Abstract
Objectives
With COVID-19 vaccination underway, this study aimed to understand belief, attitude and intention of the people in the South Asia region towards the vaccine.
Methods
We conducted a cross-sectional study using semi-structured questionnaires among 18201 individuals in four South Asian countries; Bangladesh, India, Pakistan, and Nepal between January 17 and February 2, 2021. We used the Health Belief Model (HBM) to identify the predictors related to vaccine acceptance. STATA (v16.1) was used for all analyses.
Results
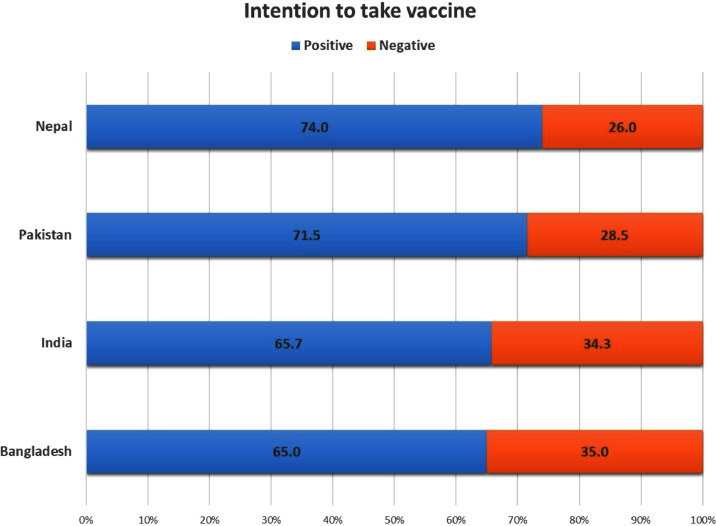
The percentage of respondents willing to be vaccinated against COVID-19 was 65%, 66%, 72% and 74% for Bangladesh, India, Pakistan and Nepal, respectively. Perceived destructive impact of COVID-19, positive perception of vaccines and concern about possible side effects were significant in modifying respondents’ intentions.. In multivariable logistic regression, age, sex, marital status, education, comorbidities, worry about getting infected, perceived COVID-19 impact, belief regarding vaccine efficacy, positive attitude towards mandatory measures, and vaccine availability were found to be associated with vaccine acceptance across countries.
Conclusion
Nearabout two-third of the respondants were willing to take COVID-19 vaccine in the four South Asia countries.
Keywords: COVID-19, Vaccine, Vaccine hesitancy, Vaccine acceptance, Health Belief Model, South Asia
Introduction
The COVID-19 pandemic, caused by SARS-CoV-2, is wreaking havoc around the world. Originating from China, the virus quickly spread worldwide to infect more than 100 million people and has caused more than 2 million deaths as of January 31, 2021 (World Health Organization, 2021). South Asia is among the most densely populated and poverty-stricken regions of the world and comprises a significant portion of global cases of COVID-19 (Chalise, 2020).
Although social distancing and quarantine have slowed down the spread of the virus and flattened the epidemic curve in many countries, only vaccination can entirely curtail infection spread, particularly in densely populated countries. Globally scientists have emphasized the importance of relatively high vaccine acceptance rates and the vaccination of comorbid people and the elderly (Harapan et al., 2020). Thus, the application of vaccines is a crucial step in tackling the ongoing crisis.
A total of 65 vaccines are in development globally, with 9 (including Sputnik V, Oxford-AstraZeneca and BBIBP-CorV) authorized in several countries, and the others in their second or third phase of development, as of January 26 2021 (Craven, 2021). Tagged as the most extensive vaccination campaign in history, more than 68.1 million people in 56 countries have been vaccinated to date (Randall et al., n.d.). However, the success of this campaign can be threatened by vaccine hesitancy. The World Health Organization labelled vaccine hesitancy as 1 of their 10 threats to global health in 2019 (World Health Organization, 2019); they defined it as “delay in acceptance or refusal of vaccines despite the availability of vaccination services”. Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines; it is influenced by factors such as complacency, convenience, and confidence (Sage Working Group, 2014). A relevant study has shown that COVID-19 vaccine acceptance varies from country to country, with no specific trend (Sallam, 2021). In developed countries, 15%–20% of the population have expressed unwillingness to receive the vaccine, while in developing countries reluctance can be as high as 63.2% (Mohamud et al., 2021).
The Health Belief Model (HBM) is a popular framework to understand human health behaviors. The HBM construct comprises different domains: perceived severity, perceived susceptibility, perceived benefits, perceived barriers, cues to action and self-efficacy (Jones et al., 2015). Perceived severity refers to a person's belief about the seriousness of consequences from infection, while perceived susceptibility refers to their beliefs regarding their vulnerability to infection. In terms of vaccine acceptance, perceived benefits refer to a person's beliefs regarding useful returns from being vaccinated, and perceived barriers are their beliefs about obstacles that stand in their way to being vaccinated. Whereas, self-efficacy is an individual's belief about his or her ability to do necessary actions to get vaccinated. Finally, cues to action can be defined as extraneous factors that influence a particular health behavior. The HBM model has been used in many studies to understand influenza vaccination uptake behavior (Brewer et al., 2007; Shahrabani et al., 2008). Identifying significant items from the HBM framework that influence COVID-19 vaccine acceptance could be a crucial step in enhancing vaccine coverage.
Literature is scarce on COVID-19 vaccine hesitancy in South Asian countries. A baseline study regarding vaccine acceptance in healthcare workers and the general population in South Asia may help to introduce vaccine hesitancy countermeasures to ensure vaccination program success. Therefore, our study aimed to understand the intention, belief, and attitude towards COVID-19 vaccines among the general population of four South Asian countries—namely Bangladesh, India, Pakistan and Nepal—before country-wide vaccination gets started.
Methodology
Study design and participants
We conducted a multi-country cross-sectional study. A convenience sampling technique was used because of limitations to doing extensive field research during the current active second wave of the COVID-19 outbreak in South Asia. We collected samples from our target adult population (aged ≥18 years) in four South Asian countries—Bangladesh, India, Pakistan, and Nepal—between January 17 and February 2, 2021. People with known mental illness were excluded. A total of 18201 people participated in the study.
Study procedure
A team of 36 experienced and trained researchers conducted and monitored data collection. As a convenience sampling technique was used, the interviewers were instructed to approach as many people as possible irrespective of their backgrounds. The team assigned and trained interviewers based on their locality to avoid language barriers. Participants were approached in public places like hospital outdoors, pharmacies, food markets, roads, offices, and at homes. In addition to approaching people in general, relatives, friends, colleagues, and students of the researchers were invited for the interview. Lockdown measures were relatively easened during the time of interview as the transmission of SARS-CoV-2 decreased. This ensured a large participation in the study. We translated the complicated terms of the questionnaire into a simplified, native version for ease of understanding by the study participants. Our interviewers provided explanations to help participants to understand specific item(s) while answering the questionnaire. The interviewers took necessary infection prevention measures before approaching participants. Participation was voluntary, and informed written consent was secured before inclusion in the study.
Measures
We used a semi-structured questionnaire to conduct face-to-face interviews to assess respondents’ beliefs, attitudes and intention to take the COVID-19 vaccine. The questionnaire consisted of sections on: 1) socio-demographic information, health profile, COVID-19 experience and previous vaccination history; 2) HBM constructs surrounding COVID-19 and vaccine; 3) acceptance of COVID-19 vaccine. The term COVID-19 was preferentially used during the face-to-face interview instead of coronavirus disease or SARS-CoV-2 infection as the term is more readily understood by the general population. After the literature review, the draft questionnaire was designed in English based on the tool used by Sherman et al. (2020). The questions were designed to cover the domains of the HBM model proposed by a group of social psychologists at the United States Public Health Service (Rosenstock, 1990). We modified and adjusted the framing and wording of questions according to the socio-cultural context of the South Asian subcontinent. The questionnaire was then translated into Bangla, Hindi, Urdu and Nepalese. Translated versions were validated by iterative revisions, and consensus by the investigators. Because of the time-sensitive nature of the study, forward-background translation by professional translators and review by relevant experts were out of the scope of the study. However, the face validity of the questionnaire was ensured in two steps. First, we shared the tool with the study supervisor and other researchers to give their expert opinion concerning its clarity, relevance and significance. Second, a pilot study was performed by selecting a limited population (n = 200) who shared their views on simplifying and shortening the questionnaire. We selected participants from different socio-economic backgrounds for the pilot study. Participants' amendments were considered and incorporated into the survey, thus maintaining continuity with contemporary literature. After a thorough discussion, the authors finalized the questionnaire (26 items) and distributed it for the study purpose. It took approximately 7–8 minutes per participant to complete. The complete questionnaire is available in the supplementary materials.
Socio-demographic information, health profile, COVID-19 experience and previous vaccination history
Personal details, including address, age, gender, education, marital status, occupation, size of the family, and average monthly family income, were collected. Respondents were asked if they had experienced COVID-19, whether they had any chronic diseases, and if they had taken any vaccine within the last few years (willingly/out of need). Respondents were asked whether any of their family members had been infected with COVID-19 and whether they had any elderly family member(s).
HBM constructs surrounding COVID-19 and vaccine
Items derived from the HBM were used to assess respondents’ beliefs about COVID-19 infection and vaccination. The items probed perceived susceptibility to COVID-19 infection (2 items), perceived severity of COVID-19 infection and pandemic situation (3 items), perceived benefits of COVID-19 vaccination (3 items), perceived barriers to COVID-19 vaccine (1 item), and cues to action regarding COVID-19 and its vaccine (3 items). The binary response option of ‘Yes’/’No’ was used to keep things simple for a study conducted among the general population.
COVID-19 vaccine acceptance
Acceptance of COVID-19 vaccine among the study population was assessed using a single item (If a COVID-19 vaccine is available to you, are you willing to be vaccinated?) on a 3 point-scale (‘Yes’, ‘No and ‘Not Sure’).
Statistical analysis
Descriptive statistics were used to characterize socio-demographic information of the participants from Bangladesh, India, Pakistan, and Nepal. The responses to the question about willingness to get vaccinated- 'No' and 'Not sure' were merged to produce one response 'No' for statistical analysis. Beliefs and attitudes towards COVID-19 and its vaccines and their association with willingness to be vaccinated were analyzed using the Chi-square test. Multivariable binary logistic regression analysis was performed to determine the association of COVID-19 vaccine acceptance among people with socio-demographic factors, health indicators and belief and attitude regarding vaccine. Estimated adjusted odds ratios (AOR) were expressed with corresponding 95% confidence interval (CI) . Statistical software STATA (Version 16.1) was used for all analyses.
Ethical statement
All the procedures were conducted following the ethical guidelines of the Institutional Review Board (IRB)/Ethical Review Committee (ERC) of North South University, Bangladesh (2021/OR-NSU/IRB-No.0304). The ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards were followed wherever applicable. We obtained written informed consent from all the participants involved in the study during the face-to-face interviews.
Results
The vaccine acceptance rate was 65%, 65.7%, 71.5% and 74.0% among participants in Bangladesh, India, Pakistan and Nepal, respectively (Figure 1 ).
Figure. 1.
Country specific COVID-19 vaccine acceptance rate
Table 1 shows the demographic profile of participants in relation to vaccine acceptance. The predominant age group in Bangladesh and India was 26–35 years, with ∼61.16% and ∼65.01%, respectively, of that age group willing to be vaccinated (p<0.001). Vaccine acceptance was significantly (P<0.001) higher among males (56.98%) in India, among females (69.02%) in Pakistan and statistically similar in both genders in Bangladesh and Nepal. In both Bangladesh (64.06%, P=0.036) and India (65.94%, P=<0.001), more married than unmarried participants were willing to be vaccinated, while in Pakistan, more unmarried participants were willing (78.37%, P=0.002). Being a graduate was significantly associated with vaccine acceptance in all countries except Nepal (P<0.05). The occupation group with the largest percentage willing to be vaccinated was students in Bangladesh (75.04%, P<0.001), while in India, it was service holders (68.08%) and other occupations (69.94%, P<0.001). Surprisingly, in Pakistan and Nepal, a large proportion of healthcare workers were not willing to be vaccinated (P>0.05). In terms of income, more than half (53.28%) of the participants from Bangladesh willing to be vaccinated belonged to the ‘no income to 20 000 Bangladeshi Taka’ group (P=<0.001). In India, vaccine acceptance was higher in people residing in city areas (71.74%, P=<0.001, while it was higher in rural areas of Bangladesh (74.03%, P=<0.001)
Table 1.
Socio-demographic characteristics of participants stratified by COVID-19 vaccine acceptance
| Bangladesh |
India |
Pakistan |
Nepal |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | ||||
| No (%) | Yes (%) | No (%) | Yes (%) | No (%) | Yes (%) | No (%) | Yes (%) | |||||
| Age | ||||||||||||
| <=25 | 612 (32.87) | 1250 (67.13) | <0.001 | 314 (43.55) | 407 (56.45) | <0.001 | - | - | - | 109(24.38) | 338(75.62) | 0.304 |
| 26–35 | 1008 (38.84) | 1587 (61.16) | 387 (34.99) | 719 (65.01) | - | - | 142(28.69) | 353(71.31) | ||||
| 36–45 | 531 (36.80) | 912 (63.20) | 162 (27.27) | 432 (72.73) | - | - | 71(25.45) | 208(74.55) | ||||
| 46–55 | 263 (27.86) | 681 (72.14) | 83 (36.40) | 145 (63.60) | - | - | 43(27.74) | 112(72.26) | ||||
| ≥ 56 | 156 (30.83) | 350 (69.17) | 40 (18.35) | 178 (81.65) | - | - | 35(21.08) | 131(78.92) | ||||
| Gender | ||||||||||||
| Male | 1717 (35.63) | 3102 (64.37) | 0.064 | 651 (37.74) | 1074 (62.26) | <0.001 | 669 (32.10) | 1415 (67.90) | <0.001 | 228(27.64) | 597(72.36) | 0.103 |
| Female | 846 (33.47) | 1682 (66.53) | 355 (37.74) | 811 (70.77) | 1147 (26.67) | 3153 (73.33) | 172(23.99) | 545(76.01) | ||||
| Marital status | ||||||||||||
| Married | 1776 (35.63) | 3209 (64.37) | 0.036 | 523 (29.61) | 1243 (70.39) | <0.001 | 325 (25.67) | 941 (74.33) | 0.002 | 248(26.75) | 679(73.25) | 0.352 |
| Unmarried | 754 (34.06) | 1460 (65.94) | 424 (44.96) | 519 (55.04) | 1457 (28.93) | 3580 (71.07) | 146(25.22) | 433(74.78) | ||||
| Divorced/Widowed/Separated | 42 (26.58) | 116 (73.42) | 39 (24.07) | 123 (75.93) | 34 (41.98) | 47 (58.02) | 6(16.67) | 30(80.33) | ||||
| Level of education | ||||||||||||
| No or Primary education | 484 (37.35) | 812 (62.65) | <0.001 | 88 (18.37) | 391 (81.63) | <0.001 | 77 (32.08) | 163 (67.92) | 0.005 | 2(25.00) | 6(75.00) | 0.318 |
| Secondary or equivalent | 810 (45.97) | 952 (54.03) | 115 (39.79) | 174 (60.21) | 106 (28.80) | 262 (71.20) | 113(25.00) | 339(75.00) | ||||
| Higher secondary or equivalent | 569 (35.30) | 1043 (64.70) | 269 (50.09) | 268 (49.91) | 395 (30.88) | 884 (69.12) | 111(24.61) | 340(75.39) | ||||
| Graduate | 490 (25.86) | 1405 (74.14) | 344 (25.74) | 649 (65.36) | 656 (29.40) | 1575 (70.60) | 146(26.40) | 407(73.60) | ||||
| Post-Graduate | 219 (27.65) | 573 (72.35) | 87 (25.74) | 251 (74.26) | 582 (25.68) | 1684 (74.32) | 28(35.90) | 50(64.10) | ||||
| Occupation | ||||||||||||
| Service holder | 1016 (35.31) | 1861 (64.69) | <0.001 | 264 (31.92) | 563 (68.08) | <0.001 | 342 (30.08) | 795 (69.92) | 0.069 | 158(25.69) | 457(74.31) | 0.524 |
| Businessperson | 572 (43.20) | 752 (56.80) | 161 (34.18) | 310 (65.82) | 106 (28.42) | 267 (71.58) | 50(29.24) | 121(70.76) | ||||
| Student | 315 (24.96) | 947 (75.04) | 260 (44.75) | 321 (55.25) | 1231 (28.61) | 3072 (71.39) | 108(27.00) | 292(73.00) | ||||
| Others | 666 (35.35) | 1218 (64.65) | 297 (30.06) | 691 (69.94) | 137 (23.99) | 434 (76.01) | 84(24.60) | 272(76.40) | ||||
| Health care worker | ||||||||||||
| No | 2203 (34.53) | 4177 (65.47) | 0.048 | 959 (34.53) | 1818 (65.47) | 0.041 | 1433 (28.65) | 3569 (71.35) | 0.495 | 312(25.41) | 916(74.59) | 0.345 |
| Yes | 369 (37.77) | 608 (62.23) | 20 (23.81) | 64 (76.19) | 383 (27.71) | 999 (72.29) | 88(28.03) | 226(71.97) | ||||
| Monthly Income | ||||||||||||
| No income to 20000 | 1623 (39) | 2539 (61) | <0.001 | 428 (34.05) | 829 (65.95) | 0.652 | 1062 (28.59) | 2652 (71.41) | 0.257 | 36(25.53) | 105(74.47) | 0.488 |
| 21000 to 40000 | 720 (34.62) | 1360 (65.38) | 239 (35.41) | 436 (64.95) | 270 (30.24) | 623 (69.76) | 61(29.33) | 147(70.67) | ||||
| 41000 and above | 225 (20.62) | 866 (79.38) | 269 (33.13) | 543 (66.87) | 484 (27.24) | 1293 (72.76) | 303(25.40) | 890(74.60) | ||||
| No. of Household members | ||||||||||||
| Small | 1181 (34.07) | 2285 (65.93) | 0.107 | 483 (33.38) | 964 (66.62) | 0.366 | 391 (28.29) | 991 (71.71) | 0.886 | 313(25.83) | 899(74.17) | 0.820 |
| Large | 1378 (35.88) | 2463 (64.12) | 476 (35.00) | 884 (65) | 1425 (28.49) | 3577 (71.51) | 87(26.44) | 242(73.56) | ||||
| Residence | ||||||||||||
| Rural | 514 (25.97) | 1465 (74.03) | <0.001 | 361 (33.27) | 724 (66.73) | <0.001 | 264 (30.73) | 595 (69.27) | 0.071 | 116(23.87) | 370(76.13) | 0.174 |
| Semi-urban | 533 (47.51) | 611 (52.49) | 324 (44.14) | 410 (55.86) | 1428 (28.41) | 3599 (71.59) | 107(29.48) | 256(70.52) | ||||
| City | 1504 (35.01) | 2708 (64.29) | 295 (28.26) | 749 (71.74) | 124 (24.90) | 374 (75.10) | 177(25.58) | 515(74.42) | ||||
Among the four countries, only in India was vaccine acceptance significantly higher among participants with prior COVID-19 infection (P=0.007) (Table 2). However, the presence of COVID-19 infected members in the family was a significant determinant of vaccine acceptance among participants in Bangladesh (P=0.028) and Pakistan (P<0.001). In India and Pakistan, a significantly higher proportion of participants with chronic disease were willing to be vaccinated (P=0.024, P=<0.001, respectively) than those without chronic disease. A reverse picture was seen in Bangladesh, with 59.04% vaccine acceptance in those with chronic disease and 66.71% in those without (P<0.001). This difference was not significant in Nepal. Only in Pakistan was having an elderly family member (>60 years) a significant factor influencing vaccine acceptance (P<0.001). Participants with a history of prior vaccination within the last few years were significantly more likely to indicate vaccine acceptance in all countries except Nepal (P=<0.001).
Table 2.
Vulnerabilities of participants to COVID and their association with vaccine acceptance
| Bangladesh |
India |
Pakistan |
Nepal |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | ||||
| No | Yes | No | Yes | No | Yes | No | Yes | |||||
| Were you diagnosed as having COVID-19? (Q10) | ||||||||||||
| No | 2379(35.08) | 4403(64.92) | 0.465 | 836(35.17) | 1541(64.83) | 0.007 | 1634(28.68) | 4064(71.32) | 0.239 | 342(26.45) | 951(73.55) | 0.298 |
| Yes | 193(33.57) | 382(66.43) | 139(28.78) | 344(71.22) | 182(26.53) | 504(73.47) | 58(23.29) | 191(76.71) | ||||
| Were any of your family members affected by COVID-19? (Q11) | ||||||||||||
| No | 2370(35.34) | 4336(64.66) | 0.028 | 713(34.70) | 1342(65.30) | 0.304 | 1508(30.17) | 3490(69.83) | <0.001 | 298(26.03) | 847(73.97) | 0.896 |
| Yes | 202(31.03) | 449(68.97) | 262(32.67) | 540(67.33) | 308(22.22) | 1078(77.78) | 102(25.69) | 295(74.31) | ||||
| Do you have any chronic disease (e.g., DM, HTN, CKD, COPD, CLD, or any other chronic diseases)? (Q12) | ||||||||||||
| No | 1917(33.29) | 3841(66.71) | <0.001 | 827(35.04) | 1,533(64.96) | 0.024 | 1730(29.05) | 4226(70.95) | <0.001 | 350(26.06) | 993(73.94) | 0.809 |
| Yes | 655(40.96) | 944(59.04) | 148(29.78) | 349(70.22) | 86(20.09) | 342(79.91) | 50(25.25) | 148(74.75) | ||||
| Do you have any members in your family who are over 60 years old? (Q13) | ||||||||||||
| No | 1327(34.49) | 2520(65.51) | 0.381 | 486(35.79) | 872(64.21) | 0.090 | 1006(30.83) | 2257(69.17) | <0.001 | 156(28.62) | 389(71.38) | 0.077 |
| Yes | 1245(35.47) | 2265(64.53) | 490(32.78) | 1005(67.22) | 810(25.95) | 2311(74.05) | 244(24.50) | 752(75.50) | ||||
| Did you take any vaccine within the last few years (willingly/out of need)? (Q14) | ||||||||||||
| No | 2088(36.61) | 3616(63.39) | <0.001 | 874(36.96) | 1491(63.04) | <0.001 | 1584(30.21) | 3659(69.79) | <0.001 | 374(26.43) | 1041(73.57) | 0.142 |
| Yes | 468(28.59) | 1169(71.41) | 58(13.49) | 372(86.51) | 232(20.33) | 909(79.67) | 26(20.47) | 101(79.53) | ||||
Participants were asked 12 questions covering the 5 domains of the HBM. Table 3 shows the association between participants' health beliefs and vaccine acceptance. On the perceived susceptibility domain, more than three-quarters of the participants in Pakistan (77.67%) and India (76.66%) who were worried about catching the coronavirus had vaccine acceptance that was significantly higher than those without this worry (P=<0.001). In Bangladesh, this number was 68.83% (P=<0.001), and in Nepal, vaccine acceptance was not associated with this worry (P=0.066). If the participant believed that he/she was immune to the virus there was significantly lower vaccine acceptance: Bangladesh (56.01% vs 73.54%), India (54.27% vs 72.16%) and Pakistan (67.79% vs 74.70%) (P<0.001 for all). On the perceived severity domain, those who thought coronavirus would be a mild illness for them were significantly less likely to be willing to be vaccinated in all countries except Nepal (P=0.058 Nepal, P<0.001 all other countries). This scenario was the same for those who thought too much fuss was being made about the risk of the coronavirus in Bangladesh (P<0.001) and India (P<0.001), however, in Pakistan and Nepal, this did not affect vaccine acceptance. However, vaccine acceptance was significantly higher among participants who perceived that the coronavirus pandemic had, had a big impact on their lives in India (68.35% vs 62.48%, P=0.006), Pakistan (75.91% vs 53.51%, P<0.001) and Nepal (75.30% vs 69.94%, P=0.043). Unexpectedly, in Bangladesh, the reverse was true, with vaccine acceptance significantly higher among the opposite group (62.60% vs 69.17%, P<0.001). On the perceived benefit domain, participants in all countries who thought only seriously ill people needed to take the vaccine were less likely to be willing to be vaccinated, with the difference being significant in Bangladesh (50.27% vs 75.13%) and India (45.10% vs 80.74%) (P<0.001 for both). In all four countries, those who believed that the vaccine would work against COVID-19 and those who thought the vaccine should be made mandatory were significantly more likely to be willing to be vaccinated (P<0.001 for all). On the perceived barriers domain, concern about the side effects of vaccines was negatively associated with vaccine acceptance in Bangladesh and India (P<0.001). However, participants in Pakistan and Nepal were significantly more likely to be willing to be vaccinated despite the concern (P<0.001 and P=0.036, respectively). On the cues to action domain, participants who thought that all are responsible for reducing the spread of the virus were more likely to be willing to be vaccinated in all countries except Bangladesh. Additionally, in all four countries, participants were significantly more likely to be willing to be vaccinated if the government recommended it (P<0.001) and if they would take it even if it was not free (P<0.05).
Table 3.
Association of vaccine acceptance within five domains of health belief model
| Bangladesh |
India |
Pakistan |
Nepal |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | Intent to accept vaccine |
P-value | ||||
| No | Yes | No | Yes | No | Yes | No | Yes | |||||
| Perceived susceptibility | ||||||||||||
| Are you worried about catching the Coronavirus? | ||||||||||||
| P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value | P-value |
| No | 1695 (37.31) | 2848 (62.69) | <0.001 | 509 (51.68) | 476 (48.32) | <0.001 | 755 (46.26) | 877 (53.74) | <0.001 | 148(28.85) | 365(71.15) | 0.066 |
| Yes | 877 (31.17) | 1937 (68.83) | 425 (23.34) | 1396 (76.66) | 1061 (22.33) | 3691 (77.67) | 252(24.49) | 777(75.51) | ||||
| Do you believe you are immune to the Coronavirus? | ||||||||||||
| No | 1003 (26.46) | 2787 (73.54) | <0.001 | 553 (27.84) | 1433 (72.16) | <0.001 | 880 (25.30) | 2598 (74.70) | <0.001 | 278(25.00) | 834(75.00) | 0.175 |
| Yes | 1569 (43.99) | 1998 (56.01) | 359 (45.73) | 426 (54.27) | 936 (32.21) | 1970 (67.79) | 122(28.37) | 308(71.63) | ||||
| Perceived severity | ||||||||||||
| Do you believe that the Coronavirus disease would be a mild illness for you? | ||||||||||||
| No | 1275 (30.18) | 2950 (69.82) | <0.001 | 327 (22.47) | 1128 (77.53) | <0.001 | 947 (32.59) | 1959 (67.41) | <0.001 | 286(24.72) | 871(75.28) | 0.058 |
| Yes | 1297 (41.41) | 1835 (58.59) | 587 (44.40) | 735 (55.60) | 869 (24.99) | 2609 (75.01) | 114(29.61) | 271(70.39) | ||||
| Do you think too much fuss is being made about the risk of the Coronavirus? | ||||||||||||
| No | 1791 (23.25) | 3762 (67.75) | <0.001 | 556 (26.35) | 1554 (73.65) | <0.001 | 831 (32.91) | 1694 (67.09) | <0.001 | 68(26.56) | 188(73.44) | 0.804 |
| Yes | 781 (43.29) | 1023 (56.71) | 303 (55.49) | 243 (44.51) | 985 (25.52) | 2874 (74.48) | 332(25.82) | 954(74.18) | ||||
| Did the Coronavirus pandemic have a big impact on your life? | ||||||||||||
| No | 842 (30.83) | 1889 (69.17) | <0.001 | 236 (37.52) | 393 (62.48) | 0.006 | 577 (46.49) | 664 (53.51) | <0.001 | 107(30.06) | 249(69.94) | 0.043 |
| Yes | 1730 (37.40) | 2896 (62.60) | 651 (31.65) | 1406 (68.35) | 1239 (24.09) | 3904 (75.91) | 293(24.70) | 893(75.30) | ||||
| Perceived benefits | ||||||||||||
| Do you think only people who are at a risk of serious illness from the Coronavirus need to be vaccinated? | ||||||||||||
| No | 1087 (24.87) | 3284 (75.13) | <0.001 | 307 (19.26) | 1287 (80.74) | <0.001 | 632 (27.25) | 1687 (72.75) | 0.111 | 302(25.15) | 899(74.85) | 0.172 |
| Yes | 1485 (49.73) | 1501 (50.27) | 599 (54.90) | 492 (45.10) | 1184 (29.13) | 2881 (70.87) | 98(28.82) | 242(71.18) | ||||
| Do you think vaccines will work against the COVID-19? | ||||||||||||
| No | 1093 (51.24) | 1040 (48.76) | <0.001 | 447 (79.68) | 114 (20.32) | <0.001 | 784 (64.90) | 424 (35.10) | <0.001 | 140(35.90) | 250(64.10) | <0.001 |
| Yes | 1479 (28.31) | 3745 (71.69) | 358 (19.42) | 1599 (66.51) | 1032 (19.94) | 4144 (80.06) | 260(22.57) | 892(77.43) | ||||
| Do you think vaccination should be made mandatory for everyone? | ||||||||||||
| No | 1333 (58.03) | 964 (41.97) | <0.001 | 506 (72.49) | 192 (27.51) | <0.001 | 1019 (64.29) | 566 (35.71) | <0.001 | 95(38.62) | 151(61.38) | <0.001 |
| Yes | 1239 (24.49) | 3821 (75.51) | 315 (16.71) | 1570 (83.29) | 797 (16.61) | 4002 (83.39) | 305(23.53) | 991(76.47) | ||||
| Perceived barriers | ||||||||||||
| Are you afraid/concerned about the safety/side effects of the COVID-19 vaccine? | ||||||||||||
| No | 576 (19.99) | 2305 (80.01) | <0.001 | 222 (24.05) | 701 (75.95) | <0.001 | 670 (40.12) | 1000 (59.88) | <0.001 | 47(33.33) | 94(66.67) | 0.036 |
| Yes | 1996 (44.59) | 2480 (55.41) | 690 (37.30) | 1160 (62.70) | 1146 (24.31) | 3568 (75.69) | 353(25.20) | 1048(74.80) | ||||
| Cues to action | ||||||||||||
| Do you think we are all responsible for reducing the spread of the Coronavirus? | ||||||||||||
| No | 240 (29.34) | 578 (70.66) | <0.001 | 400 (6.16) | 254 (38.84) | <0.001 | 438 (51.59) | 411 (48.41) | <0.001 | 54(27.27) | 144(72.73) | 0.647 |
| Yes | 2332 (35.66) | 4207 (64.34) | 481 (23.74) | 1545 (76.26) | 1378 (24.90) | 4157 (75.10) | 346(25.74) | 998(74.26) | ||||
| If the Coronavirus vaccination were recommended by the Government, would you get vaccinated? | ||||||||||||
| No | 1153 (65.44) | 609 (34.56) | <0.001 | 475 (85.59) | 80 (14.41) | <0.001 | - | - | - | 196(97.03) | 6(2.97) | <0.001 |
| Yes | 1419 (25.36) | 4176 (74.64) | 432 (19.49) | 1784 (80.51) | - | - | - | 204(15.22) | 1136(84.78) | |||
| Do you agree to take the COVID-19 vaccine if it is not free? | ||||||||||||
| No | 1935 (47.74) | 2118 (52.26) | <0.001 | 783 (44.64) | 971 (55.36) | <0.001 | 1315 (53.56) | 1140 (46.44) | <0.001 | 174(30.26) | 401(69.74) | 0.003 |
| Yes | 637 (19.28) | 2667 (80.72) | 165 (15.39) | 907 (84.61) | 501 (12.75) | 3428 (87.25) | 226(23.37) | 741(76.63) | ||||
Table 4.
Multivariable logistic regression analysis exploring factors associated with COVID-19 vaccine acceptance
| Variables | Bangladesh | India | Pakistan | Nepal |
|---|---|---|---|---|
| Age | ||||
| ≤ 25 | 1 | 1 | - | 1 |
| 26–35 | 1.03 (0.86 – 1.26) | 1.24 (0.71 – 2.18) | - | 0.86 (0.50 – 1.47) |
| 36–45 | 1.23 (0.98 – 1.54) | 1.15 (0.60 – 2.20) | - | 1.06 (0.53 – 2.14) |
| 46–55 | 1.70 (1.32 – 2.20) | 1.68 (0.74 – 3.79) | - | 1.05 (0.48 – 2.28) |
| ≥ 56 | 1.58 (1.17 – 2.15) | 2.36 (0.76 – 7.39) | - | 1.00 (0.42 – 2.39) |
| Sex | ||||
| Male | 1 | 1 | 1 | 1 |
| Female | 1.08 (0.94 – 1.24) | 1.74 (1.23 – 2.45) | 0.87 (0.74 – 1.03) | 0.90 (0.66 – 1.23) |
| Marital Status | ||||
| Married | 1 | 1 | 1 | 1 |
| Unmarried | 0.97 (0.82 – 1.16) | 0.87 (0.54 – 1.39) | 0.95 (0.75 - 1.20) | 1.08 (0.66 – 1.77) |
| Divorced/ Widowed/ Separated | 1.66 (1.08 – 2.57) | 1.51 (0.68 – 3.37) | 0.81 (0.44 – 1.47) | 1.26 (0.40 – 3.92) |
| Education | ||||
| No or primary education | 1 | 1 | 1 | 1 |
| Secondary or equivalent | 0.87 (0.71 – 1.05) | 0.41 (0.22 - 0.74) | 0.75 (0.47 – 1.18) | 0.26 (0.01 – 6.94) |
| Higher secondary or diploma | 1.30 (1.04 – 1.63) | 0.27 (0.14 - 0.52) | 0.66 (0.45 – 0.97) | 0.27 (0.01 – 7.14) |
| Graduate | 1.91 (1.50 – 2.44) | 0.38 (0.20 - 0.73) | 0.78 (0.54 – 1.13) | 0.26 (0.01 – 6.97) |
| Post-graduate | 1.39 (1.05 – 1.84) | 0.62 (0.27 – 1.41) | 1.00 (0.69 – 1.46) | 0.13 (0.00 – 3.72) |
| Occupation | ||||
| Service holder | 1 | 1 | 1 | 1 |
| Businessperson | 0.80 (0.67 – 0.96) | 1.84 (1.07 – 3.18) | 1.00 (0.72 – 1.40) | 0.72 (0.43 – 1.20) |
| Student | 1.87 (1.48 – 2.36) | 1.09 (0.54 – 2.18) | 1.12 (0.89 – 1.41) | 0.90 (0.53 – 1.53) |
| Others | 1.17 (0.96 – 1.43) | 0.67 (0.39 – 1.14) | 1.03 (0.75 – 1.42) | 0.87 (0.51 – 1.49) |
| Healthcare workers | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.76 (0.63 - 0.93) | 5.14 (2.03 – 12.98) | 0.94 (0.79 – 1.11) | 0.68 (0.45 – 1.02) |
| Income | ||||
| No income to 20000 | 1 | 1 | 1 | 1 |
| 21000 to 40000 | 1.12 (0.95 – 1.30) | 0.59 (0.36 - 0.95) | 0.89 (0.72 – 1.10) | 0.58 (0.29 – 1.14) |
| 41000 and above | 1.84 (1.48 – 2.28) | 0.30 (0.18 – 0.52) | 1.00 (0.84 – 1.18) | 0.72 (0.39 – 1.34) |
| Family size | ||||
| Small | 1 | 1 | 1 | 1 |
| Large | 1.02 (0.91 – 1.15) | 0.84 (0.61 – 1.16) | 0.89 (0.76 – 1.06) | 0.84 (0.58 – 1.21) |
| Residence | ||||
| Rural | 1 | 1 | 1 | 1 |
| Semi-urban | 0.35 (0.29 - 0.42) | 1.18 (0.75 – 1.84) | 1.02 (0.84 – 1.25) | 0.85 (0.57 – 1.28) |
| Urban | 0.45 (0.38 – 0.52) | 1.50 (0.91 – 2.47) | 1.46 (1.07 – 1.99) | 1.08 (0.75 – 1.55) |
| Were you diagnosed as having COVID-19? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.80 (0.63 - 1.03) | 0.66 (0.41 – 1.06) | 1.14 (0.89 – 1.44) | 1.29 (0.84 – 2.00) |
| Were any of your family members affected by COVID-19? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.37 (1.08 – 1.75) | 0.83 (0.53 – 1.32) | 1.19 (0.99 – 1.44) | 0.96 (0.68 – 1.37) |
| Do you have any chronic disease (e.g., DM, HTN, CKD, COPD, CLD, or any other chronic diseases)? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.78 (0.67 - 0.90) | 0.89 (0.55 – 1.46) | 1.70 (1.24 – 2.32) | 0.98 (0.58 – 1.66) |
| Do you have any members in your family who are over 60 years old? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.88 (0.78 - 1.00) | 1.63 (1.15 – 2.31) | 1.03 (0.89 – 1.18) | 1.29 (0.94 – 1.78) |
| Did you take any vaccine within the last few years (willingly/out of need)? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 2.16 (1.85 – 2.52) | 1.44 (0.88 – 2.36) | 1.16 (0.96 – 1.42) | 1.14 (0.66 – 1.99) |
| Perceived susceptibility | ||||
| Are you worried about catching coronavirus? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.18 (1.04 - 1.35) | 2.96 (2.08 – 4.22) | 1.46 (1.24 – 1.72) | 1.21 (0.88 – 1.68) |
| Do you believe you are immune to the Coronavirus? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.72 (0.63 - 0.83) | 0.28 (0.18 - 0.43) | 0.93 (0.81 – 1.06) | 0.83 (0.59 – 1.18) |
| Perceived severity | ||||
| Do you believe that the Coronavirus disease would be a mild illness for you? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.98 (0.86 – 1.12) | 0.23 (0.16 - 0.33) | 1.08 (0.94 – 1.24) | 0.68 (0.48 – 0.94) |
| Do you think too much fuss is being made about the risk of the Coronavirus? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.48 (1.28 – 1.72) | 1.40 (0.89 – 2.18) | 1.08 (0.94 – 1.25) | 1.16 (0.67 – 2.01) |
| Did the Coronavirus pandemic have a big impact on your life? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.16 (1.01 – 1.33) | 0.60 (0.38 - 0.95) | 1.21 (1.02 – 1.44) | 1.09 (0.76 – 1.57) |
| Perceived benefits | ||||
| Do you think only people, who are at risk of serious illness from the Coronavirus, need to be vaccinated? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.83 (0.73 - 0.95) | 0.53 (0.36 - 0.77) | 0.58 (0.50 - 0.68) | 1.02 (0.70 – 1.47) |
| Do you think vaccines will work against the COVID-19? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.70 (1.49 – 1.94) | 3.34 (2.04 – 5.47) | 2.93 (2.47 – 3.47) | 1.57 (1.12 – 2.21) |
| Do you think vaccination should be made mandatory for everyone? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 2.05 (1.77 – 2.36) | 4.76 (2.96 – 7.66) | 4.30 (3.69 – 5.00) | 1.56 (1.05 – 2.33) |
| Perceived barriers | ||||
| Are you afraid/concerned about the safety/side effects of the COVID-19 vaccine? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 0.44 (0.38 - 0.50) | 0.28 (0.19 - 0.42) | 1.03 (0.87 – 1.21) | 1.34 (0.81 – 2.21) |
| Cues to action | ||||
| Do you think we are all responsible for reducing the spread of the Coronavirus? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.01 (0.82 – 1.24) | 0.68 (0.41- 1.14) | 1.49 (1.21 – 1.82) | 1.23 (0.65 – 2.31) |
| If the Coronavirus vaccination were recommended by the Government, would you get vaccinated? | ||||
| No | 1 | 1 | - | 1 |
| Yes | 2.98 (2.58 – 3.44) | 9.33 (5.70 – 15.27) | - | 199.69 (85.79 – 464.83) |
| Do you agree to take the COVID-19 vaccine if it is not free? | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.70 (1.48 – 1.94) | 2.41 (1.70 – 3.41) | 4.35 (3.78 – 5.00) | 1.17 (0.86 – 1.60) |
We performed a multivariable binary logistic regression analysis to identify the independent determinants of COVID-19 vaccine acceptance in the four South Asian countries (Table 4). In Bangladesh, participants aged 46–55 years were x1.70 (95% CI: 1.32–2.20) more likely to be willing to be vaccinated than those aged <25 years; this was also true for people aged ≥56 years (AOR: 1.58, 95% CI: 1.17–2.15). COVID-19 vaccine acceptance was x1.74 (95% CI: 1.23–2.45) more common among females than males in India. Graduates in Bangladesh were significantly more likely than participants with lower education levels to be willing to be vaccinated (AOR: 1.91; 95% CI: 1.50–2.44) but considerably less so in India (AOR: 0.38; 95% CI: 0.20–0.73). Students and businesspersons were significantly more likely to be willing to be vaccinated than other occupation groups in Bangladesh (AOR: 1.87, 95% CI: 1.48–2.36) and India (AOR: 1.84, 95% CI: 1.07–3.18). However, our analysis showed that only in Bangladesh did vaccine acceptance significantly increase with people's income. Participants from urban Bangladesh were 55% (AOR: 0.45; 95% CI: 0.38-0.52) less likely to be willing to be vaccinated than those from rural areas, whereas, in Pakistan, urban participants had x1.46 (AOR: 1.46; 95% CI: 1.07–1.99) higher vaccine acceptance. Respondents in Bangladesh were x1.37 (AOR: 1.37; 95% CI: 1.08–1.75) more likely to be willing to be vaccinated if they had COVID-19 affected family members. People with comorbidities showed substantially less vaccine acceptance than those without in Bangladesh (AOR: 0.78; 95% CI: 0.67–0.90); however, in Pakistan, this group were x1.70 (95% CI: 1.24-2.32) more likely to be willing to be vaccinated.
With regard to perceived severity, vaccine acceptance was x1.18 (AOR: 1.18; 95% CI: 1.04–1.35), x2.96 (AOR: 2.96; 95% CI: 2.08–4.22) and x1.46 (AOR: 1.46; 95% CI: 1.24–1.72) higher among people who were worried about catching the coronavirus in Bangladesh, India and Pakistan, respectively. Conversely, participants in Bangladesh and India who believed they were immune to the coronavirus were less likely to be willing to be vaccinated (AOR: 0.72, 95% CI: 0.63–0.83; AOR: 0.28, 95% CI: 0.18–0.43, respectively). Participants in India and Nepal who thought COVID-19 would be a mild disease for them were, respectively, 77% (AOR: 0.23; 95% CI: 0.16–0.33) and 32% (AOR: 0.68; 95% CI: 0.48–0.94) less likely to be willing to be vaccinated. On the other hand, in Bangladesh and Pakistan, those for whom the COVID-19 pandemic had, had a big impact on their lives were, respectively, x1.16 (AOR: 1.16; 95% CI: 1.01–1.33) and x1.21 (AOR: 1.21; 95% CI: 1.02–1.44) more likely to be willing to be vaccinated, whereas they were 40% (AOR: 0.60; 95% CI: 0.38–0.95) less likely in India.
In these South Asian countries, participants with a positive belief in mandatory vaccination and vaccine efficacy (perceived benefit domain of HBM) were more likely to be willing to be vaccinated than those who did not. In the perceived barriers domain, concern about the side effects of vaccines tended to diminish vaccine acceptance in Bangladesh (AOR: 0.44; 95% CI: 0.38 - 0.50) and India (AOR: 0.28; 95% CI: 0.19 - 0.42). In the cues to action domain of HBM, participants were significantly more likely to be willing to be vaccinated if the government recommended it in Bangladesh (AOR 2.98; 95% CI 2.58–3.44), India (AOR 9.33; 95% CI 5.70–15.27) and Nepal (AOR 199.69, 95% CI 85.79–464.83). Finally, in all countries, participants were more likely to be willing to be vaccinated if the vaccine were free.
Discussion
Nearly two-thirds of participants in Bangladesh and India, and nearly three-quarters in Pakistan and Nepal, had vaccine acceptance. Given that a substantial proportion of the population needs to be vaccinated to achieve herd immunity against COVID-19 and that the approved vaccines are not 100% effective in reducing the risk of contracting the disease (Olliaro et al., 2021), this acceptance rate appears low. As many people are getting natural immunity through infection, the higher the coverage of vaccination the smoother the path to normality would become (Gu, 2021). Our study explored the effect of socio-demographic factors, the impact of COVID-19, and the health belief domains of participants towards the COVID-19 vaccine in Bangladesh, India, Pakistan and Nepal.
In Bangladesh, participants aged ≥46 years were more likely to be willing to be vaccinated than those aged ≤25. This association of increasing age with vaccine acceptance was also observed in a study in Hong Kong (Wong et al., 2021). Young people have been described as having a greater proclivity for "invulnerability bias" and are therefore considered the most apprehensive about COVID-19 immunization (Barello et al., 2020; Neumann-Böhme et al., 2020). Female participants in India were more likely to be willing to be vaccinated than men. In the USA, it has recently been found that more women receive COVID-19 vaccines than men, even though more men die of the disease (Ungar, 2021). However, in most Indian states, disparities in distribution were exacerbated by misinformation, access issues and patriarchal social norms, and women have received fewer vaccinations than men (Guha, 2021). According to Neumann-Böhme et al., the female population can be more easily convinced than men to get vaccinated for herd immunity (Neumann-Böhme et al., 2020). People with secondary education or higher were more likely to be willing to be vaccinated than those with primary or no education in Bangladesh. Similar associations of higher education level and vaccine acceptance have been found in the USA (Kelly et al., 2021) and China (Gan et al., 2021). According to Gan et al., people with higher-level education may have a better understanding of COVID-19 and immunization than those with less formal education (Gan et al., 2021). Surprisingly, in India, people with secondary education or higher were less likely to be willing to be vaccinated than people with primary or no education. A similar trend was also observed in Pakistani participants. One reason could be an overly cautious approach to their health and concerns about side effects.
In India, businesspeople were more likely than other occupations to be willing to be vaccinated, but this group were less likely in Bangladesh compared with service holders in the South Asian countrie. Additionally, students were more likely to be willing to be vaccinated compared with service holders in Bangladesh. Healthcare workers in India were more likely than other occupations to be willing to be vaccinated, but less likely in Bangladesh. Healthcare workers in Ghana have also been found to be likely to be willing to be vaccinated when compared with the general population (Agyekum et al., 2021). On the other hand, another study conducted among six countries in Asia-Pacific region comprising of China, India, Indonesia, Singapore, Vietnam and Bhutan found that most health professionals in this region are willing to receive COVID-19 vaccine despite vaccine safety concerns (Chew et al., 2021). Participants with higher income levels in Bangladesh were more likely to be willing to be vaccinated, but significantly less likely in India compared with participants with no income or an income level ≤20 000 units. Low-income groups have been shown to be at an increased risk of contracting COVID-19 due to crowded living standards, their reliance on public transportation, and their increased likelihood of continuing to work outside the home (Bono et al., 2021). Therefore, our findings are concerning for the people of Bangladesh. Moreover, people living in semi-urban and urban areas of Bangladesh were less likely to be willing to be vaccinated than people living in rural Bangladesh, consistent with vaccine hesitancy in participants from lower socioeconomic strata. Policymakers need to take note of this issue in planning vaccination coverage in the country. The scenario was different in Pakistan, where vaccine acceptance was significantly higher in urban areas than rural. Local health practitioners, healthcare professionals and local partners must confront vaccine reluctance in rural areas of Pakistan as most rural inhabitants reported having confidence in their own medical care providers when it comes to COVID-19 vaccine information, highlighting the critical role of public healthcare professionals collaborating with established health care structures in rural areas (Kirzinger et al., 2021).
Among study participants in Bangladesh, those who had family members infected with COVID-19 had higher vaccine acceptance compared with those who did not. Social responsibility and a favorable attitude toward vaccination and immunization services may have played a role here (Ruiz & Bell, 2021). However, people in Bangladesh with chronic diseases were less likely to be willing to be vaccinated than those without chronic diseases. Another study confirmed this finding; it reasoned that uncertainty about vaccine effectiveness, potential side effects, and a lack of trust in vaccines might contribute to hesitancy (Abedin et al., 2021). Conversely, Pakistani participants with chronic disease were more likely to be willing to be vaccinated than those without chronic disease. Another study found a similar result; that people with comorbidities associated with poorer COVID-19 clinical outcomes are significantly more willing to engage in risk-reducing behaviors such as social isolation and mask use and support a variety of community-level interventions (Ricotta et al., 2021). In India, participants with family members >60 years old were significantly more likely to be willing to be vaccinated. As older persons are at a higher risk of developing severe COVID-19, participants with an older family member might reasonably have felt more cautious.
In Bangladesh, we observed that participants with a history of previous vaccination were significantly more likely to be willing to be vaccinated. A similar association of previous vaccine history with willingness to receive a COVID-19 vaccine has been observed in Ethiopia (Zewude & Habtegiorgis, 2021) and Kuwait (Alqudeimat et al., 2021).
We wanted to explore how the HBM framework helps predict vaccine acceptance in South Asian population-dense countries. The study was conducted during a period of gradual decline in COVID-19 cases in India, Bangladesh, Pakistan and Nepal. Between January 17 and February 2, 2021, the average daily confirmed COVID-19 cases were <300 in Nepal, <800 in Bangladesh, <1500 in Pakistan and <10 000 in India. Notably, our data indicate that participants from Bangladesh, India, and Pakistan worried about catching the coronavirus had higher vaccine acceptance. Moreover, participants in Bangladesh and India who believed they were not immune to the coronavirus were more likely to be willing to be vaccinated, indicating that participants with a perceived susceptibility towards the disease had significantly higher vaccine acceptance. This finding is supported by previous research, which observed that increased perceived susceptibility and risk results in more effective preventive actions and improved epidemic control (Verelst et al., 2016). Regarding perceived severity, Indian and Nepalese participants who thought coronavirus disease would cause only mild illness were significantly less likely to be willing to be vaccinated. Lower perceived severity may allay one's fears about contracting the virus (Baines et al., 2021), thereby negatively impacting vaccine acceptance. In Bangladesh and Pakistan, study participants who believed the coronavirus had a big impact on their life were more likely to be willing to be vaccinated. A Chinese study found that the pandemic has profoundly impacted jobs, income, and daily lives in China (Wang et al., 2020). China has adopted dramatic steps and public health interventions to restrict the spread of COVID-19, which has significantly slowed the disease's progress (Leung et al., 2020; Tian et al., 2020; Zhang et al., 2021). Whereas, our study indicates that a favorable perception of vaccine benefits and decreased perceived barriers to vaccination were the two most influential constructs influencing vaccine acceptance. Regarding perceived benefits, in all countries, participants who thought vaccination should be mandatory for everyone were more likely to be willing to be vaccinated. According to a study conducted by Liora Shmueli et al., those with vaccine acceptance perceived high benefits from getting the COVID-19 vaccine in terms of protecting themselves and others (Shmueli, 2021); this is similar to a study reported by Dror et al., which indicates that vaccine compliance is based on an individual's risk-benefit perception (Dror et al., 2020).
Participants who thought only people at risk of serious illness needed to be vaccinated were less likely to be willing to be vaccinated. This finding was significant in Bangladesh, India and Pakistan. A similar significant finding was reported by Sherman et al. in the UK (Sherman et al., 2020). In our study, respondents in all four countries who believed in COVID-19 vaccine efficacy had a higher level of vaccine acceptance. This is reasonable as people place a higher priority on vaccine efficacy and safety than on vaccine cost (Lin et al., 2020). Furthermore, in our study, those who agreed to take the COVID-19 vaccine even if it is not free were more likely to be willing to be vaccinated than those who did not.
With regard to perceived barriers, participants in Bangladesh and India who thought the vaccine might have side effects were less likely to be willing to be vaccinated. Perceived barriers to COVID-19 vaccination observed in our study have been found in earlier studies on the introduction of new vaccines, including concerns about vaccine negative effects, efficacy and safety (Schmid et al., 2017).
In terms of cues to action, we found that Pakistani participants who believed they were accountable for reducing the spread of COVID-19 were more likely to be willing to be vaccinated than those who did not. Participants from Bangladesh, India and Nepal were more likely to be willing to be vaccinated if the government recommended taking the vaccine. Wong et al. in a population-based survey in Hong Kong found similar results and noted that government advice was a significantly more powerful cue than advice from doctors and family members (Wong et al., 2021).
Bangladesh and India have recently experienced a second wave of COVID-19 with the Delta-V variant, which was discovered in India during a vaccine shortage (Frayer & Pathak, 2021). Mass vaccination is crucial to slow down the virus. However, as seen in Pakistan, lack of education, misinformation, vaccine reluctance, and inadequate promotion are some reasons for slow vaccination rates (ANI, 2021). Our study observed that public vaccine acceptance depends on a complex interaction of socio-demographic factors and health-related perceptions and beliefs. Although these factors do not fit clearly within a framework in the four countries, certain areas have emerged where work can be done to increase vaccine acceptance, and the respective health authorities would benefit from these findings.
Data collection in our study was limited by convenience sampling; however, structured sampling from four countries within a short period was not possible because of the limitations created by the ongoing COVID-19 pandemic. The strength of our study is that this was the first multi-country study on COVID-19 vaccine acceptance with a large sample size in the South Asian region.
Conclusion
Our multi-country study found that belief, attitude, and intention to accept the COVID-19 vaccine among the South Asian population are similar. The study revealed several important determinants of vaccine acceptance, including age, education, marital status, occupation, income, residence status, comorbidities, impact of COVID-19 in the family, perceived severity of the disease, positive belief towards vaccine efficacy, and government recommendation of vaccines. The findings of our study should be helpful to policymakers and health management personnel in the countries studied in vaccination implementation and management.
Funding
No funding was received for this study.
Author's contribution
DHH, MUR, MASK, MAH, MoH, MMAH and SYB carried out the literature search. DHH, MHN and MLR conceived and designed the study. DHH, MASK, MUR and MAH oversaw its implementation, analysis, and write-up. MLR, MASK and TA planned the statistical analyses. MUR outlined the data collection procedure. MUR and MAH led the field implementation of the study. MMAH, MoH and KFM were responsible for data entry. AN, MMAH, SS, SYB, MoH, KFM, SRS, MUR, MASK, MAH, MAR, MG, RMM, MYA, SMRH, RM, SK, JZK, MeH, RR, JK, OK, AMKI, NN, AHMA, HU, NI, UA, MN, IK, SKP and SG contributed to the field implementation of the study and undertook data entry. DHH, MLR, MASK, MMAH, KFM and TA verified the underlying data. TA, MASK and MLR were responsible for the statistical analyses. DHH, MHN, MLR, MASK, MAH, MUR, MMAH, MoH, KFM, RMM, SYB, SS, SMRH, MeH and SK wrote the first draft of the manuscript. All authors read and approved the manuscript.
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
Acknowledgments
We would like to express our sincere thanks and gratitude to the study participants for their patience and cooperation during the interview.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijid.2021.09.056.
Appendix. Supplementary materials
References
- Abedin M., Islam M.A., Rahman F.N., Reza H.M., Hossain M.Z., Hossain M.A., Arefin A., Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLOS ONE. 2021;16(4) doi: 10.1371/JOURNAL.PONE.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agyekum M.W., Afrifa-Anane G.F., Kyei-Arthur F., Addo B. Advances in Public Health; 2021. Acceptability of COVID-19 Vaccination among Health Care Workers in Ghana. 2021. [DOI] [Google Scholar]
- Alqudeimat Y., Alenezi D., AlHajri B., Alfouzan H., Almokhaizeem Z., Altamimi S., Almansouri W., Alzalzalah S., Ziyab A.H. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Medical Principles and Practice. 2021;30(3):262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANI. (2021). Pakistan's pace of Covid-19 vaccination remains “very slow” - Times of India. https://timesofindia.indiatimes.com/world/pakistan/pakistans-pace-of-covid-19-vaccination-remains-very-slow/articleshow/84059670.cms
- Baines A., Ittefaq M., Abwao M. #Scamdemic, #Plandemic, or #Scaredemic: What Parler Social Media Platform Tells Us about COVID-19 Vaccine. Vaccines. 2021;9(5):421. doi: 10.3390/VACCINES9050421. 2021, Vol. 9, Page 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello S., Nania T., Dellafiore F., Graffigna G., Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. European Journal of Epidemiology. 2020;35(8):781–783. doi: 10.1007/S10654-020-00670-Z. 2020 35:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bono S.A., Villela E.F., de M., Siau C.S., Chen W.S., Pengpid S., Hasan M.T., Sessou P., Ditekemena J.D., Amodan B.O., Hosseinipour M.C., Dolo H., Fodjo J.N.S., Low W.Y., Colebunders R. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines. 2021;9(5):515. doi: 10.3390/VACCINES9050515. 2021, Vol. 9, Page 515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Chalise H.N. COVID-19 Situation and Challenges for Nepal. Asia Pacific Journal of Public Health. 2020;32(5):281–282. doi: 10.1177/1010539520932709. [DOI] [PubMed] [Google Scholar]
- Chew N.W.S., Cheong C., Kong G., Phua K., Ngiam J.N., Tan B.Y.Q., Wang B., Hao F., Tan W., Han X., Tran B.X., Hoang M.T., Pham H.Q., Vu G.T., Chen Y., Danuaji R., RN K., PV M., Talati K.…Sharma V.K. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. International Journal of Infectious Diseases. 2021;106:52–60. doi: 10.1016/J.IJID.2021.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craven J. 2021. COVID-19 vaccine tracker.https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker August 23. [Google Scholar]
- Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., Srouji S., Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. European Journal of Epidemiology. 2020;35(8):775–779. doi: 10.1007/S10654-020-00671-Y. 2020 35:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayer, L., & Pathak, S. (2021). Bangladesh Shuts Down As Daily COVID Cases Rise : Coronavirus Updates : NPR. https://www.npr.org/sections/coronavirus-live-updates/2021/07/01/1012106091/bangladesh-locks-down-as-daily-covid-cases-quintuple
- Gan L., Chen Y., Hu P., Wu D., Zhu Y., Tan J., Li Y., Zhang D. Willingness to Receive SARS-CoV-2 Vaccination and Associated Factors among Chinese Adults: A Cross Sectional Survey. International Journal of Environmental Research and Public Health 2021. 2021;18(4):1993. doi: 10.3390/IJERPH18041993. Vol. 18, Page 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y. 2021. Path to Normality - COVID-19 Vaccine Projections.https://covid19-projections.com/path-to-herd-immunity/ [Google Scholar]
- Guha N. 2021. India's Covid gender gap: women left behind in vaccination drive | Global development | The Guardian.https://www.theguardian.com/global-development/2021/jun/28/india-covid-gender-gap-women-left-behind-in-vaccination-drive [Google Scholar]
- Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., Setiawan A.M., Rajamoorthy Y., Sofyan H., Mudatsir M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Frontiers in Public Health. 2020;0:381. doi: 10.3389/FPUBH.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C.L., Jensen J.D., Scherr C.L., Brown N.R., Christy K., Weaver J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Communication. 2015;30(6):566–576. doi: 10.1080/10410236.2013.873363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B.J., Southwell B.G., McCormack L.A., Bann C.M., MacDonald P.D.M., Frasier A.M., Bevc C.A., Brewer N.T., Squiers L.B. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infectious Diseases. 2021;21(1):1–7. doi: 10.1186/S12879-021-06023-9. 2021 21:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirzinger, A., Muñana, C., & Brodie, M. (2021, January 7). Vaccine Hesitancy in Rural America | KFF. https://www.kff.org/coronavirus-covid-19/poll-finding/vaccine-hesitancy-in-rural-america/
- Leung K., Wu J.T., Liu D., Leung G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. The Lancet. 2020;395(10233):1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLOS Neglected Tropical Diseases. 2020;14(12) doi: 10.1371/JOURNAL.PNTD.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamud I., Abdullahi Mohamed S., Abdullahi Jimale K. Assessments of a COVID-19 vaccine acceptance rate in population of Benadir region, Somalia. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN. 2021;20:1–04. doi: 10.9790/0853-2001050104. [DOI] [Google Scholar]
- Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., Exel J., van, Schreyögg J., Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. The European Journal of Health Economics. 2020;21(7):977–982. doi: 10.1007/S10198-020-01208-6. 2020 21:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olliaro P., Torreele E., Vaillant M. COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room. The Lancet Microbe. 2021;2(7):e279–e280. doi: 10.1016/S2666-5247(21)00069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricotta E.E., Kwan J.L., Smith B.A., Evans N.G. Chronic diseases: Perceptions about Covid-19 risk and vaccination. MedRxiv. 2021;03(17) doi: 10.1101/2021.03.17.21253760. 2021. [DOI] [Google Scholar]
- Rosenstock I.M. The Health Belief Model: Explaining health behavior through expectancies. Health Behavior and Health Education. 1990 [Google Scholar]
- Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/J.VACCINE.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sage Working Group . 2014. Report of the sage working group on vaccine hesitancy. [Google Scholar]
- Sallam M. Vol. 9. 2021. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates; p. 160. (Vaccines 2021). Vol. 9, Page 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.-L. Barriers of Influenza Vaccination Intention and Behavior – A Systematic Review of Influenza Vaccine Hesitancy, 2005 –2016. PLOS ONE. 2017;12(1) doi: 10.1371/JOURNAL.PONE.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahrabani S., Benzion U., Din G.Y. Factors affecting nurses’ decision to get the flu vaccine. The European Journal of Health Economics. 2008;10(2):227–231. doi: 10.1007/S10198-008-0124-3. 2008 10:2. [DOI] [PubMed] [Google Scholar]
- Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H., Rubin G.J., Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Human Vaccines & Immunotherapeutics. 2020;17(6):1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):1–13. doi: 10.1186/S12889-021-10816-7. 2021 21:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.-H., Chen B., Kraemer M.U.G., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O.N., Yang R., Grenfell B.T.…Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/SCIENCE.ABB6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungar L. 2021. The Gender Vaccine Gap: More Women Than Men Are Getting Covid Shots.https://khn.org/news/article/gender-vaccine-gap-more-women-than-men-vaccinated-against-covid/ [Google Scholar]
- Verelst F., Willem L., Beutels P. Behavioural change models for infectious disease transmission: a systematic review (2010–2015) Journal of The Royal Society Interface. 2016;13(125) doi: 10.1098/RSIF.2016.0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., Fang H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines. 2020;8(3):482. doi: 10.3390/VACCINES8030482. 2020, Vol. 8, Page 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M., Wong E.L.Y., Huang J., Cheung A.W.L., Law K., Chong M.K.C., Ng R.W.Y., Lai C.K.C., Boon S.S., Lau J.T.F., Chen Z., Chan P.K.S. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi: 10.1016/J.VACCINE.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2019). Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- World Health Organization . 2021. Weekly epidemiological update - 2 February 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update—2-february-2021. [Google Scholar]
- Zewude B., Habtegiorgis T. Willingness to Take COVID-19 Vaccine Among People Most at Risk of Exposure in Southern Ethiopia. Pragmatic and Observational Research. 2021;12:37–47. doi: 10.2147/POR.S313991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Feng B., Wu Y., Xu P., Ke R., Dong N. The effect of human mobility and control measures on traffic safety during COVID-19 pandemic. PLOS ONE. 2021;16(3) doi: 10.1371/JOURNAL.PONE.0243263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.