Abstract
Objective:
To evaluate the influence of an app-based approach in a protocol for domestic oral hygiene maintenance in a group of adolescent patients wearing fixed multibracket appliances.
Materials and Methods:
Eighty adolescent patients scheduled to start an orthodontic multibracket treatment were randomly divided into two groups of 40. Plaque index (PI), gingival index (GI), white spots (WS), and caries presence were recorded in all patients, and they were instructed regarding domestic oral hygiene maintenance on the day of braces application (t0) and every 3 months (t1, t2, t3, t4) during the first year of treatment. Study group (SG) patients were enrolled in a WhatsApp chat room–based competition and instructed to share monthly with the other participants two self-photographs (selfies) showing their oral hygiene status.
Results:
SG patient participation in the chat room was regular and active throughout the observation period. At t2, t3, and t4, SG patients had significantly lower values of both PI and GI and a lower incidence of new WS and caries, compared with the control group.
Conclusion:
Integration of new “social” technologies in a standard oral hygiene motivation protocol is effective in improving compliance of adolescent patients and in improving their oral health status during orthodontic multibracket treatment.
Keywords: App, Oral hygiene, Compliance, Adolescent, Orthodontics
INTRODUCTION
A stable occlusal relationship and pleasant smile esthetics with healthy masticatory function are the main objectives of orthodontic treatment. An ideal alignment of the teeth simplifies domestic oral hygiene maintenance and consequently is supposed to reduce caries and periodontal disease. However, the fixed and removable appliances used for orthodontic treatment, which usually lasts from 18 to 30 months, increase plaque formation and accumulation and make the daily maintenance of oral hygiene status more difficult, with a consequent increase in periodontal inflammation and enamel lesions ranging from white spots (WS) to caries formation.1–7 Multibracket orthodontic treatments are usually performed in adolescent patients who have additional age-related problems: their manual ability and overall motivation regarding oral hygiene maintenance are often suboptimal; worsened esthetic appearance due to the presence of orthodontic appliances, which are often visible, usually leads to reduced self-confidence, feelings of discomfort in interpersonal relationships, and, in extreme cases, bullying; and their refusal of therapy is sometimes perceived to have been imposed by the parents.8
Communication habits, especially between adolescents, are increasingly brief and immediate, using images instead of words. This new way of communicating requires tools such as smartphones and tablets with their multiple apps, which influence communication through their networking capability and immediacy. Progressive lowering of the price of electronic devices and mobile Internet connections has also contributed to the spread of this now universal phenomenon. This represents a challenge throughout the educational field: the old approach, based mainly on reading and listening to standardized content, now requires customization and active involvement, using communication tools that are familiar to adolescents.9,10
The aim of this study was to test the efficacy of an app-based approach applied to a protocol for domestic oral hygiene maintenance in improving hygiene compliance and oral health in a group of adolescent patients wearing fixed multibracket appliances.
MATERIALS AND METHODS
This study enrolled 80 adolescent patients who were scheduled to start orthodontic multibracket treatment, owned a smartphone, and were able to be online daily. Exclusion criteria were the presence of a significant medical history, a restrictive dietary regimen, and difficulties in reading or speaking the national language. The study protocol was approved by the review board of the Dental School of Brescia.
Plaque index (PI), gingival index (GI), WS, and presence of caries were recorded in all patients along with personal data, and a stratified randomization list was produced by an external office, taking into account baseline dental health, gender, age, and socioeconomic status.11–14
All patients were treated with the same fixed orthodontic system (Victory braces, Low Profile series, MBT prescription, 0.022-inch slot, power arm on canines, 3M Unitek, Monrovia, Calif.) applied with an indirect bonding protocol. On the day of braces application (t0), each patient received standardized oral hygiene instructions along with an oral hygiene kit containing toothpaste, toothbrush, mouthwash, interproximal brush, dental floss, and plaque-disclosing tablets. The external office was then contacted for patient allocation to the control group (CG) or study group (SG). SG patients were instructed to download smartphone-specific video tutorials regarding oral hygiene maintenance during their orthodontic treatment, and consent/assent was obtained by these patients and their parents to share self-photographs (selfies) and text messages in a WhatsApp-based anonymous chat room, moderated by one of the authors of the study who was not involved in study measurements.7 In the chat room, the SG patients used a fictional nickname and were forbidden to share photographs or send text messages that could disclose their real identity to other participants. This chat room was named “Brush Game” and all participants were instructed to share two selfies of their teeth weekly, before and after using the plaque-disclosing tablets, to show their ability in maintaining oral hygiene. The patients were also allowed to use this chat room to share information, pictures, and movies regarding oral hygiene and orthodontic treatment. Each Saturday, the moderator, after visual evaluation of the patients' photographs and level of participation in the chat room, published a ranking of the five best participants of the week.
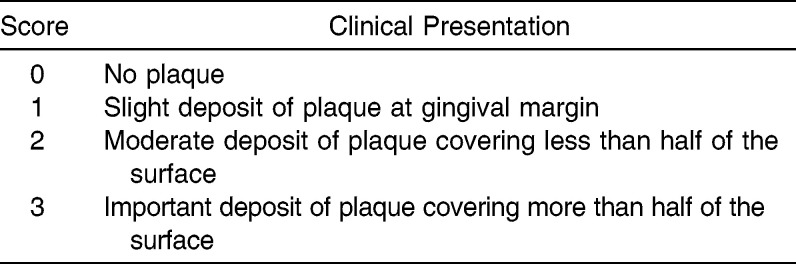
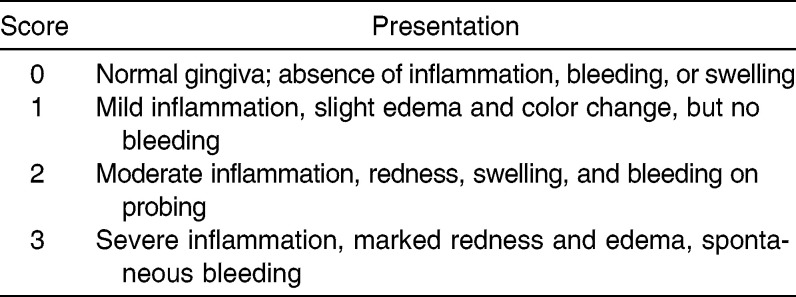
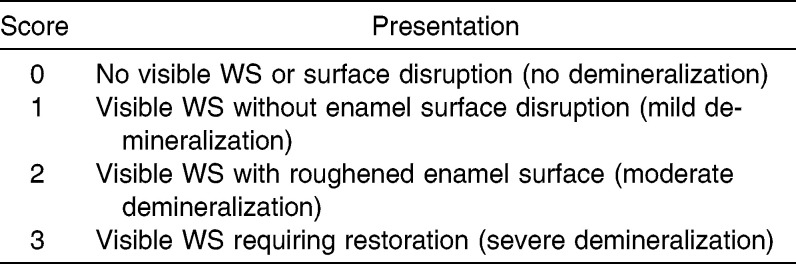
Every 3 months (t1, t2, t3, t4) during the first year of orthodontic treatment, all patients were examined, and PI, GI, WS, and caries presence were recorded by the same blinded examiner. PI was scored by evaluating the presence of plaque at four surfaces (mesial, buccal, distal, and lingual) of tooth 1.6, 1.2, 2.4, 3.6, 3.2, and 4.4, assigning a score from 0 to 3 for each surface, and calculating the mean overall value. PI scoring is described in Table 1. GI was scored by evaluating the presence of inflammation on the same teeth as for PI and assigning a score from 0 to 3 as described in Table 2. Buccal WS presence on each bonded tooth was scored after 5 seconds of air drying and assigned a score from 0 to 3 as described in Table 3.15 Caries presence and extent was visually and radiographically evaluated and recorded.
Table 1.
Plaque Index Measurements
Table 2.
Gingival Index Measurements
Table 3.
White Spots (WS) Measurements
An a priori sample size (n) calculation, with the periodontal indices as the main outcomes, was performed, fixing a power (β) of 90% (zβ = 1.28) and an α of 5% (zα/2 = 1.96), considering clinically significant a difference of 0.25 in the means (μ) of the outcomes between the two groups, with a standard deviation (σ) of 0.5 estimated from a previously performed pilot study, using the following formula:
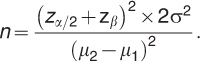 |
The rater repeatability in measuring PI, GI, WS extent, and presence of caries was evaluated at each time point using the intraclass correlation coefficient (ICC) applied to double measurements recorded twice at an interval of 1 hour from 10 randomly selected patients. ICC was interpreted as follows: values ≤ 0.20 indicated poor agreement; 0.21–0.30, slight agreement; 0.31–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.70, substantial agreement; 0.71–0.80, strong agreement; 0.81–0.99, almost perfect agreement; and 1, perfect agreement.
After a descriptive statistical analysis of all collected data, Shapiro-Wilk normality test and Levene test for equality of variances were performed. For the continuous variables PI and GI, mean intragroup differences among t0, t1, t2, t3, and t4, were analyzed with the Friedman test; intergroup differences at t0, t1, t2, t3, and t4, were analyzed with the Wilcoxon-Mann-Whitney test. Mean intergroup differences across t0, t1, t2, t3, and t4 for the ordinal variable “WS lesion” were analyzed with the Pearson chi-square test after converting WS into an absence (score = 0) or presence (scores = 1, 2, or 3) dichotomous nominal variable; Cochran Q test, followed by the post-hoc pairwise McNemar test with Bonferroni correction, was applied to identify significant intragroup changes across the time points. SPSS software version 22 (IBM, Armonk, NY) was used for all calculations.
RESULTS
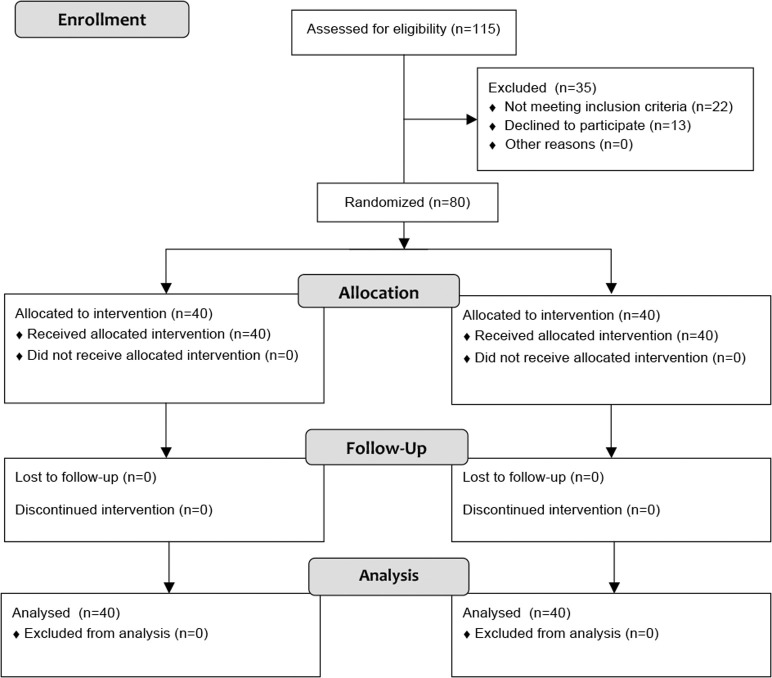
Ninety-three consecutive patients matching the inclusion/exclusion criteria were asked to participate in the present study to achieve 80 participants (ie, 13 did not agree to participate). At t0, the CG patients (17 boys and 23 girls) had a mean age of 13.6 years; the SG patients (17 boys and 23 girls) had a mean age of 14.1 years. Any dropout was registered (Figure 1).
Figure 1.
CONSORT 2010 flow diagram.
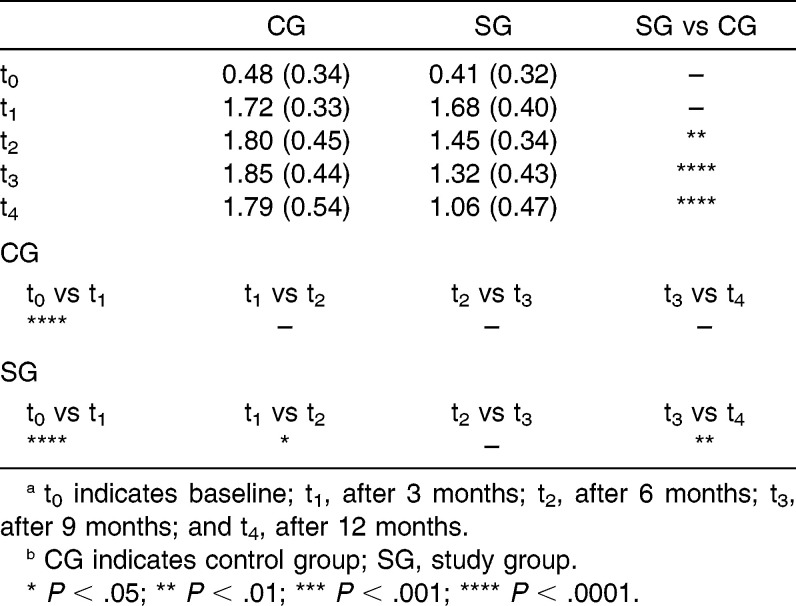
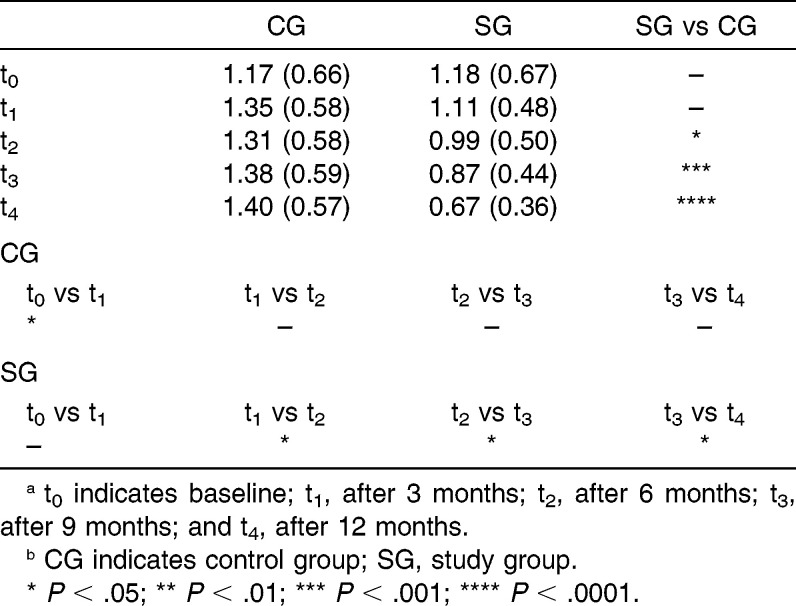
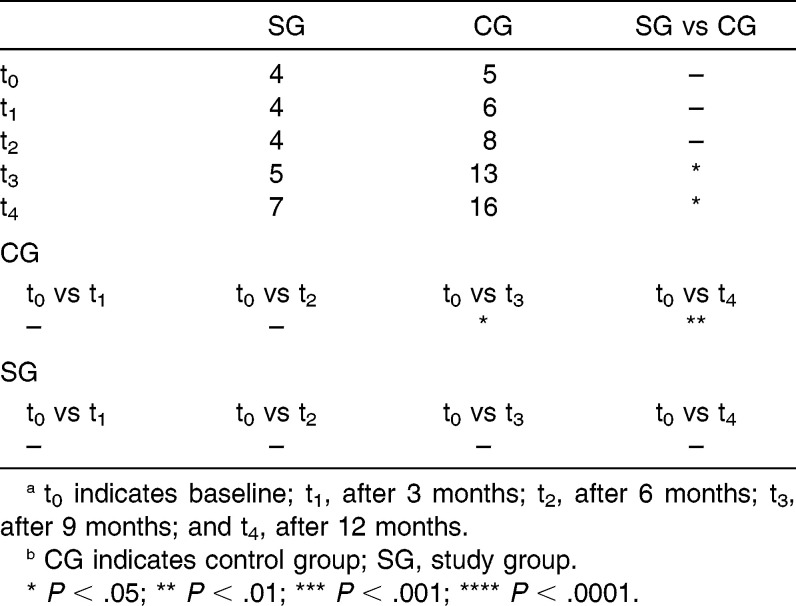
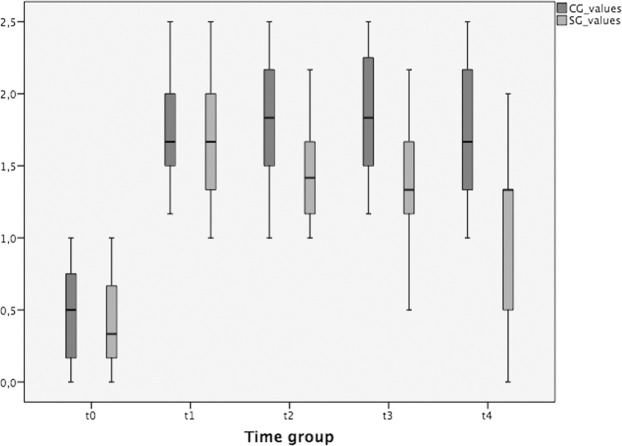
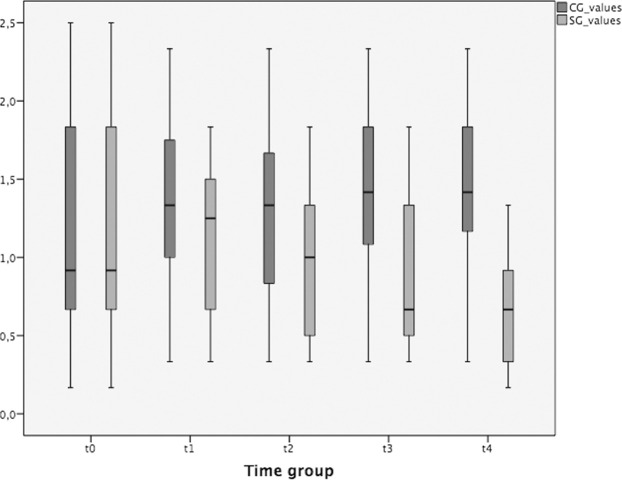
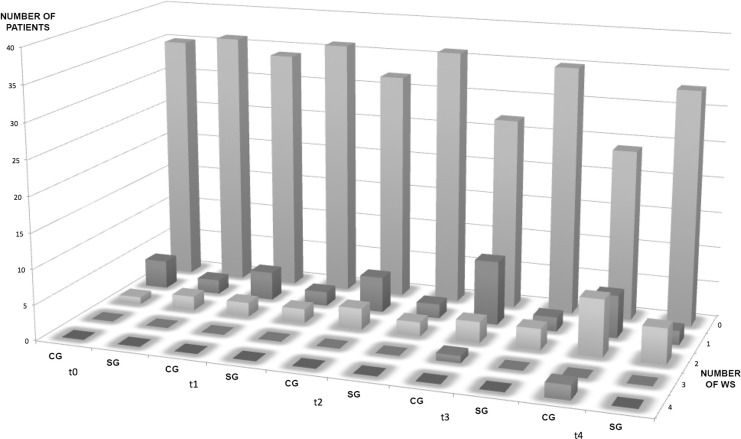
ICC values indicated almost perfect repeatability of evaluator measurements, ranging from 0.88 to 0.95. PI, GI, and WS values at the five time points are summarized in Tables 4 through 6. Any new caries formation during the trial was recorded. At t0 and t1, no difference was found between the CG and SG. At t2, t3, and t4, the statistical significance of intergroup differences regarding PI and GI increased progressively, whereas differences regarding WS values were found to be statistically significant only at t3 and t4. Intragroup analysis revealed an improvement regarding PI between t1 and t2 and between t3 and t4 in SG patients that was not found in the CG; similar results were obtained regarding GI, with a constant improvement from t1 to t4 in SG patients that was not found in the CG; incidence of WS lesions was significantly higher, compared to t0 (12.5% of patients with preexisting WS lesions), at t3 (32.5%) and t4 (40.0%) within the CG, whereas in the SG there was not any significant difference across the time points (t0 10%, t3 12.5%, t4 17.5%). Variations in PI, GI, and WS presence are represented graphically in Figures 2 through 4, respectively.
Table 4.
Mean (SD) Plaque Index Scores at t0, t1, t2, t3, t4ab
Table 5.
Mean (SD) Gingival Index Scores at t0, t1, t2, t3, t4ab
Table 6.
Number of Patients With White Spots at t0, t1, t2, t3, t4ab
Figure 2.
PI trend during the study.
Figure 3.
GI trend during the study.
Figure 4.
WS trend during the study.
DISCUSSION
This study investigated the efficacy of app-based chat room participation in improving oral hygiene compliance in a group of adolescent patients wearing fixed multibracket appliances. We collected data on PI, GI, WS, and the presence of caries because these indicators are widely used and accepted for the evaluation of oral hygiene and dental health. We excluded patients with restricted dietary regimens because these have been found to influence the incidence of WS lesions.16,17
The baseline (t0) oral and personal characteristics of the control and study subjects were similar due to a stratified randomization procedure performed to maximize initial group homogeneity. Furthermore, we adopted in all patients a specific indirect bonding protocol that limits the extent of the area that is unnecessarily etched around the brace base to minimize differences in plaque accumulation due to undetected changes in enamel surface integrity.18,19 After 3 months (t1), we did not find any statically significant difference between the CG and SG patients, whereas subsequent (t2, t3, and t4) SG performance was significantly better for all parameters with the exception of onset of new caries, for which no difference was observed between the groups throughout the duration of the trial.
Several studies have demonstrated that the first months after braces placement are the most challenging for patients who have to familiarize themselves with and acquire new manual abilities to maintain the orthodontic appliance in a proper hygienic condition. This can have an effect on motivation and could explain why the performance of the two groups, as measured by PI and GI, was similar at t1. During the middle part of orthodontic treatment, patient enthusiasm and motivation tend to decrease progressively, often leading to worsening oral hygiene. At this time, motivational strategies play a crucial role in maintaining adequate compliance until the final phase of treatment, when patients' motivation usually increases due to the approach of braces debonding.
We know from the literature that even 3 weeks of incomplete plaque removal around braces can be enough for WS to develop; usually, they appear clinically after the first 6 months of treatment. For this reason, we conducted our study over the first year of treatment, and, indeed, differences in the incidence of new WS between SG and CG patients became evident only from t3. We did not find any new caries in either group. This could be a consequence of the fact that all patients were aware that they were involved in a scientific study and that the CG patients may have felt psychological pressure regarding their personal performance. It could also be due to the efficacy of our traditional oral hygiene maintenance and instruction protocol, which we have used for a long period of time in all of our orthodontic patients.
We have noticed increasing interest during the last 5 years in the use of new technologies in orthodontic patient motivation protocols, with several studies demonstrating the efficacy of short message service (SMS) and e-mail reminders in improving patient compliance with and acceptance of orthodontic treatment.20–27 In general dentistry, it is sometimes difficult for the treating dentist and dental staff to educate the patient to understand fully the importance of the given recommendations and to motivate him or her to maintain compliance throughout the treatment. This is particularly the case in orthodontics because of the usually young age of the patients who struggle to focus on the future benefit of their treatment and tend to concentrate on the present esthetic impairment and discomfort. Invisible appliances such as lingual braces and transparent aligners are increasingly being used in adolescent patients but still require active cooperation for the constant wearing of removable appliances and tolerance of lingual braces.28–33
In summary, it appears evident that means of communication must be evaluated, identified, and customized for each patient to achieve optimal compliance and maximize treatment success. Compared with traditional approaches, we consider interactive multimedia and visual materials, administered through familiar communication channels, to be more appropriate for communicating with and motivating adolescent patients. Furthermore, they allow the direct involvement of these young patients in their treatment and make them more responsible for their health, bypassing the need for parent mediation. The present study demonstrates the enthusiasm and active participation of the study subjects in the chat room; all patients uploaded their selfies punctually and some uploaded extra content, such as video tutorials and images, regarding oral hygiene and orthodontic treatment, thereby creating a community of peers sharing their experiences. This underlines how the use of a platform, already well known to and in common use by adolescent patients, can improve their involvement and consequently their collaboration during orthodontic treatment.
After careful consideration of privacy and legal issues, the use of a web-based chat room should be recommended to all orthodontists to improve the oral hygiene compliance of their adolescent patients; the use of social networks or dedicated interactive multimedia could be a step in implementing this innovative approach. A similar approach could also be introduced in other fields of dentistry when is important to have strong patient compliance.
CONCLUSIONS
Weekly sharing of selfies of their smiles in a WhatsApp-based chat room contest is an effective and long-lasting way to improve oral hygiene compliance in adolescent orthodontic patients.
This innovative approach is also effective in decreasing incidence of white spot lesions during the first year of treatment with a multibracket appliance.
REFERENCES
- 1.Cantekin K, Celikoglu M, Karadas M, Yildirim H, Erdem A. Effects of orthodontic treatment with fixed appliances on oral health status: a comprehensive study. J Dent Sci. 2011;6:235–238. [Google Scholar]
- 2.Chapman J, Roberts W, Eckert G, Kula K, Gonzalez-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;138:188–194. doi: 10.1016/j.ajodo.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Hadler-Olsen S, Sandvik K, El-Agroudi MA, Øgaard B. The incidence of caries and white spot lesions in orthodontically treated adolescents with a comprehensive caries prophylactic regimen—a prospective study. Eur J Orthod. 2012;34:633–699. doi: 10.1093/ejo/cjr068. [DOI] [PubMed] [Google Scholar]
- 4.Lundstrom F, Krasse B. Caries incidence in orthodontic patients with high levels of Streptococcus mutans. Eur J Orthod. 1987;9:117–121. doi: 10.1093/ejo/9.2.117. [DOI] [PubMed] [Google Scholar]
- 5.Machen D. Legal aspects of orthodontic practice: risk management concepts. Am J Orthod Dentofacial Orthop. 1991;100:93–94. [PubMed] [Google Scholar]
- 6.Migliorati M, Isaia L, Cassaro A, et al. Efficacy of professional hygiene and prophylaxis on preventing plaque increase in orthodontic patients with multibracket appliances: a systematic review [published online ahead of print September 22, 2014] Eur J Orthod. doi: 10.1093/ejo/cju044. pii: cju044. [DOI] [PubMed] [Google Scholar]
- 7.Zachrisson BU, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand J Dent Res. 1971;79:394–401. doi: 10.1111/j.1600-0722.1971.tb02028.x. [DOI] [PubMed] [Google Scholar]
- 8.Olivieri A, Ferro R, Benacchio L, Besostri A, Stellini E. Validity of Italian version of the Child Perceptions Questionnaire (CPQ11-14) BMC Oral Health. 2013;13:55. doi: 10.1186/1472-6831-13-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mas FG, Plass J, Kane WM, Papenfuss RL. Health education and multimedia learning: educational psychology and health behavior theory (Part 1) Health Promot Pract. 2003;4:288–292. doi: 10.1177/1524839903004003013. [DOI] [PubMed] [Google Scholar]
- 10.Mas FG, Plass J, Kane WM, Papenfuss RL. Health education and multimedia learning: connecting theory and practice (Part 2) Health Promot Pract. 2003;4:464–469. doi: 10.1177/1524839903255411. [DOI] [PubMed] [Google Scholar]
- 11.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 12.Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967;38:610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 13.Tufekci E, Dixon J, Gunsolley J, Lindauer S. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–210. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rösing CK. Association between gingival bleeding and gingival enlargement and oral health-related quality of life (OHRQoL) of subjects under fixed orthodontic treatment: a cross-sectional study. BMC Oral Health. 2012;12:53. doi: 10.1186/1472-6831-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–647. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laffranchi L, Zotti F, Bonetti S, Dalessandri D, Fontana P. Oral implications of the vegan diet. Observational study. Minerva Stomatol. 2010;59:583–591. [PubMed] [Google Scholar]
- 17.Zotti F, Laffranchi L, Fontana P, Dalessandri D, Bonetti S. Effects of the fluorotherapy on oral changes caused by a vegan diet. Minerva Stomatol. 2014;63:179–188. [PubMed] [Google Scholar]
- 18.Menini A, Cozzani M, Sfondrini MF, Scribante A, Cozzani P, Gandini P. A 15-month evaluation of bond failures of orthodontic brackets bonded with direct versus indirect bonding technique: a clinical trial. Prog Orthod. 2014;15:70. doi: 10.1186/s40510-014-0070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalessandri D, Dalessandri M, Bonetti S, Visconti L, Paganelli C. Effectiveness of an indirect bonding technique in reducing plaque accumulation around braces. Angle Orthod. 2012;82:313–318. doi: 10.2319/041811-273.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vervloet M, Linn AJ, van Weert JC, de Bakker DH, Bouvy ML, van Dijk L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19:696–704. doi: 10.1136/amiajnl-2011-000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Car J, Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2012;7:CD007458. doi: 10.1002/14651858.CD007458.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12:CD007457. doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012;12:CD007459. doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armstrong AW, Watson AJ, Makredes M, Frangos JE, Kimball AB, Kvedar JC. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Arch Dermatol. 2009;145:1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- 25.Shegog R, Markham C, Peskin M, Dancel M, Coton C, Tortolero S. “It's your game”: an innovative multimedia virtual world to prevent HIV/STI and pregnancy in middle school youth. Stud Health Technol Inform. 2007;129:983–987. [PubMed] [Google Scholar]
- 26.Pinto A, Selvaggi S, Sicignano G, et al. E-learning tools for education: regulatory aspects, current applications in radiology and future prospects. Radiol Med. 2008;113:144–157. doi: 10.1007/s11547-008-0227-z. [DOI] [PubMed] [Google Scholar]
- 27.Eppright M, Shroff B, Best AM, Barcoma E, Lindauer SJ. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2014;84:208–213. doi: 10.2319/062813-481.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goren S, Zoizner R, Geron S, Romano R. Lingual orthodontics versus buccal orthodontics: biomechanical and clinical aspects. J Lingual Orthod. 2003;3:1–7. [Google Scholar]
- 29.Wu A, McGrath C, Wong RW, Wiechmann D, Rabie AB. Comparison of oral impacts experienced by patients treated with labial or customized lingual fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2011;139:784–790. doi: 10.1016/j.ajodo.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 30.Dalessandri D, Lazzaroni E, Migliorati M, Piancino MG, Tonni I, Bonetti S. Self-ligating fully customized lingual appliance and chair-time reduction: a typodont study followed by a randomized clinical trial. Eur J Orthod. 2013;35:758–765. doi: 10.1093/ejo/cjs093. [DOI] [PubMed] [Google Scholar]
- 31.Schott TC, Göz G. Color fading of the blue compliance indicator encapsulated in removable clear Invisalign Teen® aligners. Angle Orthod. 2011;81:185–191. doi: 10.2319/052610-288.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buschang PH, Shaw SG, Ross M, Crosby D, Campbell PM. Comparative time efficiency of aligner therapy and conventional edgewise braces. Angle Orthod. 2014;84:391–396. doi: 10.2319/062113-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper-Kazaz R, Ivgi I, Canetti L, et al. The impact of personality on adult patients' adjustability to orthodontic appliances. Angle Orthod. 2013;83:76–82. doi: 10.2319/010312-6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]