Abstract
Objective
To determine the frequency of neurologic complications associated with influenza in hospitalized children.
Stud design
We performed a cross-sectional study of children (2 months through 17 years of age) with influenza discharged from 49 children’s hospitals in the Pediatric Health Information System during the influenza seasons of 2015–2020. Neurologic complications were defined as encephalopathy, encephalitis, aseptic meningitis, febrile seizure, nonfebrile seizure, brain abscess and bacterial meningitis, Reye syndrome, and cerebral infarction. We assessed length of stay (LOS), intensive care unit (ICU) admission, ICU LOS, 30-day hospital readmissions, deaths, and hospital costs associated with these events. Patient-level risk factors associated with neurologic complications were identified using multivariable logistic regression.
Results
Of 29 676 children hospitalized with influenza, 2246 (7.6%) had a concurrent diagnosis of a neurologic complication; the most frequent were febrile seizures (5.0%), encephalopathy (1.7%), and nonfebrile seizures (1.2%). Hospital LOS, ICU admission, ICU LOS, deaths, and hospital costs were greater in children with neurologic complications compared with those without complications. Risk factors associated with neurologic complications included male sex (aOR 1.1, 95% CI 1.02–1.21), Asian race/ethnicity (aOR 1.7, 95% CI 1.4–2.1) (compared with non-Hispanic White), and the presence of a chronic neurologic condition (aOR 3.7, 95% CI 3.1–4.2).
Conclusions
Neurologic complications are common in children hospitalized with influenza, especially among those with chronic neurologic conditions, and are associated with worse outcomes compared with children without neurologic complications. These findings emphasize the strategic importance of influenza immunization and treatment, especially in high-risk populations.
According to statistics from the Centers for Disease Control and Prevention (CDC), 8% of the US population is infected with influenza, and up to 1 million individuals are hospitalized each season.1,2 The disease burden among young children is disproportionally high and severe.3 For example, the rate of influenza-related acute respiratory tract illness in children is almost twice the rate in elderly patients.4 Influenza results in approximately 27 visits to the emergency department and 1 hospitalization per 1000 infected children.3 In the US, approximately 25 000 children are hospitalized annually, accounting for up to 10% of all pediatric hospitalizations during the winter season.5,6
The most common complications of influenza include lower respiratory tract infection, pneumonia, acute respiratory failure, and acute respiratory distress syndrome.1,7 During the 2009 pandemic, there were several reports of neurologic complication in children with influenza.8,9 Since that time, there has been increasing awareness of, and concern for, neurologic complications associated with influenza infection, particularly in children.7,10,11 Neurologic complications associated with influenza include seizures (febrile and nonfebrile), encephalitis, encephalopathy, acute necrotizing encephalopathy, aseptic meningitis, myelitis, secondary bacterial meningitis and brain abscess, and, rarely, cerebral infarction or Reye syndrome.10–12
Recent studies attempting to characterize neurologic complications of influenza in children have reported conflicting results and were limited by small sample size or narrowly defined populations that may not be generalizable.7,13–21 A single-center study of the 2000–2004 influenza seasons in the US found that 8.6% of children hospitalized with influenza had a neurologic complication. In this study, younger age, concurrent neurologic condition, and influenza B infection were associated with neurologic complications.7 In contrast, 2 large retrospective studies performed in Japan during the 1997–200116 and 2012–201615 influenza seasons found that influenza A infection was more common among those hospitalized with neurologic complications.
Because previous studies have been limited in scope and have yielded conflicting results, the objectives of this study were to determine the prevalence of influenza-associated neurologic complications in hospitalized children and determine the risk factors and outcomes associated with these complications.
Methods
We conducted a multicenter cross-sectional study of children admitted (inpatient and observation status) to children’s hospitals that contribute data to the Pediatric Health Information System (PHIS) database. The PHIS administrative database includes billing and use data from 49 tertiary care children’s hospitals across the US that are affiliated with the Children’s Hospital Association. Data quality and reliability are ensured through a joint effort between the Children’s Hospital Association and participating hospitals. Hospitals submit discharge data including demographics, diagnoses, procedures using International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), as well as detailed daily resource use.
Study Population
We included children from 2 months through 17 years of age hospitalized at a PHIS hospital with a discharge ICD-10-CM diagnosis of influenza (Table I; available at www.jpeds.com) during influenza seasons (see Influenza Season Definition section) from 2015 through 2020. Laboratory confirmation of influenza diagnosis was not available in the PHIS database. Children cared for in the neonatal intensive care unit (ICU) and those with a surgical primary diagnosis were excluded. Children younger than 2 months of age were excluded, as there are special considerations for hospitalization in this age group.
Table I.
Influenza diagnosis codes
| ICD-10-CM code | B9789, H669, H6690, H6691, H6692, H6693, J00, J019, J0190, J069, J10, J09, J09X, J09X1, J09X2, J09X3, J09X9, J10, J100, J1000, J1001, J1008, J101, J102, J108, J1081, J1082, J1083, J1089, J11, J110, J1100, J1108, J111, J112, J118, J1181, J1182, J1183, J1189, J1289, J129, J18, J181, J188, J189, J209, J40, R05, R509 |
Influenza Season Definition
Seasonal influenza activity, obtained from the CDC Flu Activity & Surveillance program and stratified by week and geographic census division, was used to define the influenza season for each year of the study.2 The specificity of influenza diagnosis is directly related to circulating prevalence of the virus.22,23 To increase the specificity of influenza cases and mitigate the potential for misclassification of influenza diagnoses included in the study, the influenza season comprised the 13 consecutive weeks that contained the maximum number of influenza cases for each geographic census division, similar to previous published studies (Table II; available at www.jpeds.com).3 The maximum number of influenza cases per geographic region was defined as the calendar week with the greatest frequency of laboratory-confirmed cases for the referenced season.
Table II.
Study definition of influenza season by region*
| Years | East North Central | East South Central | Middle Atlantic | Mountain | New England | Pacific | South Atlantic | West North Central | West South Central |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 2015–2016 | January 23 to April 16 | February 6 to April 30 | February 6 to April 30 | January 16 to April 9 | February 6 to April 30 | January 23 to April 16 | February 6 to April 30 | January 30 to April 23 | February 6 to April 30 |
| 2016–2017 | January 7 to April 1 | January 14 to April 8 | December 17 to March 18 | December 24 to March 18 | January 14 to April 8 | December 17 to March 18 | January 7 to April 1 | January 14 to April 8 | December 31 to March 25 |
| 2017–2018 | December 10 to March 3 | December 16 to March 10 | December 16 to March 10 | December 10 to March 3 | December 23 to March 17 | December 16 to March 10 | December 23 to March 17 | December 16 to March 10 | December 2 to February 24 |
| 2018–2019 | January 12 to April 6 | December 29 to March 23 | January 5 to March 30 | December 22 to March 16 | December 29 to March 23 | January 5 to March 30 | January 19 to April 13 | January 12 to April 6 | January 12 to April 6 |
| 2019–2020 | December 21 to March 13 | December 14 to March 7 | December 14 to March 7 | December 14 to March 7 | December 14 to March 7 | Nov 30 to February 22 | December 14 to March 7 | December 21 to March 13 | December 14 to March 7 |
Influenza season defined as the 13 consecutive weeks that contained the maximum number of influenza cases for each geographic census division per the CDC Flu Activity & Surveillance program.
Risk Factors for Neurologic Complications
Potential risk factors for influenza complications include age, sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, Other [defined as Pacific Islander, American Indian, multiracial, and other unspecified race/ethnicity]), geographic region (based on census division), chronic neurologic conditions (neurologic conditions defined using the pediatric complex chronic conditions classification system version 2),24 other complex chronic conditions, ICU status, and predominant influenza type or subtype. Influenza type/subtype (A/H1N1, A/H3N2, or B) was extrapolated from each patient’s census division during the week of admission for each encounter, identified by CDC Flu Activity & Surveillance on week of admission.
Outcomes
The primary outcome was a neurologic complication identified during the hospitalization by ICD-10-CM diagnostic codes. Neurologic complications were categorized as encephalopathy, encephalitis, aseptic meningitis, febrile seizure, nonfebrile seizure, brain abscess and bacterial meningitis, Reye syndrome, or cerebral infarction (Table III; available at www.jpeds.com). Our secondary, hospital-based outcomes included length of stay (LOS), admission to the ICU, ICU LOS, in-hospital death, and costs associated with hospitalizations in which an influenza-associated neurologic complication occurred. Costs were estimated from charges using hospital-specific cost-to-charge ratios and adjusted for hospital location using the Centers for Medicare and Medicaid price wage index.
Table III.
Neurologic complication diagnosis codes
| Outcomes | ICD-10-CM codes |
|---|---|
|
| |
| Encephalopathy | G043, G0430, G934, G9340, G9349, J1081, J1181 |
| Other* | R4182, F05, R404 |
| Encephalitis | A85, A858, A86, B941, G04, G040, G048, G049, G05, G053 |
| Aseptic meningitis | A87, A878, A879, G038, G039, G030, G039, G03 |
| Cerebral infarctions | I63, I630, I631, I632, I633, I634, I635, I636, I638, I639 |
| Febrile seizures | R560, R5600, R5601, R569 |
| Nonfebrile seizures | G401, G4020, G4021, G4030, G4031, G404, G405, G406, G407, G408, G409, R568, R569 |
| Brain abscess and bacterial meningitis | G060, G060, CG060, EG060, FA5482, A0221, A3211, A390, A5481, G000, G001, G002, G003, G008, G009, G01 |
| Reye syndrome | G937 |
Other diagnoses included altered mental status, delirium, and transient alteration of awareness.
Statistical Analyses
Demographic characteristics were summarized using frequencies and percentages for categorical variables and geometric means with SDs for continuous variables. Bivariate comparisons using χ2 tests were made between children with and without neurologic complications. The proportion of children with neurologic complications was calculated by dividing the number of influenza-associated hospitalizations with neurologic complications by the total number of influenza-associated hospitalizations. Results were stratified by neurologic complication category. Factors independently associated with neurologic complications were evaluated using multivariable logistic regression incorporating the following covariates: age, sex, race/ethnicity, payer, number of complex chronic conditions,24 neurologic complications status, and predominant circulating influenza strain. aOR for each risk factor were generated using generalized linear mixed effects models with a binomial distribution and random intercepts for each hospital. Febrile seizures, by definition, occur in children ≤6 years in age and are a known complication of viral illnesses. Therefore, we conducted analyses stratified by age ≤6 years and ≥7 years of age to account for the frequent occurrence of febrile seizures among younger children. We also performed a sensitivity analysis excluding febrile seizures from the outcome definition. All analyses were performed using SAS, version 9.4 (SAS Institute), and P < .05 was considered statistically significant.
Results
Study Population
A total of 29 676 influenza-associated hospitalizations were included in the study. Of these, 15 406 (51.9%) had a primary diagnosis of influenza. The most common primary diagnoses recorded when influenza was listed as a secondary diagnosis included dehydration (2151, 10.5%), acute respiratory failure with hypoxia (8.1%), and sepsis (3.8%). The majority of influenza-associated hospitalizations occurred in male patients (16,627, 56%), children ≤6 years of age (19 644; 66.2%), and those with government insurance (18 336; 61.8%). Most patients (7509; 74.7%) received an antiviral medication during the hospitalization. More than one-third (37.1%) of children had a complex chronic condition, and 8.1% had at least 1 neurologic complex chronic condition. Additional demographic characteristics are shown in Table IV.
Table IV.
Patient demographics
| Demographics | All patients (n = 296 76) | No neurologic complications (n = 27 430, 92.4%) | Neurologic complications (n = 2246, 7.6%) | P value |
|---|---|---|---|---|
|
| ||||
| Age, y, median [IQR] | 4 [1, 8] | 4 [1, 8] | 3 [1, 7] | <.001 |
| Flu diagnosis position | ||||
| Primary | 15 406 (51.9) | 14 547 (53) | 859 (38.2) | <.001 |
| Secondary | 14 270 (48.1) | 12 883 (47) | 1387 (61.8) | |
| Age, y | ||||
| <1 | 8960 (30.2) | 8159 (29.7) | 801 (35.7) | <.001 |
| 1–6 | 10 684 (36) | 9862 (36) | 822 (36.6) | |
| 7–11 | 5653 (19) | 5307 (19.3) | 346 (15.4) | |
| 12–17 | 4379 (14.8) | 4102 (15) | 277 (12.3) | |
| Sex | ||||
| Male | 16 627 (56) | 15 307 (55.8) | 1320 (58.8) | .004 |
| Female | 13 041 (43.9) | 12 117 (44.2) | 924 (41.1) | |
| Race | ||||
| Non-Hispanic White | 12 211 (41.1) | 11 332 (41.3) | 879 (39.1) | <.001 |
| Non-Hispanic Black | 7356 (24.8) | 6790 (24.8) | 566 (25.2) | |
| Hispanic | 6453 (21.7) | 5992 (21.8) | 461 (20.5) | |
| Asian | 842 (2.8) | 744 (2.7) | 98 (4.4) | |
| Other | 2814 (9.5) | 2572 (9.4) | 242 (10.8) | |
| Payor | ||||
| Government | 18 336 (61.8) | 16 918 (61.7) | 1418 (63.1) | .040 |
| Private | 9648 (32.5) | 8965 (32.7) | 683 (30.4) | |
| Other | 1692 (5.7) | 1547 (5.6) | 145 (6.5) | |
| Census division | ||||
| East North Central | 5495 (18.5) | 5103 (18.6) | 392 (17.5) | <.001 |
| East South Central | 2500 (8.4) | 2288 (8.3) | 212 (9.4) | |
| Middle Atlantic | 2633 (8.9) | 2438 (8.9) | 195 (8.7) | |
| Mountain | 2407 (8.1) | 2244 (8.2) | 163 (7.3) | |
| New England | 1044 (3.5) | 987 (3.6) | 57 (2.5) | |
| Pacific | 4013 (13.5) | 3692 (13.5) | 321 (14.3) | |
| South Atlantic | 4152 (14) | 3861 (14.1) | 291 (13) | |
| West North Central | 2515 (8.5) | 2273 (8.3) | 242 (10.8) | |
| West South Central | 4917 (16.6) | 4544 (16.6) | 373 (16.6) | |
| Any complex chronic condition | ||||
| No | 18 662 (62.9) | 17 153 (62.5) | 1509 (67.2) | <.001 |
| Yes | 11 014 (37.1) | 10 277 (37.5) | 737 (32.8) | |
| Number of non-neurologic complex chronic conditions | ||||
| 0 | 18 668 (62.9) | 17 158 (62.6) | 1510 (67.2) | <.001 |
| 1 | 6546 (22.1) | 6196 (22.6) | 350 (15.6) | |
| 2–3 | 3894 (13.1) | 3588 (13.1) | 306 (13.6) | |
| >3 | 568 (1.9) | 488 (1.8) | 80 (3.6) | |
| Neurologic complex chronic condition | ||||
| No | 27 258 (91.9) | 25 405 (92.6) | 1853 (82.5) | <.001 |
| Yes | 2418 (8.1) | 2025 (7.4) | 393 (17.5) | |
| ICU | ||||
| No | 24 932 (84) | 23 237 (84.7) | 1695 (75.5) | <.001 |
| Yes | 4744 (16) | 4193 (15.3) | 551 (24.5) | |
| Predominant circulating influenza strain during season* | ||||
| Influenza A H1N1 | 7297 (24.6) | 6725 (24.5) | 572 (25.5) | .602 |
| Influenza A H3N2 | 17 299 (58.3) | 16 004 (58.3) | 1295 (57.7) | |
| Influenza B | 5080 (17.1) | 4701 (17.1) | 379 (16.9) | |
| In-hospital antiviral medication | ||||
| No | 7509 (25.3) | 7029 (25.6) | 480 (21.4) | <.001 |
| Yes | 22 167 (74.7) | 20 401 (74.4) | 1766 (78.6) | |
Column percentages listed in parentheses after each value except where otherwise noted.
Influenza strain was extrapolated from each patient’s census division during the week of admission for each encounter, identified by CDC Flu Activity & Surveillance on week of admission.
Prevalence of Neurologic Complications
Of the 29 676 influenza-associated hospitalizations, 2246 (7.6%) children had a neurologic complication. The most common neurologic complication was febrile seizure (1477; 5.0%) followed by encephalopathy (514; 1.7%) and nonfebrile seizure (364; 1.2%). The least common neurologic complications were brain abscess and bacterial meningitis (29; 0.1%), cerebral infarction (16; 0.05%), and Reye syndrome (2; 0.01%) (Table V). The proportion of children receiving antiviral therapy was greater in children with neurologic complications compared with those with influenza without neurologic complication (78.6% vs 74.4%, P < .001). Oseltamivir accounted for more than 99.9% of antiviral agents used (Table VI; available at www.jpeds.com).
Table V.
Influenza-associated neurologic complications in hospitalized children with influenza
| Neurologic complications | No. (%) | Percent of encounters with neurologic complications (95% CI) |
|---|---|---|
|
| ||
| Febrile seizure | 1477 (53.7) | 4.98 (4.73–5.22) |
| Encephalopathy | 514 (18.7) | 1.73 (1.58–1.88) |
| Nonfebrile seizure | 364 (13.2) | 1.23 (1.1–1.35) |
| Other | 283 (10.3) | 0.95 (0.84–1.06) |
| Encephalitis | 35 (1.3) | 0.12 (0.08–0.16) |
| Aseptic meningitis | 29 (1.1) | 0.1 (0.06–0.13) |
| Brain abscess and bacterial meningitis | 29 (1.1) | 0.1 (0.06–0.13) |
| Cerebral infarction | 16 (0.6) | 0.05 (0.03–0.08) |
| Reye syndrome | 2 (0.1) | 0.01 (0–0.02) |
Table VI.
Antiviral prescribing in hospitalized children with and without neurologic complications
| Antivirals | All patients | No neurologic complications | Neurologic complications | P value |
|---|---|---|---|---|
|
| ||||
| Any | 22 167 (74.7) | 20 401 (74.4) | 1766 (78.6) | <.001 |
| Oseltamivir | 22 145 (74.6) | 20 381 (74.3) | 1764 (78.5) | <.001 |
| Zanamavir | 3 (0) | 3 (0) | 0 (0.0) | .620 |
| Peramivir | 70 (0.2) | 53 (0.2) | 17 (0.8) | <.001 |
| Baloxavir | 6 (0) | 6 (0) | 0 (0.0) | .483 |
Hospital-Based Outcomes
In unadjusted analysis, compared with children without neurologic complications, children with neurologic complications had longer hospital LOS (2.5 vs 2.2 days, P < .001), longer ICU LOS (2.7 vs 2.2 days, P < .05), more ICU admissions (24.5% vs 15.3%, P < .001), more in-hospital deaths (0.7% vs 0.2%, P < .001), and greater hospital costs ($6013 vs $5282, P < .001). When stratified by age, all reported hospital outcomes were worse in children >6 years old compared with younger children (Table VII).
Table VII.
Hospital outcomes associated with neurologic complications in children hospitalized with influenza
| All ages |
≤6 years |
>6 years |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Hospital outcomes | All patients | No neurologic complication | Neurologic complication | All patients | No neurologic complication | Neurologic complication | All patients | No neurologic complication | Neurologic complication |
|
| |||||||||
| LOS, d* | 2.2 (2.2) | 2.2 (2.2) | 2.2 (2.5) | 2.1 (2.1) | 2.1 (2.1) | 1.9 (2.3) | 2.3 (2.3) | 2.3 (2.3) | 3.2 (2.8) |
| ICU | 4744 (16) | 4193 (15.3) | 551 (24.5) | 2974 (15.1) | 2661 (14.8) | 313 (19.3) | 1770 (17.6) | 1532 (16.3) | 238 (38.2) |
| ICU LOS, d* | 2.5 (2.4) | 2.4 (2.4) | 2.8 (2.7) | 2.4 (2.4) | 2.4 (2.3) | 2.3 (2.5) | 2.6 (2.5) | 2.5 (2.5) | 3.4 (2.8) |
| Death, No. (%) | 63 (0.2) | 48 (0.2) | 15 (0.7) | 33 (0.2) | 24 (0.1) | 9 (0.6) | 30 (0.3) | 24 (0.3) | 6 (1) |
| Hospital costs* | 5333.6 (2.8) | 5281.5 (2.7) | 6012.9 (3.4) | 4827.2 (2.7) | 4832.7 (2.6) | 4766.4 (3.1) | 6484.2 (2.8) | 6260.7 (2.8) | 11 013.8 (3.5) |
| 30-day readmission, No. (%) | 2265 (7.6) | 2105 (7.7) | 160 (7.1) | 1451 (7.4) | 1340 (7.4) | 814 (8.1) | 765 (8.1) | 49 (7.9) | 814 (8.1) |
All outcome comparisons were statistically significant with a P < .05 except for 30-day readmissions.
Geometric mean (SD).
Factors Associated with Neurologic Complications
In multivariable analyses including all ages, children with neurologic complications were more likely to be male (aOR 1.1, 95% CI 1.0–1.2), Asian (aOR 1.7, 95% CI 1.4–2.1), or other race (which includes Pacific Islander, American Indian, multiracial, and other unspecified race/ethnicities) (aOR 1.2, 95% CI 1.03–1.4), and have a chronic neurologic condition (aOR 3.7, 95% CI 3.1–4.2) compared with children without neurologic complications. Children with 2–3 complex chronic conditions had lower odds of neurologic complications compared with children with no complex chronic conditions (aOR 0.6, 95% CI 0.5–0.7). This association was not significant in children with 4 or more non-neurologic complex chronic conditions. There were no significant differences in age, payor types, or predominant circulating influenza strain between those with and without neurologic complications (Figure and Table VIII [available at www.jpeds.com]).
Figure.
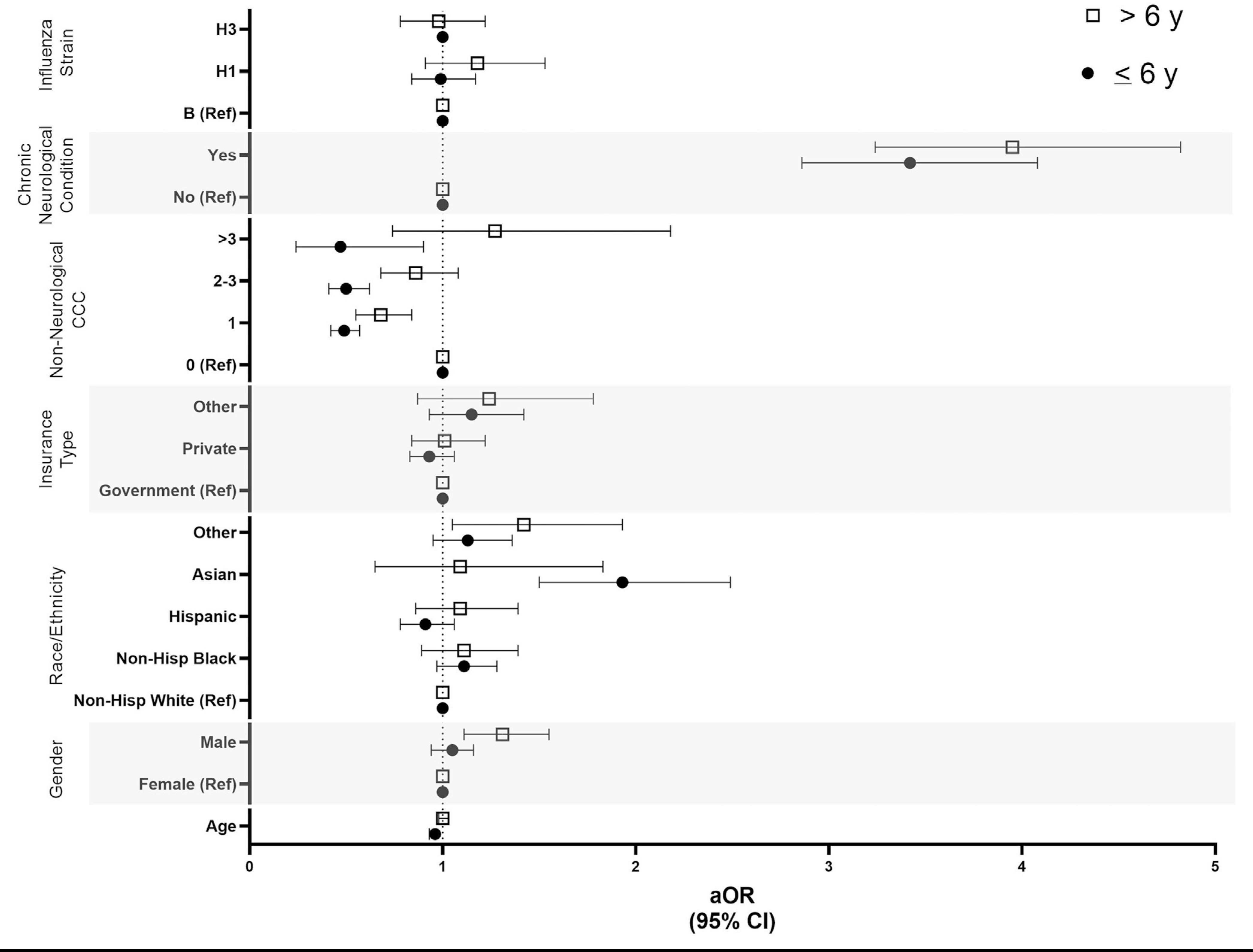
Forest plot of risk factors for influenza-associated neurologic complications in hospitalized children. aORs were derived using multivariable logistic following covariates: age, sex, race/ethnicity, payer, non-neurologic complex chronic condition, neurologic complex chronic condition, and predominant circulating influenza strain. CCC, complex chronic condition.
Table VIII.
Risk factors associated with neurologic complications in children hospitalized with influenza
| aOR (95% CI) |
|||
|---|---|---|---|
| Risk factors | All | ≤6 years | >6 years |
|
| |||
| Age, y | 0.97 (0.96–0.98) | 0.96 (0.93–0.98) | 1 (0.98–1.03) |
| Sex | |||
| Male | 1.11 (1.02–1.21) | 1.05 (0.94–1.16) | 1.31 (1.11–1.55) |
| Female | Reference | Reference | Reference |
| Race | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 1.11 (0.98–1.24) | 1.11 (0.97–1.28) | 1.11 (0.89–1.39) |
| Hispanic | 0.96 (0.85–1.1) | 0.91 (0.78–1.06) | 1.09 (0.86–1.39) |
| Asian | 1.69 (1.35–2.12) | 1.93 (1.5–2.49) | 1.09 (0.65–1.83) |
| Other | 1.2 (1.03–1.4) | 1.13 (0.95–1.36) | 1.42 (1.05–1.93) |
| Payor | |||
| Government | Reference | Reference | Reference |
| Private | 0.95 (0.85–1.05) | 0.93 (0.83–1.06) | 1.01 (0.84–1.22) |
| Other | 1.17 (0.97–1.4) | 1.15 (0.93–1.42) | 1.24 (0.87–1.78) |
| Non-neurologic complex chronic condition | |||
| 0 | Reference | Reference | Reference |
| 1 | 0.54 (0.48–0.61) | 0.49 (0.42–0.57) | 0.68 (0.55–0.84) |
| 2–3 | 0.63 (0.54–0.73) | 0.5 (0.41–0.62) | 0.86 (0.68–1.08) |
| >3 | 0.75 (0.5–1.14) | 0.47 (0.24–0.9) | 1.27 (0.74–2.18) |
| Chronic neurologic condition | |||
| No | Reference | Reference | Reference |
| Yes | 3.65 (3.2–4.16) | 3.42 (2.86–4.08) | 3.95 (3.24–4.82) |
| Predominant influenza strain | |||
| H1 | 1.04 (0.91–1.2) | 0.99 (0.84– 1.17) | 1.18 (0.91–1.53) |
| H3 | 1.01 (0.89–1.14) | 1 (0.87–1.16) | 0.98 (0.78–1.22) |
| B | Reference | Reference | Reference |
To account for the greater prevalence of febrile seizures in younger children, results were stratified by those ≤6 and ≥7 years. Among children ≤6 years old, age (aOR 0.97, 95% CI 0.96–0.98), Asian (aOR 1.7, 95% CI 1.3, 2.1) and other race (aOR 1.2, 95% CI 1.03–1.4), and chronic neurologic conditions (aOR 3.7, 95% CI 3.2–4.2) were associated with neurologic complications. Among children ≥7 years old, male sex (aOR 1.3 95% CI 1.1–1.6), other race (aOR 1.4, 95% CI 1.05–1.9), and chronic neurologic conditions (aOR 4.0, 95% CI 3.2–4.8) were associated with neurologic complications, but Asian race was not (Figure and Table VIII).
Sensitivity Analysis
A sensitivity analysis excluding febrile seizures from the outcome definition was performed. Removing febrile seizures resulted in an overall reduction of neurologic compilations (1181; 4.0%). Hospital outcomes in children >6 years were unchanged and remained overall worse than children ≤6 years (Table IX; available at www.jpeds.com). When evaluating risk factors for neurologic complications, there was no association between race/ethnicity and neurologic complications (Table X; available at www.jpeds.com).
Table IX.
Hospital outcomes associated with neurologic complications in children hospitalized with influenza in sensitivity analysis population*
| All ages |
≤6 years |
>6 years |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Hospital outcomes | All patients | No neurologic complication | Neurologic complication | All patients | No neurologic complication | Neurologic complication | All patients | No neurologic complication | Neurologic complication |
|
| |||||||||
| LOS, d | 2.2 (2.2) | 2.1 (2.2) | 3.2 (2.8) | 2.1 (2.1) | 2.1 (2.1) | 3.1 (2.7) | 2.3 (2.3) | 2.3 (2.3) | 3.3 (2.9) |
| ICU | 4744 (16) | 4288 (15) | 456 (38.6) | 2974 (15.1) | 2755 (14.5) | 219 (37) | 1770 (17.6) | 1533 (16.2) | 237 (40.2) |
| ICU LOS, d | 2.5 (2.4) | 2.4 (2.4) | 3.2 (2.7) | 2.4 (2.4) | 2.4 (2.3) | 2.9 (2.6) | 2.6 (2.5) | 2.5 (2.5) | 3.5 (2.8) |
| Death | 63 (0.2) | 48 (0.2) | 15 (1.3) | 33 (0.2) | 24 (0.1) | 9 (1.5) | 30 (0.3) | 24 (0.3) | 6 (1) |
| 30-day readmission | 2265 (7.6) | 2141 (7.5) | 124 (10.5) | 1451 (7.4) | 1375 (7.2) | 76 (12.8) | 814 (8.1) | 766 (8.1) | 48 (8.1) |
| Hospital costs | 5333.6 (2.8) | 5184.8 (2.7) | 10 559.2 (3.5) | 4827.2 (2.7) | 4725.6 (2.6) | 9574.3 (3.5) | 6484.2 (2.8) | 6251.5 (2.8) | 11 651.2 (3.5) |
All outcome comparisons were statistically significant with a P < .05 except for 30-day readmlsslons In children >6 years.
Excluded febrile seizures from the outcome definition.
Table X.
Risk factors associated with neurological complications in children hospitalized with influenza in sensitivity analysis population*
| Risk factors | aOR (95% CI) |
|---|---|
|
| |
| Age | 1.05 (1.04–1.06) |
| Sex | |
| Male | 1.16 (1.03–1.3) |
| Female | Reference |
| Race | |
| Non-Hispanic White | Reference |
| Non-Hispanic Black | 1.02 (0.87–1.2) |
| Hispanic | 0.9 (0.76–1.08) |
| Asian | 0.98 (0.68–1.41) |
| Other | 1.18 (0.95–1.46) |
| Payor | |
| Government | Reference |
| Private | 0.98 (0.86–1.13) |
| Other | 1.01 (0.77–1.33) |
| Non-neurologic complex chronic condition | |
| 0 | Reference |
| 1 | 0.88 (0.76–1.02) |
| 2–3 | 1.04 (0.87–1.24) |
| >3 | 1.26 (0.82–1.96) |
| Chronic neurologic condition | |
| No | Reference |
| Yes | 4.91 (4.24–5.68) |
| Predominant influenza strain | |
| H1 | 1.09 (0.9–1.31) |
| H3 | 0.92 (0.78–1.09) |
| B | Reference |
Excludes febrile seizures from the outcome definition.
Discussion
In this large, multicenter study evaluating neurologic complications among children hospitalized with influenza in the US, we conclude that neurologic complications are common and are associated with prolonged LOS, increased hospital costs, and increased in-hospital mortality compared with influenza hospitalizations without neurologic complications. Factors associated with neurologic complications included Asian and other races, male sex, and chronic neurologic conditions.
Much of the literature on influenza associated neurologic complications has involved a small number of cases (eg, 6 children,21 8 children,18 14 children,19 and 23 children20). In a study of 72 children hospitalized with influenza during the 2002–2004 influenza seasons, 10% had neurologic complications.7 A similar study of 59 children hospitalized with influenza, neurologic complications were present in 9.7%.17 We found a slightly lower 7.6% prevalence during more recent influenza seasons, which is consistent with a single center study including 23 children with influenza and neurologic complications.20
Although our study had similar rates for encephalopathy and seizures compared with other studies,7,17 there were differences in the proportion of seizures by type. Whereas the Newland study documented a similar proportion of febrile and nonfebrile seizures (3.2% and 3.4%, respectively), our study found a clear predominance of febrile seizures (5%) compared with nonfebrile seizures (1.2%), which is similar to the study of Khandaker et al (4.5% and 3%, respectively).6 The reason for these differences is unclear but may be related to population differences and sample size. A smaller (72 neurologic complications) single-center study did not report Table V. Influenza-associated neurologic complications in hospitalized children with influenza patient demographics.7 The study of Khandaker et al was performed in Australia with a relatively high proportion of Asian, Aboriginal Australian, and Pacific Islander patients. It is possible that these study populations had a different composition of sociodemographic and clinical characteristics, which were found to be risk factors for neurologic complications in our study.
We found that medical care for children with influenza and neurologic complications was uniformly more resource intense, with more ICU admissions, greater hospital costs, and longer hospital stays as well as more deaths than in children without neurologic complications. When stratified by age, the differences in outcomes were magnified in children ≥7 years of age. This may be due to the greater frequency of febrile seizures in the younger age group, which are self-limited and relatively benign compared with other neurologic complications. Therefore, the decreased LOS and lower costs found in children ≤6 years of age may be driven by short hospitalizations in children admitted for febrile seizures. It also is possible that younger children may recover more quickly or have less severe complications than children in older age groups. In addition, there likely is variability in admission rate for febrile seizures and some overlap in diagnosis of febrile and non-febrile seizures.
We found that Asian race was a risk factor for neurologic complications; however, this was only observed in children ≤6 years and likely driven by the frequent occurrence of febrile seizures in this age group. Febrile seizures are known to occur more frequently in the Asian population25 and with influenza,26 and febrile seizures were a very common neurologic complication in our population. We also found an increased risk of neurologic complications in children ≥7 years in the Other race/ethnicity cohort, which comprised Pacific Islander, American Indian, multiracial, and other unspecified race/ethnicities.27 The reason for this is unclear but social determinants have been linked to influenza outcomes.28 Data from the CDC demonstrate that American Indians and Pacific Islanders have a lower rate of influenza immunization compared with Asian and non-Hispanic White persons. Non-Hispanic Black, American Indian, and Alaska Natives also have greater rates of influenza hospitalizations compared with other race ethnicities.29
Unlike previous studies,7,16,30 we did not find an association between age or influenza type/subtype and neurologic complications. Our definition of influenza season was also highly specific, which likely minimized the inclusion of false-positive influenza cases. However, influenza subtype and strain information were not available for individual patients; thus, we categorized each influenza-associated hospitalization using the predominant regional circulating virus at the time of admission. It is possible that weak associations between neurologic complications and less common circulating influenza strains were not measured using this strain definition.
Children with chronic neurologic conditions have a diverse array of conditions including epilepsy, neuromuscular disorders, and cerebral palsy.24,31 Many of these children also have concurrent cardiac and respiratory conditions and represent a broad range of functional impairment.32,33 Children with underlying neurologic conditions are a particularly vulnerable population that is at high risk for influenza infection and resulting influenza associated complications, including hospitalization and death.7,8,13,34,35 As in other studies,7,17 we identified a strong association with underlying neurologic conditions. Acute respiratory infections are known to elicit seizures in children and fever can lower the seizure trigger threshold in those with epilepsy.36–39 These factors may contribute to the observed association between chronic neurologic conditions and neurologic complications.
The number of chronic non-neurologic conditions was negatively associated with risk of influenza complications, although the reasons for this are unclear. It is possible that children with chronic conditions have a lower clinical threshold for admission to the hospital than children without chronic condition. Children with chronic conditions also may have an increased rate of non-neurologic symptoms that precipitate admission, such as dehydration or inability to take oral medications.
Limitations of our findings include the retrospective nature of the study and that we only included children’s hospitals, which may limit the generalizability of our results to the outpatient setting. Diagnosis codes were used to identify our population and outcomes, which may have led to misclassification. For example, some mild influenza cases or neurologic complications, such assimple febrile seizures, not identified by ICD-10-CM code may have been excluded from the study, thus potentially underestimating the proportion of neurologic complications associated with influenza. It is also possible that mild influenza cases were not captured resulting in an overestimate of neurologic complications. However, our specific definition of the influenza season, limiting the season to peak influenza incidence, likely mitigated misclassification. Due to limitation of the PHIS databases, we were unable to ascertain use of antiviral medications or immunization status before hospitalization and were unable to account for these covariates in our analysis. Similarly, a history of febrile seizures is not included in the definition of chronic neurologic condition but is a predictor of febrile seizure. History of febrile seizures would not be accounted for in this analysis.
Chronic neurologic conditions are associated with poor influenza outcomes, including influenza associated complications and death.8 Our findings emphasizing the strategic importance of influenza immunization and treatment in this high-risk population40 provide targets for immediate, actionable changes in clinical practice.
Acknowledgments
Supported by the National Heart, Lung, and Blood Institute (K12 HL137943 [to J.A.]) and National Institute of Allergy and Infectious Diseases (K23AI121325 [to T.F.], K23AI141621 [to L.H.], K24 AI148459 [to C.G.], and R01AI125642 [to D.W.]) of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. C.G. has received consulting fees from Pfizer, Sanofi, and Merck.
Glossary
- CDC
Centers for Disease Control and Prevention
- ICD-10-CM
International Classification of Diseases, Tenth Revision, Clinical Modification
- ICU
Intensive care unit
- LOS
Length of stay
- PHIS
Pediatric Health Information System
Footnotes
The other authors declare no conflicts of interest.
References
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA 2004;292:1333–40. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and PreventionCDC Flu View. Accessed January 22, 2021. https://www.cdc.gov/flu/weekly/index.htm
- 3.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, et al. The underrecognized burden of influenza in young children. N Engl J Med 2006;355:31–40. [DOI] [PubMed] [Google Scholar]
- 4.Long CE, Hall CB, Cunningham CK, Weiner LB, Alger KP, Gouveia M, et al. Influenza surveillance in community-dwelling elderly compared with children. Arch Fam Med 1997;6:459–65. [DOI] [PubMed] [Google Scholar]
- 5.Miyakawa R, Barreto NB, Kato RM, Neely MN, Russell CJ. Early use of anti-influenza medications in hospitalized children with tracheostomy. Pediatrics 2019;143(3):e20182608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rolfes MA, Foppa IM, Garg S, Flannery B, Brammer L, Singleton JA, et al. Annual estimates of the burden of seasonal influenza in the United States: a tool for strengthening influenza surveillance and preparedness. Influenza Other Respir Viruses 2018;12:132–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newland JG, Laurich VM, Rosenquist AW, Heydon K, Licht DJ, Keren R, et al. Neurologic complications in children hospitalized with influenza: characteristics, incidence, and risk factors. J Pediatr 2007;150:306–10. [DOI] [PubMed] [Google Scholar]
- 8.Blanton L, Peacock G, Cox C, Jhung M, Finelli L, Moore C. Neurologic disorders among pediatric deaths associated with the 2009 pandemic influenza. Pediatrics 2012;130:390–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farooq O, Faden HS, Cohen ME, Ramanathan M, Barrett H, Farkas MK, et al. Neurologic complications of 2009 influenza-a H1N1 infection in children. J Child Neurol 2012;27:431–8. [DOI] [PubMed] [Google Scholar]
- 10.Shah S, Keil A, Gara K, Nagarajan L. Neurologic complications of influenza. J Child Neurol 2014;29:NP49–53. [DOI] [PubMed] [Google Scholar]
- 11.Chen Q, Peiqing L, Li S, Ziao W, Yang S, Lu H. Brain complications with influenza infection in children. J Behav Brain Sci 2020;10:129–52. [Google Scholar]
- 12.Ruben FL, Michaels RH. Reye syndrome with associated influenza A and B infection. JAMA 1975;234:410–2. [PubMed] [Google Scholar]
- 13.Coffin SE, Zaoutis TE, Rosenquist AB, Heydon K, Herrera G, Bridges CB, et al. Incidence, complications, and risk factors for prolonged stay in children hospitalized with community-acquired influenza. Pediatrics 2007;119:740–8. [DOI] [PubMed] [Google Scholar]
- 14.Okuno H, Yahata Y, Tanaka-Taya K, Arai S, Satoh H, Morino S, et al. Characteristics and outcomes of influenza-associated encephalopathy cases among children and adults in Japan, 2010–2015. Clin Infect Dis 2018;66:1831–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yokomichi H, Mochizuki M, Lee JJ, Kojima R, Yokoyama T, Yamagata Z. Incidence of hospitalisation for severe complications of influenza virus infection in Japanese patients between 2012 and 2016: a cross-sectional study using routinely collected administrative data. BMJ Open 2019;9:e024687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshikawa H, Yamazaki S, Watanabe T, Abe T. Study of influenza-associated encephalitis/encephalopathy in children during the 1997 to 2001 influenza seasons. J Child Neurol 2001;16:885–90. [DOI] [PubMed] [Google Scholar]
- 17.Khandaker G, Zurynski Y, Buttery J, Marshall H, Richmond PC, Dale RC, et al. Neurologic complications of influenza A(H1N1)pdm09: surveillance in 6 pediatric hospitals. Neurology 2012;79:1474–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maricich SM, Neul JL, Lotze TE, Cazacu AC, Uyeki TM, Demmler GJ, et al. Neurologic complications associated with influenza A in children during the 2003–2004 influenza season in Houston, Texas. Pediatrics 2004;114:e626–33. [DOI] [PubMed] [Google Scholar]
- 19.Landau YE, Grisaru-Soen G, Reif S, Fattal-Valevski A. Pediatric neurologic complications associated with influenza A H1N1. Pediatr Neurol 2011;44:47–51. [DOI] [PubMed] [Google Scholar]
- 20.Kedia S, Stroud B, Parsons J, Schreiner T, Curtis DJ, Bagdure D, et al. Pediatric neurological complications of 2009 pandemic influenza A (H1N1). Arch Neurol 2011;68:455–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goenka A, Michael BD, Ledger E, Hart IJ, Absoud M, Chow G, et al. Neurological manifestations of influenza infection in children and adults: results of a National British Surveillance Study. Clin Infect Dis 2014;58:775–84. [DOI] [PubMed] [Google Scholar]
- 22.Leeflang MM, Rutjes AW, Reitsma JB, Hooft L, Bossuyt PM. Variation of a test’s sensitivity and specificity with disease prevalence. CMAJ 2013;185:E537–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green DA, StGeorge K. Rapid antigen tests for influenza: rationale and significance of the FDA reclassification. J Clin Microbiol 2018;56: e00711–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung S Febrile seizures. Korean J Pediatr 2014;57:384–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiu SS, Tse CY, Lau YL, Peiris M. Influenza A infection is an important cause of febrile seizures. Pediatrics 2001;108:E63. [DOI] [PubMed] [Google Scholar]
- 27.Hadler JL, Yousey-Hindes K, Perez A, Anderson EJ, Bargsten M, Bohm SR, et al. Influenza-related hospitalizations and poverty levels—United States, 2010–2012. MMWR Morb Mortal Wkly Rep 2016;65: 101–5. [DOI] [PubMed] [Google Scholar]
- 28.Chandrasekhar R, Sloan C, Mitchel E, Ndi D, Alden N, Thomas A, et al. Social determinants of influenza hospitalization in the United States. Influenza Other Respir Viruses 2017;11:479–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health 2011;101:285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Togashi T, Matsuzono Y, Narita M. Epidemiology of influenza-associated encephalitis-encephalopathy in Hokkaido, the northernmost island of Japan. Pediatr Int 2000;42:192–6. [DOI] [PubMed] [Google Scholar]
- 31.Thomson JE, Feinstein JA, Hall M, Gay JC, Butts B, Berry JG. Identification of children with high-intensity neurological impairment. JAMA Pediatr 2019;173:989–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics 2011;127:529–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry JG, Poduri A, Bonkowsky JL, Zhou J, Graham DA, Welch C, et al. Trends in resource utilization by children with neurological impairment in the United States inpatient health care system: a repeat cross-sectional study. PLoS Med 2012;9:e1001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eriksson CO, Graham DA, Uyeki TM, Randolph AG. Risk factors for mechanical ventilation in U.S. children hospitalized with seasonal influenza and 2009 pandemic influenza A. Pediatr Crit Care Med 2012;13: 625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keren R, Zaoutis TE, Bridges CB, Herrera G, Watson BM, Wheeler AB, et al. Neurological and neuromuscular disease as a risk factor for respiratory failure in children hospitalized with influenza infection. JAMA 2005;294:2188–94. [DOI] [PubMed] [Google Scholar]
- 36.Bohmwald K, Galvez NMS, Rios M, Kalergis AM. Neurologic alterations due to respiratory virus infections. Front Cell Neurosci 2018;12:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang J, Yan W, Li Y, Zhang B, Gu Q. Relationship between common viral upper respiratory tract infections and febrile seizures in children from Suzhou, China. J Child Neurol 2014;29:1327–32. [DOI] [PubMed] [Google Scholar]
- 38.Vezzani A, Fujinami RS, White HS, Preux PM, Blumcke I, Sander JW, et al. Infections, inflammation and epilepsy. Acta Neuropathol 2016;131:211–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cha T, Choi YJ, Oh JW, Kim CR, Park DW, Seol IJ, et al. Respiratory syncytial virus-associated seizures in Korean children, 2011–2016. Korean J Pediatr 2019;62:131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith M, Peacock G, Uyeki TM, Moore C. Influenza vaccination in children with neurologic or neurodevelopmental disorders. Vaccine 2015;33:2322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


