8.Clark TR, Freedman SB, Croft AJ, et al. Medical graduates becoming rural doctors: rural background versus extended rural placement. Med J Australia. 2013; 199(11):779-782. 10.5694/mja13.10036 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . 2010. Increasing access to health workers in remote and rural areas through improved retention: Global policy recommendations. Geneva: World Health Organization. https://www.who.int/hrh/retention/guidelines/en/ [Accessed Aug 26, 2020]. [PubMed] [Google Scholar]
- 10.College of Family Physicians of Canada . Postgraduate education for rural family practice. Vision and recommendations for the new millennium: a report of the working group on postgraduate education for rural family practice. Can Fam Physician. 1999; 45:2698-2700, 2703,-2704, 2717-2721. [PMC free article] [PubMed] [Google Scholar]
- 11.Bosco C, Oandasan I. Review of family medicine within rural and remote Canada: education, practice, and policy. Mississauga, ON: College of Family Physicians of Canada. 2016. Available at https://portal.cfpc.ca/resourcesdocs/uploadedFiles/Publications/News_Releases/News_Items/ARFM_BackgroundPaper_Eng_WEB_FINAL.pdf [Accessed Aug 5, 2020]. [Google Scholar]
- 12.Malhi, RL, Ornstein J, Myhre D.. The impact of rural rotations on urban based postgraduate learners: a literature review. Med Teach, 2019; 41(7): 830-838. 10.1080/0142159X.2019.1588458 [DOI] [PubMed] [Google Scholar]
- 13.Barritt A, Silagy C, Worley P, Watts R, Marley J, Gill D. Attitudes of rural general practitioners towards undergraduate medical student attachments. Aust Fam Physician. 1997. 26(S2):S87-90. [PubMed] [Google Scholar]
- 14.Baker PG, Dalton L, Walker J. Rural general practitioner preceptors–how can effective undergraduate teaching be supported or improved? Rural Remote Health. 2003; 3(1):107. 10.22605/RRH107 [DOI] [PubMed] [Google Scholar]
- 15.Walters L, Worley P, Prideaux D, Rolfe H, Keaney C. The impact of medical students on rural general practitioner preceptors. Rural Remote Health 2005; 18(3):338-355. 10.1080/13576280500307272 [DOI] [PubMed] [Google Scholar]
- 16.Cuncic C, Regehr G, Frost H, Bates J. It’s all about relationships: a qualitative study of family physicians’ teaching experiences in rural longitudinal clerkships. Perspect Med Educ. 2018; 7(2): 100-109. 10.1007/s40037-018-0416-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waters L, Lo K, Maloney S. What impact do students have on clinical educators and the way they practise? Adv Health Sci Educ. 2018; 23:611-631. 10.1007/s10459-017-9785-y [DOI] [PubMed] [Google Scholar]
- 18.Ingham G, Fry J, O’Meara P, Tourle V. Why and how do general practitioners teach? An exploration of the motivations and experiences of rural Australian general practitioner supervisors. BMC Med Educ. 2015; 15:190. 10.1186/s12909-015-0474-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3(2): 77-101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 20.Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965; 12(4):436–445. 10.2307/798843 [DOI] [Google Scholar]
- 21.Hecker K, Violato C. Medical school curricula: do curricular approaches affect competence in medicine? Fam Med. 2009; 41(6):420-426. [PubMed] [Google Scholar]
- 22.Chong A, Kiroff G. Preparing surgeons for rural Australia: the RACS rural surgical training program. ANZ J Surg. 2015; 85(3):108-112. 10.1111/ans.12880 [DOI] [PubMed] [Google Scholar]
- 23.Szafran O, Myhre D, Torti J, Schipper S. Factors influencing rural career choice of urban background family medicine graduates: a qualitative analysis. Can Med Educ J. 2020; 11(3):e21-e30. 10.36834/cmej.56976 [DOI] [PMC free article] [PubMed] [Google Scholar]


