Abstract
Purpose. We investigated 1) perceived roles in decision-making among advanced cancer patients in 5 Asian countries 2) associations of patient characteristics with these roles, and 3) the association of perceived roles with quality of life and perceived quality of care. Methods. We surveyed 1585 patients with stage IV solid cancer. Multinomial logistic regressions were used to analyze associations of patient characteristics with decision-making roles. Multivariate regressions were used to analyze associations of decision-making roles with quality of life and care. Results. The most common perceived-role was no patient involvement. Most patients (73%) reported roles consistent with their preferences. Being male, nonminority, higher educated, aware of advanced cancer diagnosis, and knowledge of cancer diagnosis for ≥1 year were associated with higher levels of patient involvement in decision-making. Compared to no patient involvement, joint decision-making (together with physicians/family) was associated with higher social (β = 2.49, P < 0.01) and spiritual (β = 2.64, P < 0.01) well-being, and better quality of physician communication (β = 9.73, P < 0.01) and care coordination (β = 13.96, P < 0.01) while making decisions alone was associated with lower emotional (β = −1.43, P < 0.01), social (β = −2.39, P < 0.01), and spiritual (β = −2.98, P < 0.01) well-being. Conclusions. Findings suggest that a substantial number of advanced cancer patients were not (and preferred not to be) involved in decision-making. Despite this finding, joint decision-making together with physicians/family was associated with better quality of life and care. Implications. Physicians should explain the benefits of shared decision making to patients and encourage participation in decision-making, while ensuring that patients feel supported and do not find decision-making overwhelming.
Keywords: shared decision making, low- and middle-income countries, LMICs, advanced cancer
Introduction
Shared decision making (SDM) is advocated to improve patient quality of life and quality of care. 1 However, the degrees to which patients are involved in decision-making vary due to cultural, social, and other factors.2–4 A consistent finding is that patients in Asian societies and patients who are ethnically Asian tend to report lower levels of involvement in decision-making than their counterparts in Western societies. 5 This might be explained by a prevalent paternalistic view of the physician-patient relationship. 6 Physicians are perceived to be of higher social status in Asian societies where social hierarchy is traditionally more prominent and more socially accepted. 7 In addition, collectivism in Asian societies with closer familial relationship also facilitates families to make important decisions, such as medical decisions, together. 8 Although there has been recent evidence of increased patient involvement in decision-making and efforts to improve patient empowerment in Asian societies, these are mostly from high-income Asian countries.9–11 In low- and middle-income countries (LMICs), where the educational gap and, thus, social distance between physicians and patients are generally larger, it remains to be seen to what extent patients with terminal diseases, such as advanced cancer, are involved in decision-making, and whether these perceived roles are concordant with their preferred roles.
Studies have shown that patients coming from socially and/or economically advantaged groups are likelier to report higher levels of involvement in decision-making. Patients who are younger 12 and have attained higher education 13 are more likely to participate in decision-making. Those who are older, 14 in minority ethnic groups,13,15,16 and lower-income households 13 reported lower levels of involvement in decision-making. Evidence on gender 17 and marital status18,19 seems to be mixed. In terms of medical factors, evidence is lacking on whether awareness of prognosis is associated with higher or lower levels of involvement in decision-making. 9
A systematic review of SDM in cancer treatment 20 found evidence suggesting a positive relationship between greater perceived involvement in decision-making and quality of life. However, there are also studies involving cancer patients that have found weak 21 or no 22 association between decision-making roles and quality of life. In terms of perceived quality of care, evidence shows that involvement in decision-making is associated with higher quality of care 23 and satisfaction with consultation. 24 However, apart from a handful of studies, these outcomes have not been well studied, 25 and none of these studies were on patient populations from LMICs in Asia. Due to the cultural differences discussed above, the association of decision-making roles with quality of life and quality of care may be different for this patient subpopulation than those from Western societies.
The objectives of this study were to assess patient-reported perceived roles in decision-making (no patient involvement, physician/family-led decision-making, joint decision-making, patient-led decision-making, patient-alone decision-making) in five LMICs (Bangladesh, China, India, Sri Lanka, and Vietnam) in Asia, and to examine to what extent perceived roles were concordant with preferences. We hypothesize that the majority of the patients in our sample will report lower levels of involvement in decision-making (i.e., no involvement or physician/family-led decision-making). Second, we investigate the associations of patient (sociodemographic and medical) characteristics with perceived roles in decision-making. Third, we examine whether the characteristics of patients whose perceived roles were not concordant with their preferences different than the characteristics of patients whose roles were concordant. Last, we investigate the associations of perceived roles in decision-making with quality of life (emotional, social, and spiritual well-being) and perceived quality of care (quality of physician communication and care coordination). We hypothesize that SDM (i.e., joint decision-making with physicians and/or family) will be associated with higher quality of life and perceived quality of care; however, patient-only decision-making will be associated with lower quality of life and perceived quality of care due to perceived burden from decision-making and feeling alone or uncared for given the cultural context of collectivism in Asia.
Methods
Study Participants and Setting
The Asian Patient Perspectives Regarding Oncology Awareness, Care and Health (APPROACH) is a multicountry cross-sectional survey on cancer care across LMICs in Asia.
Participants for this particular study were recruited in five countries—Bangladesh, China, India, Sri Lanka, and Vietnam—with a cancer incidence rate of 95, 315, 96, 138, and 188 per 100,000, respectively, in 2020.26–30 The recruitment sites were eight major public or nonprofit hospitals with three hospitals in India, two in Bangladesh, and one each for other countries. We targeted the leading referral or tertiary hospitals for cancer treatment in each country where patients are offered anticancer treatments as well as palliative care.
A convenience sample of approximately 200 participants were recruited from the medical oncology and/or palliative care departments at each hospital and surveys were conducted through face-to-face interviews. The inclusion criteria included the following: 1) at least 21 years of age; 2) having a diagnosis of stage IV solid cancer; 3) being a citizen of the participating country; and 4) being aware of their cancer diagnosis. While verbal consent was taken from Vietnam, written consent was provided by the participants in other countries.
A total of 1585 patients were recruited across the eight hospitals. Sixty-four (4%) participants were dropped after assessing the interviewer responses to whether they felt the patient was mentally competent enough to provide adequate responses, whether the patient understood the questions, and whether the patient’s hearing/visual difficulties adversely affected the survey. Fourteen (0.9%) patients were dropped due to missing responses to questions on decision-making and/or main outcomes. This resulted in an analytical sample of 1506.
The APPROACH study was approved by the Institutional Review Board of the National University of Singapore (Reference: B-15-319) as well as the ethics committees of each participating hospital.
Survey Development
The questionnaire was developed in consultation with oncologists. It comprised questions developed by the study investigators, and others taken or adapted from validated instruments. The questions designed by the study investigators were first developed in English. Subsequently, they were translated by professional translators into the most commonly spoken languages in each study site, and then back-translated to English. The original and back-translated English versions were compared, and reconciliations were made where necessary. Further revisions were made based on feedback from the physicians and cognitive interviews with 10 eligible patients in each study site.
Roles in Decision-Making
We asked patients the involvement of, and roles played by their family, physician, and themselves on decision-making for cancer treatment via two questions. The first question asked who was responsible for the important decisions regarding the patient’s treatments. Participants could choose any combination of three options: themselves, their family, and their physician. If a participant chose more than one option, a second question asked the participant to assign the role each party played in the decision-making. The roles were either being the final decision maker or being involved in discussions without making the final decision. For example, if the patient and patient’s family were chosen in the first question, the options for the second question would include the following: “I made the decisions after considering my family’s opinion” or “My family made the decision after considering my opinion” or “My family and I made the decision together.” We asked a similar set of questions to assess the preferred roles. The actual survey questions can be found in Table S1, Supplementary Material.
Based on the two questions, we categorized roles in decision-making into five different categories from lowest to highest level of involvement: 1) No patient involvement: patient’s family and/or physician makes decisions without patient involvement; 2) Physician- or family-led decision making: patient’s physician and/or family makes decisions after considering patient’s opinion; 3) Joint decision-making: patient makes decisions together with family and/or physician; 4) Patient-led decision-making: patient makes decisions after considering family’s and/or physician’s opinion; and 5) Patient-only decision-making: patient makes decisions alone. The exact categorization can be found in Table S2, Supplementary Material.
Quality of Life
We measured emotional, social, and spiritual well-being. Emotional and social well-being were measured using the relevant domains from the Functional Assessment of Cancer Therapy–General (FACT-G) (Version 4), which is a validated instrument designed to measure different domains of quality of life in cancer patients. The emotional well-being subscale ranged from 0 to 24, while the social well-being ranged from 0 to 28. Higher scores indicate greater well-being. Spiritual well-being was assessed with the Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being (FACIT-SP-12) Scale, a 12-item questionnaire. Total score ranged from 0 to 48 where higher scores indicated higher spiritual well-being.
For countries that did not have a validated version of FACIT-Sp (Sri Lanka and Vietnam), the scale was translated as per the translation protocol laid out by the license owner. Final translations were approved by the license owner.
Perceived Quality of Care
We examined the perceived quality of care based on the Cancer Care Outcomes Research and Surveillance Survey (CanCORS) study, which was developed to understand experiences of cancer patients.31,32 We assessed two domains: physician communication (five items) and coordination and responsiveness of care (six items). Each domain was converted into a 100-point scale with 0 representing the worst possible quality of care and 100 for optimal quality of care.
Patient Characteristics
Patients reported their age, gender, marital status, years of education, self-reported socioeconomic status (whether belonging to low income, lower-middle income, upper-middle income, or high income), belonging to majority/minority group or caste, years since they first learned about their cancer, and type of cancer. Patients were also asked, “Do you know the current stage (i.e., severity) of your cancer?” They could choose 1) Early Stage (stage I, II, or III), 2) Advanced Stage (stage IV), or 3) I don’t know. Those who selected advanced stage were considered aware of their cancer stage.
Statistical Analysis
We described distributions of patient sociodemographic characteristics, quality of life scores, and perceived quality of care scores both for the total sample population and for each country separately. We then presented distributions of patient-reported perceived roles in decision-making and to what extent these roles were concordant with patient preferences for each country.
We investigated the predictors of perceived roles in decision-making using a multinomial logit model. The dependent variable was the five-category decision-making roles where “no patient involvement” was set as the reference category. The independent variables were gender (female = 0, male = 1), marital status (married = 1, otherwise = 0), age, years of education, self-reported socioeconomic status (low-income = 0, lower-middle income = 1, upper [upper-middle or high] income = 1), belonging to a minority (e.g., ethnicity) or disadvantaged group (e.g., lower caste), awareness of advanced stage (Stage IV = 1, otherwise = 0), years since first learned about cancer (less than 6 months = 0, 6 months to 1 year = 1, more than 1 year = 1), and cancer type (lung cancer = 1, breast cancer = 1, colorectal cancer = 1, otherwise = 0).
We also examined whether the characteristics of patients who had discordance between their perceived and preferred roles in decision-making were different than those who had concordance between their perceived and preferred roles in decision-making. We used a multinomial logit model where the dependent variable had three categories: 1) involved in decision-making less than preferred, 2) involved in decision-making more than preferred, or 3) involved in decision-making at the preferred level, that is, concordance (reference category). The independent variables were the same as described above.
To investigate associations of roles in decision-making with patient outcomes, we estimated multivariate linear regression analyses which are used for models with more than one outcome. The outcome variables were the emotional well-being, social well-being, spiritual well-being, and perceived quality of physician communication and care coordination. The independent variables of interest were the five-category decision-making roles with “no patient involvement” as the reference category. We first investigated the unadjusted effects and then adjusted effects by controlling for patient characteristics (gender, age, education, marital status, self-reported socioeconomic status, belonging to a minority/disadvantage group, and awareness of advanced cancer stage) as described above.
We also added country dummy variables (reference: India) to control for any unobserved economic and cultural differences across the countries in all models.
For missing item responses, a missing category was created for categorical responses. For continuous responses, a mean of all nonmissing responses was imputed and an indicator variable for missing was created and interacted with the original variable. For all the regressions described above, we also conducted complete case analysis by excluding observations with missing data. All analyses were conducted using Stata version 15.1 (StataCorp LLC, College Station, TX).
Results
Sample Characteristics
The average (standard deviation [SD]) age of the entire sample was about 52 (13), with Bangladesh having the youngest average age of 48 (Table 1). The average (SD) number of years of education was about 8 (6) years. The patient sample from China had, on average, more years of education at 11 years. Just over half of the total participants (53%) were male, with Bangladesh having a higher proportion of males (65%) while Sri Lanka (34%) had a lower proportion of males. Eighty-four percent of participants were married across all sites. This was consistent across countries, with Sri Lanka having the lowest proportion of married participants (76%). The sample consisted of 30% participants from minority/disadvantaged groups, with Vietnam reporting the lowest (1%) and India reporting the highest (58%) rates. On average, 32% of the sample identified themselves as “low income,” 47% as “lower-middle income,” and 20% as “upper-middle or high income” family. China reported the lowest (9%) and Bangladesh reported the highest (43%) rates of “low income.”
Table 1.
Descriptive Statistics of Patient Characteristics
| Total | Bangladesh | China | India | Sri Lanka | Vietnam | |
|---|---|---|---|---|---|---|
| Sample size | 1506 | 336 | 178 | 593 | 200 | 199 |
| Gender a | ||||||
| Male | 795 (53%) | 217 (65%) | 93 (52%) | 311 (52%) | 67 (34%) | 107 (54%) |
| Missing | 1 (0%) | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Marital status | ||||||
| Married | 1265 (84%) | 286 (85%) | 157 (88%) | 501 (84%) | 151 (76%) | 170 (85%) |
| Missing | 1 (0%) | 0 (0%) | 0 (0%) | 1 (0%) | 0 (0%) | 0 (0%) |
| Age (years) | 52.13 (13.22) | 48.38 (13.58) | 58.24 (13.61) | 50.15 (12.52) | 55.81 (12.79) | 55.21 (11.15) |
| Education (years) | 7.88 (5.73) | 6.84 (6.43) | 11.39 (3.76) | 6.05 (5.95) | 9.95 (4.27) | 9.85 (3.44) |
| Working (part-time or full-time) | 882 (59%) | 169 (50%) | 75 (43%) | 388 (66%) | 103 (52%) | 147 (74%) |
| Minority-majority group | ||||||
| Minority/disadvantaged group | 451 (30%) | 64 (19%) | 11 (6%) | 346 (58%) | 28 (14%) | 2 (1%) |
| Missing | 36 (2%) | 0 (0%) | 1 (1%) | 35 (6%) | 0 (0%) | 0 (0%) |
| Self-reported socioeconomic status | ||||||
| Low income | 484 (32%) | 146 (43%) | 16 (9%) | 202 (34%) | 55 (28%) | 65 (33%) |
| Lower-middle income | 711 (47%) | 158 (47%) | 74 (42%) | 285 (48%) | 114 (57%) | 80 (40%) |
| Upper (upper-middle or high) income | 308 (20%) | 32 (9%) | 86 (48%) | 105 (18%) | 31 (16%) | 54 (28%) |
| Missing | 3 (0%) | 0 (0%) | 2 (1%) | 1 (0%) | 0 (0%) | 0 (0%) |
| Knowledge of cancer stage | ||||||
| Advanced stage | 425 (28%) | 93 (28%) | 72 (40%) | 92 (16%) | 65 (33%) | 103 (52%) |
| Not sure | 879 (58%) | 232 (69%) | 54 (30%) | 467 (79%) | 84 (42%) | 42 (21%) |
| Duration of first learning about cancer | ||||||
| Less than 6 months | 547 (36%) | 142 (42%) | 60 (34%) | 200 (34%) | 65 (32%) | 80 (40%) |
| 6 months to 1 year | 402 (27%) | 114 (34%) | 30 (17%) | 150 (25%) | 50 (25%) | 58 (29%) |
| More than 1 year | 536 (36%) | 80 (24%) | 76 (43%) | 237 (40%) | 84 (42%) | 59 (30%) |
| Missing | 21 (1%) | 0 (0%) | 12 (7%) | 6 (1%) | 1 (<1%) | 2 (1%) |
| Cancer type | ||||||
| Lung | 280 (19%) | 49 (15%) | 43 (24%) | 115 (19%) | 29 (14%) | 44 (22%) |
| Breast | 258 (17%) | 43 (13%) | 16 (9%) | 107 (18%) | 47 (23%) | 45 (23%) |
| Colorectal | 108 (7%) | 17 (5%) | 28 (16%) | 12 (2%) | 31 (15%) | 20 (10%) |
| Gastric | 91 (6%) | 38 (11%) | 13 (7%) | 27 (5%) | 4 (2%) | 9 (5%) |
| Liver | 58 (4%) | 37 (11%) | 2 (1%) | 15 (3%) | 1 (<1%) | 3 (2%) |
| Ovarian | 64 (4%) | 6 (2%) | 10 (6%) | 15 (3%) | 23 (11%) | 10 (5%) |
| Quality of life | ||||||
| Social well-being (out of 24) | 19.53 (5.58) | 18.29 (5.06) | 23.05 (4.59) | 18.02 (5.79) | 20.74 (5.36) | 21.76 (4.23) |
| Emotional well-being (out of 28) | 14.68 (6.30) | 9.94 (4.85) | 18.99 (4.43) | 15.87 (6.35) | 16.66 (5.26) | 13.34 (5.57) |
| Spiritual well-being (out of 48) | 29.94 (9.07) | 25.32 (7.43) | 33.42 (9.15) | 30.82 (8.95) | 31.22 (9.33) | 30.73 (8.84) |
| Perceive quality of care | ||||||
| Physician communication (out of 100) | 68.26 (35.51) | 40.26 (32.36) | 68.40 (32.55) | 77.17 (33.30) | 77.50 (27.92) | 79.50 (31.43) |
| Care coordination (out of 100) | 59.99 (35.15) | 31.05 (30.48) | 65.97 (25.21) | 65.72 (35.41) | 73.22 (20.88) | 71.61 (34.98) |
Count (%) shown for categorical variables and mean (standard deviation) shown for continuous variables.
Twenty-eight percent of patients were aware of that their cancer was stage IV, with the highest rate of awareness (52%) in the Vietnamese sample. The majority of the patients were not aware of their cancer stage with 58% reporting that they were not sure of their cancer stage and 14% reporting that they had early stage cancer. Thirty-six percent of the patients knew of their cancer for less than 6 months while another 36% knew of it for more than 1 year at the time of the survey. The most common cancer types in the sample were lung (19%), breast (17%), and colorectal (7%) cancer. These are consistent with the most common cancer types observed at the population level in these counties, except for colorectal cancer in Bangladesh.26–30
The average (SD) scores were 19.53 (5.58) for social well-being, 14.68 (6.30) for emotional well-being, and 29.94 (9.07) for spiritual well-being. China scored the highest average score for all three quality of life scales, while Bangladesh scored the lowest for emotional and spiritual well-being and second lowest for social well-being (Table 1).
The perceived quality of care average scores were 68.26 (35.51) for physician communication and 59.99 (35.15) for coordination and care responsiveness. These scores were lowest in Bangladesh (Table 1).
Perceived Roles in Decision-Making
The most commonly reported decision-making role was “no patient involvement” in each country. All other roles in decision-making had less than 20% of individuals in each country, with the only exception of “joint decision-making” in China (Figure 1).
Figure 1.
Distribution of perceived roles in decision-making for each country: 1) No patient involvement; 2) Physician/Family-led; 3) Joint decision; 4) Patient led; 5) Patient only.
Concordance/Discordance Between Perceived and Preferred Roles in Decision-Making
The majority of patients (73%) participated in decision-making at a level concordant with their preferences, with Sri Lanka having the highest percentage of such patients (95%) and Vietnam the lowest (54%). Overall, 15% of patients reported that they were involved more than preferred and 11% reported that they were involved less than they preferred. For Bangladesh, more patients reported that they were involved more than they preferred (24%) compared to those who reported being involved less than preferred (10%). The other countries had roughly similar numbers of those who perceived more and those who perceived less involvement than preferred (Figure 2 and Table S3, Supplementary Material).
Figure 2.
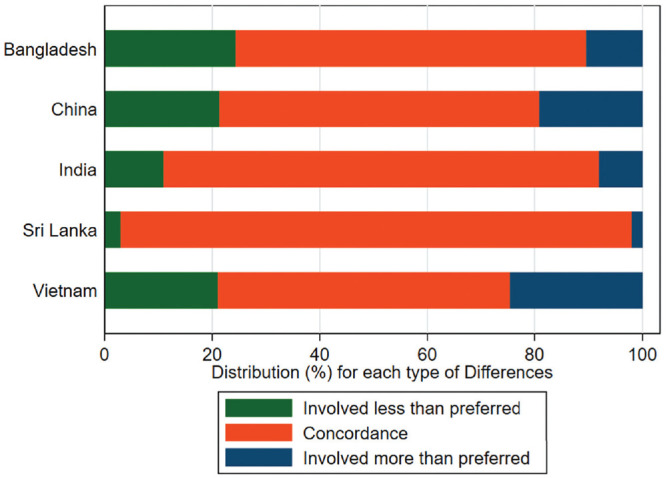
Distribution of discordance/concordance between perceived and preferred roles in decision-making.
Associations of Patient Characteristics With Perceived Roles in Decision-Making
Compared to no patient involvement, male patients were more likely to report patient-led (β = 0.69, P < 0.01) or patient-only (β = 0.68, P = 0.01) decision-making (Table 2). Education was associated with patient involvement at any level compared to no involvement (P < 0.05 for all). Compared to low-income patients, lower-middle-income and upper-income patients were more likely to report physician/family-led decision-making (β = 0.57, P = 0.03; β = 0.69, P = 0.03) and less likely to report patient-only decision-making (β = −0.76, P < 0.01; β = −0.66, P = 0.03). Patients from minority/disadvantaged groups were more likely to report physician/family-led decision-making (β = 0.58, P = 0.03), and were less likely to report joint decision-making (β = −0.62, P < 0.01) or patient-only decision-making (β = −0.85, P < 0.01). Those who were aware of their advanced cancer stage were more likely to report physician/family-led decision-making (β = 0.68, P < 0.01) or patient-led decision-making (β = 0.49, P = 0.02). Compared to patients who had known about their cancer for less than 6 months, those who had known for more than 1 year were more likely to report joint (β = 0.55, P < 0.01) or patient-led (β = 0.74, P < 0.01) or patient-only (β = 0.67, P < 0.01) decision-making. Those with breast cancer were more likely to report patient-led decision-making (β = 0.59, P = 0.02). The complete case analysis produced very similar findings (Table S4, Supplementary Material).
Table 2.
Multinomial Logistic Regression: Associations of Patient Characteristics With Perceived Roles in Decision-Making (Reference: No Patient Involvement), N = 1506
| Physician/Family Led | Joint Decision | Patient Led | Patient Only | |
|---|---|---|---|---|
| Gender (Ref: Female) | ||||
| Male | −0.09 | 0.10 | 0.69*** | 0.68*** |
| Missing | −13.47 | −13.89 | −12.31 | −11.60 |
| Marital status (Ref: Single) | ||||
| Married | 0.41 | −0.02 | −0.002 | −0.31 |
| Missing | 0.17 | −1.14 | 20.32 | −2.02 |
| Age (years) | −0.003 | −0.009 | −0.001 | −0.01* |
| Education (years) | ||||
| Education | 0.08*** | 0.07*** | 0.04** | 0.05** |
| Education (missing) | 0.03 | 0.02 | −0.05 | −1.51 |
| Self-reported socioeconomic status (Ref: Low income) | ||||
| Lower-middle income | 0.57** | 0.02 | −0.10 | −0.76*** |
| Upper income | 0.69** | −0.27 | −0.005 | −0.66** |
| Missing | −12.15 | 0.78 | 1.25 | −12.67 |
| Minority-majority group (Ref: Majority) | ||||
| Minority/disadvantaged | 0.58** | −0.62*** | −0.06 | −0.85*** |
| Missing | 0.70 | −0.98 | −0.04 | −0.21 |
| Awareness of advanced stage of cancer (Ref: Unaware) | ||||
| Aware | 0.68*** | 0.05 | 0.49** | 0.38* |
| Duration of knowing cancer (Ref: Less than 6 months) | ||||
| 6 months to 1 year | 0.36 | 0.31 | 0.18 | 0.15 |
| More than 1 year | 0.43* | 0.55*** | 0.74*** | 0.67*** |
| Missing | 0.85 | 0.56 | −0.22 | 2.04*** |
| Cancer type (Ref: Other types) | ||||
| Lung | −0.09 | −0.17 | −0.30 | 0.15 |
| Breast | −0.18 | −0.22 | −0.59** | 0.09 |
| Colorectal | −0.10 | −0.009 | 0.40 | 0.42 |
| Country (Ref: India) | ||||
| Bangladesh | 1.34*** | −0.01 | −0.52* | −0.30 |
| China | 0.80** | 0.18 | −0.56 | −1.34** |
| Sri Lanka | 0.38 | −0.66** | −0.68** | 0.30 |
| Vietnam | 1.37*** | −0.05 | 0.27 | 0.51 |
| Constant | −4.41*** | −1.14*** | −2.44*** | −1.39** |
P < 0.01. **P < 0.05. *P < 0.1.
Associations of Patient Characteristics With Discordance Between Perceived and Preferred Roles in Decision-Making
Age had a negative association (β = −0.02, P < 0.01) such that older patients were less likely to report being involved in decision-making less than they preferred. Male patients (β = 0.43, P = 0.02) and those with higher education (β = 0.04, P < 0.01) were more likely to report being involved more than they preferred (Table 3). Complete case analysis resulted in the same findings (Table S5, Supplementary Material).
Table 3.
Multinomial Logistic Regression: Associations of Patient Characteristics With Discordance Between Perceived and Preferred Roles (Reference: Concordance), N = 1506
| Involved Less Than Preferred | Involved More Than Preferred | |
|---|---|---|
| Gender (Ref: Female) | ||
| Male | 0.13 | 0.43** |
| Missing | −12.67 | −12.40 |
| Marital status (Ref: Single) | ||
| Married | 0.29 | 0.09 |
| Missing | 1.07 | 17.26 |
| Age (years) | −0.02*** | −0.009 |
| Education (years) | ||
| Education | 0.02 | 0.04*** |
| Education (missing) | 0.09 | 0.04 |
| Self-reported socioeconomic status (Ref: Low income) | ||
| Lower-middle income | −0.004 | 0.07 |
| Upper income | 0.19 | −0.16 |
| Missing | −12.46 | 0.47 |
| Minority-majority group (Ref: Majority) | ||
| Minority/disadvantaged | 0.48* | −0.03 |
| Missing | 1.01* | 0.51 |
| Awareness of advanced stage of cancer (Ref: Unaware) | ||
| Aware | 0.15 | 0.02 |
| Duration of knowing cancer (Ref: Less than 6 months) | ||
| 6 months to 1 year | −0.23 | 0.21 |
| More than 1 year | −0.11 | 0.39** |
| Missing | 0.27 | 0.38 |
| Cancer type (Ref: Other types) | ||
| Lung | −0.08 | 0.16 |
| Breast | 0.44* | 0.45* |
| Colorectal | −0.11 | 0.48* |
| Country (Ref: India) | ||
| Bangladesh | 0.70** | 1.03*** |
| China | 1.42*** | 0.85*** |
| Sri Lanka | −1.27** | −1.57*** |
| Vietnam | 1.82*** | 0.99*** |
| Constant | −2.21*** | −2.58*** |
P < 0.01. **P < 0.05. *P < 0.1.
Associations of Perceived Roles in Decision-Making With Quality of Life and Perceived Quality of Care
Utilizing the joint test of all categories of perceived decision-making roles in the five regressions returned a P-value <0.01, suggesting significant associations of perceived roles with quality of life and perceived quality of care (Table 4 and Table S6, Supplementary Material). Compared to no patient involvement, physician/family-led decision-making was associated with higher perceived quality of care coordination (β = 6.53, P = 0.03). Joint decision-making was associated with higher social (β = 2.49, P < 0.01) and spiritual well-being (β = 2.64, P < 0.01), and higher perceived quality of physician communication (β = 9.73, P < 0.01) and care coordination (β = 13.96, P < 0.01; Table 4). Patient-led decision-making was associated with higher social (β = 0.89, P = 0.03) and spiritual well-being (β = 2.71, P < 0.01), and higher perceived quality of care coordination (β = 5.14, P = 0.05). On the other hand, patient-alone decision-making was associated with lower emotional (β = −1.43, P < 0.01), social (β = −2.39, P < 0.01), and spiritual well-being (β = −2.98, P < 0.01). A score of 0.8 and 1.9 in mean differences is considered a medium effect for social well-being and emotional well-being, respectively. 33 Our findings show more than medium effect for social well-being and close to medium effect for emotional well-being. For spiritual well-being and perceived quality of physician communication and care coordination, the effects sizes were much smaller than one standard deviation for each scale.
Table 4.
Multivariate Linear Regressions: Associations of Perceived Roles in Decision-Making With Quality of Life and Perceived Quality of Care, N = 1506 a
| Emotional Well-Bring | Social Well-Being | Spiritual Well-Being | Quality of Physician Communication | Quality of Coordination of Care | |
|---|---|---|---|---|---|
| Role in decision-making (Reference: No patient involvement) | |||||
| Physician/Family led | |||||
| Beta | −0.28 | 0.16 | 1.33 | 1.52 | 6.53** |
| P value | 0.604 | 0.747 | 0.104 | 0.627 | 0.031 |
| Joint decision | |||||
| Beta | −0.63 | 2.49*** | 2.64*** | 9.73*** | 13.96*** |
| P value | 0.105 | <0.001 | <0.001 | <0.001 | <0.001 |
| Patient led | |||||
| Beta | 0.21 | 0.89** | 2.71*** | −0.98 | 5.14** |
| P value | 0.647 | 0.033 | <0.001 | 0.715 | 0.049 |
| Patient only | |||||
| Beta | −1.43*** | −2.39*** | −2.98*** | −2.36 | −0.21 |
| P value | 0.007 | <0.001 | <0.001 | 0.444 | 0.945 |
| Critical significance level after using Bonferroni method | 0.002 | ||||
| Breusch-Pagan test of residuals | <0.001 | ||||
| Joint test of significance for decision-making | <0.001 | ||||
These models are controlled for gender, marital status, age, education, socioeconomic status, ethnicity, awareness of advanced stage of cancer, and country of recruitment.
P < 0.01. **P < 0.05. *P < 0.1.
To account for multiple comparisons and control for Type 1 error inflation, we also used the Bonferroni method. 34 The corrected α level after using the Bonferroni method would be 0.002, where the critical significance level (0.05) was divided by the number of statistical tests. 25 The associations of physician/family-led decision-making (with quality of care coordination) and patient-led decision-making (with social well-being and quality of care coordination) were no longer significant.
The results were similar with slightly larger effect sizes in the unadjusted analyses. The largest differences between the unadjusted and adjusted (i.e., multivariate) effects were observed for the associations of physician/family-led decision-making (Δβ = 1.29), joint decision-making (Δβ = 1.53), and patient-led decision-making (Δβ = 0.95) with perceived quality of care coordination (Table S7, Supplementary Material). The complete case analyses also resulted in similar findings as those from the analyses of all participants including the missing data. The largest effect size difference (0.58) was observed for the association between joint decision-making and quality of physician communication (Table S8, Supplementary Material).
Discussion
The main aim of this study was to examine the decision-making roles of the family, physician, and patient himself or herself as perceived by patients in five LMICs in Asia, namely, Bangladesh, China, India, Sri Lanka, and Vietnam, and the associations of these roles with patient quality of life and perceived quality of care. Our findings show that the most commonly reported perceived and preferred decision-making role in all countries was no patient involvement. This is likely due to the fact that countries involved in this study can be identified as collectivistic societies, where the family is a main stakeholder in decisions5,35–38 and a more paternalistic view of physicians is prevalent. 37 These findings suggest that despite the evidence on increasing support for and promotion of SDM in high-income Asian countries,39–41 a passive role in decision-making may still be commonly experienced and preferred among advanced cancer patients in low and middle income countries in Asia.
Despite most patients reporting no patient involvement, majority of participants (73%) perceived their participation in decision-making at a level concordant with their preferences, with Sri Lanka having the highest percentage of such participants (95%) and Vietnam the lowest (54%). This is an interesting finding given that Sri Lanka had the highest percentage of no-patient involvement as perceived role, but at the same time the highest percentage of concordant roles. These findings suggest that SDM may not necessarily be desired by substantial number of patients in these countries and that not all patients value autonomy equally. 42 Future research could investigate the reasons behind patients’ preferences for lower levels of involvement in decision-making, and whether this is due to the lack of awareness regarding their decision-making rights or the absence of a conducive setting for shared decisions.
Our study found that male patients were more likely to perceive a patient-led or patient-only decision-making process than no patient involvement. This is unsurprising as males tend to have more dominant roles (i.e., main or sole breadwinner, “head” of the house) in low- or middle-income Asian societies compared to females. Higher education, being aware of advanced cancer stage, and knowledge of cancer diagnosis for more than 1 year were associated with higher levels of patient involvement in decision-making. These variables all indicate having more knowledge and/or experience with cancer. Patients from minority/disadvantaged groups were more likely to report a physician/family-led decision-making, and less likely to report a patient-only decision-making. This finding is consistent with previous studies.13,15,16 A possible explanation for this may be that those from migrant or disadvantaged backgrounds may be less self-efficacious or confident when communicating with their health care providers, which in turn may increase their reliance on their family members or physicians for decision-making support. 15
A puzzling finding was that lower-middle-income and upper-income patients (v. low-income patients) were more likely to report physician/family-led decision-making and less likely to report patient-alone decision-making. This might be because those with better socioeconomic status are more likely to have better social support system and receive better support from their physicians and family members, or more likely to trust and rely on modern medicine compared to patients with lower socioeconomic status.
Overall findings suggest that those coming from socially advantaged groups (male, educated, nonminority) were more likely to report higher levels of involvement in decision-making. Consistent with these findings, we also found that advantaged groups, such as males, older patients, and those with higher education, were more likely to be involved in decision-making more than they preferred.
Compared to no patient involvement, joint decision-making was associated with higher social and spiritual well-being. This suggests that patients experiencing collaborative decision-making with their caregivers and/or physicians feel that they have meaningful and positive social relationships. For spiritual well-being, making their own care decisions might have allowed patients to explore and achieve treatment goals consistent with their faith, and in the process find meaning. Joint decision-making was also associated with higher perceived quality of physician communication and care coordination. This finding points to SDM being a potential factor in patient satisfaction with care. Patients who are actively involved in decision-making may be more likely to clarify treatment-related uncertainties, ensuring that their treatments are in line with their preferences and values. This would allow them to experience or perceive better communication with their physicians and better healthcare in general.
Consistent with our hypothesis, patient-alone decision-making was associated with lower social, emotional, and spiritual well-being. This might be due to the fact that in collectivistic Asian societies like the ones studied in this article, those who are sick tend to be cared for by their family or communities, and this care comprises the duty of decision-making. Experiencing or perceiving making decisions alone may cause people in these societies to feel burdened, isolated, or uncared for, especially considering the complexity of decision-making in advanced cancer.
Limitations
There are several limitations of the study. First, the study design was cross-sectional and hence did not allow drawing of causal conclusions. Second, although we targeted major public hospitals in the study counties, the specific hospitals were selected through profession networks based on convenience. Thus, the services the study hospitals provide and care needs by their patients are likely to be different across the different sites included in the study as well as different than those in the other public and private hospitals within the same country. We also used convenience sampling for patient recruitment. Therefore, the results may not be generalizable to other hospitals in the study countries or other countries in the region. Third, we recruited patients who are aware of their cancer diagnosis. Lack of diagnostic awareness is quite common in Asian countries, and experiences of these patients in decision-making might be very different from those who are aware of their cancer. Last, we used a subjective measure of socioeconomic status as a control variable. The subjective measures of socioeconomic status were found to be predictors of health outcomes in previous studies, and also allowed us to use a comparable measure of socioeconomic status across multiple countries. 43
Conclusions
To the best of our knowledge, this study is the first to examine the associations of perceived roles in decision-making and patient outcomes among advanced cancer patients in the low- and middle-income countries studied in this article. Our findings are important as they highlight the likelihood that some cancer patients in these countries may not be involved in decision-making, and do not report involvement to be their preference. Despite this, we found that joint decision-making was associated with higher well-being and perceived quality of care. We also found that socially disadvantaged groups such as females, lower educated, and those from minority groups were more likely to report lower levels involvement in decision-making. We recommend that care teams explain the benefits of SDM to their patients and encourage them, especially those from socially disadvantaged groups, to participate in decision-making. Patients should feel supported throughout the decision-making process and every effort should be made to ensure that they do not find the responsibility of decision-making overwhelming.
Supplemental Material
Supplemental material, sj-docx-1-mpp-10.1177_23814683211061398 for Patient-Reported Roles in Decision-Making Among Asian Patients With Advanced Cancer: A Multicountry Study by Semra Ozdemir, Chetna Malhotra, Irene Teo, Si Ning Germaine Tan, Wei Han Melvin Wong, Anjum S. Khan Joad, Thushari Hapuarachchi, Gayatri Palat, Pham Nguyen Tuong, Sushma Bhatnagar, Rubayat Rahman, Lubna Mariam, Xiaohong Ning and Eric Andrew Finkelstein in MDM Policy & Practice
Acknowledgments
We would like to thank the APPROACH Study Group for helping with the APPROACH study conducted in all sites in this study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Lien Centre for Palliative Care.
Authors’ Note: Reasonable requests to access underlying research materials may be made to the corresponding author.
Research Ethics and Patient Consent: The APPROACH study was approved by the Institutional Review Board of the National University of Singapore (Reference: B-15-319) as well as the ethics committees of each participating hospital. All participants provided informed consent to the study.
ORCID iDs: Semra Ozdemir  https://orcid.org/0000-0001-7556-1601
https://orcid.org/0000-0001-7556-1601
Si Ning Germaine Tan  https://orcid.org/0000-0001-6357-9521
https://orcid.org/0000-0001-6357-9521
Wei Han Melvin Wong  https://orcid.org/0000-0003-2882-7117
https://orcid.org/0000-0003-2882-7117
Supplemental Material: Supplemental material for this article is available on the Medical Decision Making Policy & Practice website at https://journals.sagepub.com/home/mpp.
Contributor Information
Semra Ozdemir, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore; Saw Swee Hock School of Public Health, National University of Singapore, Singapore.
Chetna Malhotra, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore.
Irene Teo, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore.
Si Ning Germaine Tan, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore.
Wei Han Melvin Wong, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore.
Anjum S. Khan Joad, Department of Palliative Care, Bhagwan Mahaveer Cancer Hospital and Research Centre, Jaipur, Rajasthan, India.
Thushari Hapuarachchi, National Cancer Institute, Apeksha Hospital, Maharagama, Sri Lanka.
Gayatri Palat, Department of Pain and Palliative Medicine, MNJ Institute of Oncology and Regional Cancer Centre, Hyderabad, India; Two Worlds Cancer Collaboration-INCTR, Vancouver, British Columbia, Canada; Palliative Access Program, MNJ Institute of Oncology and Regional Cancer Centre, Hyderabad, India.
Pham Nguyen Tuong, Oncology Center, Hue Central Hospital, Hue city, Vietnam.
Sushma Bhatnagar, Palliative Access Program, MNJ Institute of Oncology and Regional Cancer Centre, Hyderabad, India.
Rubayat Rahman, Centre for Palliative Care, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Lubna Mariam, Radiation Oncology, National Institute of Cancer Research and Hospital, Dhaka, Bangladesh.
Xiaohong Ning, Department of Geriatrics, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China.
Eric Andrew Finkelstein, Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; Health Services and System Research, Duke-NUS Medical School, Singapore; Saw Swee Hock School of Public Health, National University of Singapore, Singapore; Duke Global Health Institute, Duke University, Durham, North Carolina.
References
- 1. Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. National Academies Press; 2013. [PubMed] [Google Scholar]
- 2. Beaver K, Luker KA, Owens RG, Leinster SJ, Degner LF, Sloan JA. Treatment decision-making in women newly diagnosed with breast cancer. Cancer Nurs. 1996;19(1):8–19. [DOI] [PubMed] [Google Scholar]
- 3. Bruera E, Willey JS, Palmer JL, Rosales M. Treatment decisions for breast carcinoma: patient preferences and physician perceptions. Cancer. 2002;94(7):2076–80. [DOI] [PubMed] [Google Scholar]
- 4. Degner LF, Sloan JA. Decision-making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45(9):941–50. [DOI] [PubMed] [Google Scholar]
- 5. Chattopadhyay S, Simon A. East meets West: cross-cultural perspective in end-of-life decision-making from Indian and German viewpoints. Med Health Care Philos. 2008;11(2):165–74. [DOI] [PubMed] [Google Scholar]
- 6. Tai MCT, Tsai TP. Who makes the decision? Patient’s autonomy vs paternalism in a Confucian society. Croat Med J. 2003;44(5):558–61. [PubMed] [Google Scholar]
- 7. Claramita M, Utarini A, Soebono H, Van Dalen J, Van der Vleuten C. Doctor-patient communication in a Southeast Asian setting: the conflict between ideal and reality. Adv Health Sci Educ Theory Pract. 2011;16(1):69–80. doi: 10.1007/s10459-010-9242-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mori M, Morita T. End-of-life decision-making in Asia: a need for in-depth cultural consideration. Palliat Med. Published online January 20, 2020. doi:10.1177/0269216319896932 [DOI] [PubMed] [Google Scholar]
- 9. Mo HN, Shin DW, Woo JH, et al. Is patient autonomy a critical determinant of quality of life in Korea? End-of-life decision-making from the perspective of the patient. Palliat Med. 2012;26(3):222–31. [DOI] [PubMed] [Google Scholar]
- 10. Tariman JD, Berry D, Cochrane B, Doorenbos A, Schepp K. Preferred and actual participation roles during health care decision-making in persons with cancer: a systematic review. Ann Oncol. 2010;21(6):1145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yennurajalingam S, Rodrigues LF, Shamieh OM, et al. Decisional control preferences among patients with advanced cancer: an international multicenter cross-sectional survey. Palliat Med. 2018;32(4):870–80. [DOI] [PubMed] [Google Scholar]
- 12. Sainio C, Lauri S, Eriksson E. Cancer patients’ views and experiences of participation in care and decision-making. Nurs Ethics. 2001;8(2):97–113. doi:10.1177/096973300100800203 [DOI] [PubMed] [Google Scholar]
- 13. Murray E, Pollack L, White M, Lo B. Clinical decision-making: patients’ preferences and experiences. Patient Educ Couns. 2007;65(2):189–96. doi: 10.1016/j.pec.2006.07.007 [DOI] [PubMed] [Google Scholar]
- 14. Chong JA, Quah YL, Yang GM, Menon S, Radha Krishna LK. Patient and family involvement in decision-making for management of cancer patients at a centre in Singapore. BMJ Support Palliat Care. 2015;5(4):420–6. doi: 10.1136/bmjspcare-2012-000323 [DOI] [PubMed] [Google Scholar]
- 15. Mead EL, Doorenbos AZ, Javid SH, et al. Shared decision making for cancer care among racial and ethnic minorities: a systematic review. Am J Public Health. 2013;103(12):e15–e29. doi: 10.2105/ajph.2013.301631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shaw J, Zou X, Butow P. Treatment decision-making experiences of migrant cancer patients and their families in Australia. Patient Educ Couns. 2015;98(6):742–7. doi: 10.1016/j.pec.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 17. Hack TF, Pickles T, Ruether JD, et al. Predictors of distress and quality of life in patients undergoing cancer therapy: impact of treatment type and decisional role. Psychooncology. 2010;19(6):606–16. [DOI] [PubMed] [Google Scholar]
- 18. Orom H, Biddle C, Underwood W, 3rd, Nelson CJ, Homish DL. What is a “Good” treatment decision? Decisional control, knowledge, treatment decision-making, and quality of life in men with clinically localized prostate cancer. Med Decis Making. 2016;36(6):714–25. doi: 10.1177/0272989x16635633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blanchard CG, Labrecque MS, Ruckdeschel JC, Blanchard EB. Information and decision-making preferences of hospitalized adult cancer patients. Soc Sci Med. 1988;27(11):1139–45. doi: 10.1016/0277-9536(88)90343-7 [DOI] [PubMed] [Google Scholar]
- 20. Kashaf MS, McGill E. Does shared decision-making in cancer treatment improve quality of life? A systematic literature review. Med Decis Making. 2015;35(8):1037–48. doi: 10.1177/0272989X15598529 [DOI] [PubMed] [Google Scholar]
- 21. Hölzel LP, Kriston L, Härter M. Patient preference for involvement, experienced involvement, decisional conflict, and satisfaction with physician: a structural equation model test. BMC Health Serv Res. 2013;13(1):231. doi: 10.1186/1472-6963-13-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Suzuki M. Quality of life, uncertainty, and perceived involvement in decision-making in patients with head and neck cancer. Oncol Nurs Forum. 2012;39(6):541–8. [DOI] [PubMed] [Google Scholar]
- 23. Kehl KL, Landrum MB, Arora NK, et al. Association of actual and preferred decision roles with patient-reported quality of care: shared decision making in cancer care. JAMA Oncol. 2015;1(1):50–8. doi: 10.1001/jamaoncol.2014.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med. 2001;52(12):1865–78. [DOI] [PubMed] [Google Scholar]
- 25. Hawley ST, Jagsi R. Shared decision making in cancer care: does one size fit all? JAMA Oncol. 2015;1(1):58–9. doi: 10.1001/jamaoncol.2014.186 [DOI] [PubMed] [Google Scholar]
- 26. International Agency for Research on Cancer, World Health Organisation. Viet Nam. Available from: https://gco.iarc.fr/today/data/factsheets/populations/704-viet-nam-fact-sheets.pdf [Google Scholar]
- 27. International Agency for Research on Cancer, World Health Organisation. Sri Lanka. Available from: https://gco.iarc.fr/today/data/factsheets/populations/144-sri-lanka-fact-sheets.pdf [Google Scholar]
- 28. International Agency for Research on Cancer, World Health Organisation. India. Available from: https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf [Google Scholar]
- 29. International Agency for Research on Cancer, World Health Organisation. China. Available from: https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf [Google Scholar]
- 30. International Agency for Research on Cancer, World Health Organisation. Bangladesh. Available from: https://gco.iarc.fr/today/data/factsheets/populations/50-bangladesh-fact-sheets.pdf [Google Scholar]
- 31. Malin JL, Ko C, Ayanian JZ, et al. Understanding cancer patients’ experience and outcomes: development and pilot study of the Cancer Care Outcomes Research and Surveillance patient survey. Support Care Cancer. 2006;14(8):837–48. doi: 10.1007/s00520-005-0902-8 [DOI] [PubMed] [Google Scholar]
- 32. Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28(27):4154–61. doi: 10.1200/jco.2009.27.3268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. King MT, Cella D, Osoba D, et al. Meta-analysis provides evidence-based interpretation guidelines for the clinical significance of mean differences for the FACT-G, a cancer-specific quality of life questionnaire. Patient Relat Outcome Meas. 2010;1:119–26. doi: 10.2147/PROM.S10621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Aickin M, Gensler H. Adjusting for multiple testing when reporting research results: the Bonferroni vs Holm methods. Am J Public Health. 1996;86(5):726–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Calimag MMP. Community-based palliative care for chronic cancer patients in the Philippines. In: Silbermann M, ed. Palliative Care for Chronic Cancer Patients in the Community: Global Approaches and Future Applications. Springer; 2021. p. 563–71. [Google Scholar]
- 36. Chiu TY, Hu WY, Chen CY. Prevalence and severity of symptoms in terminal cancer patients: a study in Taiwan. Support Care Cancer. 2000;8(4):311–3. [DOI] [PubMed] [Google Scholar]
- 37. Xing YF, Lin JX, Li X, et al. Advance directives: cancer patients’ preferences and family-based decision-making. Oncotarget. 2017;8(28):45391–8. doi: 10.18632/oncotarget.17525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zhai H, Lavender C, Li C, Wu H, Gong N, Cheng Y. Who decides? Shared decision making among colorectal cancer surgery patients in China. Support Care Cancer. 2020;28(11):5353–61. doi: 10.1007/s00520-020-05391-3 [DOI] [PubMed] [Google Scholar]
- 39. Elwyn TS, Fetters MD, Gorenflo DW, Tsuda T. Cancer disclosure in Japan: historical comparisons, current practices. Soc Sci Med. 1998;46(9):1151–63. [DOI] [PubMed] [Google Scholar]
- 40. Sheu SJ, Huang SH, Tang FI, Huang SL. Ethical decision-making on truth telling in terminal cancer: medical students’ choices between patient autonomy and family paternalism. Med Educ. 2006;40(6):590–8. [DOI] [PubMed] [Google Scholar]
- 41. Yun YH, Lee CG, Kim Sy, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol. 2004;22(2):307–14. [DOI] [PubMed] [Google Scholar]
- 42. Winzelberg GS, Hanson LC, Tulsky JA. Beyond autonomy: diversifying end-of-life decision-making approaches to serve patients and families. J Am Geriatr Soc. 2005;53(6):1046–50. doi: 10.1111/j.1532-5415.2005.53317.x [DOI] [PubMed] [Google Scholar]
- 43. Zang E, Bardo AR. Objective and subjective socioeconomic status, their discrepancy, and health: evidence from East Asia. Soc Indic Res. 2019;143(2):765–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-mpp-10.1177_23814683211061398 for Patient-Reported Roles in Decision-Making Among Asian Patients With Advanced Cancer: A Multicountry Study by Semra Ozdemir, Chetna Malhotra, Irene Teo, Si Ning Germaine Tan, Wei Han Melvin Wong, Anjum S. Khan Joad, Thushari Hapuarachchi, Gayatri Palat, Pham Nguyen Tuong, Sushma Bhatnagar, Rubayat Rahman, Lubna Mariam, Xiaohong Ning and Eric Andrew Finkelstein in MDM Policy & Practice



