Abstract
Background
Achieving the best possible reperfusion is a key determinant of clinical outcome after mechanical thrombectomy (MT). However, data on the safety and efficacy of intra-arterial (IA) fibrinolytics as an adjunct to MT with the intention to improve reperfusion are sparse.
Methods
We performed a PROSPERO-registered (CRD42020149124) systematic review and meta-analysis accessing MEDLINE, PubMed, and Embase from January 1, 2000 to January 1, 2020. A random-effect estimate (Mantel-Haenszel) was computed and summary OR with 95% CI were used as a measure of added IA fibrinolytics versus control on the risk of symptomatic intracranial hemorrhage (sICH) and secondary endpoints (modified Rankin Scale ≤2, mortality at 90 days).
Results
The search identified six observational cohort studies and three observational datasets of MT randomized-controlled trial data reporting on IA fibrinolytics with MT as compared with MT alone, including 2797 patients (405 with additional IA fibrinolytics (100 urokinase (uPA), 305 tissue plasminogen activator (tPA)) and 2392 patients without IA fibrinolytics). Of 405 MT patients treated with additional IA fibrinolytics, 209 (51.6%) received prior intravenous tPA. We did not observe an increased risk of sICH after administration of IA fibrinolytics as adjunct to MT (OR 1.06, 95% CI 0.64 to 1.76), nor excess mortality (0.81, 95% CI 0.60 to 1.08). Although the mode of reporting was heterogeneous, some studies observed improved reperfusion after IA fibrinolytics.
Conclusion
The quality of evidence regarding peri-interventional administration of IA fibrinolytics in MT is low and limited to observational data. In highly selected patients, no increase in sICH was observed, but there is large uncertainty.
Keywords: thrombectomy, thrombolysis, stroke
Introduction
Achieving complete reperfusion is the most important modifiable predictor for maximizing the treatment effect of mechanical thrombectomy (MT).1–3 Although the chances for a clinical benefit are optimal if complete reperfusion is attained after the first pass,4 5 there is a growing body of evidence suggesting that an effect of improved reperfusion is still tangible after multiple attempts and prolonged procedure time.6–8 Despite recent technical advances, failed reperfusion (Thrombolysis in Cerebral Infarction (TICI) 0/1) is the final result of MT in every 10th patient,9–11 and most patients treated successfully do not reach complete reperfusion (TICI 3).12 13 Treatment options in these scenarios are distal MT of thrombus fragments,7 14 bailout stenting15 or administration of intra-arterial (IA) fibrinolytics.16 17
According to a survey by investigators of the German Stroke Registry, up to 40% of interventionalists administer IA fibrinolytics during or after MT on a case-by-case basis,18 and a recent US survey described the use of IA thrombolysis in 61% of the survey’s responders.19 The recently published updated American Stroke Association/American Heart Association guidelines state that IA fibrinolysis constitutes a reasonable supplement to achieve TICI grade 2b/3 results20; however, data on the safety and efficacy of IA fibrinolytics as adjunct to MT are still scarce.16 17 21 22
In view of clinical equipoise, and with the intention to inform the planning of potential randomized controlled trials, we conducted a systematic review and meta-analysis to report on observational data comparing safety and efficacy outcomes in patients with MT, either additionally treated with IA fibrinolytics or best medical management.
Methods
This study is reported according to the recommendations of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) reporting guideline.23
Protocol and registration
The protocol for this study was published before performing the analysis (PROSPERO: CRD42020149124).
Study eligibility criteria
Eligible studies included all age groups and all ethnic groups reporting on adults (older than 18 years) with an acute ischemic stroke and IA fibrinolytic therapy as adjunct to MT treatment of a target large-vessel occlusion. Acute ischemic stroke had to be diagnosed by qualified personnel (in an emergency department, stroke center, department of neurology, or similar unit) and large-vessel occlusion had to be confirmed by pre-interventional imaging (MR angiography/CT angiography or first diagnostic digital subtraction angiography runs). Studies had to report symptomatic intracranial hemorrhage (sICH) or adequate surrogates (eg, parenchymal hematoma type II according to the European Cooperative Acute Stroke Study (ECASS) criteria) in patients treated with second-generation MT (aspiration technique or stent-retriever devices) with strata of administration of IA fibrinolytics during MT (with or without additional IA fibrinolytics, respectively). Fibrinolytics considered were (pro)urokinase, alteplase, reteplase and tenecteplase. In this manuscript, tPA (tissue plasminogen activator) and uPA exclusively refer to alteplase and urokinase, respectively. We excluded studies reporting on historical mechanical treatments such as balloon angioplasty, guidewire clot disruption or first-generation devices, and we did not consider bailout stenting for this analysis. Abstracts were included if the authors were able to provide the required data for this meta-analysis. Otherwise, we included peer-reviewed, original studies only. Since state-of-the-art endovascular therapy was used in the last two decades, we only considered publications beyond January 1, 2000 for analysis. Additionally, we contacted the Principal Investigators of randomized-controlled trials included in the HERMES collaboration,24 if the trial protocol allowed administration of IA fibrinolytics in the mechanical thrombectomy arm (ESCAPE (Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times),25 MR CLEAN (Multicenter Randomized CLinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands),26 THRACE (Trial and Cost Effectiveness Evaluation of Intra-arterial Thrombectomy in Acute Ischemic Stroke)27). Corresponding authors of the included observational studies were contacted to provide the median dose of fibrinoloytics and rates of sICH with strata of intravenous thrombolysis (IVT)+MT+IA versus IVT+MT and direct MT+IA versus direct MT only. We excluded studies with duplicate data, or no specific strata of patients receiving adjunct fibrinolytic therapy. When sICH was the primary outcome of a study, but the authors did not report numbers for patients receiving additional fibrinolytic therapy, authors were contacted to report events of sICH and mortality in patients receiving additional fibrinolytic therapy during or after aspiration or mechanical thrombectomy. We excluded studies with <10 patients undergoing endovascular treatment.
Data sources and searches
Data for this review were identified via a search on MEDLINE, PubMed and Embase, as well as references from relevant articles using a predefined search strategy formulated according to the Population, Intervention, Comparison and Outcome (PICO) format search strategy (online supplemental information 1). Only articles published in English, French, Spanish and German between January 1, 2000 and January 1, 2020 were included.
neurintsurg-2020-016680supp001.pdf (973.7KB, pdf)
Study selection
Publications were uploaded into the Covidence online review tool. Their relevance was assessed against the predetermined inclusion and exclusion criteria by two independent researchers (JK and TRM), who screened all titles and abstracts. Forward and backward reference searching complemented the database searches. Full-text manuscripts were obtained for all studies entering full-text review. Any uncertainties about including a specific manuscript in the review were resolved by consensus.
Data collection process and data items
Data were extracted into the Review Manager Program (RevMan, Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) by TRM and reviewed by JK. Data items included type of study, unadjusted and adjusted odds for the primary and secondary outcomes with a description of parameters adjusted for, type of sICH scale applied, and presence of differences in baseline characteristics between patients with and without additional IA fibrinolytics within a study. All extracted raw frequency counts can be found in the forest plots.
Risk of bias in individual and across studies
We compared data items, outcomes, design strengths and weaknesses across the studies. For each study, the risk of bias was assessed at the study level using the Cochrane ROBINS-I bias assessment tool with study-specific items, and this information was incorporated when interpretation of data was given in the synthesis.
Outcomes
The main outcome was the occurrence of sICH according to the study-specific definition in the acute phase of stroke care (usually within 24 hours, see online supplemental table 1 for definition of sICH). If not available, other surrogates (eg, parenchymal hematoma type II according to ECASS) were considered, because it is associated with a high likelihood of neurological deterioration.28 Secondary outcomes included all-cause mortality at 90 days, good functional outcome at 90 days (modified Rankin Scale (mRS) 0–2), and angiographic effect regarding the additional administration of IA fibrinolytics. This could be reported as frequencies of final TICI score with strata of MT patients with and without IA fibrinolytics or dedicated improvement of reperfusion analyses after administration of IA fibrinolytics. Successful reperfusion was defined as TICI 2b/3. For the summary estimate regarding successful reperfusion, we divided the studies into those reporting on patients with the primary intention to improve unsuccessful or incomplete reperfusion (high risk of reperfusion bias towards poor TICI grades in the IA groups), and studies where IA fibrinolytics were mainly applied during or before initial stent-retriever deployment or studies in which the control group of patients without IA fibrinolytics also consisted of patients with unsuccessful or incomplete MT patients (low risk of reperfusion bias towards poor TICI grades in the IA group). Studies without documented reason for administering IA fibrinolytics were rated as unknown risk of reperfusion bias.
Synthesis of results and summary measures
If available and consistent throughout the studies, the summary estimates of effect sizes (summarized ORs, and adjusted summarized ORs (aOR)) for sICH in MT patients with additional IA fibrinolytics as compared with MT patients without additional IA fibrinolytics (control patients) were calculated using a random-effects model (Mantel-Haenszel method). Adjusted ORs were summarized separately, if available. Heterogeneity was assessed by p value of χ2 statistics and I 2 which describes the percentage of variability in the estimates that cannot be explained by chance.29 We considered study-level estimates to be heterogeneous if the I 2 statistic was >50%. All p values were calculated by two-sided tests and a significance level of 0.05 was used. Visual inspection of the funnel plot was used for the evaluation of publication bias. Data analysis was performed using R30 with the R package ‘meta’ 4.9–7.31 If available, calculations were made for secondary outcomes using the same analysis tools.
Results
The database searches and citation tracking yielded 711 hits, of which 447 records were screened as potentially relevant after removing duplicates (see online supplemental figure 1 for PRISMA flow-chart). Reasons for excluding relevant publications after full-text review are also shown in online supplemental figure 1). In total, five publications met the inclusion criteria of reporting the risk of sICH after failed or incomplete large vessel occlusion MT in patients receiving fibrinolytics and inclusion of a control group receiving no fibrinolytics (all non-randomized observational studies). We also contacted the main author of a published abstract to provide the study data with strata of MT+IA versus MT alone.32 In addition, three of the principal investigators of recent MT trials allowing for the use of IA fibrinolytics provided unadjusted estimates regarding the frequency of sICH, as well as mRS 0–2 and mortality at 90 days with strata of additional administration of IA fibrinolytics.25–27 One principal investigator of recent MT trials allowing for the use of IA fibrinolytics also provided adjusted estimates correcting for age, sex and baseline National Institutes of Health Stroke Scale (NIHSS). In summary, nine studies reporting on 2797 patients were included.
The characteristics of these six observational cohort studies and observational data derived from the three included MT trials are shown in table 1. Eight studies compared IA tPA with control,16 17 21 22 25–27 32 and one study compared IA urokinase with control.33 Rates of sICH were available in eight of nine studies, with one study reporting rates of parenchymal hematoma type 2 (PH2) only.17 The definitions of sICH and comparator groups across studies were somewhat heterogeneous, but most studies used a compound definition of radiological verification of intracranial hemorrhage together with a neurological deterioration of ≥4 points on the NIHSS (see online supplemental table 1). Nearly all studies were confined to patients with small or medium size core infarct volumes and some studies reported significant baseline differences between the groups, most commonly favoring the group who additionally received IA fibrinolytics (ie, younger age, or earlier presentation, see online supplemental table 1).
Table 1.
Summary of included studies
| Study | Study type | N | Type of fibrinolytic | Median dose (IQR) | Median dose in patients after IV tPA | Timing | IA fibrinolytics administered after IV tPA | Main indication | MT Technique | sICH definition available | ||
| IA | Non-IA | Rescue after failed or incomplete MT | Primary as conjunction with MT | |||||||||
| Anadani et al 17 | RO of prospective database | 67 | 419 | tPA | 5 mg (2–6 mg) | 5 mg | N/A | Yes (13/67, 19.4%) | Yes | No | ADAPT | No (PH2 used) |
| Heiferman et al 21 | RO | 28 | 12 | tPA | 13.25 mg (8–15.25 mg) | 10 mg | N/A | Yes (15/28) | No | Yes | Stent-retriever thrombectomy | Yes |
| Yi et al 22 | RO | 37 | 56 | tPA | NA, reported as <5 mg | N/A | Not reported | Yes (17/37, 45.9%) | No | Yes | Stent-retriever thrombectomy | Yes |
| Zaidi et al 16 | RO | 37 | 44 | tPA | NA | NA | Not reported | Yes (17/37, 46%) | Yes | No | Stent-retriever thrombectomy | Yes |
| Kaesmacher et al 33 | RO of prospective database | 100 | 893 | uPA | 300000 IU (250000–500000 IU) | 250000 (250000–500000) | Median time to uPA (275 min, IQR 229–313) | Yes (43/100, 43%) | Yes (75%) | Yes (25%) | >90% stent-retriever thrombectomy | Yes |
| Bracard et al 27 | RO of RCT data (THRACE) | 15 | 124 | tPA | 7 mg (3–10 mg) | 7 mg | N/A | Yes (15/15, 100%) | Yes | No | 77.1% stent-retriever thrombectomy 9.3% aspiration 13.6% multiple systems |
Yes |
| Berkhemer et al 26 | RO of RCTA data (MR CLEAN) | 22 | 169 | tPA | NA, reported as 5 mg single dose, up to 30 mg | N/A | N/A | Yes (18/21, 86%, 1 unknown) | Yes | No | Stent-retriever thrombectomy | Yes |
| Goyal et al 25 | RO of RCT data (ESCAPE) | 7 | 158 | tPA | Median dose 5 mg (range 1–7 mg) | N/A | N/A | Yes (5/7, 71.4%) | N/A | N/A | Stent-retriever thrombectomy | Yes |
| Castonguay et al 32 | RO of a prospective database (STRATIS, MCA occlusions only) | 92* | 518* | tPA | Median dose 4 mg (IQR 2–10 mg) | 4 mg | N/A | Yes (66/92, 65.6%) | Yes (20%) | Yes (75%) | Stent-retriever thrombectomy | Yes |
| Total | 9 RO | 405 | 2392 | 8 x tPA, 1 x uPA | Median range tPA 4–13.25 mg | 51.6% (209/405) | >80% stent-retriever | 8/9 Yes | ||||
* numbers slightly differ in comparison to the abstract version, because in this meta-analysis, only patient with available data on sICH are included.
ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times; IA, intra-arterial; IV, intravenous; MCA, middle cerebral artery; MRCLEAN, Multicenter Randomized CLinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands; MT, mechanical thrombectomy; N/A, not available; PH2, parenchymal hematoma type 2; RCT, randomized controlled trial; RO, retrospective observational; sICH, symptomatic intracranial hemorrhage; STRATIS, Systematic Evaluation of Patients Treated With Stroke Devices for Acute Ischemic Stroke; THRACE, Trial and Cost Effectiveness Evaluation of Intra-arterial Thrombectomy in Acute Ischemic Stroke; tPA, tissue plasminogen activator, alteplase; uPA, urokinase.
In total, we included 405 cases with additional administration of IA fibrinolytics (100 urokinase, 305 tPA), and 2392 controls in the meta-analysis. Of 405 patients receiving IA fibrinolytics, 209 were pretreated with intravenous tPA (51.6%). Applied median dose of IA fibrinolytics ranged from 4–13.25 mg for tPA and was 300 000 U for IA urokinase. In eight studies with available information, reasons for administration of IA fibrinolytics consisted of rescue after failed MT (TICI0/1, 4/8 studies), incomplete reperfusion (TICI2a/b, 5/8 studies), administration during stent-retriever deployment at the discretion of the operator (4/8 studies), and treatment of emboli to new territories (1/8 studies).
Except for one study,21 follow-up duration was 3 months in all studies. The Cochrane ROBINS-I risk of bias assessment for the included studies with adoption of items for observational data are summarized in online supplemental figure 2. All trials had performance bias due to non-blinding of intervention and three trials had attrition bias due to incomplete outcome data.
Symptomatic intracranial hemorrhage and mortality
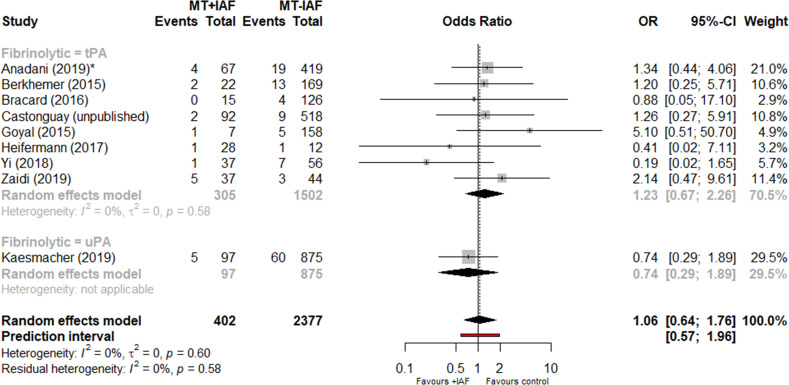
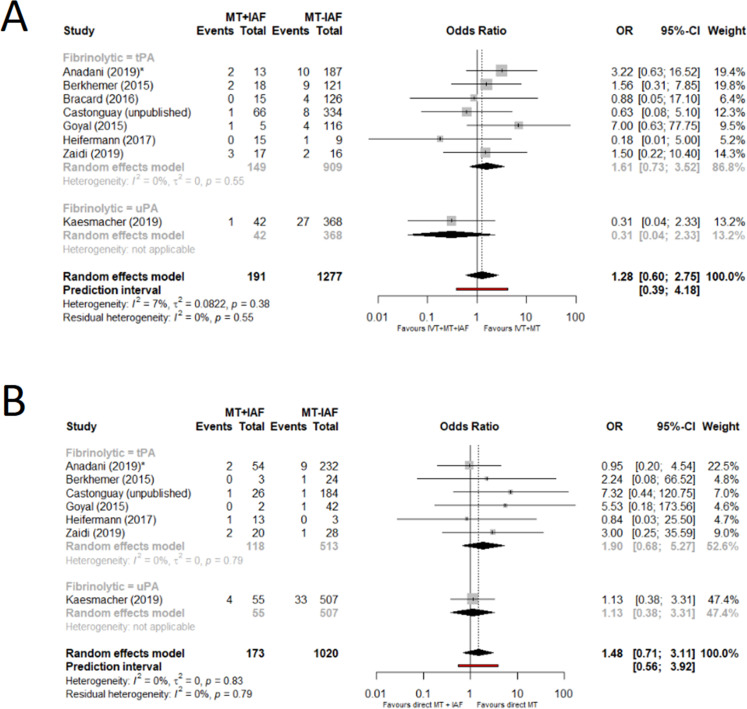
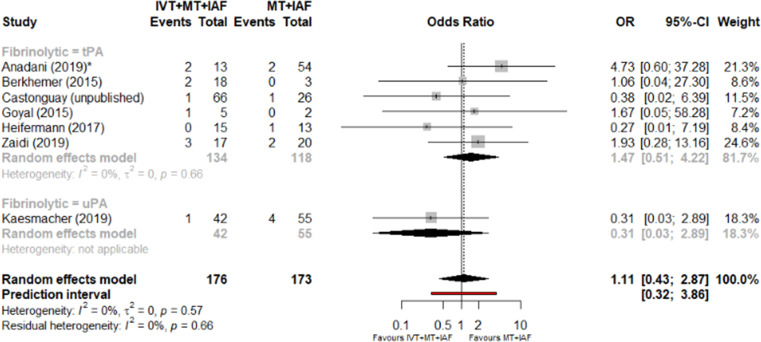
Pooling the results from all studies using the random-effects model showed that added IA fibrinolytics compared with control were not associated with an increased risk of sICH (OR 1.06, 95% CI 0.64 to 1.76; I 2=0%) (figure 1). Limiting observations to IA tPA only yielded a point estimate of OR 1.23 (95% CI 0.67 to 2.26). There was no evidence of publication bias on funnel plot analysis (online supplemental figure 3). There was no significant heterogeneity of the effect of added IA fibrinolytics with strata of IVT pretreatment status (IVT+MT+IA vs IVT+MT, OR 1.28, 95% CI 0.60 to 2.75; and direct MT+IA vs direct MT only, OR 1.48, 95% CI 0.71 to 3.11) (figure 2). Additionally, a direct comparison of patients treated with IVT+MT+IA fibrinolytics versus MT+IA fibrinolytics yielded no evidence of a significant difference (OR 1.11, 95% CI 0.43 to 2.87) (figure 3).
Figure 1.
Forest plot of summary odds ratios for sICH in patients with and without adjunctive administration of IAF during MT. *For Anadani et al we used PH2 as sICH surrogate. IAF, intra-arterial fibrinolytics; MT, mechanical thrombectomy; PH2, parenchymal hematoma type 2; sICH, symptomatic intracranial hemorrhage; tPA, tissue plasminogen activator; uPA, urokinase.
Figure 2.
Forest plot of summary odds ratios for sICH in patients with and without adjunctive administration of IAF during MT with strata of IVT before MT. (A) With intravenous tPA (IVT) before MT. (B) Without IVT MT. *For Anadani et al we used PH2 as sICH surrogate. IAF, intra-arterial fibrinolytics; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; PH2, parenchymal hematoma type 2; sICH, symptomatic intracranial hemorrhage; tPA, tissue plasminogen activator; uPA, urokinase.
Figure 3.
Forest plot of summary odds ratios for sICH comparing patients with bridging therapy, MT and added IAF to patients with direct MT and added IAF. *For Anadani et al we used PH2 as sICH surrogate. IAF, intra-arterial fibrinolytics; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; PH2, parenchymal hematoma type 2; sICH, symptomatic intracranial hemorrhage; tPA, tissue plasminogen activator; uPA, urokinase.
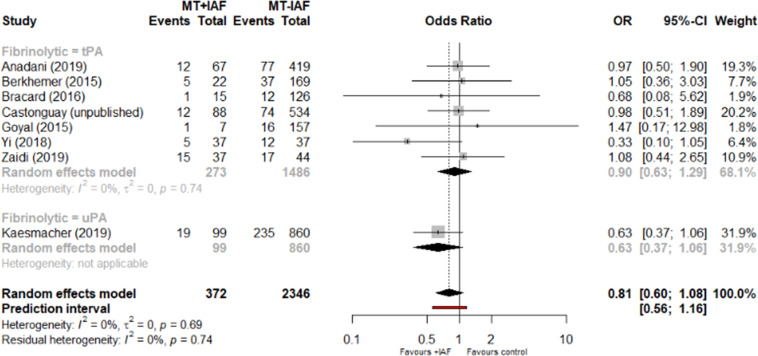
Meta regression, limited to five studies reporting on median IA tPA dose applied (median dose range 4–10 mg), did not provide evidence for heterogeneity or dose-dependency regarding the association of MT+IA fibrinolytics versus MT and sICH with strata of different dose regimens applied (mixed effect model, estimate −0.15, 95% CI −0.48 to 0.19 per mg, see online supplemental figure 4) for bubble plot). No excess mortality after additional treatment with IA fibrinolytics was found (OR 0.81, 95% CI 0.60 to 1.08, I 2 =0%; OR 0.90, 95% CI 0.63 to 1.29 for tPA only, figure 4). Further subgroup analyses and restriction to adjusted estimates for safety endpoints can be found in online supplemental information 2.
Figure 4.
Forest plot of unadjusted odds ratios for mortality at 3 months in patients with and without adjunctive administration of IAF during MT. *For Anadani et al we used PH2 as sICH surrogate. IAF, intra-arterial fibrinolytics; MT, mechanical thrombectomy; PH2, parenchymal hematoma type 2; sICH, symptomatic intracranial hemorrhage; tPA, tissue plasminogen activator; uPA, urokinase.
Functional outcome and angiographic efficacy
There was no difference in functional outcome (OR 1.08, 95% CI 0.78 to 1.49, I 2=35%) (online supplemental figure 5 and 6) or successful reperfusion (OR 0.85, 95% CI 0.66 to 1.29) (online supplemental figure 7) between patients treated with additional IA fibrinolytics and those without. The point estimate of reperfusion differed based on the degree of reperfusion bias (online supplemental figure 7) and on qualitative study-level analyses. The reporting of angiographic reperfusion improvement after added IA fibrinolytics was heterogeneous across the included studies, with some studies reporting improved angiographic perfusion (online supplemental table 2).
Discussion
We found the following: (1) The quality of evidence regarding the relative benefits of additive IA fibrinolytics versus standard of care during contemporary MT is low and limited to observational data. (2) IA fibrinolytics are often not administered according to a standardized protocol, but with the following indications—after failed or incomplete MT, during MT at the discretion of the operator, and for treatment of emboli in new territories during MT. (3) In a highly selected subgroup, additional administration of IA fibrinolytics was not associated with a clear excess risk of sICH or 90 day mortality, but there is large uncertainty. (4) Considering adjusted estimates and qualitative angiographic efficacy analyses reported by some studies, IA fibrinolytics may improve reperfusion after failed or incomplete MT.
Frequency of IA fibrinolytics in contemporary MT
Currently it is unknown whether administration of IA fibrinolytics is safe when applied as additive to MT. In the MRCLEAN26 and ESCAPE25 trials, additional use of IA thrombolysis was reported, although no subgroup analyses were available. Also in the THRACE trial, IA tPA was used to a maximum dose of 0.3 mg/kg. Here, IA tPA was administered in 15/141 patients (10.6%) with a mean dose of 8.8 mg after full dose IV tPA, without significant difference regarding functional outcome between patients treated with or without additional tPA (7/15 (46.7%) vs 64/126 (50.8%), p=0.76).27 Corroborating these findings, administration of IA fibrinolytics during or after MT also seems relatively common in clinical real-life practice outside randomized controlled trials according to recent survey data.18 19 In the TREVO registry, IA tPA was administered in 28 of 65 cases as a rescue therapy (43%)13 and IA tPA was used in 14% of patients harboring a middle cerebral artery occlusion treated with MT in in the STRATIS registry.12 Although not representative, the relative frequency of administering IA fibrinolytics was 14.8% in patients treated with MT in our meta-analysis. Interestingly, IA fibrinolytics were also administered after preceding treatment with intravenous thrombolysis, which was the case in 51.6% of patients in this meta-analysis. In addition, the current review also shed light on indications for IA fibrinolytics, ranging from incomplete or failed MT to administration before or during stent-retriever deployment or as a treatment option for emboli to new territory.
Risk of sICH
We did not find a significant association between sICH and administration of IA fibrinolytics and there was no significant heterogeneity as to intravenous tPA pretreatment status or dose regimens applied (median range 4–13.25 mg). However, point estimates favored MT without IA and 95% confidence and prediction intervals were large and patients were highly selected (mostly small core patients included). Beside favorable patient selection, an overall lack of a clear association between the administration of IA fibrinolytics and increased risk of sICH may have several other reasons. First, improved reperfusion is generally associated with reduced rates of hemorrhagic transformations and sICH.6 34 35 Hence, improved reperfusion after IA fibrinolytics could counterbalance the potential increase of sICH after administration of IA fibrinolytics. Second, IA fibrinolytics were not administered in a randomized manner, and the comparison of baseline characteristics revealed significant differences, some of which have been associated with an a priori lower risk of sICH in the IA fibrinolytics group, potentially leading to selection bias (eg, earlier presentation or younger age). Third, associations may be weak when applied as low-dose adjunct to MT and larger sample sizes would be needed to detect a significant association. Lastly, we pooled different types of fibrinolytics and risk of sICH might differ, although previous studies suggested a comparable risk profile when administered intra-arterially.36
Some evidence on the safety of IA fibrinolytics as adjunct to MT is derived from the transition phase between first- and second-generation devices, and here results were contradictory and may thus not be easily transferable to current practice. In the SWIFT (Solitaire With the Intention For Thrombectomy) trial, rescue with IA thrombolysis was associated with an increased risk of bleeding (OR 12.1, 95% CI 1.082 to 134.5), although most bleedings occurred in the MERCI group and no analysis of sICH stratified for the use of additive IA fibrinolytics is available.37 In contrast, administration of IA tPA was associated with lower chances of PH (aOR 0.57, 95% CI 0.35 to 0.90) in a large heterogeneous cohort of patients treated with first- and second-generation devices in the USA.38
Angiographic efficacy
If IA fibrinolytics were administered in order to improve unsuccessful or incomplete reperfusion, rates of successful reperfusion tended to be lower than in the control group for obvious selection reasons. There was, however, no significant difference between the groups if low reperfusion bias studies were considered. Given that the reperfusion result is inherently associated with the indication to administer IA fibrinolytics, we think that a mere pooling of the rates of successful reperfusion across the groups is not advisable, which is why we added a qualitative analysis regarding reperfusion efficacy. Despite homogenous indications and ways of reporting, hints towards an improved angiographic reperfusion after the additive use of IA fibrinolytics were observed on an individual study level.
Outlook and future direction
Currently, we are aware of two trials evaluating IA fibrinolytics as adjunct to MT. In one small single-arm pilot trial from China (NCT04202458) patients will receive IA administration of 4 mg tenecteplase (TNK), which is continuously given after the first attempt of thrombectomy device pass for 30 min. The BRETIS-TNK (Boosting REcanalization of Thrombectomy for Ischemic Stroke by Intra-arterial TNK) trial will include 30 patients. Currently the data on the safety and efficacy of IA TNK are sparse and limited to small observational studies39 or case reports40 and no data of IA TNK as adjunct to MT are available. The European randomized controlled trial CHOICE (CHemical OptImization of Cerebral Embolectomy in patients with acute stroke treated with mechanical thrombectomy) will evaluate the administration of IA fibrinolytics after incomplete (TICI2b) reperfusion with MT.41 In this trial, patients will be randomized to receive either a 30 min IA infusion with weight-adapted tPA or IA placebo. The study will enroll 200 patients, with an expected increase from TICI2b to TICI2c/3 of 60% in the experimental arm and 5% in the placebo arm. Given reports synthesized here, 60% improvement in the experimental arm seems high considering that one study reported 50% overall reperfusion improvement, with only around 30% being TICI grade relevant.33 However, the presented data provide some reasurrance that administration of IA fibrinolytics does not markly increase the risk of sICH in highly selected patients and when low dose regimens are applied.
Lastly, the data presented stress the need for a future standardized reporting pattern when describing patients treated with IA fibrinolytics as adjunct to MT. This includes a precise description of indication, time-point of administration, dosage, and evaluation of angiographic or follow-up perfusion efficacy. Further prospective, multicenter studies are urgently needed to elaborate the role of IA fibrinolytics in contemporary stroke MT.
Limitations
This study has several limitations, some related to potential sources of bias inherent to the included observational studies. In all included studies, indications for and administration of IA fibrinolytics was neither randomized nor standardized, thus prompting selection bias. Some studies provided adjusted analyses (matching or logistic regression), which may have mitigated, but presumably could not entirely account for selection bias effects. Moreover, we pooled data on the occurrence of sICH, despite heterogeneous definitions. Angiographic efficacy analysis was limited to qualitative analysis, because heterogeneous indications and discrepant ways of reporting limited the usefulness of summary estimates. Lastly, new devices and different modes and combination of flow-arrest during MT have entered the market and clinical routine in recent years, thus potentially changing the need for and respective value of additional administration of IA fibrinolytics.
Conclusion
The quality of evidence regarding the relative benefits of additional IA fibrinolytics versus standard of care during contemporary MT is low and limited to observational data. In highly selected patients treated with MT ± preceding intravenous thrombolysis, additional administration of IA fibrinolytics (uPA or tPA) does not seem to increase the risk of sICH. Further studies evaluating its potential to improve reperfusion after incomplete or failed MT are warranted.
Footnotes
Twitter: @mihill68
Contributors: All authors contributed to the presented work by substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work and drafting the work or revising it critically for important intellectual content and final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This work was supported by the Swiss Stroke Society, the Bangerter Foundation, and the Swiss Academy of Medical Sciences through the “Young Talents in Clinical Research” program.
Disclaimer: Neither of the funding agencies took part in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: Related: UF and JG are global PIs for the SWIFT DIRECT study (Solitaire With the Intention for Thrombectomy Plus Intravenous t-PA Versus DIRECT Solitaire Stent-Retriever Thrombectomy in Acute Anterior Circulation Stroke) supported by Medtronic. Unrelated: JG is a global PI of STAR (Solitaire FR Thrombectomy for Acute Revascularisation Observational study), Clinical Event Committee member of the PROMISE study (European Registry on the ACE Reperfusion Catheters and the Penumbra System in the Treatment of Acute Ischemic Stroke; Penumbra), Consultancy, and receives Swiss National Science Foundation (SNSF) grants for MRI in stroke. UF receives research grants from SNSF and serves as a consultant for Medtronic and Stryker. MA received speaker honoraria from Bayer, Boehringer Ingelheim, and Covidien; advisory board honoraria from Amgen Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Covidien, Daichy Sankyo and Nestlé Health Science; research grant provided by the Swiss Heart Foundation. JK reports grants from SAMW / Bangerter Foundation, the Swiss Stroke Society and non-financial support from Stryker and Pfizer outside the submitted work. DWJD reports funding from the Dutch Heart Foundation, Brain Foundation Netherlands, The Netherlands Organisation for Health Research and Development, Health Holland Top Sector Life Sciences & Health, and unrestricted grants from AngioCare BV, Covidien/EV3®, MEDAC Gmbh/LAMEPRO, Penumbra Inc., Top Medical/Concentric, Stryker, Stryker European Operations BV, Medtronic, Thrombolytic Science, LLC and Cerenovus for research, all paid to institution. MG reports licensing agreement for systems of acute stroke diagnosis for GE Healthcare and Consultancy for Medtronic, Stryker, MicroVention and Mentice as well as unrestricted research grant by Stryker for the UNMASK-EVT study. MDH has a patent Systems and Methods for Assisting in Decision-Making and Triaging for Acute Stroke Patients pending to US patent office number 62/086077 and owns stock in Calgary Scientific, Inc—a company that focuses on medical imaging software.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data included in the manuscript is visible in forest plot or has already been published in the referenced articles.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethics approval was obtained by each contributing site (see methods section of respective manuscripts included).
References
- 1. Liebeskind DS, Bracard S, Guillemin F, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg 2019;11:433–8. 10.1136/neurintsurg-2018-014127 [DOI] [PubMed] [Google Scholar]
- 2. Rizvi A, Seyedsaadat SM, Murad MH, et al. Redefining 'success': a systematic review and meta-analysis comparing outcomes between incomplete and complete revascularization. J Neurointerv Surg 2019;11:9–13. 10.1136/neurintsurg-2018-013950 [DOI] [PubMed] [Google Scholar]
- 3. Kaesmacher J, Dobrocky T, Heldner MR, et al. Systematic review and meta-analysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: success revisited. J Neurol Neurosurg Psychiatry 2018;89:910–7. 10.1136/jnnp-2017-317602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke 2018;49:660–6. 10.1161/STROKEAHA.117.020315 [DOI] [PubMed] [Google Scholar]
- 5. Nikoubashman O, Dekeyzer S, Riabikin A, et al. True first-pass effect. Stroke 2019;50:2140–6. 10.1161/STROKEAHA.119.025148 [DOI] [PubMed] [Google Scholar]
- 6. Tonetti DA, Desai SM, Casillo S, et al. Successful reperfusion, rather than number of passes, predicts clinical outcome after mechanical thrombectomy. J Neurointerv Surg 2020;12:548–51. 10.1136/neurintsurg-2019-015330 [DOI] [PubMed] [Google Scholar]
- 7. Kaesmacher J, Maegerlein C, Zibold F, et al. Improving mTICI2b reperfusion to mTICI2c/3 reperfusions: a retrospective observational study assessing technical feasibility, safety and clinical efficacy. Eur Radiol 2018;28:274–82. 10.1007/s00330-017-4928-3 [DOI] [PubMed] [Google Scholar]
- 8. Behme D, Gera RG, Tsogkas I, et al. Impact of time on thrombolysis in cerebral infarction score results. Clin Neuroradiol 2020;30:345–53. 10.1007/s00062-019-00786-0 [DOI] [PubMed] [Google Scholar]
- 9. Leischner H, Flottmann F, Hanning U, et al. Reasons for failed endovascular recanalization attempts in stroke patients. J Neurointerv Surg 2019;11:439–42. 10.1136/neurintsurg-2018-014060 [DOI] [PubMed] [Google Scholar]
- 10. Kaesmacher J, Gralla J, Mosimann PJ, et al. Reasons for reperfusion failures in stent-retriever-based thrombectomy: registry analysis and proposal of a classification system. AJNR Am J Neuroradiol 2018;39:1848–53. 10.3174/ajnr.A5759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim BM. Causes and solutions of endovascular treatment failure. J Stroke 2017;19:131–42. 10.5853/jos.2017.00283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mueller-Kronast NH, Zaidat OO, Froehler MT, et al. Systematic evaluation of patients treated with neurothrombectomy devices for acute ischemic stroke: primary results of the STRATIS registry. Stroke 2017;48:2760–8. 10.1161/STROKEAHA.117.016456 [DOI] [PubMed] [Google Scholar]
- 13. Zaidat OO, Castonguay AC, Nogueira RG, et al. TREVO stent-retriever mechanical thrombectomy for acute ischemic stroke secondary to large vessel occlusion registry. J Neurointerv Surg 2018;10:516-524. 10.1136/neurintsurg-2017-013328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grossberg JA, Rebello LC, Haussen DC, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke 2018;49:1662–8. 10.1161/STROKEAHA.118.020567 [DOI] [PubMed] [Google Scholar]
- 15. Wareham J, Flood R, Phan K, et al. A systematic review and meta-analysis of observational evidence for the use of bailout self-expandable stents following failed anterior circulation stroke thrombectomy. J Neurointerv Surg 2019;11:675–82. 10.1136/neurintsurg-2018-014459 [DOI] [PubMed] [Google Scholar]
- 16. Zaidi SF, Castonguay AC, Jumaa MA, et al. Intraarterial thrombolysis as rescue therapy for large vessel occlusions. Stroke 2019;50:1003–6. 10.1161/STROKEAHA.118.024442 [DOI] [PubMed] [Google Scholar]
- 17. Anadani M, Ajinkya S, Alawieh A, et al. Intra-arterial tissue plasminogen activator is a safe rescue therapy with mechanical thrombectomy. World Neurosurg 2019;123:e604–8. 10.1016/j.wneu.2018.11.232 [DOI] [PubMed] [Google Scholar]
- 18. Kellert L, Wollenweber FA, Thomalla G, et al. Thrombolysis management in thrombectomy patients: real-life data from German stroke centres. Eur Stroke J 2017;2:356–60. 10.1177/2396987317727229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Castonguay AC, Jumaa MA, Zaidat OO, et al. Insights into intra-arterial thrombolysis in the modern era of mechanical thrombectomy. Front Neurol 2019;10:1195. 10.3389/fneur.2019.01195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Warner JJ, Harrington RA, Sacco RL, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. Stroke 2019;50:3331–2. 10.1161/STROKEAHA.119.027708 [DOI] [PubMed] [Google Scholar]
- 21. Heiferman DM, Li DD, Pecoraro NC, et al. Intra-arterial alteplase thrombolysis during mechanical thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis 2017;26:3004–8. 10.1016/j.jstrokecerebrovasdis.2017.07.031 [DOI] [PubMed] [Google Scholar]
- 22. Yi T-Y, Chen W-H, Wu Y-M, et al. Adjuvant intra-arterial rt-PA injection at the initially deployed Solitaire stent enhances the efficacy of mechanical thrombectomy in acute ischemic stroke. J Neurol Sci 2018;386:69–73. 10.1016/j.jns.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 23. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 25. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 26. Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 27. Bracard S, Ducrocq X, Mas JL, Guillemin F, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 2016;15:104. 10.1016/S1474-4422(16)30177-6 [DOI] [PubMed] [Google Scholar]
- 28. Fiorelli M, Bastianello S, von Kummer Rüdiger, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct. Stroke 1999;30:2280–4. 10.1161/01.STR.30.11.2280 [DOI] [PubMed] [Google Scholar]
- 29. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 30. R Core Team . R: a language and environment for statistical computing [Internet], 2019. [Google Scholar]
- 31. Schwarzer G. meta: {A}n {R} package for meta-analysis. 7. R News, 2007: 40–5. [Google Scholar]
- 32. Castonguay A, Zaidi S, Jumaa M. Intra-arterial thrombolysis as rescue therapy in MCA occlusions: subanalysis from the STRATIS registry. J Neurointerv Surg 2019;11. 10.1136/neurintsurg-2019-SNIS.231 [DOI] [Google Scholar]
- 33. Kaesmacher J, Bellwald S, Dobrocky T, et al. Safety and efficacy of intra-arterial urokinase after failed, unsuccessful, or incomplete mechanical thrombectomy in anterior circulation large-vessel occlusion stroke. JAMA Neurol 2020;77:318–26. 10.1001/jamaneurol.2019.4192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kaesmacher J, Kaesmacher M, Maegerlein C, et al. Hemorrhagic transformations after thrombectomy: risk factors and clinical relevance. Cerebrovasc Dis 2017;43:294–304. 10.1159/000460265 [DOI] [PubMed] [Google Scholar]
- 35. Lee YB, Yoon W, Lee YY, et al. Predictors and impact of hemorrhagic transformations after endovascular thrombectomy in patients with acute large vessel occlusions. J Neurointerv Surg 2019;11:469–73. 10.1136/neurintsurg-2018-014080 [DOI] [PubMed] [Google Scholar]
- 36. Lee M, Hong K-S, Saver JL. Efficacy of intra-arterial fibrinolysis for acute ischemic stroke: meta-analysis of randomized controlled trials. Stroke 2010;41:932–7. 10.1161/STROKEAHA.109.574335 [DOI] [PubMed] [Google Scholar]
- 37. Raychev R, Jahan R, Liebeskind D, et al. Determinants of intracranial hemorrhage occurrence and outcome after neurothrombectomy therapy: insights from the Solitaire FR with intention for thrombectomy randomized trial. AJNR Am J Neuroradiol 2015;36:2303–7. 10.3174/ajnr.A4482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nogueira RG, Gupta R, Jovin TG, et al. Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg 2015;7:16–21. 10.1136/neurintsurg-2013-010743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Georgiadis AL, Memon MZ, Shah QA, et al. Intra‐arterial tenecteplase for treatment of acute ischemic stroke: feasibility and comparative outcomes. J Neuroimaging 2012;22:249–54. 10.1111/j.1552-6569.2011.00628.x [DOI] [PubMed] [Google Scholar]
- 40. Meenakshi-Sundaram S, Periakaruppan A, Karuppiah SNKP, et al. Complete recovery following intra-arterial tenecteplase administration in a woman with acute ischemic stroke. J Clin Neurosci 2013;20:1786–8. 10.1016/j.jocn.2012.12.027 [DOI] [PubMed] [Google Scholar]
- 41. Renú A, Blasco J, Millán M, et al. The chemical optimization of cerebral embolectomy trial: study protocol. Int J Stroke 2019;174749301989565:174749301989565. 10.1177/1747493019895656 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2020-016680supp001.pdf (973.7KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data included in the manuscript is visible in forest plot or has already been published in the referenced articles.