Abstract
Background:
The degree of knee hyperextension in isolation has not been studied in detail as a risk factor that could lead to increased looseness or graft failure after anterior cruciate ligament (ACL) reconstruction.
Purpose:
To analyze whether more than 5° of passive knee hyperextension is associated with worse functional outcomes and greater risk of graft failure after primary ACL reconstruction with hamstring tendon autograft.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A cohort of patients who had primary ACL reconstruction with hamstring tendon autografts was divided into 2 groups based on passive contralateral knee hyperextension greater than 5° (hyperextension group) and less than 5° (control group) of hyperextension. Groups were matched by age, sex, and associated meniscal tears. The following data were collected and compared between the groups: patient data (age and sex), time from injury to surgery, passive knee hyperextension, KT-1000 arthrometer laxity, pivot shift, associated meniscal injury and treatment (meniscectomy or repair), contralateral knee ligament injury, intra-articular graft size, follow-up time, occurrence of graft failure, and postoperative Lysholm knee scale and International Knee Documentation Committee subjective form scores.
Results:
Data from 358 patients initially included in the study were analyzed; 22 were excluded because the time from injury to surgery was greater than 24 months, and 22 were lost to follow-up. From the cohort of 314 patients, 102 had more than 5° of knee hyperextension. A control group of the same size (n = 102) was selected by matching among the other 212 patients. Significant differences in the incidence of graft failure (14.7% vs 2.9%; P = .005) and Lysholm knee scale score (86.4 ± 9.8 vs 89.6 ± 6.1; P = .018) were found between the 2 groups.
Conclusion:
Patients with more than 5° of contralateral knee hyperextension submitted to single-bundle ACL reconstruction with hamstring tendons have a higher failure rate than patients with less than 5° of knee hyperextension.
Keywords: anterior cruciate ligament, knee hyperextension, graft failure, hamstring
The anterior cruciate ligament (ACL) is the most frequently injured ligament of the knee, and ACL injuries commonly keep athletes from sports practice. 28 About 200,000 ACL reconstruction surgeries are performed each year in the United States. 5,28 Even though nonoperative treatment or ACL repair can be performed in specific situations, 6,30 the most accepted treatment for an ACL injury in active populations is reconstruction. Overall, ACL reconstruction presents good results in functional scales and a low failure rate. 15 However, some specific populations are known to have a higher risk for a failed reconstruction, including young patients involved in sports activities, patients with hyperlaxity, and patients with major preoperative knee anterior and anterolateral instabilities. 11,16
The outcome of ACL reconstruction surgery depends on many factors. Surgical technique and proper graft positioning, restoration of anterior and rotatory knee stability, and restoration of full range of motion and muscle strength are some of the factors that affect the final function of the knee in the postoperative period. 2 Even though some factors such as technique and graft options are modified by the surgeon, patients might have intrinsic factors of bony morphology and hyperlaxity that the surgeon cannot modify. 13,27
There is a concern that higher degrees of hyperextension may lead to increased looseness or graft failure after ACL reconstruction. Markolf et al 19,20 showed there are high forces generated in the ACL graft during hyperextension, and this might account for ACL graft stretching and failure. One cohort study carried out by Benner et al 2 concluded that there is no increase in rupture or insufficiency of the ACL graft in patients with a high degree of hyperextension. However, the study evaluated only patients who received patellar tendon autografts; no other type of graft was used. Another cohort study, from the Multicenter ACL Revision Study (MARS) Group, evaluated patients who underwent ACL reconstruction revision and concluded that a passive hyperextension of the knee greater than 5° was an important predictor of graft failure. 21 To the authors’ knowledge, this conclusion is not yet applicable to primary ACL reconstructions. Only a few authors performed the same evaluation in primary ACL reconstruction cases with double-bundle and single-bundle hamstring autografts. Even though generalized joint laxity is known to be an important risk factor for ACL reconstruction failure, the degree of knee hyperextension in isolation has not been studied in detail. Larson et al 16 showed a failure rate of 24.4% and Helito et al 11 a failure rate of 21.7% when evaluating patients with higher Beighton scores; however, none of these authors isolated knee hyperextension in the analysis.
Therefore, the purpose of this study was to analyze whether a high degree (more than 5°) of passive hyperextension of the knee was associated with worse functional outcomes and greater risk of graft failure after primary ACL reconstructions with hamstring tendon autografts in adult patients. Our hypothesis was that patients with more than 5° of passive knee hyperextension would have a higher rate of graft tear/failure and lower subjective scores after surgery than patients with less knee extension.
Methods
The study was approved by the ethics committee of our institution, and informed consent was obtained. This was a retrospective cohort study designed to assess the functional outcome of patients undergoing primary ACL reconstruction with hamstring tendon autografts. Patients who underwent surgery from June 2013 to June 2018 were included. Inclusion criteria were patients aged between 18 and 60 years, with acute or chronic ACL injury, who underwent anatomic, single-bundle, intra-articular ACL reconstruction with autologous hamstring autografts with a minimum follow-up of 2 years. Patients with associated injuries that required additional surgical procedures, such as peripheral ligament reconstructions (including anterolateral ligament reconstruction or iliotibial band tenodesis), posterior cruciate ligament reconstruction, osteotomy, and cartilage procedures and patients with previous contralateral knee injury were not included for this evaluation. Patients who had surgery more than 24 months after the ACL tear and patients lost to follow-up were excluded.
ACL reconstruction was performed using the outside-in technique for preparing the femoral tunnel. The tunnel was positioned close to the anteromedial bundle of the ACL in the lateral femoral condyle. The tibial tunnel was created at the center of the ACL footprint. The hamstring graft was passed from the tibia to the femur, and fixation was performed with absorbable interference screws. The femur was fixed first and the tibia second, with around 30° of knee flexion.
Data were collected from medical records and databases of operated patients completed prospectively during normal patient follow-up. The following data were collected: patient data (age and sex), time from injury to surgery, passive knee hyperextension, KT-1000 arthrometer laxity, pivot shift, associated meniscal injury and treatment (meniscectomy or repair), contralateral knee ligament injury, intra-articular graft size, follow-up time, occurrence of graft failure, and postoperative Lysholm knee scale 3 and International Knee Documentation Committee (IKDC) subjective form scores. 10 Passive knee hyperextension was measured preoperatively (at the time of the surgical procedure and under anesthesia) using a goniometer in the contralateral knee to minimize the effects of the ACL injury on the affected knee, assuming both knees had the same degree of mobility before the ACL injury (Figure 1). Patients with a previous contralateral knee injury were not included. Graft failure was based on clinical ACL failure criteria (physical examination showing laxity with no clear endpoint for Lachman and anterior drawer tests [at least +2/+3] or pivot-shift positivity [at least +2/+3] associated with instability complaints) and when imaging showed a new graft rupture.
Figure 1.

Knee showing passive hyperextension, observed with the patient under anesthesia.
All patients who did not undergo meniscal repair followed the same rehabilitation protocol. No immobilization device of any type was used, and movement was not restricted. Patients were encouraged to walk as tolerated on the operated limb, and the range of motion was free and stimulated since the first day after surgery. In patients who underwent meniscal repair, the rehabilitation included weightbearing as tolerated with a knee brace and range of motion restricted from 0° to 90° for 4 weeks. After that, the protocol was similar to that for the other patients. The range of motion goal was to return the knee to the same contralateral range of motion, including the hyperextension degree. Full return to sports activities was not allowed until at least 8 months and only if the patient was evaluated with good muscular control.
A hyperextension group was formed comprised of patients with passive knee hyperextension. A control group with the same number of patients was selected by matching among the other patients of the cohort. The matching was performed using age (each patient in the case group was paired with a patient up to 5 years older or 5 years younger), sex, and associated meniscal tear. Physical examination parameters were not used to match patients as they could be influenced by the knee laxity of each patient. We also did not use Beighton classification for this study and focused only on the knee hyperextension parameters.
Continuous variables were reported as means and standard deviations for normal distributions and medians and interquartile ranges for non-normal distributions, according to the Shapiro-Wilk test and histogram analysis. Group comparisons were made using the Student t test or Mann-Whitney U test, according to the normality of the variable. Categorical variables were reported as absolute number and percentage within the group, and the Fisher’s test was used in the respective contingency tables.
No sample size estimation was performed, as all patients in our database who met the inclusion criteria were analyzed. A post hoc power calculation revealed an achieved power of 85% for graft failure, which was considered adequate for the study. Statistical significance was considered when the P < .05. We used SPSS Version 24 (IBM) and G*Power 3.1.9.3 (Erdfelder et al, Universität Düsseldorf, 2009) for the statistical analyses.
Results
A total of 358 patients were initially included in the study; 22 were excluded because the time from injury to surgery was greater than 24 months, and 22 were excluded because they had less than 24 months of follow-up (lost to follow-up). From our cohort of 314 patients, 102 had more than 5° of knee hyperextension. A control group of the same size (n = 102) was selected by matching among the other 212 patients (Figure 2).
Figure 2.
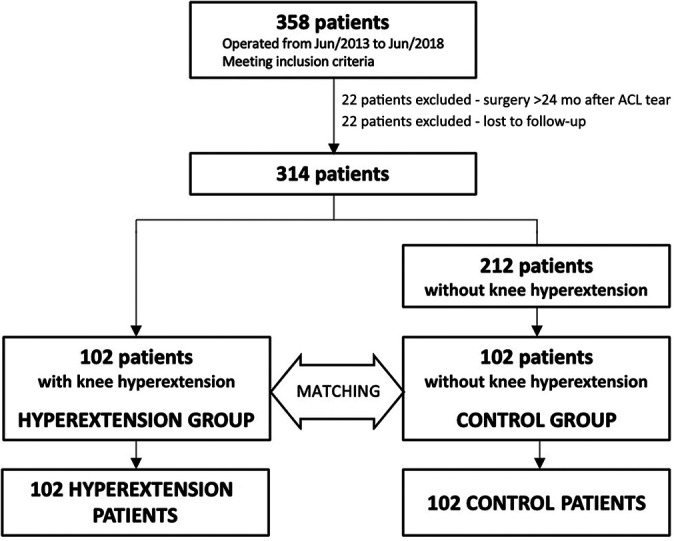
Flowchart of study participants. ACL, anterior cruciate ligament.
Data from 204 patients (102 patients in the hyperextension group and 102 patients in the control group) were evaluated. Patient characteristics and preoperative clinical data are shown in Table 1. Both groups were similar regarding all variables with the exception of passive knee hyperextension, which presented a mean of 1.6° ± 1.8° for the control group and 9.6° ± 3.1° for the hyperextension group (P < .001). Follow-up time was also higher in the hyperextension group by a mean difference of 3.3 months (P = .028).
Table 1.
Patient Characteristics and Preoperative Clinical Data a
| Control Group (n = 102) | Hyperextension Group (n = 102) | P Value | |
|---|---|---|---|
| Age, y | 31.5 ± 9.1 | 31.6 ± 9 | .753 |
| Female patients | 35 (34.3) | 35 (34.3) | |
| Time from injury to surgery, mo | 7.9 ± 6.5 | 7.9 ± 5.9 | .838 |
| KT-1000 arthrometer laxity, preoperative, mm | 7.5 ± 1.1 | 7.5 ± 1.2 | .727 |
| Pivot shift, preoperative, 0-3 | .261 | ||
| 1 | 28 (27.5) | 18 (17.6) | |
| 2 | 48 (47.1) | 55 (53.9) | |
| 3 | 26 (25.5) | 29 (28.4) | |
| Knee passive hyperextension, deg | 1.6 ± 1.8 | 9.6 ± 3.1 | <.001 |
| Associated meniscal injury | 28 (27.5) | 28 (27.5) | ≥.999 |
| Contralateral knee ligament injury | 2 (2) | 2 (2) | ≥.999 |
| Follow-up time, mo | 34.7 ± 12.8 | 38 ± 13.2 | .028 |
a Data are presented as mean ± SD or n (%). Bolded P value indicates a statistically significant difference between groups (P < .05).
A significant difference in the incidence of graft failure and Lysholm score between the 2 groups was found (Table 2). Subjective IKDC scores did not present any difference between the groups. Graft failure occurred at an incidence of 2.9% in the control group and 14.7% in the hyperextension group (P = .005). All patients evaluated with a graft failure were scheduled for revision surgery. The mean hyperextension for graft failure cases was 1.3° ± 1.5° for the control group and 9.3° ± 2.0° for the hyperextension group. There was no statistical difference in hyperextension between graft failures and nonfailures within each group (P = .667 for the control group and P = .384 for the hyperextension group). The Lysholm score was 89.6 ± 6.1 in the control group and 86.4 ± 9.8 in the hyperextension group (P = .018)
Table 2.
Outcomes a
| Control Group | Hyperextension Group | P Value | |
|---|---|---|---|
| Intra-articular graft size, mm | 7.8 ± 0.7 | 8.2 ± 0.8 | <.001 |
| Graft failure | 3 (2.9) | 15 (14.7) | .005 |
| KT-1000 arthrometer laxity, postoperative, mm | 2.0 ± 1.2 | 2.1 ± 1.4 | .833 |
| Pivot shift, postoperative, 0-3 | .876 | ||
| 0 | 62 (60.8) | 61 (59.8) | |
| 1 | 37 (36.3) | 36 (35.3) | |
| 2 | 3 (2.9) | 5 (4.9) | |
| Residual pivot shift | 40 (39.2) | 41 (40.2) | ≥.999 |
| IKDC subjective score | 87.9 ± 7.9 | 84.7 ± 11.6 | .141 |
| Lysholm score | 89.6 ± 6.1 | 86.4 ± 9.8 | .018 |
a Data are presented as mean ± SD or n (%). Bolded P values indicate a statistically significant difference between groups (P < .05). IKDC, International Knee Documentation Committee.
A significant difference was also found in the intra-articular graft size between the 2 groups, which was slightly larger in the hyperextension group (8.2 ± 0.8 mm vs 7.8 ± 0.7 mm; P < .001).
Discussion
This study showed that patients with preoperative knee hyperextension greater than 5° have a higher failure rate after an ACL reconstruction performed with hamstring grafts than patients with less than 5° or no hyperextension. This finding is important as it suggests that this type of graft should be used with caution as a first choice for this specific population or should be associated with an extra-articular augmentation procedure if chosen for primary ACL reconstruction. The difference in graft failure was significant, with a study power of 85% that corroborates the results.
Patients with generalized ligamentous hyperlaxity based on the Beighton classification are known to have a higher failure rate after ACL reconstruction. Recent studies by Larson et al 16 and Helito et al 11 showed failure rates above 20%, while the average failure for the general population is around 6% according to a systematic review published by Wright et al. 33 Helito et al 11 found a failure rate of 21.7% in reconstructions with hamstring grafts, and Larson et al 16 found a failure rate of 25% for hamstring grafts and 21.1% for bone–patellar tendon–bone (BTB) grafts. Kim et al 14 also reported an IKDC index of C and D in patients with hyperlaxity for reconstruction with both hamstring grafts (36.4%) and BTB grafts (20%). In a systematic review, Sundemo et al 29 also showed that generalized hyperlaxity leads to worse functional results. Despite the results above, few studies have evaluated only cases of knee hyperextension, outside the context of generalized ligamentous laxity, and its significance as an isolated risk factor for ACL failure is still controversial. Saita et al 24 suggested that because of their greater preoperative anterolateral rotational instability, cases with hyperextension could also have a higher failure rate, but Nagai et al 22 found no increase in anterior translation or internal knee rotation in the postoperative period of ACL reconstruction in cases of hyperextension. In an editorial published in 2018, Owens 23 pointed that the current literature presented conflicting results regarding knee hyperextension.
Ettinger et al 7 performed a study on cadavers and showed that a single-bundle ACL reconstruction in patients with hyperextension did not interfere with the postoperative extension values, unlike the double-bundle reconstruction that decreased the knee extension. These data are important because they show that single-bundle reconstruction does not impair knee motion in these cases, possibly unlike the double-bundle reconstruction. However, the average hyperextension studied by these authors was 4° to 5° for all groups, with no cases of greater hyperextension as in our study, in which the lower limit for the hyperextension group was 5°. As the study by Ettinger et al was carried out on cadavers, it was not possible to assess the clinical effect of this possible constriction. On the other hand, Saito et al 26 clinically evaluated patients with hyperextension of more or less than 10° submitted to double-bundle reconstruction with hamstring grafts and found greater loss of extension and greater partial laceration of the graft in patients with more than 10° of preoperative hyperextension. However, these authors did not find significant differences in the functional scores between the groups, showing that reconstruction with the double-bundle graft in these patients did not generate worse functional outcomes.
In a multicenter study, Ueki et al 31 concluded that hyperextension greater than 10° was related to the presence of residual pivot shift 12 months after the ACL reconstruction; despite having a short follow-up and a diversity of techniques, most of them were performed with double-bundle graft. These authors found only hyperextension and preoperative pivot shift as risk factors for postoperative rotational residual instability and suggest that in these situations, an eventual extra-articular surgical procedure associated with the ACL should be performed to obtain better functional results. The MARS Group also showed that hyperextension greater than 5° was considered an independent risk factor for failure in cases of revision ACL reconstruction. 21 On the other hand, Benner et al 2 concluded that there were no functional differences and failure rates in patients with knee hyperextension in a comparative study using only BTB grafts. These authors evaluated a group of patients with more than 6° of hypertension and another group with less than 3°, leaving patients with 4° and 5° out of the analysis.
In our study, we used the cutoff value of 5° for hyperextension based on the MARS Group study, since there is no precise definition in the current literature as to which degree of hyperextension can be considered as a risk factor for ACL reconstruction failure. Although some studies use 10° based on the Beighton classification—even though this classification value has been questioned recently 18 —cutoff values of 5° or 6° can also be found in the literature. According to our findings, hyperextension did not worsen the clinical anterior instability measured by KT-1000 or anterolateral instability measured by pivot-shift test, but it was an important risk factor for failure. If we consider that the diameter of the graft was 0.4 mm thicker in the hyperextension group and that, despite some controversy, as pointed by Wernecke et al, 32 graft diameters can be a potential risk factor for graft failure, it is possible that the difference in favor of the control group is even greater. 4,17 The Lysholm functional scale also showed a difference of 3.2 in favor of the control group, which, despite being statistically significant, tends to not be clinically significant since the minimum significance value for this scale is 8.9 points. 9
Considering our findings, which showed a 5 times higher failure rate in the hyperextension group, we believe that the hamstring graft should not be used in primary ACL reconstructions in patients with knee hyperextension greater than 5°. Owens 23 previously pointed out that “it is possible that graft choice may have an influence on the finding of increased laxity after ACL reconstruction in patients with hyperextension,” mainly based on the results of Kim et al 14 showing more pronounced laxity in patients undergoing hamstring graft reconstructions compared with BTB grafts. The current study presents more evidence to support this scenario. Although the hamstrings are the most used graft for ACL reconstructions worldwide, in these situations, we recommend the use of another option. Benner et al 2 showed satisfactory results using BTB grafts for a similar population, but there is still no established gold-standard graft for these situations. The addition of an anterolateral extra-articular augmentation may also be an alternative if the use of hamstring graft is chosen or mandatory for any reason. 1,25 Helito et al 11 showed that anterolateral ligament reconstruction in patients with ligamentous hyperlaxity reduced the failure rate from 21.7% to 3.3%. Both ALL reconstruction and iliotibial tract tenodesis could be used in this situation since both have good functional results and a low rate of complications according to recent studies. 8,12 Also, the rehabilitation program might have a role in this higher failure rate in the hyperextension population. It is possible that a program in which full extension is restricted with a knee brace in order to try to achieve less than 5° of hyperextension in the postoperative period could improve the results. However, so far, there are no data to fully support this.
The present study has some limitations. The sample was retrospectively analyzed; there was only a small difference in follow-up between the groups, although we believe that 3 months in the context of around 3 years is not clinically relevant; there was a difference in graft diameter between the groups, although the difference tended to favor the group with hyperextension, which had the worst results; use of the Tegner activity scale was absent in the analysis; and the 5° cutoff value used between groups was arbitrary, as there is no clear cutoff in the literature for this specific evaluation. Studies decreasing the cutoff value of knee hyperextension should now be carried out to assess whether any hyperextension can generate an increase in graft failures when using hamstring grafts or if there is a magic number that can be considered safe. Also, because we did not use the full Beighton score, it could be that the hyperextension numbers found were just a surrogate for Beighton scores greater than 6.
Conclusion
The study results indicated that patients with more than 5° of knee hyperextension treated with a single-bundle ACL reconstruction with hamstring grafts have a higher failure rate than patients with less than 5° of knee hyperextension.
Footnotes
Final revision submitted August 10, 2021; accepted August 24, 2021.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained (CAAE control No. 32727320.2.0000.0068/SGP 11257).
References
- 1. Ariel de Lima D, Helito CP, de Lima FRA, Leite JAD. Surgical indications for anterior cruciate ligament reconstruction combined with extra-articular lateral tenodesis or anterolateral ligament reconstruction. Rev Bras Ortop. 2018;53(6):661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Benner RW, Shelbourne KD, Gray T. The degree of knee extension does not affect postoperative stability or subsequent graft tear rate after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2016;44(4):844–849. [DOI] [PubMed] [Google Scholar]
- 3. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Richard Steadman J. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee. Am J Sports Med. 2009;37(5):890–897. doi:10.1177/0363546508330143 [DOI] [PubMed] [Google Scholar]
- 4. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 5. Dai B, Herman D, Liu H, Garrett WE, Yu B. Prevention of ACL injury, part I: injury characteristics, risk factors, and loading mechanism. Res Sports Med. 2012;20(3-4):180–197. [DOI] [PubMed] [Google Scholar]
- 6. Delaloye JR, Murar J, Vieira TD, et al. Combined anterior cruciate ligament repair and anterolateral ligament reconstruction. Arthrosc Tech. 2019;8(1):e23–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ettinger M, Petri M, Guenther D, et al. Anatomic double-bundle ACL reconstruction restricts knee extension in knees with hyperextension. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2057–2062. [DOI] [PubMed] [Google Scholar]
- 8. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY Study randomized clinical trial. Am J Sports Med. 2020;48(2):285–297. [DOI] [PubMed] [Google Scholar]
- 9. Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A. Research pearls: the significance of statistics and perils of pooling. Part 1: clinical versus statistical significance. Arthroscopy. 2017;33(6):1102–1112. [DOI] [PubMed] [Google Scholar]
- 10. Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 11. Helito CP, Sobrado MF, Giglio PN, et al. Combined reconstruction of the anterolateral ligament in patients with anterior cruciate ligament injury and ligamentous hyperlaxity leads to better clinical stability and a lower failure rate than isolated anterior cruciate ligament reconstruction. Arthroscopy. 2019;35(9):2648–2654. [DOI] [PubMed] [Google Scholar]
- 12. Helito CP, Sobrado MF, Giglio PN, et al. Surgical timing does not interfere on clinical outcomes in combined reconstruction of the anterior cruciate ligament and anterolateral ligament: a comparative study with minimum 2-year follow-up. Arthroscopy. 2021;37(6):1909–1917. doi:10.1016/j.arthro.2021.01.045 [DOI] [PubMed] [Google Scholar]
- 13. Jagodzinski M, Richter GM, Pässler HH. Biomechanical analysis of knee hyperextension and of the impingement of the anterior cruciate ligament: a cinematographic MRI study with impact on tibial tunnel positioning in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;8(1):11–19. [DOI] [PubMed] [Google Scholar]
- 14. Kim SJ, Moon HK, Kim SG, Chun YM, Oh KS. Does severity or specific joint laxity influence clinical outcomes of anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2010;468(4):1136–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krause M, Freudenthaler F, Frosch KH, Achtnich A, Petersen W, Akoto R. Operative versus conservative treatment of anterior cruciate ligament rupture. Dtsch Arztebl Int. 2018;115(51-52):855–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Larson CM, Bedi A, Dietrich ME, et al. Generalized hypermobility, knee hyperextension, and outcomes after anterior cruciate ligament reconstruction: prospective, case-control study with mean 6 years follow-up. Arthroscopy. 2017;33(10):1852–1858. [DOI] [PubMed] [Google Scholar]
- 17. Magnussen RA, Lawrence JTR, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 18. Malek S, Reinhold EJ, Pearce GS. The Beighton Score as a measure of generalised joint hypermobility. Rheumatol Int. 2021;41(10):1707–1716. doi:10.1007/s00296-021-04832-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. [DOI] [PubMed] [Google Scholar]
- 20. Markolf KL, Gorek JF, Kabo JM, Shapiro MS. Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–567. [PubMed] [Google Scholar]
- 21. MARS Group; Cooper DE, Dunn WR, Huston LJ, et al. Physiologic preoperative knee hyperextension is a predictor of failure in an anterior cruciate ligament revision cohort: a report from the MARS Group. Am J Sports Med. 2018;46(12):2836–2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nagai K, Gale T, Herbst E, et al. Knee hyperextension does not adversely affect dynamic in vivo kinematics after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):448–454. [DOI] [PubMed] [Google Scholar]
- 23. Owens BD. Recurvatum. Am J Sports Med. 2018;46(12):2833–2835. [DOI] [PubMed] [Google Scholar]
- 24. Saita Y, Schoenhuber H, Thiébat G, et al. Knee hyperextension and a small lateral condyle are associated with greater quantified antero-lateral rotatory instability in the patients with a complete anterior cruciate ligament (ACL) rupture. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):868–874. [DOI] [PubMed] [Google Scholar]
- 25. Saithna A, Daggett M, Helito CP, et al. Clinical results of combined ACL and anterolateral ligament reconstruction: a narrative review from the SANTI Study Group. J Knee Surg. 2021;34(9):962–970. doi:10.1055/s-0040-1701220 [DOI] [PubMed] [Google Scholar]
- 26. Saito K, Hatayama K, Terauchi M, Hagiwara K, Higuchi H, Takagishi K. Clinical outcomes after anatomic double-bundle anterior cruciate ligament reconstruction: comparison of extreme knee hyperextension and normal to mild knee hyperextension. Arthroscopy. 2015;31(7):1310–1317. [DOI] [PubMed] [Google Scholar]
- 27. Shen L, Jin ZG, Dong QR, Li LB. Anatomical risk factors of anterior cruciate ligament injury. Chin Med J. 2018;131(24):2960–2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Siegel L, Vandenakker-Albanese C, Siegel D. Anterior cruciate ligament injuries: anatomy, physiology, biomechanics, and management. Clin J Sport Med. 2012;22(4):349–355. [DOI] [PubMed] [Google Scholar]
- 29. Sundemo D, Hamrin Senorski E, Karlsson L, et al. Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. BMJ Open Sport Exerc Med. 2019;5(1):e000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Temponi EF, de Carvalho Júnior LH, Sonnery-Cottet B, Chambat P. Partial tearing of the anterior cruciate ligament: diagnosis and treatment. Rev Bras Ortop. 2015;50(1):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ueki H, Nakagawa Y, Ohara T, et al. Risk factors for residual pivot shift after anterior cruciate ligament reconstruction: data from the MAKS group. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3724–3730. [DOI] [PubMed] [Google Scholar]
- 32. Wernecke GC, Constantinidis A, Harris IA, Seeto BG, Chen DB, MacDessi SJ. The diameter of single bundle, hamstring autograft does not significantly influence revision rate or clinical outcomes after anterior cruciate ligament reconstruction. Knee. 2017;24(5):1033–1038. [DOI] [PubMed] [Google Scholar]
- 33. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]


