Abstract
Over 700,000 children throughout the U.S. have received insurance coverage through welcome mat effects of Medicaid expansion, including children with autism spectrum disorder (ASD). Utilizing health workforce data from the Health Resources and Services Administration, we examined workforce growth (2008–2017) among three types of health providers for children with ASD as a result of Medicaid expansion: child psychiatrists, board-certified behavioral analysts (BCBAs) and pediatricians. We found that state Medicaid expansion was associated with a 9% increase in BCBAs per 100,000 children one year after enactment, a 5% increase in child psychiatrists, and was not associated with growth in pediatricians. Results indicate the importance of new policies that directly address a shortage of providers for children with ASD.
Keywords: Autism spectrum disorder, autism, Medicaid expansion, workforce, child psychiatrists
INTRODUCTION
The estimated prevalence of autism spectrum disorder (ASD) in the United States has tripled over the past 20 years: from 1 in 150 children in 2000 to 1 in 54 children in 2016 (CDC 2018). Health providers have struggled to adequately meet the complex health care needs of this large pediatric population (R. K. McBain, Kareddy, et al. 2019). This is driven partly by a shortage of healthcare providers such as child psychiatrists and board-certified behavioral analysts (BCBAs) (R. K. McBain, Kofner, et al. 2019), and partly by insufficient training for other provider groups such as pediatricians (Carbone et al. 2010; Nolan et al. 2016).
To improve access to health care services for children with ASD, federal and state lawmakers have passed legislation to broaden insurance benefits. For example, state insurance mandates—which compel private insurers to cover autism-related healthcare services (NCSL 2018)—have been shown to increase utilization of services (Barry et al. 2017) and the workforce for ASD (R. K. McBain, Cantor, Kofner, Callaghan, et al. 2020; R. K. McBain, Cantor, Kofner, Stein, et al. 2020). Similar to state insurance mandates, Medicaid expansion under the Affordable Care Act (ACA) varied across states. However, few studies have examined how the ACA’s Medicaid expansion have affected the health workforce or labor participation among those eligible for public insurance (Gooptu et al. 2016; Hill et al. 2019).
ACA Medicaid expansion has extended insurance benefits to millions of Americans. While direct beneficiaries of Medicaid expansion are typically lower-income adults, there is also evidence that over 700,000 children throughout the U.S. have received health insurance coverage through “welcome mat” effects of Medicaid expansion (Hudson and Moriya 2017). This has been the result of information campaigns about Medicaid eligibility, and many states having adopted a “no wrong door” policy of determining eligibility across programs. Past studies have similarly identified parental effects of joint parent-child eligibility for Medicaid (DeVoe, Crawford, et al. 2015; DeVoe, Marino, et al. 2015; Dubay and Kenney 2003). Moreover, at the same time as states began implementing Medicaid expansion the Department of Health and Human Services in 2014 issued new guidance on early and periodic screening, diagnosis and treatment for children with ASD enrolled in Medicaid (Mann 2014).
Given the substantial increase in Medicaid enrollment for children, one would expect demand for pediatric health services will be higher in states with Medicaid expansion, and consequently lead to an increase in the supply of health services for children—including children with ASD. Prior studies have identified growth in the U.S. health workforce as a function of implementing the Children’s Health Insurance Program (CHIP) in the 1990s and the early 2000s (Hill et al. 2019). However, no studies have examined how ACA Medicaid expansion has affected the health care workforce serving children with ASD.
To fill this gap, we evaluated the effect of ACA Medicaid expansion on workforce growth for children with ASD, focusing on three types of providers who routinely offer services to this population: child psychiatrists, pediatricians, and BCBAs. We hypothesized that Medicaid expansion would be associated with workforce growth in BCBAs, a highly specialized and rapidly expanding cadre of workers who support children with ASD. We hypothesized a weaker relationship with the supply of child psychiatrists and no relationship with pediatricians, as these providers are less specialized in serving children with ASD and are overstretched with existing patient volume (Bridgemohan et al. 2018; R. K. McBain, Kofner, et al. 2019).
METHODS
Sampling Frame
This study examines Medicaid expansion legislation across all 50 U.S. states from 2008–2017, a period during which 31 states implemented Medicaid expansion. The District of Columbia was not included because of the limited geographic area and population, which has the potential to distort prevalence estimates. This study was deemed exempt from review by the lead author’s Institutional Review Board.
Measures
Medicaid Expansion.
We abstracted information on Medicaid expansion dates as documented by the Kaiser Family Foundation (Kaiser Family Foundation, 2020). We enumerated Medicaid expansion at the state level as a dichotomous exposure, with states yet to implement Medicaid expansion quantified as zero, and as one following year of enactment.
Workforce.
We abstracted annual data on health workforce supply from the Department of Health and Human Services’ Area Health Resource File (AHRF), which includes state-level numbers of child psychiatrists and pediatricians, updated on an annual basis. For pediatricians, we included only general pediatricians; we did not include developmental pediatricians, as they represent a qualitatively unique and small cohort of specialized providers. Board certified behavioral analyst (BCBA) workforce supply at the state level was abstracted from the Behavior Analyst Certification Board (BACB 2019), through which all BCBAs obtain certification and register to practice. For all provider types, we calculated providers per 100,000 children for each study year. The U.S. Census Bureau reports annual counts of children and adolescents 0–19 at the state level, which served as the denominator in this estimate (US Census Bureau 2017).
Covariates.
We included five additional measures as covariates, three of which have been previously demonstrated to correlate with the supply of behavioral health services: income per capita, race and ethnicity (Cook et al. 2017; Cummings et al. 2017). With regard to income per capita, we assessed median income per capita at the state level based on data reported annually by the U.S. Department of Commerce—measured as personal income, which includes wages, salary and other sources of non-cash income such as employer-provided insurance (U.S. Department of Commerce 2019). With regard to race/ethnicity, we included two covariates from the U.S. Census Bureau: first, percent black non-Hispanic, and second, percent Hispanic (US Census Bureau 2017). For each of these, we assessed the percentage of the total state population represented by these categories. Other minority categories (e.g. percent Asian American) collectively represent under 10% of the U.S. population and, due to statistical power considerations, were not included. As a fourth, time-varying covariate, we included an indicator variable for whether states had ratified state insurance mandates compelling insurers to provide coverage for ASD-related services (NCSL 2018). We considered this a potentially confounding health policy affecting generosity of autism-related services that occurred over the period of interest. Lastly, dummy variables (fixed effects) were included for each U.S. state and each year.
Statistical Analyses
After evaluating the distributional characteristics of variables, we made two adjustments to address non-linearities: first, we log-transformed outcome measures (providers per 100,000 children) to reduce right skew. Second, we introduced year fixed effects to account for non-linearity in the distribution of providers from 2008 to 2017.
Next, we estimated three separate multivariable linear regression models, one for each provider type, with state and year fixed effects. The purpose of these fixed effects is to model the relationship between workforce supply and passage of Medicaid expansion after accounting for secular within-state trajectories influenced geographic and time variance components (Meyer 2018). The independent variable of interest, Medicaid expansion, was incorporated with a one-year lag to allow sufficient time after ratification for Medicaid expansion to have an effect on workforce supply. More extended time lags were considered; however, we limited ourselves to this duration to minimize the potential for external policies and programs to influence results. To strengthen the modeling procedure, we also incorporated an extended baseline period encompassing six years of data prior to Medicaid expansion, consistent with best practices for an interrupted time series analysis design (Kontopantelis et al. 2015).
The model also included time-varying demographic covariates, as described above. We were unable, however, to account for potential differences in prevalence of ASD, apart from by proxy of child population, due to endogeneity concerns: specifically, that—while greater prevalence could lead to increased workforce supply—greater workforce supply could also lead to higher rates of ASD diagnoses.
To aid interpretation of results, we estimated predictive margins using Stata’s margins command. This provides predicted counts for each provider type based on fitted models based on the distribution of covariate values within the dataset. This approach allows easy translation of beta coefficients into outcomes estimates (i.e. expected numbers of providers) that are intuitively meaningful (Williams 2012).
Sensitivity Analyses
To assess pre-implementation time trends in workforce expansion, we employed an event study design (Abouk et al. 2019). The event study framework models the temporal effect Medicaid expansion at time points relative to year of adoption (Fry et al. 2018). We focused on the results from five years prior to enactment of the expansion through five years following enactment, to the extent these data were available. Models included state and year fixed effects and the same covariates included in our primary analysis. Results after year of enactment explain how the impact of Medicaid expansion has varied over time (Kothari and Warner 2007).
RESULTS
Descriptive Overview
From 2008 through 2017, the number of BCBAs per 100,000 children in the U.S. increased nationally from 4.81 to 29.88. The number of child psychiatrists per 100,000 children increased from 7.99 to 10.03, and the number of pediatricians per 100,000 children increased from 64.02 to 68.86. Over the same interval, 31 states passed Medicaid expansion.
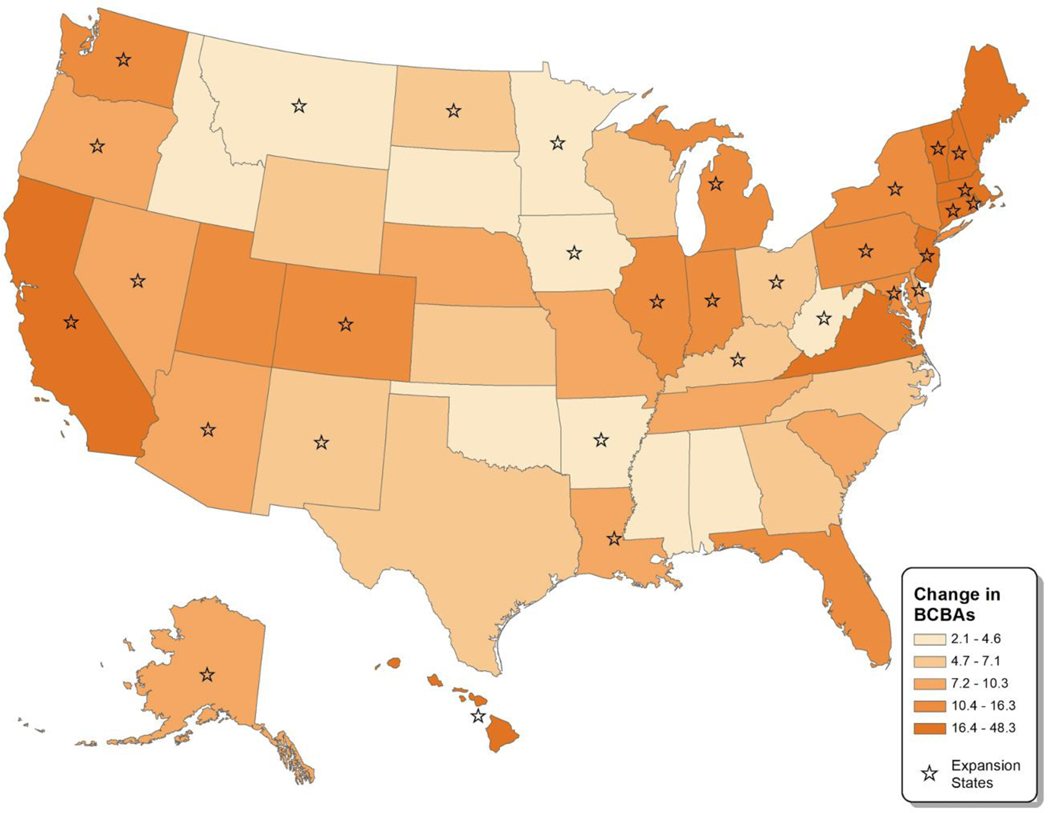
Details on the average number of BCBAs, child psychiatrists and pediatricians in states that did versus did not pass Medicaid expansion is outlined in Table 1. For both BCBAs and child psychiatrists, annualized growth in providers per 100,000 children was greater in expansion states both prior to and following expansion; however, these differences accelerated during the expansion period (2014–2017). For pediatricians, there was no discernable pattern. Figure 1 provides a visual representation of state-by-state BCBA growth during the 2014–2017 expansion period, separately for expansion and non-expansion states. It shows that most of the states with darker color—indicating more rapid BCBA growth—are expansion states.
Table 1.
Health Workforce Supply in Expansion vs. Non-Expansion States (2008–2017)
| Provider Category | Pre Medicaid Expansion | Medicaid Expansion Period | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 2008 | 2013 | Annualized Growth | 2014 | 2017 | Annualized Growth | |
| BCBAs | ||||||
|
| ||||||
| Non-expansion states (n=19) | 3.37 (3.37) | 9.23 (7.46) | 1.17 | 11.83 (9.55) | 19.59 (13.69) | 2.59 |
| Expansion states (n=31) | 5.05 (5.53) | 14.82 (13.05) | 1.95 | 19.62 (16.58) | 33.78 (27.34) | 4.72 |
|
| ||||||
| Child Psychiatrists | ||||||
|
| ||||||
| Non-expansion states (n=19) | 6.42 (2.77) | 7.10 (2.74) | 0.14 | 7.12 (2.90) | 7.48 (2.81) | 0.12 |
| Expansion states (n=31) | 9.25 (4.87) | 10.98 (5.86) | 0.35 | 11.08 (5.93) | 12.32 (7.09) | 0.41 |
|
| ||||||
| Pediatricians | ||||||
|
| ||||||
| Non-expansion states (n=19) | 49.07 (13.91) | 52.95 (14.08) | 0.78 | 53.52 (14.50) | 54.44 (15.05) | 0.31 |
| Expansion states (n=31) | 66.77 (24.55) | 71.05 (24.52) | 0.86 | 71.61 (24.91) | 72.19 (24.81) | 0.19 |
Footnote: “Pre- Medicaid Expansion” represents a time interval prior to implementation of Medicaid expansion in the U.S. (2008–2013), while the “Medicaid Expansion Period” represents a time interval (2014–2017) during which implementation of Medicaid expansion has taken place in 31 states. Workforce supply levels represented as the unadjusted, average state-level number of providers per 100,000 children. Parentheticals represent standard deviations. “Annualized Growth” is the unadjusted, average annual state-level growth in number of providers per 100,000 children during the time periods of interest.
Figure 1. Change in BCBAs per 100,000 Children during Medicaid Expansion (2014–2017).
Footnotes: “Change in BCBAs” represented as absolute change in number of BCBAs per 100,000 children at the state level during the Medicaid expansion period of 2014–2017.
Multivariate Regression Analyses
As shown in Table 2, multivariable linear regression models identified a significant relationship between Medicaid expansion and number of BCBAs per 100,000 children (β=0.086, 95%CI: 0.003, 0.168; p<0.05). Likewise, the analysis identified a significant relationship between Medicaid expansion and number of child psychiatrists per 100,000 children (β=0.046, 95%CI: 0.008, 0.085; p<0.05). We did not find evidence of a significant association between Medicaid expansion and the number of pediatricians over this period (p>0.05). Table 2 also shows the relationships between demographic variables and logged number of providers over time. The only significant finding was that growth in BCBAs was slower from 2008 to 2017 in communities with a larger Hispanic population, after adjusting for the other measures (β= −0.069, 95%CI: −0.118, −0.016; p<0.05). Furthermore, as documented in past findings, we observe a significant relationship between introduction of state insurance mandates and workforce supply of child psychiatrists (β= 0.046, 95%CI: 0.008, 0.085; p<0.05) (R. K. McBain, Cantor, Kofner, Callaghan, et al. 2020; R. K. McBain, Cantor, Kofner, Stein, et al. 2020). This relationship was not observed among BCBA, likely because of the interval restriction (2008–2017) compared to previous work looking over a longer time horizon.
Table 2.
Health Workforce Supply in Expansion vs. Non-Expansion States (2008–2017)
| BCBAs | Child Psychiatrists | Pediatricians | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Measure | β | 95% CI | β | 95% CI | β | 95% CI |
| Medicaid Expansion | 0.086* | 0.003, 0.168 | 0.046* | 0.008, 0.085 | −0.011 | −0.025, 0.003 |
| % African American | −0.073 | −0.173, 0.026 | −0.037 | −0.119, 0.042 | −0.005 | −0.039, 0.029 |
| % Hispanic | −0.071* | −0.126, −0.016 | 0.023 | −0.015, 0.062 | −0.013 | −0.025, 0.000 |
| Household Income | 0.012 | −0.004, 0.028 | −0.006 | −0.015, 0.002 | −0.003 | −0.007, 0.000 |
| State Insurance Mandate | 0.027 | −0.049, 0.102 | 0.048* | 0.008, 0.089 | 0.005 | −0.012, 0.021 |
Footnote:
p<0.05. Beta coefficients (β) represent the relationship between a one-unit change in the variable of interest and change in providers per 100,000 children. “Medicaid Expansion” is a dichotomous variable with 0 representing states that did not expand Medicaid and 1 representing states that did expand Medicaid. Household income measured in thousands ($USD). “State Insurance Mandate” is a dichotomous variable with 0 representing states that did not pass a state insurance mandate and 1 representing states that did pass a state insurance mandate.
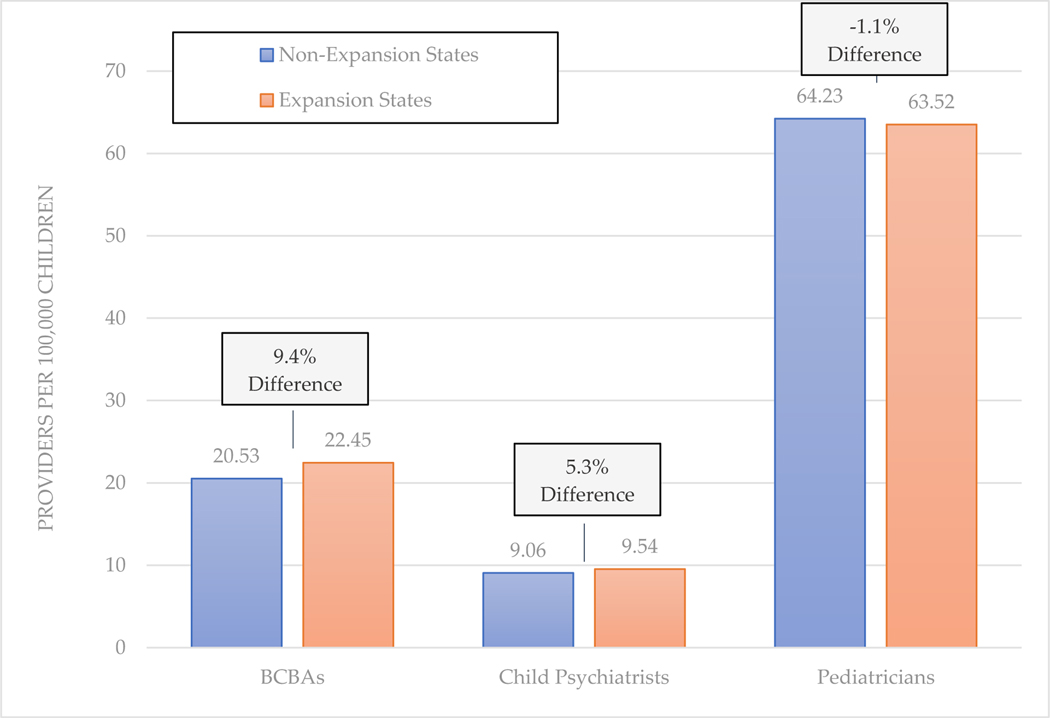
Figure 2 shows the expected number of providers in states with versus without Medicaid expansion policies as of 2017, based on marginal means from separate multivariable regression models. The largest difference is with respect to BCBAs, where expansion states would be expected to have 22.4 BCBAs per 100,000 children (95%CI: 19.5, 25.9) compared to 20.5 per 100,000 children (95%CI: 17.2, 24.4) in non-expansion states—a 9.4% difference. Among child psychiatrists, this difference was 5.3%: 9.5 child psychiatrists per 100,000 children (95%CI: 8.9, 10.2) in expansion states compared to 9.1 child psychiatrists per 100,000 children (95%CI: 8.4, 9.8) in non-expansion states. Lastly, among pediatricians, this difference was 1.1%: 63.5 child psychiatrists per 100,000 children (95%CI: 62.1, 65.0) in expansion states compared to 64.2 child psychiatrists per 100,000 children (95%CI: 62.5, 66.0) in non-expansion states.
Figure 2. Expected Number of Providers per 100,000 Children, 2017.
Footnote: Bars represent the number of providers estimated in non-expansion vs. Medicaid expansion states, based on multivariate regression models. Percent differences, in boxes, are calculated as the percent difference in number of providers per 100,000 children in Medicaid expansion states vs. non-expansion states.
Sensitivity Analysis
From the event study models, we found confirmatory results in two regards. First, in the baseline period looking back over the five years prior to implementation, there was no indication of a distortionary secular growth trend unaccounted for with indicator variables for year (p>0.05 in all instances). Second, we observed a significant effect of Medicaid expansion the year after implementation, both with regard to increased BCBAs (β=0.084, 95%CI: 0.014, 0.154, p<0.05) and child psychiatrists (β=0.042, 95%CI: 0.006, 0.080, p<0.05). We did not observe any significant relationship between Medicaid expansion and growth in pediatricians (p>0.05)
DISCUSSION
We examined the relationship between ACA Medicaid expansion and the workforce supply of BCBAs, child psychiatrists and pediatricians, routine providers of care for children with ASD. We found that Medicaid expansion was associated with an increase in BCBAs, a lesser increase in child psychiatrists, and was not associated with prevalence of pediatricians.
The marginal effect of Medicaid expansion was 1.9 additional BCBAs per 100,000 children in 2017. In the 31 states that passed Medicaid expansion as of 2017, where 49 million children reside, this would translate to approximately 900 additional BCBAs and more than 5,000 children with ASD served—based on an typical BCBA caseload 6–16 children (Dixon et al. 2016). Thus, while the impact of Medicaid expansion on this segment of the workforce was modest, the impacts are nevertheless important. We conclude a similar story for child psychiatrists: Medicaid expansion was associated with approximately 0.5 additional child psychiatrists per 100,000 children in 2017. Both findings are consistent with past evidence showing that the effect of legislation mandating insurance coverage for children with ASD had similarly weak but significant effects on workforce growth (R. K. McBain, Cantor, Kofner, Stein, et al. 2020). Further, it should be noted that the year that Medicaid expansion had its widest ranging effects—2014—included implementation of the early and periodic screening, diagnostic and treatment (EPSDT) benefit of Medicaid, which entitled beneficiaries under 21 to all health services deemed medically necessary (Autism Speaks 2020). From the vantage point of the analysis, these modifications both resulted in expansion of Medicaid eligibility and may each have contributed to the observed effects.
There are three conceptual pathways by which Medicaid expansion may have led to workforce growth in the year following state passage. First, particularly among BCBAs, ratification (or anticipation thereof) may have stimulated entry into this profession. Second, existing workforce members may have elected to relocate (e.g. back to their home state) or else assume multiple practice locations across state lines. Third, soon-to-graduate prospective members of the workforce may have decided to practice in settings with more favorable reimbursement policies.
Given that Medicaid expansion led to health insurance coverage for over 700,000 children in the U.S. (Hudson and Moriya 2017), the magnitude of workforce growth associated with these trends may be interpreted as unexceptional. However, there are several important factors to consider. First, our a priori hypothesis was that legislation focused on improving financial access to health services—achieved by extending health insurance coverage—may do little if providers are altogether absent in particular geographies (Olfson 2016; Policy 2014; Yang et al. 2014). Our results support this hypothesis. To the extent future studies confirm the results, a response that policymakers might consider would be legislation directly focusing on promoting workforce growth. This includes creating stronger financial incentives, reforming the graduate medical education system in the United States to encourage more entrants into fields such as psychiatry and pediatrics (Bärnighausen and Bloom 2009; Jackson et al. 2014; Wilensky and Berwick 2014), and expanding use of tele-education models such as Project ECHO by which primary care providers are trained by child psychiatrists to more effectively respond to children’s mental health needs in rural and underserved communities (American Academy of Child and Adolescent Psychiatry 2018).
Second, Medicaid expansion may have played a lesser role among children with ASD compared to other groups of children, as states often have multiple avenues by which children with disabilities receive subsidized healthcare (Musumeci and Chidambaram 2019). For example, over half of states cover children with significant disabilities through a home and community-based services (HCBS) waiver (Leslie et al. 2017). Lastly, it’s possible that states that have implemented Medicaid expansion are qualitatively different from those that have not—including being more progressive in expanding access to services for children with ASD. However, this seems unlikely to have played a role in our analyses, as we accounted for within-state time trends with quasi-experimental approaches (Wing et al. 2018).
In the case of pediatricians, we found no relationship between Medicaid expansion and growth of pediatricians. On the one hand, this finding is unsurprising, as pediatricians served as a useful reference point by which to compare other, specialized mental health workforce cadres: children with ASD represent a small proportion of pediatricians’ portfolio. On the other hand, to the extent that Medicaid expansion benefited uninsured children generally (not just those with ASD), one might have expected a positive relationship. However, roughly 1 in 5 pediatricians do not accept Medicaid as a form of payment or else cap their number of Medicaid enrollees (American Academy of Pediatrics 2012; Holgash and Heberlein 2019; Tang et al. 2018).
We note several study limitations. First, while our analyses are quasi-experimental, they are nevertheless observational and causal inference should be eschewed. Second, because we did not have exact locations of practices or level of provider engagement, unmet need for autism-related care may be higher or lower as a function of these factors. Third, we elected to examine the effect of Medicaid expansion one year after implementation. We restricted this to one year in order to reduce the likelihood that confounding policies and programs could shape results; however, the impact of Medicaid expansion on the workforce could expand or contract over a longer time horizon. Fourth, while there are other types of providers for children with ASD—for example, occupational therapists and registered behavioral technicians, we focused our attention on three highly-skilled professional groups for which we could identify high-quality longitudinal data. Future work should examine the effect of state Medicaid expansion on these other types of providers as data become available. Lastly, our measures set—including covariates—was restricted by availability of quality data. Additional indicators, such as prevalence estimates of ASD at county and state levels, would have further benefited these analyses; and future studies may be positioned to gather additional data tailored to specific provider groups.
CONCLUSION
We find that Medicaid expansion was associated with a modest but measurable increase in the supply of BCBAs in the U.S., a profession that is instrumental in providing behavioral services to children with ASD. The relationship between Medicaid expansion and the supply of child psychiatrists was smaller, and no significant relationship was observed with the supply of pediatricians. Our findings are consistent with evidence that the overall supply of child mental health workforce for children with ASD in the U.S. is insufficient, and they underscore the need for federal policies that directly address workforce shortages in many parts of the U.S.—akin to those highlighted in several recent reports (Hoge et al. 2013; R. McBain et al. 2021). In settings outside the U.S. with similar workforce constraints, a similar pattern of analyses should be considered to determine the impacts of existing legislation and need for additional policies.
Acknowledgements:
This study was supported by the National Institute of Mental Health (R01MH112760) and the Agency for Healthcare Research and Quality (R01HS025750).
REFERENCES
- Abouk R, Pacula RL, & Powell D (2019). Association Between State Laws Facilitating Pharmacy Distribution of Naloxone and Risk of Fatal Overdose. JAMA Internal Medicine, 179(6), 805–811. 10.1001/jamainternmed.2019.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. (2018). Project ECHO in Telepsychiatry. https://www.aacap.org/AACAP/Clinical_Practice_Center/Business_of_Practice/Telepsychiatry/Toolkit%20Videos/project_echo.aspx. Accessed 29 March 2021
- American Academy of Pediatrics. (2012). Pediatrician Participation in Medicaid and CHIP: National and State Reports. AAP.org. http://www.aap.org/en-us/professional-resources/Research/pediatrician-surveys/Pages/Pediatrician-Participation-in-Medicaid-and-CHIP-National-and-State-Reports.aspx. Accessed 11 November 2020
- Autism Speaks. (2020). Medicaid EPSDT. Autism Speaks. https://www.autismspeaks.org/medicaid-epsdt. Accessed 23 March 2021 [Google Scholar]
- BACB. (2019). Behavior Analyst Certification Board. https://www.bacb.com/. Accessed 5 December 2019
- Bärnighausen T, & Bloom DE (2009). Financial incentives for return of service in underserved areas: a systematic review. BMC health services research, 9, 86. 10.1186/1472-6963-9-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Candon MK, Xie M, & Mandell DS (2017). Effects Of State Insurance Mandates On Health Care Use And Spending For Autism Spectrum Disorder. Health Affairs, 36(10), 1754–1761. 10.1377/hlthaff.2017.0515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridgemohan C, Bauer NS, Nielsen BA, DeBattista A, Ruch-Ross HS, Paul LB, & Roizen N (2018). A Workforce Survey on Developmental-Behavioral Pediatrics. Pediatrics. 10.1542/peds.2017-2164 [DOI] [PubMed] [Google Scholar]
- Carbone PS, Behl DD, Azor V, & Murphy NA (2010). The Medical Home for Children with Autism Spectrum Disorders: Parent and Pediatrician Perspectives. Journal of Autism and Developmental Disorders, 40(3), 317–324. 10.1007/s10803-009-0874-5 [DOI] [PubMed] [Google Scholar]
- CDC. (2018, April 26). Data and Statistics | Autism Spectrum Disorder (ASD) | NCBDDD | CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/data.html. Accessed 2 July 2018 [Google Scholar]
- Cook BL, Trinh N-H, Li Z, Hou SS-Y, & Progovac AM (2017). Trends in Racial-Ethnic Disparities in Access to Mental Health Care, 2004–2012. Psychiatric Services (Washington, D.C.), 68(1), 9–16. 10.1176/appi.ps.201500453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Allen L, Clennon J, Ji X, & Druss BG (2017). Geographic Access to Specialty Mental Health Care Across High- and Low-Income US Communities. JAMA Psychiatry, 74(5), 476–484. 10.1001/jamapsychiatry.2017.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe JE, Crawford C, Angier H, O’Malley J, Gallia C, Marino M, & Gold R (2015). The Association Between Medicaid Coverage for Children and Parents Persists: 2002–2010. Maternal and child health journal, 19(8), 1766–1774. 10.1007/s10995-015-1690-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe JE, Marino M, Angier H, O’Malley JP, Crawford C, Nelson C, et al. (2015). Effect of Expanding Medicaid for Parents on Children’s Health Insurance Coverage. JAMA pediatrics, 169(1), e143145. 10.1001/jamapediatrics.2014.3145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon DR, Linstead E, Granpeesheh D, Novack MN, French R, Stevens E, et al. (2016). An Evaluation of the Impact of Supervision Intensity, Supervisor Qualifications, and Caseload on Outcomes in the Treatment of Autism Spectrum Disorder. Behavior Analysis in Practice, 9(4), 339–348. 10.1007/s40617-016-0132-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubay L, & Kenney G (2003). Expanding Public Health Insurance to Parents: Effects on Children’s Coverage under Medicaid. Health Services Research, 38(5), 1283–1302. 10.1111/1475-6773.00177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry CE, Nikpay SS, Leslie E, & Buntin MB (2018). Evaluating Community-Based Health Improvement Programs. Health Affairs (Project Hope), 37(1), 22–29. 10.1377/hlthaff.2017.1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooptu A, Moriya AS, Simon KI, & Sommers BD (2016). Medicaid Expansion Did Not Result In Significant Employment Changes Or Job Reductions In 2014. Health Affairs, 35(1), 111–118. 10.1377/hlthaff.2015.0747 [DOI] [PubMed] [Google Scholar]
- Hill BC, Coster D, & Black DR (2019). National and Regional Variation in Local Primary Care Physician Density Relative to the Uninsured and the Affordable Care Act. Inquiry: A Journal of Medical Care Organization, Provision and Financing, 56, 46958019873807. 10.1177/0046958019873807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge MA, Stuart GW, Morris J, Flaherty MT, Paris M, & Goplerud E (2013). Mental Health And Addiction Workforce Development: Federal Leadership Is Needed To Address The Growing Crisis. Health Affairs, 32(11), 2005–2012. 10.1377/hlthaff.2013.0541 [DOI] [PubMed] [Google Scholar]
- Holgash K, & Heberlein M (2019). Physician acceptance of new Medicaid patients. Washington DC: MACPAC. https://macpac.gov/wp-content/uploads/2019/01/Physician-Acceptance-of-New-Medicaid-Patients.pdf [Google Scholar]
- Hudson JL, & Moriya AS (2017). Medicaid Expansion For Adults Had Measurable ‘Welcome Mat’ Effects On Their Children. Health Affairs, 36(9), 1643–1651. 10.1377/hlthaff.2017.0347 [DOI] [PubMed] [Google Scholar]
- Jackson A, Baron RB, Jaeger J, Liebow M, Plews-Ogan M, Schwartz MD, & Society of General Internal Medicine Health Policy Committee. (2014). Addressing the nation’s physician workforce needs: The Society of General Internal Medicine (SGIM) recommendations on graduate medical education reform. Journal of General Internal Medicine, 29(11), 1546–1551. 10.1007/s11606-014-2847-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2020). Status of state action on the Medicaid expansion decision. Washington DC: Kaiser Family Foundation. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D [Google Scholar]
- Kontopantelis E, Doran T, Springate DA, Buchan I, & Reeves D (2015). Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ, 350, h2750. 10.1136/bmj.h2750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kothari SP, & Warner JB (2007). Chapter 1 - Econometrics of Event Studies. In Eckbo BE (Ed.), Handbook of Empirical Corporate Finance (pp. 3–36). San Diego: Elsevier. 10.1016/B978-0-444-53265-7.50015-9 [DOI] [Google Scholar]
- Leslie DL, Iskandarani K, Velott DL, Stein BD, Mandell DS, Agbese E, & Dick AW (2017). Medicaid Waivers Targeting Children With Autism Spectrum Disorder Reduce The Need For Parents To Stop Working. Health Affairs (Project Hope), 36(2), 282–288. 10.1377/hlthaff.2016.1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann C (2014). Clarification of Medicaid Coverage of Services to Children with Autism. Baltimore, MD: Centers for Medicare & Medicaid Services. https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-07-14.pdf [Google Scholar]
- McBain R, Eberhart N, Breslau J, Frank L, Burnam MA, Kareddy V, & Simmons M (2021). How to transform the U.S. mental health system. Santa Monica, CA: RAND Corporation. https://www.rand.org/pubs/research_reports/RRA889-1.html [Google Scholar]
- McBain RK, Cantor JH, Kofner A, Callaghan T, Stein BD, & Yu H (2020). Generosity of state insurance mandates and growth in the workforce for autism spectrum disorder. Autism: The International Journal of Research and Practice, 1362361320976744. 10.1177/1362361320976744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBain RK, Cantor JH, Kofner A, Stein BD, & Yu H (2020). State Insurance Mandates and the Workforce for Children With Autism. Pediatrics, 146(4). 10.1542/peds.2020-0836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBain RK, Kareddy V, Cantor JH, Stein BD, & Yu H (2019). Systematic Review: United States Workforce for Autism-Related Child Healthcare Services. Journal of the American Academy of Child and Adolescent Psychiatry. 10.1016/j.jaac.2019.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, & Yu H (2019). Growth and Distribution of Child Psychiatrists in the United States: 2007–2016. Pediatrics. 10.1542/peds.2019-1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J (2018, March 19). Poisson or Negative Binomial? Using Count Model Diagnostics to Select a Model. The Analysis Factor. https://www.theanalysisfactor.com/poisson-or-negative-binomial-using-count-model-diagnostics-to-select-a-model/. Accessed 29 June 2019 [Google Scholar]
- Musumeci MB, & Chidambaram P (2019, June 12). Medicaid’s Role for Children with Special Health Care Needs: A Look at Eligibility, Services, and Spending. KFF. https://www.kff.org/medicaid/issue-brief/medicaids-role-for-children-with-special-health-care-needs-a-look-at-eligibility-services-and-spending/. Accessed 11 November 2020 [Google Scholar]
- NCSL. (2018). State Insurance Mandates and the ACA Essential Benefits Provisions. https://www.ncsl.org/research/health/state-ins-mandates-and-aca-essential-benefits.aspx#Understanding. Accessed 13 April 2020
- Nolan R, Walker T, Hanson JL, & Friedman S (2016). Developmental Behavioral Pediatrician Support of the Medical Home for Children with Autism Spectrum Disorders. Journal of developmental and behavioral pediatrics: JDBP, 37(9), 687–693. 10.1097/DBP.0000000000000348 [DOI] [PubMed] [Google Scholar]
- Olfson M (2016). Building The Mental Health Workforce Capacity Needed To Treat Adults With Serious Mental Illnesses. Health Affairs, 35(6), 983–990. 10.1377/hlthaff.2015.1619 [DOI] [PubMed] [Google Scholar]
- Policy, B. on H. S. (2014). The Evolving Health Workforce. The Impacts of the Affordable Care Act on Preparedness Resources and Programs: Workshop Summary. National Academies Press; (US: ). https://www.ncbi.nlm.nih.gov/books/NBK241393/. Accessed 11 November 2020 [PubMed] [Google Scholar]
- Tang S-FS, Hudak ML, Cooley DM, Shenkin BN, & Racine AD (2018). Increased Medicaid Payment and Participation by Office-Based Primary Care Pediatricians. Pediatrics, 141(1). 10.1542/peds.2017-2570 [DOI] [PubMed] [Google Scholar]
- US Census Bureau. (2017). American Community Survey (ACS). https://www.census.gov/programs-surveys/acs. Accessed 21 February 2019
- U.S. Department of Commerce. (2019). Commerce Data Hub. Washington DC: U.S. Department of Commerce. https://data.commerce.gov/ [Google Scholar]
- Wilensky GR, & Berwick DM (2014). Reforming the financing and governance of GME. The New England Journal of Medicine, 371(9), 792–793. 10.1056/NEJMp1406174 [DOI] [PubMed] [Google Scholar]
- Williams R (2012). Using the Margins Command to Estimate and Interpret Adjusted Predictions and Marginal Effects. The Stata Journal, 12, 308–331. [Google Scholar]
- Wing C, Simon K, & Bello-Gomez RA (2018). Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annual Review of Public Health, 39(1), 453–469. 10.1146/annurev-publhealth-040617-013507 [DOI] [PubMed] [Google Scholar]
- Yang W, Williams JH, Hogan PF, Bruinooge SS, Rodriguez GI, Kosty MP, et al. (2014). Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. Journal of Oncology Practice, 10(1), 39–45. 10.1200/JOP.2013.001319 [DOI] [PubMed] [Google Scholar]