Abstract
Osteosarcoma (OS) is the most common primary non hematopoietic malignant tumor of bone with a strict histologic definition: the presence of unequivocal osteoid produced by neoplastic cells. Rare variants displaying low-grade histological features have been described; among which chondromyxoid fibroma-like (CMF-OS) is the rarest. However, despite its bland morphology; CMF-like OS has an aggressive clinical behavior and a poor prognosis. To the best of our knowledge, only 3 cases of CMF-OS have been previously reported in children. Because of its atypicality and scarcity; misdiagnosis is more likely to occur. Herein we describe a new case of CMF-OS in a 13 years old girl with fatal outcome. Diagnosis was based on focal malignant bone formation and correlation with imaging studies. The aim of the present case presentation is to raise awareness of this rare entity and to highlight the challenging diagnosis
Keywords: Pathology, case reports, neoplasms
Background
Osteosarcoma (OS) is the most common primary non hematopoietic malignant tumor of bone. It commonly presents in children and adolescents. 1 OS has a strict histologic definition: the presence of unequivocal osteoid produced by neoplastic cells. According to the predominant histologic pattern, anatomic location and histologic grade, OS is classified into several subtypes, with conventional OS being the most frequent. 2 Rare variants displaying low-grade histological features have been described; among which chondromyxoid fibroma-like (CMF-OS) is the rarest. 3 It is a hypocellular tumor with chondromyxoid stroma and inconspicuous osteoid, which can be misdiagnosed as a chondromyxoid fibroma. 4 However, despite its bland morphology; CMF-like OS has an aggressive clinical behavior with poor prognosis. 5 To the best of our knowledge, only 3 cases of CMF-OS have been previously reported in children.4,6,7 Because of its atypicality and scarcity; misdiagnosis is more likely to occur. 3 Herein we describe a new case of CMF-OS in a 13 years old girl with fatal outcome, to raise awareness of this rare entity presenting a highly challenging diagnosis.
Case Presentation
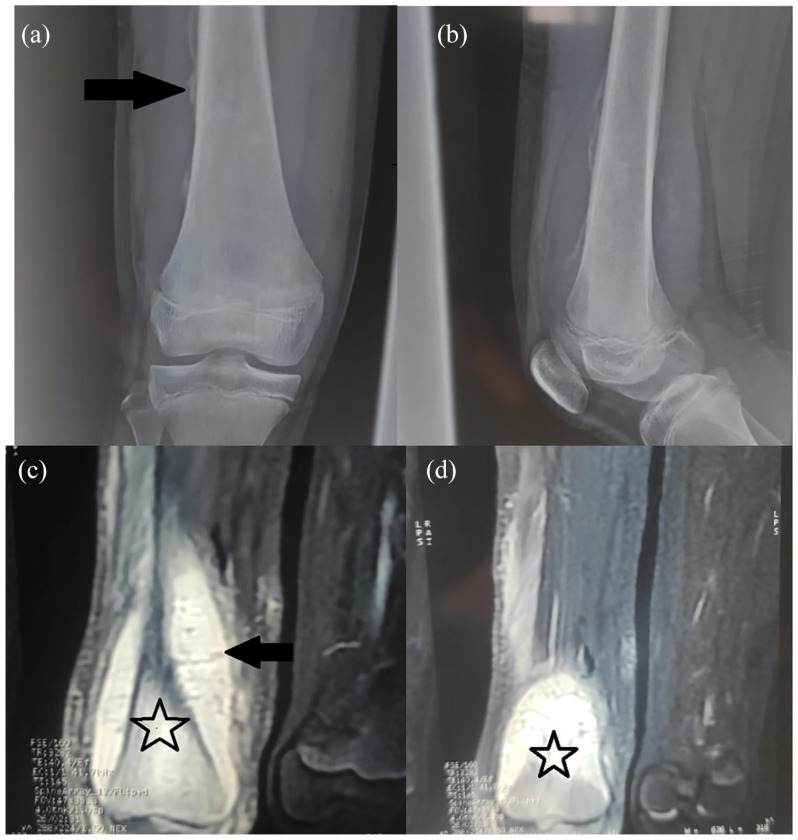
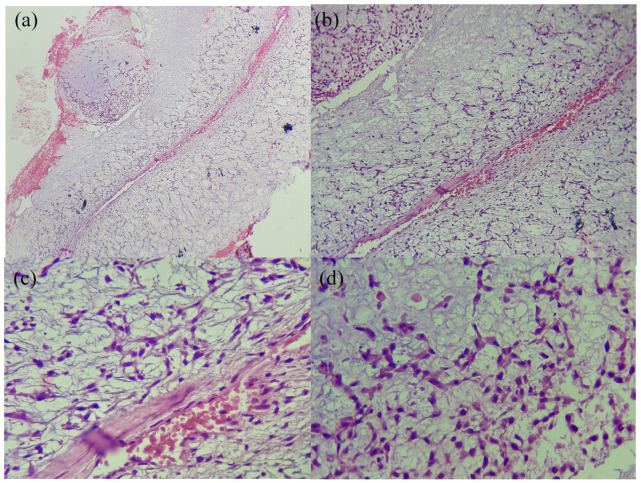
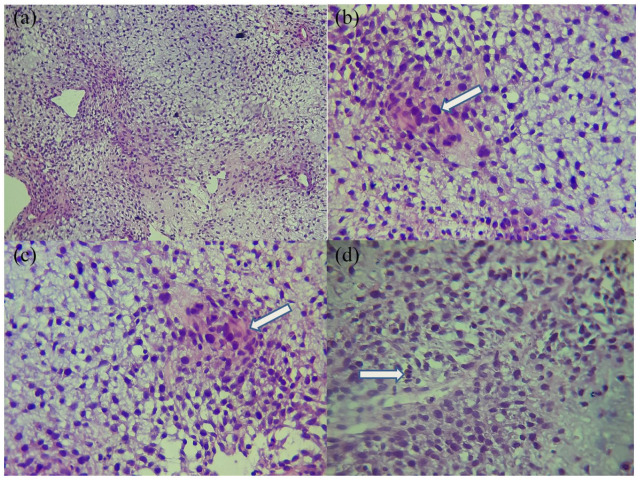
A 13-year-old previously healthy girl presented to the department of pediatric surgery with a worsening right thigh pain over the past 2 months; resulting in a limping. She didn’t experience weight loss or fatigue. There was no history of trauma. On physical examination, the distal part of the thigh was swollen and tender without motion’s limitation. Plain radiographs revealed a sunburst periosteal reaction (Figure 1). Two weeks later, CT scan showed a locally aggressive cortico-medullary diaphyso-metaphysal lesion, with pericortical extension measuring 10 cm. Surgical intracortical biopsy was carried out. The specimen consisted of 02 myxoid fragments. Histology showed a lobular tumor, with hypocellular centers and hypercellularity in the periphery of the lobules. Neoplastic cells were mildly pleomorphic, spindled to stellate-shaped, with abundant eosinophilic/clear cytoplasms. Nuclei were elongated, with diffuse chromatin, moderate hyperchromasia, inconspicuous nucleoli and low mitotic activity (1/10HPF (40×)) (Figure 2). The cells arranged in bluish myxoid background. Serial sections failed to demonstrate any evidence of osteoid neither necrosis. The diagnosis of chondromyxoid fibroma was retained. MRI was performed 2 weeks later, it demonstrated a locally advanced corticomedullary lesion in the distal femur with extension to soft tissue consistent with an osteosarcoma, which has rapidly increased in size (Figure 1). Because of the discordance between pathological and radiological findings, a second surgical biopsy was performed. Morphologically, the tumor showed similar features, but atypias were moderate to severe and mitotic count was estimated: 15 mitoses/10 HPF (Figure 3). Focal immature osteoid was observed. Given the aggressive clinical behavior, radiological findings, and histological features, the diagnosis of CMF-OS was made. Routine staging was negative for metastasis. The patient had 3 cycles of neoadjuvant chemotherapy combining doxorubicin and cisplatin. She died at home 2 weeks after the third cycle; the cause of death remained unknown as the patient died at home.
Figure 1.
Radiological findings (a and b): X-rays showing sunburst focal perisostal reaction. (c and d): MRI showing a cortico-medullary diaphyso-metaphysal lesion (white star), with pericortical extension and soft tissue invasion.
Figure 2.
Histological findings of the first biopsy: a lobular tumor, with peripheral hypercellularity. Cells are mildly pleomorphic, spindled to stellate-shaped. Nuclei are elongated, with diffuse chromatin, inconspicuous nucleoli, and low mitotic activity. (a): HE × 40B: HE × 100, (b) HE × 400, and (c) HE × 400.
Figure 3.
Histological findings of the second biopsy: a hypercellular lobular tumor (a). Cells are mildly pleomorphic, spindled to stellate-shaped. Nuclei are elongated, hyperchromatic, with diffuse chromatin (b), focal osteoid (c), and mitotic figures (d). (a) HE × 40 Lobules show hypo and hypercellular areas with peripheral condensation. (b) HE × 100 mildy pleomorphic cells with nuclear atypia (white arrow). (c) HE × 400 focal osteoid (white arrow). (d) HE × 400 mitotic figure (white arrow).
Discussion
Osteosarcoma accounts for the most common primary non hematopoietic malignancy of the bone. 2 It typically presents in children and adolescents (median age between 10 and 14 years), with a smaller peak in adults older than 40 years. The most common involvement site is the metaphysis of long tubular bones. 1 Os encompasses a spectrum of lesions with considerably diverse histologic features; with conventional OS being the most frequent subtype. 2 In 1989, Mirra et al6,8,9 firstly defined 4 variants of low-grade primary central osteosarcoma of bone. They are characterized by low grade morphology as well as low grade biological behavior, with a metastatic rate up to 10%. This group comprises: osteoblastoma-like OS, fibrous dysplasia-like OS, non-ossifying fibroma-like OS, and chondromyxoid fibroma-like OS; which is the rarest variant. However, despite having a low grade morphology, the metastatic potential is high and the prognosis is poor. 5 The largest series of CMF-like OS in the English literature comprises 6 patients, 3 in all cases the final diagnosis was made after surgical resection, thus the appropriate treatment was not initiated. This finding highlights the difficulty of diagnosis. In addition, its striking resemblance to chondromyxoid fibroma, makes it an important diagnostic pitfall. 3 Pediatric CMF-like OS have been previously reported in 3 patients, 13 years old boy, and 2 girls (9 years and 13 months). Our patient has the same age (13 years old). On imaging, non conventional OS (including CMF like OS) can be similar to a variety of benign or malignant neoplasms. 10 In fact, CMF-OS might be an osteogenic, osteolytic, or expansive lesion. Typical appearance of conventional OS has also been reported making the diagnosis of malignant tumor straight forward. 3 Radiological findings in the present case were highly suggestive of an osteosarcoma. Pathological features of CMF-like Os allow the right diagnosis in the appropriate clinical context. 11 On gross, it presents as a myxoid tumor with a mucoid glistening cut surface. 3 Histologically, CMF-like OS is characterized by lobules of loose cell’s aggregates embedded in a highly myxoid background. Lobules show hypo and hypercellular areas (with often peripheral condensation) and are separated by fibrovascular septa. Neoplastic cells vary from stellate, elongated to polygonal cells. Nuclei are mildly to moderately pleomorphic and hyperchromatic. Cytoplasm’s are eosinophilic and might be vacuolated, suggesting a chondroid differenciation.3,11 Mitotic figures range from 1 to 7 mitosis/HPF.4,8,11 Nuclear atypia and high Ki-67 proliferation index are highly suggestive for malignancy, but the diagnosis of OS is solely based on osteoid production by neoplastic cells.3,12 However, when malignant osteoid deposition is not sampled, histological diagnosis on biopsies becomes very difficult. 3 In the present case, several sections failed to show any evidence of osteoid matrix in the first biopsy and was very focal in the second one, CMF-like OS was retained based on both histologic and malignant radiologic appearance. Immunohistochemistry might be useful in the diagnosis, cells are positive for vimentin, Osteopontin, Osteonectin and are negative for S-100 protein, SOX9, P53, CD34. 5 MDM2 and CDK4 plays also an important role, as they are positive in low grade OS. 3
Given the striking similarity between CMF and CMF-like OS, the most important differential diagnosis is CMF, which is a benign fibro myxoid tumor. The age of presentation, the site, imaging findings are essential features to differentiate these entities. In fact, CMF usually occurs in patient <30, presenting as a well defined osteolytic lesion involving metaphysis of long bones (distal femur and proximal tibia) and the ilium. While CMF-like OS can occur at any age, and has a variable location in the long bone, it presents as an ill-defined osteolytic, osteogenic or expansive lesion. 3 The clue for the histologic diagnosis of CMF-like OS is osteoid formation in addition to atypia, necrosis, atypical increased mitosis, and soft tissue or bone invasion.3,13 Further more, positivity for Vimentin with negative S100 might be of a diagnostic utility. 11 Differential diagnosis also includes chondrosarcoma (CHS), other low grade OS and in some cases conventional osteosarcoma. 3 Thus, the diagnosis is based on careful histological analysis and correlation with clinico-radiological findings. Although described as a low grade OS, most cases showed limited response to chemotherapy, recurrence and a relatively increased metastatic rate. 3 Treatment is based on surgical resection preceded by systemic chemotherapy, which is an important therapeutic strategy.3,12 In our case, the patient received the treatment regimen of conventional osteosarcoma. She died within the 2 weeks following the third dose. The cause of death is not identified as the patient died at home.
In conclusion, we have reported the clinical and histopathological features of a new case of pediatric CMF—like Os, to highlight diagnostic difficulties. The first limitation of the present study, is the initial diagnosis of CMF; which led to delayed diagnosis which might explain the limited response to chemotherapy. The second limitation in the unknown cause of death. Up to present, no standard efficient treatment have been clearly identified. There is a need for a further understanding of CMF-like OS’s biology to improve its poor prognosis.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: LR and LN were responsible for the pathological diagnoses. OM and TM acquired the clinical data and LR and LN were responsible for interpretation of the data and critical revision of the manuscript. JZ and WY designed the study. All authors read and approved the final manuscript.
ORCID iD: Sabrine Derqaoui  https://orcid.org/0000-0002-8935-1346
https://orcid.org/0000-0002-8935-1346
References
- 1. Hmada YA, Bernieh A, Morris RW, Lewin J, Allen T. Chondroblastoma-like osteosarcoma. Arch Pathol Lab Med. 2020;144:15-17. [DOI] [PubMed] [Google Scholar]
- 2. Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125:555-581. [DOI] [PubMed] [Google Scholar]
- 3. Zhong J, Si L, Geng J, et al. Chondromyxoid fibroma-like osteosarcoma: a case series and literature review. BMC Musculoskelet Disord. 2020;21:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stark M, Heinrich SD, Sivashanmugam R, Mackey D, Wasilewska E, Craver R. Pediatric chondromyxoid fibroma-like osteosarcoma. Fetal Pediatr Pathol. 2017;36:154-161. [DOI] [PubMed] [Google Scholar]
- 5. Chuanchao D, Shanshan L, Yu L, Xiaoguang L, Feng W. Chondromyxoid fibroma-like osteosarcoma in thoracic spine with Azygos tumor thrombosis a case report. Preprint. Posted online October 26, 2020. bioRxiv rs.3.rs-96105. doi: 10.21203/rs.3.rs-96105/v1 [DOI] [Google Scholar]
- 6. Prasad K, Dexith J, Lalitha RM, et al. Maxillary osteosarcoma masquerading as chondromyxoid fibroma: report of a case. J Maxillofac Oral Surg. 2015;14:87-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee HC, Luk WH, Lo A, Chow LTC. A case of chondromyxoid fibroma-like osteosarcoma in a 13-month-old girl. SM J Radiol. 2015;1:1003. [Google Scholar]
- 8. Goorin AM. Book reviews. JNCI. 1990;82:968-969. [Google Scholar]
- 9. Mirra J, Picci P, Gold R. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. 1st ed. Lea & Febiger; 1989. [Google Scholar]
- 10. Yarmish G, Klein MJ, Landa J, Lefkowitz RA, Hwang S. Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics. 2010;30:1653-1672. [DOI] [PubMed] [Google Scholar]
- 11. Chow LT, Lin J, Yip KM, et al. Chondromyxoid fibroma-like osteosarcoma: a distinct variant of low-grade osteosarcoma. Histopathology. 1996;29:429-436. [DOI] [PubMed] [Google Scholar]
- 12. Wadhwa N. Osteosarcoma: diagnostic dilemmas in histopathology and prognostic factors. Indian J Orthop. 2014;48:247-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F. Chapter 16 osteogenic tumors. In: World Health Organization Classification of Tumors. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. IARC Press; 2013. [Google Scholar]