Abstract
Objective:
To compare the extent of canine distalization and the transversal changes, postdistalization gingival indices, and mobility scores between patients who were undergoing orthodontic treatment involving upper premolar extraction with (experimental group) or without piezocision.
Materials and Methods:
Twenty maxillary canines of 10 patients were evaluated with split mouth design. Pre- and postdistalization dental casts were prepared and scanned with an orthodontic scanner to compare the extent of distalization and transversal changes between the two groups. The pre- and postdistalization gingival indices and mobility scores were also calculated.
Results:
Three-dimensional analysis of the models revealed significant differences in tooth movement (lesser anchorage loss and greater canine distalization) between the experimental and control groups. Furthermore, the distalization time was shortened in the experimental group. There were no differences in the transversal changes, pre- and postdistalization gingival indices, or mobility scores between groups.
Conclusion:
Piezocision-assisted distalization accelerates tooth movement, decreases the anchorage loss for posterior teeth, and does not induce any maxillary transversal change. Moreover, piezocision does not have any adverse effects on periodontal health.
Keywords: Piezocision, Malocclusion, Model, Piezosurgery, Rapid
INTRODUCTION
An increasing number of patients are demanding orthodontic treatment for improved esthetics and/or a better mastication system.1 One of the important challenges of orthodontic treatment faced by both patients2 and orthodontists is the treatment duration. The rate of biological orthodontic tooth movement is approximately 1 mm over 4 weeks. Accordingly, in cases of upper premolar extraction and maximum anchorage, distalization of canines can take almost 7 months, leading to total treatment duration of 2 years.2 To face this challenge, several surgical techniques have been developed and attempted, including periodontal ligament distraction,3 micro-osteoperforations,4 and piezopuncture.5
Recently, Kim et al.6 and Dibart et al.7 introduced a minimally invasive technique as an alternative to induce surgical damage to the alveolar bone without any flap surgery. This technique, also known as piezocision, involved the insertion of a scalpel and mallet into the gingiva and the placement of incisions using an ultrasonic tool (piezocision). These incisions or bone injuries are responsible for the initiation of a deciduous demineralization process called the regional acceleratory phenomenon (RAP). The transient osteopenia associated with this phenomenon causes rapid tooth movement because the teeth move in a pliable environment.8,9 Because of the induced RAP effect, a pliable environment is expected after piezocision,4,7 which can lead to maxillary constriction and/or crossbites for posterior teeth.
Elastomeric power chains are often used in orthodontic practice, especially for closing spaces. Their advantages are no patient cooperation required, low cost, smooth surface, and their irritation-free nature.10,11 The objectives of this research were to evaluate the effectiveness of piezocision-assisted canine distalization using three-dimensional (3D) measurements and to assess the transversal changes, postdistalization gingival status, and mobility scores.
MATERIALS AND METHODS
This study was approved by the ethical committee at Bezmialem Vakif University. Patients indicated for maxillary first premolar extraction and bilateral canine distalization were selected from those with half or more unit Class II malocclusion. All patients had to fulfill the following criteria: healthy systemic condition and no previous orthodontic treatment. All patients were also required to have good oral hygiene, probing depth of <3 mm (measured from the bottom of the sulcus to the most apical portion of the gingival margin), no loss of periodontal attachment, and no radiographic evidence of bone loss. The study involved a split-mouth design, with the experimental quadrant selected by randomization. Twenty maxillary canines of 10 patients fulfilled all the inclusion criteria and were included. The mean age of the patients was 16.3 ± 2.4 years, including six female and four male patients. The hand-wrist radiographs revealed that all of the patients were not growing and in the adult stage, except one male patient who was in the postpeak stage.
Roth’s prescription edgewise brackets (Master Series, American Orthodontics, Sheboygan, Wis) with 0.022-inch slots were used. The teeth were leveled and aligned before canine distalization with moderate anchorage.
Before canine distalization and after the alignment and leveling phases, piezocision was performed on the experimental side. Following the induction of local anesthesia, two vertical interproximal incisions were placed through the periosteum and below the interdental papilla (not including free gingiva) on the mesiobuccal and distobuccal sides of the maxillary canines using a No. 15 blade. The grooves between the roots of the neighboring teeth were the reference for the cut lines. Vertical interproximal incisions were performed, 5 mm apical to the mesial and distal interdental papilla of the maxillary canines. Incision lengths were approximately 10 mm apically. A piezosurgery knife (BS1 insert, Piezotome, Satelec Acteon, Merignac, France) was used to create cortical alveolar incisions with a depth of 3 mm (Figure 1). The depths were verified by the millimetric signs on the piezosurgery knife. The upper 0.016 × 0.022-inch stainless steel archwire was ligated. The distalization phase was initiated after piezocision on the experimental side using elastomeric chains with an approximate force of 150 g measured using a force gauge. For the control side, distalization was started at the same time with the same mechanics. Patients were examined at 2-week intervals, and the elastomeric chains were replaced at each appointment until ideal Class I canine relationships were established. Both canines of each patient were planned to be distalized in terms of millimeters.
Figure 1.

Piezoelectric corticotomy.
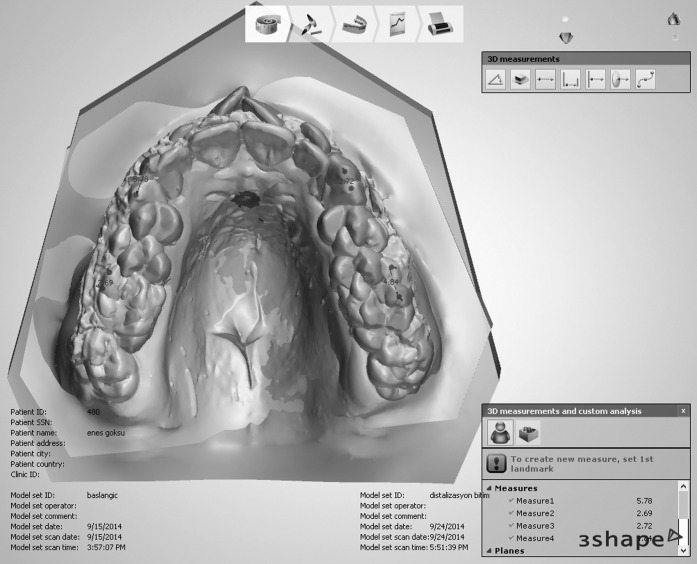
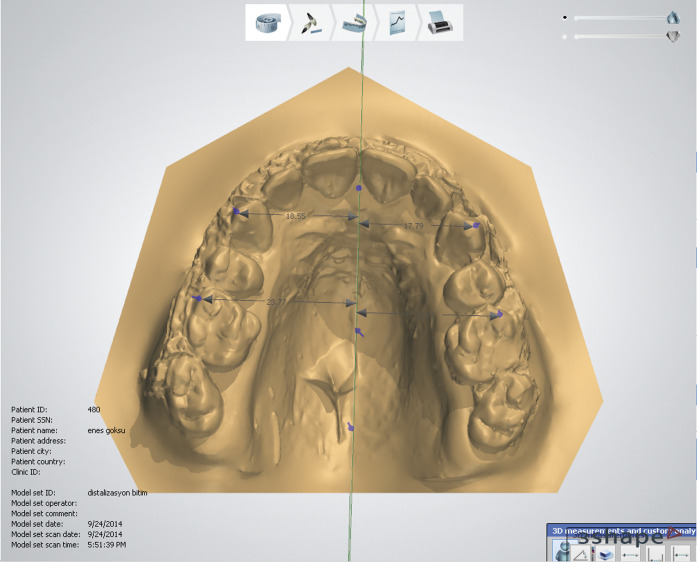
Pre- and postdistalization model casts were scanned using the 3Shape R900 scanner (3Shape A/S, Copenhagen, Denmark; Figure 2). The models were superimposed, and the changes in the models were evaluated for canine distalization changes (Figure 3). The superimpositions were performed by selecting the medial end of the third palatal rugae as reference points. The usage of these points has been performed in similar researches.12,13 The canine and molar positions were defined in superimposed views, and the pre- and postdistalization distances were measured. The pre- and postdistalization mobility scores and gingival indices for the canines were also evaluated and scored. The Muhleman’s index was used to assess mobility in our study14 as per the following scoring system: 0, no mobility; 1, >0.5 and <1 mm of mobility buccolingually; 2, >1 mm and <2 mm of mobility buccolingually; 3, >2 mm of mobility buccolingually; and 3+, both vertical and buccolingual mobility. In the current study, the Silness and Loe gingival index was used. It scores the marginal and interproximal tissues separately on the basis of 0 to 3. The criteria are 0 = normal gingiva, 1 = mild inflammation, 2 = moderate inflammation, 3 = severe inflammation.15 The transversal changes in the models were evaluated by using a midline plane following the incisive papilla and midpalatal raphe as described by Hoggan and Sadowsky.12 The distance from the canine cusp tip to the midline plane and the first molar mesiobuccal cusp tip to the midline plane was measured for pre- and postdistalization models on two separate occasions by a single examiner (Figure 4). The examiner who was responsible for the measurements was blinded.
Figure 2.

Three-dimensional analysis unit.
Figure 3.
Three-dimensional superimpositions of the models.
Figure 4.
Three-dimensional transversal measurements.
The initial measurements were repeated after 1 week. Spearman’s rho coefficients were calculated to analyze repeatability. For statistical analysis, because of nonnormal distribution, the Wilcoxon signed rank test was used to compare canine distalization, anchorage loss in the molar region, and transversal changes between the two groups. A probability of .05 was accepted as significance. All statistical analyses were performed using the Statistical Package for the Social Sciences software system (SPSS 13, SPSS, Chicago, Ill).
RESULTS
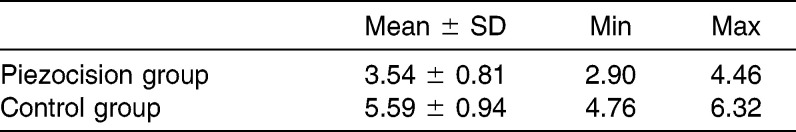
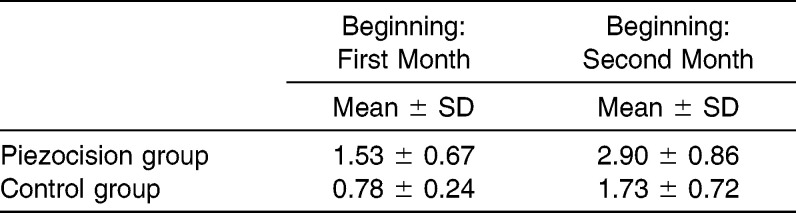
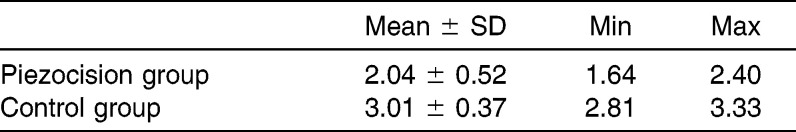
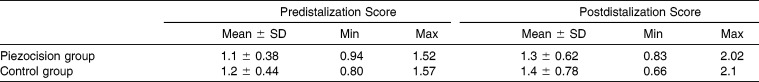
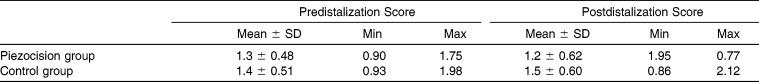
For error analysis, coefficients were found to be close to 1.00. In addition, five three-dimensional models were superimposed 1 week later, and all measurements were performed to check error analyses of the tooth movements. The results ranged from .909 to .983. Piezocision-assisted canine distalization decreased the total treatment duration and anchorage loss in the molar region. It also decreased the duration of canine distalization (Table 1). Similarly, the amount of canine distalization was greater in the piezocision group (Table 2). The anchorage loss for the first molars, measured in millimeters, was lesser and the canine distalization was greater in the piezocision group than in the control group (Table 3).
Table 1.
Time Elapsed for Canine Distalization (Months)
Table 2.
Amount of Canine Distalization (mm)
Table 3.
Molar Anchorage Loss (mm)
The pre- and postdistalization mobility scores were not significantly different between the piezocision and control groups (Table 4). However, the postdistalization mobility increased, although not significantly (P > .05), in both groups.
Table 4.
Mobility Scores
Similarly, there was no significant difference in the pre- and postdistalization gingival indices between the two groups (Table 5). Although all patients were firmly instructed to maintain regular oral hygiene, two patients exhibited an increased gingival index on both sides because of poor oral hygiene.
Table 5.
Gingival Index Scores
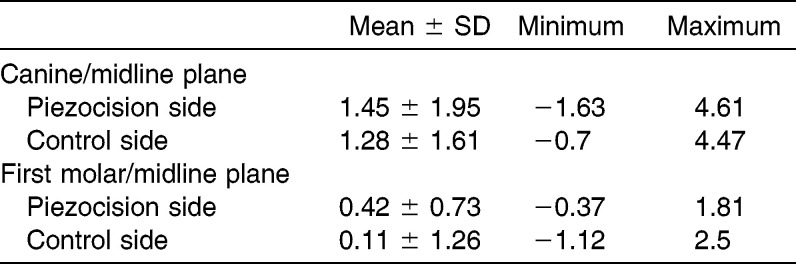
For transversal measurements, there was no significant difference between the two groups (Table 6). The results indicated that there was a slight increase in the distance from midline plane/canine and midline plane/first molar for pre- and postdistalization.
Table 6.
Pre- and Postdistalization Differences of Distances From Canine/Midline Plane and First Molar/Midline Plane (mm)
DISCUSSION
In the current study, RAP was evaluated for teeth subjected to piezocision; elastomeric chains were used with the application of optimal force for canine movement within the optimal biological limits. Compared with other similar techniques, piezocision is a minimally invasive surgical technique. The major novelty is the one-sided approach only from the buccal side; there is no requirement for intervention from the palatal or lingual side. Placement of incisions around the tooth is necessary when rapid movement is planned. Furthermore, RAP is a transient phenomenon; therefore, patients must be evaluated every 2 weeks during treatment.7,16 The effects of RAP can diminish with a decrease in tooth movement velocity over time, although the effects have been reported to last for approximately 4 months.14,17
Elastomeric chains can be preferred for space closures.10 Dixon et al.10 studied power chains and nickel titanium coil springs and concluded that although coil springs gave more rapid tooth movement, power chains were effective on space closure and they were a cheaper option for orthodontic treatment. Nightingale and Jones18 revealed power chains to be as effective as nickel titanium coil springs for retraction. It was also stated that nickel titanium coil springs, power chains, elastic threads, and magnets are all able to provide optimum tooth movement.19
The results of the current study revealed that the rate of tooth movement in the control group was similar to the rate of biological tooth movement, which is 1 to 1.5 mm over 4 weeks.2 Statistical analysis revealed an accelerated canine distalization procedure in the piezocision group approximately two times faster than the control group. This result is in accordance with Aboul-Ela et al.20 Leethanakul et al.21 reported a canine distalization of 5.4 mm over 3 months when interseptal bone reduction was performed before distalization. In the current research, the canine distalization phase was completed in 3.5 months in the experimental group. Similarly, Aboul-Ela et al.20 reported that a Class I canine relationship was established in 2 or 3 months in the experimental sides with corticotomy. The results of these studies are therefore similar, although piezocision is less traumatic and easier to perform compared with interseptal bone reduction.
The amount of canine distalization was 1.53 mm in the piezocision group for the first month. The amount decreased to 1.37 mm for the second month. These results were significantly higher than the control group. Aboul-Ela et al.20 found that a 1.89-mm corticotomy assisted canine distalization for the first month and a 1.83-mm corticotomy for the second month in their accelerated tooth movement study. Sousa et al.22 revealed 1.16-mm laser-assisted canine distalization for the first month and 0.89-mm distalization for the second month in their accelerated tooth movement study with a diode laser.
The cusp tips of the teeth were chosen as the measuring landmarks instead of the labial surfaces of the teeth. Gianelly23 used labial surfaces to determine the widest widths to prevent confusion when selected cusp tips were not distinct. These measurement points can have reasonable effects but should not be used for every study. In a similar study performed by Sukurica et al.,24 cusp tips were used. In the current study, the cusp tips were selected because of their good visibility and easy use with the 3D model analysis system. This research was undertaken to determine the effect of piezocision-assisted canine distalization on transverse dimensions. The distance from the canine/midline plane increased after distalization, and this result is consistent with a similar study performed by Luppanapornlarp and Johnston.25 Paquette et al.26 found an increase of approximately 1.0 mm in the mandibular intercanine width after extraction therapy. This is also in accordance with our study results. The difference in midline plane/first molar distance increased after distalization. The usual expectation is that the posterior region of the maxillary arch becomes narrower as the molars move anteriorly into the narrower part of the arch during space closure. However, Gianelly23 found no change for intermolar widths after extraction therapy. In the current study, slight increases were detected for the midline plane/first molar width after canine distalization. Similarly, Johnson and Smith27 stated that transverse arch width was maintained or slightly enlarged after extraction.
In the current study, no dangerous side effects on the periodontium have been observed with the gingival index.15 After piezocision, it can be difficult to brush around the canine region; moreover, the gingival index can change because of the periodontal incisions. Plaque accumulation can increase around brackets, and patients with poor oral hygiene have a greater tendency to develop periodontal problems. In addition, elastomers exhibited an increased number of microorganisms when compared with stainless steel ligation.28,29 So, the patients were informed and educated about oral hygiene. However, there was no difference in the pre- and postdistalization gingival health of the upper canines between the piezocision and control groups in our study. The Muhleman’s index was used to assess mobility in our study.14 There was no difference in pre- and postdistalization mobility scores between the two groups, although the scores increased after distalization in both groups. These results are in agreement with similar rapid tooth movement research performed with corticotomies.20,30,31
In the current study, no complications or side effects were observed. Similarly, there have been no complications related to piezocision reported in the dental literature until now. Because piezocision is similar to corticosion techniques, there can be interdental bone loss or periodontal defects.32 Postoperative swelling or hematoma can also be observed after corticotomy applications.33
CONCLUSIONS
Piezocision-assisted canine distalization increases the velocity of canine distalization and decreases the overall treatment duration.
Piezocision is also helpful for posterior anchorage control. It aids in maintaining the molars in a more stable position compared with conventional distalization.
There was no difference in the gingival and mobility indices before and after distalization in our study, indicating that piezocision does not negatively affect periodontal health.
There is no maxillary constriction after piezocision. Thus, piezosurgical incisions can be used safely without any narrowing the transversal dimensions.
REFERENCES
- 1.Mathews DP, Kokich VG. Managing treatment for the orthodontic patient with periodontal problems. Semin Orthod. 1997;3:21–38. doi: 10.1016/s1073-8746(97)80037-0. [DOI] [PubMed] [Google Scholar]
- 2.Pilon JJ, Kuijpers-Jagtman AM, Maltha JC. Magnitude of orthodontic forces and rate of bodily tooth movement: an experimental study. Am J Orthod Dentofacial Orthop. 1996;110:16–23. doi: 10.1016/s0889-5406(96)70082-3. [DOI] [PubMed] [Google Scholar]
- 3.Liou EJ, Polley JW, Figueroa AA. Distraction osteogenesis: the effects of orthodontic tooth movement on distracted mandibular bone. J Craniofac Surg. 1998;9:564–571. [PubMed] [Google Scholar]
- 4.Alikhani M, Raptis M, Zoldan B, et al. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144:639–648. doi: 10.1016/j.ajodo.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Kim YS, Kim SJ, Yoon HJ, Lee PJ, Moon W, Park YG. Effect of piezopuncture on tooth movement and bone remodeling in dogs. Am J Orthod Dentofacial Orthop. 2013;144:23–31. doi: 10.1016/j.ajodo.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Kim SJ, Moon SU, Kang SG, Park YG. Effects of low-level laser therapy after corticision on tooth movement and paradental remodeling. Lasers Surg Med. 2009;41:524–533. doi: 10.1002/lsm.20792. [DOI] [PubMed] [Google Scholar]
- 7.Dibart S, Surmenian J, Sebaoun JD, Montesani L. Rapid treatment of Class II malocclusion with piezocision: two case reports. Int J Periodontics Restorative Dent. 2010;30:487–493. [PubMed] [Google Scholar]
- 8.Frost HM. The biology of fracture healing: an overview for clinicians. Part II. Clin Orthop Relat Res. 1989:294–309. [PubMed] [Google Scholar]
- 9.Frost HM. The biology of fracture healing: an overview for clinicians. Part I. Clin Orthop Relat Res. 1989:283–293. [PubMed] [Google Scholar]
- 10.Dixon V, Read MJ, O’Brien KD, Worthington HV, Mandall NA. A randomized clinical trial to compare three methods of orthodontic space closure. J Orthod. 2002;29:31–36. doi: 10.1093/ortho/29.1.31. [DOI] [PubMed] [Google Scholar]
- 11.Kanuru RK, Azaneen M, Narayana V, Kolasani B, Indukuri RR, Babu PF. Comparison of canine retraction by in vivo method using four brands of elastomeric power chain. J Int Soc Prev Community Dent. 2014;4:S32–S37. doi: 10.4103/2231-0762.144586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoggan BR, Sadowsky C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofacial Orthop. 2001;119:482–488. doi: 10.1067/mod.2001.113001. [DOI] [PubMed] [Google Scholar]
- 13.Almeida MA, Phillips C, Kula K, Tulloch C. Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod. 1995;65:43–48. doi: 10.1043/0003-3219(1995)065<0043:SOTPRA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Muhlemann HR. Tooth mobility: a review of clinical aspects and research findings. J Periodontol. 1967;38(suppl):686–713. doi: 10.1902/jop.1967.38.6_part2.686. [DOI] [PubMed] [Google Scholar]
- 15.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 16.Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65:79–83. doi: 10.1902/jop.1994.65.1.79. [DOI] [PubMed] [Google Scholar]
- 17.Lee W, Karapetyan G, Moats R, et al. Corticotomy-/osteotomy-assisted tooth movement microCTs differ. J Dent Res. 2008;87:861–867. doi: 10.1177/154405910808700904. [DOI] [PubMed] [Google Scholar]
- 18.Nightingale C, Jones SP. A clinical investigation of force delivery systems for orthodontic space closure. J Orthod. 2003;30:229–236. doi: 10.1093/ortho/30.3.229. [DOI] [PubMed] [Google Scholar]
- 19.Daskalogiannakis J, McLachlan KR. Canine retraction with rare earth magnets: an investigation into the validity of the constant force hypothesis. Am J Orthod Dentofacial Orthop. 1996;109:489–495. doi: 10.1016/s0889-5406(96)70133-6. [DOI] [PubMed] [Google Scholar]
- 20.Aboul-Ela SM, El-Beialy AR, El-Sayed KM, Selim EM, El-Mangoury NH, Mostafa YA. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:252–259. doi: 10.1016/j.ajodo.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 21.Leethanakul C, Kanokkulchai S, Pongpanich S, Leepong N, Charoemratrote C. Interseptal bone reduction on the rate of maxillary canine retraction. Angle Orthod. 2014;84:839–845. doi: 10.2319/100613-737.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011;29:191–196. doi: 10.1089/pho.2009.2652. [DOI] [PubMed] [Google Scholar]
- 23.Gianelly AA. Arch width after extraction and nonextraction treatment. Am J Orthod Dentofacial Orthop. 2003;123:25–28. doi: 10.1067/mod.2003.57. [DOI] [PubMed] [Google Scholar]
- 24.Sukurica Y, Karaman A, Gurel HG, Dolanmaz D. Rapid canine distalization through segmental alveolar distraction osteogenesis. Angle Orthod. 2007;77:226–236. doi: 10.2319/0003-3219(2007)077[0226:RCDTSA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Luppanapornlarp S, Johnston LE., Jr The effects of premolar-extraction: a long-term comparison of outcomes in “clear-cut” extraction and nonextraction Class II patients. Angle Orthod. 1993;63:257–272. doi: 10.1043/0003-3219(1993)063<0257:TEOPAL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Paquette DE, Beattie JR, Johnston LE., Jr A long-term comparison of nonextraction and premolar extraction edgewise therapy in “borderline” Class II patients. Am J Orthod Dentofacial Orthop. 1992;102:1–14. doi: 10.1016/0889-5406(92)70009-Y. [DOI] [PubMed] [Google Scholar]
- 27.Johnson DK, Smith RJ. Smile esthetics after orthodontic treatment with and without extraction of four first premolars. Am J Orthod Dentofacial Orthop. 1995;108:162–167. doi: 10.1016/s0889-5406(95)70079-x. [DOI] [PubMed] [Google Scholar]
- 28.Forsberg CM, Brattstrom V, Malmberg E, Nord CE. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and lactobacilli. Eur J Orthod. 1991;13:416–420. doi: 10.1093/ejo/13.5.416. [DOI] [PubMed] [Google Scholar]
- 29.Turkkahraman H, Sayin MO, Bozkurt FY, Yetkin Z, Kaya S, Onal S. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod. 2005;75:231–236. doi: 10.1043/0003-3219(2005)075<0227:ALTMCA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 31.Anholm JM, Crites DA, Hoff R, Rathbun WE. Corticotomy-facilitated orthodontics. CDA J. 1986;14:7–11. [PubMed] [Google Scholar]
- 32.Dorfman HS, Turvey TA. Alterations in osseous crestal height following interdental osteotomies. Oral Surg Oral Med Oral Pathol. 1979;48:120–125. doi: 10.1016/0030-4220(79)90048-3. [DOI] [PubMed] [Google Scholar]
- 33.Ozturk M, Doruk C, Ozec I, Polat S, Babacan H, Bicakci AA. Pulpal blood flow: effects of corticotomy and midline osteotomy in surgically assisted rapid palatal expansion. J Craniomaxillofac Surg. 2003;31:97–100. doi: 10.1016/s1010-5182(02)00188-9. [DOI] [PubMed] [Google Scholar]