Abstract
Background
There is a paucity of evidence regarding the association between family physicians’ panel size and health outcomes of patients with hypertension in China.
Objective
To examine the association between family physicians’ panel size and health outcomes of patients with hypertension in urban China.
Design
This retrospective cohort study during 1 contract year from July 1, 2018, to June 31, 2019, was set in four community health centers (CHCs) in Xiamen City, China.
Participants
A total of 18,119 adult patients (18+) diagnosed with hypertension and their 61 family physicians were included.
Main Measures
Family physicians’ panel size was measured by the number of registered patients in the preceding 6 months. The outcome measures included blood pressure (BP) control rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) measured at each follow-up visit.
Key Results
Every additional 100 patients to the panel size were associated with an average of 17% increase in BP control rate (95% confidence interval [CI] = 1.15 to 1.19), and decrease in SBP (− 0.3 mmHg, 95% CI: − 0.38 to − 0.30), DBP (− 0.4 mmHg, 95% CI: − 0.39 to − 0.34), and MAP (− 0.4 mmHg, 95% CI: − 0.38 to − 0.33). After entering the quadratic term of panel size in the model, the panel size was negatively associated with BP control rate and positively associated with SBP, DBP, and MAP, while for the quadratic term, the odds ratio for BP control rate was positive and the coefficients for SBP, DBP, and MAP were negative. A U-shape association was found between panel size and health outcomes of patients with hypertension, and the turning point was about 600 patients.
Conclusions
The panel size of family physicians was curvilinearly associated with health outcomes of patients with hypertension in urban China.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06681-0.
KEY WORDS: family physicians, panel size, hypertension, health outcomes, China
INTRODUCTION
Primary care is the most frequently used point of contact for patients seeking health services. As a key component of primary health care, each family physician is responsible to provide care for a certain number of patients, which was defined as a panel size.1 Previous studies had explored the association between family physicians’ panel size and the timeliness of care including access and continuity.2–7 In addition, panel size was also associated with patients’ experience and satisfaction,2, 3, 8, 9 as well as family physicians’ burnout.10, 11 Examining an appropriate panel size is a salient topic not only to insure continuity of care and accessibility but also to improve satisfaction of both patients and primary care providers.
Several studies have examined the association between panel size and clinical health outcomes of patients with hypertension. Despite wide variations in panel size (ranging from 52 to 36,130 patients), there was little variation in the health outcomes of patients with hypertension, while larger panels were associated with better performance of some other indicators for initial diagnosis and management.12 Another study from the United States Department of Veterans Affairs (VA) assessed the association between panel size and clinical quality of patients in one fiscal year, and found that increasing panel size (from 1206 to 1566 patients) was associated with lower possibilities of pneumococcal vaccination uptake and alcohol misuse screening, but was not significantly related to health outcomes, such as blood pressure (≤ 140/90) for patients with hypertension.2 For other conditions, a study from the Mayo Clinic showed that increasing the panel size from 1876 to 4828 patients was negatively associated with diabetes care,3 while other studies found no significant association between panel size and health outcomes of patients with diabetes and ischemic heart disease, respectively.4, 13 These previous studies showed inconsistent results concerning the association between panel size and health outcomes, especially for hypertension, and they were conducted in Western countries with a well-developed family physician care system.
As part of China’s health care reform, primary health care has received considerable public attention.14 The government has introduced family physician contract service policy since 2016 by which each patient would register with a family physician team.15 This policy is still in its early stage with its potential has yet to be realized.16 Furthermore, there were no strict restrictions on family physicians’ panel size. Additionally, only a small proportion (from 4% in 2011 to 13% in 2018) of physicians in China became qualified family physicians.16 Thus, there is a lack of family physicians for patients with multiple chronic conditions, especially hypertension and diabetes.16, 17 Findings from this study can shed some light on this important health care topic in China. Hypertension is a major preventable risk factor for cardiovascular diseases and all-cause deaths globally.18–20 Compared with the USA, the UK, and Japan, China has lower blood pressure (BP) control rate.21, 22 Improving the BP control rate is a central issue with clinical and public health implications.
To examine the potential association between family physicians’ panel size and chronic disease control in China, it is helpful to assess it in regions with well-implemented family physician contract service policy. In this study, we examined the association between family physicians’ panel size and hypertension-related health outcomes measured by BP control rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) in urban China.
METHODS
Setting and Design
We conducted a population-based cohort study. Data was collected retrospectively (from July 1, 2018, to June 30, 2019) from regional electronic health record database in Xiamen City, Fujian Province, China. Xiamen City’s family physician contract service system, also called “the Joint Management by Three Professionals (JMTP),” was implemented with the goal of providing equitable and accessible treatment system for chronic conditions, especially for diabetes and hypertension, by strengthening diagnostic and treatment capacities at a primary health care level. Typically, a family physician contract service team includes three professionals: a family physician, a health manager, and a specialist.23 The JMTP system was also one of the models recommended by the Chinese government.
This study randomly selected four community health centers (CHCs) in Xiamen City according to geographic location and administrative divisions. The information of patients with hypertension in the four CHCs was obtained from regional electronic health record database, which consisted of public health information system, primary health care service cloud platform, and family physician contract system. Patients were linked across different datasets via unique encoded identifiers, and their basic characteristics (including age, sex, and health insurance status), health outcomes, and visited family physicians’ panel size in each follow-up visit were retrieved. Furthermore, in July 2019, we conducted an on-spot survey in all four CHC locations in Xiamen City, Fujian Province, China, to collect the characteristics of all family physicians, including age, sex, marital status, monthly income, education, professional title (a sign reflecting the technical level and working ability of family physicians), number of daily visits, average consultation time per patient, and working hours per day.
Study Population and Measures
A total of 22,983 patients with hypertension were identified from the database in the four CHCs. The inclusion criteria for patients were as follows: aged 18 years or older; had at least one diagnosis code related to hypertension according to the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10); and had at least two recorded visits. The inclusion criteria of family physicians were as follows: had the general practice qualified certification; participated in the contract service program in CHCs; had a panel size of more than 100 patients. We dropped 4839 patients with only one visit in CHCs during the contract year and 25 patients younger than 18 years old. Our final sample included a total of 18,119 patients with hypertension treated by 61 family physicians (see Fig. 1). The baseline covered the first community visit for each patient with hypertension. Patients had numerous follow-up visits in 1 contract year. On average, patients with and without own family physicians had 8 and 6 follow-up visits in CHCs , respectively (see Supplementary Table 1).
Fig. 1.
Flow chart of study population selection.
This study measured panel size using number of patients registered for each family physician in the preceding 6 months. In addition, patients with hypertension may be panel members of the visited family physician in a follow-up visit, or perhaps they were not in the panel because they chose other family physicians instead of their own family physicians. According to health policies in Xiamen City, the maximum panel size is 1500 patients for each family physician.
Hypertension is a major preventable risk factor for cardiovascular diseases and all-cause deaths globally.18, 24 Therefore, the reduction in mortality and incidence of cardiovascular diseases caused by hypertension are important indicators of patients’ health outcomes. In the present study, it was difficult to measure these indicators, so four indicators were regarded as health outcomes of hypertension: (1) whether BP at each follow-up visit was controlled over 1 contract year (1 = controlled, 0 = uncontrolled). Adequate BP control among patients with hypertension was defined as an average SBP less than 140 mmHg and an average DBP of less than 90 mmHg over two readings;22, 25 (2) SBP value at each visit; (3) DBP value at each visit; and (4) MAP value calculated as 1/3 (SBP) + 2/3 (DBP) at each visit.
Statistical Analyses
We produced summary statistics using frequencies and proportions for categorical variables, and means and standard deviations for continuous variables. We used the population averaged generalized estimating equations (GEE) model to estimate the longitudinal association between penal size and health outcomes of patients with hypertension. GEE model is specifically used to deal with repeated measurement data including unbalanced longitudinal data.26 After controlling for the aforementioned confounders, the population averaged GEE model was used to examine the longitudinal association between the panel size of visited family physicians and health outcomes of patients with hypertension. To account for potential “U-shape” association between the panel size of family physicians and hypertension indicators, we further adjusted for the quadratic term of the panel size in the GEE model. Analyses were conducted using Stata 13 (Stata Corporation LLC).
RESULTS
Table 1 reports the descriptive statistics of 61 family physicians by different panel sizes. Among these physicians, 42.62% were male, 78.70% were married, and 32.80% had master’s degree and above. Among family physicians with smaller panel size of less than 600 patients, 70.59% had primary title and below, while none of them had a senior title. By contrast, nearly 80% of family physicians with larger panel size had medium title and above. The average age and working years for family physicians were 36.54 and 11.75 years, respectively. Family physicians with larger panel size were nearly 7 years older than those with smaller panels, and accordingly, their working experience was about 7 years longer than physicians with smaller panels. The average income per month was China Yuan (CNY) 10.21 thousand for family physicians. There was not much difference in working hours per day (7.71 h and 7.97 h, respectively) between family physicians with small and large panels.
Table 1.
Descriptive Statistics of Family Physicians by Different Panel Sizes
| Variable | Panel size | Total | |
|---|---|---|---|
| < 600 patients | 600–1500 patients | ||
| N | 17 | 44 | 61 |
| Male, % | 35.29 | 45.45 | 42.62 |
| Age, years, mean (SD) | 31.82(3.71) | 38.36(6.52) | 36.54(6.55) |
| Married, % | 52.94 | 88.64 | 78.7 |
| Average monthly income, thousand China Yuan, mean (SD) | 8.79(2.40) | 10.76(3.12) | 10.21(3.05) |
| Master degree and above, % | 47.06 | 27.27 | 32.8 |
| Professional title, % | |||
| Primary title | 70.59 | 20.45 | 34.44 |
| Medium title | 29.41 | 59.09 | 50.82 |
| Senior title | 0 | 20.45 | 14.75 |
| Number of daily visits, number, mean (SD) | 49.12(23.92) | 60.48(33.17) | 57.31(31.11) |
| Average consultation time per patient, min, mean (SD) | 6.85(4.34) | 6.98(4.04) | 6.94(4.09)) |
| Working hours per day, h, mean (SD) | 7.71(0.77) | 7.97(1.10) | 7.90(1.02) |
| Working years, years, mean (SD) | 6.41(4.71) | 13.86(7.64) | 11.75(7.69) |
SD standard deviation
Table 2 displays the results of the GEE model using longitudinal data in 1 contract year for patients with hypertension. We controlled for other cofounders, such as patients’ and visited family physicians’ characteristics. We found that every additional 100 contracted patients in panel size would increase BP control rate (OR = 1.17, 95% CI: 1.15 to 1.19) and decrease SBP (Coef = − 0.34 mmHg, 95% CI: − 0.38 to − 0.30), DBP (Coef = − 0.37 mmHg, 95% CI: − 0.39 to − 0.34), and MAP (Coef = − 0.35 mmHg, 95% CI: − 0.38 to − 0.33).
Table 2.
Longitudinal Association Between Health Outcomes of Patients with Hypertension and the Panel Size in 1 Contract Year
| BP control | SBP | DBP | Mean arterial pressure | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Panel size | 1.17 | (1.147, 1.185) | − 0.34 | (− 0.376, − 0.299) | − 0.37 | (− 0.393, − 0.338) | − 0.35 | (− 0.383, − 0.330) |
| Whether the patient was a panel member of the visited family physician | ||||||||
| Not in the panel | REF | REF | REF | REF | ||||
| In the panel | 1.05 | (0.960, 1.145) | 0.04 | (− 0.11, 0.18) | 0.11 | (− 0.010, 0.220) | 0.09 | (− 0.020, 0.190) |
| Patients | ||||||||
| Male | 0.80 | (0.736, 0.872) | 0.34 | (0.185, 0.485) | 0.53 | (0.411, 0.651) | 0.47 | (0.355, 0.577) |
| Age | 1.00 | (0.996, 1.004) | 0.02 | (0.015, 0.028) | − 0.05 | (− 0.056, − 0.045) | − 0.03 | (− 0.031, − 0.022) |
| Having health insurance | 1.48 | (1.289, 1.707) | 0.23 | (− 0.195, 0.663) | 0.49 | (0.187, 0.799) | 0.41 | (0.110, 0.704) |
| Visited family physicians | ||||||||
| Male | 0.91 | (0.823, 0.993) | 0.68 | (0.472, 0.885) | 0.80 | (0.648, 0.955) | 0.76 | (0.615, 0.906) |
| Age | 1.00 | (0.988, 1.011) | 0.07 | (0.049, 0.084) | 0.05 | (0.031, 0.059) | 0.05 | (0.039, 0.065) |
| Married | 1.19 | (1.039, 1.365) | − 0.72 | (− 1.058, − 0.386) | 0.85 | (0.607, 1.089) | 0.32 | (0.088, 0.561) |
| Income | 0.92 | (0.907, 0.937) | − 0.13 | (− 0.169, − 0.094) | − 0.16 | (− 0.186, − 0.134) | − 0.15 | (− 0.176, − 0.125) |
| Education | ||||||||
| Bachelor degree and below | REF | REF | REF | REF | ||||
| Master degree and above | 0.95 | (0.857, 1.043) | − 1.44 | (− 1.691, − 1.186) | − 0.23 | (− 0.419, − 0.042) | − 0.63 | (− 0.815, − 0.45) |
| Professional title | ||||||||
| Primary title | REF | REF | REF | REF | ||||
| Medium title | 1.21 | (1.068, 1.377) | 2.62 | (2.292, 2.944) | 1.30 | (1.072, 1.519) | 1.74 | (1.511, 1.961) |
| Senior title | 1.39 | (1.130, 1.710) | 3.35 | (2.925, 3.765) | 1.44 | (1.135, 1.737) | 2.07 | (1.781, 2.363) |
| Number of daily visits | 1.01 | (1.008, 1.011) | 0.03 | (0.025, 0.032) | 0.01 | (0.006, 0.011) | 0.02 | (0.013, 0.018) |
| Average consultation time per patient | 0.98 | (0.970, 0.996) | 0.13 | (0.089, 0.167) | 0.02 | (− 0.010, 0.046) | 0.06 | (0.027, 0.082) |
| Working hours per day | 0.81 | (0.742, 0.876) | − 1.08 | (− 1.334, − 0.834) | 0.02 | (− 0.173, 0.213) | − 0.35 | (− 0.526, − 0.171) |
BP control blood pressure control, SBP systolic blood pressure, DBP diastolic blood pressure, MAP mean arterial pressure
We added the quadratic term of the panel size in the GEE model and found that the panel size was negatively associated with BP control (OR = 0.79, 95% CI: 0.73 to 0.86), and positively associated with SBP, DBP, and MAP (SBP, Coef = 0.24, 95% CI: 0.03 to 0.45; DBP, Coef = 0.46, 95% CI: 0.31 to 0.60; MAP, Coef = 0.38, 95% CI: 0.24 to 0.53). In contrast, the odds ratio of the quadratic term for BP control was 1.02, and the coefficients of the quadratic term of the panel size for SBP, DBP, and MAP were negative. The results indicated a U-shape association between panel size and hypertension indicators. We further found out that the turning points of panel size were 580, 430, 569, and 533 patients for BP control, SBP, DBP, and MAP, respectively (see Table 3).
Table 3.
Longitudinal Association Between Health Outcomes of Patients with Hypertension (Next Visit) and the Quadratic Term of the Panel Size in 1 Contract Year
| BP control | SBP | DBP | Mean arterial pressure | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Panel size | 0.79 | (0.731, 0.860) | 0.24 | (0.028, 0.448) | 0.46 | (0.311, 0.603) | 0.38 | (0.240, 0.528) |
| Panel size^2 | 1.02 | (1.016, 1.024) | − 0.03 | (− 0.038, − 0.018) | − 0.04 | (− 0.047, − 0.033) | − 0.04 | (− 0.043, − 0.029) |
| Whether the patient was a panel member of the visited family physician | ||||||||
| Not in the panel | REF | REF | REF | REF | ||||
| In the panel | 1.05 | (0.970, 1.150) | 0.04 | (− 0.110, 0.180) | 0.11 | (− 0.010, 0.220) | 0.08 | (− 0.020, 0.190) |
| Patients | ||||||||
| Male | 0.80 | (0.735, 0.871) | 0.34 | (0.187, 0.488) | 0.54 | (0.415, 0.654) | 0.47 | (0.358, 0.580) |
| Age | 1.00 | (0.996, 1.003) | 0.02 | (0.016, 0.028) | − 0.05 | (− 0.055, − 0.045) | − 0.03 | (− 0.031, − 0.021) |
| Having health insurance | 1.48 | (1.284, 1.702) | 0.22 | (− 0.213, 0.645) | 0.47 | (0.163, 0.771) | 0.38 | (0.087, 0.679) |
| Visited family physicians | ||||||||
| Male | 0.90 | (0.824, 0.992) | 0.64 | (0.432, 0.849) | 0.75 | (0.595, 0.899) | 0.71 | (0.566, 0.856) |
| Age | 0.99 | (0.981, 1.005) | 0.06 | (0.046, 0.082) | 0.04 | (0.027, 0.055) | 0.05 | (0.035, 0.062) |
| Married | 1.22 | (1.066, 1.389) | − 0.65 | (− 0.98, − 0.309) | 0.96 | (0.718, 1.200) | 0.42 | (0.189, 0.660) |
| Income | 0.95 | (0.932, 0.965) | − 0.17 | (− 0.209, − 0.129) | − 0.21 | (− 0.241, − 0.187) | − 0.20 | (− 0.226, − 0.172) |
| Education | ||||||||
| Bachelor degree and below | REF | REF | REF | REF | ||||
| Master degree and above | 0.96 | (0.867, 1.054) | − 1.43 | (− 1.68, − 1.176) | − 0.22 | (− 0.404, − 0.028) | − 0.62 | (− 0.802, − 0.438) |
| Professional title | ||||||||
| Primary title | REF | REF | REF | REF | ||||
| Medium title | 1.23 | (1.079, 1.394) | 2.59 | (2.271, 2.913) | 1.26 | (1.038, 1.478) | 1.70 | (1.482, 1.923) |
| Senior title | 1.43 | (1.154, 1.77) | 3.39 | (2.967, 3.806) | 1.50 | (1.199, 1.79) | 2.13 | (1.839, 2.411) |
| Number of daily visits | 1.01 | (1.004, 1.008) | 0.03 | (0.028, 0.035) | 0.01 | (0.011, 0.016) | 0.02 | (0.017, 0.022) |
| Average consultation time per patient | 0.99 | (0.979, 1.007) | 0.11 | (0.071, 0.151) | − 0.01 | (− 0.035, 0.022) | 0.03 | (0.005, 0.060) |
| Working hours per day | 0.87 | (0.801, 0.945) | − 1.18 | (− 1.425, − 0.926) | − 0.11 | (− 0.304, 0.083) | − 0.47 | (− 0.643, − 0.288) |
| Turn point of panel size | 580 | 430 | 569 | 533 | ||||
BP control blood pressure control, SBP systolic blood pressure, DBP diastolic blood pressure, MAP mean arterial pressure
Figure 2 illustrates the average marginal effect of the panel size, from which we found that, before the turning point, the average marginal effect of panel size on BP control rate was negative, but getting closer to 0; meanwhile, the average marginal effect of panel size on SBP, DBP, and MAP value was positive, and getting smaller. From the turning point to the maximum panel size (1500), the BP control rate was increasing, and the highest change rate was achieved when the panel size reached between 1100 and 1200; at the same time, SBP, DBP, and MAP values were declining.
Fig. 2.
The average marginal effect on health outcomes of the panel size with 95% CI.
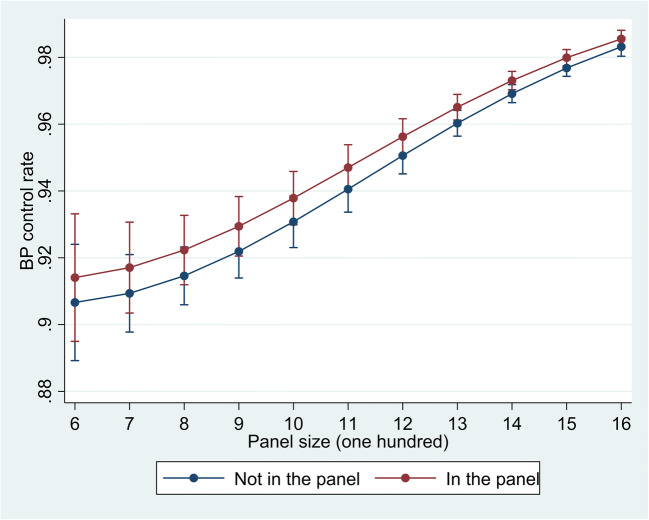
We found that the 17 family physicians with panel size fewer than 600 patients only took charge of 7% of the follow-up visits. We further dropped these follow-up visits completed by family physicians with small (< 600) panel size, and explored the association between patients’ BP control and whether the patients were panel members, and the results are shown in Figure 3. As the panel size (more than 600 patients) of visited family physicians increased, the BP control rate of patients who were in the panel would be higher compared with that of patients who were not the panel members of visited family physicians.
Fig. 3.
Predictive margins of the panel size (more than 600 patients) with 95% CI.
DISCUSSION
To the best of our knowledge, the present study is the first to explore the association between family physicians’ panel size and clinical health outcomes in China. Our results indicated that there was a curvilinear association between panel size and health outcomes of patients with hypertension. Health outcomes in smaller panels (< 600) were not better than in those in larger panels, perhaps due to physicians’ lack of work experience and capability. When the panel size was between 600 and 1500, increasing panel size was positively associated with better performance of hypertension indicators. The family physician contract service policy in China is still in its early stage,16 where it is suggested that the maximum panel size for each family physician should not exceed 2000 patients.27 However, no empirical evidence has yet identified the appropriate panel size.
Similar studies have been conducted in developed countries to explore the association between panel size and clinical health outcomes. Both patients and family physicians were more satisfied with smaller panel sizes, because smaller panel size could make it easier to get early or advance appointments, and was conducive to offering coherent and personal services.9, 28 Nevertheless, increasing panel size from 100 to 600 patients was negatively associated with health outcomes of patients with hypertension in this study. Our findings are supported by a prior study reporting that family physicians with small panel size may have inadequate capability and experience.29 Besides, family physicians with small panel size were usually isolated and poorly trained and offered narrower range of services, which may worsen patients’ health outcomes.30 Therefore, for family physicians with smaller panels, the recommended panel size should be kept smaller to leave more time for training and improving professional skills.
Increasing panel size from 600 to 1500 patients was positively associated with health outcomes of patients with hypertension. Two hypotheses have been used to explain the size-outcomes relationships. First, family physicians may develop more effective skills if they treat more patients.12 Researchers have found that panel size larger than the current mean (2959 patients) in the Mayo Clinic was associated with poorer health outcomes in terms of BP control for diabetic patients.3 In the USA, it was calculated that family physicians would take 10.6 h per day to deliver only guideline-recommended chronic disease treatments in a panel of 2500 patients.31 By comparison, the actual average working hours per day for family physicians in Xiamen City was less than 8 h under a panel size of no more than 1500 patients, so physicians were not “overextended or overworked.”32 In this sense, family physicians with larger panel size in Xiamen City had more work experience and limited work pressure, thus resulted in better health outcomes among patients.30 Second, management and delivery of care among members of the primary care team were more efficient among family physicians with larger panel size.12, 33 Chronic disease management can be complex and requires various types of services from the primary care team. Many management and treatment processes for patients with hypertension were performed by nurses or specialists in the JMTP system in Xiamen City.34 Perhaps such resource sharing might be more achievable for family physician teams of larger panel size, which generally need a wider range of staff.12 This study filled the gap in the literature related to the association between panel size and health outcomes of patients in China and countries with less-developed primary care systems.
How to estimate the appropriate panel size in primary health care is a complex issue.1, 35 This study aimed to estimate the appropriate panel size for achieving better health outcomes of patients with hypertension, but we still cannot conclude whether similar size-outcomes relationships would occur in the management of other diseases in primary care. A study estimated the panel size of a primary care physician by assuming different task delegations within the primary care team, and found that a primary care team could reasonably care for a panel of 1947, 1523, or 1387 patients under different assumptions.32 Other studies even suggested that a panel size of 10,000 to 15,000 patients may be optimal for the family physician workload.36 Therefore, the appropriate panel size is dependent on the aims, functions, and tasks of organization, and there may not be one panel size that suits all.37 In the future, more studies should be conducted among different populations using different indicators.
Limitations
This study had several limitations. Firstly, the maximum panel size of family physician in Xiamen City was 1500, and we were not able to analyze the association between hypertension indicators and panel size larger than 1500 patients. Secondly, the database used in this study only covered four CHCs in Xiamen City, so the information was probably missed if some of the patients with hypertension went to other primary care facilities during the contract year. Thirdly, our study population of patients with hypertension was retrieved from regional electronic health record database, and we did not have access to more covariates at patient level. Hence, it may be inappropriate to make national judgments about care in general practice from these data.
CONCLUSION
In conclusion, this study offered a beginning to deeper studies of the relationship between family physicians’ panel size and health outcomes of patients. The panel size of family physicians had a curvilinear association with health outcomes of patients with hypertension. For family physicians with smaller panel size (100–600 patients), they need to enhance their ability and enrich their training to improve patients’ health outcomes, and smaller panel size is more suitable for them at this stage. For family physicians with larger panel size (600–1500 patients) and sufficient competence, there was a positive association between panel size and health outcomes, indicating the potential to adequately enlarge the panel size of family physicians in China.
Supplementary Information
(DOCX 31 kb)
Acknowledgements
The survey was conducted by the Peking University Group. The authors thank the Xiamen Municipal Health Commission, China, for their willingness to provide the data of patients with hypertension. We would also like to thank anonymous reviewers whose comments have helped substantially to improve the document.
Author Contribution
RZJ and HF were responsible for the original research concept and study design. Specific study hypotheses and statistical analyses were completed by RZJ, EM, XZL, and HJZ. HF and EM were responsible for the critical revision of the article for important intellectual content. RZJ wrote the first draft of the manuscript. All authors gave final approval of the version to be published.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (grant number 71774006).
Declarations
Ethics Approval
This study was approved by the Peking University Institutional Review Board (IRB00001052-19072).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rize Jing, Email: rzjing2015@hsc.pku.edu.cn.
Elham Mahmoudi, Email: mahmoudi@med.umich.edu.
Xiaozhen Lai, Email: laixiaozhen@pku.edu.cn.
Haijun Zhang, Email: zhanghj966@bjmu.edu.cn.
Hai Fang, Email: hfang@hsc.pku.edu.cn.
References
- 1.Paige NM, Apaydin EA, Goldhaber-Fiebert JD, et al. What is the optimal primary care panel size?: a systematic review. Ann Intern Med. 2020;172(3):195–201. doi: 10.7326/M19-2491. [DOI] [PubMed] [Google Scholar]
- 2.Stefos T, Burgess JF, Jr, Mayo-Smith MF, et al. The effect of physician panel size on health care outcomes. Health Serv Manage Res. 2011;24(2):96–105. doi: 10.1258/hsmr.2011.011001. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Q, Zhao Y, Li J, Shi H (2020c) Microplastics in food: health risks. pp 343-356 Family medicine panel size with care teams: impact on quality. J Am Board Fam Med. 2016;29(4):444-51. [DOI] [PubMed]
- 4.Dahrouge S, Hogg W, Younger J, Muggah E, Russell G, Glazier RH. Primary care physician panel size and quality of care: a population-based study in Ontario. Canada. Ann Fam Med. 2016;14(1):26–33. doi: 10.1370/afm.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Francis MD, Zahnd WE, Varney A, Scaife SL, Francis ML. Effect of number of clinics and panel size on patient continuity for medical residents. J Grad Med Educ. 2009;1(2):310–5. doi: 10.4300/JGME-D-09-00017.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mittelstaedt TS, Mori M, Lambert WE, Saultz JW. Provider practice characteristics that promote interpersonal continuity. J Am Board Fam Med. 2013;26(4):356–65. doi: 10.3122/jabfm.2013.04.120306. [DOI] [PubMed] [Google Scholar]
- 7.Margolius D, Gunzler D, Hopkins M, Teng K. Panel Size, Clinician time in clinic, and access to appointments. Ann Fam Med. 2018;16(6):546–8. doi: 10.1370/afm.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta R, Bodenheimer T. How primary care practices can improve continuity of care. JAMA Intern Med. 2013;173(20):1885–6. doi: 10.1001/jamainternmed.2013.7341. [DOI] [PubMed] [Google Scholar]
- 9.Baker R. Characteristics of practices, general practitioners and patients related to levels of patients’ satisfaction with consultations. Br J Gen Pract. 1996;46(411):601–5. [PMC free article] [PubMed] [Google Scholar]
- 10.Helfrich CD, Simonetti JA, Clinton WL, et al. The association of team-specific workload and staffing with odds of burnout among VA primary care team members. J Gen Intern Med. 2017;32(7):760–6. doi: 10.1007/s11606-017-4011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582–7. doi: 10.1007/s11606-014-3112-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saxena S, Car J, Eldred D, Soljak M, Majeed A. Practice size, caseload, deprivation and quality of care of patients with coronary heart disease, hypertension and stroke in primary care: national cross-sectional study. BMC Health Serv Res. 2007;7:96. doi: 10.1186/1472-6963-7-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azeem Majeed JG. Gareth Ambler, Kevin Carroll, Andrew B Bindman. Association between practice size and quality of care of patients with ischaemic heart disease: cross sectional study. BMJ. 2003;326(7835):371–2. doi: 10.1136/bmj.326.7385.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lien K, Grattan BA, Reynard AL, Peters J, Parr JL. Factors associated with family physician follow-up 30 days post-discharge from a local Canadian community emergency department. Cureus. 2020;12(2):e7008. doi: 10.7759/cureus.7008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Medical Reform Office . Notice on Promoting Guidance for Family physicians Contract Services. 2016. [Google Scholar]
- 16.Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–12. doi: 10.1016/S0140-6736(20)30122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet. 2017;390(10112):2584–94. doi: 10.1016/S0140-6736(17)33109-4. [DOI] [PubMed] [Google Scholar]
- 18.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383(9932):1899–911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banegas JR, Lopez-Garcia E, Dallongeville J, et al. Achievement of treatment goals for primary prevention of cardiovascular disease in clinical practice across Europe: the EURIKA study. Eur Heart J. 2011;32(17):2143–52. doi: 10.1093/eurheartj/ehr080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 21.Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China. Circulation. 2018;137(22):2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 22.Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017;390(10112):2549–58. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. China multidisciplinary teams and integrated service delivery across levels of care. 2018.
- 24.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):95767. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 25.Writing Group 2018. 2018 Chinese guidelines for the management of hypertension. Chin J Cardi Med. 2019;24(1):1-44.
- 26.Liang KL, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- 27.National Health Commission of the People’s Republic of China. Guiding Opinions on Regulating the Management of Family Physician Contract Services. 2018. Available at: http://www.nhc.gov.cn/jws/s7874/201810/be6826d8d9d14e849e37bd1b57dd4915.shtml
- 28.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract. 2010;11:61. doi: 10.1186/1471-2296-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ashworth M, Schofield P, Seed P, Durbaba S, Kordowicz M, Jones R. Identifying poorly performing general practices in England: a longitudinal study using data from the quality and outcomes framework. J Health Serv Res Policy. 2011;16(1):21–7. doi: 10.1258/jhsrp.2010.010006. [DOI] [PubMed] [Google Scholar]
- 30.van den Hombergh P, Schalk-Soekar S, Kramer A, Bottema B, Campbell S, Braspenning J. Are family practice trainers and their host practices any better? Comparing practice trainers and non-trainers and their practices. BMC Fam Pract. 2013;14:23. doi: 10.1186/1471-2296-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Østbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209–14. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med. 2012;10(5):396–400. doi: 10.1370/afm.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y, O’Donnell C, Mackay D, Watt G. Practice size and quality attainment under the new GMS contract: a cross-sectional analysis. Br J Gen Pract. 2006;56(532):830–5. [PMC free article] [PubMed] [Google Scholar]
- 34.Li X, Li Z, Liu C, et al. Evaluation of the three-in-one team-based care model on hierarchical diagnosis and treatment patterns among patients with diabetes: a retrospective cohort study using Xiamen’s regional electronic health records. BMC Health Serv Res. 2017;17(1):779. doi: 10.1186/s12913-017-2705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ng CW, Ng KP. Does practice size matter? Review of effects on quality of care in primary care. Br J Gen Pract. 2013;63(614):e604–e610. doi: 10.3399/bjgp13X671588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wensing M, van den Hombergh P, Akkermans R, van Doremalen J, Grol R. Physician workload in primary care: what is the optimal size of practices? A cross-sectional study. Health Policy. 2006;77(3):260–7. doi: 10.1016/j.healthpol.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 37.Bojke C, Gravalle H, Wilkin D. Is bigger better for primary care groups and trusts? BMJ. 2001;322(7286):599–602. doi: 10.1136/bmj.322.7286.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 31 kb)