Abstract
The COVID-19 pandemic has caused the death of over half a million Americans, leaving in its wake widespread grief and despair. Using national survey data (n = 1998) and a treatment-weighting strategy, this study examines how COVID-19 bereavement associates with depressive symptoms and binge drinking. After adjustment for non-random exposure to COVID-19 bereavement, I find that respondents who have lost someone close to them to the virus report greater depressive symptomology and more frequent binge drinking. Among essential workers, the loss of a close tie to COVID-19 exacerbates these associations, with bereavement posing stronger effects for depressive symptoms and binge drinking for members of this group. The implications of these findings for the long-term mental health of the bereaved and those most vulnerable to the virus are discussed.
Keywords: United States, COVID-19, Bereavement, Essential workers, Psychological distress, Binge drinking
1. Introduction
In October 2021, the United States passed the grim milestone of 700,000 deaths due to COVID-19. The magnitude of this unprecedented loss of life will be felt for years to come, particularly among those who have lost family or friends to the virus. Initial estimates of COVID-19 bereavement projected that 1.7 million Americans would experience the death of a child, spouse, parent, sibling, or grandparent (Verdery et al., 2020). However, these estimates were based on forecasts of 190,000 deaths from the virus, placing the current figure closer to 6.3 million Americans who have lost a family member to COVID-19. Still, even these estimates overlook the considerable number of people who have lost close friends, colleagues, and neighbors to the virus, suggesting that the number of bereaved in the United States is substantially larger than these estimates.
Mental health problems have proliferated in the United States since the start of the pandemic (Czeisler et al., 2020). As health researchers have begun to examine the social and economic fallout of the virus, evidence suggests that a number of pandemic-related stressors influence mental health. Isolation stemming from social distancing protocols (Bierman & Schieman, 2020), material hardships induced by the sudden plunge into a global economic recession (Bierman et al., 2021; Donnelly & Farina, 2021), and anxiety about potential exposure to the virus (Sloan et al., 2020, pp. 1–46; Zheng et al., 2021) have all been linked to increased psychological distress. Of equal importance is understanding how the loss of a loved one to the virus also impinges upon mental health. The death of a significant other stands as one of the more devastating life events a person can experience. Abundant evidence demonstrates that the loss of a close tie can have lasting, deleterious effects on mental health (Stroebe et al., 2007; Umberson & Chen, 1994). COVID-related deaths may be especially traumatizing because these deaths are abrupt, unexpected, and premature. In many instances, hospital safety guidelines prohibited friends and family from saying “goodbye” in-person (Wakam et al., 2020). Subsequent mourning has unfolded in relative isolation absent many of supports on which people generally rely to cope with bereavement (Carr et al., 2020).
Clear-cut assessments of the relationship between COVID-19 bereavement and psychological distress are complicated by the finding that this event does not occur at random in the United States. Emerging evidence indicates that Black and Latinx people are substantially more likely to know someone who has been hospitalized or died from the virus than other racial-ethnic groups (Funk & Tyson, 2021). This issue raises empirical concerns in terms of both confounding and selection effects. Thus, as a primary objective, this study examines whether the loss of a close tie to COVID-19 is associated with depressive symptoms and binge drinking after extensive adjustment for non-random exposure to bereavement. It is also plausible that the link between COVID-related bereavement and mental health varies across the population. Stress researchers contend that exposure to a traumatic event in one's social network can cause a person to persistently ruminate on their own susceptibility to it, in turn, eroding mental health and well-being (Pearlin & Bierman, 2013). Consequently, as a secondary objective, this study also explores how a group more frequently exposed to the virus is affected by bereavement: essential workers. Findings elucidate how the loss of a close tie to COVID-19 undermines mental health, particularly among those most vulnerable to the virus.
2. Background
2.1. Bereavement as a traumatic life event
The loss of a loved one represents one of the most profound and emotionally distressing events a person can experience. In the stress process paradigm (Pearlin & Bierman, 2013), the death of a significant other is conceptualized as a traumatic life event. As Pearlin et al. (2005:2010) describe, these traumas “are etched deeply into the emotions and consciousness of people, their initial impact echoing across time.” It follows that these events typically set in motion a cascade of secondary stressors, including the loss of valued social roles (e.g., parent, spouse), economic precarity, and strained relationships (Pearlin et al., 2005; Stroebe et al., 2007).
Much of the literature on bereavement has focused on how people experience the death of close family members including spouses (Carr, 2004, 2009; Umberson et al., 1992), parents (Brewer & Sparkes, 2011; McLeod, 1991; Umberson & Chen, 1994), and children (Floyd et al., 2013; Lehman et al., 1987). While there is some variation depending on the quality of the relationship to the deceased, a recurrent finding in this literature is that the death of a significant other fosters psychological distress. These include both internalizing forms of distress like depressive symptoms (McLeod, 1991; Umberson et al., 1992) and anxiety (Stroebe et al., 2007), as well as externalizing forms of distress like increased alcohol consumption (Umberson & Chen, 1994) and anger (Carr, 2009). Although the period immediately following loss is typically the most emotionally intense, the effects of bereavement can be long-lasting, reappearing for years after the event (Johnson et al., 1986). While COVID-related deaths share certain similarities to the losses people have endured due to natural disasters and other mass trauma, the distinctive features of COVID-related deaths are worth noting as they may impede the grieving process, and in turn, prompt concerns about lingering mental health issues (Carr et al., 2020).
2.2. The unique aspects and uneven distribution of COVID-19 bereavement
Following dramatic reductions in mortality from infectious disease in the second half of the twentieth century, recent decades have witnessed a majority of people in the United States dying later in life due to chronic ailments (McKinlay & McKinlay, 1977). In many instances, these deaths can be forecasted months, and sometimes years in advance, providing individuals and their families with the opportunity to put their affairs in order and say goodbye on their own terms. The COVID-19 pandemic has upended these patterns of mortality. Among those who have died from the virus, the time from symptom onset to death spans mere weeks (median = 19 days) (Zhou et al., 2020). Due to the insidious nature of the virus, these deaths were unexpected and abrupt, creating a uniquely traumatizing experience for the bereaved (Umberson, 2017).
As much as COVID-19 has transformed other aspects of social life, it has dramatically reshaped the traditional rites and rituals of mourning. With rare exceptions, hospital safety guidelines prevented the bereaved from visiting with a loved one in-person prior to their death. Indeed, for many, these final goodbyes occurred over smart phones and tablets with the assistance of healthcare workers (Wakam et al., 2020). In a similar manner, the grieving process has been fundamentally altered. As a result of social distancing protocols, the bereaved mourn in relative seclusion, unable to access many of the social supports on which one might normally rely during times of loss (Carr et al., 2020). Limited research on COVID-19 bereavement finds that personal loss from the virus is linked to greater depressive symptomology among older adults (Wang et al., forthcoming), and further, that losses attributable to the virus cause significantly more grief than those stemming from natural causes (Eisma et al., 2021).
Central to the stress process is the notion that a person's location in the social hierarchy influences both the number and severity of stressors they face (Pearlin & Bierman, 2013). Individuals who occupy lower statuses—including members of marginalized racial-ethnic groups and those of lower socioeconomic status—are subject to inordinate amounts of stress. Providing support for this contention, there is now a preponderance of evidence that COVID-19 mortality is unevenly distributed across society in ways that further disadvantage marginalized groups. Black and Latinx people comprise a disproportionate number of COVID-related deaths in the United States (Artiga et al., 2020; Bassett et al., 2020). There is also some indication that American Indians are overrepresented among COVID-19 decedents relative to their share of the population (Artiga & Orgera, 2020). These racialized patterns are fundamentally rooted in systemic racism. As a result of historic economic marginalization, racial-ethnic minority groups are overrepresented among essential workers, placing them at greater risk of infection (Rogers et al., 2020; Williams et al., 2020). Further compounding racial-ethnic disparities in infection, many of these individuals carry the virus home with them to hyper-segregated communities (Massey & Denton, 1993).
Just as COVID-19 mortality disproportionately affects members of structurally disadvantaged groups, the loss of a significant other to the virus is also not a random event. Although research on network exposure to COVID-related deaths is more limited, a Pew Research Center report released in March 2021 found that 67% of Americans know someone who has either been hospitalized or died from the virus (Funk & Tyson, 2021). Closer inspection of this figure reveals racial-ethnic patterns in exposure that map onto those observed for COVID-19 mortality. Compared to 59% of Asian Americans and 64% of Whites, a more substantial 78% of Black and 74% of Hispanic respondents report knowing someone who has either been hospitalized or died from the disease. Other segments of American society may similarly have greater connectivity to people who have died from COVID-19. For instance, given their repeated exposure to the virus, as well as the overrepresentation of Black and Latinx people among this group, it is plausible that essential workers may also be more likely to know someone who has died from COVID-19.
The unequal social distribution of COVID-19 bereavement in the U.S. is an important consideration when assessing the relationship between personal loss and psychological distress. Unadjusted analyses of the association between COVID-19 bereavement and mental health may reflect underlying, qualitative differences that exist between those who have and have not experienced loss due to the virus (i.e., selection effects). Furthermore, because several factors that influence exposure to COVID-19 bereavement may also increase one's risk for depressive symptoms or alcohol use, confounding is another potential threat to estimates of the association between bereavement and these outcomes. Using a design that is sensitive to these concerns, I ask the following:
R1: After adjustment for differential exposure to COVID-19 bereavement, is the loss of a close tie associated with depressive symptoms and binge drinking?
2.3. Differential effects of COVID-19 bereavement: the case of essential workers
The coronavirus pandemic precipitated a global economic crisis. In just under a month's time, the unemployment rate in the U.S. eclipsed the peak of the Great Recession, topping 14% in April 2020 (Kochhar, 2020). As a corollary, Americans have experienced growing economic privation. Approximately one-in-four adults report difficulty paying their bills, while one-third have accessed retirement or savings accounts to sustain their households (Parker et al., 2020). The United States government has provided little financial relief to its citizens since the start of the pandemic. By privileging the economy over human life (Lopez & Neely, 2021), many Americans have been forced to choose between personal safety and economic survival. For essential workers—or those in occupations designated as vital for the continuing function of the economy—this calculus weighed continued employment against a high risk of exposure.
There is considerable heterogeneity in terms of salary, job security, and benefits across essential workers. While some (e.g., doctors) have access to greater resources, many of these workers are economically disadvantaged; employed in lower wage occupations including jobs in agriculture, grocery/retail, food and cleaning services, and manufacturing (Blau et al., 2020; Rogers et al., 2020). Black and Latinx people are overrepresented among essential workers, and in particular, in high-contact positions (e.g., nursing homes, home healthcare) where employees are at greatest risk of being exposed to the virus (Rogers et al., 2020; Williams et al., 2020). Men are also more likely than women to work in industries considered essential (Blau et al., 2020). These differences aside, essential workers are united by the fact that merely by showing up for work they are placing themselves and their families in danger of contracting, and potentially dying from, COVID-19 (Clouston et al., 2021). Underscoring the risk faced by this group, a study of California death records found that excess mortality has been considerably higher in economic sectors considered ‘essential’ since the start of the pandemic (Chen et al., 2021). Given the persistent strain under which these workers find themselves, it is perhaps unsurprising that substance use and suicidal ideation are more prevalent among members of this group (Czeisler et al., 2020).
It becomes increasingly difficult to deny one's own mortality when confronted by the premature death of family, friends, and significant others (Umberson, 2017). Recent theoretical elaborations of the stress process posit that exposure to traumatic events via one's social network can lead to rumination on one's own susceptibility to an event, in turn, fostering deleterious mental health outcomes (Pearlin & Bierman, 2013). Consistent with the differential vulnerability hypothesis, which posits that a person's social status can exacerbate the effects of a stressor on mental health (Kessler, 1979), essential workers may experience greater distress following the loss of a close tie to COVID-19 owing to their elevated concerns about contracting the virus (Sloan et al., 2020, pp. 1–46). Stated more formally, I ask:
R2: To what extent does the association between COVID-19 bereavement and depressive symptoms/binge drinking vary by essential worker status?
3. Data and methods
3.1. Data
This study uses data collected from 2000 Americans between July 8 and October 13, 2020. The research firm Qualtrics was contracted by the author to recruit a sample using a quota-based approach designed to approximate the racial-ethnic, sex, income, and educational composition of the American population based on U.S. Census Bureau estimates. Qualtrics fills each quota by purposively recruiting respondents from online panels consisting of hundreds of thousands of people representing different segments of the population. Qualtrics panels have been used in a variety of recent epidemiological research, including the Centers for Disease Control's Morbidity and Mortality Weekly Report (Czeisler et al., 2020). Respondents who met selection criteria (American citizens over 18 years of age) were sent study invitations to participate in the online survey. A total of 82,354 individuals were contacted in order to generate the study's sample of 2000 respondents. After removing cases with missing data on key study variables (n = 2), 1998 respondents were retained in the sample. Because respondents were not recruited at random, there is no “response rate” in the traditional sense. Accordingly, although the composition of the sample compares favorably to 2016 Current Population Survey Benchmarks (see Appendix A), its self-selected nature poses clear limitations in terms of both generalizability and the precision of estimates. In a similar vein, while the demographic characteristics of essential workers in the sample roughly parallel those of essential workers in the general population (see Appendix B) based on Current Population Survey estimates (McNicholas & Poydock, 2020), it must be emphasized that this is a non-representative sample. I elaborate further on the implications of these issues for study findings in the discussion section.
3.2. Measures
Psychological Distress. To provide a more complete accounting of the toll of COVID-19 bereavement on mental health, this study examines both internalizing and externalizing forms of psychological distress (Pearlin & Bierman, 2013; Rosenfield et al., 2005). To capture internalizing forms of distress, depressive symptoms are measured using the Center for Epidemiological Studies of Depression (CES-D) Scale (Levine, 2013; Radloff, 1977) seven-item short form. CES-D items ask about symptoms experienced over the course of the past week (e.g., feeling depressed, restless sleep). The internal consistency of the CES-D in the present sample was = .91. Response categories range from 0 = rarely or none of the time (<1 day), to 3 = most or all of the time (5–7 days). Responses on these items were summed to create a weighted count of depressive symptoms (range = 0–21). In order to gauge externalizing forms of distress, respondents’ frequency of binge drinking is assessed using an item from the National Longitudinal Study of Adolescent to Adult Health. This item asks, “During the past 12 months, on how many days did you drink five or more alcoholic drinks in a row?” with response categories including, none (=0), 1 or 2 days in the past 12 months (=1), once a month or less (=2), 2 or 3 days a month (=3), 1 or 2 days a week (=4), 3–5 days a week (=5), and every day or almost every day (=6).
COVID-19 Bereavement. The death of a significant other from COVID-19 was assessed by a single item that asked, “Have you lost someone close to you due to COVID-19” (1 = yes).
Essential Worker Status. Respondents’ designation as an essential worker was self-reported in response to an item that queried, “Are you considered an essential worker?” (1 = yes).
3.3. Covariates
To adjust for the potentially confounding effects of sociodemographic factors in estimating the association between bereavement and depressive symptoms/binge drinking, an identical set of control variables are included in both treatment and outcome models. Race-ethnicity is categorized as American Indian/Alaska Native (=1), Asian (=1), Black/African American (=1), Hispanic/Latinx (=1), Other (=1) and White (=0). Sex is coded as female (=1) and male (=0). Respondents' sexual orientation is measured as gay/lesbian (=1), bisexual (=1), other (=1), and straight (=0). Age is categorized as 18–24 (=1), 25–34 (=1), 35–44 (=1), 45–54 (=1), 55–65 (=1), and 65+ years old (=0). Relationship status is coded as single (=1), in a committed relationship (=1), divorced (=1), widowed (=1), separated (=1), and married (=0). Education is categorized as less than high school diploma (=0), high school diploma/GED (=1), some college (=1), Associate's degree (=1), Bachelor's degree (=1), and graduate degree (=1). Annual household income is measured as less than $25,000 (=0), $25,000-$49,999 (=1), $50,000-$74,999 (=1), $75,000-$99,999 (=1), $100,000-$149,999 (=1), $150,000-$199,999 (=1), and $200,000+ (=1). Respondents employment status is coded as full-time (=0), part-time (=1), unemployed (=1), retired (=1), and disabled (=1). To adjust for underlying differences in health status across respondents, controls are added for whether or not a respondent ever tested positive for COVID-19 (1 = yes), self-rated health (ordinal, 1 = poor to 5 = excellent), and number of days smoking cigarettes in the past thirty days (mean = 6.08, sd = 10.83).
To further adjust for contextual features that might influence either exposure to COVID-19 deaths or psychological distress, controls also include measures of state public health policy, state unemployment policy, and regional fluctuations in COVID-19 infection and mortality rates. Five measures of state-level public health and unemployment policy approaches to the pandemic were derived from a COVID-19 policy database maintained by Raifman et al. (2020). The first captures whether or not a respondent's home state issued a stay-at-home order at any point during the pandemic (1 = never issued stay-at-home order). The second variable indicates whether a respondent's home state had a mask mandate in place on the day the respondent participated the survey (1 = no mask mandate). The third measure captures whether a respondent's home state expanded unemployment insurance eligibility in the case of school closures or lost childcare (1 = yes). A fourth variable indicates whether the respondent's home state stopped participating in federal pandemic-related unemployment benefit programs (1 = yes). The fifth variable captures the weekly unemployment insurance maximum in a respondent's home state, including additional federal stimulus funds (mean = 1063; sd = 143). Because respondents who reside in states with higher COVID-19 infection and mortality rates may be more likely to know someone who has died from the virus, two variable were constructed that capture the seven-day rolling average of new COVID-19 cases per 100,0000, as well as COVID-19 deaths per 100,000, in the respondent's home state on the day that they participated in the survey (New York Times, 2020). Finally, all models include a control for respondent's month of participation in the survey (1 = July, 4 = October).
3.4. Analytic plan
Evidence suggests that COVID-19 bereavement does not occur at random, rendering naïve estimates of the association between bereavement and mental health susceptible to selection effects. To address this issue, I use inverse probability of treatment weighting (IPTW) with regression adjustment to estimate the relationship between bereavement and measures of psychological distress. This strategy involves a two-step procedure, which incorporates adjustments for non-random exposure to treatment into the outcome model. In the first step—presented in Appendix C—COVID-19 bereavement is regressed on covariates with standard errors clustered at the state-level to account for geographic interdependence among respondents in terms of their likelihood of losing someone to the virus. Predicted conditional probabilities from this model are used to create a propensity score (p i) for exposure to bereavement for each respondent (Rosenbaum & Rubin, 1983). These propensity scores, in turn, are used to generate weights (w i) for subsequent analyses predicting depressive symptoms and binge drinking. For these weights, w i is the inverse of the propensity score for the treated group (1/p i) and the inverse of 1-p i (1/[1-p i]) for the untreated group (Robins et al., 2000). The implementation of these weights essentially creates an artificial, pseudo-population, where covariates and treatment assignment are independent (akin to randomization) (Thoemmes & Ong, 2016). This weighting scheme assigns more or less weight to respondents with covariate values that are under- or over-represented in the treatment group (Robins, 1999). By combining propensity score weighting with regression adjustment, this approach is robust to specification error in either the selection or adjusted model (Hirano & Imbens, 2001). In theory, if the propensity or outcome regressions are properly specified, the weighted regression coefficient for the treatment (β^T) will provide an unbiased estimate of the average treatment effect (ATE) of bereavement. These weights are used in negative binomial regression models predicting depressive symptoms and ordered logistic regressions that estimate frequency of binge drinking. Models predicting depressive symptoms and binge drinking also adjust for respondents’ state of residence using a series of dummy variables for each state (omitted from tables for space considerations).
To examine whether there are differential effects of bereavement for essential workers, a series of regression models are estimated that include an interaction term for bereavement x essential worker status. Because the sign and magnitude of interaction terms in non-linear models can be misleading (Ai & Norton, 2003), predicted values from these models are used to visualize interactions. Post-estimate tests of first and second differences are reported in the text to provide a more rigorous assessment of whether bereavement has differential effects on depressive symptoms and binge drinking for essential workers relative to the rest of the sample.
In the absence of an item gauging respondents’ occupational status, supplemental analyses were conducted using household income and educational attainment as proxies to distinguish between higher and lower status essential workers. Starting with household income, models in Table 4 were re-estimated using a combination of essential worker status and educational attainment to create three groups: (1) non-essential workers (n = 1495), (2) essential workers with less than a BA (n = 327), and (3) essential workers with a BA or graduate degree (n = 176). Analyses were then replicated by cross-classifying essential worker status and household income to create three groups: (1) non-essential workers (n = 1495), (2) essential workers with a household income of $49,999 or less (n = 176), and (3) essential workers with household income of $50,000 or more (n = 327).
Table 4.
Regressions of Depressive Symptoms and Binge Drinking on Essential Worker Status x COVID-19 Bereavement (n = 1998).
| Depressive Symptoms |
p-value | Binge Drinking |
||
|---|---|---|---|---|
| Model 1 |
Model 2 |
|||
| Negative Binomial + IPTW Adjusted |
Ordered Logit + IPTW Adjusted |
|||
| IRR [95% CI] | OR [95% CI] | p-value | ||
| COVID-19 Bereavement | 1.12 | .228 | 1.28 | .235 |
| [.93,1.33] | [.85,1.94] | |||
| Essential worker | 1.01 | .915 | .92 | .693 |
| [.86,1.18] | [.59,1.41] | |||
| Essential worker x Bereavement | 1.34 | .039 | 2.51 | .017 |
| [1.02,1.77] | [1.18,5.34] | |||
| Race-Ethnicity (reference=white) | ||||
| American Indian/Alaska Native | 1.11 | .610 | 1.24 | .784 |
| [.74,1.66] | [.27,5.62] | |||
| Asian | .97 | .857 | .50 | .202 |
| [.72,1.32] | [.17,1.45] | |||
| Black/African American | .82 | .072 | .88 | .642 |
| [.66,1.02] | [.51,1.51] | |||
| Hispanic/Latinx | .91 | .345 | 1.31 | .260 |
| [.75,1.10] | [.82,2.08] | |||
| Other | .99 | .962 | .21 | .266 |
| [.56,1.73] | [.01,3.27] | |||
| Female (reference=male) | 1.00 | .974 | .50 | .003 |
| [.85,1.19] | [.32,.79] | |||
| Sexual orientation (reference=straight) | ||||
| Gay/lesbian | 1.16 | .214 | .77 | .775 |
| [.92,1.48] | [.12,4.72] | |||
| Bisexual | .90 | .281 | .64 | .309 |
| [.74,1.09] | [.27,1.52] | |||
| Other | 1.23 | .259 | 1.83 | .411 |
| [.86,1.74] | [.43,7.79] | |||
| Age (reference=65+ years old) | ||||
| 18–24 years old | 2.40 | <.001 | 8.19 | <.001 |
| [1.63,3.54] | [3.55,18.90] | |||
| 25–34 years old | 1.62 | .008 | 11.36 | <.001 |
| [1.13,2.31] | [5.31,24.29] | |||
| 35–44 years old | 1.26 | .213 | 7.31 | <.001 |
| [.88,1.82] | [3.49,15.30] | |||
| 45–54 years old | 1.46 | .029 | 2.99 | .006 |
| [1.04,2.05] | [1.38,6.50] | |||
| 55–64 years old | .97 | .870 | 2.74 | .005 |
| [.68,1.39] | [1.36,5.49] | |||
| Relationship status (reference=married) | ||||
| Single | 1.16 | .062 | 1.09 | .721 |
| [.99,1.35] | [.69,1.71] | |||
| Committed relationship | 1.34 | .014 | .65 | .096 |
| [1.06,1.70] | [.40,1.08] | |||
| Divorced | 1.00 | .540 | 1.31 | .345 |
| [1.00,1.00] | [.75,2.28] | |||
| Widowed | .93 | .964 | .91 | .865 |
| [.75,1.16] | [.30,2.71] | |||
| Separated | 1.01 | .483 | .53 | .355 |
| [.75,1.35] | [.14,2.05] | |||
| Socioeconomic Status | ||||
| Education (reference=Less than high school diploma) | ||||
| High school diploma/GED | 1.03 | .793 | 1.07 | .818 |
| [.85,1.24] | [.62,1.84] | |||
| Some college | 1.24 | .036 | 1.43 | .239 |
| [1.01,1.51] | [.79,2.57] | |||
| Associate's degree | 1.01 | .950 | 1.25 | .612 |
| [.76,1.35] | [.53,2.92] | |||
| Bachelor's degree | 1.04 | .772 | 1.54 | .213 |
| [.81,1.34] | [.78,3.04] | |||
| Graduate degree | 1.13 | .441 | 1.52 | .304 |
| [.83,1.55] | [.68,3.37] | |||
| Annual Household Income (reference=<$25,000) | ||||
| $25,000-$49,999 | 1.06 | .519 | .68 | .200 |
| [.88,1.29] | [.38,1.22] | |||
| $50,000-$74,999 | 1.02 | .836 | .66 | .214 |
| [.83,1.27] | [.35,1.27] | |||
| $75,000-$99,999 | .85 | .203 | .82 | .574 |
| [.66,1.09] | [.40,1.66] | |||
| $100,000-$149,999 | .96 | .774 | .53 | .078 |
| [.72,1.27] | [.26,1.07] | |||
| $150,000-$199,999 | .61 | .006 | .71 | .442 |
| [.43,.87] | [.30,1.70] | |||
| $200,000+ | 1.08 | .621 | .75 | .516 |
| [.79,1.49] | [.32,1.77] | |||
| Employment status (reference=full-time) | ||||
| Part-time | .85 | .097 | .85 | .555 |
| [.70,1.03] | [.49,1.46] | |||
| Unemployed | 1.05 | .653 | .47 | .013 |
| [.84,1.31] | [.26,0.86] | |||
| Retired | .66 | .026 | .51 | .051 |
| [.45,0.95] | [.26,1.00] | |||
| Disabled | 1.32 | .046 | .42 | .031 |
| [1.01,1.74] | [.19,.92] | |||
| Tested positive for COVID-19 | 1.28 | .016 | 1.47 | .153 |
| [1.05,1.57] | [.87,2.49] | |||
| Self-rated health | .75 | <.001 | 1.12 | .289 |
| [.69,0.81] | [.91,1.37] | |||
| Days smoking past month | 1.02 | <.001 | 1.05 | <.001 |
| [1.01,1.02] | [1.04,1.07] | |||
| Home state never issued stay-at-home | 3.17 | .141 | .00 | .034 |
| order | [.68,14.71] | [.00,.63] | ||
| Home state no mask mandate in public | .72 | .103 | .21 | .020 |
| spaces | [.48,1.07] | [.05,.78] | ||
| Home state expanded UI eligibility for | .54 | .411 | .02 | .020 |
| school closure/lost childcare | [.12,2.35] | [.00,.53] | ||
| Home state stopped pandemic | .29 | .016 | 1.72 | .662 |
| unemployment programs | [.11,0.80] | [.15,19.49] | ||
| Home state weekly UI maximum | 1.00 | .329 | 1.03 | .001 |
| [.99,1.00] | [1.01,1.05] | |||
| 7-day average new COVID-19 cases | 1.01 | .154 | 1.01 | .788 |
| (per 100,000 population) | [1.00,1.03] | [.95,1.07] | ||
| 7-day average COVID-19 deaths (per | .50 | .088 | 4.66 | .245 |
| 100,000 population) | [.22,1.11] | [.35,62.25] | ||
| Month of participation | 1.05 | .444 | .80 | .346 |
| [.92,1.20] |
[.50,1.28] |
|||
| Pseudo R2 | .08 | .20 | ||
| Log likelihood | −11190.96 | −4128.13 | ||
| N | 1998 | 1998 | ||
Note: Exponentiated coefficients (incidence rate ratios and odds ratios) with 95% confidence intervals in brackets. Models include controls for respondents' state of residence (omitted in the interest of space) and inverse probability of treatment weighting (IPTW) to account for selection.
4. Results
4.1. Descriptive results
Table 1 presents descriptive statistics for the sample and the results of significance tests contrasting essential workers with the rest of the sample. Overall, 9.7% of the sample reports that they have lost someone close to them due to COVID-19, while approximately 25.2% identify as essential workers. Compared to the rest of the sample, essential workers are significantly more likely to report losing someone close to them due to COVID-19 (19.28% vs. 6.49%, p < .001). As a whole this group also reports significantly more depressive symptoms (6.93 vs. 5.64. p < .001), as well as higher levels of binge drinking across nearly all categories with the exception of “1 or 2 days per week” (11.13% vs. 9.43%, p = .268). In terms of demographics, essential workers are more likely to be Black (16.70% vs. 11.04%, p=.001) or Latinx (20.48% vs. 16.32%, p=.033), and to be men (53.28% vs. 47.83%, p=.034). Essential workers in the sample are less likely to report that they did not graduate from high school (6.96% vs. 15.05%, p < .001) or belong to a household earning less than $25,000 (11.13% vs. 21.07%, p < .001). These discrepancies suggest that essential workers in the sample may be of somewhat higher socioeconomic status compared to the true population of essential workers.
Table 1.
Descriptive statistics for sociodemographic measures and key study variables (N = 1998).
| Full Sample (n = 1998) |
Non-Essential Workers (n = 1495) |
Essential Workers (n = 503) |
Difference Between Essential Workers and Rest of Sample |
||||
|---|---|---|---|---|---|---|---|
| Mean/Percent (N) | SD | Mean/Percent (N) | SD | Mean/Percent (N) | SD | p-value | |
| Dependent Variables | |||||||
| COVID-19 Bereavement | 9.71 (194) | 6.49 (97) | 19.28 (97) | <.001 | |||
| Depressive Symptoms | 5.96 (1998) | 5.46 | 5.64 (1495) | 5.37 | 6.93 (503) | 5.62 | <.001 |
| Binge Drinking | |||||||
| None | 64.31 (1285) | 68.76 (1028) | 51.09 (257) | <.001 | |||
| 1 or 2 days past year | 9.86 (197) | 9.43 (141) | 11.13 (56) | .268 | |||
| Once a month or less | 7.81 (156) | 7.09 (106) | 9.94 (50) | .039 | |||
| 2 or 3 days a month | 7.16 (143) | 5.62 (84) | 11.73 (59) | <.001 | |||
| 1 or 2 days a week | 5.71 (114) | 4.75 (71) | 8.55 (43) | .001 | |||
| 3–5 days a week | 3.40 (68) | 2.94 (44) | 4.77 (24) | .050 | |||
| Every day or almost every day | 1.75 (35) | 1.40 (21) | 2.78 (14) | .041 | |||
| Race-Ethnicity | |||||||
| American Indian/Alaska Native | 1.10 (22) | .94 (14) | 1.59 (8) | .224 | |||
| Asian | 5.46 (109) | 5.62 (84) | 4.97 (25) | .580 | |||
| Black/African American | 12.46 (249) | 11.04 (165) | 16.70 (84) | .001 | |||
| Hispanic/Latinx | 17.37 (347) | 16.32 (244) | 20.48 (103) | .033 | |||
| White | 62.36 (1246) | 64.68 (967) | 55.47 (279) | <.001 | |||
| Other | 1.25 (25) | 1.40 (21) | .80 (4) | .287 | |||
| Sex | |||||||
| Female | 50.80 (1015) | 52.17 (780) | 46.72 (235) | .034 | |||
| Male | 49.20 (983) | 47.83 (715) | 53.28 (268) | .034 | |||
| Sexual Orientation | |||||||
| Straight | 93.84 (1875) | 94.05 (1406) | 93.24 (469) | .515 | |||
| Gay/lesbian | 1.55 (31) | 1.54 (23) | 1.59 (8) | .935 | |||
| Bisexual | 3.90 (78) | 3.75 (56) | 4.37 (22) | .529 | |||
| Other | .70 (14) | .67 (10) | .80 (4) | .769 | |||
| Age | |||||||
| 18–24 years old | 12.96 (259) | 12.37 (185) | 14.71 (74) | .177 | |||
| 25–34 years old | 17.72 (354) | 15.12 (226) | 25.44 (128) | <.001 | |||
| 35–44 years old | 17.57 (351) | 14.25 (213) | 27.44 (138) | <.001 | |||
| 45–54 years old | 14.81 (296) | 14.11 (211) | 16.90 (85) | .128 | |||
| 55–64 years old | 17.22 (344) | 19.00 (284) | 11.93 (60) | <.001 | |||
| 65+ years old | 19.72 (394) | 25.15 (376) | 3.58 (18) | <.001 | |||
| Relationship Status | |||||||
| Single | 26.98 (539) | 25.95 (388) | 30.02 (151) | .075 | |||
| Committed Relationship | 11.51 (230) | 10.30 (154) | 15.11 (76) | .003 | |||
| Married | 49.40 (987) | 50.64 (757) | 45.73 (230) | .057 | |||
| Divorced | 7.41 (148) | 7.83 (117) | 6.16 (31) | .218 | |||
| Widowed | 3.35 (67) | 4.21 (63) | .80 (4) | <.001 | |||
| Separated | 1.35 (27) | 1.07 (16) | 2.19 (11) | .061 | |||
| Socioeconomic Status | |||||||
| Education | |||||||
| Less than high school diploma | 13.01 (260) | 15.05 (225) | 6.96 (35) | <.001 | |||
| High school diploma/GED | 27.98 (559) | 27.49 (411) | 29.42 (148) | .404 | |||
| Some college | 20.97 (419) | 21.67 (324) | 18.89 (95) | .184 | |||
| Associate's degree | 8.01 (160) | 7.42 (111) | 9.74 (49) | .098 | |||
| Bachelor's degree | 19.02 (380) | 18.13 (271) | 21.67 (109) | .080 | |||
| Graduate degree | 11.01 (220) | 10.23 (153) | 13.32 (67) | .056 | |||
| Annual Household Income | |||||||
| Less than $25,000 | 18.57 (371) | 21.07 (315) | 11.13 (56) | <.001 | |||
| $25,000-$49,999 | 22.72 (454) | 22.34 (334) | 23.86 (120) | .483 | |||
| $50,000-$74,999 | 19.27 (385) | 19.53 (292) | 18.49 (93) | .608 | |||
| $75,000-$99,999 | 14.31 (286) | 13.24 (198) | 17.50 (88) | .019 | |||
| $100,000-$149,999 | 13.56 (271) | 12.98 (194) | 15.31 (77) | .186 | |||
| $150,000-$199,999 | 6.01 (120) | 5.62 (84) | 7.16 (36) | .209 | |||
| $200,000+ | 5.56 (111) | 5.22 (78) | 6.56 (33) | .255 | |||
| Employment Status | |||||||
| Full-time | 38.64 (772) | 25.42 (380) | 77.93 (392) | <.001 | |||
| Part-time | 12.61 (252) | 9.43 (141) | 22.07 (111) | <.001 | |||
| Unemployed | 19.72 (394) | 26.35 (394) | .00 (0) | <.001 | |||
| Retired | 23.37 (467) | 31.24 (467) | .00 (0) | <.001 | |||
| Disabled | 5.66 (113) | 7.56 (113) | .00 (0) | <.001 | |||
| Essential worker | 25.18 (503) | .00 (0) | 1.00 (503) | <.001 | |||
| Tested positive for COVID-19 | 6.96 (139) | 4.15 (62) | 15.31 (77) | <.001 | |||
| Self-rated health | 3.28 (1998) | .97 | 3.23 (1495) | .96 | 3.42 (503) | .99 | <.001 |
| Days smoking past month | 6.08 (1998) | 10.83 | 5.54 (1495) | 10.71 | 7.66 (503) | 11.04 | <.001 |
| Home state never issued stay- at-home order | 2.90 (58) | 2.94 (44) | 2.78 (14) | .853 | |||
| Home state no mask mandate in public spaces | 37.09 (741) | 35.99 (538) | 40.36 (203) | .079 | |||
| Home state expanded UI eligibility for school closure/lost childcare |
37.04 (740) | 37.39 (559) | 35.98 (181) | .572 | |||
| Home state stopped participation in pandemic unemployment programs |
40.14 (802) | 38.80 (580) | 44.14 (222) | .035 | |||
| Home state weekly UI maximum | 1063.07 (1998) | 143.02 | 1063.33 (1495) | 143.12 | 1062.27 (503) | 142.85 | .886 |
| Home state 7-day average of new COVID-19 cases per 100,000 population | 17.20 (1998) | 13.58 | 17.15 (1495) | 13.76 | 17.33 (503) | 13.04 | .801 |
| Home state 7-day average of COVID-19 deaths per 100,000 population | .22 (1998) | .15 | .22 (1495) | .15 | .21 (503) | .14 | .243 |
Note: Means and percentages with standard deviations. Differences between essential workers and rest of sample tested using chi-2 tests for dichotomous variables, t-tests for continuous variables, and Wilcoxon Rank-Sum tests for ordinal variables.
4.2. Predictors of COVID-19 bereavement
Table 2 presents average marginal effects (AME) from a logistic regression model predicting COVID-19 bereavement with standard errors clustered at the state-level. Results for the logistic regression model from which AMEs are derived can be found in Appendix C. Black respondents’ probability of experiencing COVID-19 bereavement is approximately 8 percentage points higher than Whites (AME = 0.078, p = .002), whereas Latinx respondents have a roughly 4 percentage point higher probability of experiencing loss relative to White respondents—though this difference is not statistically significant (AME = 0.037, p = .080). Compared to straight respondents, gay/lesbian respondents had a nearly 13 percentage point higher probability (AME = 0.125, p = .025) of experiencing bereavement. Consistent with bivariate results (Table 1), essential workers are significantly more likely to endure a COVID-related death, with members of this group approximately four percentage points more likely to experience bereavement than other respondents (AME = .044, p=.009). Respondents who tested positive for COVID-19 had a nearly 19 percentage point higher probability (AME = 0.188, p < .001) of experiencing bereavement relative to those who were not infected by the virus. Participants with more days of smoking also had a higher probability of experiencing COVID-19 bereavement (AME = 0.002, p=<.001). Turning to state-level characteristics, respondents residing in states that never issued a stay at home order (AME = −0.057, p = .027) and those with higher rates of new COVID-19 cases (AME = −0.002, p = .002) had a decreased probability of experiencing COVID-19 bereavement net of controls. By contrast, respondents living in states with elevated rates of COVID-19 mortality had a higher probability (AME = 0.143, p = .009) of personally experiencing bereavement. As described previously, conditional predicted probabilities from this model were generated post-estimation to create inverse probability of treatment weights used in subsequent analyses.
Table 2.
Average marginal effects from logistic regression predicting COVID-19 bereavement (n = 1998).
| AME [SE] | p-value | |
|---|---|---|
| Race-Ethnicity (reference=white) | ||
| American Indian/Alaska Native | .042 | .435 |
| [.054] | ||
| Asian | .029 | .292 |
| [.027] | ||
| Black/African American | .078 | .002 |
| [.026] | ||
| Hispanic/Latinx | .037 | .080 |
| [.021] | ||
| Other | -.022 | .477 |
| [.032] | ||
| Female (reference=male) | .001 | .947 |
| [.017] | ||
| Sexual orientation (reference=straight) | ||
| Gay/lesbian | .125 | .025 |
| [.056] | ||
| Bisexual | .030 | .307 |
| [.030] | ||
| Other | .053 | .425 |
| [.067] | ||
| Age (reference=65+ years old) | ||
| 18–24 years old | .018 | .554 |
| [.030] | ||
| 25–34 years old | .020 | .359 |
| [.022] | ||
| 35–44 years old | .006 | .776 |
| [.021] | ||
| 45–54 years old | -.010 | .698 |
| [.025] | ||
| 55–64 years old | .034 | .151 |
| [.024] | ||
| Relationship status (reference=married) | ||
| Single | -.019 | .135 |
| [.013] | ||
| Committed relationship | -.020 | .255 |
| [.018] | ||
| Divorced | .034 | .240 |
| [.029] | ||
| Widowed | -.022 | .428 |
| [.028] | ||
| Separated | -.012 | .856 |
| [.068] | ||
| Socioeconomic Status | ||
| Education (reference=Less than high school diploma) | ||
| High school diploma/GED | -.025 | .093 |
| [.015] | ||
| Some college | .022 | .176 |
| [.016] | ||
| Associate's degree | -.008 | .770 |
| [.027] | ||
| Bachelor's degree | .016 | .477 |
| [.023] | ||
| Graduate degree | .028 | .236 |
| [.024] | ||
| Annual Household Income (reference=<$25,000) | ||
| $25,000-$49,999 | .011 | .451 |
| [.015] | ||
| $50,000-$74,999 | .016 | .470 |
| [.022] | ||
| $75,000-$99,999 | .016 | .401 |
| [.019] | ||
| $100,000-$149,999 | .002 | .943 |
| [.021] | ||
| $150,000-$199,999 | .000 | .999 |
| [.023] | ||
| $200,000+ | -.022 | .381 |
| [.025] | ||
| Employment status (reference=full-time) | ||
| Part-time | .020 | .223 |
| [.016] | ||
| Unemployed | .033 | .055 |
| [.017] | ||
| Retired | -.013 | .607 |
| [.024] | ||
| Disabled | .003 | .904 |
| [.027] | ||
| Essential worker | .044 | .009 |
| [.017] | ||
| Tested positive for COVID-19 | .188 | <.001 |
| [.018] | ||
| Self-rated health | -.006 | .182 |
| [.005] | ||
| Days smoking past month | .002 | <.001 |
| [.001] | ||
| Home state never issued stay-at-home order | -.057 | .027 |
| [.026] | ||
| Home state no mask mandate in public spaces | .007 | .607 |
| [.014] | ||
| Home state expanded UI eligibility for school | -.025 | .087 |
| closure/lost childcare | [.015] | |
| Home state stopped pandemic unemployment | .007 | .682 |
| Programs | [.018] | |
| Home state weekly UI maximum | .000 | .706 |
| [.000] | ||
| 7-day average new COVID-19 cases (per 100,000 | -.002 | .002 |
| population) | [.001] | |
| 7-day average COVID-19 deaths (per 100,000 | .143 | .009 |
| population) | [.054] | |
| Month of participation | -.012 | .365 |
| [.014] |
||
| N | 1998 | |
Note: Average marginal effects calculated at the observed values for all observations. Delta-method standard errors clustered at the state-level in brackets. Average marginal effects are derived from logistic regression model found in Appendix C.
4.3. Associations among COVID-19 bereavement, depressive symptoms, and binge drinking
Table 3 presents average marginal effects from a series of regression models predicting depressive symptoms and frequency of binge drinking (the full models from which AMEs are derived can found in Appendix D). These models are estimated both with and without the inclusion of inverse probability of treatment weights. In model 1 (unweighted), respondents who experienced COVID-19 bereavement report CES-D scores that are 1.72 (p = .001) points higher, on average, than respondents who did not experience COVID-related loss. This finding suggests that scores on the CES-D scale are nearly one-third of a standard deviation higher among the bereaved. Model 2 re-estimates this association with inverse probability of treatment weights. In this model, participants who experienced COVID-19 bereavement report CES-D scores that are 1.29 (p = .016) points higher, on average, than respondents who did not. These results indicate that the magnitude of the effect of bereavement on depressive symptoms is diminished by 25% ([1.29–1.72]/1.72∗100 = -25.00) after adjusting for non-random exposure to COVID-19 mortality. Indeed, net of selection effects, the bereaved report scores on the CES-D scale that are closer to one-fifth of a standard deviation higher than those who were spared this loss.
Table 3.
Average marginal effects from regressions of depressive symptoms and binge drinking on COVID-19 bereavement and study variables (n = 1998).
| Depressive Symptoms |
Binge Drinking |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||||
| Negative Binomial |
Negative Binomial + IPTW Adjusted |
Ordered Logit |
Ordered Logit + IPTW Adjusted |
||||||
| AME [SE] |
p-value |
AME [SE] |
p-value |
AME [SE] |
p-value |
AME [SE] |
p-value |
||
| Response Category | |||||||||
| COVID-19 Bereavement | 1.72 | .001 | 1.29 | .016 | None | -.10 | .002 | -.076 | .003 |
| [.529] | [.533] | [.033] | [.026] | ||||||
| 1 or 2 days in past | .015 | .004 | .005 | .006 | |||||
| 12 months | [005] | [.002] | |||||||
| Once a month or less | .018 | .003 | .017 | .009 | |||||
| [.006] | [.006] | ||||||||
| 2 or 3 days a month | .021 | .003 | .014 | .009 | |||||
| [.007] | [.005] | ||||||||
| 1 or 2 days a week | .021 | .003 | .019 | .023 | |||||
| [.007] | [.008] | ||||||||
| 3–5 days a week | .015 | .004 | .015 | .008 | |||||
| [.005] | [.006] | ||||||||
| Every day or almost | .009 | .006 | .006 | .015 | |||||
| every day |
[.003] |
[.003] |
|||||||
| N | 1998 | 1.998 | 1998 | 1998 | |||||
Note: Average marginal effects calculated at the observed values for all observations. Delta-method standard errors in brackets. Average marginal effects are derived from models found in Appendix D, with other covariates omitted for space considerations. IPTW = Inverse probability of treatment weighting.
Moving to binge drinking, in the unweighted model, respondents who experienced COVID-19 bereavement are 10 percentage points less likely (AME = −0.10, p = .002) to say they did not engage in any binge drinking in the past year compared respondents who did not lose a close tie to the virus (Model 3). Although the discrepancy between these groups is less sizable at higher levels of binge drinking, the bereaved are between ∼1 and 2 percentage points more likely than those unaffected by COVID-related loss to indicate that they engage in binge drinking more frequently; ranging from 2.1 percentage points more likely to drink 1 or 2 days a week (AME = 0.021, p = .003) to 0.9 percentage points more likely say they drink every day (AME = 0.009, p = .006). These effects remain relatively unchanged when inverse probability of treatment weights are introduced in model 4. Cumulatively, findings suggest that the effects of COVID-19 bereavement on depressive symptoms and binge drinking are robust to selection effects.
4.4. Differential effects of bereavement for essential workers
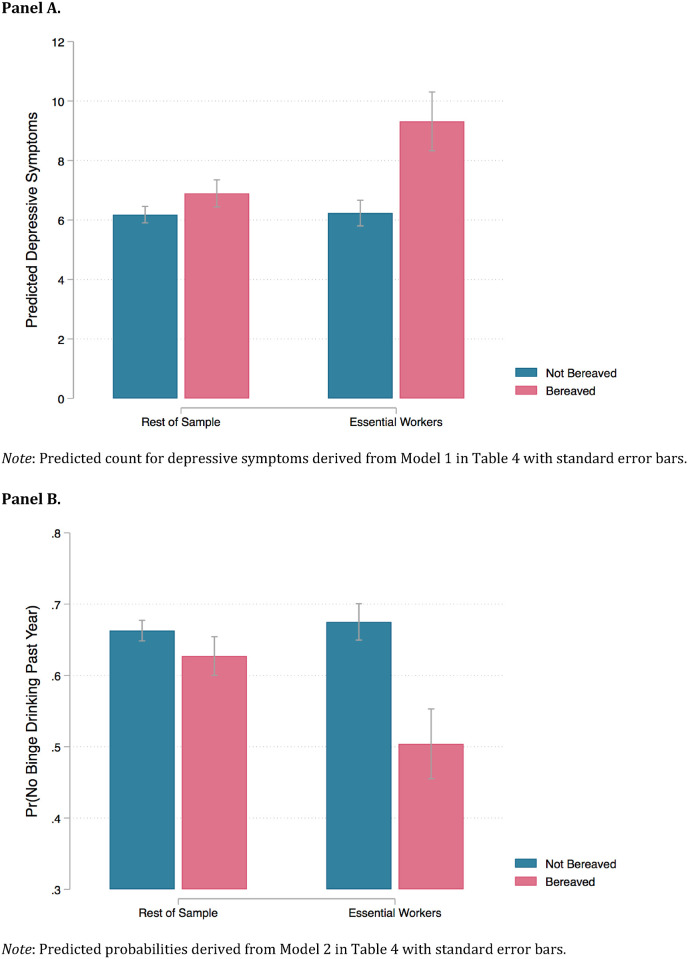
Table 4 presents the results of models where psychological distress variables are regressed on interactions between COVID-19 bereavement and essential worker status. The results of these models are consistent across outcomes, revealing a significant, positive interaction between COVID-19 bereavement and essential worker status. To facilitate interpretation, these interactions are visualized in Fig. 1 using predictions generated from models 1 and 2 with all other covariates held at their mean values.
Fig. 1.
Predictions of depressive symptoms and probability of not binge drinking by COVID-19 bereavement and essential worker status.
As depicted in Panel A, non-essential workers who lost someone to COVID-19 report slightly more depressive symptoms (6.90) than those who did not (6.18), however this difference is not statistically significant net of adjustments (Δ = 0.72; p=.236). By contrast, essential workers who experienced bereavement report substantially more depressive symptoms (9.32) than essential workers who did not lose someone to the virus (6.23; Δ = 3.09; p=.002), with this difference equivalent to more than one-half of a standard deviation on the CES-D scale. Correspondingly, the effect of bereavement on depressive symptoms is significantly greater for essential workers than it is for the rest of the sample (second difference: 3.09–0.72 = 2.37, p=.042).
For illustrative purposes, Panel B examines respondents' likelihood of indicating that they did not binge drink during the past year using predictions generated from model 2 of Table 4. Among respondents in the sample who were not essential workers, those who lost someone to COVID-19 had a slightly lower probability of not binge drinking during the past year (0.63) relative to respondents who did not endure this loss (0.66), although this three-percentage point difference is not statistically significant (Δ = -0.03; p=.235). By contrast, essential workers who experienced bereavement (0.50) are about eighteen percentage points less likely to indicate that they did not binge drink during the past year compared to essential workers who did not lose a close tie the virus (0.68; Δ = -0.18; p=.001). The effects of bereavement on one's likelihood of indicating they did not binge drink in the past year is significantly greater for essential workers than for other respondents in the sample (second difference: −0.18 – [-0.03] = -0.15; p=.016).
4.5. Supplemental analyses
Because there is reason to suspect that essential workers with fewer resources are more vulnerable to the deleterious consequences of bereavement, auxiliary analyses separated higher and lower status essential workers using educational attainment and household income as indicators of social status. Turning first to models where essential workers are stratified by educational attainment (Appendix E), there is a positive, significant interaction between more educated essential worker x bereavement for depressive symptoms (IRR = 2.09, 95% CI = 1.35–3.22, p = .001), whereas the incidence rate ratio for the interaction between less educated workers x bereavement is indistinguishable from 1.00 (IRR = 1.03, 95% CI = 0.77–1.39, p = .827), or indicative of a null association (model 1). Moving to binge drinking (model 2), although the interaction between more educated essential worker x bereavement does not meet the standard threshold for statistical significance (p = .060), the odds ratio for the interaction between more educated essential workers x bereavement (OR = 3.04, 95% CI = 0.95–9.69) is notably larger than the interaction term between less educated essential worker x bereavement (OR = 2.19, 95% CI = 0.88–5.43, p = .091).
Turning to models where essential workers are stratified by household income (Appendix F), the interaction between higher income essential worker x bereavement is positive and significant with respect to depressive symptoms (IRR = 1.64, 95% CI = 1.19–2.25, p = .002), suggesting elevated depressive symptomology among higher income essential workers who experienced loss. By contrast, the interaction for lower income essential worker x bereavement is not significant (IRR = 0.75, 95% CI = 0.47–1.18, p = .213). A similar set of findings can be found for binge drinking (model 2), where there is a positive and significant interaction between higher income essential worker x bereavement (OR = 2.79, 95% CI = 1.26–6.20, p = .012), indicative of more intense binge drinking among higher income essential workers who have lost someone close to them to the virus. As with depressive symptoms, there is a non-significant interaction between lower income essential worker x bereavement for binge drinking (OR = 1.28, 95% CI = 0.34–4.86, p = .714). Although these analyses cumulatively provide evidence that higher status workers may be driving the stronger effects of bereavement on depressive symptoms and binge drinking among essential workers, these results should be interpreted as suggestive in the absence of more precise measures of occupational status.
5. Discussion
The past year has been the deadliest in American history, largely owing to the coronavirus pandemic (Associated Press, 2020). This study builds upon the insights of recent research on the psychological correlates of pandemic-related stressors (Bierman et al., 2021; Donnelly & Farina, 2021; Zheng et al., 2021) by examining the associations between COVID-19 bereavement and mental health. There are two principal contributions of this research. First, findings demonstrate that even after adjustment for non-random exposure to COVID-19 bereavement, the loss of a close tie to the virus is still robustly associated with depressive symptoms and binge drinking. Second, the strength of these relationships varies across different segments of society, as the associations between COVID-19 bereavement and depressive symptoms and binge drinking were accentuated among essential workers relative to other respondents.
The loss of a significant other to COVID-19 is not a stochastic event. Members of marginalized racial-ethnic groups are substantially more likely to know someone who has either been hospitalized or killed by the virus (Funk & Tyson, 2021). Thus, selection poses a key concern when attempting to gauge the true effect of COVID-19 bereavement on mental health. That is, unadjusted estimates may reflect underlying differences in life experiences and stress exposure between these groups rather than the direct consequences of losing a close tie to COVID-19. To address this concern, I implemented an inverse probability of treatment weighting approach designed to incorporate selection into treatment (i.e., losing someone close to the virus) as a component of outcome models. These results indicated that the loss of a close tie to COVID-19 remained associated with greater depressive symptoms and more frequent binge drinking even after adjustment for non-random exposure to bereavement. Broadly speaking, these results align with prior research on the mental health consequences of bereavement, which finds that the death of a significant other is associated with elevated risk of depression (McLeod, 1991; Umberson et al., 1992) and greater alcohol use (Umberson & Chen, 1994).
Although COVID-19 deaths are similar in some respects to those resulting from disasters or unnatural causes—for instance, in their abruptness and the inability of the bereaved to say goodbye or lay to rest lingering conflicts—they are distinct in that the mourning process has been sharply circumscribed. People who would normally have access to high levels of social support have grieved in relative isolation, robbed of this coping resource by the same social distancing protocols designed to protect them. Obstructed access to these supports augurs poorly for the mental health of the bereaved (Carr et al., 2020). Just as generous state policies have weakened the damaging effects of recessionary income shocks on mental health during the pandemic (Donnelly & Farina, 2021), government assistance will be vital to addressing the looming bereavement crisis. These resources are critical for the mobilization of grief counselors, crisis hotlines, and community-based centers (Brewer & Sparkes, 2011) necessary to mitigate the emergence of grief-related disorders.
The present study also offers further insight into the plight of essential workers during the pandemic. Essential workers in the study were significantly more likely to report losing someone close to them due to COVID-19. In turn, bereavement was associated with more depressive symptoms and binge drinking among members of this group relative to other respondents. Although essential workers were lauded by the public at the outset of the pandemic, this enthusiasm has not been met with sufficient material resources or workplace protections for this group. Most of these workers have been denied hazard pay, while state and local governments have failed to provide them with appropriate personal protective equipment (Williams et al., 2020). Despite substantial variation in salary and job security, essential workers generally earn lower wages and have less decision-making latitude than other occupations (Blau et al., 2020). As a result, many of these workers were coerced into working under perilous conditions in order to avert economic ruin. While the approval of highly effective vaccines signals a potential end to the pandemic may be in sight, in the intervening months essential workers will continue to labor amidst potential risk of infection. To help defray the mental health burdens associated with this circumstance, essential workers and their families should be prioritized for vaccination (Buckner et al., 2021), and programs should be implemented that bring vaccinations directly to the workplaces of essential workers. Furthermore, essential workers who have been infected with the virus should be granted sufficient insurance to treat long-term ailments associated with it (Shim & Starks, 2021). Frontline occupations experienced the greatest increase in excess mortality during the COVID-19 pandemic (Chen et al., 2021). Although it will never replace those who have been lost, the families of essential workers who died due to workplace exposure should be entitled to recompense for the sacrifices they have made during this global crisis.
While it is beyond the scope of this study to empirically test the mechanisms underlying the stronger associations found between bereavement and psychological distress for essential workers, prior theoretical work is suggestive. Pearlin and Bierman (2013) posit that vicarious experience of a traumatic event in a person's social network may prompt them to consider their own susceptibility to it. Following from this contention, I hypothesized that because essential workers live with the daily knowledge they might be exposed to the virus, the loss of a close tie to COVID-19 might increase their anticipatory stress about contracting it and prove particularly damaging to mental health (Sloan et al., 2020, pp. 1–46). Another possible explanation is that bereavement further compounds the wide array of stressors experienced by members of this group in an overarching process of cumulative disadvantage (Dannefer, 2003). As detailed previously, essential workers generally possess little job autonomy and receive lower wages relative to other workers. Further contributing to their stress burden, these workers have labored in unsafe, hazardous working conditions. Consequently, the interactive effect between bereavement and essential worker status may reflect the insidious accretion of multiple stressors among this group.
5.1. Limitations
This study has several limitations that require comment. Foremost among them are issues related to the survey items used to gauge COVID-19 bereavement and essential worker status. Starting with the former, bereavement was measured using respondents' self-report of whether they had lost someone close to them due to COVID-19. This measure did not ask respondents to specify either how many people they had lost to the virus, or the nature of their relationship to the deceased. It is entirely possible that the loss of more intimate ties (e.g., a romantic partner or a child) is associated with more severe psychological distress than the loss of distant relations (e.g., a co-worker). However, because this measure collapses relationships of varying degrees closeness, it is not possible to discern whether the strength of the association between bereavement and distress is sensitive to a respondents’ level of intimacy with the deceased.
Another limitation of the bereavement measure is that information regarding the decedent's official cause of death was ascertained directly from the respondent without verification of this designation by a healthcare provider. Emerging evidence on excess deaths during the pandemic suggest that a notable portion of COVID-19 deaths during the early days of the pandemic went undocumented due to a nationwide scarcity of testing (Woolf et al., 2020). Rates of detection were significantly lower among decedents between the ages of 25–44 (Faust et al., 2021) and in counties comprised of a greater proportion of lower income and Black residents (Stokes et al., 2021). As such, it is likely that some respondents in the sample lost a close tie due to COVID-19, but were unaware of the virus' role in their passing. Another consideration is that people who are more depressed or inclined to binge drink may also be more likely to attribute the recent loss of a loved one to COVID-19, either as a direct or indirect (e.g., unmet medical care for another health conditions, drug overdose death) cause. Jointly, these circumstances suggest that caution must be exercised when interpreting the magnitude of the association between bereavement and distress documented in this study.
Turning to the measure of essential worker status, because respondents' occupation was not established, there is no way to systematically determine whether there were qualitative differences in the effects of bereavement on depressive symptoms or binge drinking across different types of essential workers. Essential workers are a diverse group, and correspondingly, there are a number of important distinctions among them. Some essential workers are better equipped than others to contend with sickness and the uncertainty of potential exposure. A recent study conducted in Australia found that depression and anxiety were less prevalent among healthcare workers than other essential workers (Toh et al., 2021). These findings suggest that workers with more resources—e.g., income, insurance, and sick leave—are less susceptible to pandemic-related stressors. It follows that economically precarious essential workers may be more vulnerable to the inimical effects of pandemic stressors on mental health, among them, the loss of a close tie to the virus. In an attempt to discern how status differences might contribute to the potentiated association between COVID-19 bereavement and psychological distress among this group, supplemental analyses used educational attainment and household income as proxies for occupational status. These results suggest that the stronger effects of bereavement on depressive symptoms and binge drinking among essential workers may be driven by higher status workers. Prior research indicates that high status workers are advantaged relative to lower status workers with respect to autonomy and schedule flexibility. These benefits generally enable high status workers to ‘block out’ hours on their official schedule for self-care (e.g., catching up on sleep or attending therapy), or make up for unexpected overtime by taking ‘unofficial’ days off from work (Moen et al., 2013). Given the nature of essential work–which by its very definition precludes the ability to work remotely or exert much control over one's work schedule—high status essential workers may be unable to deploy the coping resources utilized by high status workers in other sectors of the economy to safeguard their mental health against pandemic-related stressors. Absent measures of occupation or industry type, however, the present study is unable to fully adjudicate whether status differences among essential workers serve to either amplify or mitigate the association between COVID-related bereavement and psychological distress. Indeed, by examining essential workers in the aggregate, the results of this study obscure potentially important nuance in terms of how the social and economic resources that come bundled with occupational status may be leveraged to shield one's mental health during the pandemic. Finally, because essential worker status was self-reported, it is possible that some respondents self-identified as essential workers despite working in economic sectors not officially designated as such. Considering these issues, the absence of an item classifying occupation is a regrettable oversight that should be remedied in future research on the mental health of essential workers.
Although the present study was designed to approximate the demographic composition of the United States, these data are not representative. Respondents were not selected at random, but rather participated because the study was of some interest to them. In view of declining response rates across the social sciences (Galea & Tracy, 2007), it is reasonable to suspect that people who opt-into survey research differ from the general population in ways that cannot be empirically assessed here. For instance, because the survey was administered electronically, individuals of lower income and educational attainment likely had a reduced probability of participating in the study due to enduring disparities in internet access in the U.S. (Greenberg-Worisek et al., 2019).
Beyond issues of generalizability, however, the quota-based, convenience sample used in this study might also have more direct bearing on the magnitude and significance of the observed associations between COVID-19 bereavement and psychological distress. Because the study uses a non-probability sample, it is plausible that respondents systematically differ from the general population in terms of either their exposure to COVD-related deaths or their underlying propensity to binge drink or experience depression. This form of selection bias could have the effect of misrepresenting the association between exposure and outcome variables. A further threat to the validity of findings would occur under a condition in which the sample systematically differed from the general population with respect to an unmeasured characteristic that operates as an effect modifier of the link between bereavement and distress (Keyes & Westreich, 2019). That is, if COVID-19 bereavement were to interact with an unobserved factor whose prevalence sharply diverges between respondents in the sample and those in general population, the magnitude of the association between bereavement and distress depicted in this study would necessarily be imprecise. As a final caveat, because these data are cross-sectional, it is not possible to rule out reverse causality, including the prospect that people who were more depressed or inclined to binge drink prior to the pandemic were also more likely to experience to COVID-19 bereavement. Such a scenario would render the apparent association between bereavement and distress an artifact of the data generating process. In view of these limitations, I wish to emphasize that my intention is to provide preliminary insight into the societal consequences of COVID-19 bereavement, and encourage the pursuit of representative studies that interrogate how COVID-related loss may disproportionately burden the mental health of individuals already more susceptible to the economic and social strains of the pandemic.
6. Conclusion
The profound loss of human life due to the COVID-19 pandemic will have consequences for mental health that reverberate for years to come. The findings of this study demonstrate that people who endured the death of a close tie in the first few months of the pandemic experienced greater depressive symptomology and engaged in more frequent binge drinking than those who were spared this loss. Notably, these effects were even more pronounced among essential workers. Despite these insights, there is an urgent need for longitudinal research that identifies the long-term sequelae of COVID-19 bereavement. To date, millions of Americans have grieved in relative solitude, largely removed from the social supports that sustain people during times of loss. Even after widespread vaccination and economic recovery, for many, the mourning process will be in its nascent stages. It will be crucial to identify those most at-risk for developing prolonged grief and substance use disorders, and to dedicate sufficient resources to assisting these individuals as they navigate the grieving process.
Declaration of competing interest
Funding for this study was received from Hamilton College through an early career faculty grant. The author has no financial or other form of conflict to support. This study was approved by the Institutional Review Board at Hamilton College: Protocol #S20-105.
Acknowledgements
Support for this study was received from Hamilton College through an early career faculty grant. This study was approved by the Institutional Review Board at Hamilton College: Protocol #S20-105.
Appendix A. Comparison of Sociodemographic Composition of Study Sample to 2016 Census Current Population Survey Benchmarks
| Sample (n = 1998) | Census CPS | |
|---|---|---|
| Sex | ||
| Female | 50.80% | 50.80% |
| Male | 49.20% | 49.20% |
| Race-Ethnicity | ||
| American Indian/Alaska Native | 1.10% | .70% |
| Asian/Native Hawaiian/Other Pacific Islander | 5.46% | 5.30% |
| Black/African American | 12.46% | 12.30% |
| Hispanic/Latinx | 17.37% | 17.40% |
| White | 62.36% | 61.90% |
| Other | 1.25% | 2.40% |
| Education | ||
| Less than high school diploma | 13.01% | 13.00% |
| High school diploma/GED | 27.98% | 28.00% |
| Some college | 20.97% | 21.00% |
| Associate's degree | 8.01% | 8.00% |
| Bachelor's degree | 19.02% | 19.00% |
| Graduate degree | 11.01% | 11.00% |
| Annual Household Income | ||
| Less than $25,000 | 18.57% | 18.00% |
| $25,000-$49,999 | 22.72% | 22.00% |
| $50,000-$74,999 | 19.27% | 19.00% |
| $75,000-$99,999 | 14.31% | 14.00% |
| $100,000-$149,999 | 13.56% | 15.00% |
| $150,000-$199,999 | 6.01% | 6.00% |
| $200,000+ | 5.56% | 6.00% |
Note: Percentages for may not sum to 100 due to rounding.
Source: Current Population Survey, Annual Social and Economic Supplement (2016). U.S. Census Bureau. (U.S. Census Bureau, 2016)
Appendix B. Sociodemographic Characteristics of Essential Workers in Sample compared to General Population
| Essential Workers in Sample (n = 503) | Essential Workers in Population (n = 55,217,845) | |
|---|---|---|
| Race-Ethnicity | ||
| American Indiana/Alaska Native/Other | 1.59% | 1% |
| Asian | 4.97% | 6% |
| Black/African American | 16.70% | 15% |
| Hispanic/Latinx | 20.48% | 21% |
| White | 55.47% | 55% |
| Sex | ||
| Female | 46.72% | 49% |
| Male | 53.28% | 51% |
| Education | ||
| Less than high school diploma | 6.96% | 10% |
| High school diploma/GED | 29.42% | 29% |
| Some college | 28.63% | 30% |
| Bachelor's degree | 21.67% | 20% |
| Advanced degree | 13.32% | 11% |
Source: Economic Policy Institute (EPI) analysis of Current Population Survey Outgoing Rotation Group microdata, EPI Current Population Survey Extracts, Version 1.0.2 (2020). https://www.epi.org/blog/who-are-essential-workers-a-comprehensive-look-at-their-wages-demographics-and-unionization-rates/.
Appendix C. Logistic Regression of COVID-19 Bereavement on Key Study Variables (n = 1998)
| OR [95% CI] | p-value | |
|---|---|---|
| Race-Ethnicity (reference=white) | ||
| American Indian/Alaska Native | 2.04 | .349 |
| [.46, 9.08] | ||
| Asian | 1.67 | .244 |
| [.70, 3.98] | ||
| Black/African American | 3.14∗∗∗ | <.001 |
| [1.71, 5.79] | ||
| Hispanic/Latinx | 1.89∗ | .041 |
| [1.03, 3.47] | ||
| Other | .58 | .535 |
| [.11, 3.20] | ||
| Female (reference=male) | 1.02 | .947 |
| [.57, 1.84] | ||
| Sexual orientation (reference=straight) | ||
| Gay/lesbian | 4.35∗∗ | .002 |
| [1.71, 11.04] | ||
| Bisexual | 1.61 | .244 |
| [.72, 3.58] | ||
| Other | 2.16 | .337 |
| [.45, 10.37] | ||
| Age (reference=65+ years old) | ||
| 18–24 years old | 1.38 | .553 |
| [.47, 4.04] | ||
| 25–34 years old | 1.42 | .374 |
| [.65, 3.10] | ||
| 35–44 years old | 1.12 | .779 |
| [.51, 2.44] | ||
| 45–54 years old | .81 | .697 |
| [.29, 2.29] | ||
| 55–64 years old | 1.77 | .135 |
| [.84, 3.72] | ||
| Relationship status (reference=married) | ||
| Single | .70 | .159 |
| [.43, 1.15] | ||
| Committed relationship | .70 | .282 |
| [.36, 1.35] | ||
| Divorced | 1.63 | .207 |
| [.76, 3.50] | ||
| Widowed | .66 | .470 |
| [.22, 2.02] | ||
| Separated | .81 | .864 |
| [.07, 9.35] | ||
| Socioeconomic Status | ||
| Education (reference=Less than high school diploma) | ||
| High school diploma/GED | .60 | .087 |
| [.33, 1.08] | ||
| Some college | 1.41 | .206 |
| [.83, 2.42] | ||
| Associate's degree | .87 | .773 |
| [.32, 2.31] | ||
| Bachelor's degree | 1.31 | .478 |
| [.62, 2.77] | ||
| Graduate degree | 1.56 | .224 |
| [.76, 3.18] | ||
| Annual Household Income (reference=<$25,000) | ||
| $25,000-$49,999 | 1.22 | .456 |
| [.72, 2.05] | ||
| $50,000-$74,999 | 1.31 | .463 |
| [.63, 2.72] | ||
| $75,000-$99,999 | 1.33 | .397 |
| [.69, 2.55] | ||
| $100,000-$149,999 | 1.03 | .943 |
| [.47, 2.25] | ||
| $150,000-$199,999 | 1.00 | .999 |
| [.42, 2.37] | ||
| $200,000+ | .62 | .433 |
| [.19, 2.03] | ||
| Employment status (reference=full-time) | ||
| Part-time | 1.41 | .203 |
| [.83, 2.38] | ||
| Unemployed | 1.71∗ | .042 |
| [1.02, 2.86] | ||
| Retired | .78 | .622 |
| [.29, 2.11] | ||
| Disabled | 1.06 | .903 |
| [.41, 2.75] | ||
| Essential worker | 2.15∗∗ | .005 |
| [1.26, 3.67] | ||
| Tested positive for COVID-19 | 27.11∗∗∗ | <.001 |
| [14.35, 51.22] | ||
| Self-rated health | .90 | .180 |
| [.76, 1.05] | ||
| Days smoking past month | 1.04∗∗∗ | <.001 |
| [1.03, 1.06] | ||
| Home state never issued stay-at-home order | .37∗ | .017 |
| [.16, .84] | ||
| Home state no mask mandate in public spaces | 1.13 | .604 |
| [.70, 1.82] | ||
| Home state expanded UI eligibility for school | .64 | .087 |
| closure/lost childcare | [.39, 1.07] | |
| Home state stopped pandemic unemployment | 1.14 | .680 |
| Programs | [.62, 2.11] | |
| Home state weekly UI maximum | 1.00 | .710 |
| [1.00, 1.00] | ||
| 7-day average new COVID-19 cases (per 100,000 | .96∗∗ | .003 |
| population) | [.94, .99] | |
| 7-day average COVID-19 deaths (per 100,000 | 12.15∗ | .010 |
| population) | [1.81, 81.69] | |
| Month of participation | .80 | .353 |
| [.51, 1.27] |
||
| Pseudo R2 | .341 | |
| Log likelihood | −419.7183 | |
| N | 1998 | |
Note: Exponentiated coefficients (odds ratios) with 95% confidence intervals in brackets. Standard errors clustered at the state-level.
Appendix D. Regressions of Depressive Symptoms and Binge Drinking on COVID-19 Bereavement and Study Variables (n = 1998)
| Depressive Symptoms |
Binge Drinking |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
| Negative Binomial |
Negative Binomial + IPTW Adjusted |
Ordered Logit |
Ordered Logit + IPTW Adjusted |
|||||
| IRR [95% CI] | p-value | IRR [95% CI] | p-value | OR [95% CI] | p-value | OR [95% CI] | p-value | |
| COVID-19 Bereavement | 1.33 | .001 | 1.21 | .013 | 1.72 | .003 | 1.70 | .004 |
| [1.12, 1.57] | [1.04, 1.40] | [1.21, 2.45] | [1.19, 2.45] | |||||
| Race-Ethnicity (reference=white) | ||||||||
| American Indian/Alaska Native | .86 | .456 | 1.10 | .635 | .72 | .440 | 1.28 | .752 |
| [.57, 1.29] | [.75, 1.61] | [.31, 1.67] | [.28, 5.77] | |||||
| Asian | .84 | .127 | .97 | .853 | .47 | .004 | .51 | .218 |
| [.67, 1.05] | [.72, 1.32] | [.29, .78] | [.18, 1.48] | |||||
| Black/African American | .99 | .902 | .83 | .080 | 1.02 | .909 | .90 | .702 |
| [.85, 1.15] | [.67, 1.02] | [.74, 1.40] | [.52, 1.54] | |||||
| Hispanic/Latinx | .93 | .290 | .91 | .329 | 1.01 | .966 | 1.29 | .293 |
| [.82, 1.06] | [.75, 1.10] | [.76, 1.34] | [.80, 2.07] | |||||
| Other | .96 | .837 | .99 | .980 | .37 | .101 | .23 | .249 |
| [.64, 1.43] | [.57, 1.73] | [.11, 1.21] | [.02, 2.82] | |||||
| Female (reference=male) | 1.04 | .474 | 1.01 | .944 | .50 | <.001 | .51 | .003 |
| [.93, 1.17] | [.85, 1.20] | [.39, .64] | [.32, .80] | |||||
| Sexual orientation (reference=straight) | ||||||||
| Gay/lesbian | 1.03 | .856 | 1.15 | .248 | .67 | .289 | .74 | .742 |
| [.73, 1.46] | [.91, 1.45] | [.32, 1.41] | [.12, 4.57] | |||||
| Bisexual | 1.10 | .384 | .90 | .263 | .94 | .809 | .64 | .310 |
| [.89, 1.37] | [.74, 1.08] | [.57, 1.54] | [.28, 1.51] | |||||
| Other | 1.14 | .603 | 1.21 | .311 | 1.04 | .952 | 1.57 | .529 |
| [.69, 1.89] | [.84, 1.74] | [.33, 3.24] | [.39, 6.35] | |||||
| Age (reference=65+ years old) | ||||||||
| 18–24 years old | 2.27 | <.001 | 2.40 | <.001 | 5.45 | <.001 | 7.77 | <.001 |
| [1.81, 2.84] | [1.63, 3.55] | [3.12, 9.51] | [3.35, 18.06] | |||||
| 25–34 years old | 1.93 | <.001 | 1.64 | .006 | 6.85 | <.001 | 11.53 | <.001 |
| [1.56, 2.38] | [1.15, 2.35] | [4.08, 11.52] | [5.37, 24.77] | |||||
| 35–44 years old | 1.69 | <.001 | 1.27 | .205 | 5.25 | <.001 | 7.27 | <.001 |
| [1.37, 2.08] | [.88, 1.83] | [3.14, 8.76] | [3.45, 15.36] | |||||
| 45–54 years old | 1.50 | <.001 | 1.52 | .016 | 3.67 | <.001 | 3.29 | .003 |
| [1.22, 1.84] | [1.08, 2.13] | [2.19, 6.15] | [1.52, 7.14] | |||||
| 55–64 years old | 1.09 | .361 | .98 | .933 | 2.32 | <.001 | 2.78 | .005 |
| [.91, 1.30] | [.69, 1.41] | [1.47, 3.69] | [1.36, 5.66] | |||||
| Relationship status (reference=married) | ||||||||
| Single | 1.10 | .115 | 1.14 | .092 | .99 | .915 | 1.05 | .826 |
| [.98, 1.24] | [.98, 1.32] | [.75, 1.29] | [.67, 1.65] | |||||
| Committed relationship | 1.11 | .175 | 1.32 | .022 | 1.05 | .791 | .64 | .086 |
| [.96, 1.28] | [1.04, 1.67] | [.75, 1.45] | [.39, 1.06] | |||||
| Divorced | .96 | .668 | .93 | .509 | 1.50 | .047 | 1.29 | .368 |
| [.81, 1.15] | [.75, 1.16] | [1.01, 2.24] | [.74, 2.24] | |||||
| Widowed | 1.03 | .847 | 1.02 | .893 | .65 | .258 | .94 | .914 |
| [.79, 1.33] | [.76, 1.37] | [.30, 1.38] | [.32, 2.81] | |||||
| Separated | .96 | .848 | 1.14 | .546 | .98 | .962 | .50 | .405 |
| [.66, 1.40] | [.75, 1.72] | [.43, 2.25] | [.10, 2.53] | |||||
| Socioeconomic Status | ||||||||
| Education (reference=Less than high school diploma) | ||||||||
| High school diploma/GED | .95 | .513 | 1.00 | .965 | .76 | .115 | 1.01 | .960 |
| [.82, 1.11] | [.83, 1.22] | [.53, 1.07] | [.59, 1.74] | |||||
| Some college | .99 | .938 | 1.23 | .048 | .94 | .755 | 1.41 | .250 |
| [.84, 1.17] | [1.00, 1.50] | [.65, 1.37] | [.79, 2.53] | |||||
| Associate's degree | 1.03 | .747 | .99 | .931 | .96 | .877 | 1.15 | .741 |
| [.84, 1.27] | [.74, 1.32] | [.61, 1.53] | [.49, 2.72] | |||||
| Bachelor's degree | .96 | .676 | 1.04 | .790 | .92 | .685 | 1.49 | .247 |
| [.80, 1.16] | [.80, 1.34] | [.60, 1.39] | [.76, 2.92] | |||||
| Graduate degree | .89 | .271 | 1.17 | .348 | 1.06 | .818 | 1.65 | .200 |
| [.71, 1.10] | [.84, 1.61] | [.65, 1.72] | [.77, 3.57] | |||||
| Annual Household Income (reference=<$25,000) | ||||||||
| $25,000-$49,999 | 1.09 | .227 | 1.07 | .501 | 1.05 | .761 | .70 | .221 |
| [.95, 1.25] | [.88, 1.29] | [.76, 1.45] | [.39, 1.24] | |||||
| $50,000-$74,999 | 1.00 | .994 | 1.04 | .746 | 1.19 | .333 | .69 | .275 |
| [.86, 1.16] | [.84, 1.28] | [.84, 1.68] | [.36, 1.34] | |||||
| $75,000-$99,999 | .94 | .443 | .85 | .214 | 1.36 | .114 | .81 | .571 |
| [.79, 1.11] | [.66, 1.10] | [.93, 2.00] | [.40, 1.65] | |||||
| $100,000-$149,999 | 1.08 | .391 | .96 | .772 | 1.29 | .226 | .55 | .098 |
| [.90, 1.30] | [.72, 1.28] | [.85, 1.96] | [.27, 1.12] | |||||
| $150,000-$199,999 | .92 | .469 | .60 | .006 | .95 | .834 | .72 | .459 |
| [.73, 1.15] | [.42, 0.87] | [.56, 1.59] | [.31, 1.70] | |||||
| $200,000+ | 1.24 | .075 | 1.06 | .724 | 1.24 | .429 | .70 | .407 |
| [.98, 1.57] | [.77, 1.46] | [.72, 2.13] | [.30, 1.63] | |||||
| Employment status (reference=full-time) | ||||||||
| Part-time | .96 | .546 | .86 | .140 | .87 | .386 | .90 | .703 |
| [.83, 1.11] | [.71, 1.05] | [.64, 1.19] | [.52, 1.56] | |||||
| Unemployed | 1.01 | .864 | 1.05 | .634 | .64 | .009 | .49 | .018 |
| [.88, 1.17] | [.85, 1.31] | [.46, .89] | [.27, 0.89] | |||||
| Retired | .80 | .014 | .65 | .027 | .79 | .297 | .51 | .058 |
| [.66, 0.96] | [.45, .95] | [.51, 1.22] | [.26, 1.02] | |||||
| Disabled | 1.21 | .077 | 1.31 | .050 | .79 | .356 | .44 | .046 |
| [.98, 1.50] | [1.00, 1.72] | [.48, 1.30] | [.19, .99] | |||||
| Essential worker | 1.02 | .741 | 1.14 | .114 | .97 | .824 | 1.36 | .175 |
| [.90, 1.15] | [.97, 1.34] | [.75, 1.26] | [.87, 2.12] | |||||
| Tested positive for COVID-19 | 1.26 | .021 | 1.31 | .008 | 1.37 | .118 | 1.56 | .081 |
| [1.04, 1.53] | [1.07, 1.60] | [.92, 2.04] | [.95, 2.57] | |||||
| Self-rated health | .76 | <.001 | .75 | <.001 | 1.03 | .618 | 1.11 | .331 |
| [.72, .79] | [.69, 0.81] | [.92, 1.15] | [.90, 1.36] | |||||
| Days smoking past month | 1.01 | <.001 | 1.02 | <.001 | 1.05 | <.001 | 1.05 | <.001 |
| [1.01, 1.02] | [1.01, 1.02] | [1.04, 1.06] | [1.04, 1.07] | |||||
| Home state never issued stay-at-home | .82 | .806 | 2.98 | .168 | .06 | .170 | .00 | .042 |
| order | [.17, 3.96] | [.63, 14.09] | [.00, 3.27] | [.00, 0.79] | ||||
| Home state no mask mandate in public | .94 | .738 | .68 | .071 | .46 | .084 | .17 | .014 |
| spaces | [.63, 1.38] | [.45, 1.03] | [.19, 1.11] | [.04, 0.70] | ||||
| Home state expanded UI eligibility for | .84 | .805 | .53 | .405 | .29 | .473 | .02 | .018 |
| school closure/lost childcare | [.20, 3.49] | [.12, 2.36] | [.01, 8.38] | [.00, .50] | ||||
| Home state stopped pandemic | 1.21 | .581 | .32 | .026 | 2.15 | .346 | 2.33 | .487 |
| unemployment programs | [.62, 2.35] | [.12, .87] | [.44, 10.60] | [.22, 25.15] | ||||
| Home state weekly UI maximum | 1.00 | .815 | 1.00 | .382 | 1.01 | .170 | 1.03 | <.001 |
| [.99, 1.00] | [.99, 1.00] | [1.00, 1.02] | [1.01, 1.05] | |||||
| 7-day average new COVID-19 cases | 1.00 | .833 | 1.01 | .195 | 1.00 | .774 | 1.00 | .905 |
| (per 100,000 population) | [.99, 1.01] | [.99, 1.03] | [.97, 1.03] | [.95, 1.06] | ||||
| 7-day average COVID-19 deaths (per | .76 | .413 | .45 | .050 | .81 | .764 | 2.95 | .404 |
| 100,000 population) | [.40, 1.45] | [.20, 1.00] | [.20, 3.28] | [.23, 37.50] | ||||
| Month of participation | 1.04 | .505 | 1.04 | .523 | .89 | .360 | .78 | .291 |
| [.93, 1.15] |
[.91, 1.19] |
[.70, 1.14] |
[.49, 1.24] |
|||||
| Pseudo R2 | .05 | .08 | .10 | .20 | ||||
| Log likelihood | −5432.83 | −11200.77 | −2243.81 | −4141.66 | ||||
| N | 1998 | 1998 | 1998 | 1998 | ||||
Note: Exponentiated coefficients (incidence rate ratios and odds ratios) with 95% confidence intervals in brackets. All models include controls for respondents' state of residence (omitted in the interest of space). Models 2 and 4 include inverse probability of treatment weighting (IPTW) to account for selection.
Appendix E. Regressions of Depressive Symptoms and Binge Drinking on Essential Worker Status x COVID-19 Bereavement (n = 1998)
| Depressive Symptoms |
Binge Drinking |
|||
|---|---|---|---|---|
| Model 1 |
Model 2 |
|||
| Negative Binomial + IPTW Adjusted |
Ordered Logit + IPTW Adjusted |
|||
| IRR [95% CI] | p-value | OR [95% CI] | p-value | |
| COVID-19 Bereavement | 1.13 | .170 | 1.28 | .230 |
| [.95, 1.35] | [.86, 1.92] | |||
| Less education essential worker | 1.07 | .416 | .77 | .303 |
| [.91, 1.25] | [.48, 1.26] | |||
| More education essential worker | .97 | .805 | 1.37 | .390 |
| [.75, 1.25] | [.67, 2.81] | |||
| Less education essential worker x | 1.03 | .827 | 2.19 | .091 |
| bereavement | [.77, 1.39] | [.88, 5.43] | ||
| More education essential worker x | 2.09 | .001 | 3.04 | .060 |
| bereavement | [1.35, 3.22] | [.95, 9.69] | ||
| Race-Ethnicity (reference=white) | ||||
| American Indian/Alaska Native | 1.07 | .757 | 1.12 | .881 |
| [.71, 1.60] | [.25, 4.94] | |||
| Asian | .97 | .839 | .54 | .262 |
| [.72, 1.31] | [.18, 1.59] | |||
| Black/African American | .85 | .126 | .90 | .692 |
| [.68, 1.05] | [.52, 1.54] | |||
| Hispanic/Latinx | .94 | .556 | 1.33 | .250 |
| [.77, 1.15] | [.82, 2.14] | |||
| Other | .99 | .973 | .20 | .285 |
| [.58, 1.68] | [.01, 3.80] | |||
| Female (reference=male) | 1.01 | .914 | .47 | <.001 |
| [.85, 1.20] | [.30, .74] | |||
| Sexual orientation (reference=straight) | ||||
| Gay/lesbian | 1.23 | .079 | .83 | .850 |
| [.98, 1.54] | [.12, 5.55] | |||
| Bisexual | .93 | .451 | .69 | .412 |
| [.77, 1.12] | [.29, 1.66] | |||
| Other | 1.27 | .181 | 1.82 | .399 |
| [.90, 1.80] | [.45, 7.39] | |||
| Age (reference=65+ years old) | ||||
| 18–24 years old | 2.38 | <.001 | 7.51 | <.001 |
| [1.61, 3.54] | [3.37, 16.73] | |||
| 25–34 years old | 1.65 | .007 | 11.01 | <.001 |
| [1.15, 2.37] | [5.22, 23.25] | |||
| 35–44 years old | 1.32 | .157 | 7.43 | <.001 |
| [.90, 1.93] | [3.55, 15.55] | |||
| 45–54 years old | 1.45 | .036 | 2.84 | .009 |
| [1.03, 2.05] | [1.30, 6.18] | |||
| 55–64 years old | .98 | .903 | 2.66 | .005 |
| [.67, 1.42] | [1.34, 5.25] | |||
| Relationship status (reference=married) | ||||
| Single | 1.14 | .101 | 1.07 | .775 |
| [.97, 1.33] | [.68, 1.69] | |||
| Committed relationship | 1.28 | .044 | .62 | .066 |
| [1.01, 1.62] | [.37, 1.03] | |||
| Divorced | .92 | .446 | 1.32 | .331 |
| [.74, 1.14] | [.76, 2.29] | |||
| Widowed | 1.02 | .918 | .93 | .904 |
| [.76, 1.36] | [.31, 2.84] | |||
| Separated | 1.04 | .877 | .41 | .188 |
| [.65, 1.65] | [.11, 1.54] | |||
| Socioeconomic Status | ||||
| Annual Household Income (reference=<$25,000) | ||||
| $25,000-$49,999 | 1.11 | .292 | .73 | .269 |
| [.92, 1.34] | [.41, 1.28] | |||
| $50,000-$74,999 | 1.03 | .780 | .67 | .225 |
| [.83, 1.28] | [.35, 1.28] | |||
| $75,000-$99,999 | .85 | .199 | .85 | .636 |
| [.66, 1.09] | [.43, 1.67] | |||
| $100,000-$149,999 | .98 | .868 | .57 | .105 |
| [.74, 1.29] | [.28, 1.13] | |||
| $150,000-$199,999 | .60 | .006 | .72 | .447 |
| [.41, .86] | [.32, 1.66] | |||
| $200,000+ | 1.14 | .397 | .83 | .651 |
| [.84, 1.55] | [.38, 1.84] | |||
| Employment status (reference=full-time) | ||||
| Part-time | .89 | .195 | .90 | .695 |
| [.74, 1.06] | [.52, 1.55] | |||
| Unemployed | 1.09 | .407 | .47 | .011 |
| [.89, 1.35] | [.26, .84] | |||
| Retired | .68 | .040 | .51 | .048 |
| [.47, .98] | [.26, 1.00] | |||
| Disabled | 1.36 | .016 | .39 | .020 |
| [1.06, 1.75] | [.18, 0.86] | |||
| Tested positive for COVID-19 | 1.24 | .034 | 1.40 | .209 |
| [1.02, 1.52] | [.83, 2.38] | |||
| Self-rated health | .74 | <.001 | 1.10 | .357 |
| [.69, .81] | [.89, 1.36] | |||
| Days smoking past month | 1.01 | <.001 | 1.05 | <.001 |
| [1.01, 1.02] | [1.04, 1.07] | |||
| Home state never issued stay-at-home | 2.74 | .199 | .00 | .017 |
| order | [.59, 12.81] | [.00, .33] | ||
| Home state no mask mandate in public | .73 | .120 | .22 | .022 |
| spaces | [.49, 1.09] | [.06, .80] | ||
| Home state expanded UI eligibility for | .59 | .501 | .02 | .023 |
| school closure/lost childcare | [.13, 2.73] | [.00, .60] | ||
| Home state stopped pandemic | .31 | .021 | 2.46 | .456 |
| unemployment programs | [.11, 0.84] | [.23, 26.18] | ||
| Home state weekly UI maximum | 1.00 | .274 | 1.03 | .001 |
| [.99, 1.00] | [1.01, 1.05] | |||
| 7-day average new COVID-19 cases | 1.01 | .168 | 1.00 | .911 |
| (per 100,000 population) | [.99, 1.03] | [.95, 1.06] | ||
| 7-day average COVID-19 deaths (per | .36 | .008 | 3.05 | .367 |
| 100,000 population) | [.17, .76] | [.27, 34.53] | ||
| Month of participation | 1.03 | .677 | .79 | .312 |
| [.90, 1.18] |
[.50, 1.25] |
|||
| Pseudo R2 | .08 | .21 | ||
| Log likelihood | −11180.01 | −4121.96 | ||
| N | 1998 | 1998 | ||
Note: Exponentiated coefficients (incidence rate ratios and odds ratios) with 95% confidence intervals in brackets. Models include controls for respondents' state of residence and inverse probability of treatment weighting (IPTW) to account for selection.
Appendix F. Regressions of Depressive Symptoms and Binge Drinking on Essential Worker Status x COVID-19 Bereavement (n = 1998)
| Depressive Symptoms |
Binge Drinking |
|||
|---|---|---|---|---|
| Model 1 |
Model 2 |
|||
| Negative Binomial + IPTW Adjusted |
Ordered Logit + ITPW Adjusted |
|||
| IRR [95% CI] | p-value | OR [95% CI] | p-value | |
| COVID-19 Bereavement | 1.11 | .268 | 1.33 | .184 |
| [.92, 1.34] | [.87, 2.02] | |||
| Lower income essential worker | 1.07 | .508 | .70 | .222 |
| [.88, 1.30] | [.40, 1.24] | |||
| Higher income essential worker | .96 | .622 | 1.07 | .789 |
| [.80, 1.14] | [.64, 1.80] | |||
| Lower income essential worker x | .75 | .213 | 1.28 | .714 |
| bereavement | [.47, 1.18] | [.34, 4.86] | ||
| Higher income essential worker x | 1.64 | .002 | 2.79 | .012 |
| bereavement | [1.19, 2.25] | [1.26, 6.20] | ||
| Race-Ethnicity (reference=white) | ||||
| American Indian/Alaska Native | 1.03 | .891 | 1.29 | .729 |
| [.71, 1.49] | [.31, 5.35] | |||
| Asian | 1.02 | .889 | .58 | .340 |
| [.75, 1.40] | [.19, 1.79] | |||
| Black/African American | .86 | .164 | .96 | .880 |
| [.70, 1.06] | [.57, 1.62] | |||
| Hispanic/Latinx | .94 | .560 | 1.39 | .195 |
| [.77, 1.15] | [.85, 2.27] | |||
| Other | 1.03 | .930 | .19 | .318 |
| [.59, 1.80] | [.01, 4.87] | |||
| Female (reference=male) | 1.05 | .546 | .55 | .010 |
| [.89, 1.25] | [.34, 0.86] | |||
| Sexual orientation (reference=straight) | ||||
| Gay/lesbian | 1.22 | .132 | .86 | .875 |
| [.94, 1.57] | [.13, 5.66] | |||
| Bisexual | .94 | .543 | .64 | .299 |
| [.77, 1.15] | [.27, 1.49] | |||
| Other | 1.19 | .353 | 1.94 | .389 |
| [.82, 1.72] | [.43, 8.75] | |||
| Age (reference=65+ years old) | ||||
| 18–24 years old | 2.32 | <.001 | 7.26 | <.001 |
| [1.55, 3.48] | [3.14, 16.77] | |||
| 25–34 years old | 1.58 | .015 | 10.91 | <.001 |
| [1.09, 2.28] | [4.98, 23.89] | |||
| 35–44 years old | 1.28 | .195 | 7.43 | <.001 |
| [.88, 1.85] | [3.47, 15.90] | |||
| 45–54 years old | 1.37 | .077 | 2.74 | .014 |
| [.97, 1.96] | [1.22, 6.11] | |||
| 55–64 years old | .95 | .773 | 2.52 | .011 |
| [.64, 1.39] | [1.23, 5.15] | |||
| Relationship status (reference=married) | ||||
| Single | 1.19 | .041 | 1.24 | .384 |
| [1.01, 1.41] | [.77, 2.00] | |||
| Committed relationship | 1.38 | .009 | .74 | .208 |
| [1.08, 1.76] | [.46, 1.18] | |||
| Divorced | .95 | .636 | 1.46 | .175 |
| [.76, 1.18] | [.84, 2.53] | |||
| Widowed | 1.01 | .944 | .99 | .984 |
| [.76, 1.34] | [.34, 2.88] | |||
| Separated | 1.18 | .478 | .46 | .273 |
| [.75, 1.85] | [.11, 1.86] | |||
| Socioeconomic Status | ||||
| Education (reference=Less than high school diploma) | ||||
| High school diploma/GED | 1.04 | .644 | 1.10 | .733 |
| [.87, 1.26] | [.64, 1.90] | |||
| Some college | 1.25 | .020 | 1.44 | .218 |
| [1.04, 1.51] | [.80, 2.59] | |||
| Associate's degree | .99 | .925 | 1.31 | .532 |
| [.73, 1.33] | [.56, 3.02] | |||
| Bachelor's degree | .93 | .570 | 1.34 | .384 |
| [.71, 1.20] | [.69, 2.61] | |||
| Graduate degree | 1.06 | .700 | 1.32 | .490 |
| [.80, 1.40] | [.60, 2.88] | |||
| Employment status (reference=full-time) | ||||
| Part-time | .86 | .140 | .86 | .595 |
| [.70, 1.05] | [.50, 1.49] | |||
| Unemployed | 1.03 | .801 | .52 | .031 |
| [.82, 1.29] | [.29, .94] | |||
| Retired | .65 | .027 | .52 | .062 |
| [.45, .95] | [.26, 1.03] | |||
| Disabled | 1.32 | .036 | .46 | .044 |
| [1.02, 1.72] | [.21, .98] | |||
| Tested positive for COVID-19 | 1.26 | .018 | 1.49 | .131 |
| [1.04, 1.53] | [.89, 2.49] | |||
| Self-rated health | .75 | <.001 | 1.13 | .227 |
| [.69, .82] | [.93, 1.37] | |||
| Days smoking past month | 1.02 | <.001 | 1.05 | <.001 |
| [1.01, 1.02] | [1.04, 1.07] | |||
| Home state never issued stay-at-home | 2.67 | .225 | .00 | .029 |
| order | [.55, 13.05] | [.00, 0.55] | ||
| Home state no mask mandate in public | .62 | .045 | .17 | .012 |
| spaces | [.39, 0.99] | [.04, 0.67] | ||
| Home state expanded UI eligibility for | .45 | .294 | .02 | .032 |
| school closure/lost childcare | [.10, 2.00] | [.00, .72] | ||
| Home state stopped pandemic | .32 | .035 | 2.25 | .525 |
| unemployment programs | [.11, 0.92] | [.18, 27.46] | ||
| Home state weekly UI maximum | 1.00 | .573 | 1.03 | .001 |
| [1.00, 1.00] | [1.01, 1.04] | |||
| 7-day average new COVID-19 cases | 1.01 | .268 | 1.01 | .782 |
| (per 100,000 population) | [.99, 1.03] | [.95, 1.07] | ||
| 7-day average COVID-19 deaths (per | .46 | .049 | 3.59 | .328 |
| 100,000 population) | [.21, 1.00] | [.28, 46.41] | ||
| Month of participation | 1.09 | .204 | .80 | .330 |
| [.95, 1.24] |
[.51, 1.26] |
|||
| Pseudo R2 | .08 | .21 | ||
| Log likelihood | −11203.58 | −4124.86 | ||
| N | 1998 | 1998 | ||
Note: Exponentiated coefficients (incidence rate ratios and odds ratios) with 95% confidence intervals in brackets. Models include controls for respondents' state of residence and inverse probability of treatment weighting (IPTW) to account for selection.
References
- Ai C.R., Norton E.C. Interaction terms in logit and probit models. Economics Letters. 2003;80:123–129. [Google Scholar]
- Artiga S., Corallo B., Pham O. Kaiser Family Foundation; 2020. Racial disparities in COVID-19: Key findings from available data and analysis. [Google Scholar]
- Artiga S., Orgera K. Kaiser Family Foundation; 2020. COVID-19 presents significant risks for American Indian and Alaska native people. [Google Scholar]
- Associated Press . NBC News; 2020. Covid pandemic turned 2020 into deadliest year in U.S. history, CDC finds. [Google Scholar]
- Bassett M.T., Chen J.T., Krieger N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Medicine. 2020;17:1–14. doi: 10.1371/journal.pmed.1003402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman A., Schieman S. Social estrangement and psychological distress before and during the COVID-19 pandemic: Patterns of change in Canadian workers. Journal of Health and Social Behavior. 2020;61:398–417. doi: 10.1177/0022146520970190. [DOI] [PubMed] [Google Scholar]
- Bierman A., Upenieks L., Glavin P., Schieman S. Accumulation of economic hardship and health during the COVID-19 pandemic: Social causation or selection? Social Science & Medicine. 2021 doi: 10.1016/j.socscimed.2021.113774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blau F.D., Koebe J., Meyerhofer P.A. NBER; 2020. Who are essential and frontline workers? [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer J.D., Sparkes A.C. Young people living with parental bereavement: Insights from an ethnographic study of a UK childhood bereavement service. Social Science & Medicine. 2011;72:283–290. doi: 10.1016/j.socscimed.2010.10.032. [DOI] [PubMed] [Google Scholar]
- Buckner J.H., Chowell G., Springborn M.R. Dynamic prioritization of COVID-19 vaccines when social distancing is limited for essential workers. Proceedings of the National Academy of Sciences. 2021;118 doi: 10.1073/pnas.2025786118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D. Gender, preloss marital dependence, and older adults' adjustment to widowhood. Journal of Marriage and Family. 2004;66:220–235. [Google Scholar]
- Carr D. Who's to blame? Perceived responsibility for spousal death and psychological distress among older widowed persons. Journal of Health and Social Behavior. 2009;50:359–375. doi: 10.1177/002214650905000308. [DOI] [PubMed] [Google Scholar]
- Carr D., Boerner K., Moorman S. Bereavement in the time of coronavirus: Unprecedented challenges demand novel interventions. Journal of Aging & Social Policy. 2020;32:425–431. doi: 10.1080/08959420.2020.1764320. [DOI] [PubMed] [Google Scholar]
- Chen Y.-H., Glymour M., Riley A., Balmes J., Duchowny K., Harrison R., Matthay E., Bibbins-Domingo K. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. MedRxiv Prepr. 2021;1–10 doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston S.A.P., Natale G., Link B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: A examination of the emergence of social inequalities. Social Science & Medicine. 2021;268 doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M., Lane R., Petrosky E., Wiley J., Christensen A., Njai R., Weaver M., Robbins R., Facer-Childs E., Barger L., Czeisler C., Howard M., Rajaratnam S. Centers for Disease Control; 2020. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020, morbidity and mortality weekly report. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannefer D. Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2003;58:S327–S337. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Donnelly R., Farina M.P. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Social Science & Medicine. 2021;269:113557. doi: 10.1016/j.socscimed.2020.113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisma M.C., Tamminga A., Smid G.E., Boelen P.A. Acute grief after deaths due to COVID-19, natural causes and unnatural causes: An empirical comparison. Journal of Affective Disorders. 2021;278:54–56. doi: 10.1016/j.jad.2020.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faust J.S., Krumholz H.M., Du C., Mayes K.D., Lin Z., Gilman C., Walensky R.P. All-cause excess mortality and COVID-19–related mortality among US adults aged 25-44 Years, March-July 2020. Journal of the American Medical Association. 2021;325:785–787. doi: 10.1001/jama.2020.24243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd F.J., Seltzer M.M., Greenberg J.S., Song J. Parental bereavement during mid-to-later life: Pre-to-Post- bereavement functioning and intrapersonal resources for coping. Psychology and Aging. 2013;28:402–413. doi: 10.1037/a0029986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk C., Tyson A. Pew Research Center; 2021. Growing share of Americans say they plan to get a COVID-19 vaccine – or already have. [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Annals of Epidemiology. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Greenberg-Worisek A.J., Kurani S., Finney Rutten L., Blake K.D., Moser R.P., Hesse B.W. Tracking healthy people 2020 internet, broadband, and mobile device access goals: An update using data from the health information national trends survey. Journal of Medical Internet Research. 2019;21 doi: 10.2196/13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirano K., Imbens G.W. Estimation of causal effects using propensity score weighting: An application to data on right heart catheterization. Health Services & Outcomes Research Methodology. 2001;2:259–278. [Google Scholar]
- Johnson R.T., Lund D.A., Dimond M.F. Stress, self-esteem and coping during bereavement among the elderly. Social Psychology Quarterly. 1986;49:273–279. [Google Scholar]
- Kessler R.C. A strategy for studying differential vulnerability to the psychological consequences of stress. Journal of Health and Social Behavior. 1979;20:100–108. [PubMed] [Google Scholar]
- Keyes K.M., Westreich D. UK Biobank, big data, and the consequences of non-representativeness. Lancet. 2019;39:1297. doi: 10.1016/S0140-6736(18)33067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar R. Pew Research Center; 2020. Unemployment rose higher in three months of COVID-19 than it did in two years of the Great Recession. [Google Scholar]
- Lehman D.R., Wortman C.B., Williams A.F. Long-term effects of losing a spouse or child in a motor vehicle crash. Journal of Personality and Social Psychology. 1987;52:219–231. doi: 10.1037//0022-3514.52.1.218. [DOI] [PubMed] [Google Scholar]
- Levine S.Z. Evaluating the seven-item center for epidemiologic studies depression scale short-form: A longitudinal US community study. Social Psychiatry and Psychiatric Epidemiology. 2013;48:1519–1526. doi: 10.1007/s00127-012-0650-2. [DOI] [PubMed] [Google Scholar]
- Lopez P.J., Neely A.H. Fundamentally uncaring: The differential multi-scalar impacts of COVID-19 in the. US Social Science & Medicine. 2021;272 doi: 10.1016/j.socscimed.2021.113707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D., Denton N.A. Harvard University Press; Cambridge, MA: 1993. American apartheid: Segregation and the making of the underclass. [Google Scholar]
- McKinlay J.B., McKinlay S.M. The questionable contribution of medical measures to the decline of mortality in the United States in the twentieth century. Milbank Memorial Fund Quarterly - Health & Society. 1977;55:405–428. [PubMed] [Google Scholar]
- McLeod J. Childhood parental loss and adult depression. Journal of Health and Social Behavior. 1991;32:205–220. [PubMed] [Google Scholar]
- McNicholas C., Poydock M. Economic Policy Institute; 2020. Who are essential workers? A comprehensive look at their wages, demographics, and unionization rates. [Google Scholar]
- Moen P., Lam J., Ammons S., Kelly E.L. Time work by overworked professionals: Strategies in response to the stress of higher status. Work and Occupations. 2013;40:79–114. doi: 10.1177/0730888413481482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York Times Coronavirus in the U.S.: Latest map and case count. 2020. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#states WWW Document. 11.24.20.
- Parker K., Minkin R., Bennett J. Pew Research Center; 2020. Economic fallout from COVID-19 continues to hit lower-income Americans the hardest. [Google Scholar]
- Pearlin L.I., Bierman A. In: Handbook of the sociology of mental health. Aneshensel C.S., Phelan J.C., Bierman A., editors. Springer; New York: 2013. Current issues and future directions in research into the stress process; pp. 325–340. [Google Scholar]
- Pearlin L.I., Schieman S., Fazio E.M., Meersman S.C. Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raifman J., Nocka K., Jones D., Bor J., Lipson S., Jay J., Chan P. COVID-19 U.S. State policy database. 2020. www.tinyurl.com/statepolicies [WWW Document]. URL. 11.24.20.
- Robins J.M. Association, causation, and marginal structural models. Synthese. 1999;121:151–179. [Google Scholar]
- Robins J.M., Hernán M.Á., Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- Rogers T., Rogers C., VanSant-Webb E., Gu L., Yan B., Qeadan F. Racial disparities in COVID-19 mortality among essential workers in the United States. World med. Health Policy. 2020;12:311–327. doi: 10.1002/wmh3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Rosenfield S., Lennon M.C., White H.R. The self and mental health: Self-salience and the emergence of internalizing and externalizing problems. Journal of Health and Social Behavior. 2005;46:323–340. doi: 10.1177/002214650504600402. [DOI] [PubMed] [Google Scholar]
- Shim R.S., Starks S.M. COVID-19, structural racism, and mental health inequities: Policy implications for an emerging syndemic. Psychiatric Services. 2021;1–6 doi: 10.1176/appi.ps.202000725. [DOI] [PubMed] [Google Scholar]
- Sloan M., Haner M., Graham A., Cullen F., Pickett J., Johnson C.L. Pap. Univ. South Fla; 2020. Pandemic emotions: The extent, correlates, and mental health consequences of personal and altruistic fear of COVID-19. Work; pp. 1–46. [Google Scholar]
- Stokes A.C., Lundberg D.J., Elo I.T., Hempstead K., Bor J., Preston S.H. COVID-19 and excess mortality in the United States: A county-level analysis. PLoS Medicine. 2021 doi: 10.1371/journal.pmed.1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M., Schut H., Stroebe W. Health outcomes of bereavement. Lancet. 2007;370:1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- Thoemmes F., Ong A.D. A primer on inverse probability of treatment weighting and marginal structural models. Emerg. Adulthood. 2016;4:40–59. [Google Scholar]
- Toh W.L., Meyer D., Phillipou A., Tan E.J., Van Rheenen T.E., Neill E., Rossell S.L. Mental health status of healthcare versus other essential workers in Australia amidst the COVID-19 pandemic: Initial results from the collate project. Psychiatry Research. 2021;298:113822. doi: 10.1016/j.psychres.2021.113822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D. Black deaths matter: Race, relationship loss, and effects on survivors. Journal of Health and Social Behavior. 2017;58:405–420. doi: 10.1177/0022146517739317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D., Chen M.D. Effects of a parent's death on adult children: Relationship salience and reaction to loss. American Sociological Review. 1994;59:152–168. [Google Scholar]
- Umberson D., Wortman C.B., Kessler R.C. Widowhood and depression: Explaining long-term gender differences in vulnerability. Journal of Health and Social Behavior. 1992;33:10–24. [PubMed] [Google Scholar]
- U.S. Census Bureau Annual Social and Economic Supplement. Current Population Survey. 2016 [Google Scholar]
- Verdery A., Smith-Greenaway E., Margolis R., Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences. 2020;117:17695–17701. doi: 10.1073/pnas.2007476117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakam G.K., Montgomery J.R., Biesterveld B.E., Brown C.S. Not dying alone — modern compassionate care in the covid-19 pandemic. New England Journal of Medicine. 2020;382:e881–e882. doi: 10.1056/NEJMp2007781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H., Verdery, A.M., Margolis, R., Smith-Greenaway, E., Forthcoming. Bereavement from COVID-19, gender, and reports of depression among older adults in Europe. Journals of Gerontology Series . [DOI] [PMC free article] [PubMed]
- Williams J.C., Anderson N., Holloway T., Samford E., III, Eugene J., Isom J. Reopening the United States: Black and hispanic workers are essential and expendable again. American Journal of Public Health. 2020;110:1506–1508. doi: 10.2105/AJPH.2020.305879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D.H. Excess deaths from COVID-19 and other causes, march-July 2020. Journal of the American Medical Association. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng J., Morstead T., Sin N., Klaiber P., Umberson D., Kamble S., DeLongis A. Psychological distress in North America during COVID-19: The role of Pandemic-related stressors. Social Science & Medicine. 2021;270:113687. doi: 10.1016/j.socscimed.2021.113687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in wuhan, China: A retrospective cohort study. The Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]