Abstract
Background. Veterans’ access to Veterans Affairs (VA)-purchased community care expanded due to large increases in funding provided in the 2014 Veterans Choice Act. Objectives. To compare costs between VA-delivered care and VA payments for purchased care for two commonly performed surgeries: total knee arthroplasties (TKAs) and cataract surgeries. Research Design. Descriptive statistics and regressions examining costs in VA-delivered and VA-purchased care (fiscal year [FY] 2018 [October 2017 to September 2018]). Subjects. A total of 13,718 TKAs, of which 6,293 (46%) were performed in VA. A total of 91,659 cataract surgeries, of which 65,799 (72%) were performed in VA. Measures. Costs of VA-delivered care based on activity-based cost estimates; costs of VA-purchased care based on approved and paid claims. Results. Ninety-eight percent of VA-delivered TKAs occurred in inpatient hospitals, with an average cost of $28,969 (SD $10,778). The majority (86%) of VA-purchased TKAs were also performed at inpatient hospitals, with an average payment of $13,339 (SD $23,698). VA-delivered cataract surgeries were performed at hospitals as outpatient procedures, with an average cost of $4,301 (SD $2,835). VA-purchased cataract surgeries performed at hospitals averaged $1,585 (SD $629); those performed at ambulatory surgical centers cost an average of $1,346 (SD $463). We also found significantly higher Nosos risk scores for patients who used VA-delivered versus VA-purchased care. Conclusions. Costs of VA-delivered care were higher than payments for VA-purchased care, but this partly reflects legislative caps limiting VA payments to community providers to Medicare amounts. Higher patient risk scores in the VA could indicate that community providers are reluctant to accept high-risk patients because of Medicare reimbursements, or that VA providers prefer to keep the more complex patients in VA.
Keywords: costs, dual system use, out of system utilization, payments
Introduction
In 2014, Congress allocated an additional $15 billion in funding for the US Department of Veterans Affairs (VA) to address concerns about timely access to health care. Five billion dollars were allocated to expand VA clinics and reduce wait times, with the remainder ($10 billion) designated to expand VA’s ability to purchase care in the community through the Veterans Choice Program. Congress enacted the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act in 2018, with a continued emphasis on purchasing community care.
VA’s increasing emphasis on purchasing care has raised questions about the cost and quality of VA-purchased care, especially in comparison to VA-delivered care.1–3 Cost comparisons are challenging for a number of reasons. First, VA has very different institutional and regulatory structures than private sector hospitals. For instance, VA facilities receive capitated payments and hire physicians as staff, creating a set of incentives that could lead to less intensive treatment. Alternatively, VA-purchased care is paid on a fee-for-service basis, which creates incentives for providing more resource intensive treatment. 4
Second, over the past 5 years, VA has transitioned to a new database for managing community care payments. While VA’s traditional Fee Basis and Fee Basis Claims System datasets have been well-documented and widely used in past research,5–8 VA now aggregates VA-purchased claims into the Program Integrity Tool (PIT), which was originally established for monitoring fraud, waste, and abuse. Researchers have less experience using the PIT data and little knowledge of what variables are most accurate for use in analyses.
Recognizing these challenges, we sought to develop methods for identifying the payments for VA-purchased care. These payments reflect the cost of purchasing care for the VA, not the cost of providing the purchased care. We then compared VA-purchased care to VA-delivered care, which represents the total costs of producing the care, including labor and capital. To develop these methods, we selected two common elective surgical procedures: total knee arthroplasty (TKA) and cataract surgery. In these examples, we take into account patient risk given that differences in VA-purchased and VA-delivered costs could create financial incentives for risk selection and possible gaming.
Methods
Study Samples
We identified veterans who had TKAs using procedure codes in fiscal year (FY) 2018 (October 1, 2017, to September 30, 2018) from VA’s Corporate Data Warehouse (CDW). TKA is a common surgical procedure in the United States with more than 715,000 conducted in 2018, 9 and approximately 7,000 a year in VA. 10 TKA procedures were traditionally handled as inpatient procedures, but starting in 2018, the Centers for Medicare and Medicaid Services (CMS) removed TKAs from the Inpatient-Only list, enabling reimbursement for TKAs performed in a hospital outpatient department. 11 CMS changed its payment policies to cover TKAs in ambulatory surgical centers (ASCs) in 2020. Following CMS methodology, we identified TKAs using Current Procedural Terminology (CPT) code 27447 and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) procedure codes (0SRC069, 0SRC06A, 0SRC06Z, 0SRC0J9, 0SRC0JA, 0SRC0JZ, 0SRD069, 0SRD06A, 0SRD06Z, 0SRD0J9, 0SRD0JA, 0SRD0JZ). We also extracted records with a Diagnosis Related Group (DRG) of 470; however, because DRG 470 includes both hip and knee procedures, we used the specific procedure codes (noted above) to identify knee procedures.
Cataract surgery is the most common ambulatory surgical procedure in the United States, with more than a million performed annually. 12 Cataract surgeries are also common in VA. In FY2015, the VA provided 58,050 procedures and purchased another 25,825. 13 Cataract surgeries are commonly performed in hospital outpatient departments and ASCs. According to the Medicare Payment Advisory Commission, cataracts were the most commonly reimbursed ASC procedure, accounting for 18.8% of all Medicare ASC payments in 2018. 14 Consequently, cataract surgeries have been used to gauge equitable access by tracking wait times, and provider quality by tracking complications in international comparisons. 15 For cataracts, we also followed CMS methodology to identify complex (CPT code 66982) and routine (66984) surgeries, respectively (including the eye modifiers). 16
For VA-purchased care, we included claims that were listed as current and accepted claims that were paid using Choice Act funds. These restrictions were recommended by the VA Office of Community Care to remove unpaid or rejected claims. 17 As required by the Choice and MISSION Acts, VA payments cannot exceed Medicare payments, with a few exceptions. For some procedures, such as TKAs, Medicare imposes additional payment limits on bilateral TKAs. Thus, for TKAs, we restricted our sample to the first TKA present in the data if multiple procedure codes suggested that the patient had a bilateral procedure. For cataracts, we included the most expensive cataract surgery if more than one was performed on the same day. For both procedures, we focus on the cost of the surgery along with associated procedures for the outpatient service or inpatient stay. Estimating costs over time, which would include complications or readmissions over a 30- or 90-day period, is outside the scope of this article.
VA-Purchased Care
We obtained claims for VA-purchased care from the PIT database residing in the CDW. Since institutions and providers submit separate bills, the data are structured as claim line items with separate tables labeled as “institutional payments” and “professional fees.” Calculating the total payments for a surgical visit requires merging data across all billing entities (professional and institutional) as well as capturing claims for all related procedures. Institutional payments are based on CPT codes for ambulatory care and DRGs for inpatient care, while all professional fees are based only on CPT codes. Since FY2016, the PIT data include both CPT and ICD-10-CM procedure codes, though the CPT codes are more commonly used given their link with payments.
We extracted all PIT claims for cataract surgeries and TKAs using the codes listed above. We used the Place of Service variable in the PIT data to identify where the cataract surgery was performed: hospital outpatient department, ASC, or outpatient clinic. We used the Place of Service and Bill Type Code variables to distinguish between inpatient and outpatient care.
PIT data are organized as claim line numbers with payments for each CPT or DRG code. Extracting claim lines using specific procedure codes will overlook concurrent procedures necessary for performing the procedure of interest. For example, extracting cataract claim lines using a CPT code specific to cataract surgery will miss other procedures, such as anesthesia, that were conducted as part of the cataract procedure. These concurrent codes are necessary when estimating total payments for a procedure. To capture related services, we used the PIT Authorization Key to identify other procedures that shared the same authorization as the cataract surgery or knee arthroplasty. This method did not always generate related claim lines accurately. For example, we found colonoscopy CPT codes that shared the same authorization key with the cataract surgery. To filter out unrelated procedures which would have inflated costs, we created a table of “related CPT codes,” which was then reviewed by a clinician familiar with the services related to each procedure (i.e., cataract surgery and TKA). This table enabled us to filter out community care procedures that shared the same authorization key but were not related to the procedure.
Miscoding and missing data can be problematic when analyzing costs from claims data. For cataracts, CPT modifiers are used to identify which eye had the cataract, but they can also be used to denote a preoperative or postoperative visit, which often have an average cost under $200. In our primary cost analysis, we excluded 1,266 records that had a CPT modifier for preoperative or postoperative care. We then tested two other methods with the cataract data. In the first one, we used a strict criterion and excluded any record that was missing an eye-side modifier. In the second method, we excluded cataract claims where the payment was less than $200 to eliminate any potential pre- or postoperative care. We analyzed average VA payments for the samples generated by each of these algorithms.
VA-purchased care claims exclude the cost of VA’s Office of Community Care (i.e., overhead) and the cost of fees paid to third-party administrators who develop and manage the network of community providers who are willing to treat a veteran. We developed methods to estimate these costs. The VA Financial Management System tracks the Office of Community Care expenditures by facility using VA Cost Centers #s 8661-8669, as does the Managerial Cost Accounting Office using their Account Level Budget Cost Center (ALBCC) report (Account 2500300). With assistance from the VA Managerial Cost Accounting Office, we tabulated costs for community care in FY2018. The Office of Community Care also maintains internal documentation on third-party administrator fees by FY.
Total VA spending on VA-purchased care was $14.86 billion in FY2018 and the cost of operating the Office of Community Care was $355.78 million. Thus, the cost of operating the Office of Community Care adds 2.4% to each paid claim in FY2018. Additionally, third-party administrator fees are not included in the PIT claim payments. In FY2018, the total expenditures for third-party administrator fees were $379.15 million. As a proportion of spending on community care, this adds to 2.55%. In total, the Office of Community Care and the third-party administrator fees add $4.95 per $100 dollars of community care claims in FY2018. We then added these costs into the data for our analyses.
VA-Delivered Care
For procedures performed in the VA, we identified patients in the CDW and then linked these patients by scrambled social security number to the VA Managerial Cost Accounting (MCA) System, an activity-based cost accounting system that has provided precise cost estimates for over two decades.18,19 The MCA data estimate the VA’s cost to produce care based on activities specific to the hospital or clinic where the patient received care. MCA costs include all services associated with the surgery (e.g., anesthesia). We used the MCA outpatient dataset to obtain outpatient costs, and the treating specialty dataset for inpatient care. The VA Health Economics Resource Center provides guidebooks for merging the MCA data to other tables in the CDW. 20
In FY2018, VA performed all cataract surgeries on an outpatient basis; thus, the cost for the cataract surgery represents the total cost of the cataract, plus the related services, provided in the ophthalmology clinic on that day. The VA cost of the TKA reflects the medical and surgical costs of providing care from time of admission through discharge. To make the VA-delivered and VA-purchased amounts as comparable as possible, we limited VA-delivered costs to medical and surgical treating specialties only, thus excluding any transfers to skilled nursing care. As an integrated provider, veterans living in institutional settings can get a TKA; we included these cases but only analyzed costs from their medical/surgical care. In the PIT data, we also focused on medical/surgical care and excluded any skilled nursing care captured on claims using the Patient Discharge Status and Place of Service codes. The MCA data include variable and fixed cost subtotals; in this analysis, we used total costs, which reflect the variable (e.g., labor) and fixed (e.g., space) costs. The MCA fully enumerates all costs, with the exception of capital financing, which is borne by the US Department of the Treasury. MCA data have been widely used in health services research and documented elsewhere.21–23
Covariates
We linked the PIT data to patient sociodemographic and clinical information located in the CDW. We extracted age and gender for all patients. We also extracted their Nosos concurrent FY2018 risk score. Nosos is a VA risk score that predicts total VA costs using CMS’s Hierarchical Condition Category risk score with additional VA-specific information, including the PsyCMS mental health conditions and VA medication use.24,25 The Nosos score also includes adjustments for other demographic information, such as age, gender, and the veteran’s VA priority group (an enrollment hierarchy based on service connection, income status, and other factors), as represented in the CDW. 24 The Nosos score is calibrated to 1; a value of 1 represents a veteran whose VA costs in the year is the average for all VA users. Scores above 1 have higher than average expected costs, and scores below 1 have lower than expected average costs. In FY2018, the Nosos 25th percentile was .27, the 75th percentile was .96, and the maximum was 44.7. The VA Health Economic Resource Center’s website and technical reports describe the Nosos risk score and updates to the risk score over time. 26
Analysis
VA costs and VA payments represented FY2018 dollars. We compared average total VA costs to the average total VA payments made to community providers. We tabulated averages by type of community provider: ASCs, hospital outpatient departments, and clinics, with P values based on analysis of variance. We then regressed costs on age, gender, and the Nosos risk score using ordinary least squares (OLS). For the TKA analysis, we also included the location of care. The OLS results were similar to those from a general linear model (GLM) with gamma distribution and a log link, so we present the OLS results for ease of interpretation. People can have more than one cataract or TKA, so we adjusted the standard errors for clustering within person.
Results
Sample Characteristics
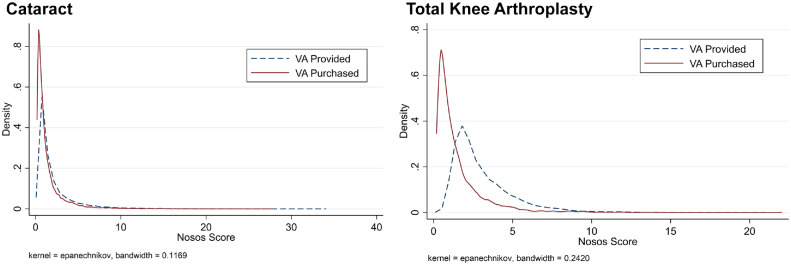
The descriptive characteristics of the patients who received TKA and cataract surgery are presented in Table 1. The average age of TKA patients was approximately 66.6 years old for veterans who received VA-delivered care vs. 65.7 years old for veterans using VA-purchased care. Male veterans comprised 92% of all TKA patients in the sample. The Nosos risk score was significantly higher for veterans who received VA delivered care (mean 3.04) than for veterans who received VA-delivered care (mean 1.5). Because Nosos relies predominantly on diagnostic and pharmacy data, 24 a higher Nosos risk score indicates that veterans getting care at VA had more expensive health conditions and used more expensive medications than those receiving care in the community. The distribution of Nosos scores for cataract and total knee arthroplasty procedures is shown in Figure 1.
Table 1.
Sample Characteristics for VA-Delivered and VA-Purchased Knee Arthroplasties and Cataract Surgeries in FY2018
| VA-Delivered Care | VA-Purchased Care | P Value | |||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | ||
| TKA | |||||||
| Age | 6,293 | 66.6 | 8.2 | 7,424 | 65.7 | 8.9 | <0.001 |
| Male (%) | 6,293 | 92% | 7,425 | 92% | 0.67 | ||
| Nosos score | 6,293 | 3.04 | 1.91 | 7,357 | 1.50 | 1.59 | <0.001 |
| Cataracts | |||||||
| Age | 65,799 | 72.1 | 7.9 | 25,855 | 72.0 | 7.7 | 0.029 |
| Male (%) | 65,799 | 96% | 25,860 | 89% | <0.001 | ||
| Nosos score | 65,799 | 1.90 | 2.30 | 25,342 | 1.44 | 1.87 | <0.001 |
SD, standard deviation; TKA, total knee arthroplasty; VA, Veterans Health Administration.
Figure 1.
Distribution of the Nosos score for cataracts and total knee arthroplasty (FY2018).
Among the cataract sample, the average age for patients with a cataract surgery was 72. Among veterans who received a cataract surgery, men were more likely to receive it at the VA (96%) than women (86%). The risk profiles, as measured by the Nosos score, indicated that sicker patients received cataract surgery in the VA (average score 1.90) compared to the community (average score 1.44).
TKA Costs
On average, VA-delivered inpatient TKAs cost $28,969 (SD $10,778). The average length of stay was 3.7 (SD 2.0) in the VA. The average cost of a VA-delivered outpatient TKA was $19,127 (SD $7,127). Table 2 also shows the median, 5%, and 95% values for comparison.
Table 2.
VA-Delivered Costs and VA-Purchased Care Payments for Total Knee Arthroplasties and Cataract Surgeries in FY2018
| n | Mean | Median | SD | 5% | 95% | |
|---|---|---|---|---|---|---|
| TKAs | ||||||
| VA-provided care | ||||||
| Inpatient hospital | 6,179 | 28,969 | 27,032 | 10,778 | 17,361 | 46,747 |
| Outpatient hospital a | 114 | 19,127 | 19,754 | 7,127 | 10,806 | 27,080 |
| VA-purchased care | ||||||
| Inpatient hospital | 6,337 | 13,339 | 14,552 | 23,698 | 1,411 | 23,832 |
| ASC | 31 | 16,561 | 10,744 | 32,935 | 1,185 | 80,149 |
| Outpatient hospital | 1,017 | 9,348 | 9,974 | 8,577 | 1,394 | 21,802 |
| Cataract surgeries | ||||||
| VA-provided care | ||||||
| Outpatient hospital | 65,799 | 4,301 | 3,869 | 2,835 | 1,589 | 8,188 |
| VA-purchased care | ||||||
| ASC | 19,480 | 1,346 | 1,540 | 463 | 578 | 1,823 |
| Outpatient hospital | 5,959 | 1,585 | 1,760 | 629 | 577 | 2,384 |
| Office | 341 | 876 | 673 | 891 | 110 | 1,820 |
| Other | 80 | 824 | 677 | 373 | 321 | 1,662 |
ASC, ambulatory surgical center; SD, standard deviation; TKA, total knee arthroplasty; VA, Veterans Health Administration.
Outpatient hospital refers to a hospital outpatient department.
The majority of VA-purchased TKAs (86%) were performed at an inpatient hospital, where the unadjusted average payment was $13,339 (SD $23,698), including both the institutional payment and the professional fee. Among these inpatient TKAs, the average length of stay was 2.7 (SD 2.0). Outpatient TKAs were less commonly observed in the PIT claims; 1,017 were performed at hospitals and 31 at ASCs. Average payment was $9,348, and $16,561 at hospital outpatient departments and ASCs, respectively.
VA rules stipulate that VA-purchased care payments should not exceed Medicare payments, unless there are extenuating circumstances. CMS provides tools that estimate the average payment for specific procedures. The average VA payment was consistent with CMS’s estimated 2019 payment (2018 payments were not available) for hospital outpatient departments at $10,900 and their estimated professional fee payment ranged from $1,249 to $1,799. (Of note, CMS did not allow payments to ASCs for TKAs in 2018.) This suggests that VA payments were consistent with the Medicare fee schedules, as stipulated in the Choice Act.
The regression analysis reported in Table 3 shows that TKAs performed in a VA inpatient setting cost $14,869 (standard error [SE] 299.9) more than the payments for TKAs performed as inpatient procedures at a community hospital. This comparison controlled for location of service, age, gender, and patient risk as measured by the Nosos score. The results were robust to model choice; the GLM model yielded a predicted mean difference of $15,269.
Table 3.
Ordinary Least Squares Regression Comparing VA-Delivered Care to VA-Purchased Care for Knee Arthroplasties and Cataract Surgeries in FY2018 a
| TKA | Cataract Surgeries b | |||
|---|---|---|---|---|
| Coefficient | P Value | Coefficient | P Value | |
| VA-purchased | Reference | Reference | ||
| VA-provided | 14869.2 (299.9) | <0.001 | 2680.0 (15.8) | <0.001 |
| Location | ||||
| Inpatient hospital | Reference | — | — | |
| Outpatient hospital | 4562.9 (375.3) | <0.001 | — | — |
| Outpatient ASC | 3499.5 (5,990.2) | 0.56 | — | — |
| Age | ||||
| <65 | Reference | Reference | ||
| 65-70 | 339.3 (481.0) | 0.48 | −60.3 (36.9) | 0.103 |
| 70-74 | 421.6 (366.2) | 0.25 | −75.7 (35.8) | 0.035 |
| 75-84 | 225.3 (399.1) | 0.57 | −0.50 (45.0) | 0.99 |
| 85+ | −346.1 (430.7) | 0.42 | 252.6 (40.2) | <0.001 |
| Nosos | 376.0 (87.3) | <0.001 | 55.9 (13.6) | <0.001 |
| Gender | ||||
| Female | Reference | Reference | ||
| Male | −273.0 (395.8) | 0.49 | 92.7 (50.8) | 0.067 |
| Constant | 12917.7 (422.0) | <0.001 | 1423.8 (55.2) | <0.001 |
| N | 13,600 | 71,598 | ||
Standard errors (SE) adjust for clustering within person, in parentheses.
Estimated for outpatient only.
Cataract Costs
In 2018, VA performed 67,353 cataract surgeries at an unadjusted average cost of $4,301 (SD $2,835). In addition, VA processed 25,860 payments for cataract surgeries from community providers during this time (see Table 2). We compared VA-delivered care to VA-purchased care by setting. The majority (75%) of the claims were from ASCs with an average payment of $1,346 (SD $463). Cataract surgeries conducted at a hospital outpatient department were more expensive (average $1,585, SD $629) than at ASCs. Cataract procedures in a clinic office were the least common, but in these cases, the average payment was $876 (SD $891). Data from CMS’ website indicated that the 2019 average payment for a cataract was $1,012 when provided in an ASC and $2,021 when provided in a hospital outpatient department. Again, this shows that VA payments were consistent with the Medicare fee schedules.
The regression results in Table 3 show that cataracts performed in a VA hospital cost $2,680 (SE 15.8) more than the VA payments for cataracts performed at community hospitals. This comparison controls for age, gender, and risk as measured by the Nosos score. The results were robust to model choice; the GLM model yielded a predicted mean difference of $2,773.
Missing Claims Data
In our primary analysis, we excluded 1,266 cataract records that had a CPT modifier for preoperative or postoperative care. For the remaining claims, we assumed that the information was complete, although the low costs shown in Table 2 suggest that pre- or postoperative care with missing modifier codes may still have been present in the data. The results changed little when we relaxed or tightened our selection criteria. When we required all cataract claims to have an eye-side modifier, thereby excluding 5,251 claims, the average cataract payment to ASCs increased by $1. Second, when we excluded 2,505 cataract claims with a payment <$200 (which we assumed was for pre- or postoperative care with missing modifier codes), the average cataract payment for ASCs increased by $40.
Overhead and Fees
Our cost analysis includes the cost of operating the VA Office of Community Care and third-party administrator fees that the VA pays (an additional 4.95%). To assess whether overhead and fees change over time, we examined these costs in FY2019. The cost of operating the Office of Community Care increased faster in FY2019 than spending on community care, such that each claim should add 9.6% in FY19 (4.7% for operating the Office of Community Care and 4.85% for third-party administrator fees). The FY19 amount was double the FY18 amount.
Discussion
In 2014, Congress enacted legislation to enable more veterans to receive VA-purchased care from community providers. VA modernized its Office of Community Care so that it would be able to handle the increasing number of claims incurring through community care. The VA Office of Community Care also developed partnerships with third-party administrators to create networks of community providers willing to treat veterans. Although there has been some research on quality of care and patient experience,16,27–29 there has been little research on costs and none on value of care, in part because this required gaining experience with VA’s new claims database (PIT).
The VA employs multiple claims processing systems, which researchers cannot access directly, and centralizes these claims in the PIT, which VA researchers can access. The PIT data are organized as individual claim lines, and these need to be threaded together to estimate total payments. This can be facilitated by using the PIT Authorization Key, but additional steps are needed to exclude claims that share the authorization key but are unrelated to the procedure under study. The PIT claims are subject to duplication and missing information, such as missing modifier codes. This can lead to both high and low costs. Thus, researchers should use these data with caution, and ensure to the best of their ability, that the average payment is accurate and not unduly influenced by low or high costs. In our work with cataracts, the average costs were robust to different exclusion and inclusion criteria, but this should not be assumed in other samples. Despite the extra effort required to use the PIT data, they have some advantages over legacy systems. For example, the PIT data include the billing and rendering national provider identifier, which can be linked to CMS’s National Plan and Provider Enumeration System (NPPES). This enables further examination of the provider or geocoding of the data to address questions about network adequacy or travel distance. 13 VA is currently developing a replacement for the PIT, although the release date of this new system has not been provided.
The PIT reports VA payments, but it excludes overhead and fees incurred from third-party administrators, both of which are needed to obtain more accurate total costs of community care. In FY2018, the overhead cost for operating VA’s Office of Community Care was 2.4%, while third-party administrator fees added another 2.6%. Caution is warranted in applying these percentages to other years; we saw large increases in overhead and fees in FY2019, which may reflect implementation of the MISSION Act on June 6, 2019. Our estimates of overhead diverge sharply from those produced by Arnsdorf and Greenberg, 30 who estimated the overhead costs from the Choice Act through a Freedom of Information Act request. They reported that 24% of dollars since the Choice Act began in 2014 were being spent on overhead to the third-party administrators. Since we do not know how their overhead costs were calculated, we cannot examine the reasons for these differences in overhead costs in this article. Future research needs to examine this issue in greater detail so that more accurate overhead costs can be determined, and VA can better estimate its future resource allocations. This may be particularly salient due to the implementation of the MISSION Act, which enables even greater access to community care than the Choice Act.
With the implementation of the Choice and MISSION Acts, VA tasked VA clinicians with coordinating care when veterans receive purchased care in the community. Although the VA is hoping that this will prevent many of the problems that have been associated with fragmentation in the early Choice era,31–34 this requires that VA physicians integrate information across multiple systems. Our cost estimates do not include time for care coordination. The VA Office of Primary Care is conducting a time and motion study, which will provide insights into this issue. The added time by VA providers needs to be considered in comparisons of costs and quality.
VA payments for cataract surgeries and TKAs in the community were less than the VA cost of providing these services in the VA. These differences offer opportunities for VA to examine why it has higher costs and, when appropriate, implement innovations to lower its costs. Through FY2018, VA conducted most of its cataract surgeries in operating rooms, which are encumbered with added fixed costs. Similarly, as of 2018, all VA-delivered TKAs were performed in the inpatient setting, whereas non-VA hospitals began to perform TKAs in ambulatory care with the passage of the CMS rule in January 2018 allowing reimbursement to hospital outpatient departments. Moving clinically appropriate procedures to less-intensive settings, some of which has already started, will be important for helping the VA to optimize its variable and fixed costs, possibly saving resources and expanding access in the long run.
VA payments to community providers reflect the Choice and MISSION Acts, which cap VA payments using Medicare prices, with a few exceptions. VA payments were very similar to estimated Medicare payments that published on CMS websites. This may lessen the need for future cost comparisons, because VA can estimate its expected fee-for-service payments ahead of time. This also suggests more fruitful comparisons in the future. If community providers are concerned about VA’s reimbursement, the main options facing them include the following: 1) not accepting VA cases, 2) selecting patients based on risk, 3) choosing a treatment or setting that maximizes reimbursement, or 4) inducing demand for more services once a patient has been referred. 35 Head-to-head comparisons may wish to examine these possible mechanisms directly. Of these four options, our data highlight the need for more research on risk selection. We show that patients who received VA-purchased TKAs had half the risk score of patients receiving VA-delivered TKA. In prior work, we found considerable heterogeneity in veterans using community care, with lower risk scores for people enrolling in the Choice program compared to veterans who used the more traditional Fee program. 36 Future work is critically needed to understand the differences in patient risk and whether this reflects patient selection, provider selection, or the “crowding-out” of services that were previously covered by Medicare. 37 Future research should also consider costs over time because the Choice and MISSION Act pay based on the Medicare fee schedule and do not place any constraints on quantity of services over time or value.
This study has limitations that merit discussion. Although we considered missing data, we assumed that the procedure codes and the procedure dates of service were accurate and complete. The low and high costs raise questions about data accuracy, suggesting that CPT modifiers may be missing. In addition, we also observed 31 payments to ASCs for TKAs in FY2018, although CMS did not authorize reimbursement for TKAs at ASCs until 2020. Future studies may need to develop algorithms to clean the data, flagging any records that warrant further investigation or inclusion in a sensitivity analysis. It is also important to remember that PIT is a database that accumulates claims from multiple source systems. Currently, researchers cannot access the source system, thus care is warranted in checking the PIT data for duplicates. We also focused on two elective surgical procedures, but these findings may not generalize to other procedures. Finally, we did not control for hospital’s teaching status given the considerable debate about whether teaching hospitals lead to higher costs.38,39 Future research should examine whether teaching hospitals are less likely to treat veterans given the payment cap.
In conclusion, the VA has rapidly expanded its purchasing of health care in the community. We present methods for extracting claims for VA-purchased care and estimating the total payments including the cost of the VA Office of Community Care and the third-party administrator fees. These methods can be used to help VA understand its costs of purchasing care and how that compares to VA-delivered care.
Acknowledgments
We acknowledge the comments from Kristin Cunningham, from the VA Office of Community Care, and Glenn Cockerham and Nicholas Giori, both from the Palo Alto VA.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support was provided by a grant through the VA Health Services Research and Development (HSR&D) Service (SDR 18-318, Award No. 1I01HX002646).
Todd Wagner is also supported by an HSR&D Research Career Scientist award (RCS 17-154). Megan Vanneman is also supported by an HSR&D Career Development Award (CDA 15-259, Award No. 1IK2HX00262). Amy Rosen is also supported by an HSR&D Senior Research Career Scientist award (RCS 97-401).
ORCID iD: Todd H. Wagner  https://orcid.org/0000-0001-7625-3504
https://orcid.org/0000-0001-7625-3504
Contributor Information
Todd H. Wagner, Health Economics Resource Center, VA Palo Alto Health Care System, Menlo Park, California; Department of Surgery, Stanford University, Stanford, California.
Jeanie Lo, Health Economics Resource Center, VA Palo Alto Health Care System, Menlo Park, California.
Erin Beilstein-Wedel, Center for Healthcare Organization and Implementation Research (CHOIR), VA Boston Healthcare System, Boston, Massachusetts.
Megan E. Vanneman, Informatics, Decision-Enhancement and Analytic Sciences Center, VA Salt Lake City Health Care System, Salt Lake City, Utah Division of Epidemiology, Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, Utah; Division of Health System Innovation and Research, Department of Population Health Sciences, University of Utah School of Medicine, Salt Lake City, Utah.
Michael Shwartz, Center for Healthcare Organization and Implementation Research (CHOIR), VA Boston Healthcare System, Boston, Massachusetts.
Amy K. Rosen, Center for Healthcare Organization and Implementation Research (CHOIR), VA Boston Healthcare System, Boston, Massachusetts Department of Surgery, Boston University School of Medicine, Boston, Massachusetts.
References
- 1. Mattocks KM, Kroll-Desrosiers A, Kinney R, Elwy AR, Cunningham KJ, Mengeling MA. Understanding VA’s use of and relationships with community care providers under the MISSION Act. Med Care. 2021;59(Suppl 3):S252–S258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Massarweh NN, Itani KM, Morris MS. The VA MISSION act and the future of Veterans’ access to quality health care. JAMA. 2020;324(4):343–4. [DOI] [PubMed] [Google Scholar]
- 3. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping Veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Robinson JC. Theory and practice in the design of physician payment incentives. Milbank Q. 2001;79(2):149–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gidwani RA, Hong J, Murrell S. HERC: fee basis data: a guide for researchers [cited October 21, 2021]. Available from: https://www.herc.research.va.gov/include/page.asp?id=guidebook-fee-basis
- 6. Wang V, Maciejewski ML, Patel UD, Stechuchak KM, Hynes DM, Weinberger M. Comparison of outcomes for Veterans receiving dialysis care from VA and non-VA providers. BMC Health Serv Res. 2013;13(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leslie DL, Goulet J, Skanderson M, Mattocks K, Haskell S, Brandt C. VA health care utilization and costs among male and female Veterans in the year after service in Afghanistan and Iraq. Mil Med. 2011;176(3):265–9. [DOI] [PubMed] [Google Scholar]
- 8. Vanneman ME, Harris AHS, Asch SM, Scott WJ, Murrell SS, Wagner TH. Iraq and Afghanistan Veterans’ use of Veterans Health Administration and purchased care before and after Veterans Choice Program implementation. Med Care. 2017;55(Suppl 7, Suppl 1):S37–S44. [DOI] [PubMed] [Google Scholar]
- 9. Agency for Healthcare Research and Quality. Most common operations in hospital inpatient stays [cited October 21, 2021]. Available from: https://hcup-us.ahrq.gov/faststats/NationalProceduresServlet?year1=2014&characteristic1=0&included1=1&year2=2008&characteristic2=54&included2=1&expansionInfoState=hide&dataTablesState=hide&definitionsState=hide&exportState=hide
- 10. Frisch NB, Courtney PM, Darrith B, Copeland LA, Gerlinger TL. Veterans undergoing total hip and knee arthroplasty: 30-day outcomes as compared to the general population. J Am Acad Orthop Surg. 2020;28(22):923–9. [DOI] [PubMed] [Google Scholar]
- 11. Lam V, Teutsch S, Fielding J. Hip and knee replacements: a neglected potential savings opportunity. JAMA. 2018;319(10):977–8. [DOI] [PubMed] [Google Scholar]
- 12. Karaca Z, McDermott KW. High-volume invasive, therapeutic ambulatory surgeries performed in hospital-owned facilities, 2016. [cited October 21, 2021]. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb252-Invasive-Ambulatory-Surgeries-2016.jsp [PubMed]
- 13. Pettey WBP, Wagner TH, Rosen AK, Beilstein-Wedel E, Shwartz M, Vanneman ME. Comparing driving miles for Department of Veterans Affairs–delivered versus Department of Veterans Affairs–purchased cataract surgery. Med Care. 2021;59(Suppl 3):S307–S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. MEDPAC. Ambulatory surgical center services [cited October 21, 2021]. Available from: http://www.medpac.gov/docs/default-source/reports/mar21_medpac_report_ch5_sec.pdf?sfvrsn=0
- 15. Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries. Health Policy. 2014;118(3):292–303. [DOI] [PubMed] [Google Scholar]
- 16. Rosen AK, Vanneman ME, O’Brien WJ, et al. Comparing cataract surgery complication rates in Veterans receiving VA and community care. Health Serv Res. 2020;55(5):690–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khristoforov V. VA Paid claims. Personal communication. January 24, 2019. [Google Scholar]
- 18. Barnett PG. An improved set of standards for finding cost for cost-effectiveness analysis. Med Care. 2009;47(7 Suppl 1):S82–S88. [DOI] [PubMed] [Google Scholar]
- 19. Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009;18(10):1181–201. [DOI] [PubMed] [Google Scholar]
- 20. Phibbs CS, Barnett PG, Fan A. HERC: research guide to the managerial cost accounting national cost extracts [cited October 21, 2021]. Available from: https://www.herc.research.va.gov/include/page.asp?id=guidebook-mca-nde
- 21. Shroyer ALW, Quin JA, Wagner TH, et al. Off-pump versus on-pump impact: diabetic patient 5-year coronary artery bypass clinical outcomes. Ann Thorac Surg. 2019;107(1):92–8. [DOI] [PubMed] [Google Scholar]
- 22. Carey K, Stefos T, Zhao S, Borzecki AM, Rosen AK. Excess costs attributable to postoperative complications. Med Care Res Rev. 2011;68(4):490–503. [DOI] [PubMed] [Google Scholar]
- 23. Nelson RE, Suo Y, Pettey W, et al. Costs associated with health care services accessed through VA and in the community through Medicare for Veterans experiencing homelessness. Health Serv Res. 2018;53(Suppl 3):5352–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wagner TH, Upadhyay A, Cowgill E, et al. Risk adjustment tools for learning health systems: a comparison of DxCG and CMS-HCC V21. Health Serv Res. 2016;51(5):2002–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wagner TH, Gehlert E, Rosen AK, Valenstein M. Technical Report 31: Updating the Psychiatric Case Mix System (PsyCMS) Mental Health and Substance Use Grouper for ICD-10-CM. Health Economics Resource Center; 2016. Available from: https://www.herc.research.va.gov/include/page.asp?id=technical-report-psycms-icd10 [Google Scholar]
- 26. Wagner TH, Stefos T, Moran E, et al. Risk Adjustment: Guide to the V21 and Nosos Risk Score Programs. Health Economics Resource Center; 2016. Available from: https://www.herc.research.va.gov/include/page.asp?id=technical-report-risk-adjustment [Google Scholar]
- 27. Waldo SW, Glorioso TJ, Barón AE, et al. Outcomes among patients undergoing elective percutaneous coronary intervention at Veterans Affairs and Community Care Hospitals. J Am Coll Cardiol. 2020;76(9):1112–6. [DOI] [PubMed] [Google Scholar]
- 28. Harris AHS, Beilstein-Wedel EE, Rosen AK, et al. Comparing complication rates after elective total knee arthroplasty delivered or purchased by the VA. Health Aff (Millwood). 2021;40(8):1312–20. [DOI] [PubMed] [Google Scholar]
- 29. Vanneman ME, Wagner TH, Shwartz M, et al. Veterans’ experiences with outpatient care: comparing the Veterans Affairs System with Community-Based Care: study compares Veterans’ experiences in VA-delivered and community-based outpatient care. Health Aff (Millwood). 2020;39(8):1368–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arnsdorf I, Greenberg J. The VA’s Private Care Program gave companies billions and vets longer waits [cited April 20, 2021]. Available from: https://www.propublica.org/article/va-private-care-program-gave-companies-billions-and-vets-longer-waits?token=S9_I6_c58F6Tw8NAV_XfYacS7qYZyogW
- 31. Cebul RD, Rebitzer JB, Taylor LJ, Votruba ME. Organizational fragmentation and care quality in the US healthcare system. J Econ Perspect. 2008;22(4):93–113. [DOI] [PubMed] [Google Scholar]
- 32. Cordasco KM, Frayne SM, Kansagara D, et al. Coordinating care across VA providers and settings: policy and research recommendations from VA’s state of the art conference. J Gen Intern Med. 2019;34(Suppl 1):11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kern LM, Seirup JK, Rajan M, Jawahar R, Stuard SS. Fragmented ambulatory care and subsequent healthcare utilization among Medicare beneficiaries. Am J Manag Care. 2018;24(9):e278–e284. [PubMed] [Google Scholar]
- 34. Frandsen BR, Joynt KE, Rebitzer JB, Jha AK. Care fragmentation, quality, and costs among chronically ill patients. Am J Manag Care. 2015;21(5):355–62. [PubMed] [Google Scholar]
- 35. Nguyen LL, Smith AD, Scully RE, et al. Provider-induced demand in the treatment of carotid artery stenosis: variation in treatment decisions between private sector fee-for-service vs salary-based military physicians. JAMA Surg. 2017;152(6):565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rosen AK, Wagner TH, Pettey WBP, et al. Differences in risk scores of Veterans receiving community care purchased by the Veterans Health Administration. Health Serv Res. 2018;53(Suppl 3):5438–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gruber J, Simon K. Crowd-out 10 years later: have recent public insurance expansions crowded out private health insurance? J Health Econ. 2008;27(2):201–17. [DOI] [PubMed] [Google Scholar]
- 38. Chandra A, Khullar D, Wilensky GR. The economics of graduate medical education. N Engl J Med. 2014;370(25):2357–60. [DOI] [PubMed] [Google Scholar]
- 39. Sloan FA. Quality and cost of care by hospital teaching status: what are the differences? Milbank Q. 2021;99(1):273–327. [DOI] [PMC free article] [PubMed] [Google Scholar]