Highlights
-
•
Thermoplastic masks are widely used in clinical routine on conventional LINACs.
-
•
Patient setup is more challenging on MR-LINAC systems.
-
•
lOn the MRIdian system, there is no dedicated holder for the anterior receiver coil.
-
•
We evaluated the suitability of a customised coil support system for MRgRT.
-
•
(MR) image uniformity measurements demonstrated improved image uniformity.
-
•
Fixed distancing between the receiver coils and the patient is possible.
-
•
This coil support system represents a solution for stable anterior coil placement.
Keywords: MR-guided radiotherapy, Head-and-neck tumours, Coil support, Patient immobilisation
Abstract
Magnetic resonance imaging (MR)-guided online adaptive radiotherapy is a promising technique in the field of radiation oncology providing excellent visualisation of soft-tissues, and allowing for online plan adaptation and tumour tracking. In order to facilitate the accurate dose delivery to the target volume while sparing healthy surrounding normal tissue in the brain or head-and-neck (H&N) region, precise patient immobilisation with good image quality is pertinent. Herein, we present a customised thermoplastic mask holder with an integrated anterior MR receiver coil support system for MR-guided online adaptive radiotherapy in the brain and head-and-neck region. The approved medical product was developed by Innovative Technologie Voelp (IT-V), Innsbruck, Austria. MR image uniformity measurements demonstrated improved image uniformity at the expense of decreased signal-to-noise ratio due to a more defined and larger distance between the anterior receiver coil and the phantom or patient. This integrated coil support system represents a practical solution facilitating stable and reproducible anterior coil placement while maintaining the thermoplastic mask holder functionality, a widely established immobilisation technique.
Introduction
Online adaptive MR-guided radiotherapy (MRgRT) has emerged as a promising development in the field of radiation oncology [1]. Generally, MRgRT allows for a superior visualisation of soft-tissues (compared to conventional cone beam computed tomography imaging), for online plan adaptation following anatomical and functional changes, and for automated gating [1], [2]. In particular, MRgRT might prove beneficial in fast-responding virus-induced tumours e.g. HPV-positive tumours or EBV-positive nasopharyngeal cancers [3]. Currently, there are two integrated hybrid MR linear accelerator (linac) systems (MR-linacs) commercially available: the Unity system (Elekta AB, Stockholm, Sweden) based on a 1.5 T MR scanner with a 7 MV linac and the MRIdian system (Viewray Inc., Oakwood, USA), based on a 0.35 T split MR scanner with a 6 MV linear accelerator [4], [5], [6].
Accurate and reproducible patient positioning is crucial for the accurate and safe treatment of tumours in the brain/head-and-neck region. Thermoplastic masks are widely used in clinical routine to reduce intrafractional motion during radiotherapy [7], [8].
Such masks can also be used on MR-linac systems, but patient setup is generally more challenging compared to conventional RT. This is due to the need for the placement of a relatively heavy (∼2.5 kg) MR receiver coil close to the patient and the limited space inside the bore. Furthermore, all equipment used in an MRI environment must be MRI compatible. Manufacturers are required to guarantee MRI compatibility. Our group recently published a multi-institutional joint review on patient and immobilisation procedures on MRgRT treatment platforms [9]. The Viewray MRIdian system has been in clinical use at our clinic since early 2020. In contrast to the Unity system, in which the anterior 4-element coil is positioned floating just above the patient mounted on a bridge, there is no holder integrated in the Viewray MR-linac system for the anterior receiver coil, which would make patient setup easier. To address this issue we evaluated the suitability of a customised coil support system for MRgRT. Additionally, we examined the potential influence of the receiver coil holder on MR image quality.
Description
We commissioned the MR-compatible thermoplastic mask holder with integrated coil support system, which was developed by Innovative Technologie Voelp (IT-V), Innsbruck, Austria at the 0.35 T MR-linac. The device was tested on site for imaging artefacts and no clinically relevant interference was observed during imaging (Fig. 1).
Fig. 1.
MR simulation scan acquired on the Viewray MRIdian system in a patient referred for treatment in the H&N region. No relevant artefacts were noted.
The different patient treatment setups have been previously described [9]. Briefly, there are two different set-ups for treatment of brain and H&N. For treatments of brain targets, a posterior receiver coil is placed on the couch and the HeadSTEP (HS) system (IT-V Innsbruck, Austria) is positioned on top of the posterior coil and mounted on the table using an indexing bar. The patient’s head is positioned using a pillow and fixated with a custom-made thermoplastic mask (IT-V, Innsbruck, Austria). The anterior receiver coil is then placed on the patient’s ventral surface and hooked into the novel HS Flex coil holder of the HeadSTEP system in order to avoid direct contact with the thermoplastic mask or the patient’s face. The setup for patients treated for H&N tumours is very similar. However, since the field of view for MR imaging of H&N tumours is usually located more caudally, the so called torso coil is used as the posterior receiver coil and the dedicated MR-compatible HeadSTEP system is mounted on top of it with the height-adjustable HS Flex coil holder for adequate positioning of the anterior receiver coil (Fig. 2, Fig. 3). Each receiver coil consists of radiolucent phased arrays with 2 × 5 channels, which are embedded in low-density foam and show relatively uniform beam attenuating characteristics [10]. All regulatory procedures for the modified immobilisation device with integrated coil support were undertaken by IT-V with approval obtained for the medical device prior to clinical use. The dedicated HeadSTEP system was modified to enable fixation of the coil holder in order to support the anterior (upper) receiver coil with adjustable height. The holding device is composed of glass fibre (Fig. 2, Fig. 3). For reproducibility, the thermoplastic mask system is indexed and fixed to the treatment couch and the anterior and posterior receiver coils are connected to each other with a fastener (Fig. 4, Fig. 5).
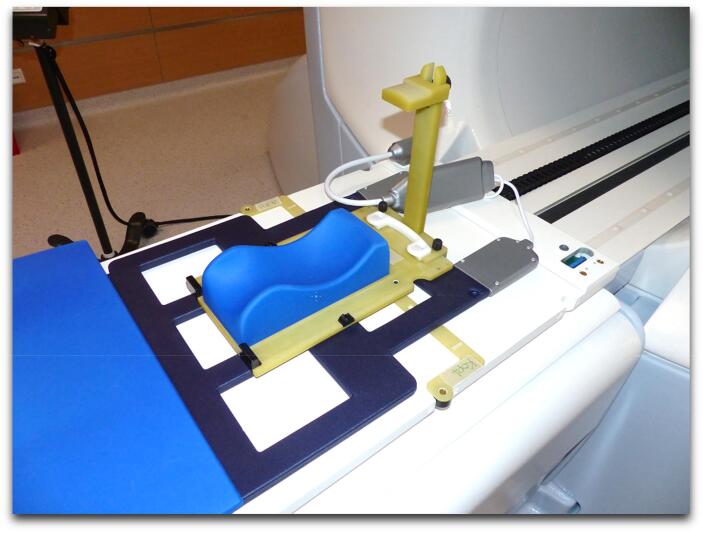
Fig. 2.
Novel receive coil support system with height adjustment (set-up for head and neck tumours).
Fig. 3.
Novel coil support system with height adjustment (set-up for brain tumours).
Fig. 4.
Example of patient setup with the novel coil support system for head and neck tumours.
Fig. 5.
Example of patient setup with the novel coil support system for brain tumours.
Influence on MR image quality
To assess the potential influence of the coil holder on MR image parameters, such as uniformity and signal-to-noise ratio, MR-images were acquired using a spherical water-filled polymethyl metacrylate (PMMA) phantom (diameter: 24.0 cm). This was done with and without the novel coil support system in place. The first set of MR images was acquired at a fixed distance (2.0 cm) from the phantom using the novel coil support system and the second set of MR images was acquired with placement of the anterior coil directly on the phantom. Images were acquired in the transversal, sagittal and coronal planes (Fig. 6). Image uniformity and signal-to-noise-ratio (SNR) were evaluated within a circular region of interest (diameter: 20.6 cm) centered in the phantom.
Fig. 6.
Axial (1 & 4), sagittal (2 & 5) and coronal (3 & 6) MR images of a water-filled spherical PMMA phantom (Window/Level in all images: 1000/850). Top row: images acquired without the receiver coil holder; the anterior receiver coil was placed directly on the phantom. Bottom row: images acquired with the coil holder in place, resulting in a defined distance (∼2 cm) between anterior coil and phantom surface.
Furthermore, in order to quantify the potential influence of the coil holder on the spatial integrity of the MR images (e.g. due to susceptibility-induced magnetic field changes close to the coil holder material), spatial integrity measurements were performed with a dedicated phantom, first without the coil holder, and second with the holder directly next to the phantom. The experimental setup allowed us to quantify the spatial integrity as close as 1.2 cm to the coil holder.
Results
For the uniformity and SNR evaluation, MR images were acquired in the transversal, sagittal and coronal plane without using the novel support device (see Fig. 6.1, 6.2 and 6.3). In contrast, Fig. 6.4, 6.5 and 6.6 depict image acquisition with the coil support system at a fixed distance of 2.0 cm. The image uniformity values (ideally 100) with/without the coil support system were 79.6/53.2, 83.3/47.6 and 83.4/71.1 in the transversal, sagittal and coronal planes, respectively. In contrast, the SNR values (ideally 100) with/without the coil support system were 47.7/67.2, 48.8/69.1, and 32.8/46.1 again in the transversal, sagittal and coronal planes, respectively.
The spatial integrity measurement showed a mean deviation between geometric features of the phantom in the MR image and the ideal position of these geometric features of (0.60 ± 0.32) mm (maximum = 1.74 mm) without the coil holder and (0.60 ± 0.33) mm (maximum = 1.73 mm) with the coil holder.
After implementation, the device has been used in 12 patients (8 brain and 4 H&N patients). An acquired MR-image of one representative H&N case is depicted in Fig. 1. There were no imaging artefacts related to the presence of the coil holder.
Discussion
In clinical routine, coil placement during H&N or brain tumour MRgRT can be challenging. There is a paucity of literature on immobilisation and support devices in the MRgRT setting. Many institutions use customised in-house developments to address this issue [9]. In addition, to our best knowledge, only one research group has published their initial experience in treating primary and recurrent head-and-neck cancers on the Viewray system [11], [12]. In their setting, radiotherapy was delivered on the Viewray 0.35 T MRI scanner with a tri-source Cobalt-60 system. From the patient immobilisation excerpt, the authors provide a detailed description of the placement of the bottom receiver coil. However, it remains unclear whether a coil support system was used for the anterior receiver coil, which, given its weight of approximately 2.5 kg, could potentially present some additional discomfort already experienced under the thermoplastic mask. In contrast, the anterior 4-element coil on the Elekta Unity system is positioned floating just above the patient mounted on a bridge [5]. As such, in another study of H&N patients treated on the Unity system, an additional support system was not required [13].
Given the lengthier treatment times for MRgRT versus treatments on a conventional linear accelerator, the placement of the anterior coil directly on the patient’s face could potentially compromise treatment tolerance. This is complicated by the potential presence of a tracheostoma or disease-related coughing. We were therefore interested in finding a practical solution that would improve stability and reproducibility of the anterior coil placement. With the newly developed support system, a stable placement of the upper receiver coil over the region of interest is possible. Patient-reported experience measures showed overall positive feedback.
Regarding MR image quality, qualitative and quantitative analysis consistently showed improved image uniformity at the cost of reduced SNR when using the coil holder. This is because the coil holder allows a fixed distance of the anterior receiver coil to the phantom/patient. As a result, the image uniformity is improved. However, the SNR is reduced, since an increased distance between receiver coil and phantom/patient results in a loss of measured signal strength while the noise background stays constant. This can be seen in the upper row of Fig. 6, where the signal is stronger near the upper coil (white areas).
No significant influence on the spatial integrity was found. Overall, the use of the coil holder does not negatively affect the MR image quality.
Currently, a number of prospective trials investigating MRgRT in H&N cancers have been initiated [2]. To the best of our knowledge, one such trial (MARTHA) is treating patients on the Viewray MRIdian system (NCT03972072).
Acknowledging one limitation of this report, only a small sample size of patients have been treated with the novel integrated coil support system so far, precluding any definitive statements. However, with the new system, a practical solution for placement of the upper receiver coil is now available, which could benefit other clinics with the 0.35 T MR-linac platform treating brain or H&N tumours
Conclusion
We introduced a novel coil support system for MRgRT in brain or H&N cancers at our clinic providing a practical solution for anterior receiver coil placement. No adverse influence on image quality was found. Currently, we have started recruiting patients to our institutional prospective registry study.
Furthermore, we have no existing conflicts of interest with Innovative Technologie Voelp (IT-V), Innsbruck, Austria. Payment was made in full for the medical device.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: SC and CB have received research grants and speaker fees/travel support from Viewray Inc (Oakwood Village, Ohio). MN has received research grants from Viewray (Oakwood Village, Ohio). All other authors declare no conflict of interest related to this work. Furthermore, we have no existing conflicts of interest with Innovative Technologie Voelp (IT-V), Innsbruck, Austria. Payment was made in full for the medical device.
References
- 1.Corradini S., et al. MR-guidance in clinical reality: current treatment challenges and future perspectives. Radiation Oncol. 2019;14(1):1–12. doi: 10.1186/s13014-019-1308-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boeke S., Mönnich D., van Timmeren J.E., Balermpas P. MR-guided radiotherapy for head and neck cancer: current developments, perspectives, and challenges. Front Oncol. 2021;11(March):1–9. doi: 10.3389/fonc.2021.616156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown E., Porceddu S., Owen R., Harden F. Developing an adaptive radiotherapy technique for virally mediated head and neck cancer. J Med Imaging Radiat Sci. 2013;44(3):134–140. doi: 10.1016/j.jmir.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Mutic S., Dempsey J.F. The ViewRay System: Magnetic Resonance-Guided and Controlled Radiotherapy. Semin Radiat Oncol. 2014;24(3):196–199. doi: 10.1016/j.semradonc.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Raaymakers B.W., Jürgenliemk-Schulz I.M., Bol G.H., Glitzner M., Kotte A.N.T.J., van Asselen B., et al. First patients treated with a 1.5 T MRI-Linac: Clinical proof of concept of a high-precision, high-field MRI guided radiotherapy treatment. Phys Med Biol. 2017;62(23):L41–L50. doi: 10.1088/1361-6560/aa9517. [DOI] [PubMed] [Google Scholar]
- 6.Winkel D., Bol G.H., Kroon P.S., van Asselen B., Hackett S.S., Werensteijn-Honingh A.M., et al. Adaptive radiotherapy: The Elekta Unity MR-linac concept. Clin Transl Radiat Oncol. 2019;18:54–59. doi: 10.1016/j.ctro.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilbeau L., Octave-Prignot M., Loncol T., Renard L., Scalliet P., Grégoire V. Comparison of setup accuracy of three different thermoplastic masks for the treatment of brain and head and neck tumors. Radiother Oncol. 2001;58(2):155–162. doi: 10.1016/S0167-8140(00)00280-2. [DOI] [PubMed] [Google Scholar]
- 8.Hess C.F., Kortmann R.D., Jany R., Hamberger A., Bamberg M. Accuracy of field alignment in radiotherapy of head and neck cancer utilizing individualized face mask immobilization: a retrospective analysis of clinical practice. Radiother Oncol. 1995;34(1):69–72. doi: 10.1016/0167-8140(94)01497-Q. [DOI] [PubMed] [Google Scholar]
- 9.Cuccia F., et al. Patient positioning and immobilization procedures for hybrid MR-Linac systems. Radiat Oncol. 2021;16(1):1–14. doi: 10.1186/S13014-021-01910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klüter S. Technical design and concept of a 0.35 T MR-Linac. Clin Transl Radiat Oncol. 2019;18:98–101. doi: 10.1016/j.ctro.2019.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen A.M., Hsu S., Lamb J., Yang Y., Agazaryan N., Steinberg M.L., et al. MRI-guided radiotherapy for head and neck cancer: initial clinical experience. Clin Transl Oncol. 2018;20(2):160–168. doi: 10.1007/s12094-017-1704-4. [DOI] [PubMed] [Google Scholar]
- 12.Chen A.M., Cao M., Hsu S., Lamb J., Mikaeilian A., Yang Y., et al. Magnetic resonance imaging guided reirradiation of recurrent and second primary head and neck cancer. Adv Radiat Oncol. 2017;2(2):167–175. doi: 10.1016/j.adro.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonald B.A., Vedam S., Yang J., Wang J., Castillo P., Lee B., et al. Initial Feasibility and Clinical Implementation of Daily MR-Guided Adaptive Head and Neck Cancer Radiation Therapy on a 1.5T MR-Linac System: Prospective R-IDEAL 2a/2b Systematic Clinical Evaluation of Technical Innovation. Int J Radiat Oncol Biol Phys. 2021;109(5):1606–1618. doi: 10.1016/j.ijrobp.2020.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]