Abstract
Background
Bilateral sinus disease is relatively uncommon in horses, accounting for 3%–4.5% of horses with sinonasal disease, but may require bilateral paranasal surgery for complete resolution. Complications and recurrence following bilateral sinusotomy have not been reported or compared to those following unilateral procedures.
Objective
To describe clinical features and outcomes in horses undergoing standing single, caudally based bilateral frontonasal sinusotomy compared to unilateral frontonasal surgery.
Methods
Records of horses (n = 37) undergoing surgical treatment for sinus disease (five bilateral, 32 unilateral) were retrospectively reviewed (2010–2017) for signalment, presenting complaint, duration of signs preoperatively, diagnostic imaging, treatments administered, duration hospitalization, complications, and owner satisfaction with the procedure. Mann–Whitney testing was used to compare age, duration of hospitalization, and follow‐up time in horses undergoing unilateral or bilateral procedures. Fisher's exact testing was used to determine if sex predilection was present for unilateral or bilateral disease. Survival time and time to recurrence were compared by Kaplan–Meier survival curves and log‐rank curve comparison testing. Significance was assessed at p < 0.05.
Results
Length of signs prior to admission did not differ between horses with unilateral and bilateral disease (p = 0.09), but there was a tendency for horses with bilateral disease to have clinical signs for longer. Age (p = 0.19) and hospitalization duration (p = 0.53) did not differ between horses undergoing unilateral versus bilateral procedures. Recurrence or failure to resolve signs was reported in 11/32 (34%) of unilateral and 0/5 bilateral cases (p = 0.07).
Conclusions
The bilateral single, caudally based sinusotomy approach may be considered to effectively treat bilateral paranasal sinus disease without concern for increased risk of life‐threatening complications or longer hospitalization duration than would be typical for unilateral sinusotomy procedures.
Keywords: bilateral, equine, sinus, sinusotomy
Bilateral paranasal sinus disease was safely and effectively treated in standing, sedated horses through a single, caudally based bilateral front‐nasal bone flap approach, resulting in return to intended use in all cases. The bilateral approach may be considered to treat bilateral paranasal sinus disease without concern for increased risk of life‐threatening complications or longer hospitalization than would be typical for unilateral sinus bone flap procedures.

1. INTRODUCTION
Diseases of the paranasal sinuses of the horse that may require surgery include primary sinusitis, neoplasia, equine ethmoid hematomas, sinus cysts, fistulas, trauma, mycotic infections, polyps, or dental disease (Dixon et al., 2012b; Tremaine & Dixon, 2001b). Bilateral disease is relatively uncommon, accounting for 3%–4.5% of horses with sinonasal disease, and may require bilateral paranasal sinus surgery for complete resolution (Beard et al., 1990; Coumbre et al., 1987; Dixon et al., 2011; Dixon et al., 2012a; Easley & DE, 2013; Silva et al., 2009; Tremaine & Dixon, 2001a, 2001b; Woodford & Lane, 2006). Surgical approaches to the paranasal sinuses have been previously described in standing, sedated horses, with the advantages of reduced cost and lower risk of haemorrhage and complications associated with general anaesthesia (Barakzai & Dixon, 2014; Freeman et al., 1990; Quinn et al., 2005; Schumacher et al., 2000). For unilateral disease, a large frontonasal sinusostomy through the conchofrontal sinus provides improved exposure of multiple sinus compartments when compared to maxillary approaches, and the nasal passages may further be accessed through perforation of the medial wall (Freeman et al., 1990; Quinn et al., 2005; Schumacher et al., 2000). As an alternative to performing two individual flaps in cases of bilateral disease, a single, bilateral caudally based approach has been described in the treatment of bilateral mucocele in a Miniature Horse and bilateral sinus cysts in a Thoroughbred gelding (Easley & DE, 2013; Robert et al., 2019). Several studies have reported on recurrence rates and postoperative complications associated with sinusotomy in horses with unilateral paranasal sinus disease, describing long‐term response to treatment for paranasal sinus disease between 12% and 92%, depending on the reason for performing surgery (Dixon et al., 2012b; Head & Dixon, 1999; Tremaine & Dixon, 2001b). However, the single, caudally based bilateral bone flap has not been evaluated relative to the unilateral frontonasal approach with respect to patient outcomes and complication rates postoperatively. As this approach represents a more recently reported modified procedure that might be rarely performed, information comparing the single, caudally based bilateral procedure to the more commonly done unilateral sinusotomy would be useful to practitioners to dispel concerns regarding instability of the bilateral sinusotomy or other postoperative complications or outcomes.
The objective of this study was to describe clinical features, complications and outcomes in horses undergoing a single, caudally based bilateral sinusotomy, and to compare those findings with horses undergoing unilateral frontonasal sinusotomy at a single academic referral centre over the same time period. We hypothesized that in the population of horses examined, horses undergoing the single, caudally based bilateral frontonasal sinusotomy would not differ in terms of postoperative complications and would have equivalent or improved rates of recurrence of clinical signs compared to those undergoing unilateral sinusotomy.
2. MATERIALS AND METHODS
2.1. Retrospective medical record review
A computerized search of medical records was performed to identify horses undergoing sinusotomy to treat paranasal sinus disease at the Colorado State University between 1 January 2010 and 31 December 2017. Medical records were reviewed retrospectively and data collected included signalment, paranasal sinus approach (frontonasal or maxillary, unilateral or bilateral), preoperative advanced diagnostic imaging (i.e. computed tomography (CT) scan of the skull), perioperative treatments administered (e.g. blood transfusions), length of clinical signs prior to surgery, diagnosis, days hospitalized, complications, and rate of recurrence or lack of resolution of clinical signs.
2.2. Perioperative patient management
Routine perioperative treatment included IV administration of balanced isotonic fluids at 50–100 ml/kg/day (approximately 1–2 L/h) intraoperatively or longer postoperatively depending on clinician preference and based on interpretation of laboratory findings, intraoperative blood loss, and clinical assessment. Approximately 30 min prior to surgery and for at least 3–7 days following surgery, horses received perioperative antibiotics, which included some combination of trimethoprim sulfamethoxazole (30 mg/kg PO q12h), doxycycline (10 mg/kg PO q12h), cephazolin (11 mg/kg IV q8h), and gentamicin (6.6 mg/kg IV q24h), based on the preference of the attending clinician. All horses received anti‐inflammatories (either phenylbutazone (2.2 mg/kg PO q12h) or flunixin meglumine (1.1 mg/kg PO q12h)) at 30 min preoperatively and for at least 3 days postoperatively.
All procedures, unilateral and bilateral, were performed with horses standing and sedated. Horses were restrained in the stocks by an experienced handler and sedated with an initial bolus of detomidine (0.01 mg/kg IV) and butorphanol tartrate (0.01 mg/kg IV) followed by detomidine (20 mg in 1 L NaCl, titrated to effect). Prior to creating the sinusotomy incision, the skin along the edges of the proposed surgical incision site was desensitized with approximately 30 ml local anaesthetic solution (2% mepivacaine). The skin, subcutaneous tissues, and periosteum overlying the bone was incised in such a way as to overlap the bone incision by 5 mm. For both unilateral and bilateral procedures, an oscillating bone saw was used to cut the periosteum and underlying exposed bone in order to create the flap sinusotomy.
Postoperatively, blood transfusion was performed based on clinician discretion following clinical and clinicopathologic assessment during surgery (perceived volume of blood loss, heart rate, haematocrit, and lactate). Additional postoperative pain management (butorphanol tartrate 0.01–0.1 mg/kg IM) was administered based on perceived postoperative discomfort. Sinus packing was removed 1–2 days postoperatively through the nostril. Additional postoperative sinus lavage was not performed in any case.
2.3. Surgical techniques
All procedures were performed with horses standing and sedated. The surgical procedures used for unilateral frontonasal sinusotomy and the single, caudally based bilateral sinus flap were performed similarly to that previously described by Schumacher et al. (2000), Freeman et al. (1990), and Easley and Freeman (2013).
For the unilateral frontonasal sinusotomy, the caudal margin of the incision was identified as a line at right angles to the dorsal midline, midway between the supraorbital foramen and medial canthus of the eye (Dixon et al., 2011). The lateral margin was initiated 2–2.5 cm medial to the medial canthus of the eye and extended approximately two‐thirds the distance from the medial canthus of the eye to the infraorbital foramen, with the goal of extending the flap as wide as possible while not interfering with the nasolacrimal duct. The rostral margin of the flap was at right angles to dorsal midline. The opening to the sinuses created in this fashion allowed access to the unilateral conchofrontal sinus, ethmoid labyrinth, and frontomaxillary opening.
In creating the single bilateral flap sinusotomy, the rostral and lateral margins are similar to the unilateral frontonasal flap described by Freeman et al. (1990), with the difference that the bilateral approach spanned both frontal bones. The skin along the edges of the proposed incision site was desensitized with approximately 30 ml 2% mepivacaine. Compatible blood donors were identified preoperatively by cross matching in all cases. Before performing the flap, two stab incisions were made at a distance of 2 cm to the right and left of midline at the caudal border of the proposed flap. A 2.0 mm Steinman pin on a hand‐held chuck was used to create a hole through the frontal bone in each stab for infusion of 50 ml of 2% mepivacaine into the frontal sinuses to desensitize a portion of the sinus mucosa prior to entering the sinuses. The lateral margins were identified at approximately 2 cm medial to the medial canthus of each eye and extended rostrally two‐thirds the distance from the medial canthus of the eye to the infraorbital foramen (Figure 1). The skin and subcutaneous tissues were incised using a #20 scalpel blade to be approximately 5 mm larger than the periosteal and bone incision. The periosteum was elevated 5 mm from the site of the proposed osteotomy incision using the handle of a scalpel blade. An oscillating bone saw was used to cut the underlying exposed bone perpendicular to its surface to create the bone flap. The bone along the caudal edge of the sinusotomy was fractured as the flap was lifted with the assistance of osteotomes to break down the dorsal nasal septum, creating a ‘hinge’ to allow access to the sinuses. Two 10 mm wide osteotomes were placed under the flap on both sides of midline to elevate it further. The attachment of the frontal bone to the midline septum of the frontal sinuses was torn upon raising the flap and broken down manually while elevating the flap in some cases. This bilateral approach allowed access to the left and right conchofrontal sinuses, sphenopalatine sinuses, ethmoid labyrinth, and frontomaxillary aperture, with perforation of the maxillary septal bulla. Ventral dissection through the floor of the dorsal conchal sinus and through the maxillary sinus septal bulla allowed access to the nasal passages and the rostral maxillary and ventral conchal sinuses, respectively (Freeman et al., 1990).
FIGURE 1.
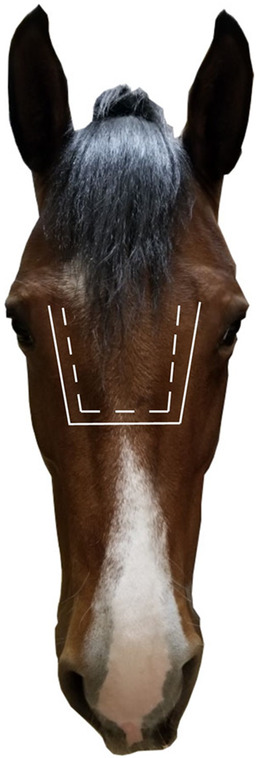
Incisional location to perform single caudally based bilateral bone flap to access right and left paranasal sinuses simultaneously. The skin and subcutaneous incisions are designated as solid lines. The periosteal and bone incisions are indicated by broken lines
Following surgical exploration of the sinuses through the proposed flap sinusotomy approach, the sinuses were lavaged thoroughly and packed bilaterally in four of five bilateral cases with antimicrobial impregnated kerlix AMD gauze (Covidien), and the ends of the gauze were sutured to the nares to reduce haemorrhage following the procedure. In the fifth case, tracheotomy was not performed, and the sinus was packed unilaterally postoperatively. The sinusotomy flap was repositioned with the bone edges aligned evenly with the margins of the parent bone. The periosteum was closed in simple continuous fashion using 2‐0 Glycomer 631. The subcutaneous tissues were closed at the corners and at selected points along the margins of the incision in a simple interrupted pattern using 2‐0 Glycomer 631, and then the remainder of the subcutaneous tissues were closed between interrupted sutures in a simple continuous pattern. The skin was closed with simple interrupted sutures using 2‐0 polydioxanone. The incision site was bandaged with kerlix AMD gauze and 4″ elastikon (Johnson and Johnson).
2.4. Long‐term follow‐up
Owners were contacted by telephone for follow‐up information. Information collected included general health of the horse, postoperative complications, recurrence or lack of resolution of clinical signs, and subsequent treatment following hospital dismissal if applicable.
2.5. Data analysis
Continuous data were reported as median and interquartile ranges (IQR). Mann–Whitney testing was used to compare the age, duration of hospitalization, and follow‐up time in horses undergoing unilateral or bilateral procedures. Fisher's exact testing was utilized to determine if a sex predilection was present for unilateral or bilateral disease. Survival time and time to recurrence were compared by constructing Kaplan–Meier survival curves and performing log‐rank curve comparison testing. GraphPad Prism v 8.4.1 (GraphPad Software Inc.) was used for data analysis.
3. RESULTS
During the defined time period, 51 standing surgeries were performed to address paranasal sinus disease. Of these, 37 horses were identified as undergoing frontonasal sinusotomy, including 32 horses with unilateral procedures and five horses with bilateral procedures. Bilateral frontonasal flap sinusotomy procedures were performed by four board‐certified surgeons, with two surgeons involved in each of four of the five cases (Table 1). Unilateral sinusotomy procedures were performed by six board‐certified surgeons. Of the horses undergoing unilateral frontonasal sinusotomy, 22 were geldings, nine were mares and one was a stallion. Of the horses undergoing bilateral caudally based frontonasal sinusotomies, four were geldings and one was a stallion. Sex of horses presenting for treatment of unilateral or bilateral disease did not differ between groups (p = 0.56). Median age of horses with unilateral disease was 17 years (IQR: 11–20 years). Median age of horses with bilateral disease was 11 years (IQR: 6–17 years). Age did not differ between horses with unilateral and bilateral disease (p = 0.19) (Figure 2).
TABLE 1.
Summary of bilaterally affected cases
| Case | Age (years) | Breed | Gender | Imaging | Pathology | Sinus compartments | Location origin disease | Duration signs (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 3 | MH | MC | Radiographs; CT | Malformation bilateral frontal, maxillary, sphenoid sinuses | Bilateral frontal, maxillary, sphneoid | Congenital malformation disrupting anatomy | 12 |
| 2 | 16 | QH | MC | Endoscopy | Bilateral ethmoid hematomas | Bilateral frontal, dorsal concal, sphenopalatine, right caudal maxillary | Bilateral lesions | 108 |
| 3 | 18 | WB | MC | Radiographs, endoscopy | Bilateral ethmoid hematomas | Bilateral frontal, dorsal conchal, rostal and caudal maxillary | Bilateral lesions | 4 |
| 4 | 11 | WB | MI | Radiographs, endoscopy | Bilateral paranasal cysts | Left caudal and rostral maxillary, left ventral conchal, left ethmoid | Left unilateral extending through septum | 2 |
| 5 | 9 | QH | MC | Radiographs, CT | Obstructive sinusitis, pressure resorption surrounding bone | Bilateral frontal, right dorsal conchal, right caudal maxillary | Head trauma disrupting anatomy | 24 |
Abbreviations: CT, computed tomography scan; MH, Miniature horse; QH, Quarter horse; WB, warmblood.
FIGURE 2.
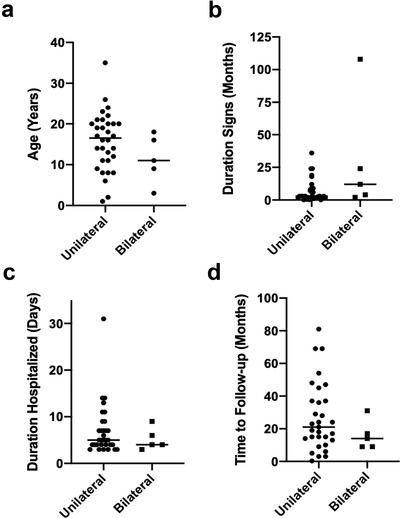
Comparison of age, duration of clinical signs, duration of hospitalization postoperatively, and time interval to follow‐up between horses treated with unilateral and single caudally based bilateral frontonasal sinusotomy. (a) Age did not differ between horses with unilateral and bilateral disease (p = 0.19). Median age of horses with unilateral disease was 17 years (interquartile ranges (IQR): 11–20 years). Median age of horses with bilateral disease was 11 years (IQR: 6–17 years). (b) Duration of clinical signs prior to admission did not differ between horses with unilateral and bilateral disease (p = 0.09), but there was a tendency for horses with bilateral disease to have clinical signs for a longer time period. Median length of clinical signs prior to hospitalization and sinusotomy was 3 months (IQR: 2–9 months) for horses with unilateral disease and 12 months (IQR: 3–66 months) for horses with bilateral disease. (c) Duration of hospitalization did not differ between horses undergoing unilateral or bilateral procedures (p = 0.53). Median duration of hospitalization of horses undergoing unilateral procedures was 5 days (IQR: 4–9 days). Median duration of hospitalization of horses undergoing bilateral procedures was 4 days (IQR: 3–8 days). (d) Follow‐up interval was not different between horses undergoing unilateral and bilateral procedures (p = 0.28). Median follow‐up time for horses undergoing unilateral procedures was 21 months (IQR: 13–37 months). Median follow‐up time for horses undergoing bilateral procedures was 14 months (IQR: 9–24 months)
Breeds of horses with unilateral disease were variable and included American Quarter Horse (n = 5), Draft horse (n = 4), Thoroughbred (n = 5), Warmblood (n = 5), Paint (n = 3), and other breeds (one Appaloosa, one American Saddlebred, one Andalusian, one donkey, two mixed breeds, one Missouri Foxtrotter, one pony, and two Arabians). Breeds of horses with bilateral disease included American Quarter Horse (n = 2), Warmblood (n = 2), and American Miniature Horse (n = 1). Median length of clinical signs prior to hospitalization and sinusotomy was 3 months (IQR: 2–9 months) for horses with unilateral disease and 12 months (IQR: 3–66 months) for horses with bilateral disease. Length of signs prior to admission did not differ between horses with unilateral and bilateral disease (p = 0.09), but there was a tendency for horses with bilateral disease to have clinical signs for a longer time period (Figure 2). Clinical signs in horses presenting for unilateral disease included nasal discharge (n = 28), reduced airflow through the nasal passages including laboured breathing (n = 7), facial swelling (n = 4), lethargy (n = 3), draining tract (n = 2), mass protruding from the nasal passages (n = 2), ocular discharge (n = 1), exophthalmos (n = 1), decreased appetite (n = 1), and elevated body temperature (n = 1). Clinical signs in horses presenting for bilateral disease included nasal discharge (n = 4), reduced nasal passage airflow with laboured breathing (n = 3), ocular discharge (n = 1), exophthalmos (n = 1), facial swelling (n = 1), and decreased appetite (n = 1). Of horses presenting for unilateral disease, several had previously undergone procedures prior to presentation, including trephination and sinus lavage (n = 7), tooth extraction (n = 5), intralesional formalin injections (n = 3), and nasal tumour debulking through the nasal passages (n = 1). Of horses presenting for bilateral disease, one horse had previously received intralesional formalin injections.
Advanced preoperative diagnostic imaging (CT scan of the skull) was performed in 13/32 (41%) of horses undergoing unilateral frontonasal sinus flap surgery and in 2/5 (40%) of horses undergoing bilateral surgery. Computed tomography scan was offered in all cases undergoing bilateral sinusotomy and performed in Cases 1 and 3. Of the bilaterally operated cases, skull radiographs were also performed in four cases (Cases 1,3–5; radiographs from Case 5, presented in Figure 3), and endoscopy of the upper respiratory tract was performed in three cases (Cases 2, 4, 5). Diagnoses (i.e. reasons for performing surgery) of horses undergoing unilateral frontonasal sinus flap surgery included primary sinusitis (n = 4), sinusitis secondary to periodontal disease (n = 12), sinusitis secondary to paranasal sinus mass (five ethmoid hematoma, three cysts, one osteoma, one fibroblastic osteosarcoma, one congenital osseous bulla, one amyloid tumour, and three masses were undefined by histopathology), and fracture of frontal and lacrimal bones (n = 1). Diagnoses of horses undergoing bilateral surgery included bilateral ethmoid hematoma (n = 2), bilateral paranasal sinus cysts (n = 1), bilateral congenital malformation of the frontal, maxillary and sphenoid sinuses (n = 1), and obstructive sinusitis with pressure resorption of surrounding bones and non‐union fractures of maxillary and frontal bones secondary to previous trauma (n = 1). Of the horses undergoing bilateral surgery, two horses had distinct separate lesions growing independently within both the right and left paranasal sinuses (Cases 2 and 3), one had a space occupying lesion that expanded through the frontal sinus midline septum to result in bilateral disease (Case 4), and two horses had complete disruption of the normal sinus anatomy as a result of congenital malformation or head trauma (Cases 1 and 5). Sinus compartments involved in bilaterally affected cases are summarized in Table 1.
FIGURE 3.
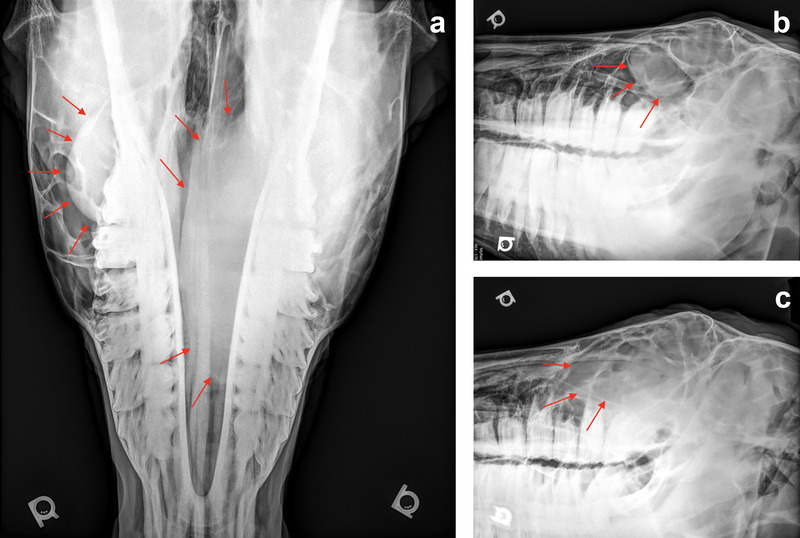
Case 5, preoperative radiographic projections. An 11‐year‐old Hanoverian gelding presented for evaluation of left‐sided nasal discharge and increased inspiratory stertor while exercising of 2 months duration. Radiographs (dorsoventral, left lateral) revealed a large left maxillary soft tissue mass and well‐defined right conchofrontal sinus mass
Preoperative antibiotics administered in unilaterally operated cases were trimethoprim sulfamethoxazole (30 mg/kg PO) in 23 cases, cephazolin (11 mg/kg IV) and gentamicin (6.6 mg/kg IV) in five cases, doxycycline (10 mg/kg PO q12h) in one case, potassium penicillin (22,000 MU/kg IV) and gentamicin (6.6 mg/kg IV) in two cases, ceftiofur crystalline (0.66 mg/kg IM) in one case, and no antibiotics in one case. Preoperative antibiotics administered in bilaterally operated cases were either trimethoprim sulfamethoxazole (30 mg/kg PO) in two cases or a combination of cephazolin (11 mg/kg IV) and gentamicin (6.6 mg/kg IV) in three cases. Postoperatively, horses were treated with up to 14 days of oral antibiotics, including trimethoprim sulfamethoxazole, doxycycline (10 mg/kg PO q12h), and/or metronidazole (30 mg/kg PO q12h). Median duration of hospitalization of horses undergoing unilateral procedures was 5 days (IQR: 4–9 days). Median duration of hospitalization of horses undergoing bilateral procedures was 4 days (IQR: 3–8 days). Duration of hospitalization did not differ between horses undergoing unilateral or bilateral procedures (p = 0.53) (Figure 2).
Complications postoperatively were reported in 15/32 (47%) unilateral cases, including suture periostitis (n = 1), haemorrhage (n = 2), corneal ulcer/chemosis (n = 2), colic/colitis/reduced faecal output (n = 4), incisional infection (n = 2), oro‐antral fistula (n = 2), trigeminal neuritis (n = 1), and acute death attributed to pneumocephalus (n = 1). One horse undergoing unilateral sinus flap surgery was euthanized in the immediate postoperative period due to (suspected) antibiotic‐induced colitis that did not improve with medical management. Intra‐ and postoperative complications were reported in 4/5 (80%) cases undergoing bilateral surgery. In 3/4 (75%) cases, complications were considered mild, including incisional infection (n = 2) and inappetence with elevated triglycerides (n = 2), fever (n = 1) and reduced manure production postoperatively (n = 1). One case (Case 1) experienced what was perceived to be considerable haemorrhage and had an elevated heart rate intraoperatively (HR = 56 bpm), which was treated with a blood transfusion during surgery. In this case, the packed cell volume dropped to 20% with lactate 1.7 mmol/L postoperatively. The patient additionally spiked a fever at 2 days postoperatively, which was attributed to catheter site inflammation as no other causes were identified based on physical examination, bloodwork (complete blood count, diagnostic panel), and abdominal or thoracic ultrasound, and which resolved following removal of the intravenous catheter. Additional postoperative pain management (butorphanol tartrate 0.01–0.1 mg/kg IM) was administered in one case based on perceived postoperative discomfort. Incisional infections that developed in two cases postoperatively were successfully treated with local aseptic preparation and oral antibiotics (trimethoprim sulfamethoxazole 30 mg/kg PO q12h, 14 days).
Long‐term follow‐up was achieved by telephone interview in 5/5 (100%) of bilateral cases and 24/32 (75%) of unilateral cases. Follow‐up interval was not different between horses undergoing unilateral and bilateral procedures (p = 0.28) (Figure 2). Median follow‐up time for horses undergoing unilateral procedures was 21 months (IQR: 13–37 months). Median follow‐up time for horses undergoing bilateral procedures was 14 months (IQR: 9–24 months). Overall recurrence rate or failure to resolve clinical signs of sinusitis following surgery was reported by owners in 11/32 (34.4%) cases where unilateral procedure was performed, with recurrence resulting in a second surgical procedure in 6/32 (18.6%) cases. There were no reported recurrences in any of the five cases undergoing bilateral flap sinusotomy at the time of this report (0%). Recurrence rate when compared between groups of horses undergoing unilateral versus bilateral sinusotomy was not significantly different (p = 0.07), but there was a tendency for horses with unilateral sinusotomy to have higher recurrence rates (Figure 2).
For survival at long‐term follow‐up, 5/5 (100%) of horses undergoing bilateral sinusotomy were alive at the time of follow‐up, while only 13/24 horses undergoing unilateral sinusotomy for which follow‐up was available were alive at the time of follow‐up. Of the horses which underwent unilateral sinusotomy and were dead at the time of long‐term follow‐up, owners cited recurrence of clinical signs or failure to resolve signs as the reason for electing euthanasia in 8/11 cases. Overall, survival time between groups was not significantly different at the time of long‐term follow‐up (p = 0.14) (Figure 2). Owners reported that they were satisfied with the sinusotomy procedure in 5/5 (100%) cases in which the bilateral sinusotomy was performed and 17/24 (71%) of unilateral cases for which long‐term follow‐up was available.
4. DISCUSSION
This is the first study to compare outcomes of horses undergoing flap sinusotomy with either a single, caudally based bilateral or a unilateral frontonasal procedure. The results of this retrospective study demonstrate that bilateral paranasal sinus disease can be effectively treated through the single, caudally based approach described here without increased risk for life‐threatening postoperative complications or duration of hospitalization. The improved visualization of the sinus compartments provided by the bilateral approach could make this procedure advantageous to rule out more extensive disease in cases where available imaging is inconclusive for bilateral involvement. All cases undergoing the bilateral procedure described here experienced full resolution of clinical signs without recurrence at the time of this clinical report despite involving more wide‐spread disease processes. Case selection and surgical technique likely also impact prognosis and probability of recurrence following sinusotomy.
Local anaesthetic applied along the intended surgical incision site and as lavage within the sinuses prior to flap creation was sufficient to desensitize the surgical region and minimize reaction during creation of the bilateral flap when cutting the dorsal septum between sinuses. Although additional analgesia for frontonasal sinus flaps has been described using maxillary or infraorbital nerve blocks, performed caudal to the pterygopalatine fossa or rostral at the infraorbital foramen, respectively, (Bardell et al., 2020; O'Neill et al., 2014; Staszyk et al., 2008; Stauffer et al., 2017) nerve blocks are not routinely performed in the authors’ practice as local anaesthesia is generally considered good with sinus lavage and local infusion, and complications induced by nerve blocks in that region include intra‐arterial injection and nerve damage. (O'Neill et al., 2014; Stauffer et al., 2017) Although peri‐incisional local anaesthetic injection has been suggested to result in delayed wound healing, which would potentially be an argument for achieving analgesia through nerve blocking, the published effects of local anaesthetics on incisional healing are mixed, with some studies actually demonstrating no detrimental effect on tissue healing and others indicating that there exists a differential effect depending on the type of local anaesthetic used (Abrao et al., 2014; Baxter et al., 2013; Bicer et al., 2018; Hanci et al., 2012; Kesici et al., 2018; Panneerselvam et al., 2016; Waite et al., 2010; Zeren et al., 2013). In summary, sinus lavage and local infusion were considered sufficient to perform the bilateral procedure in the cases presented.
Volume of haemorrhage that may occur when implementing the single, bilateral caudally based approach was a concern preoperatively, particularly when breaking down the underlying midline attachments between the dorsal aspect of the nasal septum and the septum between sinuses. However, haemorrhage was in most cases judged by clinicians as mild, and not more severe than can be expected through a unilateral approach in the standing position, consistent with the previous report of this technique for the treatment of mucocele in a Miniature Horse (Easley & Freeman, 2013). Intra‐operative transfusion was considered necessary in one of the five cases, based on elevated pulse rate, perceived volume of blood loss during surgery, and decreasing haematocrit. This lack of additional haemorrhage may be explained in part by the disruption of normal underlying anatomy in cases with bilateral disease, as described previously (Easley & Freeman, 2013). In addition, the standing approach described here further reduces the risk of haemorrhage and is advocated by the authors in all cases if otherwise suitable for the individual patient as previously described (Schumacher et al., 2000).
Increased risk of incisional infection and dehiscence postoperatively due to interruption of the blood supply to the rostral end of the bilateral caudally based sinusotomy was also a concern with use of the bilateral approach. Postoperative incisional infection occurred in two of five cases, both of which were mild, responded as expected to oral antibiotics administered for 2 weeks and local aseptic preparation with betadine and saline lavage, and resolved completely. All horses in this case series received empirical broad‐spectrum prophylactic antibiotic pre‐ and postoperatively. In cases of incisional infection, bacterial culture and sensitivity were not performed as infection resolved quickly. Excessive surgical trauma or lack of perioperative antibiotic usage could also predispose to post‐operative incisional infection in sinusotomy (Easley & Freeman, 2013).
The recurrence of clinical signs suggestive of sinusitis (e.g. nasal discharge) following sinusotomy procedures has been reported previously to occur in 13%–28% of unilaterally operated cases and is usually attributable to an on‐going underlying problem, such as failure to remove inspissated pus from a compartment, residual presence of an intra‐sinus mass, or an undetected infected cheek tooth (Quinn et al., 2005; Tremaine & Dixon, 2001a, 2001b; Woodford & Lane, 2006). This is consistent with the findings of this study in patients undergoing the unilateral frontonasal sinus flap procedure, where overall failure to resolve clinical signs or recurrence was reported in 11/32 (34.4%) of cases, with recurrence necessitating surgery in 18.7% of cases. At the time of follow‐up, no cases of recurrence were reported in the group of horses undergoing bilateral bone flap. The relatively higher rate of recurrence in unilateral cases may be attributed to the greater heterogeneity in unilateral cases, with higher occurrence of unilateral dental disease (12/32 cases or 37.5%) and neoplastic processes (15/32 cases or 46.9%), both of which are less likely to be associated with complete resolution (Dixon et al., 2012b). It is acknowledged that true recurrence versus lack of resolution was difficult or impossible to distinguish in some of these cases as repeat CT scan was not possible postoperatively in most cases due to financial constraints. In summary, postoperative complications associated with the single caudally based flap approach were most frequently mild and not more severe than would generally be expected with a unilateral frontonasal approach based on previous reports and evaluation of our clinical population, indicating the bilateral approach may be considered safe to perform in cases with bilateral disease processes or where bilateral involvement cannot be definitively ruled out with available imaging (Barakzai, 2008; Quinn al., 2005; Tremaine, 2006).
Alternative approaches to the single, caudally based bone flap described here to treat bilateral paranasal sinus disease include bilateral trephination or two separate unilateral flaps performed in one or two procedures. Performing the single, caudally based approach versus two unilateral staged procedures could reduce cost and stress to the patient without increasing risk for postoperative complications based on this report. The complications encountered in cases operated bilaterally in this study (haemorrhage necessitating transfusion in one case, incisional infection in two cases) were successfully resolved in all cases, and in the authors’ opinion, would not warrant further hesitation regarding the safety of the surgical technique described. Trephination and lavage may be successfully implemented in some cases of bilateral disease but given the chronicity and disruption of normal sinus anatomy in the cases described here, the open approach was considered necessary to resolve clinical signs. Given the lack of recurrence, the single, caudally based bilateral sinusotomy procedure seemed to allow adequate exposure to resolve sinusitis in all cases without recurrence to date, although it is acknowledged that alternate treatments including trephination and sinoscopic guided therapies may have been employed with equal success. Further evaluation of a greater number of cases from multiple institutions is needed to compare these techniques in terms of relative outcome and complications.
Multiplanar diagnostic imaging (CT, magnetic resonance imaging) provides detailed information in assessing sinus disease in horses for a more accurate preoperative diagnosis to guide surgical planning (Easley & Freeman, 2013; Ostrowska et al., 2019; Textor et al., 2012). Patients that experience recurrence or lack of resolution of clinical signs following sinusotomy are good candidates for CT examination if the cause of recurrence is not apparent (Barakzai & Dixon, 2014). Computed tomography scans were performed preoperatively in a similar percentage of cases (13/32 or 41% unilateral cases, 2/5 or 40% bilateral cases) with recurrence of clinical signs reported in 11/32 (34%) of unilateral cases. Of the eleven horses operated unilaterally that presented with recurrence or lack of resolution of clinical signs, 3/11 (27.3%) had undergone CT scans preoperatively. The higher recurrence in unilateral cases may be explained in part by the higher frequency of dental disease and neoplasia as the primary cause of sinusitis in this group of horses. Advanced diagnostic imaging (CT scan) is supported by the authors preoperatively in all cases when financially possible, and particularly in those where the cause of disease was not well‐established with other imaging techniques or in which clinical signs have already recurred.
Limitations of the study include the retrospective nature of study design, relatively small number of horses evaluated that underwent bilateral sinusotomy and lack of a control group of horses that underwent two unilateral frontonasal sinusotomies. The retrospective study design restricts data collection in some instances due to the incompleteness of the medical records provided. The invoice, hospitalization report, and imaging reports were accessed to provide the most accurate representation of the data. Furthermore, this study evaluated cases of sinusitis at a single tertiary referral hospital, representing a population of horses that were selected for referral, in some cases following unsuccessful prolonged treatment by referring veterinarians. However, as active surveillance (i.e. contacting owners) was performed, it was likely that the rate of complications was accurately described. As bilateral sinus disease is relatively uncommon, comparison of outcome parameters between different surgical centres over a longer time period may allow determination of whether the bilateral sinusotomy procedure is relatively more useful to resolve specific types of bilateral sinus disease.
In conclusion, the single caudally based bilateral frontonasal sinusotomy should be considered for surgical treatment of bilateral paranasal sinus disease as postoperative complication rates and duration of hospitalization were comparable to that described for unilateral surgery. Preoperative CT scan is recommended to definitively confirm bilateral involvement. Case selection and surgical technique likely impact prognosis and probability of recurrence following bilateral bone flap.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Jeremiah T. Easley and Eileen S. Hackett contributed to study conception and design. Jeremiah T. Easley, Eileen S. Hackett, and Lynn M. Pezzanite contributed to management of cases described. Lynn M. Pezzanite and Erin McCready contributed to data acquisition and draft of the manuscript. All authors contributed to and approved the final manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/vms3.607
ACKNOWLEDMENTS
The authors would like to acknowledge the CCTSI NIH/NCATS CTSA TL1TR002533, NIH 5T32OD010437‐19, and Carolyn Quan and Porter Bennett for providing stipend support for Lynn M. Pezzanite towards data collection for this study.
Pezzanite, L. M. , Hackett, E. S. , McCready, E. , & Easley, J. T. (2021). Outcomes following single, caudally based bilateral versus unilateral frontonasal sinusotomy for treatment of equine paranasal sinus disease. Veterinary Medicine and Science, 7, 2209–2218. 10.1002/vms3.607
REFERENCES
- Abrao, J. , Fernandes, C. R. , White, P. F. , Shimano, A. C. , Okubo, R. , Lima, G. B. , Bachur, J. A. , & Garcia, S. B. (2014). Effect of local anaesthetic infiltration with bupivacaine and ropivacaine on wound healing: A placebo‐controlled study. International Wound Journal, 11, 379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barakzai, S. (2008). Standing sinus surgery in the horse: Indications, techniques, and complications. In Practice, 30, 252–262. [Google Scholar]
- Barakzai, S. Z. , & Dixon, P. M. (2014). Standing equine sinus surgery. Veterinary Clinics: Equine Practice, 30, 45–62. [DOI] [PubMed] [Google Scholar]
- Bardell, D. , Iff, I. , & Mosing, M. (2020). A cadaver study comparing two approaches to perform a maxillary nerve block in the horse. Equine Veterinary Journal, 42, 721–725 [DOI] [PubMed] [Google Scholar]
- Baxter, R. , Bramlett, K. , Onel, E. , & Daniels, S. (2013). Impact of local administration of liposome bupivacaine for postsurgical analgesia on wound healing: A review of data from ten prospective, controlled clinical studies. Clinical Therapeutics, 25, 312–320. [DOI] [PubMed] [Google Scholar]
- Beard, W. L. , Robertson, J. T. , & Leeth, B. (1990). Bilateral congenital cysts in the frontal sinuses of a horse. Journal of the American Veterinary Medical Association, 196, 453–454. [PubMed] [Google Scholar]
- Bicer, C. , Yontar, Y. , Gokahmetoglu, G. , & Eskitascioglu, T. (2018). Comparison of effects of levobupivacaine and ropivacaine infiltration on cutaneous wound healing in a rat model. Journal of Investigative Surgery, 31, 515–520. [DOI] [PubMed] [Google Scholar]
- Coumbre, K. M. , Jones, R. D. , & Kenward, J. H. (1987). Bilateral sinus empyema in a six‐year old mare. Equine Veterinary Journal, 19, 559–560. [DOI] [PubMed] [Google Scholar]
- Dixon, P. M. , Parkin, T. D. , Collins, N. , Hawkes, C. , Townsend, N. , Tremaine, W. H. , Fisher, G. , Ealey, R. , & Barakzai, S. Z. (2012a). Equine paranasal sinus disease—a long‐term study of 200 cases (1997–2009): Ancillary diagnostic findings and involvement of the various sinus compartments. Equine Veterinary Journal, 44, 267–271. [DOI] [PubMed] [Google Scholar]
- Dixon, P. M. , Parkin, T. D. , Collins, N. , Hawkes, C. , Townsend, N. , Tremaine, W. H. , Fisher, G. , Ealey, R. , & Barakzai, S. Z. (2012b). Equine paranasal sinus disease: A long‐term study of 200 cases (1997‐2009): Treatments and long‐term results of treatments. Equine Veterinary Journal, 44, 272–276. [DOI] [PubMed] [Google Scholar]
- Dixon, P. M. , Parkin, T. D. , Collins, N. , Hawkes, C. , Townsend, N. B. , Fisher, G. , Ealey, R. , & Barakzai, S. Z. (2011). Historical and clinical features of 200 cases of equine sinus disease. Veterinary Record, 169, 439. [DOI] [PubMed] [Google Scholar]
- Easley, J. T. , & Freeman, D. E. (2013). A single caudally based frontonasal bone flap for treatment of bilateral mucocele in the paranasal sinuses of an American Miniature Horse. Veterinary Surgery, 42, 427–432. [DOI] [PubMed] [Google Scholar]
- Freeman, D. E. , Orsini, P. G. , Ross, M. W. , & Madison, J. B. (1990). A large frontonasal bone flap for sinus surgery in the horse. Veterinary Surgery, 19, 122–130. [DOI] [PubMed] [Google Scholar]
- Hanci, V. , Hakimoglu, S. , Ozacmak, H. , Bektas, S. , Ozacmak, H. S. , Ozdamar, S. O. , Yurtlu, S. , & Turan, I. O. (2012). Comparison of the effects of bupivacaine, lidocaine, and tramadol infiltration on wound healing in rats. Revista Brasileira De Anestesiologia, 62, 799–810. [DOI] [PubMed] [Google Scholar]
- Head, K. W. , & Dixon, P. M. (1999), Equine nasal and paranasal sinus tumours. Part 1: Review of the literature and tumour classification. Veterinary Journal, 157, 261–278. [DOI] [PubMed] [Google Scholar]
- Kesici, S. , Kesici, U. , Ulusoy, H. , Erturkuner, P. , Turkmen, A. , & Arda, O. (2018). Effects of local anesthetics on wound healing. Revista Brasileira De Anestesiologia, 68, 375–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill, H. D. , Garcia‐Pereira, F. L. , & Mohankumar, P. S. (2014). Ultrasound‐guided injection of the maxillary nerve in the horse. Equine Veterinary Journal, 46, 180–184. [DOI] [PubMed] [Google Scholar]
- Ostrowska, J. , Lindström, L. , Tóth, T. , Hansson, K. , Uhlhorn, M. , & Ley, C. J. (2019). Computed tomography characteristics of equine paranasal sinus cysts. Equine Veterinary Journal, 52(4), 538–546. 10.1111/evj.13212. [DOI] [PubMed] [Google Scholar]
- Panneerselvam, E. , Balasubramanian, S. , Raja, V. B. , Kannan, R. , Rajaram, K. , & Rajendra, S. (2016). Plain lidocaine vs. lignocaine with vasoconstrictor – Comparative evaluation of pain during administration and post‐extraction wound healing by a double blinded randomized controlled clinical trial. Acta Odontologica Scandinavica, 74, 374–379. [DOI] [PubMed] [Google Scholar]
- Quinn, G. C. , Kidd, J. A. , & Lane, J. G. (2005). Modified frontonasal sinus flap surgery in standing horses: Surgical findings and outcomes of 60 cases. Equine Veterinary Journal, 37, 138–142. [DOI] [PubMed] [Google Scholar]
- Robert, M. P. , Stemmet, G. P. , & Smit, Y. A. (2019). bilateral sinus cyst treated via a bilateralfrontonasal bone flap in a standing horse. Journal of the South African Veterinary Association, 90, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher, J. , Dutton, D. M. , Murphy, D. J. , Hague, B. , & Taylor, T. S. (2000). Paranasal sinus surgery through a frontonasal flap in sedated, standing horses. Veterinary Surgery, 29, 173–177. [DOI] [PubMed] [Google Scholar]
- Silva, L. , Zoppa, A. L. V. , & Fernandes, W. R. (2009). Bilateral sinus cysts in a filly treated by endoscopic sinus surgery. Canadian Veterinary Journal, 50, 417–420. [PMC free article] [PubMed] [Google Scholar]
- Staszyk, C. , Bienert, A. , & Gasse, H. (2008). Stimulation of local anaesthetic nerve block of the infraorbital nerve within the pterygopalatine fossa: Anatomical landmarkers defined by computed tomography. Research in Veterinary Science, 178, 399–406. [DOI] [PubMed] [Google Scholar]
- Stauffer, S. , Cordner, B. , Dixon, J. , & Witte, T. (2017). Maxillary nerve blocks in horses: An experimental comparison of surface landmark and ultrasound‐guided techniques. Veterinary Anaesthesia and Analgesia, 44, 951–958. [DOI] [PubMed] [Google Scholar]
- Textor, J. A. , Puchalski, S. M. , Affolter, V. K. , MacDonald, M. H. , Galuppo, L. D. , & Wisner, E. R. (2012). Results of computed tomography in horses with ethmoid hematoma: 16 cases (1993‐2005). Journal of the American Veterinary Medical Association, 240, 1338–1344. [DOI] [PubMed] [Google Scholar]
- Tremaine, W. H. (2006). Complications associated with dental and paranasal sinus surgery. Proceedings of the AAEP Focus Meeting, Indianapolis, IN. [Google Scholar]
- Tremaine, W. H. , & Dixon, P. M. (2001a). A long‐term study of 277 cases of equine sinonasal disease. Part 1: Details of horses, historical, clinical and ancillary diagnostic findings. Equine Veterinary Journal, 33, 271–282. [DOI] [PubMed] [Google Scholar]
- Tremaine, W. H. , & Dixon, P. M. (2001b). A long‐term study of 277 cases of equine sinonasal disease. Part 2: treatments and results of treatments. Equine Veterinary Journal, 33, 283–289. [DOI] [PubMed] [Google Scholar]
- Waite, A. , Gilliver, S. C. , Masterson, G. R. , Hardman, M. J. , & Ashcroft, G. S. (2010). Clinically relevant doses of lidocaine and bupivacaine do not impair cutaneous wound healing in mice. British Journal of Anaesthesia, 104, 768–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodford, N. S. , & Lane, J. G. (2006). Long‐term retrospective study of 52 horses with sinunasal cysts. Equine Veterinary Journal, 38, 198–202. [DOI] [PubMed] [Google Scholar]
- Zeren, S. , Kesici, S. , Kesici, U. , Isbilir, S. , Turkmen, U. A. , Ulusoy, H. , Karpuz, V. , Ozcan, O. , Polat, E. , Ipcioglu, O. M. , & Sari, M. K. (2013). Effects of levobupivacaine on wound healing. Anesthesia and Analgesia, 116, 495–499. [DOI] [PubMed] [Google Scholar]


