Abstract
Objective
There have been no reports suggesting a relationship between the COVID-19 mRNA vaccines that encodes the spike glycoprotein of SARS-CoV-2 and cerebrovascular disease. A case of repeated cardioembolic stroke after vaccination with the BNT162b2 (Pfizer) COVID-19 mRNA vaccine is presented.
Methods
Imaging and laboratory findings, treatment decisions, and the outcome of this case are presented.
Results
An 83-year-old Japanese woman developed right hemiplegia and motor aphasia three days after receiving her first dose of the BNT162b2 (Pfizer) COVID-19 mRNA vaccine. She had been taking rivaroxaban for persistent atrial fibrillation for 10 years, but had no symptomatic ischemic strokes. On magnetic resonance imaging (MRI) the left middle cerebral artery (MCA) was occluded. Intravenous recombinant tissue-plasminogen activator (rt-PA) therapy and mechanical thrombectomy were performed, and she recovered almost fully. However, three days after the second dose, she developed left hemiplegia and left hemispatial neglect. MRI showed occlusion of the right MCA. Only mechanical thrombectomy was performed again, but it could not be resumed due to the hard thrombus.
Discussion
In this case, it is difficult to exclude a causal relationship between the COVID-19 mRNA vaccine and ischemic stroke. This association needs to be carefully monitored.
Key Words: COVID-19, mRNA vaccine, ischemic stroke, recurrent stroke
Background
Vaccination against COVID-19, which is causing a pandemic, is spreading rapidly around the world. COVID-19 has been reported to cause cerebrovascular diseases,1, 2, 3 and the COVID-19 adenovirus vector vaccine may also cause vaccine-induced immune thrombocytopenia (VITT).4 However, there are no reports suggesting a relationship between the COVID-19 mRNA vaccine, which encodes the spike glycoprotein of SARS-CoV-2, and cerebrovascular disease. A case of repeated cardioembolic stroke after the BNT162b2 (Pfizer) COVID-19 mRNA vaccination is presented.
Case report
An 83-year-old Japanese woman developed right hemiplegia and motor aphasia three days after receiving her first dose of the BNT162b2 (Pfizer) COVID-19 mRNA vaccine. She had been taking rivaroxaban for persistent atrial fibrillation for 10 years, but had no symptomatic ischemic strokes. She lived in a nursing home due to osteoarthritis, but never forgot to take her medication. Blood tests showed elevated thrombin-antithrombin complex (TAT) of 12.7 ng/mL (normal range, <1.0 ng/mL), and D-dimer of 2.8 μg/mL (<1.0 μg/mL). Thrombocytopenia and hyperlipidaemia were not shown. PCR test for SARS-CoV-2 and antibodies for platelet factor 4 were not performed. Atrial fibrillation was detected on her ECG. Magnetic resonance imaging (MRI) showed that the proximal M1 segment of the left middle cerebral artery (MCA) was occluded (Fig. 1 D), but the ischemic area was localized to only a part of the left insular cortex and corona radiata (Fig. 1A,B). Intravenous recombinant tissue-plasminogen activator (rt-PA) therapy and mechanical thrombectomy were performed, and the patient was successfully recanalized about 3.5 hours after onset. With rehabilitation, she recovered almost fully and was discharged to the nursing home. Transthoracic echocardiography showed no thrombus in the left atrial appendage, but transoesophageal echocardiography was not performed. Rivaroxaban was replaced with edoxaban.
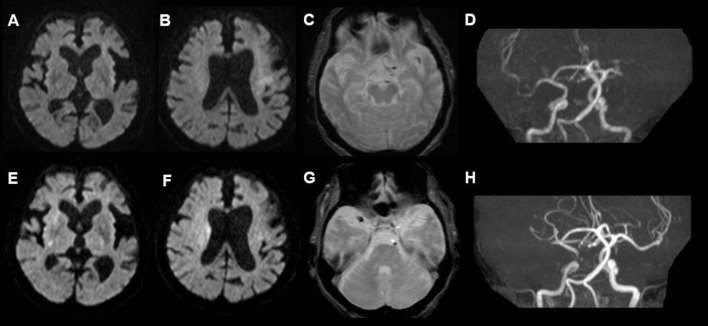
Fig. 1.
First admission: (A-D) diffusion-weighted images (DWI) show acute infarction in the left insular cortex and corona radiata (A, B). Susceptibility vessel signs are seen in the left middle cerebral artery (MCA) on the T2*-weighted image (C). On magnetic resonance angiography (MRA), the left MCA is occluded at the proximal M1 segment (D). 2nd admission: (E-H) DWI shows acute infarction in the right insular cortex, caudate, and corona radiata (E, F). This T2*-weighted image shows the susceptibility vessel sign in the right MCA (G), and MRA shows that the right MCA is occluded at the proximal M1 segment (H).
Three weeks after the first injection, she received her second dose of the vaccine. She did not forget to take edoxaban after discharge. However, three days after the second dose, she developed left hemiplegia and left hemispatial neglect. On the blood tests, her TAT was again high at 23.0 ng/dL, and D-dimer at 3.2 μg/mL. MRI showed occlusion of the right MCA proximal M1 segment (Fig. 1H), but the ischemic areas were found only in a part of the right insular cortex, caudate, and corona radiata (Fig. 1E,F). Since rt-PA was contraindicated, only mechanical thrombectomy was performed again, but it could not be resumed due to the hard thrombus. MRI re-examination showed that the ischemic area had spread to almost the entire right MCA area, and the symptoms did not recover. Additional examinations were performed, but antiphospholipid antibodies were negative, and the transoesophageal echocardiogram showed no thrombus in the left atrial appendage. Blood coagulation and fibrinolysis system markers were almost normalized two weeks after the onset of the second stroke.
Discussion
In this case, it is difficult to exclude a causal relationship between the COVID-19 mRNA vaccine and ischemic stroke, because the stroke occurred in a patient with atrial fibrillation who was on anticoagulant therapy for 10 years with no symptomatic ischemic stroke, and it recurred at the same time after the second vaccination. It is possible that the remaining left atrial thrombus caused the second embolism, but except for it, there was no other cause more suspicious than the vaccine. At the time of writing, the number of COVID-19 mRNA vaccines administered is lower in Asia than in other regions. Since the incidence of strokes in COVID-19 has been reported to be higher in Asian than in European and North American populations,2 the spread of the vaccine to Asia may result in more such cases. Although we cannot infer a causal relationship between the vaccine and ischemic stroke based on this case alone, this association needs to be carefully monitored and caution may be needed in patients who have a stroke soon after the first dose.
Conclusion
The relationship between the COVID-19 mRNA vaccine and ischemic stroke needs to be carefully monitored.
References
- 1.Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nannoni S, Groot R, Bell S, et al. Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke. 2021;16:137–149. doi: 10.1177/1747493020972922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan YK, Goh C, Leow AST, Tambyah PA, et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis. 2020;50:587–595. doi: 10.1007/s11239-020-02228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scully M, Singh D, Lown R, et al. N Eng J Med. 2021;384:2202–2211. doi: 10.1056/NEJMoa2105385. [DOI] [PMC free article] [PubMed] [Google Scholar]