Abstract
Background:
Total knee replacement (TKR) and total hip replacement (THR) are two of the most common orthopedic surgical procedures in the United States. These procedures, with fairly low mortality rates, incur significant healthcare costs, with almost 40% of the costs associated with post-acute care. We assessed the impact of general vs. neuraxial anesthesia on discharge destination and 30 day readmissions in patients that underwent total knee and hip replacement in our health system.
Methods:
This was a retrospective cohort study of 24,684 patients undergoing total knee or hip replacement in 13 hospitals of a large healthcare network. Following propensity score matching, we studied the impact of type of anesthetic technique on discharge destination (primary outcome) and post-operative complications including readmissions in 8,613 patients that underwent THR and 13,004 patients for TKR
Results:
Our results showed that in patients undergoing THR and TKR, neuraxial anesthesia is associated with higher odds of being discharged from hospital to home versus other facilities compared to general anesthesia (OR=1.63, 95%CI=1.52, 1.76, p<0.01) and (OR=1.58, 95%CI=1.49, 1.67, p<0.01) respectively.
Conclusions:
Our results suggest an association between use of neuraxial anesthesia for total joint arthroplasty and a higher probability of discharge to home and a reduction in readmissions.
Introduction
Total knee replacement (TKR) and total hip replacement (THR) are two of the most commonly performed orthopedic surgical procedures in the United States with increasing incidence. According to the Centers for Disease Control and Prevention (CDC), 332,000 THRs and 719,000 TKRs were performed in 2010.1,2 As the demand for these procedures is constantly growing with 600,000 THRs and 1.4 million TKRs predicted by 2030, the potential incremental incurred costs are striking. Post-acute care expenses are approximately 40% of primary TKR and THR costs. Healthcare systems are addressing inpatient costs via programs aimed at decreasing hospital length of stay (LOS) for these surgeries. As a trade-off, use of extended care facilities (ECFs) have become more common in the post-acute care period.3 Within both voluntary and mandated bundled care arrangements, however, the providing hospitals and surgeons become responsible for the cost of the 90 days of care after the index procedures, creating an incentive to decrease post-acute care expenses. An improved understanding of the factors that determine a patient’s discharge destination is key to optimize resources and patient satisfaction, speed the resumption of activities of daily living, reduce readmissions, and lead to care processes that are more cost effective.4–7
The anesthetic technique selected for a surgical procedure has been previously shown to impact patients’ ability to meet post-anesthesia care unit (PACU) discharge criteria and influence LOS and, as a result, may influence pain management and rehabilitation goals in the postoperative period, impacting discharge destination.8 In patients with multiple comorbidities undergoing joint replacements, the type of anesthetic approach can have a significant impact on the ability to meet rehabilitation goals and resource utilization for the healthcare system.9,10
In this study, we determined the role of types of anesthetic technique on discharge destinations and investigated secondary outcomes associated with readmissions. We hypothesized that patients who received neuraxial anesthesia would be more likely to go home than to an extended care facilities as compared to those who received general anesthesia. To test our hypothesis, we compared the discharge destinations of patients undergoing THR and TKR following propensity matching within a large, tertiary healthcare system.
Methods
Design:
We performed a retrospective cohort study on data from patients who underwent elective TKR and THR from 2011 to 2014 within UPMC (University of Pittsburgh Medical Center), a single network with 13 hospitals. The requirement for written informed consent was waived by the IRB.
Study Population
Patients were included in the study based on the following ICD-9 CM procedure codes: 81.51 for primary hip and 81.54 for primary knee replacements. Patients undergoing emergency surgery were excluded from the study population.
Data Elements
Data regarding comorbidities, outcomes, and patient and hospital characteristics were collected from each electronic medical record (EMR) and administrative database; see Supplemental Table 1 for the complete list.
Data Management
Institutional Review Board approval was obtained prior to collecting information. Data was stored on secure servers in encrypted files due to the characteristics of the information contained. All identifiers were stripped from the files before exporting information for analysis.
Outcome Variables:
The main outcome was immediate discharge destination after hospital stay, with a binary division of either “Home,” coded in the EMR as home health agency, or home self-care, or “Not Home,” which included leaving against medical advice, death, or transfer to another hospital (short- or long-term), rehabilitation unit, clinical assisted living facility, skilled nursing facility, hospice medical facility, or any other type of facility. Secondary outcome was the 30-day readmission rate, as defined by the ICD-9 codes specified in Supplemental Table 1 and calculated as a binary category.
Independent Variables
The independent variable was the type of anesthesia. The information was retrieved from the EMRs and categorized as either general or neuraxial anesthesia. For the neuraxial anesthesia category, only anesthetics coded as spinal or epidural were considered; patients with codes indicating both general and spinal anesthetics were excluded. See Supplemental Table 2.
Due to the limitations of documentation, it was not possible to reliably identify which patients received peripheral nerve blocks and therefore it was not included in the analysis.
Opioid administration was calculated as total morphine milligram equivalents (MME) that included the total administration of hydromorphone, oxycodone, morphine and fentanyl during the patient hospital stay. We were unable to obtain from the EMR the amount administered to patients that had a patient controlled analgesia (PCA) pump, therefore we did not include it for the calculation of the total MME; this represents a significant confounder and is a study limitation.
Statistical Analysis
All analyses were performed using STATA software V14 (StataCorp LP, College Station, Texas). All tests were two-sided with a significance level of α=0.05.
Modeling Approach:
We built separate logistic regression models for patients undergoing primary THR and TKR. As patients who received neuraxial or general anesthesia were not randomly assigned to their anesthetic technique, we performed propensity score matching to achieve groups with similar characteristics. We developed propensity score models to predict the likelihood of receiving neuraxial or general anesthesia during THR or TKR.
Variables in the propensity score were age, American Society of Anesthesiologists (ASA) physical status classification, sex, comorbidities (hypertension, chronic lung disease, immunocompromise, coronary artery disease [CAD], peripheral artery disease [PAD], hemodialysis, diabetes, previous MI, chronic heart failure 11), patient finance group and hospital.
To estimate the propensity score we used multilevel mixed effects logistic regression with two-level random-intercept model. Posterior modal estimates were used for the estimation of the random effect of Hospital in the calculation of the propensity score.
Variables were tested for collinearity using the variance inflation factor with a cut point >10. Standardized differences and percentage of bias reduction were used to assess the balance of the covariates, using an absolute value of >0.2 for the standardized difference as an indicator of significant residual imbalance.12 We performed 3:1 matching with replacement using the propensity score. For the analysis we used a multilevel mixed-effects logistic regression model accounting for the matched pairs. Standard errors were adjusted so that they were robust to heteroscedasticity and autocorrelation.
We performed two independent secondary analysis, one including body mass index in the model and the second one including the total morphine milligram equivalents received during hospital stay as a mediating variable since the opioid consumption can be directly affected by the anesthetic plan. Opioid consumption can also be a factor when selecting the discharge destination of the patient. Bootstrapping was used for standard error calculation.13–15
The secondary outcome of 30-day readmission was analyzed using similar methods as the primary outcome.
Missing Data:
There were no missing values for the types of anesthesia, comorbidities, or outcomes. BMI was missing on 44.47% of the THR and 47.77% of the TKR. No missing data patterns were identified. Univariate imputation with predictive mean matching was used with 10 imputations. After calculation of the multiple imputation estimates there was no percentage increase in the standard error and no changes on the estimates.
Since BMI was used for a secondary analysis, Figure 1 and Table 1 describe the full database before imputation was performed.
Figure 1:
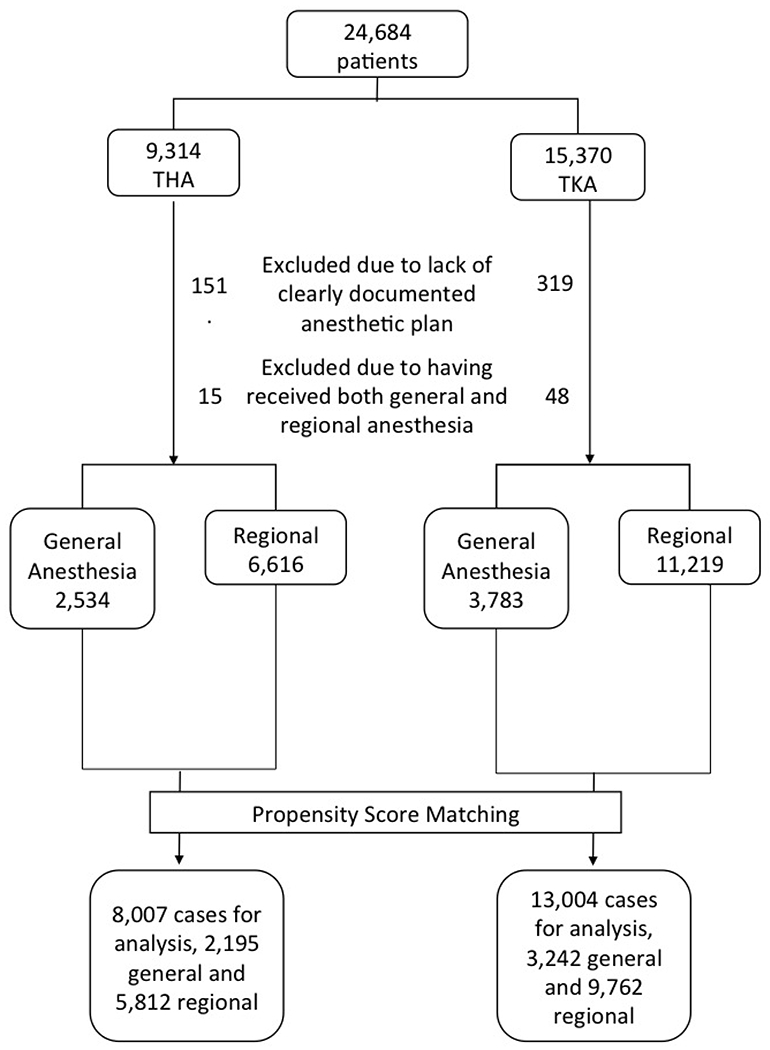
Flowchart of participants from the study included in the final analysis.
Abbreviations: THR, Total hip arthroplasty; TKR, Total knee arthroplasty
Table 1:
Demographics of study population undergoing total hip and knee replacement under general or regional anesthesia
| Characteristics | Knee | Hip | |||||
|---|---|---|---|---|---|---|---|
| General N=3,783 | Regional N=11,219 | p-value | General N=2,534 | Regional N=6,616 | p-valuea | ||
| Age, mean (SD), y | 64.5 (10.5) | 66.0 (9.6) | <0.01 | 64.2 (13.1) | 63.9 (11.5) | 0.42 | |
| Gender, No. (%) | Male | 1,388 (36.7) | 4,308 (38.4) | 0.06 | 1,139 (44.9) | 3,047 (46.1) | 0.34 |
| Female | 2,395 (63.3) | 6,911 (61.6) | 1,395 (55.1) | 3,569 (53.9) | |||
| ASA physical status, No. (%) | 1 | 26 (0.8) | 99 (1.0) | 28 (1.3) | 159 (2.7) | ||
| 2 | 1,193 (36.7) | 4,374 (44.8) | <0.01 | 806 (36.6) | 2,939 (50.5) | <0.01 | |
| 3 | 1,950 (60.0) | 5,169 (52.9) | 1,261 (57.2) | 2,628 (45.1) | |||
| 4 | 72 (2.2) | 119 (1.2) | 100 (4.5) | 84 (1.4) | |||
| Ethnicity, No. (%) | Hispanic or Latino | 4 (0.1) | 15 (0.2) | <0.01 | 3 (0.1) | 6 (0.1) | <0.01 |
| Race, No. (%) | African American | 343 (9.1) | 666 (6.0) | <0.01 | 197 (7.8) | 366 (5.6) | <0.01 |
| White | 3,385 (89.5) | 10,262 (91.7) | 2,299 (90.9) | 5,875 (89.3) | |||
| Hypertension | 2,845 (75.2) | 8,020 (71.5) | <0.01 | 1,795 (70.8) | 4,083 (61.7) | <0.01 | |
| Immunocompromise | 11 (0.3) | 25 (0.2) | 0.46 | 19 (0.7) | 33 (0.5) | 0.15 | |
| Chronic Lung disease | 561 (14.8) | 1,055 (9.4) | <0.01 | 411 (16.2) | 725 (11.0) | <0.01 | |
| Coronary Disease | 796 (21.0) | 1,899 (16.9) | <0.01 | 530 (20.9) | 1,028 (15.5) | <0.01 | |
| Comorbidities, No. (%) | Peripheral Artery Disease | 267 (7.1) | 528 (4.7) | <0.01 | 222 (8.8) | 362 (5.5) | <0.01 |
| Renal Failure on Dialysis | 12 (0.3) | 32 (0.3) | <0.01 | 20 (0.8) | 19 (0.3) | <0.01 | |
| History of VTE | 408 (10.8) | 782 (7.0) | <0.01 | 266 (10.5) | 399 (6.0) | <0.01 | |
| Diabetes Mellitus | 1,018 (26.9) | 2,471 (22.0) | <0.01 | 568 (22.4) | 992 (15.0) | <0.01 | |
| History of Myocardial Infarction | 296 (7.8) | 674 (6.0) | <0.01 | 210 (8.3) | 376 (5.7) | <0.01 | |
| Chronic Heart Failure | 310 (8.2) | 599 (5.3) | <0.01 | 272 (10.7) | 395 (6.0) | <0.01 | |
p-values for comparison of the demographic characteristics between patients that received general anesthesia and regional anesthesia. Data are shown as mean (SD) for continuous variables and No (%) for categorical variables.
Equator guidelines:
This manuscript adheres to the applicable STROBE guidelines.
Results
Patient Characteristics
The study population included 9,314 THR and 15,370 TKR patients. From those, we excluded patients lacking clear documentation of an anesthetic plan or who received both general and neuraxial anesthesia, as depicted in Figure 1.
After exclusion, from the 9,150 patients undergoing THR, 6,616 (72.3%) were performed under neuraxial anesthesia and 2,534 (27.6%) under general anesthesia. For the TKRs, 11,219 were performed under neuraxial anesthesia and 3,783 under general anesthesia.
The caseload per hospital ranged from as low as 23 up to 3,601, and most of the procedures were performed in urban hospital settings (94%), with more than 90% of population being white and less than 1% of Hispanic or Latino.16
The entire cohort before propensity score matching was 59.1% women (n=14,270); average age at the time of surgery was 65.0 ± 10.8 years, and average BMI was 31.26 ± 7.12 kg/m2. The most commonly reported comorbidities were hypertension in 69.3% and diabetes in 20.9%. (See Table 1 for basic demographics and comorbidities).
Of the 24,684 patients included across 13 hospitals, 17,266 (71.49%) were discharged to home, which was defined as home self-care or home health agency. The average LOS for TKR cases was 3.28 days, and 3.07 days for THR cases. The 30-day readmission rate was 3.6% of the entire cohort.
Matching
After 3:1 matching with replacement, a balanced cohort was created between the neuraxial (THR: 6,293 cases, TKR: 9,162 cases) and general anesthesia (THR: 2,320 cases, TKR: 3,242 cases) groups. No significant differences were found between groups on the matching variable (age, ASA classification, sex, comorbidities [hypertension, chronic lung disease, immunocompromise, CAD, PAD, hemodialysis, diabetes, previous MI, CHF], patient finance group, and hospital), mitigating any possible confounding variables between the cohorts in our work. Figure 2 presents changes in standardized difference of the variables before and after the propensity score matching.
Figure 2:
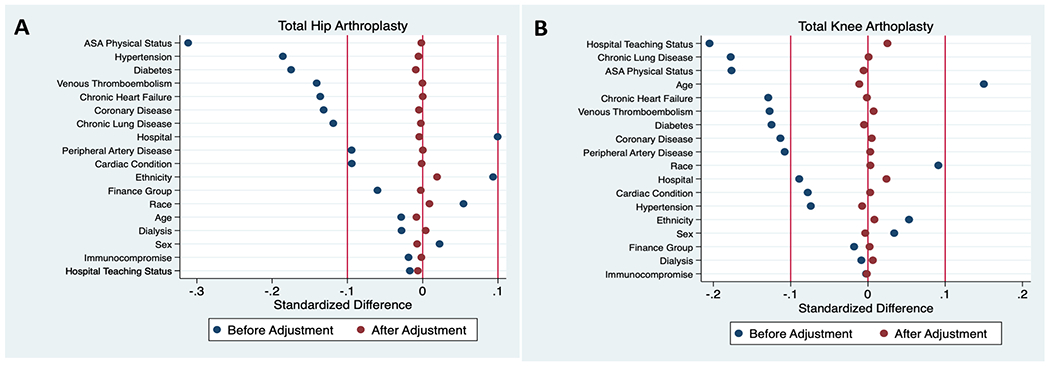
Comparison of the distribution of baseline covariates between groups before and after propensity-score adjustment.
A. Patients that received primary total hip replacement.
B. Patients that received primary total knee replacement
Abbreviations: ASA, American Society of Anesthesiologists
Hip Replacement
After propensity score matching our results showed that neuraxial anesthesia is associated with higher odds of discharge to home compared to general anesthesia for patients that had a THR (OR=1.63, 95%CI=1.52, 1.76, p<0.01) (Figure 3).
Figure 3:
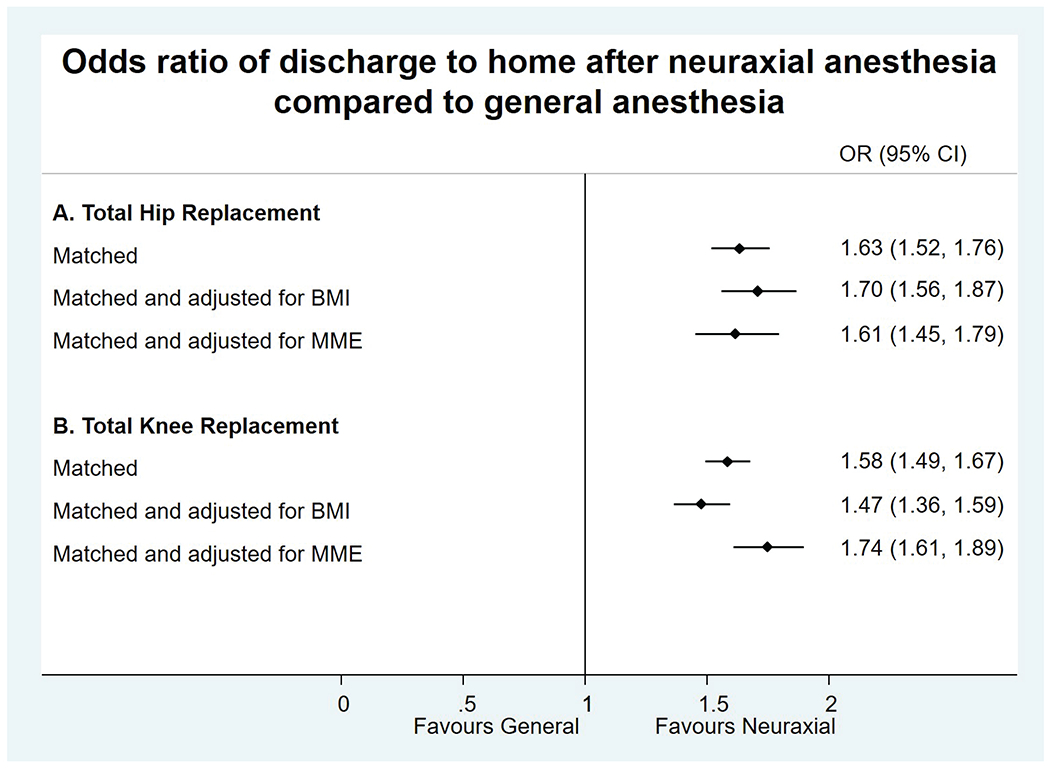
Measurement of primary outcome: Discharge to home with self-care or home health, data is presented in OR (95% CI).
A. Patients that received primary total hip replacement
B. Patients that received primary total knee replacement
Abbreviations: OR, Odds Ratio; CI, Confidence interval; ASA, American Society of Anesthesiologists
After secondary analysis adjusting for the effect of BMI, neuraxial anesthesia was still associated with higher odds of home discharge compared to general anesthesia (OR=1.70, 95% CI=1.56, 1.87, p<0.01).
The estimated proportion of the total effect of neuraxial anesthesia on discharge destination mediated by total MME consumption was 8.3% (95% CI=7.3%, 9.4%)
Knee Replacement
After propensity score matching our results showed that neuraxial anesthesia is associated with higher odds of discharge to home compared to general anesthesia for patients that had a TKR (OR=1.58, 95% CI=1.49, 1.67, p<0.01) (Figure 3).
After secondary analysis adjusting for the effect of BMI, neuraxial anesthesia was still associated with higher odds of home discharge compared to general anesthesia (OR=1.47, 95% CI=1.36, 1.59, p<0.01).
The estimated proportion of the total effect of neuraxial anesthesia on discharge destination mediated by total MME consumption was 7% (95% CI=6.4%, 8.5%)
Secondary Outcome
We included 30-day readmission as an outcome, finding a significant association between neuraxial anesthesia and decreased odds of readmission during the first 30 days after surgery for both hip and knee replacements, (OR=0.55, 95% CI=0.47, 0.65, p<0.01) and (OR=0.69, 95% CI=0.61, 0.79, p<0.01) respectively (Figure 4).
Figure 4:
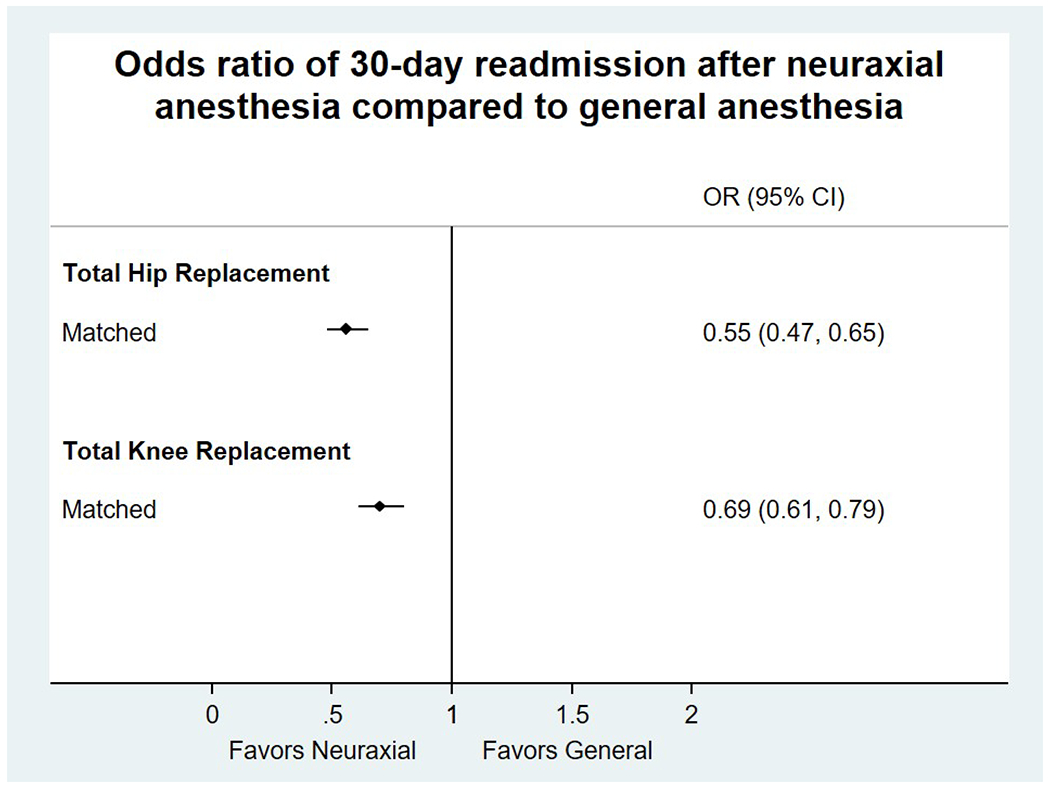
Measurement of secondary outcome: 30-day readmission, data is presented in OR (95% CI).
Abbreviations: OR, Odds Ratio; CI, Confidence interval
Discussion
In the present work from a large, multi-hospital healthcare system, neuraxial anesthesia was associated with increased odds of being discharged to home following elective THR and TKR procedures and decreased 30-day readmission rates when compared to general anesthesia.
THR is a cost-effective treatment for improving functional outcomes and remains one of the most commonly performed elective surgical procedures worldwide, with estimates of between 277,000 and 562,000 cases annually in the United States by 2030.17 Post-acute care and readmissions in the first 90 days represent a significant financial burden to healthcare systems and compromise ~40% of primary THR and TKR costs, making discharge destination to home one of the desired goals.18,19 For example, home discharge and outpatient rehabilitation saves between $4,700-15,000 compared to discharging the same patient to an inpatient rehabilitation facility.6,20,21 Interestingly, Global Orthopaedic Registry showed that after THR in the United States, 53% of patients are discharged to an inpatient rehabilitation facility compared with 81% in Japan and only 3%-6% in the UK.22,23 Such variations in the post-acute care for a procedure with relatively reproducible outcomes suggests that algorithms featuring scalable positive impact on post-acute care could optimize patient outcomes and costs. Therefore primary THR and TKR are popular targets for fixed-cost, pay-for-performance programs such as bundled payments.24 The comprehensive care for joint replacement (CJR) model introduced by Medicare led to decreased LOS and increased discharge to home, with decreasing readmission rates and cost-savings without compromising the quality of care.25 The CJR includes all preoperative, acute, and post–acute care up to 90 days after surgery.26 In the acute setting, reducing a patient’s LOS, reducing implant costs, and eliminating unnecessary testing have been primary drivers for cost reduction.27
Bini et al. showed that of 9,150 primary TJA patients, those discharged to a SNF had significantly higher readmission rates (5.2% vs. 2.4%, p=0.001) compared to those discharged home, similar to our findings of 6.24% vs. 2.56% 30-day readmission rates among patients discharged to a different facility vs. those that went home.28 Discharge to a SNF and associated higher readmission rates may be due to more frail patients being discharged to a SNF. However, Bini et al. found an OR for 90-day readmission of 1.6-1.9 in healthy patients discharged to a SNF when controlling for age, sex, and ASA classification making home discharge a desirable goal.28
Multiple studies have identified age, female gender, Medicare insurance, living alone, obesity, heart failure, ASA classification of 3/4, longer LOS, hospital volume, and post-operative pain as risk factors for non-home discharge for primary TJA.29–31 Beyond these, our study identified that neuraxial anesthesia was associated with increased likelihood of home discharge destination. Previous studies also found payer status, race, sex, medical comorbidities, discharge disposition, and LOS to be independently associated with 30-day readmission.28,32 Many prior studies evaluated short-term outcomes such as DVT, PE, estimated blood loss, and transfusion requirement, suggesting better outcomes for patients receiving neuraxial compared to general anesthesia.33–35 Evaluation of long-term outcomes is needed to assess the comparative effectiveness of anesthetic techniques beyond the hospitalization.36
In our cohort, patients receiving neuraxial anesthesia for both THR and TKR had significantly lower 30-day readmission rates after controlling for age, ASA classification, sex, comorbidities (hypertension, chronic lung disease, immunocompromise, CAD, PAD, hemodialysis, diabetes, previous MI, CHF), patient finance group, and hospital. Also, among patients in both neuraxial as well as general anesthesia groups, the ones who went home after discharge had lower readmission rates. While our data was not granular to identify the causes for readmissions, from recent literature, the top five causes of 30-day readmission include superficial surgical site infection (SSI; 9.7%), non-SSI infection (9.5%), cardiovascular complications (CV; 9.3%), gastrointestinal complications (8.8%), and venous thromboembolisms (8.8%).37
We believe that our results support growing evidence that agrees with the advantages of neuraxial anesthesia compared to general anesthesia. The main outcome of home vs. non-home discharge has scalable systems-level implications impacting not only on patient outcomes, but also resource utilization, cost-effectiveness, value-based care, and patient satisfaction.
Limitations
Our retrospective study has several limitations. Given the larger sample size, reviewing every medical note for every patient for comorbidities and complications was not feasible, so we evaluated the ICD-9 codes reported in the EMR for the comorbidities and complications during the hospitalization. It remains impossible to control all variables influencing the decision-making process between the anesthesiologist and patient, receiving general anesthesia could be a marker of presence of other comorbidities not reported with ICD-9 codes on the EMR or coagulation dysfunction, which could also affect discharge destination and were unable to be measured in this study.
Second, within the home cohort, we were unable to distinguish between home self-managed patients vs. those discharged home with home health services. It is likely, however, that most patients who go home after TJA will receive some home health services. Third, our work covers the pre-CJR era of 2015, which likely influenced practice patterns nationwide.
In our system, nerve blocks are documented as a clinical note and are not part of the anesthesia record, therefore any documentation of nerve blocks on the anesthesia record grossly underestimates the prevalence of nerve blocks in all groups, we recognize this as a mayor limitation since peripheral nerve blocks themselves could be considered as confounders when attempting to zero in on operating room anesthetic effects on discharge disposition and may limit the generalization of the results.
We also encountered limitations when evaluating opioid administration, we were unable to retrieve the amount administered through the PCA pumps from our medical records, although we were able to identify which patients had one, we decided against including it in the analysis since PCA as a categorical variable has minimal clinical significance compared to the amount of medications being administered.
As with any retrospective study, the possibility of bias and confounding factors cannot be ignored. Even with rigorous propensity score adjustment, additional unmeasured factors such as socioeconomic status, baseline functional level, and home/community factors likely influence discharge disposition after TJA.38.
Despite being a single network study, we included 13 different hospitals with patients from different insurance status, multiple providers for surgical and anesthetic team which could allow our results to be generalized to a broad population, however the association between neuraxial anesthesia and home discharge may not have as strong an effect on a younger healthier population since most of our patients had multiple comorbidities, were on average above 60 years old and most of them were overweight.
In addition, most of our procedures were performed in urban hospital settings that could limit the generalizability to rural areas and this data also might not extrapolate non-Caucasian patients since 90% of our population was Caucasian.
Supplementary Material
Key Points:
Question:
Is neuraxial anesthesia associated with patient disposition after hospital discharge?
Findings:
Patients have a higher likelihood of going home after THR and TKR under neuraxial anesthesia as compared to general anesthesia.
Meaning:
As post-acute care costs compromise ~40% of primary THR and TKR and emphasis is on value-based healthcare delivery, discharge destination to home becomes a desired goal and neuraxial anesthesia plays a crucial role.
Acknowledgments
Financial disclosures: M.D., A.J.Y., A. Monahan, and S.W. are supported by departmental funding, M.P.S., A. Mahajan, and A.M.K. are supported by departmental funding and NIH.
Glossary of Terms:
- TKR
Total knee replacement
- THR
total hip replacement
- CDC
Centers for Disease Control and Prevention
- ECFs
extended care facilities
- LOS
length of stay
- UPMC
University of Pittsburgh Medical Center
- EMR
electronic medical record
- ASA
American Society of Anesthesiologists
- CAD
coronary artery disease
- PAD
peripheral artery disease
- MI
hemodialysis, diabetes, previous
- CHF
chronic heart failure
- BMI
Body Mass Index
- OR
odds ratio
- TJA
total joint arthroplasty
- CJR
care for joint replacement
- SNF
skilled nursing facility
- HRRP
Hospital Readmissions Reduction Program
- SSI
surgical site infection
- CV
cardiovascular
- MME
morphine milligram equivalents
- PCA
patient controlled analgesia
Footnotes
Conflicts of interest: None
References
- 1.Hospitalization for Total Hip Replacement Among Inpatients Aged 45 and Over: United States, 2000–2010. Centers for Disease Control and Prevention; 2015.
- 2.Hospitalization for Total Knee Replacement Among Inpatients Aged 45 and Over: United States, 2000–2010. Centers for Disease Control and Prevention; 2015.
- 3.Tarity TD, Swall MM. Current Trends in Discharge Disposition and Post-discharge Care After Total Joint Arthroplasty. Curr Rev Musculoskelet Med. 2017;10(3):397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keswani A, Tasi MC, Fields A, Lovy AJ, Moucha CS, Bozic KJ. Discharge Destination After Total Joint Arthroplasty: An Analysis of Postdischarge Outcomes, Placement Risk Factors, and Recent Trends. The Journal of arthroplasty. 2016;31(6):1155–1162. [DOI] [PubMed] [Google Scholar]
- 5.Barsoum WK, Murray TG, Klika AK, et al. Predicting patient discharge disposition after total joint arthroplasty in the United States. The Journal of arthroplasty. 2010;25(6):885–892. [DOI] [PubMed] [Google Scholar]
- 6.Sigurdsson E, Siggeirsdottir K, Jonsson H Jr., Gudnason V, Matthiasson T, Jonsson BY. Early discharge and home intervention reduces unit costs after total hip replacement: results of a cost analysis in a randomized study. Int J Health Care Finance Econ. 2008;8(3):181–192. [DOI] [PubMed] [Google Scholar]
- 7.Keswani A, Weiser MC, Shin J, Lovy AJ, Moucha CS. Discharge Destination After Revision Total Joint Arthroplasty: An Analysis of Postdischarge Outcomes and Placement Risk Factors. The Journal of arthroplasty. 2016;31(9):1866–1872 e1861. [DOI] [PubMed] [Google Scholar]
- 8.Ilfeld BM, Ball ST, Gearen PF, et al. Ambulatory continuous posterior lumbar plexus nerve blocks after hip arthroplasty: a dual-center, randomized, triple-masked, placebo-controlled trial. Anesthesiology. 2008;109(3):491–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117(1):72–92. [DOI] [PubMed] [Google Scholar]
- 10.Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472(1):188–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chambers JC, Zhang W, Sehmi J, et al. Genome-wide association study identifies loci influencing concentrations of liver enzymes in plasma. Nature genetics. 2011;43(11):1131–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang D, Dalton J. A unified approach to measuring the effect size between two groups using SAS. Paper presented at: SAS Global Forum2012. [Google Scholar]
- 13.Krull JL, MacKinnon DP. Multilevel Modeling of Individual and Group Level Mediated Effects. Multivariate Behav Res. 2001;36(2):249–277. [DOI] [PubMed] [Google Scholar]
- 14.Mascha EJ, Dalton JE, Kurz A, Saager L. Statistical grand rounds: understanding the mechanism: mediation analysis in randomized and nonrandomized studies. Anesthesia and analgesia. 2013;117(4):980–994. [DOI] [PubMed] [Google Scholar]
- 15.Zhang Z, Zyphur MJ, Preacher KJ. Testing Multilevel Mediation Using Hierarchical Linear Models Problems and Solutions. Organ Res Methods. 2009;12(4):695–719. [Google Scholar]
- 16.Hall MJ, Owings M. Rural and urban hospitals’ role in providing inpatient care, 2010. NCHS Data Brief. 2014(147):1–8. [PubMed] [Google Scholar]
- 17.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. The Journal of bone and joint surgery American volume. 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 18.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. [DOI] [PubMed] [Google Scholar]
- 19.Snow R, Granata J, Ruhil AV, Vogel K, McShane M, Wasielewski R. Associations between preoperative physical therapy and post-acute care utilization patterns and cost in total joint replacement. The Journal of bone and joint surgery American volume. 2014;96(19):e165. [DOI] [PubMed] [Google Scholar]
- 20.Ramos NL, Wang EL, Karia RJ, Hutzler LH, Lajam CM, Bosco JA. Correlation between physician specific discharge costs, LOS, and 30-day readmission rates: an analysis of 1,831 cases. The Journal of arthroplasty. 2014;29(9):1717–1722. [DOI] [PubMed] [Google Scholar]
- 21.Slover JD, Mullaly KA, Payne A, Iorio R, Bosco J. What is the Best Strategy to Minimize After-Care Costs for Total Joint Arthroplasty in a Bundled Payment Environment? The Journal of arthroplasty. 2016;31(12):2710–2713. [DOI] [PubMed] [Google Scholar]
- 22.Waddell J, Johnson K, Hein W, Raabe J, FitzGerald G, Turibio F. Orthopaedic practice in total hip arthroplasty and total knee arthroplasty: results from the Global Orthopaedic Registry (GLORY). Am J Orthop (Belle Mead NJ). 2010;39(9 Suppl):5–13. [PubMed] [Google Scholar]
- 23.Hayes JH, Cleary R, Gillespie WJ, Pinder IM, Sher JL. Are clinical and patient assessed outcomes affected by reducing length of hospital stay for total hip arthroplasty? The Journal of arthroplasty. 2000;15(4):448–452. [DOI] [PubMed] [Google Scholar]
- 24.Sood N, Huckfeldt PJ, Escarce JJ, Grabowski DC, Newhouse JP. Medicare’s bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood). 2011;30(9):1708–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Navathe AS, Troxel AB, Liao JM, et al. Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med. 2017;177(2):214–222. [DOI] [PubMed] [Google Scholar]
- 26.Clement RC, Gray CM, Kheir MM, et al. Will Medicare Readmission Penalties Motivate Hospitals to Reduce Arthroplasty Readmissions? The Journal of arthroplasty. 2017;32(3):709–713. [DOI] [PubMed] [Google Scholar]
- 27.Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. The Journal of bone and joint surgery American volume. 2002;84-A(3):348–353. [DOI] [PubMed] [Google Scholar]
- 28.Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? The Journal of arthroplasty. 2010;25(1):114–117. [DOI] [PubMed] [Google Scholar]
- 29.de Pablo P, Losina E, Phillips CB, et al. Determinants of discharge destination following elective total hip replacement. Arthritis and rheumatism. 2004;51(6):1009–1017. [DOI] [PubMed] [Google Scholar]
- 30.Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Which Hospital and Clinical Factors Drive 30- and 90-Day Readmission After TKA? The Journal of arthroplasty. 2016;31(10):2099–2107. [DOI] [PubMed] [Google Scholar]
- 31.Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Hospital, Patient, and Clinical Factors Influence 30- and 90-Day Readmission After Primary Total Hip Arthroplasty. The Journal of arthroplasty. 2016;31(10):2130–2138. [DOI] [PubMed] [Google Scholar]
- 32.Clement RC, Derman PB, Graham DS, et al. Risk factors, causes, and the economic implications of unplanned readmissions following total hip arthroplasty. The Journal of arthroplasty. 2013;28(8 Suppl):7–10. [DOI] [PubMed] [Google Scholar]
- 33.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. The Journal of bone and joint surgery American volume. 2013;95(3):193–199. [DOI] [PubMed] [Google Scholar]
- 34.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesthesia and analgesia. 2006;103(4):1018–1025. [DOI] [PubMed] [Google Scholar]
- 35.Johnson RL, Kopp SL, Burkle CM, et al. Neuraxial vs general anaesthesia for total hip and total knee arthroplasty: a systematic review of comparative-effectiveness research. Br J Anaesth. 2016;116(2):163–176. [DOI] [PubMed] [Google Scholar]
- 36.Perlas A, Chan VW, Beattie S. Anesthesia Technique and Mortality after Total Hip or Knee Arthroplasty: A Retrospective, Propensity Score-matched Cohort Study. Anesthesiology. 2016;125(4):724–731. [DOI] [PubMed] [Google Scholar]
- 37.Curtis GL, Jawad M, Samuel LT, et al. Incidence, Causes, and Timing of 30-Day Readmission Following Total Knee Arthroplasty. The Journal of arthroplasty. 2019. [DOI] [PubMed] [Google Scholar]
- 38.Inneh IA, Clair AJ, Slover JD, Iorio R. Disparities in Discharge Destination After Lower Extremity Joint Arthroplasty: Analysis of 7924 Patients in an Urban Setting. The Journal of arthroplasty. 2016;31(12):2700–2704. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


