Abstract
Background and Objective.
Low-income populations are more likely to experience food and nutrition insecurity and suffer a greater burden of non-communicable disease than the general population. The UnProcessed Pantry Project (UP3) is an intervention aimed to reduce ultra-processed food availability and consumption of food pantry clients accessing the emergency food system.
Methods.
The pilot study included nutrition education, food boxes, and social support for 16-weeks at two food pantries. Data collection included the ASA24 dietary recall to calculate Healthy Eating Index-2015 (HEI-2015) scores, biomarkers (hemoglobin A1C, total cholesterol, blood pressure, waist circumference, BMI), and a demographic and psychosocial survey.
Results.
Dietary quality among 43 participants significantly (p<0.05) improved as measured by the HEI-2015 for total HEI-2015, whole grains, total protein foods, and added sugars scores. BMI, total cholesterol, and waist circumference also significantly improved across study participants.
Conclusions.
Findings indicate that the emergency food system may be an effective access point to apply frameworks including UP3 to address ultra-processed food consumption, dietary quality, and non-communicable chronic disease risk among food insecure populations. Programs and policies that limit the amount of ultra-processed food in the emergency food system should be further tested and could be efficacious in addressing disparities among vulnerable populations.
Keywords: ultra-processed food, chronic disease, diet quality, food security, nutrition security
Introduction
Worldwide, poor diets are now responsible for more non-communicable disease (NCD) and premature death than all other risk factors.1,2 Evidence suggests that there is a relationship between the development of NCD and the consumption of ultra-processed food (UPF) across populations.3–5 UPFs, coined by the NOVA (not an acronym) classification system, is a class of food products that are usually industrially formulated and packaged, high in caloric sweeteners, salt, saturated fat, and energy, and manipulated with artificial ingredients.
UPF is increasing in prevalence and dominates the global food supply as a part of the nutrition transition where, as countries become more industrialized, traditional diets shift more calories from sugar, saturated fat, and processed food.1,2,6 It is challenging to achieve a healthy diet in the face of UPFs that are heavily marketed, hyper-palatable, energy-dense, convenient, and inexpensive.6–10 In the US, 71% of the packaged food supply is ultra-processed, while over 60% of calories consumed by Americans are ultra-processed.11,12
Notably, a disparity exists for low-income populations in the United States (US), who are more likely to consume UPF, experience food and nutrition insecurity, and suffer a greater burden of NCD than the general population (Figure 1).13–18 In the US, healthy diets cost more in money and time than energy-dense diets that include UPFs.15,16 Food and nutrition insecurity herein addresses both quantity (enough food) and quality (nutritious food) and is defined and measured as “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways.”19
Figure 1.
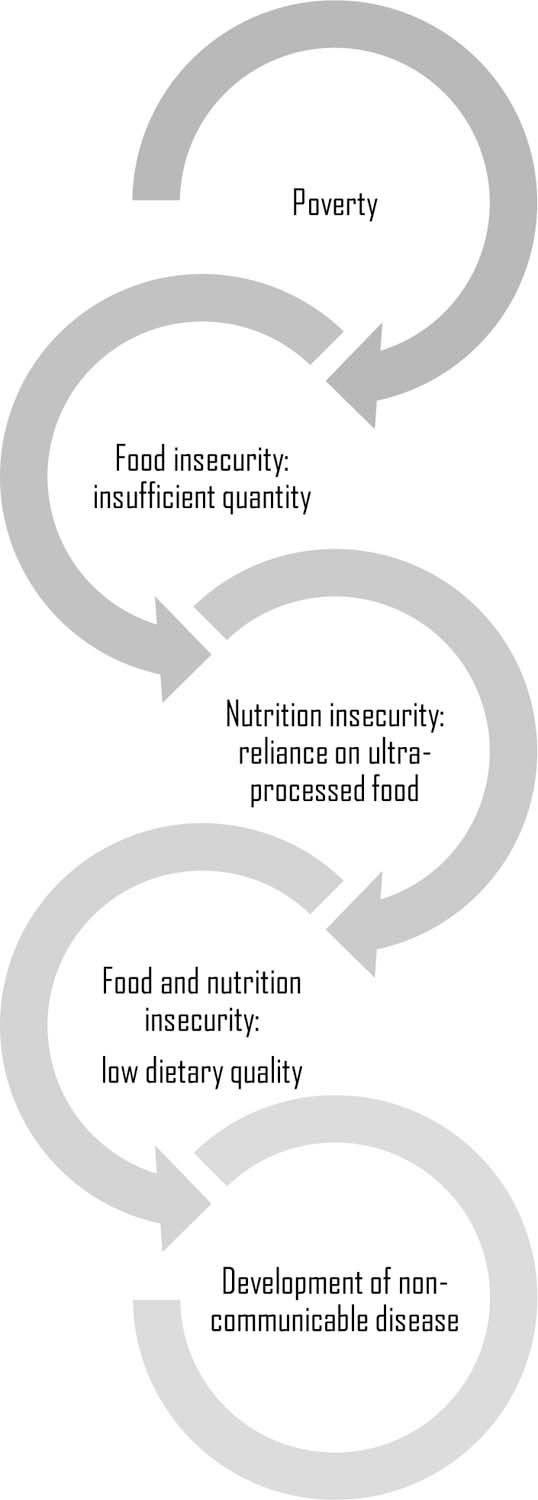
Causes and Consequences of Ultra-Processed Food Consumption Among Food and Nutrition Insecure Individuals in the United States
Systemic inequities drive food and nutrition insecurity. Low-income households below 185% are most likely to be food insecure. Non-Hispanic Black, Hispanic, and single women with children are more likely to experience food insecurity than other demographic groups. Households with grandchildren, a disabled parent or child, a previously incarcerated adult, an adult smoker, or in a rural area or more likely to be food insecure in the US. The ability to afford and acquire sufficient food is not equivalent for all. Significant differences between groups highlight a lack of equity that leads to health disparities among food insecure populations.
Food insecure households in the US utilize the emergency food system, usually through food pantries, to support their food needs.20 The emergency food system supports over 40 million food insecure individuals and is a key pathway to address dietary intake of UPFs and the adverse impact on health outcomes frequently experienced by low-income populations.20–22 Findings across studies suggest food banks and food pantries tend to rely primarily on non-perishable food, characterized as shelf-stable, easy to store, and requiring less infrastructure to meet the immediate food deprivation needs of clients, and typically have a limited capacity to provide perishable, nutrient-dense food.22–27 UPF falls within the non-perishable category of foods. Importantly, the food supply itself is not uniform at many food pantries, resulting in an inconsistent quality of available foods and wide variability in clients’ access to nutritious foods.
Diet quality of food pantry clients has been generally low when compared to dietary recommendations, especially for fruits, vegetables, or dairy products.22–28 Although food pantry interventions have typically focused on enhancing nutrition knowledge, attitudes, skills, and behaviors of clients or the food environment, studies have not adequately addressed UPF, were short in duration, and commonly rely on survey questions only to assess outcomes.29–31
The UnProcessed Pantry Project (UP3) is a 16-week pilot study designed to reduce health disparities faced by food insecure clients. The short-term goal of this research was to test an innovative intervention suitable for the emergency food system to reduce UPF availability and consumption. To our knowledge, this is the first intervention to directly address UPF in a specific population or within the emergency food system.
UP3 Intervention Development
A UP3 Toolkit was developed with a Community Advisory Board (CAB) of professionals focused in response to an identified need for a coordinated intervention to support food insecure individuals at risk for chronic disease development to access nutritious foods. The CAB consisted of representatives from two food pantries, a hospital, a health department, Registered Dietitians, researchers, and students. The CAB developed the UP3 Toolkit from previously tested strategies with strong evidence for success with two main components: the UP3 Framework to guide food choices21 and tools for facilitating dietary change among clients at any food pantry. The UP3 Framework was created to guide food pantry staff and clients to choose nutritious foods based upon two categories, unprocessed or ultra-processed. The UP3 Toolkit tools (curriculum, food supply, intervention measures) were developed to influence the interconnected systems at the food pantry to provide more unprocessed food in the food supply and for the individual. Supplement A describes the intervention development in detail.
Methods
The 16-week UP3 pilot study provided a framework for participants to limit UPF consumption, by providing each participant with nutritious food choices from the food pantry, nutrition education, and social support. The pilot study was conducted among 43 participants using a single group design with no control group at two food pantries. The Montana State University Institutional Review Board approved this study under expedited review.
Participants
The UP3 intervention was conducted at two rural food pantries that applied a self-select shopping model with clients between March and June of 2019. The food pantries were selected to participate in the intervention because their staff and directors were involved in the development of UP3 from the onset. To guarantee the availability of nutritious choices at the two sites, the UP3 team worked with the sites to implement the UP3 Toolkit. The two food pantries collectively served almost 4,000 individuals monthly and were in locations classified as rural.33
In January and February 2019, potential participants were recruited through flyers, during their normal intake process at the food pantry, and through the local health department in partnership with a federally qualified health center. A screening survey was used to determine eligibility. Participants were eligible to participate in the study if they were at least 18 years old, had no food allergies, were not pregnant, able to attend scheduled UP3 appointments once per week for 16 weeks, and currently at risk for, or previously had, a chronic condition assessed by if their doctor had ever indicated risk for a chronic disease or scored 5 or higher on the CDC Prediabetes Risk Test.34 Eligible participants were invited to join the study by telephone and, if interested, asked to attend an introductory meeting to complete informed consent. Following informed consent, participants met with a Registered Dietitian and research staff to receive the intervention protocol and undergo baseline research measures. To understand confounders, participants were asked if they currently followed other diets for weight loss and not to continue or begin a new diet regimen during the study periods.
UP3 Intervention
Every week, participants obtained unprocessed food at the food pantry according to a UP3 Shopping List, with the quantity of food created according to the Dietary Guidelines for Americans35 to include food groups and serving sizes for 50% of the household diet. To increase the number of perishable foods that participants regularly accessed, the study included weekly food pickups versus the standard monthly pickups typical at the food pantries. Study staff guided participants choices the first six weeks of the intervention and, following, were available to assist with questions about food selection and preparation while participants shopped.
Every other week, participants attended group (6–8 participants) experiential nutrition education sessions led by Registered Dietitian Nutritionists and trained staff that lasted 20 to 30 minutes. The participatory nutrition education targeted knowledge, attitudes, and perceptions about increasing unprocessed food intake and decreasing UPF intake.
To provide individualized social support, participants met one-on-one with a member of the research team for a check-in about the UP3 intervention on weeks when experiential nutrition education was not conducted, on 6 occasions per participant for a total of approximately 1.5 hours. Participants were compensated to offset costs incurred for their time spent the intervention. Supplement A describes the intervention implementation in detail.
Measures
Dietary quality, the primary outcome, was assessed using the ASA24 (Automated-Self Administered Recall System) version 2018, developed by the National Cancer Institute (Bethesda, Maryland, USA).37 ASA24 output can be used to assess dietary quality to calculate the Healthy Eating Index-2015 score.38
Health biomarkers, including Hemoglobin A1c (HbA1c), total cholesterol, blood pressure, waist circumference, and height and weight to assess BMI, were collected at 0, 5, and 15 weeks to evaluate the effects of UP3 and the feasibility of collecting these measures during a dietary intervention in a food pantry setting. Participants received a printout of their results and discussed health improvements and concerns with trained research staff. A protocol was developed to refer participants to local health care providers if necessary. See Supplement B for a detailed description of health measures.
Participant demographic and socioeconomic information was assessed via survey. Food security status was assessed using a validated 2-item scale.39,40 The psychometrically tested FRESH Foods Survey was also used to estimate weekly intake of energy-rich and nutrient-rich foods.41,42 Perceptions about fruits and vegetable consumption, engagement in food practices, and number of dinners at home were also assessed.
Interviews were conducted with participants by asking target questions about intervention comprehension and satisfaction at 4 “check-in” timepoints during the intervention (weeks 3, 8, 12, 16). Check-ins asked participants for specific feedback about intervention components (food distribution, nutrition education, support), noticeable changes in their health, and challenges and successes of following an unprocessed diet.
A 6-month follow-up was conducted by phone for exploratory purposes about the longer-term impact of the UP3 intervention on participants’ dietary patterns and health. The follow-up included multiple-choice questions regarding barriers to eating unprocessed food and the two aforementioned food security questions. Open-ended questions asked about noticeable changes in dietary habits and health and overall recommendations about intervention components. Supplement A describes the intervention measures in detail.
Analysis
Data was analyzed using IBM SPSS (version 19.9, Armonk, NY: IBM Corp.). Descriptive statistics were calculated to quantitatively describe the population’s demographics and socioeconomic characteristics. Descriptive analyses of baseline data used data from all enrolled subjects. One-way analysis of variance (ANOVA) was used to test whether mean change in outcome measures differed by baseline categorical variables, separately for change from baseline to midpoint and change from baseline to endpoint. Pearson correlation coefficients were calculated to test the association between change in outcomes and continuous baseline variables. Paired t-tests were used to test whether the outcome measures changed from baseline to midpoint and baseline to endpoint. Analyses of change in outcomes were complete-case analyses, using only cases that have both baseline and follow-up data at each time point. Qualitative process evaluation data was coded using thematic analysis for common themes across participants.43,44
Results
Retention and Dosage
For the screening period, 96 individuals completed surveys to assess their eligibility to participate in the study and 59 were eligible based upon inclusion and exclusion criteria. At food pantry A, 25 participants were enrolled. At food pantry B, 18 participants were enrolled. In total, 43 participants initially enrolled in the study and completed baseline measures, 40 (93%) participants completed measures at 5 weeks, and 37 (86%) completed measures at 15 weeks. At 15 weeks, 2 participants were unable to attend the outcomes data collection but did participate in the entire intervention. Other participants dropped late in the intervention because of moving to another town (n=2) or personal emergencies that prevented participation (n=2). No significant differences in demographic variables were detected between food pantries or those that dropped out of the intervention and those that remained in the intervention.
Demographic and socioeconomic characteristics of enrolled participants that completed pre and post measures are in Table 1. Participants were mostly female (78.4%), with a mean age of 46.9 (±14.3), approximately half were employed, a majority had a high school degree or less (40.5%), and 75.6% earned less than 25K per year.
Table 1.
Baseline Demographic Characteristics of Participants that Completeda All Measures during the UnProcessed Pantry Project, 2019 (n=37)
| Category | All Participants | Site A | Site B |
|---|---|---|---|
| N(%) | |||
| Gender | |||
| Female | 29(78.4) | 15(71.4) | 14(87.5) |
| Male | 8(21.6) | 6(28.6) | 2(12.5) |
| Other | 0(0.0) | 0(0.0) | 0(0.0) |
|
Age
(Mean Age 46.9 ± 14.4) |
|||
| 20–29 | 6(16.2) | 3(14.3) | 3(18.8) |
| 30–39 | 5(13.5) | 3(14.3) | 2(12.5) |
| 40–49 | 9(24.3) | 4(19.0) | 5(31.3) |
| 50–59 | 11(29.7) | 9(42.9) | 2(12.5) |
| 60+ | 6(16.2) | 2(9.5) | 4(25.0) |
| Education | |||
| High school or less | 15(40.5) | 7(33.3) | 8(50.0) |
| Some college | 13(35.1) | 8(38.1) | 5(31.3) |
| 2 or 4 year degree | 8(21.6) | 5(23.8) | 3(18.8) |
| Prefer not to answer | 1(2.7) | 1(4.8) | 0(0.0) |
| Annual Household Income | |||
| Less than 5,001K | 3(8.1) | 2(9.5) | 1(6.3) |
| 5,001K-15K | 13(35.1) | 8(38.1) | 5(31.3) |
| 15,001K-25K | 12(32.4) | 6(28.6) | 6(37.5) |
| 25,001K-35K | 6(16.2) | 4(19.0) | 2(12.5) |
| 35,001K-45K | 2(5.4) | 1(4.8) | 1(6.3) |
| 45,001K-50K | 0(0.0) | 0(0.0) | 0(0.0) |
| More than 50K | 1(2.7) | 0(0.0) | 1(6.3) |
| Employment Status | |||
| Not employed; not looking for work | 3(8.1) | 1(4.8) | 2(12.5) |
| Not employed, but looking for a job | 7(18.9) | 4(19.0) | 3(18.8) |
| Retired, disabled, full time homemaker/stay-at-home parent, or full-time student | 7(18.9) | 4(19.0) | 3(18.8) |
| Employed in a temporary or seasonal job | 1(2.7) | 0(0.0) | 1(6.3) |
| Employed year-round in a job for 1–10 hours per week | 1(2.7) | 1(4.8) | 0(0.0) |
| Employed year-round in a job for 11–29 hours per week | 2(5.4) | 0(0.0) | 2(12.5) |
| Employed year-round in a job for more than 30 hours per week | 14(37.8) | 10(47.6) | 4(25.0) |
| Other | 2(5.4) | 1(4.8) | 1(6.3) |
| Married or Partnered | |||
| Yes | 19(51.4) | 11(52.4) | 8(50.0) |
| No | 17(45.9) | 10(47.6) | 7(43.8) |
| Prefer not to answer | 1(2.7) | 0(0.0) | 1(6.3) |
| How many other adults live, share a room, or stay with you on a regular basis? | |||
| 0 | 12(33.3) | 9(45.0) | 3(18.8) |
| 1 | 14(38.9) | 4(20.0) | 10(62.5) |
| 2+ | 10(27.8) | 7(35.0) | 3(18.8) |
| How many children under 18 years old live, share a room, or stay with you on a regular basis at least half of the time? | |||
| 0 | 20(57.1) | 13(65.0) | 7(46.7) |
| 1–2 | 9(25.7) | 4(20.0) | 5(33.3) |
| 3+ | 6(17.1) | 3(15.0) | 3(20.0) |
| About how long has it been since you last visited a doctor for a routine checkup? | |||
| Within the past year(anytime less than 12 months ago) | 31(83.8) | 15(71.4) | 16(100) |
| Within the past 2 years(1 year but less than 2 years ago) | 6(16.2) | 6(28.6) | 0(0.0) |
| Within the past 5 years(2 years but less than 5 years ago) | 0(0.0) | 0(0.0) | 0(0.0) |
| 5 or more years ago | 0(0.0) | 0(0.0) | 0(0.0) |
| Health care coverage, including health insurance, prepaid plans, or government plans | |||
| Yes | 34(91.9) | 19(90.5) | 15(93.8) |
| No | 3(8.1) | 2(9.5) | 1(6.3) |
In total, 43 participants initially enrolled in the study and completed baseline measures, 40 (93%) participants completed measures at 5 weeks, and 37 (86%) completed measures at 15 weeks.
Original to this manuscript.
Outcomes
Baseline and post health measures are included in Table 2. A majority of participants were food insecure (93.0%), obese as calculated by BMI (69.8%), and had a waist circumference that indicated high risk for chronic disease (95.3%). Slightly more than half of participants had normal HbA1c (55.8%) and other participants were classified with a prediabetic HbA1c (27.9%), or a diabetic HbA1c (16.3%). Over half (62.8%) of participants exhibited hypertension as ascertained by blood pressure. BMI, total cholesterol, and waist circumference significantly (p<0.05) improved across participants. Weight in kilograms calculated for BMI changed from 98.7±29.8 at pre to 96.9 ±30.1 at post. No significant difference was observed in systolic blood pressure, diastolic pressure, and HbA1c.
Table 2.
Health Characteristics of Participants that Completeda Measures for the UnProcessed Pantry Project, 2019 (n=37)
| Category | Baselinea | Posta | ||
|---|---|---|---|---|
| N(%) | Mean±SD | N(%) | Mean±SD | |
| Body Mass Index | 36.66±9.50 | 36.05±9.67* | ||
| Normal weight (18.5 to 24.99) |
2(5.4) | 3(8.1) | ||
| Overweight (25 to 29.99) |
9(24.3) | 8(21.6) | ||
| Obese (Greater than or equal to 30) |
26(70.3) | 26(70.3) | ||
| HbA1cb (%) | 5.88±1.18 | 5.91±1.00 | ||
| Normal (Less than 5.8) |
21(56.8) | 18(48.6) | ||
| Prediabetes (Greater than or equal to 5.7) |
9(24.3) | 12(32.4) | ||
| Diabetes (Greater than or equal to 6.5) |
7(18.9) | 7(18.9) | ||
|
Hypertension
(Systolicc / Diastolicd; mmHg) |
130.03±16.19 / 72.22±10.52 |
127.76±16.58 / 70.57±13.76 |
||
| Normal(Less than 120 and less than 80) | 11(29.7) | 10(27.0) | ||
| Elevated (120–129 and less than 80) |
5(13.5) | 8(21.6) | ||
| Hypertension Stage 1 (130–139 or 80–89) |
12(32.4) | 10(27.0) | ||
| Hypertension Stage 2 (140–179 or 90–119) |
9(24.3) | 8(21.6) | ||
| Hypertensive Crisis (Greater than or equal to 180 and/or greater than or equal to 120) |
0(0.0) | 1(2.7) | ||
| Cholesterol(mg/dL) | 200.95±43.98 | 192.03±41.55* | ||
| Desirable (Less than 200) |
18(48.6) | 24(64.9) | ||
| Borderline (200–239) |
14(37.8) | 8(21.6) | ||
| High Risk (Greater than or equal to 240) |
5(13.5) | 5(13.5) | ||
| Waist Circumference(inches) | 47.17±7.98 | 44.52±7.86* | ||
| Normal Risk ≤ 40 inches for men or 35 inches for women | 3(8.1) | 4(10.8) | ||
| Increased Risk > 40 inches for men or 35 inches for women | 34(91.9) | 33(89.2) | ||
| Food Insecure | -- | -- | ||
| No | 3(8.1) | 6(16.2) | ||
| Yes | 34(91.9) | 31(83.8) | ||
In total, 43 participants initially enrolled in the study and completed baseline measures (pre), 40 (93%) participants completed measures at 5 weeks (mid), and 37 (86%) completed measures at 15 weeks (post).
Due to instrumentation, clinically significant changes are observed at 0.05.
Due to instrumentation, clinically significant changes are observed at 10mmHG.
Due to instrumentation, clinically significant changes are observed at 5mmHG.
Significant differences detected when p < 0.05 from pre to post.
Original to this manuscript.
The 37 participants that completed pre and post measures participated in a mean of 14.5 (±2.3) out of 17 total lessons, food distribution, social support, and measures offered. The 6 participants that did not complete post measures due to unforeseen circumstances, completed a mean of 9.7 (±3.3) out of 17 total intervention activities offered.
Dietary quality for several components significantly (p<0.05) improved as measured by the HEI-2015 (Table 3). Scores for total HEI-2015, whole grains, total protein foods, and added sugars (an increase in HEI score for added sugars indicates that the participants decreased added sugar consumption) significantly improved, while kilocalories significantly decreased.
Table 3.
Changes in Dietary Quality from Pre to Post as Measured by the Healthy Eating-Index 2015a for the UnProcessed Pantry Project 2019 (n = 37)
| Maximum Valuea | Pre (Mean±SD) |
Post (Mean±SD) |
P Valueb | |
|---|---|---|---|---|
| Total HEI-2015 Score | 100 | 47.18±12.20 | 54.53±13.18 | 0.01 |
| Total Vegetables | 5 | 2.88±1.86 | 3.06±1.81 | 0.66 |
| Greens and Beans | 5 | 1.88±2.27 | 1.74±2.32 | 0.79 |
| Total Fruit | 5 | 1.71±1.85 | 2.07±2.34 | 0.45 |
| Whole Fruit | 5 | 2.19±2.29 | 2.29±2.43 | 0.84 |
| Whole Grains | 10 | 1.88±2.68 | 4.07±4.17 | 0.01 |
| Dairy | 10 | 4.95±3.62 | 4.83±4.06 | 0.89 |
| Total Protein Foods | 5 | 3.99±1.46 | 4.55±1.06 | 0.05 |
| Seafood and Plant Proteins | 5 | 2.00±2.26 | 2.13±2.42 | 0.80 |
| Fatty Acid Ratio | 10 | 4.10±3.96 | 4.90±4.11 | 0.41 |
| Sodium | 10 | 3.91±3.98 | 3.62±2.62 | 0.73 |
| Refined Grains | 10 | 6.78±3.33 | 8.03±3.14 | 0.13 |
| Saturated Fats | 10 | 4.12±4.00 | 5.03±3.82 | 0.36 |
| Added Sugars | 10 | 6.64±3.64 | 8.20±2.80 | 0.03 |
| Kilocalories | --- | 2181.58±1092.89 | 1579.31±842.14 | 0.01 |
The Healthy Eating Index-2015 (HEI-2015) is a measure of diet quality used to assess how well a set of foods aligns with the 2015–2020 Dietary Guidelines for Americans. The HEI-2015 includes 13 components that can be summed to a maximum total score of 100 points. The components capture the balance among food groups, subgroups, and dietary elements including those to encourage, called adequacy components, and those for which there are limits, called moderation components. For the adequacy components, higher scores reflect higher intakes that meet or exceed the standards. For the moderation components, higher scores reflect lower intakes because lower intakes are more desirable. A higher total score indicates a diet that aligns better with the Dietary Guidelines.
Significant differences detected when p<0.05.
Original to this manuscript.
Significant decreases in energy-rich (p=0.000) and significant increases in nutrient-rich (p=0.017) food intake frequency over the past week, as measured by scales created from the FRESH Foods Survey, were observed from pre to post. Significant decreases in the availability of energy-rich (p=0.000) and increases in the availability of nutrient-rich (p=0.011) foods self-reported at home were observed from pre to post. Perceptions about fruit and vegetable consumption significantly increased (p=0.007) from pre to post. Engagement in healthy food practices, including planning, preparation, and procurement, and dinners cooked at home significantly increased (p=0.045) from pre to post.
Implementation
When check-ins were conducted and participants were asked, “Tell me about how following an unprocessed diet is going for you” the most frequent responses were that participants liked the format of the intervention, chose more unprocessed options over UPFs, prepared more meals at home, ate more fruits and vegetables, and felt better. The most common catalysts of these successes were using recipes, being mindful of portion sizes, and reading nutrition labels to make food choices. Participants noted that not having time to plan and prepare unprocessed meals, having to battle sugar and salt cravings, and breaking old habits were the three most noted challenges participants faced. A common theme as the intervention progressed was that engagement in healthy food practices became easier and participants’ tastes for food started to change. For example, as one participant commented, “sweetened yogurt is now way too sweet”.
A sample of 22 participants responded to a follow-up survey 6 months post intervention. A majority stated that they now ate or drank more unprocessed food since the study concluded, especially fruits and vegetables. Participants generally agreed that cost and time to prepare were barriers to sustaining an unprocessed food diet. Participants generally agreed that cooking skills, transportation, equipment, social support, reading an ingredient label for UPFs, and taste were not barriers to eating unprocessed food. In total, 14 of these participants (64%) were food insecure at follow-up, which represents a decrease from post measures. Weight maintenance, improvement in cholesterol and blood sugars, and increased energy were cited as sustained health changes. After UP3, participants found education about food processing categories and recipes as facilitators of success. Very few participants had input about aspects of UP3 that were not helpful. In the future, participants recommended more variety of food, quieter space to conduct lessons, and more recipes.
Discussion
The UP3 intervention demonstrates that the emergency food system can be leveraged to positively impact the health of food and nutrition insecure populations through a dietary intervention. It is important to design interventions that consider the complexities and resources required to make change in organizations that serve communities.
Commonly, food pantry users have relied on the emergency food system to gain access to a higher quantity of food, often sacrificing nutrient quality for shelf-stable UPFs. Food pantries are key food environments to assist individuals in acquiring enough nutrient-dense food to overcome dietary and health disparities experienced by this vulnerable population at risk of over-nutrition and related NCD. The food pantries in the intervention had to engage in organizational changes to provide space, time, and staffing to ensure participants had access to unprocessed food and UP3 could operate within the setting. The food pantries involved were participants on the CAB and had a high level of capacity to support the implementation of a dietary intervention. UP3 needs to be tested in food pantries with varying capacities to understand what aspects are easier or more difficult to adopt.
UP3 provides evidence that a relatively short and tailored intervention can reverse the trend of UPF being a staple component of the food pantry experience. In 16 weeks, UP3 intervention participants significantly improved their scores for Total HEI-2015, whole grains, total protein foods, and added sugar. The mean HEI-2015 at pre was 45 and at post was 55 for intervention participants compared to the average HEI-2015 score for Americans of 59.45
Across the public health field, NCD prevention and treatment has focused on individual education about eliminating specific health conditions (i.e., obesity), but has seen limited impact in curbing the global epidemic, especially among socially disadvantaged populations.1,2,46,49 Conversely, UP3 focused on the upstream factor of reducing UPF and increasing dietary quality at multiple levels of the food supply and individual education. Simultaneously providing access and education about nutritious foods through the food pantry setting provided an innovative and effective approach to shifting diets. Small, but significant improvements in dietary quality translated into various biomarker improvements, including a statistically significant reduction in participants’ BMI, total cholesterol, and waist circumference.
Biomarker changes are plausible to address and measure in a food pantry setting, as evidenced by UP3 and other interventions. For example, Seligman et al. conducted a 6-month pilot food bank intervention aiming to improve glycemic control among and observed significant positive changes.31 Positive changes observed during UP3 are significant and even small improvements in health metrics in the present can have benefits both medically and financially in the future.
The educational component of UP3 is novel because it focuses on eliminating UPF as a key food category that further exacerbates health disparities, already experienced by low-income populations. Previous research has demonstrated the importance of using a participatory process to identify needs and gaps in the food pantry setting in order to develop strategies that are tailored specifically to stakeholders of the emergency food system.48,49 Education about UPF helps individuals to understand a tangible root cause of many of their adverse health outcomes. One participant stated that UP3 is a program to learn “a new way of eating and taking care of yourself.” Another stated that UP3 is a program designed to “look at food in a different way, including the benefits and enjoyment of eating healthier. It’s not as difficult as I had imagined.” Other participants noted that UP3 provided them motivation, support, a sense of purpose, and has become part of their life.
At the 6-month follow-up, some participants suggested the low cost of UPF outweighed their desire to purchase unprocessed foods. This highlights the importance of the emergency food system to limit the availability of UPFs and increase unprocessed options for clients. The UP3 Framework provides a basis to procure a nutritious food supply. In a food system dominated by UPF, such an undertaking will take the involvement and commitment of stakeholders across the food system, including donors, staff, policymakers, and clients.
The success of UP3 in this context was in large part due to the active involvement and strong partnerships of the CAB and the commitment to build upon the evidence base for UP3. For example, studies have found that augmenting the food environment with tastings, recipes, or fruits and vegetables, improves consumption of whole foods among clients and therefore integrating these components into the UP3 Toolkit.50–52 This participatory approach ensured that the feedback of numerous stakeholders was incorporated into a rigorous intervention and added value by addressing food insecurity and NCD risk simultaneously.
From a public health standpoint, the evidence that participants increased engagement with beneficial food practices, improved their perceptions towards fruits and vegetables, and made positive and significant changes in availability and intake of energy-dense and nutrient-dense food provides justification for an intervention that focuses on eliminating UPF consumption. Furthermore, this intervention demonstrated that food pantries, and the emergency food system as a whole, may be an effective entry point for public health interventions that aim to reduce food insecurity and chronic disease risk.
Strengths and Limitations
This research is not without limitations. The sample size of participants was small, mostly female, and was conducted within two food pantries within a specific and rural geographic region, so generalizability may be limited. There was no control group, and although results of the study seem promising, they cannot be attributed to the study with certainty until a control trial confirms UP3’s observational results. The CAB was committed to demonstrating the benefit of UP3 with any eligible participants for the initial intervention, and a control group will be tested in the future. Retention rates remained high, with 86% (n=37) of participants completing baseline and post measures. Participants were committed to UP3 and dropping out was due to extenuating circumstances. It is possible that self-reported outcome data is subject to bias. However, the findings from more objective measures of health, such as cholesterol and BMI, are in line with findings from self-reported measures, including dietary quality. In the future, UP3 should be tested with diverse populations and in food pantry settings located in different geographies and with varying capacities.
Conclusions
The UP3 intervention provides evidence that emergency food systems may be an optimal entry point for improving diet among food and nutrition insecure and low-income populations. Improved food and nutrition security, particularly of diet quality away from UPFs, has multiple health benefits including a reduction in chronic disease risk. The setting for this intervention is already in place, considering there are more than 60,000 food pantries across the US,53 which facilitates the ease in which the UP3 intervention could be replicated and scaled with a commitment to space, time, and staffing. The authors suggest further research be conducted to test whether this intervention is feasible across geographies and with populations that were not included in this study.
More broadly, UP3 could serve as a catalyst for a dietary “sea change” within the emergency food system environment. While many food pantries strive to assist individuals in putting enough food on the table, this intervention also strives to improve the type of food that individuals are selecting, while instilling nutritional knowledge to make improved dietary selection sustainable far beyond the project period.
Supplementary Material
Acknowledgments
The authors are grateful to the UnProcessed Pantry Project (UP3) advisory board, Livingston Food Resource Center and Gallatin Valley Food Bank staff and volunteers, and Montana State University students who helped to design and implement the research and provided critical feedback during the process. The authors are grateful to Kevin Cain for statistical consulting.
Funding Disclosure
This publication was supported by Institutional Development Awards (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant numbers P20GM104417 and P20GM103474 and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR002319.
Footnotes
Conflicts of Interest The authors have no conflicts of interest to disclose.
References
- 1.Afshin A, Patrick JS, Kairsten AF et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393,1958–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forouhi N Global diet and health: old questions, fresh evidence, and new horizons. Lancet 2019;393,1916–1918. [DOI] [PubMed] [Google Scholar]
- 3.Srour B, Fezeu LK, Kesse-Guyot E et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). Br Med J 2019;365,1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rico-Campà A, Martínez-Fonzález MA, Alvarez-Alvarez I et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. Br Med J 2019;365,1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawrence MA, Baker PI. Ultra-processed food and adverse health outcomes. Br Med J 2019;365,2289. [DOI] [PubMed] [Google Scholar]
- 6.Monteiro CA, Cannon G, Levy R et al. NOVA. The star shines bright. World Nutriton 2016;7,1–3. [Google Scholar]
- 7.Poti JM, Braga B, Qin B. Ultra-processed food intake and obesity: What really matters for health—processing or nutrient content? BMC Public Health 2018;6,420–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro CA, Moubarac JC, Levy RB et al. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr 2018;21,18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Djupegot IL, Nenseth CB, Bere E et al. The association between time scarcity, sociodemographic correlates and consumption of ultra-processed foods among parents in Norway: a cross sectional study. BMC Public Health Published online: 15 May 2017. doi: 10.1186/s12889-017-4408-3. [DOI] [PMC free article] [PubMed]
- 10.The World Bank. World Bank Country and Lending Groups 2020. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 11.Baldridge AS, Huffman MD, Taylor F et al. The healthfulness of the US packaged food and beverage supply: a cross-sectional study. Nutrients 2019;11,1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steele EM, Baraldi LG, da Costa Louzada ML et al. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. Br Med J 2015;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vercammen KA, Moran AJ, McClain AC et al. Food security and 10-year cardiovascular disease risk among U.S. adults. Am J Prev Med 2019;56,689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2019;140,304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jetter KM, Cassady DL. The availability and cost of healthier food alternatives. Am J Prev Med 2006;30,38–44. [DOI] [PubMed] [Google Scholar]
- 16.Drewnowski A, Eichelsdoerfer P. Can low-income Americans afford a healthy diet? Nutr Today 2010;44,246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta S, Hawk T, Aggarwal A et al. (2019) Characterizing ultra-processed foods by energy density, nutrient density, and cost. Front. Nutr 2019;6,70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moran AJ, Khandpur N, Polacsek M et al. What factors influence ultra-processed food purchases and consumption in households with children? A comparison between participants and non-participants in Supplemental Nutrition Assistant Program (SNAP). Appetite 2018;134,1–8. [DOI] [PubMed] [Google Scholar]
- 19.Bickel G, Nord M, Price C et al. Guide to Measuring household food security USDA Food and Nutrition Service 2000.
- 20.Weinfield NS, Mills WG, Borger C et al. Hunger in America 2014. Feeding America Rockville and Washington, DC: Westat and the Urban Institute. 2014. [Google Scholar]
- 21.Byker Shanks C, Weinmann E, Holder J. The unprocessed pantry project framework to address nutrition in the emergency food system. Am J Public Health 2019;109,1368–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byker Shanks C Promoting food pantry environments that encourage nutritious eating behaviors. J Acad Nutr Diet 2017;117,523–525. [DOI] [PubMed] [Google Scholar]
- 23.Simmet A, Depa J, Tinnemann P et al. The nutritional quality of food provided from food pantries: a systematic review of existing literature. J Acad Nutr Diet 2017;117, 577–588. [DOI] [PubMed] [Google Scholar]
- 24.Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav 2013;45,159–164. [DOI] [PubMed] [Google Scholar]
- 25.Simmet A, Depa J, Tinnemann P et al. The dietary quality of food pantry users: a systematic review of existing literature. J Acad Nutr Diet 2017;17,563–576. [DOI] [PubMed] [Google Scholar]
- 26.Bazerghi C, McKay F, Dunn M. The role of food banks in addressing food insecurity: a systematic review. J Community Health 2016;41,732–740. [DOI] [PubMed] [Google Scholar]
- 27.Wetherill MS, Williams MB, White KC et al. Food pantries as partners in population health: Assessing organizational and personnel readiness for delivering nutrition-focused charitable food assistance. J Hunger Environ Nutr 2018;14, 50–69. [Google Scholar]
- 28.Seligman HK, Lyles C, Marshall MB et al. A pilot food bank intervention featuring diabetes—appropriate food improved glycemic control among clients in three states. Health Aff 2015;34. [DOI] [PubMed] [Google Scholar]
- 29.Rustad C, Smith C. Nutrition knowledge and associated behavior changes in a holistic, short-term nutrition education intervention with low-income women. J Nutr Educ Behav 2013;45,490–498. [DOI] [PubMed] [Google Scholar]
- 30.Martin KS, Wu R, Wolff M et al. A novel food pantry program: food security, self-sufficiency, and diet-quality outcomes. Am J Prev Med 2013;45,569–575. [DOI] [PubMed] [Google Scholar]
- 31.An R, Wang J, Liu J et al. A systematic review of food pantry-based interventions in the USA. Public Health Nutr 2019;22,1704–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Department of Agriculture (n.d.) SNAP-Ed Toolkit—Strategies & Interventions https://snaped.fns.usda.gov/program-administration/snap-ed-toolkit-strategies-interventions.
- 33.US Department of Agriculture. Rural-Urban Commuting Area Codes https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. 2019.
- 34.National Diabetes Prevention Program (n.d.) Prediabetes Risk Test https://www.cdc.gov/diabetes/prevention/pdf/Prediabetes-Risk-Test-Final.pdf.
- 35.US Department of Health and Human Services and US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans 8th ed. https://health.gov/dietaryguidelines/2015/. [Google Scholar]
- 36.Doran GT. There’s a SMART way to write management’s goals and objectives. Management Review 1981;70,35–36. [Google Scholar]
- 37.National Cancer Institute. Automated Self-Administered 24-Hour (ASA24®) Dietary Assessment Tool 2020. https://epi.grants.cancer.gov/asa24/.
- 38.National Cancer Institute. ASA24 ® Resources Related to the Healthy Eating Index (HEI) 2020. https://epi.grants.cancer.gov/asa24/resources/hei.html.
- 39.Hager ER, Quigg AM, Black MM et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126,26–32. [DOI] [PubMed] [Google Scholar]
- 40.Radandt NE, Corbridge T, Johnson DB et al. Validation of a two-item food security screening tool in a dental setting. J Dent Child 2018;85,114–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Calloway EE, Seligman HK, Boyd LW, et al. Development and testing of the FRESH Foods Survey to assess food pantry clients’ dietary behaviours and correlates. Public Health Nutr 2019;21,1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith TM, Calloway EE, Pinard CA et al. Using secondary 24-hour dietary recall data to estimate daily dietary factor intake from the FLASHE study dietary screener. Am J Prev Med 2017;52,856–862. [DOI] [PubMed] [Google Scholar]
- 43.Creswell JW. Research Design Qualitative, Quantitative, and Mixed Methods Approaches 2014;4,304. Thousand Oaks: Sage Publications. [Google Scholar]
- 44.Patton MQ. Qualitative research & evaluation methods 2001;3. Thousand Oaks: Sage Publications. [Google Scholar]
- 45.US Department of Agriculture. HEI Scores for Americans 2019. https://www.fns.usda.gov/hei-scores-americans.
- 46.Kumanyika SK. A Framework for increasing equity impact in obesity prevention. Am J Public Health Published online: 4 September 2019. 10.2105/AJPH.2019.305221. [DOI] [PMC free article] [PubMed]
- 47.Lean MEJ, Astrup A, Roberta SB. Making progress on the global crisis of obesity and weight management. Br Med J 2018;361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hoisington A, Shultz JA, Butkus S. Coping strategies and nutrition education needs among food pantry users. J Nutr Educ Behav 2002;34,326–333. [DOI] [PubMed] [Google Scholar]
- 49.Dave JM, Thompson DI, Svendsen-Sanchez A. Development of a nutrition education intervention for food bank clients. Health Promot Pract 2016;18, 221–228. [DOI] [PubMed] [Google Scholar]
- 50.Yao P, Ozier A, Brasseur K. Food pantry nutrition education about whole grains and self-efficacy. Fam Consum Sci Res J 2013;41,426–437. [Google Scholar]
- 51.Keller-Olaman SJ, Edwards V, Elliott SJ. Evaluating a food bank recipe-tasting program. Can J Diet Pract Res 2005;66,183–186. [DOI] [PubMed] [Google Scholar]
- 52.Long CR, Rowland B, McElfish PA. Intervention to improve access to fresh fruits and vegetables among Arkansas food pantry clients. Prev Chronic Dis 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feeding America. Delivering food and services n.d. https://www.feedingamerica.org/our-work/food-bank-network.
- 54.American Diabetes Association. A1C does it all 2020. https://www.diabetes.org/a1c.
- 55.Grundy SM, Stone NJ, Bailey AL et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;139,1082–1143. [Google Scholar]
- 56.American Heart Association. Understanding Blood Pressure Reading 2017. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings.
- 57.Center for Disease Control and Prevention. Assessing Your Weight 2020. https://www.cdc.gov/healthyweight/assessing/index.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


