Abstract
Background
Studies on subsequent anterior cruciate ligament (ACL) ruptures and career length in male professional football players after ACL reconstruction (ACLR) are scarce.
Aim
To investigate the second ACL injury rate, potential predictors of second ACL injury and the career length after ACLR.
Study design
Prospective cohort study.
Setting
Men’s professional football.
Methods
118 players with index ACL injury were tracked longitudinally for subsequent ACL injury and career length over 16.9 years. Multivariable Cox regression analysis with HR was carried out to study potential predictors for subsequent ACL injury.
Results
Median follow-up was 4.3 (IQR 4.6) years after ACLR. The second ACL injury rate after return to training (RTT) was 17.8% (n=21), with 9.3% (n=11) to the ipsilateral and 8.5% (n=10) to the contralateral knee. Significant predictors for second ACL injury were a non-contact index ACL injury (HR 7.16, 95% CI 1.63 to 31.22) and an isolated index ACL injury (HR 2.73, 95% CI 1.06 to 7.07). In total, 11 of 26 players (42%) with a non-contact isolated index ACL injury suffered a second ACL injury. RTT time was not an independent predictor of second ACL injury, even though there was a tendency for a risk reduction with longer time to RTT. Median career length after ACLR was 4.1 (IQR 4.0) years and 60% of players were still playing at preinjury level 5 years after ACLR.
Conclusions
Almost one out of five top-level professional male football players sustained a second ACL injury following ACLR and return to football, with a considerably increased risk for players with a non-contact or isolated index injury.
Keywords: anterior cruciate ligament, ACL, football, rehabilitation
Introduction
Anterior cruciate ligament (ACL) injury is a serious and sometimes career-threatening injury for the male professional football player.1 Although non-surgical management could be an option in a professional player,2 early ACL reconstruction (ACLR) is considered the gold standard treatment.
Most professional players in Europe (93%–100%) are able to return to football after ACLR,1 3–6 but only 55%–65% of players still compete at the same preinjury level 3–4 years after injury.1 3 6 Moreover, even if players successfully return to play (RTP) after ACLR, performance may be negatively impacted by virtue of decreased number of matches, playing minutes and scored goals per season as compared with their preinjury statistics.4 5
Many players also sustain subsequent knee-related injuries including recurrences of ACL injury after return to training (RTT) or return to match (RTM) play.1 7 8 There is emerging evidence of a high risk of second ACL injuries in young athletes in general,9 and particularly in female football players.10–15 However, less data have been reported on professional footballers, with ipsilateral reinjury ranging from 5% to 10%1 16–18 and contralateral injuries ranging from 4% to 8%.4 19
Given the identified knowledge gap in the literature, the aim of this study on male professional footballers was to investigate (1) the rate of second ACL injuries, (2) potential factors associated with second ACL injuries and (3) the professional career length following ACLR.
Material and methods
This is a substudy of an injury surveillance study on European men’s professional football that started in 2001, the Elite Club Injury Study (ECIS), carried out in collaboration with the Union of European Football Associations (UEFA).20 In total, 68 clubs with 374 team seasons were followed prospectively over a variable number of seasons per team from January 2001 to May 2019. Detailed methodology on definitions and data collection procedures in the main study has been reported previously.21
In brief, all players with a first team contract were eligible for participation. Specifically, for this substudy, only players with a first-time complete ACL rupture, occurring either isolated or combined with a concomitant injury to the knee joint,1 and who underwent ACLR were included. Players who could not be tracked for at least 1 year after ACLR were excluded. The dominant leg was defined as the preferred kicking leg.
Data collection for primary ACL injuries
As part of the general ECIS methodology, a designated medical staff member from each club was responsible for sending injury report forms to the research centre monthly. For every ACL injury reported, an ACL injury-specific injury report form was instantly sent to club medical staff, requesting relevant information about previous knee injuries, injury mechanisms, diagnostic modalities used, associated injuries and treatment details. A non-contact ACL injury was defined as the absence of any physical contact with another player or object at the time of injury. An isolated ACL injury was defined as no other structural injuries to knee ligaments, joint cartilage or menisci. Bone marrow impaction lesions were not considered as separate structural injury. The RTT and RTM dates were identified on the exposure report form, or via the club medical staff member if the player was no longer in the squad of a team in the study (ie, team relegated from the highest league system, player being on loan or transferred to another club, etc). Time to RTT was defined as the number of days between ACLR and return to full unmodified team training, and time to RTM was defined as the number of days between ACLR and the first match at preinjury level with minutes on the pitch. First match play could be a friendly or competitive match with the first team of the club or the national team. Players were also closely monitored by the study guarantor during ACL injury rehabilitation in order to identify any knee-related problems requiring further knee surgery, including subsequent ACL injuries, before clearance to RTT.
Definition and tracking of second ACL injuries
The definition of second ACL injury in this study was a new ACL rupture (ipsilateral graft rupture or contralateral rupture of the native ACL) that occurred after the official RTT. A new ACL injury that occurred before the official RTT, that is, when the player was still completing rehabilitation, was defined as an exacerbation and was not included in the analyses of second ACL injury.
Tracking of second ACL injuries when the player was still playing in a team inside the ECIS study was completed prospectively in accordance with previously reported methodology.1 Due to the nature of the ECIS club and player inclusion criteria, a player may have left the ECIS before the final day of data collection of this substudy (31 May 2019). Routine tracking of second ACL injuries was therefore also retrospectively done by using information from public databases regardless if players were still in the ECIS study or not. The primary data source was via http://www.transfermarkt.co.uk, using a previously validated methodology,22 which has been used also recently in other football injury epidemiology studies.23–25 Secondary data sources included (1) official team web sites and (2) other national and international media. Second ACL injuries tracked outside the ECIS via the aforementioned sources were included only after the diagnosis had been confirmed from the player’s current team medical staff.
Career length after ACLR
To evaluate the influence of ACL injury and ACLR on the top-level football career length, the playing records were monitored via http://www.transfermarkt.co.uk for players leaving the ECIS before the final day of data collection of this substudy (31 May 2019). Top-level football was defined as playing in the highest league level in a country.
Patient and public involvement
No patient (player) or public involvement took place in the design or planning of the study. Club medical staff approved the specific ACL injury substudy prior to its initiation.
Equity, diversity and inclusion
This study was conducted on male professional football players only. It is likely that the subsequent ACL injury rate in women’s football is at least as high as in men’s football, and it is therefore important to carry out similar studies on women’s football. Recently, a women’s ECIS was launched in collaboration with the UEFA, and that study design also includes similar detailed data collection on ACL injuries.
Written informed consent was collected from all participating players.
Statistical analysis
The second ACL injury incidence was reported as the cumulative number of subsequent ACL injuries (ipsilateral graft ruptures and contralateral ACL ruptures) divided by the number of ACL-injured players at risk, that is, still playing top-level football (defined as the highest league play of a country). Cumulative total second ACL injury rates were calculated, as well as separate rates of ipsilateral graft ruptures and contralateral ACL ruptures. The number of second ACL injuries was used as the numerator and the number of ACL-injured players as the denominator for the three rates. The professional career length after ACL injury was reported as the number of players still playing at top-level divided by the number of players at risk at each annual follow-up up to 5 years after RTT. Mean (SD) was used for time to second ACL injury after ACLR and RTT, and median (IQR) was used for overall length of follow-up and the number of years in top-level football after RTT.
The independent t-test and the χ2 test were used to compare players who incurred a second ACL injury and those who did not for continuous and categorical variables, respectively. Normality and homogeneity of variance were assessed with the Kolmogorov-Smirnov test and with the Levene test, respectively. All expected cell counts for the χ2 test were greater than five. In the analysis of risk factors for second ACL injury, we used a Cox regression model, considering the second ACL injury as the dependent event, with the number of months at risk as the time variable, and all the candidate risk factors as independent variables. Various player (leg dominance, side of index ACL injury and playing position), surgery (graft type and associated injuries) and recovery (time to RTT) variables were considered as candidate risk factors. Only the candidate risk factors with a p<0.10 in the univariable analysis were inserted in the final multivariable regression model. Since younger age is a well known factor for subsequent ACL injury,9 age was always included in all multivariable analyses regardless of the p value in the univariable analyses. The log-rank test was used in the univariable analysis, and an enter selection method was applied for the multivariable analysis. The proportional hazard assumption underlying the Cox regression was assessed with the estat phtest (p=0.56). To verify the linear assumption of the Cox model, we plotted martingale residuals vs continuous covariates (age and RTT). Players who quit professional football or sustained a second ACL injury during the follow-up period were censored and the individual exposure up to this time point was included in the model. Independent t-test and the χ2 test were also used to compare players who presented significant independent risk factors for continuous and categorical variables, respectively. All analyses were carried out using Microsoft Excel 2010 (Microsoft, USA) and Stata V.12 (StataCorp). A statistical significance level of p<0.05 was adopted.
Results
In total, 120 players with first-time ACL injury and ACLR were identified. Two players suffered exacerbations in terms of ipsilateral graft ruptures during on-field rehabilitation before RTT and were excluded. Among the 118 included players, 20 suffered a total of 21 ACL injuries during the follow-up. One player sustained both an ipsilateral graft rupture and a contralateral native ACL rupture in two separate events; both injuries were included in the crude reinjury rate calculation, but only the first injury event was included in the Cox regression analysis. The mean age at index ACL injury was similar between players who sustained a second ACL injury and those who did not (24.9 (SD 4.2) vs 25.1 (SD 4.4) years, p=0.91).
A minimum follow-up of at least 1 year was possible for all players with a median follow-up time of 4.3 (IQR 4.6) years after ACLR. Thirty-six players were censored prior to the end of follow-up (29 quit football and 7 reduced playing level to non-elite football) after a median follow-up of 4.1 (IQR 2.6) months. For the index ACL injury, 45 players (38.1%) had sustained an isolated ACL injury, whereas 73 (61.9%) had at least one associated injury; 43 (36.4%) and 21 (17.8%) had a lateral and medial meniscus injury; 19 (16.1%) and 12 (10.2%) had a medial and lateral collateral ligament injury; and 8 (6.8%) had a cartilage injury. Non-contact ACL injury occurred more frequently in the right knee (table 1), and the mean time to both RTT and RTM was significantly shorter for isolated ACL injuries than for associated injuries (table 2). Grafts used for the index ACLRs were patellar tendon autograft in 72 (61.0%) of the cases, hamstring tendon autograft in 36 (30.5%), iliotibial tendon autograft in 5 (4.2%), quadriceps tendon autograft in 1 (0.8%) and different allografts in the remaining 4 (3.4%).
Table 1.
Player and injury characteristics stratified for mechanism of index ACL injury*
| All players (n=118) | Non-contact injury (n=67) | Contact injury (n=51) | P value | |
| Mean age, years (SD) | 25 (4.3) | 26 (4.4) | 24 (4.1) | 0.042 |
| Right-leg dominance, n (%) | 87 (73.3) | 53 (79.1) | 34 (66.7) | 0.118 |
| Right-sided ACL injury, n (%) | 81 (68.6) | 51 (76.1) | 30 (58.8) | 0.045 |
| Injury in dominant leg, n (%) | 76 (64.4) | 51 (76.1) | 25 (49.0) | 0.002 |
| Mean time to RTT, days (SD) | 192 (45) | 187 (42) | 198 (48) | 0.209 |
| Mean time to RTM, days (SD) | 239 (63) | 236 (64) | 242 (62) | 0.578 |
*Only the first subsequent injury included for the single player with bilateral subsequent injuries.
RTM, return to match; ACL, anterior cruciate ligament; RTT, return to training.
Table 2.
Player and injury characteristics stratified for pattern of index ACL injury*
| All players (n=118) | Isolated injury (n=45) | Associated injury (n=73) | P value | |
| Mean age, years (SD) | 25 (4.3) | 25 (4.2) | 25 (4.4) | 0.588 |
| Right-leg dominance, n (%) | 87 (73.3) | 31 (68.9) | 56 (76.7) | 0.330 |
| Right-sided ACL injury, n (%) | 81 (68.6) | 35 (77.8) | 46 (63.0) | 0.093 |
| Injury in dominant leg, n (%) | 76 (64.4) | 33 (73.3) | 43 (58.9) | 0.112 |
| Mean time to RTT, days (SD) | 192 (45) | 174 (35) | 202 (47) | <0.001 |
| Mean time to RTM, days (SD) | 239 (63) | 219 (55) | 250 (64) | 0.007 |
*Only the first subsequent injury included for the single player with bilateral subsequent injuries.
ACL, anterior cruciate ligament; RTM, return to match; RTT, return to training.
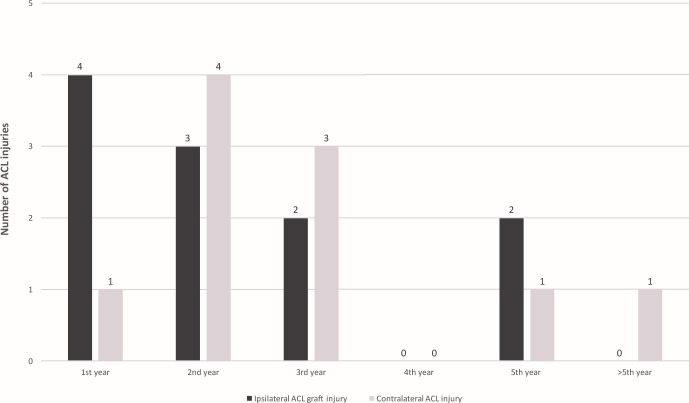
Second ACL injury incidence
The total cumulative second ACL injury incidence after RTT was 17.8% (21/118), with 9.3% (11/118) ipsilateral graft ruptures and 8.5% (10/118) contralateral ruptures. The mean time to second ACL injury was 26.5 (18.2) months (range 6.5–68.4) after ACLR and 21.5 (18.3) months (range 0.3–62.9) after RTT. Mean time to ipsilateral graft rupture was shorter than the time to contralateral ruptures, but this was not statistically significant, 23.5 (SD 18.5) vs 31.5 (SD 17.7) months postoperatively (p=0.30). More than half (57%) of the second ACL injuries occurred within 2 years following ACLR and RTT (figure 1).
Figure 1.
Annual number of second ACL injuries after ACL reconstruction and RTT stratified for injured knee. ACL, anterior cruciate ligament; RTT, return to training.
Risk factors for second ACL injury
Second ACL injuries were more common in players with non-contact and isolated index ACL injuries (table 3). Combined, 11 of the 26 players who sustained a non-contact isolated index ACL injury had a second ACL injury compared with 9 of the other 92 players (42.3% vs 9.8%, p<0.001). Out of the 92 remaining players, none of the 32 players who sustained an index ACL injury with associated injuries and due to contact (indirect or direct) suffered a second ACL injury (table 3).
Table 3.
Second ACL injury rate according to mechanism and pattern of the index ACL injury*
| Second ACL injury, n (%) | P value | |
| Injury mechanism | ||
| Non-contact injury (n=67) | 18 (26.9) | 0.001 |
| Indirect or direct contact (n=51) | 2 (3.9) | |
| Injury pattern | ||
| Isolated injury (n=45) | 13 (28.9) | 0.007 |
| Associated injury (n=73) | 7 (9.6) | |
| Combination of injury mechanism and injury pattern | ||
| Isolated non-contact injury (n=26) | 11 (42.3) | <0.001 |
| Associated non-contact injury (n=41) | 7 (17.1) | |
| Isolated indirect or direct contact injury (n=19) | 2 (10.5) | |
| Associated indirect or direct contact injury (n=32) | 0 (0) | |
*Only the first subsequent injury included for the single player with bilateral subsequent injuries.
ACL, anterior cruciate ligament.
Age and the three candidate risk factors with a p-value<0.10 from the univariable analysis (injury mechanism, injury pattern and time to RTT) were inserted into the final multivariable model. This showed that having sustained a non-contact index ACL injury increased the rate of a second ACL injury sevenfold, and having sustained an isolated index ACL injury increased the rate threefold (table 4).
Table 4.
Cox regression analysis for the rate of second ACL injury
| Univariable analysis | Multivariable analysis | |||
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Non-contact versus contact | 7.46 (1.73 to 32.20) | 0.007 | 7.16 (1.63 to 31.22) | 0.009 |
| Isolated versus associated | 3.24 (1.29 to 8.13) | 0.012 | 2.73 (1.06 to 7.07) | 0.037 |
| RTT (per month) | 0.72 (0.51 to 1.03) | 0.080 | 0.87 (0.60 to 1.25) | 0.466 |
| Age (per year) | 1.01 (0.90 to 1.12) | 0.817 | 0.96 (0.83 to 1.07) | 0.520 |
| Right-dominance vs left-dominance | 1.07 (0.38 to 2.95) | 0.893 | _ | |
| Dominant leg vs non-dominant leg | 2.28 (0.76 to 6.85) | 0.139 | _ | |
| PT autograft vs HT autograft | 1.36 (0.52 to 3.52) | 0.526 | _ | |
| PT autograft vs other grafts | 1.26 (0.28 to 5.68) | 0.765 | _ | |
ACL, anterior cruciate ligament; HR, hazard ratio; HT, hamstring tendon; PT, patellar tendon; RTT, return to training.
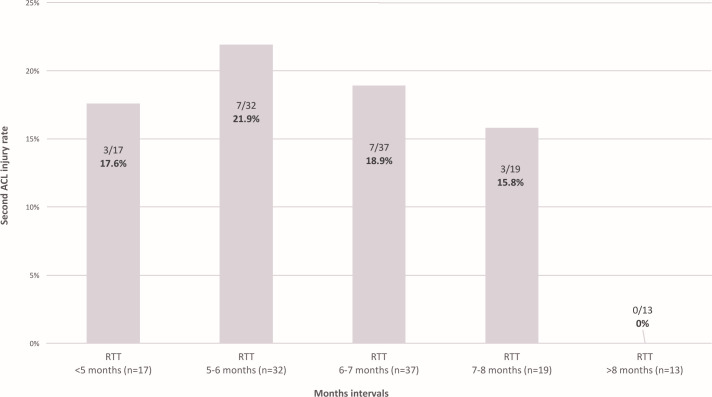
Time to RTT and second ACL injury
The mean time to RTT (177 (SD 33) vs 195 (SD 47) days, p=0.10) and to RTM (224 (SD 58) vs 241 (SD 63) days, p=0.28) were not significantly different between players who suffered a second ACL injury and those who did not. Likewise, RTT time was not an independent predictor of second ACL injury (table 4), but for every additional month before RTT there was a tendency towards a second ACL injury risk reduction (p=0.08). The other potential candidate factors, including leg dominance and graft type, were not significantly associated with second ACL injury (table 4).
In total, RTT within 5 months was seen in 14% (17/118), within 6 months in 42% (49/118), within 7 months in 73% (86/118), and within in 8 months in 89% (105/118) of the players (figure 2). None of the 13 players who had their RTT after 8 months sustained a second ACL injury, whereas 10 of 49 players (20.4%) with RTT within 6 months sustained a second ACL injury (figure 2).
Figure 2.
Second ACL injury rate stratified by return to training in monthly intervals. ACL, anterior cruciate ligament; RTT, return to training.
Risk factors for ipsilateral graft and contralateral ruptures
Having an isolated ACL injury was the only independent predictor of ipsilateral graft injury with a fourfold (HR 3.88, 95% CI 1.02 to 14.7) increased rate (online supplemental table 1). Also, a non-contact injury mechanism for the index ACL injury was the only independent predictor of contralateral ACL injury with an eightfold (HR 8.16, 95% CI 1.00 to 66.5) increased rate (online supplemental table 1).
bjsports-2020-103555supp001.pdf (27.8KB, pdf)
Career length
Career length analysis was carried out on the 118 players. At the end of the data collection, 74 players were still playing at the highest professional level, and 44 players had quit their top-level career (eight of them were still playing at lower level). Considering only players who quit top-level football within the data collection period (n=44), the median top-level career length was 4.1 (IQR 4.0) years after ACLR and 3.4 (IQR 3.9) years after RTT. The proportion of players still active at highest level 5 years after ACLR was 59.7% (table 5), and these players were significantly younger at the time of index ACL injury than players who had quit (24.2 (SD 3.4) vs 26.9 (SD 4.9) years, p=0.004). For players with a minimum follow-up of 5 years, 67% (30/45) of players 25 years or younger at the index ACLR were still playing compared with 51% (19/37) of players older than 25 years (p=0.02). Only two of 14 players over 30 years at the index ACLR were still playing at the top-level after 5 years.
Table 5.
Players still playing at the highest professional level following ACL reconstruction
| Follow-up | Players still playing at the top-level divided by the number of available players, n (%) * |
| 1 year | 114/118 (96.6) |
| 2 years | 99/107 (92.5) |
| 3 years | 77/95 (81.1) |
| 4 years | 58/84 (69.0) |
| 5 years | 49/82 (59.7) |
*The number of available players at the different follow-up times is the number of players with a minimum time from ACL reconstruction of 1, 2, 3, 4 and 5 years which means that, for example, only 82 players had a follow-up time greater than 5 years.
ACL, anterior cruciate ligament.
Discussion
The most important finding of this study on 118 male professional football players with index ACL injury and ACLR was that almost one out of five players (17.8%) sustained a second ACL injury within a median follow-up of 4.3 years. The second ACL injury incidence was particularly high for players with isolated index injuries with a non-contact injury mechanism (42%). Around 60% of players still played at top level 5 years after ACLR with a median professional career length of 3.4 years after RTT.
High second ACL injury rate
We found that 17.8% of players sustained a second ipsilateral graft or contralateral ACL rupture following ACLR and RTT within an average follow-up of 5 years. This finding extends previous literature on a general athletic population following ACLR, in particular with the pooled rate of second ACL injury (17.6%) in a systematic review including only clinical studies with a minimum follow-up of 5 years.26 Our findings are also similar to the pooled second ACL injury rate (15%) in a more recent systematic review including studies with a minimum follow-up of 1 year.9 However, second ACL injury rates in large single-centre consecutive patient series seem to be somewhat lower (9%–12% over 5 years from ACLR).27–29
Although providing important reinjury information on athletes in general, none of these reviews reflect the characteristics and environment of our cohort of professional football players. The RTT rate in this study was 100%, which is in line with other studies on male professional football players in Europe,1 3–6 but is considerably higher than in the average football player regardless of age or sex,15 30 or the general athlete.31 To date, the only existing re-injury data that aligns with our study was reported in a study on ACL anatomy and surgical technique where 21 ipsilateral graft ruptures occurred in 206 professional football players (10.2%) at a minimum follow-up of 2 years.18 No data on contralateral ACL injuries were reported in that study. Interestingly, similar rates of second ACL injuries (14%–16%) as in our study have also been reported in recent retrospective studies on professional football players in Europe using data from publicly available sources.4 19
In brief, several studies have identified an alarmingly high second ACL injury rate following ACLR and return to sport. Importantly, some studies indicate that football players seem to be more susceptible to second ACL injury than other athletes.13 32
Risk factors for second ACL injury
We identified two independent risk factors for second ACL injury. First, sustaining a non-contact ACL injury was associated with a sevenfold higher second ACL injury rate. This finding is important because non-contact injuries represent 44%–64% of ACL injuries in men’s professional football.25 33 These injuries typically occur in defensive pressing situations or when regaining balance after kicking.25 33–35 Non-contact injuries most likely reflect a preinjury predisposition to sustain ACL injury, either for non-modifiable (eg, family history, joint laxity, bony morphology, etc) or modifiable (eg, aggressive pressing playing style, altered biomechanics, neuromuscular deficits, etc) factors. These injuries and the modifiable risk factors can be targeted with neuromuscular training interventions.36–38 Second, sustaining an isolated ACL injury was associated with a threefold higher second ACL injury rate, in particular ipsilateral graft rupture. This finding therefore sheds new light on these ‘uncomplicated’ cases. For example, there was a shorter RTT time with these isolated injuries compared with ACL injuries with associated injuries (174 vs 202 days). Isolated ACL injury may reflect a different injury mechanism than ACL injury with concomitant joint injuries and this aspect needs to be further researched. A recent study found similar results on professional ski racers with an increased risk of contralateral ACL injury in athletes who had an isolated ACL injury.39
Importantly, when these two factors (non-contact and isolated ACL injury) were combined, we found that as many as 42% of players sustained a second ACL injury. The increased second ACL injury risk of non-contact and isolated ACL injuries is a novel and clinically very relevant finding which needs to be incorporated in the counselling of the player at the time of the index ACL injury in parallel with appropriate risk stratification management (such as appropriate communication of the second ACL injury risk before and following ACLR based on injury mechanism and pattern). The importance of high-quality evidence-based rehabilitation also needs to be communicated at this point together with emphasising that continuous secondary preventive strategies are warranted after RTT.40–42
RTT time and second ACL injury
Time to RTT as a continuous variable was not an independent risk factor for second ACL injury in our cohort, a finding in agreement with the two largest patient series to date involving more than 1000 patients each.28 29 It is worth noting, however, that relatively more second ACL injuries occurred among players with RTT within 6 months and that no player with RTT after 8 months sustained a second ACL injury. We found a tendency for a 28% injury risk reduction for every additional month until RTT. It is possible that a longer rehabilitation time would allow a better functional, neurological and biological recovery of the injured player.
The RTP clearance process is complex.43 There may be conflicting interests in the RTP decision,44 45 in particular for top-level professional players, with high-revenue contracts, who might have a strong internal motivation to come back as quick as possible and in turn accept a more ‘risk-taking’ approach. Given that it might take up to 2 years to achieve baseline joint biological health and function following ACLR, a delayed return to sport algorithm has been suggested.46 However, gaining acceptance of such a ‘2-year rule’ in professional football players would most likely not be feasible, considering the well-established injury risk-performance conflict in elite sports, particularly in top-level football.
Career length after index ACL injury
The average professional career length following RTT was 3.4 years in our study, which aligns closely with data from players in Major League Soccer (MLS) in the USA from 1996 to 2012.16 Two subsequent studies on the MLS between 2011 and 2016 and the two highest leagues of the ‘big 5’ European leagues between 2010 and 2017 reported shorter professional careers in ACL-injured players compared with matched controls.5 17 In our study, more than 90% of players were still playing at the top-level 2 years after ACLR, whereas this percentage dropped to 60% after 5 years, similar to the proportion (65%) previously reported from this cohort 3 years after RTT.1 One plausible explanation to this apparent year-by-year drop-off could be that ACL injury is associated with reduced performance after RTT.4 5 17 Another contributing factor is player age, with both the current study and another recent study,5 showing that players who still played at top-level after 5 years were significantly younger at injury.
Methodological considerations
This study has some limitations. First, we did not use a matched control group as some other studies in the field have done.5 13 17 However, next to studying the second ACL injury incidence, the main objective of this study was to investigate potential risk factors for second ACL injury. Second, no performance metrics data were collected. Third, no specific RTP details except for dates of first training and match (including match type and match minutes played) were collected, and we acknowledge that different rehabilitation regimes and RTT criteria may have been used in the clubs. Fourth, although most of the data after RTT were prospectively collected within the ECIS, we also relied on publicly available sources for longitudinal tracking of second ACL injuries and top-level playing career for some players having left the ECIS. This method has been used in recent studies and is valid for capture of severe injuries, in particular ACL injuries.4–6 13 19 22 Fifth, the lack of objective player data on physical and psychological parameters at the time of RTT made it impossible to study, for example, the influence of any muscle strength deficits which commonly exist at and after RTT.47 Sixth, the relative low sample size and the high HR with large CIs for the non-contact ACL injuries suggests possible sparse-data bias.48 However, considering the characteristics of our cohort and the prospective design over almost 20 years, this study has one of the largest datasets on top-level ACL-injured football players. Seventh, we did not adjust for team clustering, which should be taken into account when interpreting the width of the 95% CIs. Finally, our findings are most likely not applicable to semiprofessional or amateur male players returning to football following ACLR, nor to female or youth players.
Conclusion
The second ACL injury rate in professional male football players is high, affecting almost one out of five players over an average of 5 years. Having sustained an index non-contact injury or isolated ACL injury were both independent risk factors for second ACL injury, and these two factors combined were associated with a 42% s ACL injury rate. The median career length following RTT was 3.4 years and 60% of players still played top-level football 5 years after ACLR.
What are the findings?
The second anterior cruciate ligament (ACL) injury rate in professional male football players was 18% at a median follow-up of 4.3 years.
Index non-contact mechanism and isolated ACL injury increased the second ACL injury rate sevenfold and threefold.
Forty-two per cent of players with an index non-contact isolated ACL injury suffered a second ACL injury.
The median top-level career length following return to training after ACL reconstruction (ACLR) was 3.4 years and 60% of players still played at the same level 5 years following ACLR.
How might it impact on clinical practice in the future?
ACL injury is a serious concern for the professional footballer’s career.
Risk stratification for second ACL injury based on the injury mechanism and injury pattern of the index injury may be warranted.
Continuous secondary ACL injury reduction interventions are needed following index ACL injury.
Acknowledgments
The authors would like to thank the participating clubs (including contact persons, coaching staff, medical staff and all players) for their participation in the study. Sara De Lisio MA is acknowledged for statistical support. The Football Research Group has been established in Linköping, Sweden, in collaboration with Linköping University and through grants from the Union of European Football Associations, the Swedish Football Association, and the Swedish National Centre for Research in Sports.
Footnotes
Twitter: @fdellavilla, @MHgglund, @JanEkstrand, @MarkusWalden
Contributors: FDV, MH, SDV, JE and MW were responsible for the conception of the study. FDV and MW collected the data. FDV conducted the analyses together with the statistician; the analyses were planned and checked with MH and MW. FDV wrote the first draft of the paper which was critically revised by MH, SDV, JE and MW. All authors contributed to the interpretation of findings and had full access to all data. The final manuscript has been approved by all authors. MW is the study guarantor.
Funding: This study was funded by grants from the Union of European Football Associations.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study protocols were approved by the UEFA Football Development Division and the UEFA Medical Committee.
References
- 1. Waldén M, Hägglund M, Magnusson H, et al. ACL injuries in men's professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med 2016;50:744–50. 10.1136/bjsports-2015-095952 [DOI] [PubMed] [Google Scholar]
- 2. Weiler R, Monte-Colombo M, Mitchell A, et al. Non-operative management of a complete anterior cruciate ligament injury in an English Premier League football player with return to play in less than 8 weeks: applying common sense in the absence of evidence. BMJ Case Rep 2015. 10.1136/bcr-2014-208012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Return to sport after anterior cruciate ligament reconstruction in professional soccer players. Knee 2014;21:731–5. 10.1016/j.knee.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 4. Barth KA, Lawton CD, Touhey DC, et al. The negative impact of anterior cruciate ligament reconstruction in professional male footballers. Knee 2019;26:142–8. 10.1016/j.knee.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 5. Niederer D, Engeroff T, Wilke J, et al. Return to play, performance, and career duration after anterior cruciate ligament rupture: a case-control study in the five biggest football nations in Europe. Scand J Med Sci Sports 2018;28:2226–33. 10.1111/sms.13245 [DOI] [PubMed] [Google Scholar]
- 6. Krutsch W, Memmel C, Krutsch V, et al. High return to competition rate following ACL injury - A 10-year media-based epidemiological injury study in men's professional football. Eur J Sport Sci 2020;20:682–90. 10.1080/17461391.2019.1648557 [DOI] [PubMed] [Google Scholar]
- 7. Waldén M, Hägglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med 2006;40:158–62. 10.1136/bjsm.2005.021055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grassi A, Macchiarola L, Filippini M, et al. Epidemiology of anterior cruciate ligament injury in Italian first division soccer players. Sports Health 2020;12:279–88. 10.1177/1941738119885642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wiggins AJ, Grandhi RK, Schneider DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 2016;44:1861–76. 10.1177/0363546515621554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahldén M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 2012;40:2230–5. 10.1177/0363546512457348 [DOI] [PubMed] [Google Scholar]
- 11. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) Group. Am J Sports Med 2012;40:2517–22. 10.1177/0363546512459476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fältström A, Kvist J, Gauffin H, et al. Female soccer players with anterior cruciate ligament reconstruction have a higher risk of new knee injuries and quit soccer to a higher degree than knee-healthy controls. Am J Sports Med 2019;47:31–40. 10.1177/0363546518808006 [DOI] [PubMed] [Google Scholar]
- 13. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med 2016;44:2492–8. 10.1177/0363546516648439 [DOI] [PubMed] [Google Scholar]
- 14. Gans I, Retzky JS, Jones LC, et al. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association Sports: the injury surveillance program, 2004-2014. Orthop J Sports Med 2018;6:232596711877782. 10.1177/2325967118777823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sandon A, Engström B, Forssblad M. High risk of further anterior cruciate ligament injury in a 10-year follow-up study of anterior cruciate ligament-reconstructed soccer players in the Swedish National Knee Ligament Registry. Arthroscopy 2020;36:189–95. 10.1016/j.arthro.2019.05.052 [DOI] [PubMed] [Google Scholar]
- 16. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sports Med 2013;1:232596711349718. 10.1177/2325967113497189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arundale AJH, Silvers-Granelli HJ, Snyder-Mackler L. Career length and injury incidence after anterior cruciate ligament reconstruction in Major League Soccer players. Orthop J Sports Med 2018;6:232596711775082. 10.1177/2325967117750825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Śmigielski R, Zdanowicz U, Drwięga M, et al. The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J 2016;98-B:1020–6. 10.1302/0301-620X.98B8.37117 [DOI] [PubMed] [Google Scholar]
- 19. Schiffner E, Latz D, Grassmann JP, et al. Anterior cruciate ligament ruptures in German elite soccer players: epidemiology, mechanisms, and return to play. Knee 2018;25:219–25. 10.1016/j.knee.2018.01.010 [DOI] [PubMed] [Google Scholar]
- 20. Waldén M, Hägglund M, Ekstrand J. UEFA Champions League study: a prospective study of injuries in professional football during the 2001-2002 season. Br J Sports Med 2005;39:542–6. 10.1136/bjsm.2004.014571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hägglund M, Waldén M, Bahr R, et al. Methods for epidemiological study of injuries to professional football players: developing the UEFA model. Br J Sports Med 2005;39:340–6. 10.1136/bjsm.2005.018267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leventer L, Eek F, Hofstetter S, et al. Injury patterns among elite football players: a media-based analysis over 6 seasons with emphasis on playing position. Int J Sports Med 2016;37:898–908. 10.1055/s-0042-108201 [DOI] [PubMed] [Google Scholar]
- 23. Locks R, Utsunomiya H, Briggs KK, et al. Return to play after hip arthroscopic surgery for femoroacetabular impingement in professional soccer players. Am J Sports Med 2018;46:273–9. 10.1177/0363546517738741 [DOI] [PubMed] [Google Scholar]
- 24. Grassi A, Rossi G, D'Hooghe P, et al. Eighty-two per cent of male professional football (soccer) players return to play at the previous level two seasons after Achilles tendon rupture treated with surgical repair. Br J Sports Med 2020;54:480–6. 10.1136/bjsports-2019-100556 [DOI] [PubMed] [Google Scholar]
- 25. Della Villa F, Buckthorpe M, Grassi A, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med 2020;54:1423–32. 10.1136/bjsports-2019-101247 [DOI] [PubMed] [Google Scholar]
- 26. Wright RW, Magnussen RA, Dunn WR, et al. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am 2011;93:1159–65. 10.2106/JBJS.J.00898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 2005;21:948–57. 10.1016/j.arthro.2005.04.110 [DOI] [PubMed] [Google Scholar]
- 28. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 2009;37:246–51. 10.1177/0363546508325665 [DOI] [PubMed] [Google Scholar]
- 29. King E, Richter C, Jackson M, et al. Factors influencing return to play and second anterior cruciate ligament injury rates in level 1 athletes after primary anterior cruciate ligament reconstruction: 2-year follow-up on 1432 reconstructions at a single center. Am J Sports Med 2020;48:812–24. 10.1177/0363546519900170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sandon A, Werner S, Forssblad M. Factors associated with returning to football after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2015;23:2514–21. 10.1007/s00167-014-3023-4 [DOI] [PubMed] [Google Scholar]
- 31. Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48:1543–52. 10.1136/bjsports-2013-093398 [DOI] [PubMed] [Google Scholar]
- 32. Andernord D, Desai N, Björnsson H, et al. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med 2015;43:121–7. 10.1177/0363546514552788 [DOI] [PubMed] [Google Scholar]
- 33. Waldén M, Krosshaug T, Bjørneboe J, et al. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med 2015;49:1452–60. 10.1136/bjsports-2014-094573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grassi A, Smiley SP, Roberti di Sarsina T, et al. Mechanisms and situations of anterior cruciate ligament injuries in professional male soccer players: a YouTube-based video analysis. Eur J Orthop Surg Traumatol 2017;27:967–81. 10.1007/s00590-017-1905-0 [DOI] [PubMed] [Google Scholar]
- 35. Brophy RH, Stepan JG, Silvers HJ, et al. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports Health 2015;7:244–9. 10.1177/1941738114535184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res 2018;36:2696–708. 10.1002/jor.24043 [DOI] [PubMed] [Google Scholar]
- 37. Arundale AJH, Capin JJ, Zarzycki R, et al. Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-SPORTS). Int J Sports Phys Ther 2018;13:422–31. 10.26603/ijspt20180422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nagelli C, Di Stasi S, Tatarski R, et al. Neuromuscular training improves self-reported function and single-leg landing hip biomechanics in athletes after anterior cruciate ligament reconstruction. Orthop J Sports Med 2020;8:2325967120959347. 10.1177/2325967120959347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Csapo R, Runer A, Hoser C, et al. Contralateral ACL tears strongly contribute to high rates of secondary ACL injuries in professional Ski racers. Knee Surg Sports Traumatol Arthrosc 2020. 10.1007/s00167-020-06234-8. [Epub ahead of print: 17 Aug 2020]. [DOI] [PubMed] [Google Scholar]
- 40. Della Villa S, Boldrini L, Ricci M, et al. Clinical outcomes and return-to-sports participation of 50 soccer players after anterior cruciate ligament reconstruction through a sport-specific rehabilitation protocol. Sports Health 2012;4:17–24. 10.1177/1941738111417564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Buckthorpe M, Della Villa F, Della Villa S, et al. On-field rehabilitation Part 1: 4 pillars of high-quality on-field rehabilitation are restoring movement quality, physical conditioning, restoring sport-specific skills, and progressively developing chronic training load. J Orthop Sports Phys Ther 2019;49:565–9. 10.2519/jospt.2019.8954 [DOI] [PubMed] [Google Scholar]
- 42. Buckthorpe M, Della Villa F, Della Villa S, et al. On-field rehabilitation Part 2: a 5-stage program for the soccer player focused on linear movements, multidirectional movements, soccer-specific skills, soccer-specific movements, and modified practice. J Orthop Sports Phys Ther 2019;49:570–5. 10.2519/jospt.2019.8952 [DOI] [PubMed] [Google Scholar]
- 43. Meredith SJ, Rauer T, Chmielewski TL, et al. Return to sport after anterior cruciate ligament injury: Panther Symposium ACL Injury Return to Sport Consensus Group. Knee Surg Sports Traumatol Arthrosc 2020;28:2403–14. 10.1007/s00167-020-06009-1 [DOI] [PubMed] [Google Scholar]
- 44. Dijkstra HP, Pollock N, Chakraverty R, et al. Return to play in elite sport: a shared decision-making process. Br J Sports Med 2017;51:419–20. 10.1136/bjsports-2016-096209 [DOI] [PubMed] [Google Scholar]
- 45. McCall A, Lewin C, O'Driscoll G, et al. Return to play: the challenge of balancing research and practice. Br J Sports Med 2017;51:702–3. 10.1136/bjsports-2016-096752 [DOI] [PubMed] [Google Scholar]
- 46. Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med 2017;47:221–32. 10.1007/s40279-016-0584-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Herrington L, Ghulam H, Comfort P. Quadriceps strength and functional performance after anterior cruciate ligament reconstruction in professional soccer players at time of return to sport. J Strength Cond Res 2021:769–75. [DOI] [PubMed] [Google Scholar]
- 48. Leopold SS, Porcher R. Sparse-data bias-what the savvy reader needs to know. Clin Orthop Relat Res 2018;476:657–9. 10.1007/s11999.0000000000000228 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2020-103555supp001.pdf (27.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.