Abstract
Background
Individual differences in physical activity behavior are associated with a collection of individual and environmental factors manifesting as barriers to participation. Understanding how barriers to physical activity differ based on sociodemographic characteristics can support identification and elimination of health inequities.
Objectives
To compare the odds of reporting individual and environmental barriers to physical activity in rural and urban adults, and explore interactions between rural-urban location and sociodemographic factors to characterize patterns in barriers to physical activity.
Design
Cross-sectional.
Methods
We analyzed the 2017 Canadian Community Health Survey Barriers to Physical Activity Rapid Response, with a final weighted sample of 24,499,462 (unweighted n=21,967). The likelihood of reporting each barrier domain based on rural-urban location was examined using binary logistic regression following a model-fitting approach with sociodemographic characteristics as covariates or interaction terms.
Results
Adjusting for sociodemographic factors, rural residents showed 85% higher odds of reporting at least one social or built environmental barrier (OR=1.85 [1.66, 2.07]). Compared to urban residents, rural residents showed significantly higher odds of reporting barriers to facility access (OR=4.15 [3.58, 4.83]) and a lack of social support to be active (OR=1.17 [1.04, 1.32]). Urban residents reported lower preference for physical activity, lower enjoyment of physical activity and lower confidence in their ability to regularly engage in physical activity. Interactions between socioeconomic status and location were identified related to enjoyment and confidence to be active. There was no effect of location on predicting the odds of reporting an individual resource-related variable (e.g., time, energy).
Conclusions
Despite being more likely than urban residents to prefer and enjoy physical activity, rural residents have fewer opportunities and receive less social support to be active. It is important to consider geographic location when characterizing barriers to physical activity and in the development of context-specific health promotion strategies.
Keywords: Rural health, Barriers, Physical activity, Exercise, Health promotion, Social-ecological model, Rural-urban disparities
Highlights
-
•
Rural residents have a higher odds of reporting social or built environmental barriers to physical activity.
-
•
The most common environmental barrier for rural residents was lack of access to free or low-cost facilities.
-
•
Urban residents reported a lower preference and enjoyment of physical activity.
-
•
There was no rural-urban location-based difference in barriers related to time or costs to be active.
-
•
It is important to consider geographic location and sex when characterising barriers to physical activity.
1. Introduction
Regular participation in physical activity has well-established benefits for noncommunicable disease prevention and management, life expectancy, and quality of life (Clarke & Janssen, 2021; Ekelund et al., 2019; Lee et al., 2012; Marquez et al., 2020). Consistent inequities in physical activity participation can contribute to widening health inequities (Eikemo et al., 2014; WHO, 2013). To support uptake and promotion of physical activity guidelines, it is necessary to characterize barriers to physical activity behavior, particularly in populations at increased risk of inactivity.
Compared to adults living in urban centres, rural residents have a poorer overall health status, higher rates of noncommunicable disease, and reduced life expectancy (Long et al., 2020; Pong et al., 2009). Multiple sociostructural and environmental factors have been associated with rural-urban health inequities (Marmot et al., 2008; Leipert and George, 2008). Rural residents tend to be less physically active and more sedentary compared to their urban counterparts (Martin et al., 2005; Parks et al., 2003), although there is evidence to suggest this trend varies by country, region, measurement approach (i.e., device-based vs. self-report), and sociodemographic factors such as sex (Yip et al., 2016; Fan et al., 2014; Forbes et al., 2020; Pelletier, White, et al., 2021). Considering the undeniable benefits of physical activity, adopting a location-specific approach to characterizing barriers to physical activity will aid the development of strategies to address rural-urban health inequities.
According to the social-ecological model of behavior, physical activity is shaped by interdependent factors at individual, social, environmental, and policy levels (Bauman et al., 2012; Sallis et al., 2006). Based on the social-ecological framework, barriers to physical activity can be classified at individual/intrapersonal (e.g., time, cost), social/interpersonal (e.g., support from family, seeing other people be active), policy (e.g., traffic controls and zoning guidelines), and structural/built environmental (e.g., access to facilities) levels (Bauman et al., 2012; Sallis et al., 2006). Engagement in physical activity reflects the combination of intrapersonal and interpersonal factors within a given environment and the fit between individual and environmental circumstances. Compared to their urban counterparts, rural residents in the United States are more likely to report lower social support, limited access to and distance from exercise facilities, and built environment characteristics such as lack of accessible facilities, sidewalks and bike paths as barriers to physical activity (Brownson et al., 2000; Eyler, 2003; Parks et al., 2003; Wilcox et al., 2000). In contrast to the barriers imposed by rural environments, common features of urban environments such as access to exercise facilities, active transportation opportunities, and increased density and mixed land use facilitate physical activity participation (McCormack & Shiell, 2011; Heath et al., 2006).
In addition to the distinct social and built environmental context of rural communities, patterns of sociodemographic factors including income, educational attainment, and age vary between rural and urban populations – all factors associated with physical activity engagement (Plotnikoff et al., 2004; Singh, 2003; Zarifa et al., 2019). In our recent study examining the odds of meeting physical activity guidelines, we identified an interaction between rural-urban location and self-identified sex (Pelletier, White, et al., 2021). In this analysis, rural males were more likely to meet physical activity guidelines compared to urban males and urban females were more likely to meet physical activity guidelines compared to rural females (Pelletier, White, et al., 2021). Considering sociodemographic factors as covariates and/or moderators in the relationship between barriers to physical activity and rural-urban location is important as some barriers, such as social support and time, are more important for women (Sallis et al., 1992), and the relationship between facility access and physical activity varies based on education (Pan et al., 2009).
To understand patterns in barriers to physical activity we conducted a study aimed at: 1) comparing the odds of reporting individual and environmental barriers to physical activity in rural and urban adults; and 2) exploring the interaction between rural-urban location and sociodemographic factors to characterize barriers to physical activity.
2. Methods
2.1. Participants
We analyzed cross-sectional data from the 2017 cycle of the Canadian Community Health Survey (CCHS; response rate: 62.8%). The CCHS is an annual survey providing a representative sample of the Canadian population over 12 years of age. The CCHS excludes less than 3% of the Canadian population, including individuals living on Indigenous reserves and Crown Lands, full time members of the Canadian Forces, institutional residents, youth in foster care, and residents of other remote regions.
The Barriers to Physical Activity Rapid Response module was an optional component for CCHS respondents during the 2017 data collection cycle (collected between July and December, response rate: 61.6%) and additionally excludes those residing in the Canadian territories.
Prior to conducting any assessments of the data, we excluded all youth participants (age <18, n = 2149). Subsequently, we excluded adults who reported currently being pregnant or who did not answer (n = 296), and individuals with missing data (refusal or not stated responses) or an answer of “don't know” on any variable of interest (n=3611). Our final, unweighted sample of adult survey respondents was n=21,967, corresponding to a population-weighted n=24,499,462 Canadians per weights provided by Statistics Canada. All data were vetted following Statistics Canada policies to protect participant confidentiality.
2.2. Variables
2.2.1. Barriers to physical activity
Ten barriers were assessed with the CCHS Barriers to Physical Activity Rapid Response. One question regarding access to showers or change rooms at a participants’ place of work was removed from our analysis (BPA_050). This question was only asked for a small subset of the sample based on employment status. Thus, nine barriers are included in this analysis. We categorized barriers as individual (motivation- or resource-related) and environmental (social and built) based on the social-ecological model and to align with previous work (Bauman et al., 2012; Pan et al., 2009; Sallis et al., 2006). Participants rated their agreement with a series of statements related to individual (6 items) and environmental (3 items) barriers to physical activity from 1 = strongly agree to 4 = strongly disagree. Barriers were recoded into numeric binary variables, collapsing “Strongly Agree” and “Agree”, and “Disagree” and “Strongly Disagree”. Barriers were coded as 1 (barrier reported) or 0 (no barrier reported).
We divided individual barriers into resource-related barriers (3 items) and motivation-related barriers (3 items). Individual resource-related barriers were measured with the following items:
-
•
“I have enough energy to be physically active on a regular basis”
-
•
“I have enough time to be physically active on a regular basis”
-
•
“I can afford the costs of being physically active on a regular basis”
Individual motivation-related barriers were measured with the following items:
-
•
“I prefer to be physically active rather than sitting or lying down” For example, physical activities could include doing chores around the house, biking to work, playing sports and going to the gym. Activities while sitting or lying down could include watching TV, reading or using electronics.
-
•
“I am confident in my ability to engage in physical activity”
-
•
“I enjoy being physically active”
Three items measured environmental barriers including social (2 items) and built (1 item) environment:
-
•
“I often see people in my community being physically active” Community means an area around your house, school or work, where you spend most of your time.
-
•
“I receive support to be physically active on a regular basis from friends, family members or other people in my life”
-
•
“My neighbourhood has several free or low-cost recreation facilities, such as parks, walking trails, bike paths, recreation centres, playgrounds or public swimming pools”
2.2.2. Sociodemographic information
Participants were asked to self-identify their sex, with the options of male or female. Age was self-reported and treated as a grand-mean-centred continuous measure. Body mass index (BMI) was derived from self-reported height and weight, adjusted for self-report bias (Gorber et al., 2007), and grand-mean-centred. The three-level variable EHG2DVR3 was used to describe participants' education (less than secondary school graduation/secondary school graduation/post-secondary certificate, diploma, or university degree). A fifteen-level variable, INCDVHH, reflected participant's self-reported household income and was collapsed into roughly equal quintiles across the following income divisions: $0–29,999; $30,000–59,999; $60,000–99,999; $100,000–149,999; ≥$150,000. Self-identified sex was coded male=0 and female=1; education and income were coded such that the mode represented the reference level for the regression intercept (education: secondary school graduation=0; income: $60,000–99,999=0).
2.2.3. Perceived health
Perceived health status was reported across five levels, ranging from poor to excellent using the GENDVHDI variable. We coded this variable to “centre” a relatively representative categorical rating (Good=0) to serve as a reference level within the regression analyses.
2.2.4. Sense of belonging to community
Respondents’ sense of belonging to their community was included in the analysis based on previous quantitative (Yip et al., 2016) and qualitative (McGannon et al., 2014; Witcher et al., 2007) work indicating the role of community social engagement as a facilitator of physical activity behavior in rural communities. The variable GEN_030 was used to assess sense of belonging across four levels from Very Strong to Very Weak. This variable was reverse coded such that Very Weak=0 served as the reference level.
2.2.5. Season of data collection
The CCHS sampling strategy is subdivided into two equal data collection periods spanning: 1) July to September (Summer/Fall); and 2) October to December (Fall/Winter). Because these sampling periods roughly correspond to changing seasons, which are associated with a fluctuation in physical activity participation (Turrisi et al., 2021), this variable was included as a potential factor of interest in the regression analyses. The first sampling period in the rapid response module (July–September) was coded as 0 to anchor the regression analyses.
2.3. Data analysis
Data analysis was conducted using R 3.4.3 (R Core Team, 2019) and packages arsenal (Heinzen et al., 2019) and survey (Lumley, 2019). For all analyses, survey weights were employed to ensure the sample was representative of the Canadian population and bootstrap replicate weights were employed for variance calculations due to the complex clustering in CCHS sampling procedures.
We examined the odds of reporting barriers to physical activity using binary logistic regression with a model-fitting approach. Only variables that contributed to explaining significant variance in the outcome were retained, except for the location variable which was always retained given a priori aims.
For each outcome, a base model was first computed to examine the effect of location as a predictor1 of reported barriers. Subsequently, a covariate model was estimated adding all a priori identified covariates. Next, covariates were removed sequentially in order of smallest t-values, and model comparisons were conducted until no further covariates could be removed from the model without reducing its explanatory power. The remaining model terms were then systematically estimated in 2-way interactions with the location factor, after which any significant 2-way interactions were explored with 3-way interaction tests. Model comparisons were conducted to determine whether interaction terms added meaningfully to each model. In all cases, the final model presented represents the optimally fitted model for the dataset, retaining location as a factor of theoretical interest. Models were examined for influential cases per the recommendations for binomial logistic regression (Zhang, 2016).
To reduce the number of tests conducted across the nine barrier items, we first collapsed barriers into three high-level factors: social and built environmental, individual motivation-related, and individual resource-related (Bauman et al., 2012; Pan et al., 2009; Sallis et al., 2006). Each was treated as a binary outcome (i.e., any environmental barrier reported=1 vs. none reported=0) and the effect of location examined. If the effect of location was non-significant in the optimally fitted model, we did not pursue further analysis of barriers. Where the effect of location remained significant in the optimally fitted model, we conducted a follow-up series of models using the separate barrier items comprising the high-level category (e.g., environmental barriers were examined individually in distinct models).
3. Results
3.1. Participants
Participant sociodemographic characteristics by rural-urban location are presented in Table 1. The excluded sample differed significantly from the included sample on several sociodemographic characteristics and the reporting of several barriers to physical activity (Table 2, Table 3).
Table 1.
Population-weighted demographics by rural-urban location.
| Variables of interest | Rural (N = 4209008) |
Urban (N = 20290454) |
Total (N = 24499462) |
p-value | ||||
|---|---|---|---|---|---|---|---|---|
| N | %/SE | N | %/SE | N | %/SE | |||
| Season | Summer | 2012891 | 47.8 | 10218419 | 50.4 | 12231310 | 49.9 | 0.262 |
| Fall | 2196117 | 52.2 | 10072035 | 49.6 | 12268152 | 50.1 | ||
| Sex | Male | 2072934 | 49.2 | 10270509 | 50.6 | 12343443 | 50.4 | 0.282 |
| Female | 2136074 | 50.8 | 10019945 | 49.4 | 12156019 | 49.6 | ||
| Age | Mean | 50.6 | 0.354 | 46.1 | 0.138 | 46.9 | 0.102 | <.001 |
| 95% CI | [49.9, 51.3] | [45.8, 46.3] | [46.7, 47.1] | |||||
| BMI | Mean | 28.3 | 0.137 | 27.2 | 0.074 | 27.4 | 0.068 | <.001 |
| 95% CI | [28.0, 28.5] | [27.1, 27.4] | [27.3, 27.5] | |||||
| Education | Less than high school | 677597.1 | 16.1 | 1731009.5 | 8.5 | 2408606.6 | 9.8 | <.001 |
| High school | 1206112.2 | 28.7 | 5033644 | 24.8 | 6239756.2 | 25.5 | ||
| Post-secondary | 2325298.4 | 55.2 | 13525800.5 | 66.7 | 15851098.9 | 64.7 | ||
| Income | $0–29,999 | 485665.7 | 11.5 | 2563632.1 | 12.6 | 3049297.8 | 12.4 | <.001 |
| $30–59,999 | 942434.9 | 22.4 | 4041778 | 19.9 | 4984212.9 | 20.3 | ||
| $60–99,999 | 1126413.9 | 26.8 | 4927414.2 | 24.3 | 6053828.1 | 24.7 | ||
| $100–149,999 | 899355.1 | 21.4 | 4251121.1 | 21.0 | 5150476.2 | 21.0 | ||
| $150,000+ | 755138 | 17.9 | 4506508.5 | 22.2 | 5261646.5 | 21.5 | ||
| Perceived Health | Excellent | 1032096.9 | 24.5 | 4968586 | 24.5 | 6000682.9 | 24.5 | 0.02 |
| Very good | 1565836.6 | 37.2 | 7808784.6 | 38.5 | 9374621.2 | 38.3 | ||
| Good | 1145131.2 | 27.2 | 5649887.1 | 27.8 | 6795018.3 | 27.7 | ||
| Fair | 347232.5 | 8.2 | 1475061.9 | 7.3 | 1822294.4 | 7.4 | ||
| Poor | 118710.4 | 2.8 | 388134.4 | 1.9 | 506844.8 | 2.1 | ||
| Sense of Belonging to Community | Very Strong | 854929.3 | 20.3 | 3281955.4 | 16.2 | 4136884.7 | 16.9 | <.001 |
| Somewhat strong | 2077782 | 49.4 | 10527191.8 | 51.9 | 12604973.8 | 51.5 | ||
| Somewhat weak | 988478.6 | 23.5 | 5063461.5 | 25.0 | 6051940.1 | 24.7 | ||
| Very Weak | 287817.7 | 6.8 | 1417845.3 | 7.0 | 1705663 | 7.0 | ||
P-values obtained by t-test for continuous variables or Chi-square test for categorical factors.
Table 2.
Population-weighted demographics for included vs. excluded participants.
| Variables of interest | Excluded (N=4331267.6) |
Included (N=24499461.6) |
Total (N=28,830,729.2) |
p-value |
||||
|---|---|---|---|---|---|---|---|---|
| N | %/SE | N | %/SE | N | %/SE | |||
| Location | Urban | 3628699.7 | 83.8 | 20290454 | 82.8 | 23919153.7 | 83.0 | 0.271 |
| Rural | 702567.9 | 16.2 | 4209007.6 | 17.2 | 4911575.5 | 17.0 | ||
| Season | Summer | 2171827 | 50.1 | 12231310 | 49.9 | 14403137 | 50.0 | 0.889 |
| Fall | 2159441 | 49.9 | 12268152 | 50.1 | 14427593 | 50.0 | ||
| Sex | Male | 1837785 | 42.4 | 12343442 | 50.4 | 14181227 | 49.2 | <.001 |
| Female | 2493482 | 57.6 | 12156019 | 49.6 | 14649501 | 50.8 | ||
| Age | Mean (SE) | 54.4 | 0.5 | 46.8 | 0.1 | 48 | 0.1 | <.001 |
| 95% CI | [53.4, 55.5] | [46.7, 47.1] | [47.9, 48.1] | |||||
| BMI | Mean (SE) | 27.6 | 0.2 | 27.4 | 0.1 | 27.4 | 0.1 | 0.39 |
| 95% CI | [27.2, 27.9] | [27.3, 27.5] | [27.3, 27.5] | |||||
| Education | Less than high school | 788053.8 | 20.4 | 2455527.2 | 9.8 | 3243581 | 11.3 | <.001 |
| High school | 1003997.4 | 26.1 | 6361309.1 | 25.5 | 7365306.5 | 25.5 | ||
| Post-secondary | 2061957.2 | 53.5 | 16159884.5 | 64.7 | 18221841.7 | 63.2 | ||
| Income | $0–29,999 | 765471.3 | 17.7 | 3049297.8 | 12.4 | 3814769.1 | 13.2 | <.001 |
| $30–59,999 | 1189721.1 | 27.5 | 4984212.9 | 20.3 | 6173934 | 21.4 | ||
| $60–99,999 | 1020559.8 | 23.6 | 6053828.1 | 24.7 | 7074387.9 | 24.5 | ||
| $100–149,999 | 722784.9 | 16.7 | 5150476.2 | 21.0 | 5873261.1 | 20.4 | ||
| $150,000+ | 632730.5 | 14.6 | 5261646.6 | 21.5 | 5894377.1 | 20.4 | ||
| Perceived Health | Excellent | 339047.4 | 7.9 | 507274.4 | 2.1 | 846321.8 | 2.9 | <.001 |
| Very good | 593031.3 | 13.8 | 1823839 | 7.4 | 2416870.3 | 8.4 | ||
| Good | 1392037.4 | 32.3 | 6800777.6 | 27.7 | 8192815 | 28.4 | ||
| Fair | 1170851.4 | 27.2 | 9382566.9 | 38.3 | 10553418.3 | 36.6 | ||
| Poor | 815534.9 | 18.9 | 6005768.8 | 24.5 | 6821303.7 | 23.7 | ||
| Sense of Belonging to Community | Very Strong | 395390.7 | 12.2 | 1781127.6 | 7.0 | 2176518.3 | 7.5 | <.001 |
| Somewhat strong | 692068.2 | 21.3 | 6319699.4 | 24.7 | 7011767.6 | 24.3 | ||
| Somewhat weak | 1578679.5 | 48.6 | 13162662.4 | 51.5 | 14741341.9 | 51.1 | ||
| Very Weak | 581186.4 | 17.9 | 4319915.1 | 16.9 | 4901101.5 | 17.0 | ||
P-values obtained from t-test or Chi-square test as appropriate.
Note: total included n's for individual self-report variables may sum to greater than the sample-wide included N due to participants missing data on some but not all items. All participants with missing data on any item were marked for sample-wide exclusion.
Table 3.
Population-weighted reporting of barriers for included and excluded participants.
| Variables of interest | Excluded (N=4331267.6) |
Included (N=24499461.6) |
Total (N=28,830,729.2) |
p-value |
||||
|---|---|---|---|---|---|---|---|---|
| N | %/SE | N | %/SE | N | %/SE | |||
| Prefer to be active than sitting/lying down | Strongly agree | 59766.23 | 1.8 | 364652.64 | 1.4 | 424418.87 | 1.5 | 0.004 |
| Somewhat agree | 388393.32 | 11.4 | 2422832.66 | 9.5 | 2811225.98 | 9.8 | ||
| Somewhat disagree | 1810701.69 | 53.1 | 12561610.41 | 49.4 | 14372312.1 | 49.9 | ||
| Strongly disagree | 1150313.71 | 33.7 | 10072458.54 | 39.6 | 11222772.25 | 38.9 | ||
| Sees people in community being active | Strongly agree | 90460.47 | 2.8 | 372717.84 | 1.5 | 463178.31 | 1.6 | <.001 |
| Somewhat agree | 498240.93 | 15.5 | 3269083.82 | 12.8 | 3767324.75 | 13.1 | ||
| Somewhat disagree | 1924449.75 | 60.0 | 15153196.09 | 59.1 | 17077645.84 | 59.2 | ||
| Strongly disagree | 691612.94 | 21.6 | 6830967.36 | 26.7 | 7522580.3 | 26.1 | ||
| Receives support to be physically active | Strongly agree | 165187.5 | 5.0 | 790384.8 | 3.1 | 955572.3 | 3.3 | <.001 |
| Somewhat agree | 771864.3 | 23.6 | 4999807 | 19.6 | 5771671.3 | 20.0 | ||
| Somewhat disagree | 1701320.8 | 51.9 | 13239604.5 | 51.8 | 14940925.3 | 51.8 | ||
| Strongly disagree | 638092.8 | 19.5 | 6524467.4 | 25.5 | 7162560.2 | 24.8 | ||
| Has enough energy to be physically active | Strongly agree | 878143.32 | 25.6 | 7888364.37 | 31.1 | 8766507.69 | 30.4 | <.001 |
| Somewhat agree | 1969322.26 | 57.5 | 14427542.27 | 56.8 | 16396864.53 | 56.9 | ||
| Somewhat disagree | 484760.1 | 14.1 | 2647277.67 | 10.4 | 3132037.77 | 10.9 | ||
| Strongly disagree | 93998.87 | 2.7 | 441320.34 | 1.7 | 535319.21 | 1.9 | ||
| Has enough time to be physically active | Strongly agree | 687973 | 20.0 | 5983834.5 | 23.6 | 6671807.5 | 23.1 | 0.066 |
| Somewhat agree | 1961285.3 | 57.0 | 13972368.6 | 55.0 | 15933653.9 | 55.3 | ||
| Somewhat disagree | 685402.3 | 19.9 | 4749147.1 | 18.7 | 5434549.4 | 18.8 | ||
| Strongly disagree | 106408 | 3.1 | 684310.5 | 2.7 | 790718.5 | 2.7 | ||
| Can afford to be physically active | Strongly agree | 549635.1 | 16.9 | 6483431.8 | 25.3 | 7033066.9 | 24.4 | <.001 |
| Somewhat agree | 1929996 | 59.3 | 14848993.4 | 58.1 | 16778989.4 | 58.2 | ||
| Somewhat disagree | 634826.5 | 19.5 | 3572545.6 | 14.0 | 4207372.1 | 14.6 | ||
| Strongly disagree | 139338.8 | 4.3 | 671962.1 | 2.6 | 811300.9 | 2.8 | ||
| Neighbourhood has several free/low-cost facilities | Strongly agree | 865148.06 | 28.1 | 9124212.2 | 35.4 | 9989360.26 | 34.6 | <.001 |
| Somewhat agree | 1649956.33 | 53.5 | 13467874.05 | 52.3 | 15117830.38 | 52.4 | ||
| Somewhat disagree | 478851.81 | 15.5 | 2564759.97 | 10.0 | 3043611.78 | 10.6 | ||
| Strongly disagree | 87922.57 | 2.9 | 592004.21 | 2.3 | 679926.78 | 2.4 | ||
| Has confidence in ability to be physically active | Strongly agree | 1005478.9 | 29.6 | 9854006.7 | 38.7 | 10859485.6 | 37.7 | <.001 |
| Somewhat agree | 1959451.9 | 57.7 | 13669967.4 | 53.7 | 15629419.3 | 54.2 | ||
| Somewhat disagree | 338191.5 | 10.0 | 1595908.7 | 6.3 | 1934100.2 | 6.7 | ||
| Strongly disagree | 91420.7 | 2.7 | 316303.3 | 1.2 | 407724 | 1.4 | ||
| Enjoys physical activity | Strongly agree | 1012888.25 | 29.7 | 9921909.78 | 39.0 | 10934798.03 | 37.9 | <.001 |
| Somewhat agree | 2099144.11 | 61.6 | 13786627.89 | 54.2 | 15885772 | 55.1 | ||
| Somewhat disagree | 264094.29 | 7.8 | 1558592.06 | 6.1 | 1822686.35 | 6.3 | ||
| Strongly disagree | 29473.81 | 0.9 | 157999.01 | 0.6 | 187472.82 | 0.7 | ||
| Has access to showers at or near work | No | 1092824.2 | 38.8 | 9632549.4 | 37.0 | 10725373.6 | 37.2 | 0.246 |
| Yes | 1067459 | 37.9 | 10850832.2 | 41.7 | 11918291.2 | 41.3 | ||
| Not applicable | 654242.6 | 23.2 | 5532821.8 | 21.3 | 6187064.4 | 21.5 | ||
| Number of social and built environmental barriers | 0 | 1462692.8 | 56.1 | 16429488.58 | 62.7 | 17892181.38 | 62.1 | 0.008 |
| 1 | 773658.62 | 29.7 | 7132026.4 | 27.2 | 7905685.02 | 27.4 | ||
| 2 | 295804.26 | 11.3 | 2230102.5 | 8.5 | 2525906.76 | 8.8 | ||
| 3 | 76816.96 | 2.9 | 430139.07 | 1.6 | 506956.03 | 1.8 | ||
| Number of individual barriers | 0 | 1464091 | 51.2 | 15219868.1 | 58.6 | 16683959.1 | 57.9 | <.001 |
| 1 | 704910.6 | 24.7 | 5666590.8 | 21.8 | 6371501.4 | 22.1 | ||
| 2 | 338786 | 11.9 | 2809016.3 | 10.8 | 3147802.3 | 10.9 | ||
| 3+ | 350239.8 | 12.3 | 2277226.8 | 8.8 | 2627466.6 | 9.1 | ||
| Number of motivation-related individual barriers | 0 | 2470805.43 | 77.0 | 21145223.89 | 82.5 | 23616029.32 | 81.9 | <.001 |
| 1 | 521035.59 | 16.2 | 2897694.48 | 11.3 | 3418730.07 | 11.9 | ||
| 2 | 144692.07 | 4.5 | 1167901.15 | 4.6 | 1312593.22 | 4.6 | ||
| 3+ | 72745.72 | 2.3 | 410630.87 | 1.6 | 483376.59 | 1.7 | ||
| Number of resource-related individual barriers | 0 | 1751483.9 | 56.2 | 16547853.6 | 64.3 | 18299337.5 | 63.5 | <.001 |
| 1 | 857618.7 | 27.5 | 6051014.9 | 23.5 | 6908633.6 | 24.0 | ||
| 2 | 383543.5 | 12.3 | 2504463.2 | 9.7 | 2888006.7 | 10.0 | ||
| 3+ | 122321.8 | 3.9 | 612429.6 | 2.4 | 734751.4 | 2.5 | ||
| Number of motivation-related individual barriers (continuous) | Mean (SE) | 0.321 | 0.02 | 0.238 | 0.01 | 0.26 | 0.01 | <.001 |
| 95% CI | [0.285, 0.356] | [0.238, 0.266] | [0.247, 0.273] | |||||
| Number of resource-related individual barriers (continuous) | Mean (SE) | 0.639 | 0.03 | 0.502 | 0.01 | 0.516 | 0.01 | <.001 |
| 95% CI | [0.588, 0.690] | [0.482, 0.521] | [0.498, 0.535] | |||||
3.2. Barriers to physical activity
Irrespective of location, the most reported barriers were lack of time (21.4% reporting) and lack of support to be physically active (22.7% reporting; Table 4). For urban residents, the most reported barriers were lack of support to be active (22%) and lack of time (21.8%). For rural residents, the most reported barriers were lack of facility access (28.7%) and lack of support to be active (26%). Seventy-one percent of rural residents reported at least one social or built environmental barrier compared with 44.5% of urban residents, while individual resource-related (50.8% urban; 47.1% rural) and individual motivation-related (26% urban; 21.4% rural) barriers were reported with similar frequency by location.
Table 4.
Population-weighted frequency of barriers reported by rural-urban location.
| Domain | Item | Urban (n=20290454) | Rural (n=4209008) | Total (n=24499462) | |
|---|---|---|---|---|---|
| Individual motivation-related barriers | Prefer to be active | no barrier | 17959591 (88.5%) | 3853494 (91.6%) | 21813085 (89.0%) |
| barrier | 2330863 (11.5%) | 355514 (8.4%) | 2686377 (11.0%) | ||
| Confidence to be active | no barrier | 18751193 (92.4%) | 3906477 (92.8%) | 22657670 (92.5%) | |
| barrier | 1539261 (7.6%) | 302531 (7.2%) | 1841792 (7.5%) | ||
| Enjoy activity | no barrier | 18877756 (93.0%) | 3967611 (94.2%) | 22845367 (93.2%) | |
| barrier | 1412698 (7.0%) | 241396 (5.7%) | 1654094 (6.8%) | ||
| Social and built environmental barriers | See people active in community | no barrier | 17497544 (86.2%) | 3520208 (83.6%) | 21017752 (85.8%) |
| barrier | 2792910 (13.8%) | 688800 (16.4%) | 3481710 (14.2%) | ||
| Receive support to be active | no barrier | 15833855 (78.0%) | 3114416 (74.0%) | 18948271 (77.3%) | |
| barrier | 4456599 (22.0%) | 1094592 (26.0%) | 5551191 (22.7%) | ||
| Access to free or low-cost facilities | no barrier | 18493058 (91.1%) | 3002813 (71.3%) | 21495871 (87.7%) | |
| barrier | 1797396 (8.9%) | 1206195 (28.7%) | 3003591 (12.3%) | ||
| Individual resource-related barriers | Has energy to be active | no barrier | 17785534 (87.7%) | 3735362 (88.7%) | 21520896 (87.8%) |
| barrier | 2504920 (12.3%) | 473646 (11.3%) | 2978566 (12.2%) | ||
| Has time to be active | no barrier | 15870781 (78.2%) | 3385728 (80.4%) | 19256509 (78.6%) | |
| barrier | 4419673 (21.8%) | 823279 (19.6%) | 5242952 (21.4%) | ||
| Can afford to be active | no barrier | 16911558 83.3%) | 3522204 (83.7%) | 20433762 (83.4%) | |
| barrier | 3378897 (16.7%) | 686804 (16.3%) | 4065701 (16.6%) | ||
3.3. Individual resource-related barriers
3.3.1. Any barrier
There was no effect of location in predicting the odds of reporting any individual resource-related variable either in the base model (p > .20) or after controlling for sociodemographic factors, OR=0.95, 95% CI [0.84, 1.07], p=.393. No further analyses were conducted on separate barrier items (Table 5).
Table 5.
Odds ratios for the effect of location on likelihood of reporting individual resource-related barriers (reference: urban).
| Any resource-related barriers | Can afford to be active | Has time to be active | Has energy to be active | |
|---|---|---|---|---|
| Basemodel | 0.93 [0.78, 0.97] | not run | not run | not run |
| Final model | 0.95 [0.84, 1.07] |
Note: although the CI for the base model doesn't include 1, the p-value of the regression slope estimate is > 0.20.
3.4. Individual motivation-related barriers
3.4.1. Any barrier
Rural residents had lower odds of reporting at least one motivation-related barrier in the base model (OR=0.78, 95% CI [0.69, 0.89], p=.0002) and in the optimally fitted model (OR=0.69, 95% CI [0.60,0.79], p < .0001; Table 6). After accounting for covariates, 30% of urban and 22.9% of rural residents reported at least one motivation-related variable.
Table 6.
Odds ratios for the effect of location on likelihood of reporting individual motivation-related barriers (reference: urban).
| Any motivation-related barriers | Prefer to be active | Confidence to be active | Enjoy physical activity | |
|---|---|---|---|---|
| Base model | 0.78 [0.69, 0.89] | 0.71 [0.60, 0.84] | 0.94 [0.80, 1.12] | 0.81 [0.68, 0.97] |
| Final model | 0.69 [0.60, 0.79] | 0.69 [0.58, 0.81] | <Secondary school: 0.62 [0.43, 0.91] | Income$0-29.9k: 0.48 [0.32, 0.71] |
| Secondary school: 0.59 [0.40, 0.85] | Income$30-59.9k: 1.14 [0.83, 1.57] | |||
| Post-secondary: 0.96 [0.74, 1.23] | Income$60-99.9k: 0.57 [0.38, 0.88] | |||
| Income$100-149.9k: 0.77 [0.51, 1.18] | ||||
| Income$150k+: 0.86 [0.50, 1.46] |
Note: The optimally fitted model for reporting any motivation-related barrier included the covariates age, BMI, income, perceived health, and sense of belonging to community. The optimally fitted model for preference to be active included the same covariates with the addition of sex. The optimally fitted model for confidence to be active included sex, age, BMI, income, perceived health, sense of belonging to community, and education. The optimally fitted model for enjoyment of physical activity included covariates sex, BMI, income, perceived health, and sense of belonging to community.
3.4.2. Preference to be active
Rural residents had lower odds of reporting barriers related to preference to be active compared with laying down (i.e., they were more likely to report a preference to be active)2 in the base model (OR=0.71, 95% CI [0.60, 0.84], p < .0001) and in the optimally fitted model (OR=0.69, 95% CI [0.58, 0.81], p < .0001). In the final model, 18.8% of urban and 13.8% of rural residents reported this barrier. No interactions with location were significant.
3.4.3. Enjoyment of physical activity
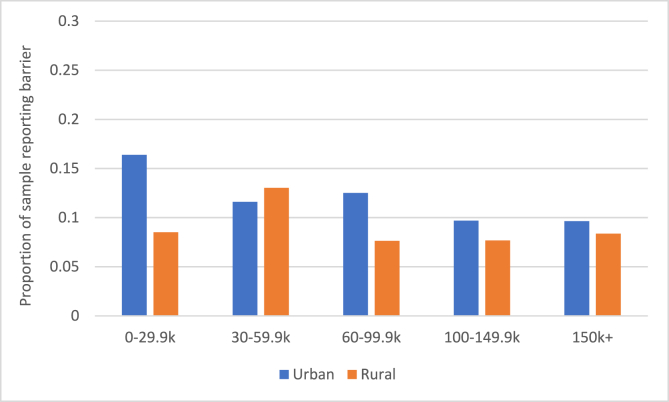
Rural residents showed lower odds of reporting enjoyment of physical activity as a barrier (i.e., they more commonly reported enjoying activity) in the base model (OR=0.81, 95% CI [0.68, 0.97], p=.023) and after controlling for sociodemographic factors as well as a significant location x income interaction (Fig. 1). The effect of location was significant for the lowest income group (OR=0.48, 95% CI [0.32, 0.71], p=.0003) and for the middle-income group (OR=0.58, 95% CI [0.38, 0.88], p=.010), but non-significant for all other groups (all ps > .20). Because income categories were derived from weighted cumulative frequencies to ensure roughly equal quintiles, this inconsistent pattern is unrelated to sample size across income categories.
Fig. 1.
Proportion of sample reporting barriers related to enjoyment of physical activity (income * location)—higher # reflects more people reporting.
3.4.4. Confidence to be active
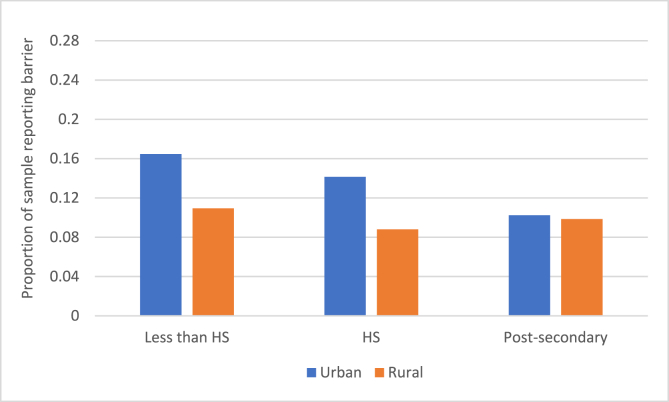
The base model revealed no significant effect of location in predicting barriers related to confidence to be active, OR=0.94, 95% CI [0.80, 1.12], p=.502. The effect of location became significant in the optimally fitted model (OR=0.59, 95% CI [0.40, 0.85], p=.005) with an identified education x location interaction (Fig. 2). For people with a post-secondary education, location did not predict barriers to confidence (p > .70), while for people reporting an education attainment at high school or less, rural residents had lower odds of reporting lack of confidence as a barrier (high school OR=0.59, 95% CI [0.40, 0.85], p=.005; less than high school OR=0.62, 95% CI [0.43, 0.91], p=.015).
Fig. 2.
Proportion of sample reporting barriers related to confidence to be active (education * location)—higher # reflects more people reporting barrier.
Note: HS, high school.
3.5. Social and built environmental barriers
3.5.1. Any barrier
Rural residents showed significantly higher odds of reporting at least one social or built environmental barrier compared to urban in the base model (OR=1.86, 95% CI [1.67, 2.07], p < .0001) and after accounting for covariates (OR=1.85, 95% CI [1.66, 2.07], p < .0001; Table 7). There were no significant interactions. In the optimally fitted model, approximately 57.8% of urban residents reported at least one environmental barrier compared with 71.8% of rural residents.
Table 7.
Odds ratios for the effect of location on likelihood of reporting social and built environmental barriers (reference: urban).
| Any environmental barriers | See people active | Access to facilities | Support to be active | |
|---|---|---|---|---|
| Base model | 1.86 [1.67, 2.07] | 1.22 [1.07, 1.41] | 4.13 [3.57, 4.79] | 1.25 [1.11, 1.40] |
| Final model | 1.84 [1.65, 2.06] | Income$0-29.9k: 0.89 [0.67, 1.19] | 4.15 [3.58, 4.83] | 1.17 [1.04, 1.32] |
| Income$30-59.9k: 1.11 [0.86, 1.43] | ||||
| Income$60-99.9k: 1.24 [0.94, 1.65] | ||||
| Income$100-149.9k: 1.09 [0.78, 1.50] | ||||
| Income$150k+: 2.06 [1.39, 3.04] |
Note: The optimally fitted model for reporting any social or built environmental barrier included covariates season of data collection, sex, age, income, perceived health, and sense of belonging to community. The optimally fitted model for seeing people active in community included covariates season of data collection, sex, income, and sense of belonging to community. The optimally fitted model for access to facilities included covariates age, income, perceived health, and sense of belonging to community. Finally, the optimally fitted model for receiving support to be active included covariates season of data collection, sex, age, income, perceived health and sense of belonging to community.
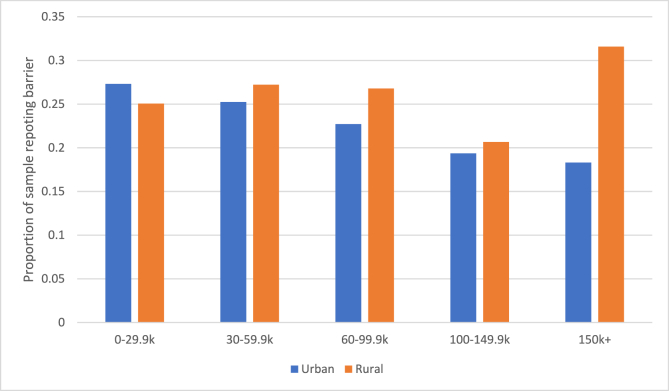
3.5.2. Seeing people active in community
In the base model, rural residents demonstrated higher odds of barriers related to seeing other people being active in their community (i.e., rural residents were less likely to report seeing other people being active in their community), OR=1.23, 95% CI [1.07, 1.41], p=.004. A significant location x income interaction was observed in the optimally fitted model (Fig. 3). Examining the effect of location across income categories revealed that this effect was non-significant (all ps > .10) for all income categories except the wealthiest, for which the effect of location was significant, OR=2.06, 95% CI [1.39, 3.05], p=.0003. Wealthy rural residents had higher odds of reporting this barrier, meaning they reported seeing people being active in their community less regularly compared to wealthy urban residents.
Fig. 3.
Proportion of sample reporting barriers related to seeing people active in community (income * location) – higher value = more people reporting.
3.5.3. Support to be active
Rural residents showed higher odds of reporting barriers to receiving support to be physically active compared to urban in the base (OR=1.25, 95% CI [1.11, 1.40], p=.0002) and optimally fitted model (OR=1.17, 95% CI [1.04, 1.32], p=.010). Per the final model, 39.6% of urban and 43.5% of rural residents reported this barrier. No interactions with location were significant.
3.5.4. Access to facilities
In the base model, the effect of location was significant such that rural residents showed higher odds of reporting barriers related to the availability of free or low-cost facilities compared to urban, OR=4.13, 95% CI [3.57, 4.79], p < .0001. The effect of location remained in the optimally fitted model (OR=4.15, 95% CI [3.58, 4.83], p < .0001). In this model 20.2% of urban and 51.3% of rural residents reported barriers to facility access. There were no interactions between location and any sociodemographic factor.
4. Discussion
The aim of this study was to compare patterns in barriers to physical activity between urban and rural-dwelling adults while considering salient sociodemographic factors. Findings demonstrate that rural residents were more likely to report social and built environmental barriers to physical activity and less likely to report individual-motivation related barriers, though some of these outcomes were qualified by interactions with sociodemographic characteristics. There was no difference in the odds of reporting individual-resource related barriers based on rural-urban location. Income and education moderated the relationship between motivation-related barriers and location and there were no interactions for rural-urban location and social and built environmental barriers (i.e., rural residents of all sociodemographic groups reported similar environmental barriers to activity).
4.1. Individual motivation and resource barriers
Our findings identify urban residents as more likely to report motivation-related barriers and a lower preference for physical activity as a barrier. However, this overall effect was qualified by an interaction between income and location such that lower preference for physical activity was only observed for urban residents within the lowest and middle-income categories; all other income categories showed no significant effect of location in relation to enjoyment of physical activity. Similarly, rural residents reported lower odds of reporting barriers related to confidence in abilities to be active compared to urban residents, but this difference was only observed for participants without post-secondary education. A positive association between socioeconomic status (as measured by education and/or income) and physical activity has been commonly reported in population-based studies (Droomers et al., 2001; Hankonen et al., 2017). Our findings suggest a more complex relationship between individual barriers to physical activity and location contingent on socioeconomic status. This complex, possibly non-linear relationship is consistent with other work, identifying the importance of considering the interaction of socioeconomic status by location and access to different types of physical activity (Eime et al., 2015).
Individual resource-related barriers (including personal energy, time, and cost) were reported by both urban and rural residents, however the odds of reporting these barriers did not differ by location. Geographical discrepancies in physical activity behavior appear to be driven by factors beyond individual-level resources and are heavily shaped by the built and social environment warranting attention for the entire population.
4.2. Social and built environmental barriers
Rural-dwelling adults are more likely than urban adults to report social and built environmental barriers to physical activity. Over 70% of rural residents reported at least one environmental barrier and, after adjusting for sociodemographic factors, over 50% reported not having access to free or low-cost facilities in their neighbourhood. There were no interactions between sociodemographic factors and location in predicting barriers to facility access, suggesting facility access is an issue for rural residents independently of self-identified sex, age, income, education, BMI, perceived health, sense of belonging and season of data collection.
Access to facilities is one of the most consistently reported environmental correlates of physical activity behavior across different populations (Bauman et al., 2012; Choi et al., 2017; Humpel et al., 2002; Parks et al., 2003; Wendel-Vos et al., 2007). A positive dose-response relationship has been identified between the number of places to be active and likelihood of meeting physical activity guidelines (Parks et al., 2003). The significantly higher odds of reporting this barrier among rural residents may suggest that lack of facilities is a key driver of physical activity inequities, although additional work is needed to confirm how these barriers impact physical activity participation based on rural-urban location.
Previous work has suggested access to spaces to be active in rural communities is dependent on socioeconomic position, noting access to indoor facilities for exercise and access to walking trails was higher among women with more education and higher income (Brownson et al., 2000). In our study, reported barriers to facility access were significantly associated with income; however, there were no interactions with any factor by location. The lack of a location-income interaction suggests income is similarly associated with facility access for rural and urban residents, while rural residents face further barriers to facility access unique to their geographic location.
Rural residents reported having lower social support to be active compared to urban residents, independently of all sociodemographic covariates. Social environmental barriers to physical activity are commonly reported among rural residents (Parks et al., 2003). The lack of social support may be particularly important for rural residents who commonly report engagement in physical activity to connect with their community and identify health and physical activity in relation to their social networks (McGannon et al., 2014; Pelletier, Ward, et al., 2021; Seguin et al., 2014). Future work is needed to confirm whether social support barriers relate to engagement in physical activity differently for rural and urban residents. As supportive social environments are an important facilitator of physical activity (McNeill et al., 2006), developing active living strategies that foster social support is a potential area of focus for physical activity promotion in rural communities.
Physical activity promotion initiatives and messaging focusing on individual factors, such as motivation to being active, benefits of being active over being sedentary (e.g., move more, reduce sedentary behavior) (Faught et al., 2020), may not be effective for rural populations, as these factors present less of a perceived barrier to activity compared to environmental factors. Instead, efforts should focus on the creation of safe, accessible spaces for activity, promote the use of outdoor recreation spaces, and provide strategies to support others (e.g., family, friends, neighbours) to be active. Our findings support the need for unique approaches to physical activity promotion with context-specific messaging for rural and urban communities (Milton et al., 2020), and collaborative action with policy makers and community planners to encourage the creation of built environments supportive of physical activity (Nykiforuk et al., 2018; Sallis et al., 1998).
For this analysis, we dichotomized rural and urban based on Statistics Canada definitions. Although the CCHS data does provide location classifications based on metropolitan influenced zone and a four-level indicator of population center size, these different definitions of rurality did not considerably alter observed patterns of reporting barriers in our analysis. Future work should continue to explore degree of rurality and remoteness in considering location-based differences in physical activity.
4.3. Limitations
The excluded sample differed from the included sample on several sociodemographic factors and reported barriers. Excluded participants were more likely to be female, have lower educational attainment and income, not meet recommended activity guidelines, and have more reported barriers to activity. Our findings thus reflect a group of people who are more physically active and have a higher socioeconomic status than the general Canadian population. We cannot make assumptions about rural-urban differences in barriers to physical activity for the excluded group. This is partially a limitation of the CCHS dataset related to biases in survey completion. The list of barriers used in this analysis were pre-defined and thus do not necessarily reflect all potential barriers experienced or a comprehensive assessment of factors impacting activity. Only one item was used to assess built environment characteristics (access to facilities), and a more robust analysis of barriers to physical activity should include a detailed exploration of built and natural environmental characteristics in rural areas. Additionally, our central theoretical focus was rural-urban location and we did not explore nuanced or interacting relationships between other sociodemographic factors (e.g., income x sex) and reported barriers to physical activity. These remain important questions for future study.
5. Conclusion
In a representative Canadian sample, people living in rural communities of any sociodemographic background are more likely to report social and built environmental barriers to physical activity than those living in urban centres. Both urban and rural residents reported time and cost as barriers to physical activity, however rural residents report additional environmental barriers including lack of facility access and inadequate social support. Future work should explore how these perceived barriers relate to physical activity behavior in both urban and rural communities to advocate for physical activity policy implementation, direct population health interventions, and support the contextually relevant messaging of physical activity guidelines.
Author credit statement
Chelsea Pelletier: Conceptualization, Methodology, Writing – original draft preparation, Writing – review & editing, Project administration, Funding acquisition. Nicole White: Methodology, Data curation, Formal analysis, Writing - original draft preparation, Writing – review & editing, Visualization. Annie Duchesne: Conceptualization, Methodology, Writing – review & editing, Funding acquisition. Larine Sluggett: Conceptualization, Methodology, Writing – review & editing.
Ethical statement
Access to data used in this manuscript is regulated and vetted by Statistics Canada to protect participant confidentiality. As such, Research Ethics Board approval is not required (per Tri-Council Policy Statement Article 2.2 and 2.4).
Funding
This study was funded by a Research Data Centre award from the University of Northern British Columbia. The funding body had no role in the design of the study, data analysis, interpretation of data, or in preparation of this manuscript.
Declaration of competing interest
None.
Footnotes
Note that we employ the term “predictor” strictly with respect to its statistical usage within the scope of regression model outcomes for our cross-sectional analysis, from which directionality of relationships between variables and/or their causal relations to one another cannot be assessed. This usage is distinguishable from the usage of the term “predictor” to reflect concepts such as risk or protective factors, or other causal relations. We do not advance any causal interpretations in the present analysis.
Note that we have retained the wording of survey items provided by Statistics Canada to facilitate replicability of analysis.
References
- Bauman A., Reis R.S., Sallis J.F., Wells J.C., Loos R.J.F., Martin B.W., &the Lancet Physical Activity Series Working Group Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- Brownson R.C., Housemann R.A., Brown D.R., Jackson-Thompson J., King A.C., Malone B.R., et al. Promoting physical activity in rural communities: Walking trail access, use, and effects. American Journal of Preventive Medicine. 2000;18(3):235–241. doi: 10.1016/s0749-3797(99)00165-8. [DOI] [PubMed] [Google Scholar]
- Choi J., Lee M., Lee J.K., Kang D., Choi J.Y. Correlates associated with participation in physical activity among adults: A systematic review of reviews and update. BMC Public Health. 2017;17:356. doi: 10.1186/s12889-017-4255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke A.E., Janssen I. A compositional analysis of time spent in sleep, sedentary behaviour and physical activity with all-cause mortality risk. International Journal of Behavioral Nutrition and Physical Activity. 2021;18:25. doi: 10.1186/s12966-021-01092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Droomers M., Schrijvers C.T.M., Mackenbach J.P. Educational level and decreases in leisure time physical activity: Predictors from the longitudinal GLOBE study. Journal of Epidemiology & Community Health. 2001;55:562–568. doi: 10.1136/jech.55.8.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikemo T.A., Hoffmann R., Kulik M.C., Kulhánová I., Toch-Marquardt M., et al. How can inequalities in mortality be reduced? A quantitative analysis of 6 risk factors in 21 European populations. PLoS One. 2014;9(11) doi: 10.1371/journal.pone.0110952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eime R.M., Charity M.J., Harvey J.T., et al. Participation in sport and physical activity: Associations with socio-economic status and geographical remoteness. BMC Public Health. 2015;15:434. doi: 10.1186/s12889-015-1796-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekelund U., Tarp J., Steene-Johnannssen J., Hansen B.H., Jefferis B., Fagerland M.W., et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonized meta-analysis. BMJ. 2019;366 doi: 10.1136/bmj.14570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyler A.A. Personal, social, and environmental correlates of physical activity in rural Midwestern white women. American Journal of Preventive Medicine. 2003;25:86–92. doi: 10.1016/s0749-3797(03)00169-7. [DOI] [PubMed] [Google Scholar]
- Fan J.X., Wen M., Kowaleski-Jones L. Rural-urban differences in objective and subjective measures of physical activity: Findings from the national health and nutrition examination survey (NHANES) 2003-2006. Preventing Chronic Disease. 2014;11 doi: 10.5888/pcd11.140189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faught E., Walters A.J., Latimer-Cheung A.E., Faulkner G., Jones R., Duggan M., et al. Optimal messaging of the Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years and older. Applied Physiology Nutrition and Metabolism. 2020;45(10):S125–S150. doi: 10.1139/apnm-2020-0494. Suppl. 2. [DOI] [PubMed] [Google Scholar]
- Forbes C.C., Yu Z.M., Cui Y., DeClercq V., Grandy S.A., Parker L., et al. Rural‐urban disparities in total physical activity, body composition, and related health indicators: An atlantic PATH study. The Journal of Rural Health. 2020;36(1):111–119. doi: 10.1111/jrh.12363. [DOI] [PubMed] [Google Scholar]
- Gorber S.C., Tremblay M., Moher D., Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obesity Reviews. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- Hankonen N., Heino M.T.J., Kujala E., et al. What explains the socioeconomic status gap in activity? Educational differences in determinants of physical activity and screentime. BMC Public Health. 2017;17:144. doi: 10.1186/s12889-016-3880-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath G.W., Brownson R.C., Kruger J., Miles R., Powell K.E., Ramsey L.T., et al. The effectiveness of urban design and land use and transport policies and practices to increase physical activity: A systematic review. Journal of Physical Activity and Health. 2006;3:S55. doi: 10.1123/jpah.3.s1.s55. [DOI] [PubMed] [Google Scholar]
- Heinzen E., Sinnwell J., Atkinson E., Gunderson T., Dougherty G. 2019. arsenal: An arsenal of 'R' functions for large-scale statistical summaries. R package version 3.3.0.https://CRAN.R-project.org/package=arsenal 2019. [Google Scholar]
- Humpel N., Owen N., Leslie E. Environmental factors associated with adults participation in physical activity: A review. American Journal of Preventive Medicine. 2002;22:58–69. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leipert B.D., George J.A. Determinants of rural women's health: A qualitative study in southwest ontario. The Journal of Rural Health. 2008;24(2):210–218. doi: 10.1111/j.1748-0361.2008.00160.x. [DOI] [PubMed] [Google Scholar]
- Long A.S., Hanlon A.L., Pellegrin K.L. Socioeconomic variables explain rural disparities in US mortality rates: Implications for rural health research and policy. SSM Population Health. 2020;6:72–74. doi: 10.1016/j.ssmph.2018.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T. 2019. survey: analysis of complex survey samples. R package version 3.36. [Google Scholar]
- Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., Commission on Social Determinants of Health Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Marquez D.X., Aguiñaga S., Vásquez P.M., Conroy D.E., Erickson K.I., Hillman C., et al. A systematic review of physical activity and quality of life and well-being. Translation Behaviour Medicine. 2020;10(5):1098–1109. doi: 10.1093/tbm/ibz198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S.L., Kirkner G.J., Mayo K., Matthews C.E., Durstine J.L., Hebert J.R. Urban, rural, and regional variations in physical activity. The Journal of Rural Health. 2005;21(3):239–244. doi: 10.1111/j.1748-0361.2005.tb00089.x. [DOI] [PubMed] [Google Scholar]
- McCormack G.R., Shiell A. In search of causality: A systematic review of the relationship between the built environment and physical activity among adults. International Journal of Behavioral Nutrition and Physical Activity. 2011;8(1):125. doi: 10.1186/1479-5868-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGannon K.R., Busanich R., Witcher C.S., Schinke R.J. A social ecological exploration of physical activity influences among rural men and women across life stages. Quality Result Sport Exercise Health. 2014;6(4):517–536. [Google Scholar]
- McNeill L.H., Kreuter M.W., Subramanian S.V. Social environment and physical activity: A review of concepts and evidence. Social Science & Medicine. 2006;63:1011–1022. doi: 10.1016/j.socscimed.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Milton K., Bauman A.E., Faulkner G., Hastings G., Bellew W., Williamson C., et al. Maximising the impact of global and national physical activity guidelines: The critical role of communication strategies. British Journal of Sexual Medicine. 2020;54(24):1463–1467. doi: 10.1136/bjsports-2020-102324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nykiforuk C.I.J., Atkey K., Brown S., Caldwell W., Galloway T., Gilliland J., et al. Promotion of physical activity in rural, remote and northern settings: A Canadian call to action. Health Promot Chronic Disease Prevention Cancer. 2018;38(11):419–435. doi: 10.24095/hpcdp.38.11.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan S.Y., Cameron C., DesMeules M., et al. Individual, social, environmental, and physical environmental correlates with physical activity among Canadians: A cross-sectional study. BMC Public Health. 2009;9:21. doi: 10.1186/1471-2458-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks S.E., Housemann R.A., Brownson R.C. Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. Journal of Epidemiology & Community Health. 2003;57:29–35. doi: 10.1136/jech.57.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier C.A., White N., Duchesne A., Sluggett L. Likelihood of meeting physical activity guidelines in rural and urban adults: cross-sectional analysis of the Canadian Community Health Survey. Canadian Journal of Public Health. 2021;112:748–757. doi: 10.17269/s41997-021-00507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier C.A., Ward K., Pousette A., Fox G. Meaning and experiences of physical activity in rural and northern communities. Qualitative Research in Sport, Exercise and Health. 2021;13:690–703. doi: 10.1080/2159676X.2020.1761434. [DOI] [Google Scholar]
- Plotnikoff R.C., Mayhew A., Birkett N., Loucaides C.A., Fodor G. Age, gender, and urban-rural differences in the correlates of physical activity. Preventive Medicine. 2004;39(6):1115–1125. doi: 10.1016/j.ypmed.2004.04.024. [DOI] [PubMed] [Google Scholar]
- Pong R.W., Desmeules M., Lagacé C. Rural-urban disparities in health: How does Canada fare and how does Canada compare with Australia? Australian Journal of Rural Health. 2009;17(1):58–64. doi: 10.1111/j.1440-1584.2008.01039.x. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Bauman A., Pratt M. Environmental and policy interventions to promote physical activity. American Journal of Preventive Medicine. 1998;15:379–397. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Cervero R.B., Ascher W., Henderson K.A., Kraft M.K., Kerr J. An ecological approach to creating active living communities. Annual Review of Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Hovell M.F., Hofstetter C.R. Predictors of adoption and maintenance of vigorous physical activity in men and women. Preventive Medicine. 1992;21:237–251. doi: 10.1016/0091-7435(92)90022-a. [DOI] [PubMed] [Google Scholar]
- Seguin R., Connor L., Nelson M., LaCroix A., Eldridge G. Understanding barriers and facilitators to healthy eating and active living in rural communities. Journal Nutrition Metabolism. 2014 doi: 10.1155/2014/146502. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G.K. Area deprivation and widening inequalities in US mortality, 1969–1998. American Journal of Public Health. 2003;93:1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrisi T.B., Bittel K.M., West A.B., et al. Seasons, weather, and device-measured movement behaviors: A scoping review from 2006 to 2020. International Journal of Behavioral Nutrition and Physical Activity. 2021;18:24. doi: 10.1186/s12966-021-01091-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendel-Vos W., Droomers M., Kremers S., Brug J., van Lenthe F. Potential environmental determinants of physical activity in adults: A systematic review. Obesity Reviews. 2007;8:425–440. doi: 10.1111/j.1467-789X.2007.00370.x. [DOI] [PubMed] [Google Scholar]
- WHO European Commission. physical activity promotion in socially disadvantaged groups: Principles for action. Final Report. 2013 [Google Scholar]
- Wilcox S., Castro C., King A.C., Housemann R., Brownson R.C. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. Journal of Epidemiology & Community Health. 2000;54:667–672. doi: 10.1136/jech.54.9.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witcher C.S., Holt N.L., Spence J.C., Cousins S.O. A case study of physical activity among older adults in rural Newfoundland, Canada. Journal of Aging and Physical Activity. 2007;15(2):166–183. doi: 10.1123/japa.15.2.166. [DOI] [PubMed] [Google Scholar]
- Yip C., Sarma S., Wilk P. The association between social cohesion and physical activity in Canada: A multilevel analysis. SSM-Population Health. 2016;2:718–723. doi: 10.1016/j.ssmph.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarifa D., Seward B., Milian R.P. Location, location, location: Examining the rural-urban skills gap in Canada. Journal of Rural Studies. 2019;72:252–263. [Google Scholar]
- Zhang Z. Residuals and regression diagnostics: Focusing on logistic regression. Annals of Translational Medicine. 2016;4(10):195–202. doi: 10.21037/atm.2016.03.36. [DOI] [PMC free article] [PubMed] [Google Scholar]