Abstract
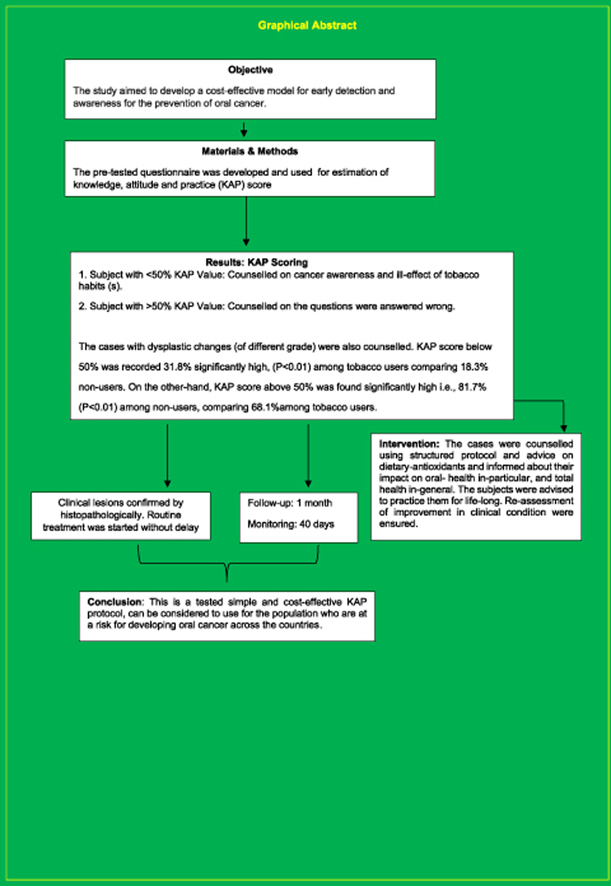
A study was conducted to establish levels of awareness of oral cancer and its causes among an Indian population.
A pre-tested structured questionnaire on Knowledge, Attitude and Practice [KAP] (open and closed ended questionnaire) was used to estimate the KAP score, followed by clinical examination of the oral mucosal lesions. The subjects were counselled immediately after completion of KAP scoring using a structured protocol of regarding tobacco cession, and given advice about intake of natural sources of anti-oxidants in the diet, of tomato, carrot and green leafy vegetables (GLV).
Subjects who had a KAP score 50% or less were counselled using a structured protocol. Subjects who had a KAP score greater than 50% were also counselled and given the correct information to their incorrect answers.
In the group of people with a KAP score 50% or less, continual behavioural therapy was given to remain tobacco free for life. The subjects were monitored weekly for between 30 and 40 days. Clinically suspect lesions of hyperplasic candidiasis, lichen planus, and all varieties of Leucoplakia were confirmed histopathologically and routine treatment (conservative or surgical) was started without delay for the group. Those cases with dysplastic changes (of all different grades) were also counselled. Regular follow-up was maintained over several months and re-assessment carried out at intervals and any improvement noted.
Conclusion
This is a cost-effective and simple method for estimation of the score on knowledge, attitude, and practice (KAP), and determinants of the ill-effect of tobacco habit(s) and engaging the popolation-in-need for their appropriate understanding about oral cancer screening and education for prevention and control.
Keywords: KAP-Intervention, Oral cancer screening & prevention, Cost-effective-model
Graphical abstract
1. Introduction, historical bacgroud and literature survey
India has the highest incidence rate of oral cancer in the world and estimated 35% of all cancers in the country.1, 2, 3 There is a strong correlation between the development and occurrence of oral cancer and the habit of chewing tobacco in India and adjacent countries.4, 5, 6 Chewing tobacco is a popular personal habit among many Indians and Nepalis from the plains. It has a long traditional history and strong cultural influences in the community in its various forms and types.7
The practice of chewing tobacco in India began in the form of ‘Paan’ chewing. ‘Paan’ is the local vernacular of quid. It is a roll of betel-vine leaf containing areca nut, lime, and Katachu, with or without tobacco and its consequences.8, 9, 10 The majority of rural households practice home-made ‘Paan’ preparation, and it therefore has a strong cultural and social impact, particularly among rural Indians. Currently, there are several commercial preparations, easily available in many small shops all over the country, containing not only the home-made constituents of ‘Paan’ but also other additives, such as colouring agents, aromatic compounds, spices and different forms of tobacco. These products are the cause of oral cancer leading to millions of disabilities and premature deaths-.10 The large proportion of the underserved rural population is prone to developing addiction to these products. Moreover, a significant proportion of young adults have started chewing tobacco. They consider chewing tobacco socially acceptable, good for health and convenient to chew in public places, compared to smoking tobacco.13
In India, there is a particular variety of the chewing tobacco known as ‘Khaini’, which is made of raw tobacco mixed with lime. The users chew ‘Khaini’ and hold the product in the lower buccal sulcus of their mouth. ‘Khaini’ is very carcinogenic, causing oral cancer with irreversible tissue damage at a molecular level.14,15 Also, anecdotally it has been revealed that ‘Khaini’ chewing is more prevalent in the North and North-eastern part of the country, especially among the rural population. In these areas many young adults have started the personal habit of ‘Khani’ chewing.
Interestingly, there is a social and cultural norm in India that expects juniors not to smoke in the presence of their known seniors (for example, parents, teachers, and any known elders to them) as a matter of courtesy. However, in the case of chewing tobacco, there is no such norm, meaning young people freely chew a roll of ‘Paan’ or a sachet of tobacco in the presence of their seniors.
The most pressing problem is that the majority of the population is unaware of the role of these personal habits in the development of oral cancer. Additionally, other habits such as, drinking alcohol and smoking represent risk factors as they might have a synergistic effect leading to oral cancer.16 It has also been observed that, especially in India, a significant proportion of population have the combined habits of smoking, chewing and drinking. Oral hygiene care among tobacco chewers has a role in the detection and care of people potentially at risk of developing oral cancer.17 The chewers have poor oral hygiene and stained oral mucosa, both of which are signs of poor life-style and may be taken as indicators for motivation of cessation.
An extensive literature search was performed to understand the situation in terms of identification of the risk group population and demographic variations of chewing tobacco habits in India. The risk group population has not been properly identified in the Indian population, although a series of extensive studies have been undertaken to understand the biological and clinical behaviour of oral mucosal lesions and their potential for malignant transformation among the rural population of the country. It included a 10 year follow-up assessment that was carried out 30 years ago by a team of researchers.18, 19, 20, 21, 22, 23
However, the studies did not specifically identify the risk group, demographic variability, estimation of level of knowledge of the ill-effects of chewing tobacco, nor the lack of cancer awareness programmes for the community in need. Few reports address the proper identification of the risk group population and those in India who would benefit from an oral cancer education programme. One report, however, found that 47% of men and 14% of women chewed as well as smoked tobacco and they were among the younger age group. The study revealed that tobacco habits (both chewing and smoking) are higher among the underserved community i.e., the economically poor and uneducated/less educated groups of the population. However, it did not identify the specific chewing habits. The finding does not provide information regarding the understanding or estimation of the level of knowledge of the ill-effects of chewing tobacco.24 Another study among Asian immigrants in Leicester, UK, revealed a relation between chewing habits and cultural beliefs, the different attitudes to tobacco and personal habits and the different preferences among different religious groups. This did not reflect the Indian scenario. Furthermore, the study did not estimate the knowledge among quid chewers regarding ill-effects.25 A study in the west of Scotland showed that when dentists take an active role raising the level of oral cancer awareness among their patients, the patients accepted the message quite quickly and were easily motivated to quit tobacco habits. In contrast to the situation in India, where there are no such initiatives, the study found there was a high percentage of attending patients unaware of the ill-effects of tobacco.26
The role of diet in the development of oral cancer is also an important issue. In India, there are diverse population groups having a variety of food habits but few reports regarding the role of diet, dietary habits and occurrence of oral cancer. It would be interesting to observe whether certain diets and food components, such as cumin (a commonly used spice and a natural colouring agent used in all types of sub-continent dishes), chillies, Kalakhar, Amrita Bindu and a few indigenous plant seeds, anti-oxidant rich fruits and vegetables can help prevention of chewing tobacco related oral cancer, also a case-control study mentioned about it regarding risk assessment of oral cancer.27,28 Diets rich with vitamins A, C and E (antioxidant group of micronutrients) have a proven role for prevention of epithelial cell cancer.29 On the other hand, fatty food has a cancer promoting role.30 An operational study was carried out in India advising for natural sources of anti-oxidants (carrot, tomatoes, green leafy vegetables) among patients who had developed chewing tobacco related oral pre-cancerous lesions that reverted. Therefore, it would be rational to estimate the knowledge regarding the beneficial effects of anti-oxidant containing diets for reversing chewing tobacco induced oral pre-cancer.
An extensive literature and internet survey was carried out to collect and collate information regarding the estimated level of knowledge of the ill-effects of chewing tobacco and also to understand the situation of oral cancer awareness programmes and measurement of the outcome of relevant programmes for the Indian population. Two websites were identified but they were not directly involved in the estimation of knowledge of the ill-effects of chewing tobacco or cancer awareness initiatives for the Indian community. The web-links do not provide the necessary information regarding mode of intervention nor estimation of the level of knowledge regarding the ill-effects of chewing tobacco 31, 32, 33,34.
2. Aims & objectives of the study
Considering the above facts, and with the aim of developing an effective oral cancer awareness programme, an estimation of the level of knowledge of the ill-effects of tobacco needed to be carried out among vulnerable groups of the population, compared to a control group.
This involved.
-
•
Identification of risk group population, by demographic variables and on the basis of the results of a questionnaire survey comparing the controls
-
•
Selection of a control group based on socio-economic status and personal habits.
-
•
A comprehensive understanding, assessment of knowledge of dietary preferences, knowledge of other associated habits, such as smoking, alcohol consumption, and the practice, if any, of oral hygiene maintenance.
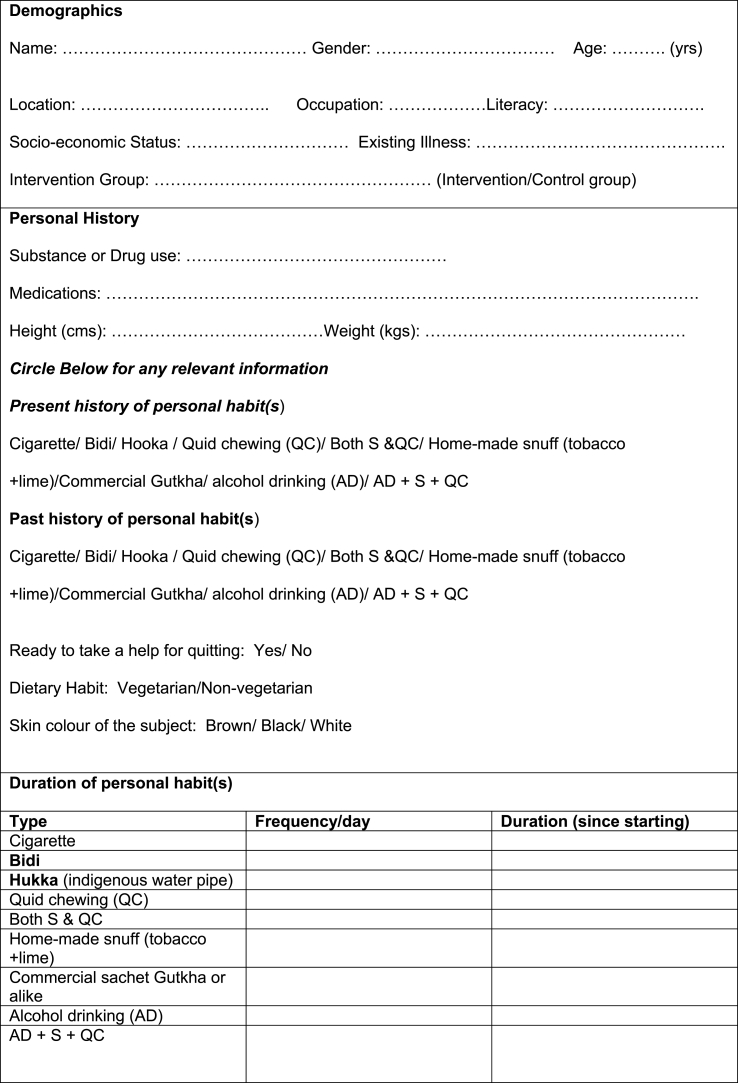
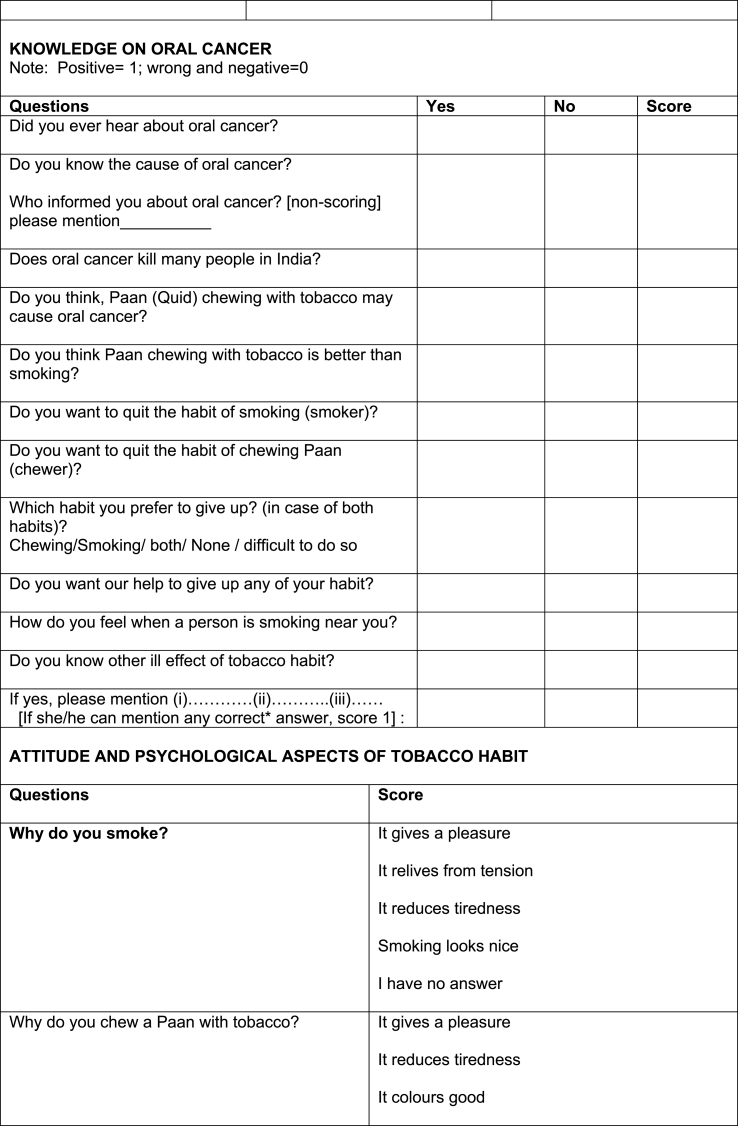
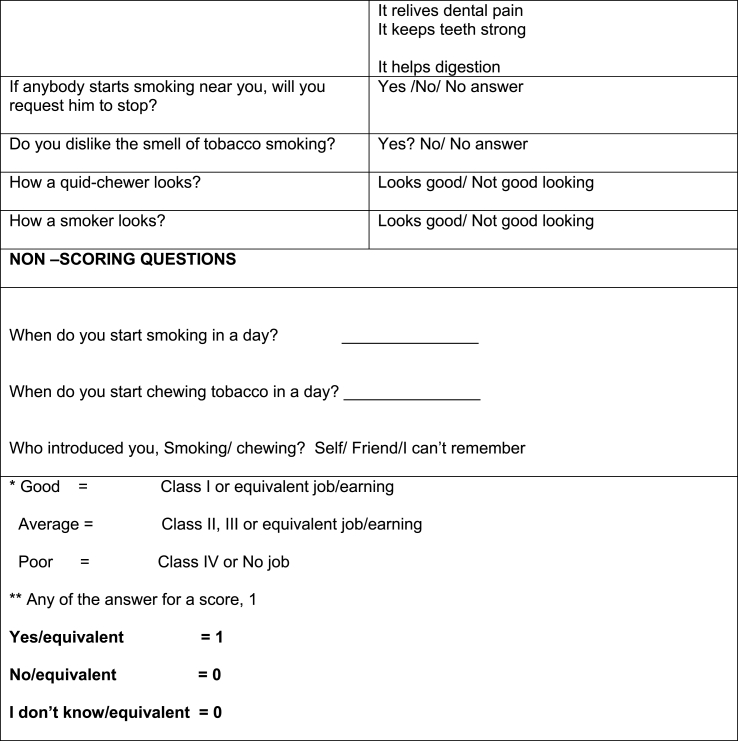
The proposed questionnaire aimed to address these points and determine the requirements for oral cancer reduction (Table 1).
Table 1.
KAP Questionnaire.
3. Materials & methods
In developing the KAP protocol for this study, the following points were taken into consideration:
-
•
Until the present date the literature search did not provide enough information regarding KAP on the ill effects of chewing habits in the risk groups of the Indian population. Therefore, this KAP study helped exploring the situation among the risk group population of the country and similar countries.
-
•
The assessment of knowledge, attitude and practice (KAP) is the ability of a person to acquire information.
-
•
Knowledge should be retained and understood. Therefore, in this context, the knowledge is reliant on the person's intellectual ability to understand the consequences of chewing quid.
In this KAP study, estimation of the level of knowledge of the ill-effects of chewing quid is an important determinant and is also vital to understanding the additional components of KAP, i.e., attitude and practice. Attitude (A) refers to inclinations to react in a certain way to certain situations; to see and interpret events according to certain predispositions; or to organize opinions into coherent and interrelated structures 35. Practice (P) refers to actions, based on the knowledge and attitude of an individual.
This study will aim to assess the personal experience, in terms of quid chewing habit (with duration and frequency of consumption), and how this may be used to help people stop such habits. Methods using the parameters of KAP are useful because the they provide measurable outcomes of an individual respondent. KAP outcomes usually serve as an educational diagnosis of the community-in-need. Therefore, the main purpose of this KAP study is to explore and estimate the changes in knowledge, attitude and practices of an individual or population group in order to gain a comprehensive understanding of an intervention.
Patient selection: A total 9288 subjects, comprising 5186 male and 4102 females who visited a dental hospital seeking dental treatment were included in the study.
Demographic information ie. location of dwelling, socio-economic status and their literacy status was recorded.
Questionnaire: Pre-tested multiple structured questionnaires were developed and the questionnaire used to carry out a survey among 15% of the sampled population (of each category). (Interview administered questionnaire survey: Table 1).
Calibration and standardisation of the examiners/interviewers: A structured training programme for the examiners was carried out. A mock survey and an assessment was performed among interviewers/examiners to avoid inconsistency and inter-examiner variation.
Statistical analysis: Chi Square test employed for statistical analysis of the data collected.
4. Results
4.1. Age and gender
Total 9288 cases, age ranging 20–89 years old (average age 64.5 year), comprising of 5186 (55.8%) male and 4102 (45.06%) female were examined. It was found that 3096 (33.3%) subjects had personal smoking, chewing or alcohol habits, and 6112 (65.8%) did not have a habit. Among the subjects with personal habits, 2631 (86.6%) were male, and 465(15.1%) were female.
4.2. Personal habit(s) by gender
280 males (60.2%) had a smoking habit, 132 (28.2%) females had a quid chewing habit. 36 (7.6%) males had both the habits. A negligible proportion of the study population (1%) answered that they had an alcohol drinking habit but 1.9% had smoking and alcohol drinking habits, and 1.2% answered that they had combined habits of smoking, alcohol drinking, and quid chewing.
4.3. KAP scores below and above 50%
A KAP score below 50% was recorded for 31.8% of tobacco users, being significantly high, (P < 0.01) compared to 18.3% non-users. On the other-hand, a KAP score above 50% was found significantly high in 81.7% (P < 0.01) among non-users, compared to 68.1% among tobacco users. Higher KAP scores reflected a higher level of knowledge, attitude, and practice regarding the ill-effects of tobacco habits and a better understanding of oral cancer and prevention provisions among the group.
4.4. Post intervention outcome
73% subjects quitted tobacco habit(s), recorded at 2nd visit (after a week). 23% had re-started the personal habit of tobacco within a month. After counselling tobacco cessation and dietary advice for the intake of antioxidant intake from fresh fruits and raw green vegetables, it was found that, 86.5% (P < 0.01) had stopped their habits, and their mucosal lesions, such as pseudo-membranous candidiasis, snuff pouch leukokeratosis, nicotini palatine, furred tongue, geographic tongue (erythema migrans linguae), median rhomboid glossitis and homogenous Leucoplakia was improved or resolved. Post-intervention KAP score was also increased (89%), which is highly significant (P < 0.01).
A high incidence rate of oral candidiasis was found in 69.8% male smokers (P < 0.01), and 61.4% among quid chewers (P < 0.001). Among the subjects who had both quid chewing and smoking habits (P < 0.001) this was found in 100%. The estimated incidence of oral candidiasis among subjects who had tobacco habits was significantly higher at 10% compared to 0.035% who did not have the habit (p < 0.01).
The post-intervention result of relapse in ninety-six (96.7%) cases was highly significant (P < 0.001). The combined habits of smoking and chewing are the highest risk factor for the development of candidal disease. Males are in the highest risk group of the population for the development of oral candidiasis. In this series, we did not find a female smoker.
5. Discussion
From the information gathered and the literature survey, it has been noted that in India (and this could be extrapolated to any other areas where there are similar identifiable problems, notably, south Asia and the Asian diaspora), the incidence rate of oral cancer is exceedingly high and is related to chewing tobacco habits. In fact, the long traditional and cultural practice of ‘Paan’ chewing has been strengthened in more recent times by the ready availability of sachets of Paan granules, and driven the enormous use of tobacco chewing habits among many Indians. Cigarettes and sachets can often be purchased from the same outlet and as these are largely uncontrolled businesses, generating huge amounts of money for a variety of operators, the resultant disability and death toll remains high. There is increasing evidence for a strong corelation between the habit of chewing tobacco and the occurrence of oral cancer. Currently, the government of India has introduced a law for a tobacco ban in public places, and also signed the WHO Framework Convention on Tobacco Control, but remarkably has failed to address the habit of chewing tobacco. There are no clear cut rules to regulate these sales or impose restrictions on chewing tobacco in public places. Therefore, we can assume the use of chewing tobacco is and will remain uncontrolled in India.
There is a perception, prevalent among Indians, that chewing ‘Paan’ or a tobacco sachet containing essentially the same components, is not dangerous for health. Moreover, the cultural norm in the community does not identify chewing tobacco as a bad habit compared to smoking and drinking. Therefore, the development of an awareness programme to stop chewing tobacco is an important and rather daunting task for India and elsewhere where these habits prevail. A consistent approach will need to be developed, after analysing the situation, including a proper assessment of the behaviour and attitudes of the affected groups of the population. It will be necessary to understand the mind of the people - how and why they started the habit of chewing tobacco and why they consider that chewing tobacco will not harm their health as does cigarettes or bidi smoking. Therefore, to develop any future awareness programme, a questionnaire such as used in this study, would need be used to estimate the level of knowledge on the ill-effect of tobacco for any future intervention.
To comprehensively estimate the level of knowledge, other related factors need to be identified, in particular, dietary habits and other co-habits such as smoking and alcohol consumption. An understanding of the level of knowledge among the population regarding role of diet in the development of oral cancer will need to be determined, aiming to develop a holistic approach for raising the level of oral cancer awareness in the community.
Although several studies published to date explain the pattern of chewing tobacco, the majority of the population living in rural areas are unaware of the causes of oral cancer, especially those due to chewing tobacco. An awareness model will need to include or exclude some of the determinants of the development of oral cancer, such as co-habits, associated medical conditions, oral hygiene and dietary habits. Understanding behavioural patterns will require critical assessment of the perception regarding chewing tobacco among the chewers, by estimation of the level of knowledge of the ill-effects of tobacco, assessing their attitude, and life-style factors. All these variables need to be assessed and estimated using a structured questionnaire survey by interview such as the one developed for this study.
Ultimately, any proposed studies will assist the policy makers in developing guidelines for the population at risk and thus help the vulnerable groups of the population by raising their anti-tobacco awareness. Dentists, doctors and community health workers should also play an active role helping patients with these habits.
6. Conclusion
Although a single approach will not be completely effective in stopping the habit of chewing tobacco in India and elsewhere in the sub-continent where the habit prevails and even in the Indian diaspora in other parts of the world, it will certainly help the chewers to reduce the frequency of chewing and ultimately complete cessation of these deadly habits, provided a structured questionnaire-based assessment and education programme is established. Therefore, the proposed questionnaire will help estimate the level of knowledge regarding the ill effects of chewing tobacco, identify the risk group population and facilitate the basis for an effective oral cancer prevention programme for the community living in low resource settings of Low and Middle Income Countries (LMICs).
Acknowledgement
Departmental Funding by the Nitte University, Mangalore, India. My team and myself are very grateful to the Chancellor N.V Hegde of Nitte (Deemed to be University) for his personal encouragement, and continuous supports in this interventional research work.
References
- 1.Sankaranarayanan R. Oral cancer in India: an epidemiologic and clinical review. Oral Surg Oral Med Oral Pathol. 1990 Mar;69(3):325–330. doi: 10.1016/0030-4220(90)90294-3. [DOI] [PubMed] [Google Scholar]
- 2.Johnson N. Tobacco use and oral cancer: a global perspective. J Dent Educ. 2001;65(4):328–339. [PubMed] [Google Scholar]
- 3.Peterson P.E., World Oral Health Report . World Health Organisation; Geneva, Switzerland: 2003. Continuous Improvement of Oral Health in the 21st Century – the Approach of the World Health Organisation Global Oral Health Programme. 2003. [Google Scholar]
- 4.Goud M.L., Mohapatra S.C., Mohapatra P., et al. vol. 6. Epidemiological Correlates between Consumption of Indian Chewing Tobacco and Oral Cancer; Jun., 1990. pp. 219–222. (European Journal of Epidemiology). 2. [DOI] [PubMed] [Google Scholar]
- 5.IARC Monographs Programme Finds Betel-Quid and Areca-Nut Chewing Carcinogenic to Humans. WHO Monograph; 2003. http://www.who.int/mediacentre/news/releases/2003/priarc/en/index.html 30.09.20221. [PubMed] [Google Scholar]
- 6.Shimkhada R., Peabody J.W. Policy and practice: tobacco control in India. Bull World Health Organ. 2003;81(1) [PMC free article] [PubMed] [Google Scholar]
- 7.Tobacco Use in India: Practices, Patterns and Prevalence. http://www.whoindia.org/linkfiles/tobacco_free_initiative_03-chapter-03.1.pdf (accessed on 30.09.2021).
- 8.Eternal Glories, colours of India: Paan chewing: http://www.eternalglories.com/paan_chewing.htm (accessed on 30.09.2021).
- 9.Ariyawardana A., Athukorala A.D., Arulanandam A. Effect of betel chewing, tobacco smoking and alcohol consumption on oral submucous fibrosis: a case-control study in Sri Lanka. J Oral Pathol Med. 2006;35:197–201. doi: 10.1111/j.1600-0714.2006.00400.x. [DOI] [PubMed] [Google Scholar]
- 10.Strickland S.S. Anthropological perspectives on use of the areca nut. Addiction Biol. 2002 Jan;7(1):85–97. doi: 10.1080/13556210120091446. [DOI] [PubMed] [Google Scholar]
- 13.Prabha S.C., Mulla U. Areca nut: the hidden Indian 'gateway' to future tobacco use and oral cancers among youth. Indian J Med Sci. 2007;61(6):319–321. [PubMed] [Google Scholar]
- 14.Nobuharu Y., Tsukasa K., Katakura K., Shibahara T., Choudhury C. Loss of heterozygosity (LOH) on chromosomes 2q, 3p and 21q in Indian oral squamous cell carcinoma. Bull Tokyo Dent Coll. 2007;48(3):109–117. doi: 10.2209/tdcpublication.48.109. [DOI] [PubMed] [Google Scholar]
- 15.Nair U., Bartsch H., Nair J. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: a review of agents and causative mechanisms. Mutagenesis. 2004;19(4):251–262. doi: 10.1093/mutage/geh036. [DOI] [PubMed] [Google Scholar]
- 16.Balaram P., Sridhar H., Rajkumar T., et al. Oral cancer in southern India: the influence of smoking, drinking, paan-chewing and oral hygiene. Int J Cancer. 2002;98(3):440–445. doi: 10.1002/ijc.10200. [DOI] [PubMed] [Google Scholar]
- 17.Maier H., Zöller J., Herrmann A., et al. Dental status and oral hygiene in patients with head and neck cancer. Otolaryngol Head Neck Surg. 1993;108(6):655–661. doi: 10.1177/019459989310800606. [DOI] [PubMed] [Google Scholar]
- 18.Mehta F.S., Gupta P.C., Daftary D.K., Pindborg J.J., et al. Epidemologic and histologic study of oral cancer and leukoplakia among 50915 villagers in India. Cancer. 1969;24:32–49. doi: 10.1002/1097-0142(196910)24:4<832::aid-cncr2820240427>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 19.Mehta F.S., Gupta P.C., Daftary D.K. An epidemiologic assessment of cancer risk in oral precancerous lesions in India with special reference to nodular leukoplakia. Cancer. 1989;63:2247–2252. doi: 10.1002/1097-0142(19890601)63:11<2247::aid-cncr2820631132>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 20.Mehta F.S., Gupta P.C., Daftary D.K., Pindborg J.J., et al. An epidemiologic study of oral cancer and precancerous conditions among 101761 villagers in Maharashtra, India. Int J Cancer. 1972;10:134–141. doi: 10.1002/ijc.2910100118. [DOI] [PubMed] [Google Scholar]
- 21.Gupta P.C., Bhonsle R.B., Murti P.R., et al. A study of dose-response relationship between tobacco habits and oral leukoplakia. Br J Cancer. 1984;50:527–531. doi: 10.1038/bjc.1984.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta P.C., Bhonsle R.B., Murti P.R., et al. An intervention study of oral cancer and pre-cancer in rural Indian populations: a preliminary report. Bull World Health Organ. 1982;60:441–446. [PMC free article] [PubMed] [Google Scholar]
- 23.Rani1 M., Bonu1 S., Jha P., et al. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tobac Control. 2003;12:e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodgers J., Macpherson L.M., Smith G.L., Crighton A.J., Carton A.T., Conway D.I. Characteristics of patients attending rapid access clinics during the West of Scotland Cancer Awareness Programme oral cancer campaign. Br Dent J. 2007 Jun 9;202(11):E28. doi: 10.1038/bdj.2007.342. discussion 680-1. [DOI] [PubMed] [Google Scholar]
- 25.Vora A.R., Yeoman C.M., Hayter J.P. Alcohol, tobacco and paan use and understanding of oral cancer risk among Asian males in Leicester. Br Dent J. 2000;188(8) doi: 10.1038/sj.bdj.4800506. [DOI] [PubMed] [Google Scholar]
- 26.Sinha R., Anderson D.E., McDonald S.S., Greenwald P. Cancer risk and diet in India. J Postgrad Med. 2003;49:222–228. [PubMed] [Google Scholar]
- 27.Rao D.N, Gnesh B, Rao R.S, Desai P.B. : Risk Assessment of Tobacco, Alcohol and Diet in Oral Cancer : A Case-Control Study. [DOI] [PubMed]
- 28.Garewal H., Meyskens F., Friedman S., et al. Oral cancer prevention: the case for carotenoids and anti-oxidant nutrients. Prev Med. 1993;22(5):701–711. doi: 10.1006/pmed.1993.1064. [DOI] [PubMed] [Google Scholar]
- 29.Kushi L, Giovannucci E. Dietary fat and cancer 2002 Am J Med.30;113 Suppl 9B:63S-70S. [DOI] [PubMed]
- 30.Bianka B., Pawel J., Winklewski2 3 * and Magdalena Wszedybyl-Winklewska2 Dietary fat and cancer—which is good, which is bad, and the body of evidence. Int J Mol Sci. 2020 Jun;21(11):4114. doi: 10.3390/ijms21114114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Computer –aided oral cancer screening and education: Gustavsson T, Chodorowski A, Chowdhury CR. http://www.sasnet.lu.se/chalsig.html (accessed 10.09 2021).
- 32.IARC Oral Cancer Screening group: http://screening.iarc.fr/oralindex.php (accessed 10.09.20121).
- 33.Joseph Bobby K. Oral cancer: prevention and detection. Med Princ Pract. 2002;11:32–35. doi: 10.1159/000057776. [DOI] [PubMed] [Google Scholar]