Abstract
Background:
Transphyseal anterior cruciate ligament (ACL) reconstruction remains the most commonly used technique for pubescent patients. The transtibial (TT) drilling technique creates vertical and central femoral tunnels to minimize the physeal area of injury at the expense of a nonanatomic femoral tunnel. The hybrid TT (HTT) technique offers the potential of an anatomic femoral position with tunnel geometry similar to that using the TT technique.
Purpose/Hypothesis:
The purpose was to perform a radiographic comparison of the HTT technique with TT and anteromedial portal (AM) techniques in adolescent patients undergoing transphyseal ACL reconstruction. It was hypothesized that femoral tunnels created during HTT would be similar to TT tunnels but significantly more vertical and central than AM tunnels.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We retrospectively screened primary transphyseal ACL reconstructions performed in adolescents at our institution between 2013 and 2019. The youngest 20 eligible patients were selected from each technique cohort: TT, AM, and HTT. Postoperative radiographs were assessed for the coronal femoral tunnel angle, as well as the location of the tunnel-physis penetration on the anteroposterior and lateral views. Physeal lesion surface area was calculated. Data were compared among the 3 groups using 1-way analysis of variance followed by pairwise comparisons.
Results:
Included were 47 patients with a mean ± SD age of 14.3 ± 1.2 years (n = 9 with TT, 18 with AM, and 20 with HTT techniques). The coronal tunnel angle was significantly more vertical in the TT (60.7° ± 7.2°) and HTT (54.4° ± 5.7) groups as compared with the AM group (48.8° ± 5.9; P = .0037 and P = .02, respectively). There was no significant difference between the TT and HTT groups (P = .066). The only significant finding regarding femoral tunnel location was that the HTT tunnels (28.9% ± 4.8%) penetrated the physis more centrally than did the AM tunnels (20.0% ± 5.1%; P = .00002) on lateral radiographs.
Conclusion:
The HTT technique presents an option for transphyseal ACL reconstruction, with femoral tunnel obliquity and estimated physeal disruption similar to that of the TT technique and significantly less than that of the AM technique. The HTT technique also results in the most central physeal perforation of all techniques, predominantly in the sagittal plane.
Keywords: ACL, pediatric sports medicine, anatomy, physis
The incidence of anterior cruciate ligament (ACL) injuries in children and adolescents is rising, 4,29 leading to steady increases in the number of ACL reconstructions performed in growing athletes. Various surgical techniques have been proposed for ACL reconstruction in the skeletally immature patient, 5 yet by far the most commonly used remains the transphyseal technique, 24 in which tunnels are drilled through the tibial and femoral physes. While no high-quality prospective studies exist to compare transphyseal reconstruction with other techniques, such as the partial transphyseal or all-epiphyseal reconstruction, a recent review 24 of the available literature showed that transphyseal and physeal-sparing techniques have comparable rates of limb length deformity (0.81% vs 1.2%, respectively), angular limb deformity (0.61% vs 0%), and graft rupture (6.2% vs 3.1%). As a result, transphyseal reconstruction remains a mainstay of pediatric ACL reconstruction, particularly in the adolescent population with <3 years of growth remaining.
With a transphyseal reconstruction, certain principles guide the technique based on basic science data correlating the surface area of physeal disruption with the risk of subsequent angular or length deformity. 14 It is widely accepted that a more vertical and central perforation of the tibial and femoral physes leads to less surface area disruption and in turn less risk of deformity. 9 This has led to the practice of drilling a vertical tunnel on the tibia, typically around 60°, which still allows easy access to the center of the tibial footprint. The bigger challenge occurs on the femoral side, where historically a transtibial (TT) femoral drilling technique has been recommended since this reliably produces a more vertical and central perforation of the femoral physis. 12,19 Indeed, minimizing injury to the distal femoral physis is critical, as it contributes nearly twice the amount of growth as the proximal tibia and violation via a reamer does result in demonstrable changes to the physis. 30 The use of a TT transphyseal technique has led to acceptable outcomes in children, although few have recommended use of this technique in prepubertal children. 24
In parallel, the adult literature on ACL reconstruction has trended heavily toward recommending “anatomic” ACL reconstruction, focusing on improving coverage of the femoral ACL footprint via reconstruction tunnels, with the goal of restoring normal knee kinematics and in particular rotational knee stability. 13 Recreating an anatomic femoral footprint is more challenging using a TT technique and cannot always be achieved. 23 This becomes particularly difficult with the smaller tibial tunnels drilled in children, which severely constrain access to the appropriate location on the femoral wall using a TT technique. 2
As a result, there has been increased interest in the pediatric sports medicine community in using tibial-independent drilling techniques (anteromedial portal [AM] or outside-in) for transphyseal reconstructions. These have been reported in small case series with good clinical outcomes and without overtly increasing the risk of limb deformity as compared with historical data using the TT technique. 15,21 However, prior radiographic studies in adolescents have shown clearly that using tibial-independent femoral drilling leads to more horizontal femoral tunnels with increased surface area of physeal damage. 3 This poses an inherent dilemma to the surgeon, who must weigh the anatomic accuracy of a transphyseal reconstruction with the likelihood that that reconstruction will lead to a limb deformity.
A potential solution to this dilemma is the use of a hybrid TT (HTT) technique using a flexible reamer, which has been described in adults 20 and validated in cadaveric models 8 as allowing >90% femoral footprint coverage while providing graft-tunnel angulation and tunnel trajectory similar to that of a TT technique. In the setting of a transphyseal reconstruction, this would allow for an anatomic tunnel location on the femur while still permitting a more vertical and central femoral tunnel trajectory to minimize volumetric disruption of the femoral physis. However, this concept has never been validated in a clinical cohort.
The purpose of the current study was to perform a radiographic comparison of the HTT technique with the TT and AM techniques in a cohort of adolescent patients undergoing transphyseal ACL reconstruction. Specifically, femoral tunnel obliquity, location of femoral physeal perforation, and calculated surface area of physeal damage were compared among these 3 surgical techniques. We hypothesized that the HTT femoral tunnels would be equivalent to TT femoral tunnels but more vertical and central than AM femoral tunnels.
Methods
Patient Selection
The study protocol was approved by an institutional review board. Given that this was a retrospective review involving the use of existing data and that only deidentified elements were recorded, the patient consent requirement was waived. Using our institutional database, we identified 284 patients between the ages of 10 and 16 years at the time of surgery who underwent an ACL reconstruction between January 2013 and December 2019. Operative reports were reviewed to identify those patients who underwent a transphyseal reconstruction. Inclusion criteria included (1) a complete transphyseal reconstruction using any graft source; (2) use of a TT, HTT, or AM femoral drilling technique; and (3) a clearly visible physis or physeal scar. Exclusion criteria included (1) revision ACL reconstruction, (2) multiligament knee reconstruction, (3) any other femoral drilling techniques except those mentioned in the inclusion criteria, and (4) the lack of at least 1 postoperative set of radiographs.
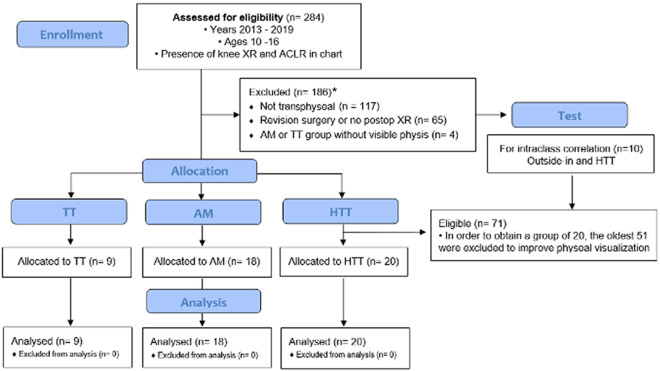
After assessing for exclusion criteria, 98 eligible patients remained: 9 in the TT group, 18 in the AM group, and 71 in the HTT group. To achieve more evenly distributed cohorts and improve the accuracy of radiographic visualization of the physis, we then selected the youngest 20 available patients from each group. This led to a final population of 47 patients, with 9 in the TT group, 18 in the AM group, and 20 in the HTT group. A flow diagram summarizing patient selection is shown in Figure 1.
Figure 1.
CONSORT flow diagram of the patient selection process. *Exclusion criteria based on group can be found in Table 1. ACLR, anterior cruciate ligament reconstruction; AM, anteromedial portal; HTT, hybrid transtibial; postop, postoperative; TT, transtibial; XR, radiograph.
Surgical Technique
Three surgeons (including J.C.R.) contributed patients to this study, each uniquely performing the AM, HTT, or TT technique. Graft choice was at the surgeon’s discretion. In all cases, after diagnostic arthroscopy and graft harvest, a tibial tunnel was prepared using a point-to-tip tibial aimer set at 60°. The tibial tunnel was then prepared using an acorn reamer matching the diameter of the graft. Care was taken to keep the starting point of the tibial tunnel fairly central on the proximal medial tibia and avoid violating the tibial tubercle apophysis.
For the AM technique, a standard rigid offset guide was inserted through the AM. This portal was intentionally kept more central than a traditional accessory AM to produce a less horizontal approach to the lateral wall of the notch. The guide was placed over the previously marked center of the femoral ACL footprint. With the knee in 125° of flexion, a rigid guide pin was advanced through the lateral femoral condyle and out the skin of the anterolateral thigh. Anteroposterior (AP) and lateral fluoroscopic views were performed to confirm a vertical trajectory for the anticipated femoral tunnel. A rigid acorn reamer matching the graft diameter was advanced over the guide pin, and the femoral tunnel was reamed to a depth of 25 to 30 mm. A flexible 4.5-mm reamer (Versitomic; Stryker) was then advanced over the guide pin to perforate the lateral cortex and allow passage of a suspensory cortical button. ACL graft passage and fixation were subsequently performed in standard fashion using cortical button fixation on the femur and interference screw fixation on the tibia.
For the HTT technique, a pathfinder guide (Danamed) with a 7-mm offset was advanced through the AM (Figure 2). A flexible guide pin with a centering sleeve was advanced through the tibial tunnel and mated with the guide within the joint. The guide was hooked on the back wall of the lateral notch and the pin was centered over the native ACL footprint. With the knee at 90° to 95° of flexion, the flexible guide pin was advanced through the lateral femur and out the skin of the anterolateral thigh. A flexible reamer matching the graft diameter (Arthrex) was advanced over the pin, and TT drilling of the femoral tunnel was performed to a depth of 25 to 30 mm. A flexible 4.5-mm reamer (Versitomic; Stryker) was used to perforate the lateral femoral cortex. Graft fixation was performed using an adjustable loop cortical button on the femur (TightRope; Arthrex) and a concave extended button on the tibia (ABS, 20 mm; Arthrex). Backup tibial fixation was achieved using a knotless screw-in anchor (SwiveLock, 4.75 mm; Arthrex).
Figure 2.
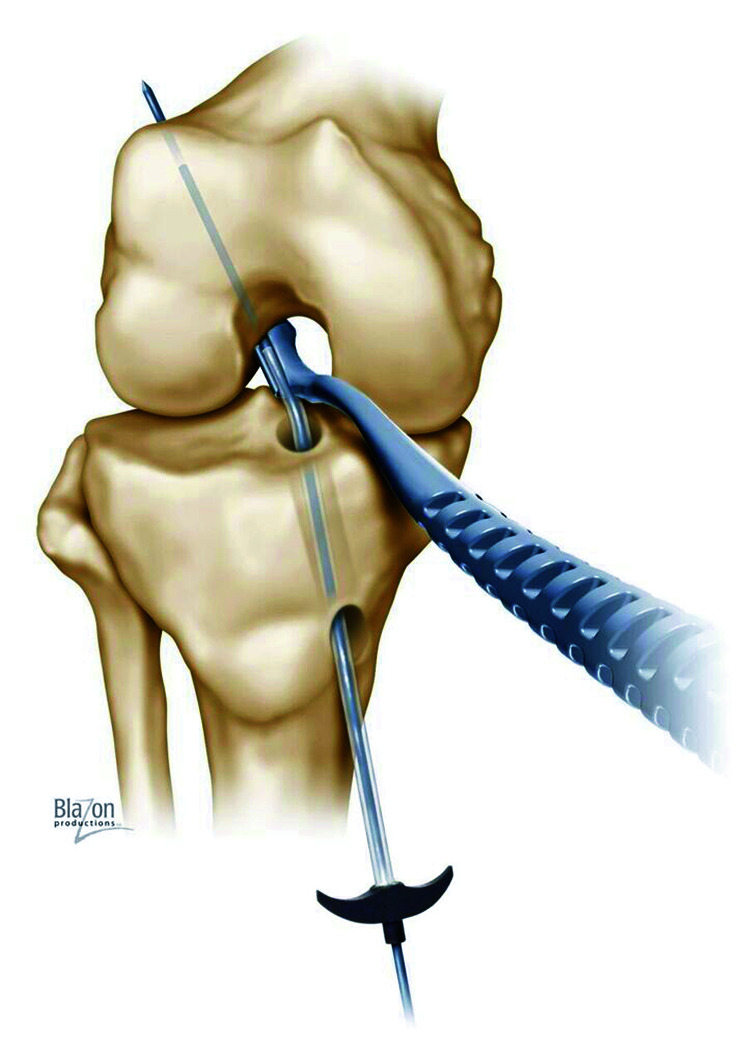
Pathfinder guide for hybrid transtibial drilling technique. 2
For the TT technique, a TT guide with 7-mm offset (Arthrex) was passed through the tibial tunnel and hooked on the back wall of the lateral femoral notch. A 2.4-mm guide pin was advanced in standard fashion. This pin was overreamed using a low-profile reamer matching the graft diameter (Arthrex). The lateral cortex was perforated using a rigid 4.5-mm tenodesis reamer (Arthrex). Graft fixation was performed using an adjustable loop cortical button on the femur (TightRope; Arthrex), and combined tibial fixation was achieved using a biocomposite interference screw (Milagro; DePuy Mitek) and a backup bicortical 4.5-mm screw and smooth washer (Arthrex).
Data Collection
Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at Duke University. 6,7 REDCap is a secure web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for data integration and interoperability with external sources. Characteristic data, including patient age at the time of surgery and sex, were collected from each chart. As skeletal age radiographs of the left hand and wrist were not routinely obtained by all surgeons, only chronological age was reported. In addition, graft choice and tibial and femoral reamer diameters were recorded from the operative note.
Radiographic Measures
All radiographs were analyzed in duplicate by 2 orthopaedic sports medicine fellows (D.L.J. and D.D.V.), and the data were input directly into REDCap. Within REDCap, the radiographs were deidentified to which cohort the patient belonged.
The postoperative radiographs were obtained at a range of 2 weeks to 2 years. This discrepancy was due to individual surgeon preferences. One surgeon obtained routine radiographs at specific postoperative intervals; others did not obtain radiographs at all; and radiographs were obtained years later for evaluation of subsequent knee pain, incidental injury, or evaluation of growth abnormalities. All radiographs were obtained at the same sports medicine clinic, with a high standard of quality AP and lateral views. The two fellows, blinded to the surgical technique, performed the following 5 measures utilizing eUnity 6.7.1 imaging viewing software (Client Outlook).
AP Radiograph
Femoral Tunnel Angle With Respect to the Physis
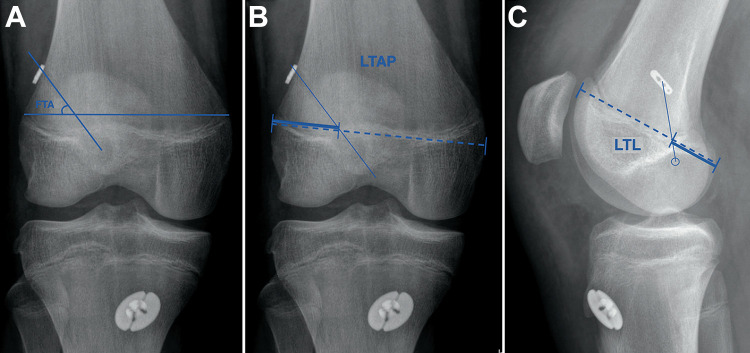
The femoral tunnel angle was defined as the angle created between the reamed femoral tunnel and the femoral physis. For this purpose, the femoral physis was defined as the line connecting the points at which the actual physis exited the medial and lateral cortices of the femur (Figure 3A). This was recorded to the nearest degree.
Figure 3.
Measurement on anteroposterior radiograph for (A) the femoral tunnel angle with respect to the physis (FTA) and (B) the location of the tunnel on the anteroposterior (LTAP), recorded in percentages as the distance from the center of the femoral tunnel as it passes through the physis to the lateral cortex (thick solid line) divided by the entire width of the distal femur along a line parallel to the distal femoral condyles (dashed line). (C) Measurement on lateral radiograph for the location of the tunnel on the lateral (LTL) view, recorded in percentages as the distance between the center of the femoral tunnel as it passes through the physis and the posterior cortex (thick solid line) divided by the entire anteroposterior dimension of the lateral condyle along a line parallel to the physis (dashed line). For the measurements in panels B and C, a smaller number represents a more peripheral tunnel location.
Location of Tunnel on the AP View
The AP tunnel location was reported as a percentage, defined as the distance (recorded to the nearest tenth of a millimeter) from the center of the femoral tunnel as it passes through the femoral physis to the lateral cortex divided by the entire width of the distal femur (along a line parallel to the distal femoral condyles) (Figure 3B). A smaller number represents a more peripheral tunnel location.
Lateral Radiograph
Location of Tunnel on the Lateral View
The lateral tunnel location was reported as a percentage, defined as the distance (recorded to the nearest tenth of a millimeter) between the center of the femoral tunnel as it passes through the physis and the posterior cortex divided by the entire AP dimension of the lateral condyle (along a line parallel to the physis) (Figure 3C). A smaller number represents a more peripheral tunnel location. While most radiographs were near “perfect” laterals, slightly oblique radiographs required proper identification of the lateral condyle based on the terminal sulcus.
Surface Area Calculation
Given the retrospective nature of this study, the time between surgery and radiographs could not be standardized. Because of the potential for tunnel widening over time, tunnel diameter was not considered a reliable metric of time-zero physeal violation. Therefore, estimates of the cross-sectional surface area of physeal disruption was calculated using the formula for an ellipse with multiple hypothetical tunnel diameters between 7.5 and 10 mm, a typical range considered in transphyseal reconstructions.
The surface area of physeal disruption was calculated based on the femoral tunnel angle, using the formula for an ellipse as a cylinder passes through a plane. 28 The area of an ellipse is the product of π and the minor and major radii. The minor radius is half the diameter of the drilled tunnel (d/2). The major radius can be calculated using trigonometry, as the product of the minor radius (d/2) and the cosecant (csc) of the femoral tunnel angle (θ FTA ). Therefore, the formula can be written as follows:
.
This formula assumes a perpendicular angle between the tunnel and physis on the lateral view, which is impossible to measure on a 2-dimensional radiograph owing to the convexity of the lateral physis posteriorly.
Quadrant Method
The quadrant method as defined by Bernard et al 1 was used to assess the accuracy of the location of the aperture of the femoral tunnel. 16,25 Given the lack of detail on the radiographs and the lack of consistent lateral positioning, the center of the intra-articular aperture femoral tunnel was simply noted to be within 1 of the 4 quadrants: proximal-anterior, proximal-posterior, distal-anterior, or distal-posterior (Figure 4).
Figure 4.
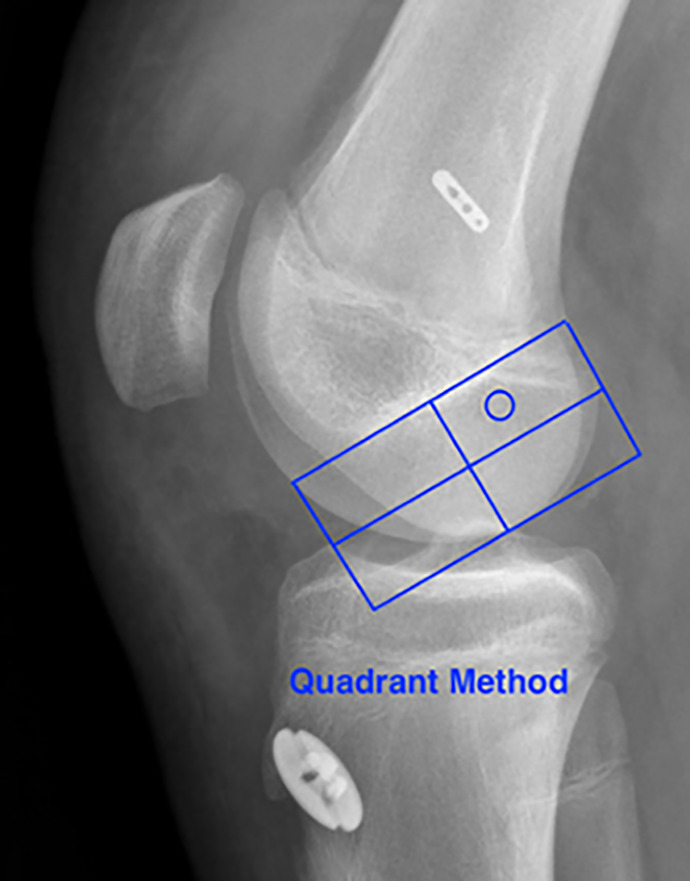
The quadrant method.
Interobserver Reliability
The intraclass correlation coefficient (ICC) was calculated for each radiographic measurement (2-way random effects absolute agreement ICC) to estimate interobserver reliability. The ICC for the femoral tunnel angle was 0.93, and the ICC for the location at which the tunnel crossed the physis was 0.86, showing excellent agreement between raters.
Statistical Analysis
All available patients from our institution were included in the analysis; therefore, a priori sample size calculations were not performed. Nonetheless, we set out to estimate our study power based on estimates of effect size from the existing literature, in which a mean 40° difference in femoral tunnel angle (and therefore surface area of physeal disruption) was observed between the TT and AM tunnels. 3 We therefore used 40° as a starting point for effect size. Standard deviations were estimated from our training set of radiographs used for assessment of interobserver reliability (6°). Since we had unbalanced numbers of patients in each group (n = 18 in the AM, 20 in the HTT, and 9 in the TT group), simulation was used to calculated estimated power using RStudio R, an open source statistical software. The planned analysis was for a 1-way analysis of variance (ANOVA) followed by pairwise comparisons of all 3 drilling groups since all radiographic measures were normally distributed as assessed using the Shapiro-Wilk test. We assumed a conservative Bonferroni-corrected alpha value of .05/3 = .017 for each pairwise comparison. Based on this, our study had 100% power for detecting differences of 40°, 30°, and 20° among groups; 95.4% power, 10°; and 23% power, 5°.
Three outcome variables were considered: the femoral tunnel angle, the location of the tunnel on the AP view (measured as a normalized distance from the lateral cortex), and the location of the tunnel on the lateral view (measured as a normalized distance from the posterior cortex). A Pearson correlation matrix was created, revealing no significant correlations among any of them. Therefore, when analyzing the role of drilling technique on the 3 outcome variables, we performed 3 separate ANOVAs using a Bonferroni-corrected cutoff of P = .017 for significance to adjust for the multiple comparisons. Post hoc analysis was performed for those variables with a significant overall ANOVA. All pairwise comparisons were performed using unpaired t tests, and the Holm procedure was used to control type I error.
Results
Patient Characteristics
As shown in Table 2, the mean ± standard deviation age of the 47 patients was 14.3 ± 1.21 years, with 44.7% being female. The mean femoral tunnel diameter for all patients was 8.9 ± 1.07 mm, with the largest-diameter reamer used for the HTT group (9.3 ± 0.866 mm), followed by the TT (8.9 ± 1.36 mm) and AM groups (8.6 ± 1.04 mm).
TABLE 2.
Characteristics and Radiographic Measures Based on Drilling Technique a
| AM (n = 18) | HTT (n = 20) | TT (n = 9) | Overall (N = 47) | |
|---|---|---|---|---|
| Age, y | ||||
| Mean ± SD | 14.8 ± 0.943 | 13.8 ± 1.07 | 14.3 ± 1.58 | 14.3 ± 1.21 |
| Median [range] | 15.0 [13.0-16.0] | 14.0 [12.0-16.0] | 15.0 [12.0-16.0] | 14.0 [12.0-16.0] |
| Sex, No. (%) | ||||
| Female | 7 (38.9) | 10 (50.0) | 4 (44.4) | 21 (44.7) |
| Male | 11 (61.1) | 10 (50.0) | 5 (55.6) | 26 (55.3) |
| Femoral reamer diameter, mm | ||||
| Mean ± SD | 8.6 ± 1.04 | 9.3 ± 0.866 | 8.9 ± 1.36 | 8.9 ± 1.07 |
| Median [range] | 8.5 [7.00-10.0] | 9.5 [7.00-10.0] | 9.0 [7.00-11.0] | 9.0 [7.00-11.0] |
| Femoral tunnel angle, deg | ||||
| Mean ± SD | 48.8 ± 5.94 | 54.4 ± 5.67 | 60.7 ± 7.16 | 53.5 ± 7.38 |
| Median [range] | 47.3 [38.5-60.5] | 54.5 [46.0-66.0] | 63.5 [48.0-69.0] | 52.5 [38.5-69.0] |
| Tunnel location, % b | ||||
| On AP radiograph | ||||
| Mean ± SD | 32.3 ± 2.55 | 33.7 ± 3.10 | 31.3 ± 3.36 | 32.7 ± 3.05 |
| Median [range] | 32.1 [28.4-38.2] | 34.2 [23.9-37.5] | 30.6 [27.5-35.5] | 33.4 [23.9-38.2] |
| On lateral radiograph | ||||
| Mean ± SD | 20.0 ± 5.12 | 28.9 ± 4.81 | 24.4 ± 3.99 | 24.6 ± 6.22 |
| Median [range] | 19.8 [8.64-29.6] | 28.4 [16.4-36.8] | 25.8 [15.6-28.1] | 25.3 [8.64-36.8] |
a AM, anteromedial portal; AP, anteroposterior; HTT, hybrid transtibial; TT, transtibial.
b See Figure 3 B and C for calculation of tunnel location.
Femoral Tunnel Angle
The AM drilling technique resulted in the most horizontal femoral tunnels with a mean angle of 48.8° ± 5.9°, whereas the TT technique yielded the most vertical femoral tunnels with a mean angle of 60.7° ± 7.2° (Figure 5). The HTT tunnels fell almost exactly in between the other 2 techniques with a mean angle of 54.4° ± 5.7°. The femoral tunnel angles created using the AM technique were significantly different from those created using the TT (P = .0037) and HTT (P = .02) techniques. The relationship of the femoral tunnel angles in the HTT and TT groups was not significantly different (P = .066).
Figure 5.
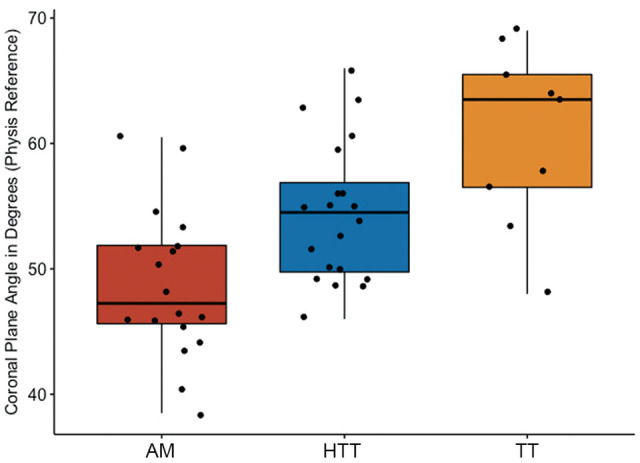
Femoral tunnel angle by drilling technique. Values are presented as median (horizontal line), interquartile range (box), and 95% CI (vertical line). AM, anteromedial portal; HTT, hybrid transtibial; TT, transtibial.
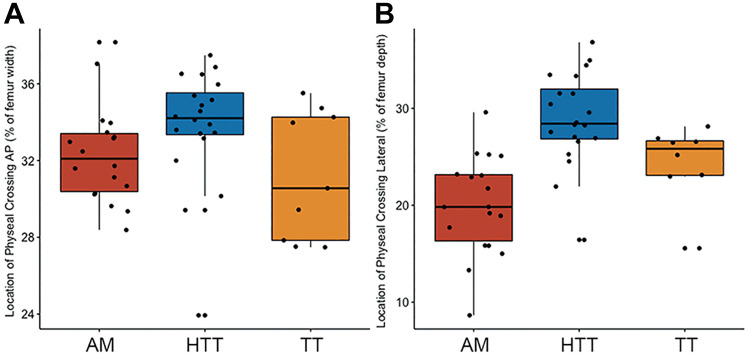
Location of the Physeal Tunnel Penetration
On the AP radiograph, the HTT tunnels penetrated the physis at a more central location (33.7% ± 3.1%) than did the AM (32.3% ± 2.6%) or TT (31.3 ± 3.4%) tunnels, although none of these differences were significant (overall ANOVA, P = .097) (Figure 6A). On the lateral radiograph, the HTT tunnels crossed the physis at a significantly more central location (28.9% ± 4.8%) than did the more posteriorly oriented AM tunnels (20.0% ± 5.1%; P = .00002) but were statistically indistinguishable from the TT tunnels (24.4% ± 4.0%; P = .066) (Figure 6B).
Figure 6.
(A) Location of tunnel on the anteroposterior (AP) radiograph. The values are reported as percentiles along the width of the femoral physis. Lower values represent more lateral locations, and higher values represent more medial locations, with 50 representing the midpoint of the femoral physis. (B) Location of tunnel on the lateral radiograph. The values are reported as percentiles along the width of the femoral physis. Lower values represent more posterior locations, and higher values represent more anterior locations, with 50 representing the midpoint of the femoral physis. Values are presented as median (horizontal line), interquartile range (box), and 95% CI (vertical line). AM, anteromedial portal; HTT, hybrid transtibial; TT, transtibial.
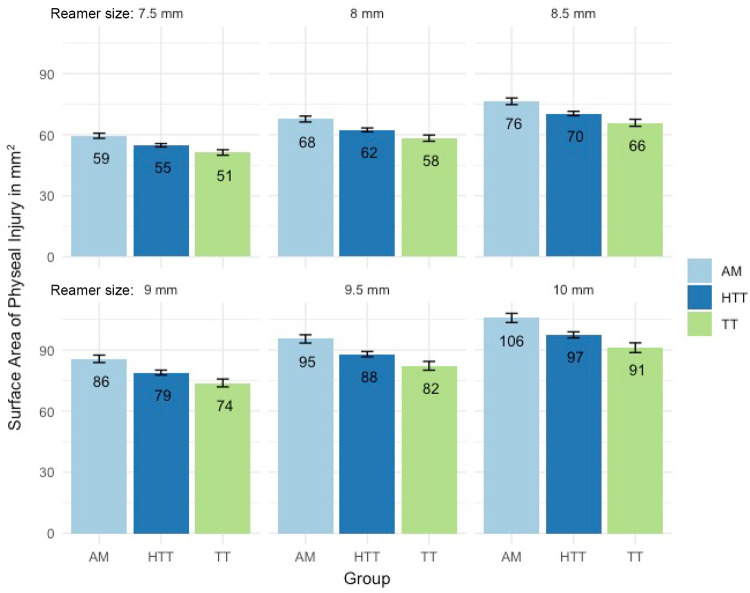
Cross-sectional Area of Physeal Disruption
Given that the surface areas reported were directly calculated from the femoral tunnel angle on the AP radiograph, the results mirror those seen in Figure 5, with the HTT technique falling almost halfway between the AM and TT techniques for any given tunnel diameter. Of note, since the tunnel diameter is squared in the surface area calculation, one can see that diameter would play a larger role in surface area of physeal disruption than would the femoral drilling technique (Figure 7).
Figure 7.
Using the formula for an ellipse, we calculated the cross-sectional surface area of physeal disruption for each drilling technique based on various hypothetical reamer sizes. The black hatches at the top of each bar represent the magnitude of error. Values are presented as median (horizontal line), interquartile range (box), and 95% CI (vertical line). AM, anteromedial portal; HTT, hybrid transtibial; TT, transtibial.
Quadrant Method: Femoral Tunnel
There was 100% tunnel accuracy according to the quadrant method in the 3 cohorts, as all 47 femoral tunnel positions were within the intended proximal-posterior quadrant.
Discussion
The principal finding of this study is that use of an HTT technique for transphyseal ACL reconstruction results in lower femoral tunnel obliquity and calculated physeal surface area disruption as compared with the AM technique while resulting in a physeal perforation that is more central. These findings suggest a possible lower risk of growth disturbance using the HTT than the AM technique while still demonstrating an accurate femoral footprint based on the radiographic quadrant method analysis.
Interestingly, the magnitude of these observed differences was certainly less than our projections, which were based on results of other comparative studies. Our study revealed a 12° difference, but Cruz et al 3 found that the femoral tunnel angle differed by >40° between the TT and AM groups, resulting in a significantly larger area of physeal disruption in the AM group than the TT group (1.64 vs 0.74 cm2). In addition, the location of physeal penetration on the AP radiograph differed by >1 cm, while in our study, there was no significant difference. In a 10-knee cadaveric study, Osier et al 18 demonstrated a 34° tunnel angulation difference (72° in the TT group, 48° in the AM group), again resulting a much more clinically meaningful difference in physeal surface area disruption. In the only other study comparing the HTT technique with the AM and TT techniques, using 24 cadaveric knees, the TT tunnels were 8° more vertical than were the HTT tunnels and 29° more vertical than were the AM tunnels. 8 The explanation for the difference in magnitude between these studies and ours likely lies in our twice-as-large sample size mitigating some of the potential type 1 error and, more influentially, the differences among surgeons using the same technique. The surgeon who performed all of the anteromedial-drilled ACL reconstructions in our study made significant and conscious efforts during surgery, even so far as using fluoroscopy, to create as vertical a femoral tunnel as possible within the limitations of the AM. This underscores the point that any of these techniques, if performed with care, probably allows for an acceptable amount of physeal disruption.
Another concept explored in the study was the discrimination of peripheral versus central physeal lesions. While it is understood that peripheral lesions resulting in physeal arrest would lead to much more severe angular deformities than would central lesions, the importance during ACL reconstruction has not been described. 17 In our study, the location of the physeal lesions in the HTT group tended to be more central on the coronal plane when compared with that in the AM group, albeit not significantly. In the sagittal plane, the HTT technique yielded a significantly more central perforation as compared with the other techniques. While this is suggestive of a more ideal location for a physeal perforation, it elicits 2 potential concerns. First, a more central perforation in the sagittal plane could be the result of a less anatomic, more anterior femoral footprint, although the femoral tunnel locations were indistinguishable among all the groups within our radiographic quadrant method analysis. Second, the ACL footprint is in a posterior location; therefore, a more central tunnel could in fact result in a more oblique tunnel. We chose not to measure the angle of the femoral tunnel on the lateral view, given the low reliability associated with accurately capturing the angle through the undulating femoral physis on a 2-dimensional view, as well as the previously reported literature from Wang et al, 27 who described no statistical correlation between femoral tunnel verticality on the sagittal view and physeal area disruption. While 3-dimensional simulation studies have proven femoral tunnel obliquity and reamer diameter to be direct correlates to the volume of physeal disruption 10,11,26 —a quantifiable and known risk factor for growth arrest—the concept that a more centrally based ACL tunnel would decrease the risk for growth arrest remains purely theoretical at this point.
While the results of our study suggest that the HTT technique may be more “physeal respecting,” boring out a smaller, more central physeal area than the AM technique, there appears to be minimal difference in physeal damage when compared with the dependable TT technique, which is the method currently recommended for a transphyseal ACL reconstruction in this pubescent age category. 22 The major distinction between the HTT and TT techniques lies in the significantly higher reliability of recreating the native ACL footprint, with the HTT tunnels overlapping 93.9% ± 5.6% of the ACL footprint versus the TT tunnels covering only 37.0% ± 28.6%, as proven by using computed tomography scan analysis per Jennings et al. 8 While 2-dimensional lateral radiographs would not allow for the precision required to adequately differentiate the accuracy of the tunnels assessed in our study, the quadrant method was applied to ensure that all of the femoral tunnels fell within a reasonable target in the sagittal plane.
Limitations
There are several limitations to this study. First and foremost, this study was based on radiographic measurements owing to the lack of available postoperative magnetic resonance imaging scans in this patient population. There is no doubt that the accuracy of measuring the femoral tunnel angle, physeal disruption, and ACL footprint would be amplified in a 3-dimensional study. In addition, the timing and technique of these radiographs were not standardized given the retrospective nature of the study, yielding films that ranged from 2 weeks to 2 years after ACL reconstruction.
Second, there is an undeniable sampling bias as a result of the lack of standardized postoperative radiographs, as demonstrated in Table 1: 97% of the HTT group had postoperative radiographs because of a protocol for that specific surgeon, while only 40.4% of the AM group and 33.3% of the TT group had postoperative radiographs. The radiographs in those groups were obtained per surgeon discretion for monitoring alignment, incidental reinjury, or continued concerns. This could inadvertently have selected for patients with worse outcomes, potentially attributed to a poor femoral tunnel technique, thereby skewing the values in these groups. None of the patients in the AM or TT group underwent revisions after these radiographs were obtained, and given the many variables that would lead to a provider obtaining a knee radiograph, we believe that this selection bias played a minimal effect on the femoral tunnel angle.
TABLE 1.
Exclusion Criteria Based on Group a
| TT | AM | HTT | Overall | |
|---|---|---|---|---|
| Patients who initially met inclusion criteria | 36 | 56 | 75 | 167 |
| Revision case | –5/36 (13.8%) | –4/56 (7.1%) | –2/75 (2.7%) | –11/167 (6.5%) |
| No postoperative radiograph | –21/31 (67.7%) | –31/52 (59.6%) | –2/73 (2.7%) | –54/156 (34.6%) |
| No visible physis/not youngest 20 patients | –1/10 (10%) | –3/21 (14.2%) | –51/71 (71.8%) | –55/102 (53.9%) |
| Final included patients | 9 | 18 | 20 | 47/167 (28.1%) |
a AM, anteromedial portal; HTT, hybrid transtibial; TT, transtibial.
A third limitation was that, although attempts were made to conceal the technique used when measurements were being taken, this was ultimately impossible given certain characteristics on the present radiographs (graft choice, fixation, date of radiograph). Fourth, the cohort sizes of each technique were limited by the fact that not all surgeons at our institution consistently obtained postoperative radiographs. Fifth, while attempting to improve the accuracy of radiographic measurements by eliminating patients in the HTT group with closing or closed physes, we may have introduced an unintended selection bias. Finally, as we did not follow the cohort longitudinally, we are unable to quantify the clinical repercussions of these described risk factors for growth arrest.
Conclusion
The HTT technique presents an acceptable option for transphyseal ACL reconstruction, with femoral tunnel obliquity and estimated physeal disruption similar to that of the classic TT technique and significantly less than that of the AM technique. The HTT technique also results in the most central physeal perforation of all techniques in the sagittal plane while not resulting in excessively anterior placement. With the known ability of the HTT technique to recreate an anatomic femoral footprint, this study suggests that it may be a more than reasonable technique for transphyseal ACL reconstruction.
Footnotes
Final revision submitted July 8, 2021; accepted August 6, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.C.R. has received research support from Biopharma, consulting fees from Stryker, and hospitality payments from Smith & Nephew and has stock/stock options in Resor3d. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Duke University School of Medicine.
References
- 1. Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL Radiographic quadrant method. Am J Knee Surg. 1997 Winter;10(1):14–21; discussion 21-2. [PubMed] [Google Scholar]
- 2. Bhatia S, Korth K, Van Thiel GS, et al. Effect of tibial tunnel diameter on femoral tunnel placement in transtibial single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):51–57. [DOI] [PubMed] [Google Scholar]
- 3. Cruz AI, Jr, Lakomkin N, Fabricant PD, Lawrence JT. Transphyseal ACL reconstruction in skeletally immature patients: does independent femoral tunnel drilling place the physis at greater risk compared with transtibial drilling? Orthop J Sports Med. 2016;4(6):2325967116650432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 Years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 5. Gausden EB, Calcei JG, Fabricant PD, Green DW. Surgical options for anterior cruciate ligament reconstruction in the young child. Curr Opin Pediatr. 2015;27(1):82–91. [DOI] [PubMed] [Google Scholar]
- 6. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jennings JK, Leas DP, Fleischli JE, D’Alessandro DF, Peindl RD, Piasecki DP. Transtibial versus anteromedial portal ACL reconstruction: is a hybrid approach the best? Orthop J Sports Med. 2017;5(8):2325967117719857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jeon JY, Lee J, Kang MS. Transphyseal anterior cruciate ligament reconstruction in adolescents with substantial remaining growth causes temporary growth arrest resulting in subclinical leg-length discrepancy. Medicine (Baltimore). 2019;98(26):e16081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kachmar M, Piazza SJ, Bader DA. Comparison of growth plate violations for transtibial and anteromedial surgical techniques in simulated adolescent anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(2):417–424. [DOI] [PubMed] [Google Scholar]
- 11. Kercher J, Xerogeanes J, Tannenbaum A, Al-Hakim R, Black JC, Zhao J. Anterior cruciate ligament reconstruction in the skeletally immature: an anatomical study utilizing 3-dimensional magnetic resonance imaging reconstructions. J Pediatr Orthop. 2009;29(2):124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89(12):2632–2639. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade RF, Moulton SG, Nitri M, Mueller W, Engebretsen L. Clinically relevant anatomy and what anatomic reconstruction means. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2950–2959. [DOI] [PubMed] [Google Scholar]
- 14. Mäkelä EA, Vainionpää S, Vihtonen K, Mero M, Rokkanen P. The effect of trauma to the lower femoral epiphyseal plate: an experimental study in rabbits. J Bone Joint Surg Br. 1988;70(2):187–191. [DOI] [PubMed] [Google Scholar]
- 15. Mathew S, Ellis HB, Wyatt CW, et al. Is anteromedial drilling safe in transphyseal anterior cruciate ligament reconstruction in adolescents with growth remaining? J Pediatr Orthop. 2019;39(4):e278–e283. [DOI] [PubMed] [Google Scholar]
- 16. Mochizuki Y, Kaneko T, Kawahara K, et al. The quadrant method measuring four points is as a reliable and accurate as the quadrant method in the evaluation after anatomical double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2389–2394. [DOI] [PubMed] [Google Scholar]
- 17. Nordentoft EL. Experimental epiphyseal injuries: grading of traumas and attempts at treating traumatic epiphyseal arrest in animals. Acta Orthop Scand. 1969;40(2):176–192. [DOI] [PubMed] [Google Scholar]
- 18. Osier CJ, Espinoza-Ervin C, Diaz De Leon A, Sims G, Ellis HB, Jr, Wilson PL. A comparison of distal femoral physeal defect and fixation position between two different drilling techniques for transphyseal anterior cruciate ligament reconstruction. J Pediatr Orthop B. 2015;24(2):106–113. [DOI] [PubMed] [Google Scholar]
- 19. Paletta GA, Jr. Complete transphyseal reconstruction of the anterior cruciate ligament in the skeletally immature. Clin Sports Med. 2011;30(4):779–788. [DOI] [PubMed] [Google Scholar]
- 20. Patel KA, Chhabra A, Makovicka JL, Bingham J, Piasecki DP, Hartigan DE. Anterior cruciate ligament tunnel placement using the pathfinder guide. Arthrosc Tech. 2017;6(4):e1291–e1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pennock AT, Johnson KP, Turk RD, et al. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: quadriceps tendon autograft versus hamstring tendon autograft. Orthop J Sports Med. 2019;7(9):2325967119872450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Perkins CA, Willimon SC. Pediatric anterior cruciate ligament reconstruction. Orthop Clin North Am. 2020;51(1):55–63. [DOI] [PubMed] [Google Scholar]
- 23. Piasecki DP, Bach BR, Jr, Espinoza Orias AA, Verma NN. Anterior cruciate ligament reconstruction: can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011;39(6):1306–1315. [DOI] [PubMed] [Google Scholar]
- 24. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. [DOI] [PubMed] [Google Scholar]
- 25. Shafizadeh S, Balke M, Kelz S, Hoeher J, Banerjee M. Low inter- and intraobserver variability allows for reliable tunnel measurement in ACL reconstruction using the quadrant method. Arch Orthop Trauma Surg. 2014;134(4):529–536. [DOI] [PubMed] [Google Scholar]
- 26. Shea KG, Belzer J, Apel PJ, Nilsson K, Grimm NL, Pfeiffer RP. Volumetric injury of the physis during single-bundle anterior cruciate ligament reconstruction in children: a 3-dimensional study using magnetic resonance imaging. Arthroscopy. 2009;25(12):1415–1422. [DOI] [PubMed] [Google Scholar]
- 27. Wang JH, Son KM, Lee DH. Magnetic resonance imaging evaluation of physeal violation in adolescents after transphyseal anterior cruciate ligament reconstruction. Arthroscopy. 2017;33(6):1211–1218. [DOI] [PubMed] [Google Scholar]
- 28. Weisstein E. Cylindrical segment. MathWorld. Accessed October 2021. http://mathworld.wolfram.com/CylindricalSegment.html
- 29. Werner BC, Yang S, Looney AM, Gwathmey FW, Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]
- 30. Yoo WJ, Kocher MS, Micheli LJ. Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop. 2011;31(6):691–696. [DOI] [PubMed] [Google Scholar]