Abstract
Background
Body temperature is tightly regulated with hormonal and cellular metabolism for normal functioning; however perioperative hypothermia is common secondary to anesthesia and surgical exposure.
Prevention and maintaining body temperature should be started 1–2hrs before induction of anesthesia, to do this both active and passive warming system are effective to prevent complications associated with perioperative hypothermia.
Methods
The aim of this systematic review is to develop a clear clinical practice protocol in prevention and management of perioperative hypothermia for elective adult surgical patients.
The study is conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline 2020. After formulating clear criteria for the evidences to be included an appropriate method of searching was conducted by using the Pub Med, Google scholar and Cochrane library using the following MeSH terms: (inadvertent hypothermia AND anesthesia, hypothermia AND perioperative management and thermoregulation AND anesthesia) were used to draw evidences.
After a reasonable amount of evidences were collected, appraisal and evaluation of study quality was based on WHO 2011 level of evidence and degree of recommendation. Final conclusions and recommendations are done by balancing the benefits and downsides of alternative management strategies for perioperative management of hypothermia.
This systematic review registered with research registry unique identifying number (UIN) of “reviewregistry1253” in addition the overall AMSTAR 2 quality of this systematic review is moderate level.
Discussion
Preserving a patient's body temperature during anesthesia and surgery is to minimize heat loss by reducing radiation and convection from the skin, evaporation from exposed surgical areas, and cooling caused by the introduction of cold intravenous fluids.
Conclusion
Hypothermia is least monitored complication during anesthesia and surgery results cardiac abnormalities, impaired wound healing, increased surgical site infections, shivering and delayed postoperative recovery, and coagulopathies.
Keywords: ASA, American Society of Anesthesiology; RCT, Randomized Control Trail; FAW, Forced Air Warming
Keywords: Hypothermia, Inadvertent perioperative hypothermia, Perioperative management of hypothermia, Thermoregulation during anesthesia
Highlights
-
•
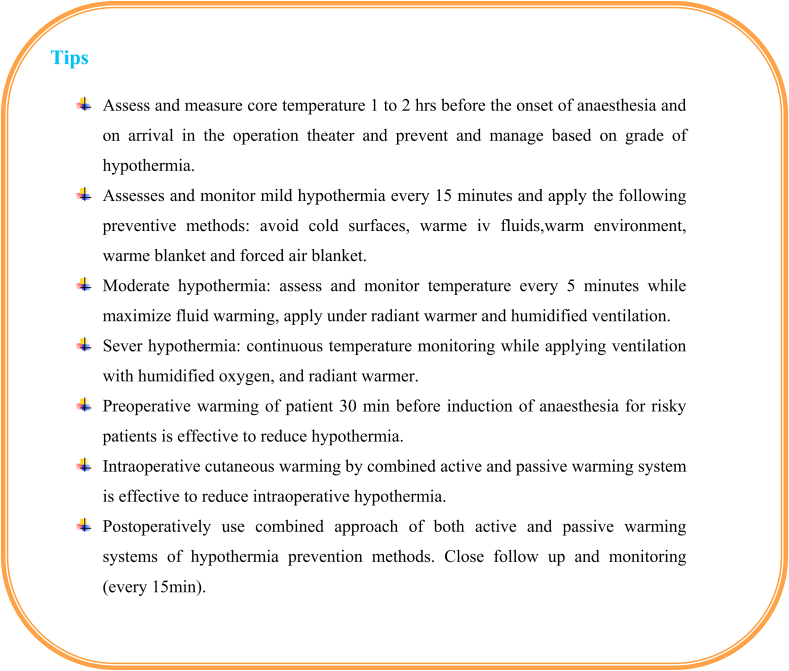
In elective surgical patient hypothrmia prevention and managment shoud started 1–2 h before the onset of anesthesia.
-
•
Mild, Moderate and Sever hypothermia should be monitor every 15,5 and continuous minutes respectively.
-
•
Combined active and passive warming system are effective to reduce in prevention and managment of perioperative hypothermia.
1. Background
Temperature is one of the five vital sign in human being's maintained within a low safety of margin lies between 36 and 37.5 °C in normal body temperature due to hormonal effects, Heat generation through cellular metabolism and physical activity [1,2].
Thermoregulation is done with in hypothalamus in combination of afferent input, central regulation, and efferent response. Efferent responses include behavioral and autonomic regulation. Behavioral regulation is the most powerful mechanism and requires conscious perception of body temperature,50% mediated by skin temperature [2,3].
Perioperative hypothermia is common occurrence due to core-to-peripheral redistribution of heat, anesthetic-related impaired thermoregulation and exposure to a cold environment [[4], [5], [6], [7]].
Hypothermia is defined as core body temperature below 36 °C(2) and is further classified as mild (34°C-36 °C), moderate (32°C-34 °C), and severe (<32 °C) [2], and most reliably monitoring sites are: pulmonary artery, distal esophagus, nasopharynx and tympanic membrane [3,6].
Perioperative heat loss is performed through radiation, Conduction, convection & evaporation among them radiation account 60% of total heat loss [6,8], Of these, convective heat loss to cold air and conductive heat loss to water are the most common mechanisms of accidental hypothermia(6).
Perioperative hypothermia causes many complications including cardiac abnormalities, impaired wound healing, increased surgical site infections, shivering and delayed postoperative recovery, increased ICU admissions,longer hospital stays and coagulopathies [9],as a result it increases economical crisis both on the patient and community at large [5,7,10].
2. Justification
Although Perioperative hypothermia is common, gives less emphasis to monitor complication during anesthesia and surgery(6, 11).Even with modern supportive care hospital mortality of patients with moderate or severe accidental hypothermia approaches 40% [12].
Maintaining a normothermic patient is quite challenging for clinician, especially for anesthetists and nurses, since it is their responsibility to install and monitor the devices in order to prevent hypothermia(1).
Studies shows that if hypothermia is left untreated, it results many adverse effects on the patient (prolonging anesthetic drug action, impair coagulation and platelet function, increases blood loss and transfusion requirements, increases wound infections, prolongs hospital stay, causes postoperative discomfort & shivering, increased oxygen consumption and increases heart rate, blood pressure, and plasma catecholamine levels) [7,13,14].
Active and passive warming systems are highly recommended to prevent hypothermia, so it is possible to use effectively the available resource with a protocol is crucial, as a result this systematic review have a nice contribution for better management and prevention of perioperative hypothermia.
The goal of preserving a patient's body temperature during anesthesia and surgery is to minimize heat loss by reducing radiation and convection from the skin, evaporation from exposed surgical areas, and cooling caused by the introduction of cold intravenous fluids(4,15).
3. Objective
-
•
To improve management of perioperative hypothermia for adult elective surgical patients.
-
•
To design clear institutional guideline for managing perioperative hypothermia in elective adult surgical patients.
4. Methods
The study is conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline 2020 [15]. After formulating clear criteria for the evidences to be included an appropriate method of searching was conducted by using the Pub Med, Google scholar and Cochrane library using the following MeSH terms: (inadvertent hypothermia AND anesthesia, hypothermia AND perioperative management and thermoregulation AND anesthesia) were used to draw evidences.
After a reasonable amount of evidences were collected, appraisal and evaluation of study quality was based on WHO 2011 level of evidence and degree of recommendation. Final conclusions and recommendations are done by balancing the benefits and downsides of alternative management strategies for perioperative management of hypothermia.
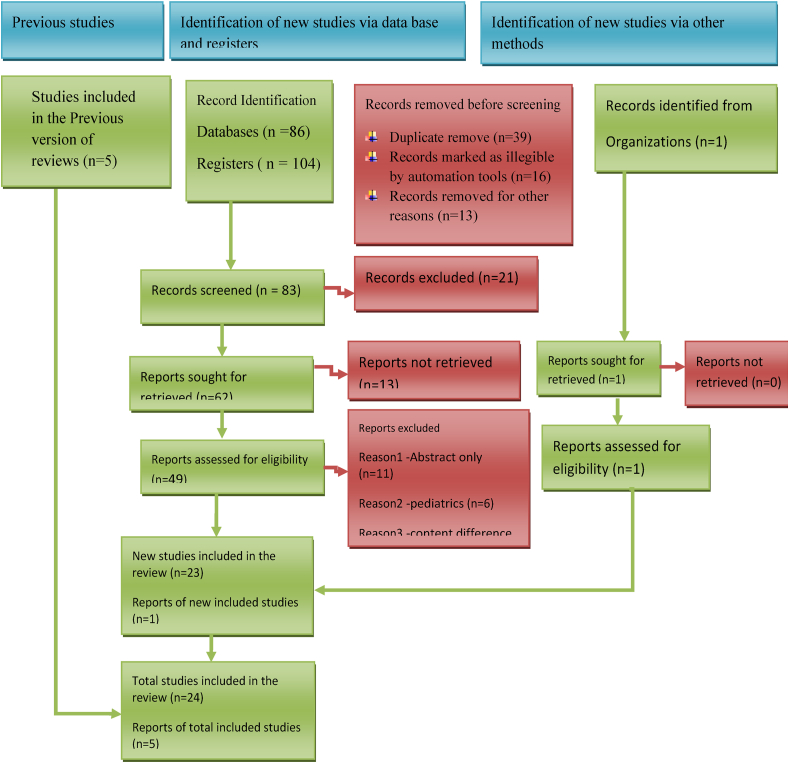
This systematic review registered with research registry unique identifying number (UIN) of “reviewregistry1253” in addition the overall AMSTAR 2 quality of this systematic review is moderate (Fig. 1).
Fig. 1.
Flow chart for selection of studies using 2020 PRISMA flow diagram.
4.1. Selection of studies
Papers fulfilling the following criteria were included in the study: studies presented as original articles, Meta analysis, systematic review, RCT and comparative studies on perioperative hypothermia management for adult elective surgical patients, inadvertent perioperative hypothermia, complication of hypothermia incidence and management studies written in English.
Studies on pediatric and geriatrics patient, surgery under induced hypothermia, studies where full articles were no longer available online were not selected to be included in the current review. All of the research articles that were identified from searches of the electronic databases were imported into the ENDNOTE software version X7.1 (Tomson Reuters, USA) and duplicates were removed. Before findings had begun, full length articles of the selected studies were read to confirm for fulfilling the inclusion criteria.
In this review, only those articles written in English language were considered for this review. Furthermore, after comprehensive and in-depth appraisal of literature, evaluation of quality was conducted according to the WHO 2011 level of evidence and degree of recommendation.
5. Areas of controversy
Perioperative hypothermia prevention and management has no a clear working protocol, regarding this evidences shows that warming irrigation fluids is not statistically significant difference to prevent intraoperative hypothermia between warmed and room fluid groups(16),But clinical practice guideline recommends that pre warmed irrigation fluids 38–40 °C is effective [3]. Another systematic review on the role of perioperative warming in surgery shows that warming both intravenous and irrigation fluids is effective in preventing perioperative hypothermia than non warming group [17].
Hypothermia management by forced air warming is more effective than resistive heating in preventing hypothermia(18),while a Cochrane systematic review concludes active body warming systems are more effective than passive warming systems, but no difference was observed between the different types of active warming systems in the effectiveness of management and prevention of hypothermia [14].
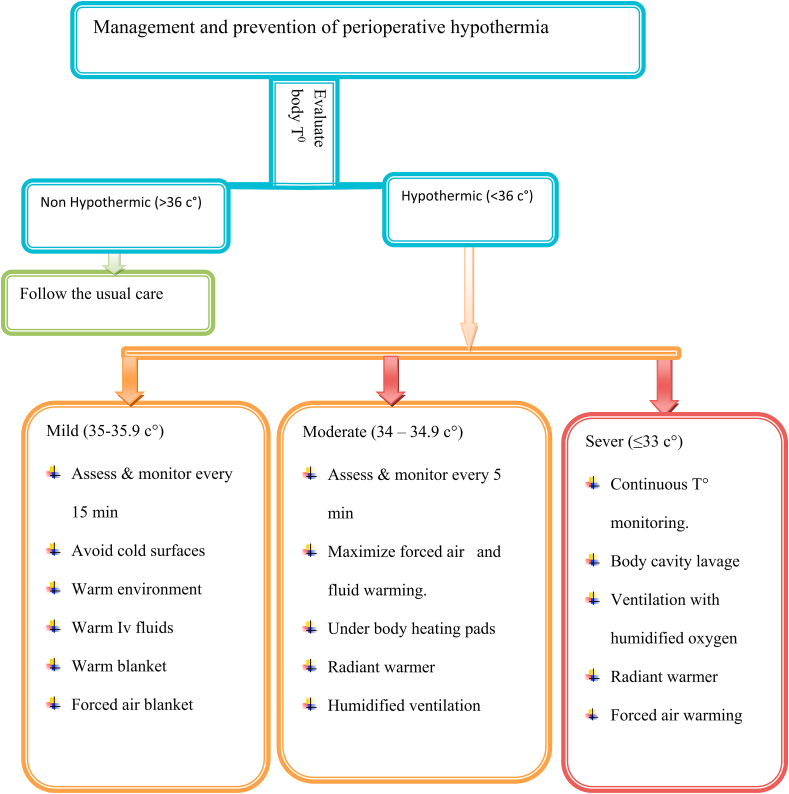
Classification of hypothermia it's associated complications is also another controversy in many literatures. A randomized control trial, classifies hypothermia as (Mild = 35-32 c°, Moderate = 32-28 c°, severe = 28-20 c° and profound = 20-14 c°) [6],but A Meta analysis study also classified in to three as mild (35–35.9 °C), moderate (34–34.9 °C) and severe (≤33 °C),which is strongly applicable & recommended(19).
6. Discussion
Perioperative hypothermia has many risk factors including head injury, ambient temperature of the OR, shock, spinal cord injury, autonomic nervous system dysfunction, coexisting illness, extremes of age, wet clothing, thyroid disease, adrenal disease, cardiac dysfunction, hepatic disease, cold intravenous fluids and blood products, long surgical exposure, type of surgery, general anesthesia>3hrs, epidural and spinal anesthesia and low preoperative temperature [[1], [2], [3],6,[20], [21], [22]].
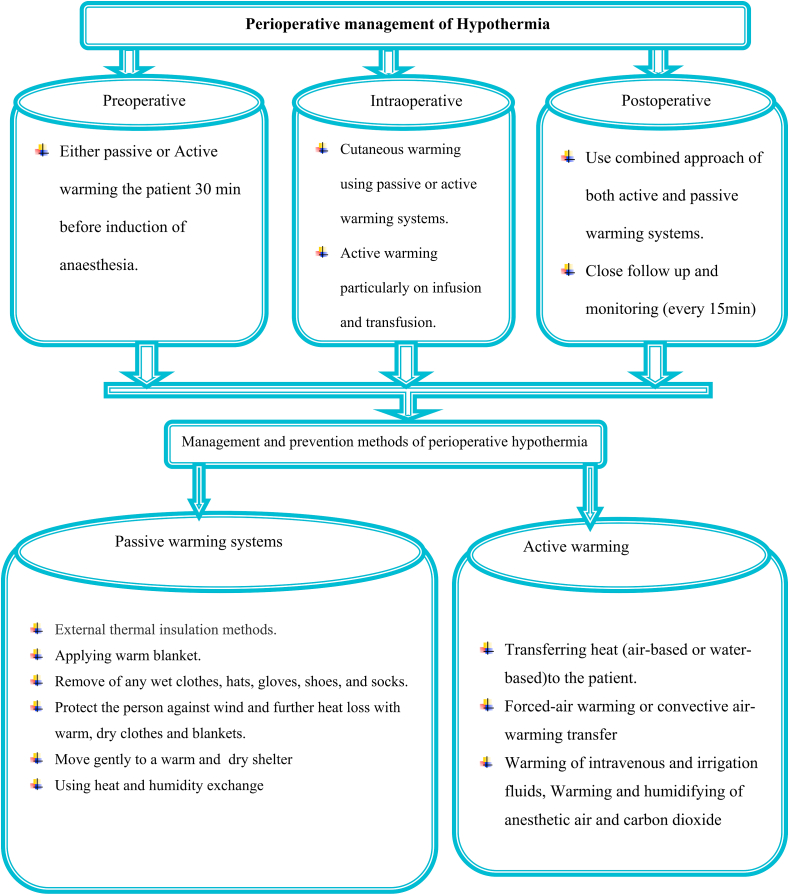
Preoperative hypothermia prevention and identification should be started 1–2 h before anesthesia administration. Intraoperative, temperature should be measured at least every 15 min [6,11].
High level evidences on prevention and management of perioperative hypothermia mainly depends on two systems.
-
i)
Passive warming systems
Thermal insulation is an external effective way of reducing radiating and convective heat loss via the skin allows intrinsic heat-generating mechanisms to counteract heat loss and usually more effective in mild hypothermia [4,6],includes increasing ambient temperature, isolation of body surface through clothes and a semi closed anesthesia circuit with low flow [14,16,19].
Passive mechanisms can be achieved by:
-
•
Augmenting the environmental temperature and applying a warm blanket.
-
•
Removal of any wet clothes, hats, gloves, shoes, and socks.
-
•
Protect the person against wind and further heat loss with warm, dry clothes and blankets.
-
•
Move gently to a warm dry shelter as soon as possible and rewarming the person with extra clothing.
-
•
Using heat and humidity exchanger
-
ii)
Active warming system:
Active warming system directly transfers heat to the patient through infrared light, electric blankets, mattresses or blankets with warm water circulation, forced-air warming or convective air-warming transfer, warming of intravenous and irrigation fluids, humidifying of anesthetic air and carbon dioxide [14,16,19].
Active warming systems can be performed:
-
•
Infrared lights, electric blankets, mattresses or blankets with warm-water circulation.
-
•
Forced-air warming or convective air-warming transfer,
-
•
Warming of intravenous and irrigation fluids,
-
•
Humidifying filtration and carbon dioxide (CO₂).
-
•
Self warming Blanket (barrier Easy Warm) it is independent of outsources power and it gives appropriate heat to the patient.
Perlman et al. shows that both passive and active external strategies are effective for mild hypothermia and can be easily applied. Radiant heaters, warming blankets, and humidified gases are effective for moderate hypothermia. Patient re warming is specifically recommended to patients with severe hypothermia [3,6].
A systematic review comparing the effectiveness of systemic warming of surgical patients with no warming concludes that patients on systemic warming reducing postoperative wound infection, shivering and perioperative blood loss [17,18].Another study on major upper abdominal surgery suggests combination of circulating water Mattress and forced air warming is equally effective in maintaining intraoperative core temperature with circulating water Garment [23,24].
A study comparing the efficiency of the thermal blanket and thermal mattress in the prevention of hypothermia during surgery concludes that the thermal mattress was more effective than the thermal blanket to prevent hypothermia in the intra and postoperative period [5]. Another study comparing prewarmed fluid vs. active fluid warming administration on the incidence of peri-operative hypothermia suggests that the administration of 1 L warmed fluid results in higher postoperative temperatures [25].
A Cochrane systematic review assessing effectiveness of perioperative warmed intravenous and irrigation fluids in preventing hypothermia during surgery suggests that warmed intravenous fluids keep patients significantly warmer than room temperature fluids, but warmed irrigation fluids has no statistically significant difference in body temperature between the warmed and room temperature fluid groups [1].
In order to decrease perioperative hypothermia patient should be actively pre warmed 20–30 min before surgery and the operation room ambient temperature should be at least 21 °C, transfusions rates greater than 500 mL/h should be warmed first and intraoperative irrigation fluids should be prewarmed to 38–40 °C [11].
Another study on thermal gown having the same base line body To demonstrated, thermal gown at 40 C° 30 min before anesthesia and throughout the surgical procedure shows 35.44 C° and 36.15 C° in the control group and in treatment groups respectively [20] (Table 1).
Table 1.
Methods of warming systems, description and mechanism of heat transfer(4, 6).
| Warming device | Description | Mechanism of Heat transfer |
|---|---|---|
| Warming blanket | Air delivered to variety of blankets at three settings: high (43 °C), medium (38 °C), low (32 °C). | Convection |
| Circulating Water garment | circulates water from the control unit to polymer hyper/hypothermia blankets. Manual settings: 4–42 °C; automatic: 30–39 °C | Conduction |
| Heated air mattress | Ineffective, because limited body surface area comes into contact with the mattress. | Conduction |
| Hot packs | Temperature at approximately 54.5 °C. Mean increase in temperature of 1.4 °C. | Conduction |
| Humidified gases | Delivery of warm, humidified gas, which can increase the core temperature by 0.5–0.65 °C/h. | Evaporation |
| Fluid warmer | Warmed fluids were found to increase the temperature by about 1.3 °C. | Conduction |
| Forced Air Warming Systems | Forcing warmed air through the warming device to the container, which is in direct contact with the patient's skin (usually a two-layer blanket). | Convection |
6.1. Methods of perioperative hypothermia prevention and management
Perioperative temperature fluctuations can be minimized through preoperative prevention and intra operative warming, is more effective, appropriate, and easier than treating hypothermia postoperatively [26].
6.1.1. Preoperative
Skin surface warming before induction of anesthesia does not significantly increase core temperature but increases peripheral tissue temperature and total body heat content. Skin surface warming for 30 min before induction of anesthesia, prevents redistribution hypothermia [3,11]26).
Any fluid, colloid or blood that runs greater than 500 ml/h should be warmed, preoperative temperature is below 36 °C, needs warming preoperatively [27].
According to the WHO keeping the patient warm is more important than warming blood,but warming of blood recommended when massive transfusions (adults: >50 ml/kg/h; children: >15 ml/kg/h) is required [3,6].
6.1.2. Intraoperative
The most important factor in determining intraoperative heat loss is the ambient operation room temperature(20).
Warm intravenous fluids appear to keep patients warmer during surgery than room temperature fluids and any fluid, colloid or blood that run greater than 500 ml/h should be warmed [18,20,28].
Patient core temperature should be measured continuously or every 15 min during surgery and ambient operation room temperature should be at least 21 °C for adult patients [3].
The amount of heat lost through the skin is proportional to the exposed body surface, so optimum temperature in the operation theater (23 °C and 26 °C in adults and infants, respectively)is the most critical factor that determines cutaneous losses through radiation, convection, and evaporation [3,5].
Both passive or active warming can achieve cutaneous warming, but passive insulation is the easiest method even if it is insufficient alone and should be used in combination with cotton blankets, surgical drapes, plastic sheets, and sleeping bags to be effective [3].
6.1.3. 1.3. Postoperative
Postoperative hypothermia should be treated by the administration of convective or conductive heat until normothermia is achieved [3]. Active warming should be continued into the postoperative period until the patient's body temperature is greater than 36 °C, and comfortably warm when transfer to recovery room/ward(20),of which,Forced air blankets and radiant heaters are most commonly used to warm patients in post-anesthesia recovery rooms [28,29].
7. Conclusion
Hypothermia is least monitored complication during anesthesia and surgery results cardiac abnormalities, impaired wound healing, increased surgical site infections, shivering and delayed postoperative recovery, and coagulopathies.
8. Strength
This systematic review develops optional management of perioperative hypothermia.
The study uses the latest PRISMA2020 diagram to find illegible studies(15).
9. Limitation
Bias of the study is not statically assessed.
Only full articles free online are included in this review.
Ethical approval
Not Required.
Sources of funding for your research
Would like to give my deepest gratitude to department of Anesthesia for the chance giving to search and develop this evidence based guideline.
Author contribution
All authors have participated in the stages of evidence searching, development, presentation and implementation of this evidence based guideline. Especially all authors critically appraise literature and present it to peers for discussion. They have participated in identifying areas of need within a perioperative period to produce appropriate recommendations.
Consent
Not required.
Registration of research studies
review registry 1253.
Guarantor
Samuel Debas Bayable.
Provenance and peer review
All authors deeply tries to address the comments given by the reviewer and editors.
Not commissioned eternal peer review
Netsanet temesgen (asst prof.)/Netsanettmsgn@gmail.com.
Helps us to restructure the flow of ideas.
Declaration of competing interest
No conflict of interest among authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.103059.
Contributor Information
Getamesay Demelash Simegn, Email: getademelash123@gmail.com.
Samuel Debas Bayable, Email: samueldebas88@yahoo.com, samueldebas1923@gmail.com.
Melaku Bantie Fetene, Email: bmelaku088@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Campbell G., Alderson P., Smith A.F., Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database Syst. Rev. 2015;(4) doi: 10.1002/14651858.CD009891.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Díaz M., Becker D.E. Thermoregulation: physiological and clinical considerations during sedation and general anesthesia. Anesth. Prog. 2010;57(1):25–33. doi: 10.2344/0003-3006-57.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bindu B., Bindra A., Rath G. Temperature management under general anesthesia: compulsion or option. J. Anaesthesiol. Clin. Pharmacol. 2017;33(3):306. doi: 10.4103/joacp.JOACP_334_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horosz B., Malec-Milewska M. Methods to prevent intraoperative hypothermia. Anaesthesiol. Intensive Ther. 2014;46(2):96–100. doi: 10.5603/AIT.2014.0019. [DOI] [PubMed] [Google Scholar]
- 5.Moysés A.M., Trettene AdS., Navarro L.H.C., Ayres J.A. Hypothermia prevention during surgery: comparison between thermal mattress and thermal blanket. Rev. Esc. Enferm. USP. 2014;48:228–235. doi: 10.1590/s0080-623420140000200005. [DOI] [PubMed] [Google Scholar]
- 6.Perlman R., Callum J., Laflamme C., Tien H., Nascimento B., Beckett A., et al. A recommended early goal-directed management guideline for the prevention of hypothermia-related transfusion, morbidity, and mortality in severely injured trauma patients. Crit. Care. 2016;20(1):1–11. doi: 10.1186/s13054-016-1271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yi J., Xiang Z., Deng X., Fan T., Fu R., Geng W., et al. Incidence of inadvertent intraoperative hypothermia and its risk factors in patients undergoing general anesthesia in Beijing: a prospective regional survey. PLoS One. 2015;10(9) doi: 10.1371/journal.pone.0136136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson W.C., Grande C.M., Hoyt D.B. CRC Press; 2007. Trauma: Resuscitation, Perioperative Management, and Critical Care. [Google Scholar]
- 9.Kurz A. Thermal care in the perioperative period. Best Pract. Res. Clin. Anaesthesiol. 2008;22(1):39–62. doi: 10.1016/j.bpa.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Yi J., Lei Y., Xu S., Si Y., Li S., Xia Z., et al. Intraoperative hypothermia and its clinical outcomes in patients undergoing general anesthesia: national study in China. PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0177221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torossian A., Bräuer A., Höcker J., Bein B., Wulf H., Horn E.-P. Preventing inadvertent perioperative hypothermia. Deutsches Ärzteblatt International. 2015;112(10):166. doi: 10.3238/arztebl.2015.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu M., Qi L. The related factors and countermeasures of hypothermia in patients during the anesthesia recovery period. Am. J. Tourism Res. 2021;13(4):3459. [PMC free article] [PubMed] [Google Scholar]
- 13.Dietrich W.D., Bramlett H.M. Therapeutic hypothermia and targeted temperature management for traumatic brain injury: experimental and clinical experience. Brain circulation. 2017;3(4):186. doi: 10.4103/bc.bc_28_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madrid E., Urrútia G., i Figuls M.R., Pardo‐Hernandez H., Campos J.M., Paniagua P., et al. Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database Syst. Rev. 2016;(4) doi: 10.1002/14651858.CD009016.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. Int. Ed. 2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horn E.P., Bein B., Böhm R., Steinfath M., Sahili N., Höcker J. The effect of short time periods of pre‐operative warming in the prevention of peri‐operative hypothermia. Anaesthesia. 2012;67(6):612–617. doi: 10.1111/j.1365-2044.2012.07073.x. [DOI] [PubMed] [Google Scholar]
- 17.Sajid M.S., Shakir A.J., Khatri K., Baig M.K. The role of perioperative warming in surgery: a systematic review. Sao Paulo Med. J. 2009;127:231–237. doi: 10.1590/S1516-31802009000400009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.John M., Crook D., Dasari K., Eljelani F., El-Haboby A., Harper C. Comparison of resistive heating and forced-air warming to prevent inadvertent perioperative hypothermia. Br. J. Addiction: Br. J. Anaesth. 2016;116(2):249–254. doi: 10.1093/bja/aev412. [DOI] [PubMed] [Google Scholar]
- 19.Sultan P., Habib A., Cho Y., Carvalho B. The Effect of patient warming during Caesarean delivery on maternal and neonatal outcomes: a meta-analysis. Br. J. Addiction: Br. J. Anaesth. 2015;115(4):500–510. doi: 10.1093/bja/aev325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bernardis RCGd, Siaulys M.M., Vieira J.E., Mathias L.A.S.T. Perioperative warming with a thermal gown prevents maternal temperature loss during elective cesarean section. A randomized clinical trial. Rev. Bras. Anestesiol. 2016;66:451–455. doi: 10.1016/j.bjan.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Cobb B., Cho Y., Hilton G., Ting V., Carvalho B. Active warming utilizing combined IV fluid and forced-air warming decreases hypothermia and improves maternal comfort during cesarean delivery: a randomized control trial. Anesth. Analg. 2016;122(5):1490–1497. doi: 10.1213/ANE.0000000000001181. [DOI] [PubMed] [Google Scholar]
- 22.Crossley S., Reid J., McLatchie R., Hayton J., Clark C., MacDougall M., et al. A systematic review of therapeutic hypothermia for adult patients following traumatic brain injury. Crit. Care. 2014;18(2):1–11. doi: 10.1186/cc13835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perez-Protto S., Sessler D., Reynolds L., Bakri M., Mascha E., Cywinski J., et al. Circulating-water garment or the combination of a circulating-water mattress and forced-air cover to maintain core temperature during major upper-abdominal surgery. Br. J. Anaesth. 2010;105(4):466–470. doi: 10.1093/bja/aeq170. [DOI] [PubMed] [Google Scholar]
- 24.Leung K., Lai A., Wu A. A randomised controlled trial of the electric heating pad vs forced‐air warming for preventing hypothermia during laparotomy. Anaesthesia. 2007;62(6):605–608. doi: 10.1111/j.1365-2044.2007.05021.x. [DOI] [PubMed] [Google Scholar]
- 25.Andrzejowski J., Turnbull D., Nandakumar A., Gowthaman S., Eapen G. A randomised single blinded study of the administration of pre‐warmed fluid vs active fluid warming on the incidence of peri‐operative hypothermia in short surgical procedures. Anaesthesia. 2010;65(9):942–945. doi: 10.1111/j.1365-2044.2010.06473.x. [DOI] [PubMed] [Google Scholar]
- 26.Sajid M.S., Shakir A.J., Khatri K., Baig M.K. The role of perioperative warming in surgery: a systematic review. Sao Paulo medical journal = Revista paulista de medicina. 2009;127(4):231–237. doi: 10.1590/S1516-31802009000400009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munday J., Hines S., Wallace K., Chang A.M., Gibbons K., Yates P. A systematic review of the effectiveness of warming interventions for women undergoing cesarean section. Worldviews Evidence-Based Nurs. 2014;11(6):383–393. doi: 10.1111/wvn.12067. [DOI] [PubMed] [Google Scholar]
- 28.Lee Y., Kim K. Optimal application of forced air warming to prevent peri-operative hypothermia during abdominal surgery: a systematic review and meta-analysis. Int. J. Environ. Res. Publ. Health. 2021;18(5):2517. doi: 10.3390/ijerph18052517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shaw C.A., Steelman V.M., DeBerg J., Schweizer M.L. Effectiveness of active and passive warming for the prevention of inadvertent hypothermia in patients receiving neuraxial anesthesia: a systematic review and meta-analysis of randomized controlled trials. J. Clin. Anesth. 2017;38:93–104. doi: 10.1016/j.jclinane.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.