Abstract
Background:
The anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) contribute greatly to the overall stability of the ankle joint; however, ATFL and combined ATFL-CFL sprains are common. Anatomic reconstruction of the lateral collateral ligament with grafts has been proposed for patients with poor tissue quality or inadequate local tissue. Anatomic reconstruction of the lateral ankle ligaments requires a good understanding of their anatomic location.
Purpose:
To describe the anatomy of the ATFL and CFL ligaments quantitatively and qualitatively and explore the relationship of some morphological parameters.
Study Design:
Descriptive laboratory study.
Methods:
A total of 66 adult ankle specimens were analyzed for ATFL band type, origin, length, width, thickness, and angle between the ATFL and CFL, and 73 adult ankle specimens were used for measuring the origin of the CFL. The coefficient of variation was used to describe and compare the respective variability of angle, length, width, and thickness. The origin of the ATFL was labeled as point A, and the leading edge of the CFL intersection with the articular surface of the calcaneus was considered point B.
Results:
The ATFL had a variable number of bands. A high degree of variability (coefficient of variation >0.2) was seen for most morphological measurements of the ATFL. In addition, the length of distance AB also varied. The CFL originated at the tip of the fibula in only 9% of specimens. It was found more commonly at the anterior border of the lateral malleolus (4.94 ± 1.70 mm from the tip). The angle between the ATFL and CFL was consistent at 100° to 105º.
Conclusion:
A fair amount of variability of ATFL length, width, and thickness were found in our study, with less variability in the ATFL-CFL angle. Most CFLs attached anterior to the tip of the fibula.
Clinical Relevance:
Providing relevant anatomic data of ATFL and CFL is important in ensuring proper surgical treatment of ankle joint injuries.
Keywords: anatomy, anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), lateral ankle collateral ligament, variability
The lateral collateral ligaments of the ankle consist of the anterior talofibular ligament (ATFL), the posterior talofibular ligament, and the calcaneofibular ligament (CFL). The ankle joint, whose most common sprain mechanism is to the lateral collateral ligament, 4,20,34,35,42 is injured easily, and ligamentous structural injuries in the ankle, caused mostly by plantarflexion injuries and valgus injuries, 57 are the most frequently occurring sports injuries. 45 Among these 3 ligaments, the ATFL, with the function of limiting plantarflexion and ankle inversion, 41,55 contributes greatly to the overall stability of the ankle joint 25 ; however, it is simultaneously the most fragile and vulnerable among the lateral collateral ligaments. 3,56 The ATFL alone accounts for approximately 65% to 73% of ankle sprains, 45,55,57 with 20% to 40% being combined ATFL-CFL sprains, 21,49 and only 2% occurring to the CFL alone. 57
Swift and precise treatment should be provided to avoid long-term complications in ATFL injuries. Chronic ankle instability, for instance, occurs in 10% to 20% of ankle injuries with inadequate management and recurrent injury. 54 When functional lateral ankle instability occurs after nonoperative treatment (rest, ice, compression, elevation, anti-inflammatory medication, physical therapy, bracing, and proprioceptive training), surgical reconstruction, both anatomic and nonanatomic, may be needed. 13,14,21,23,30,40,55
Although the Broström-Gould anatomic repair is still the standard surgical option for chronic lateral ankle instability, 5,6,11,16,36 it is not recommended for patients with poor tissue quality and inadequate local tissue, such as those with long-standing chronic ankle instability and general ligament laxity as well as those undergoing revision surgery. 11,29,30 In addition, patients with increased demands to their ankle, such as elite athletes and patients with various types of hindfoot misalignment, are reported to be at increased risk of failure after Broström-Gould repair. 12,24,46
Lateral ankle ligamentous anatomic reconstruction with grafts has been proposed as an alternative to anatomic repair 24,26,29,30,32,36,53 and has revealed successful results, improved ankle stability, reduction in pain, and marginal motion loss in the ankle and hind foot. 27 Anatomic reconstruction of the lateral ankle ligaments assumes a standardized anatomy and requires a good mastery of their anatomic locations. 2,8,13,22
The ATFL originates at the medial leading edge of the lateral malleolus and inserts into the talar neck. It usually consists of 2 fiber bundles, or “bands”; seldom have 3 bands been reported in previous studies. 9,13,15,39,43,50 The specific origin of the CFL is still vague; without detailed measurement methods and reliable statistical data, the origin of the CFL is regarded as being located roughly on the distal fibula or taken for granted to be on the tip of the lateral malleolus. 33,56 If the location of the CFL is not correct in the anatomic reconstruction, the movement of the ankle joint and subtalar joint may be limited. 9
Previous anatomic studies on the ATFL and CFL ligaments of the ankle have been limited by small sample sizes and a lack of information about the angle between the ATFL and CFL (ATFL-CFL angle). 13,15,38,39,56 Thus, the purpose of this study was to describe the anatomy of the ATFL and CFL ligaments quantitatively and qualitatively; we sought to measure the anatomic parameters of the ATFL (band type, length, width, thickness, and origins) as well as the location of the fibular origin of the CFL and the ATFL-CFL angle.
Methods
Specimens
We initially obtained 66 adult ankle specimens from the Department of Anatomy, Southern Medical University, Guangzhou, China. The specimens were taken from Asian cadavers (male to female ratio, 8:2) between the ages of 30 and 70 years. After measurement of the anatomic parameters of the ATFL and the ATFL-CFL angle in these 66 samples, 14 samples were unable to be used (broken or lost) for identification of the CFL origin. Thus, an additional 21 ankles were procured to supplement the remaining intact specimens, so that 73 specimens were used to identify the CFL origin. This study was approved by an ethics committee and was compliant with the tenets of the Declaration of Helsinki. All body donors had provided written consent to use their specimens for medical research or teaching.
The specimens were analyzed by 1 of 6 anatomy teachers (R.Q., S.H., Z.L., C.L., Z.X., H.L.) with more than 10 years of anatomic experience. We cut the skin with a scalpel, gripped the skin with toothed forceps, and then tore the tough deep fascia and removed it carefully with a scalpel if necessary. Next, 2 toothless forceps were used to separate blood vessels, nerves, and muscles and remove them using a scalpel. We separated the soft tissue around the ligaments, layer by layer, until the ligaments were completely exposed, placed the specimens in 10% formalin solution, and stored them in a natural position (90° upright) for 6 months. After that, 3 researchers (Z.C., Z.Y., J.Y.) trained in precision and methodology over the course of 6 months took the morphological measurements.
A YLD-261 electronic digital Vernier caliper (accurate to 0.01 mm; Jiangsu Yinlongdao Outdoor Products), two 0.8 mm–diameter Kirschner wires (Shanghai Kaiwei), and an electronic digital angle ruler (resolution: 0.05°; Nanjing Sutong Measuring Instrument) were used for measurements.
Observations and Measurements
Origin, Length, Width, and Thickness of the ATFL
All measurements were made with the ankle specimen fixed in a 90° upright position. The midpoint of the ATFL was set at the attachment of the fibula, the origin of the ATFL was labeled as point A, and the leading edge of the CFL intersection with the articular surface of the calcaneus was considered point B. The distance between points A and B was measured as a reference for locating the ATFL origin (Figure 1).
Figure 1.
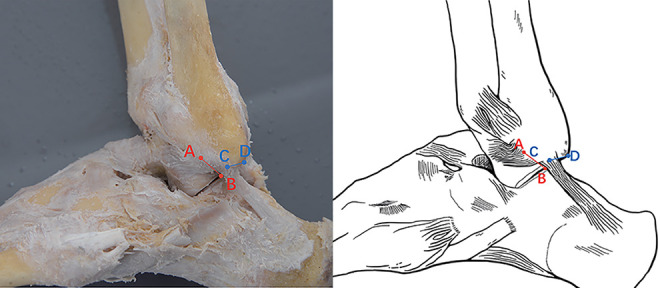
The distance from the anterior talofibular ligament (ATFL) origin to the subtalar joint (line AB) and the distance from the calcaneofibular ligament (CFL) origin to the tip of the lateral malleolus of the anterior border of the lateral malleolus type (line CD) as shown on a specimen photograph (left) and a representative drawing (right). ATFL origin/ATFL fibular attachment midpoint (A); Intersection of the CFL and the subtalar joint (B); CFL origin/CFL fibular attachment midpoint (C); tip of the lateral malleolus (D).
The distance from the midpoint of the fibular attachment to the midpoint of the talar attachment was defined as the length of the ATFL (red line in Figure 2A). The width of the ATFL was measured at the fibular insertion, at the midpoint of its length and at the talar insertion, and the average of these 3 places was considered the overall width. The thickness of ATFL was measured at the midpoint of the ligament.
Figure 2.
The 3 morphological types of the anterior talofibular ligament (ATFL) on specimen photographs (left) and representative drawings (right). (A) Single band, showing the length of the ATFL (red line) and the width of the ATFL at the fibular attachment, midpoint, and talar attachment (blue lines). (B) Double band, showing the length of the superior limb (red line), the length of the inferior limb (green line), and the width at the fibular attachment, midpoint, and talar attachment of the superior limb (blue lines) and the inferior limb (yellow lines). (C) Triple band, showing the length of the superior limb (red line), median limb (green line), and inferior limb (purple line), as well as the width at the fibular attachment, midpoint, and talar attachment of the superior limb (blue lines), the median limb (yellow lines), and the inferior limb (orange lines). Note that the ankle was fixed in the plantarflexion for the photograph in (C) for viewing purposes only. All measurements were taken in the 90° upright position.
We found 3 different ATFL morphologies in this study: single (1 fiber bundle), double band (2 fiber bundles), and triple band (3 fiber bundles). The measurement locations of the ATFL length and width are presented in Figure 2.
ATFL-CFL Angle
The ATFL-CFL angle was measured by drawing 2 intersecting lines through the origin and end point of the ATFL and CFL, respectively. Because the angle between the 2 ligaments is sometimes too small to be measured accurately, 2 Kirschner wires (Shanghai Kaiwei) were used to replace the 2 straight lines to increase measurement accuracy (Figure 3).
Figure 3.

ATFL-CFL angle as shown on a specimen photograph (left) and a representative drawing (right). ATFL origin/ATFL fibular attachment midpoint (A); CFL origin/CFL fibular attachment midpoint (C); ATFL insertion/ATFL talar attachment midpoint (E); CFL insertion/CFL calcaneal attachment midpoint (F). Blue lines represent Kirschner wires. ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
Origin of the CFL
The 73 ankle ligament specimens used to evaluate the CFL origin were placed horizontally on the experimental platform and fixed in a 90° upright position (Figure 4). The origin of the CFL was classified according to location as being at the tip of the lateral malleolus, at the anterior border of the lateral malleolus, or at the posterior border of the lateral malleolus.
Figure 4.

The calcaneofibular ligament originating at the tip of the lateral malleolus (pink dot), as shown in a photograph of a specimen (left) and a representative drawing (right).
Statistical Analysis
Given that it has not been evaluated previously, the ATFL-CFL angle was measured independently by 2 persons (observers 1 and 2, Z.Y., J.Y.), whereas other indices such as the length, width, and thickness were measured by 1 experienced individual (observers 3, 4, or 5, H.Y., M.S., Z.C.). For each specimen, each distance and angle was measured 3 times, and the average was calculated. To evaluate reliability, intraobserver intraclass correlation coefficients (ICCs) were calculated, and interobserver ICCs for observers 1 and 2 were calculated.
The coefficient of variation (CV) was used to describe and compare the respective variability of the ATFL length, width, and thickness as well as the ATFL-CFL angle. A CV of 0.2 is an important determinant of variability, 19,44 with <0.2 indicating a low degree of variability and >0.2 indicating a high degree of variability. In all statistical analyses, P <.05 were used to indicate significance. SPSS Statistics 22.0 (IBM) was used to analyze the data.
Results
Intra- and Interobserver Reliability
The intraobserver ICCs for length, width, thickness, distance AB, and the distance from the CFL origin to the tip of the lateral malleolus were 0.953, 0.908, 0.902, 0.973, and 0.970, respectively. For the ATFL-CFL angle, the intraobserver ICCs were 0.995 for observer 1 and 0.997 for observer 2, and the interobserver ICC was 0.774. These ICCs, all greater than 0.75, indicated good reliability.
ATFL-CFL Angle
Anatomic ATFL features were analyzed in 66 adult ankle specimens with a complete ligament. Among the 66 ankle specimens analyzed for ATFL, 7 (10.61%), 53 (80.30%), and 6 (9.09%) cases showed single-, double-, and triple-band type, respectively (Figure 2). Details of the ATFL-CFL angle, distance AB, and length, width, and thickness of each limb of the ATFL are shown in Table 1.
Table 1.
Morphological Parameters of ATFL a
| ATFL Type | n | ATFL-CFL Angle | Length | Width | Thickness | Distance AB |
|---|---|---|---|---|---|---|
| Single band | 7 | 104.3 ± 10.0 | 20.40 ± 1.26 | 8.68 ± 2.25 | 0.79 ± 0.40 | 8.60 ± 3.39 |
| Superior limb of double band | 53 | 103.5 ± 9.3 | 19.83 ± 3.76 | 6.89 ± 1.70 | 0.96 ± 0.39 | 10.44 ± 2.93 |
| Inferior limb of double band | 53 | 101.6 ± 13.6 | 15.83 ± 3.45 | 4.65 ± 1.66 | 0.54 ± 0.17 | 5.82 ± 3.35 |
| Superior limb of triple band | 6 | 101.3 ± 6.0 | 19.13 ± 2.90 | 5.58 ± 1.30 | 0.66 ± 0.16 | 12.78 ± 2.41 |
| Median limb of triple band | 6 | 96.6 ± 8.4 | 18.22 ± 6.30 | 3.44 ± 1.00 | 0.42 ± 0.10 | 9.57 ± 2.37 |
| Inferior limb of triple band | 6 | 104.3 ± 14.3 | 15.04 ± 5.69 | 4.02 ± 1.99 | 0.55 ± 0.34 | 5.32 ± 2.04 |
a Measurements are reported in mm as mean ± SD. ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
Coefficients of Variation for ATFL Parameters
The ATFL-CFL angle showed little variability (CV < 0.2), whereas many of the morphological parameters of the ATFL were more variable (CV > 0.2) (Table 2).
Table 2.
CV of the Morphological Parameters of the ATFL a
| ATFL Type | ATFL-CFL Angle | Length | Width | Thickness | Distance AB |
|---|---|---|---|---|---|
| Single band | 0.096 | 0.062 | 0.259 | 0.506 | 0.394 |
| Superior limb of double band | 0.090 | 0.190 | 0.247 | 0.406 | 0.281 |
| Inferior limb of double band | 0.134 | 0.218 | 0.357 | 0.315 | 0.576 |
| Superior limb of triple band | 0.059 | 0.152 | 0.233 | 0.242 | 0.189 |
| Median limb of triple band | 0.087 | 0.346 | 0.291 | 0.238 | 0.248 |
| Inferior limb of triple band | 0.137 | 0.378 | 0.495 | 0.618 | 0.383 |
a ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; CV, coefficient of variation.
To evaluate whether the similarities and differences existed between 2 separate CVs, their P values were calculated (Table 3). No significant differences were found in the CV for length, width, and thickness of the ATFL. However, significant differences were found in the CVs between the ATFL-CFL angle and each of the morphologic parameters of the ATFL.
Table 3.
The P Value Between the CVs of 2 Parameters a
| Parameter | P |
|---|---|
| ATFL-CFL angle and length | .0337 |
| ATFL-CFL angle and width | .0005 |
| ATFL-CFL angle and thickness | .0011 |
| Length and width | .1888 |
| Length and thickness | .0656 |
| Width and thickness | .3422 |
a Bold P values indicate statistically significant difference between the parameters compared (P < .05). ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; CV, coefficient of variation.
Origin of the CFL
In the 73 specimens used to analyze the CFL, the CFL origin was at the tip of the lateral malleolus in 7 cases; in the remaining 66 cases, the origin was at the anterior border of the tip of the lateral malleolus. The distance from the origin to the tip of the lateral malleolus was 4.94 ± 1.70 mm, and no CFL originated at the posterior border of the tip of the lateral malleolus (Figure 4).
Discussion
An anatomically clear knowledge of the lateral ankle ligaments is required for anatomic reconstruction of the lateral ankle ligaments. In this study, we discovered that, in general (without distinguishing ATFL band type), the ATFL-CFL angle is a more consistent finding than the length/width/thickness of the ATFL, suggesting that ATFL-CFL angle could be a secure auxiliary index of reconstruction and an evaluation indicator of effect used for double-checking during the surgery. Considerable variability was found in the length, width, and thickness of the ATFL. In addition, distance AB had a high CV, which may be caused by the anatomic variability of the ATFL origin (point A) or point B, or both. The majority of the CFLs originated at the point on the anterior border of the lateral malleolus, 4.94 ± 1.70 mm away the tip. Kelikian and Sarrafian 31 and Taser et al 50 also reported that the CFL did not extend to the tip of the lateral malleolus, but neither specified the distance of the CFL insertion from the tip. Conversely, Wenny and Duscher 56 and Liu et al 33 proposed that the CFL originated directly at the tip. Hitherto, there have been limited data available classifying the origin of the CFL. The origin in our result was divided into 2 categories according to whether it was at the anterior border or the tip of the lateral malleolus, with 66 cases (90.41%) of the former and 7 (9.59%) of the latter. Thus, we concluded that the CFL originates most often at the anterior border. Our measurement from the origin of the CFL to the tip of the lateral malleolus (4.94 ± 1.70 mm) was similar to that of Clanton et al 13 (5.3 mm) but less than that found by Kakegawa et al 28 (7.4 ± 1.7 mm). As ATFL-CFL combined reconstruction has been shown to restore motion better than isolated ATFL reconstruction, 7 it is important to master the CFL specific origin, distance away from the tip, and surgically relevant osseous landmarks.
The origin of ATFL was located by measuring distance AB (the distance from the midpoint of the fibular attachment of ATFL to the subtalar articular surface). Point B can be observed clearly on arthroscopy; this landmark is helpful in locating the ATFL origin. In the current study, a double-band ATFL (80.3%) was the most common type, followed by the single (10.6%) and triple band (9.1%). The proportions observed by Edama et al 17,18 and Kakegawa et al 28 were close to ours (Table 4), which may be because of similar sample sizes (>60) and ethnicity (Asians). Milner and Soames 38 and Uğurlu et al 51 also reported that the double-band type was the most common but at a smaller scale, with the single and the triple bands seen occasionally; the difference from the current findings could be caused by the low number of specimens (≈20) and the different ethnic groups involved.
Table 4.
Frequency of ATFL Band Types According to Various Studies a
| N | Single Band | Double Band | Triple Band | |
|---|---|---|---|---|
| Present study | 66 | 7 (10.61) | 53 (80.30) | 6 (9.09) |
| Edama et al 18 | 110 | 34 (31) | 66 (60) | 10 (9) |
| Edama et al 17 | 81 | 27 (33) | 46 (57) | 8 (10) |
| Milner and Soames 38 | 26 | 10 (38) | 13 (50) | 3 (12) |
| Uğurlu et al 51 | 22 | 5 (23) | 13 (59) | 4 (18) |
| Burks and Morgan 9 | 39 | — | — | — |
| Clanton et al 13 | 14 | 7 (50) | 7 (50) | — |
| Delfaut et al 15 | 4 | 1 (25) | 3 (75) | — |
| Neuschwander et al 39 | 8 | 2 (25) | 6 (75) | — |
| Raheem and O’Brien 43 | 20 b | 14 (70) | 5 (25) | — |
| Taser et al 50 | 42 b | 39 (93) | 1 (2) | — |
| Wenny and Duscher 56 | 17 | 17 (100) | — | — |
| Yıldız and Yalcın 58 | 45 | 34 (75.6) | 11 (24.4) | — |
| Kakegawa et al 28 | 60 | 14 (23.3) | 42 (70.0) | 4 (6.7) c |
a Data are reported as n (%). Dashes indicate data not reported. ATFL, anterior talofibular ligament.
b 5% absent.
c Multiple-type ATFL.
Regardless of the number of bands, the superior band always showed the least amount of variation in morphologic parameters. In addition, the length of the ATFL decreased gradually from top to bottom, so that single-band ATFLs were the longest (20.40 ± 1.26 mm), the superior band was longer than the inferior in double-band ATFLs, and, in the triple-band ATFLs, the superior band (19.13 ± 2.90 mm) was longer than the median band (18.22 ± 6.30 mm), followed by the inferior band (15.04 ± 5.69 mm) (see Table 1). This may indicate that the superior limb has the most important role in providing biomechanical resistance to inversion forces.
In general, the length and width of the ATFL in this study were similar to those of previous studies, whereas the thickness was quite different from that reported previously (Table 5). Matsui et al 37 suggested measuring the ATFL length “from center to center.” In the current study, ATFL length was measured from the midpoint of the fibular attachment to the midpoint of the talar attachment to obtain the best results. Previously, the length measured by Burks and Morgan 9 was the longest, probably because they measured only the longest fibers of the ATFL, whereas Yıldız and Yalcın 58 measured the longest and shortest fibers of ATFL. Our measured ATFL width was similar to that found by others, but slightly smaller than those reported by Milner and Soames 38 and Yıldız and Yalcın, although we measured ATFL width in a manner similar to both previous studies. To the best of the current authors’ knowledge, the thickness of each band of the ATFL had never been measured in detail. ATFL thickness as measured by van den Bekerom et al 52 was more than 2 SDs from this study, and this difference may be due to the absence of band distinctions.
Table 5.
ATFL Morphology in Previously Published Studies a
| Study | ATFL-CFL Angle, deg | Length, mm | Width, mm | Thickness, mm |
|---|---|---|---|---|
| Wenny and Duscher 56 | — |
|
|
— |
| Neuschwander et al 39 | — |
|
— | — |
| Yıldız and Yalcın 58 |
|
|
11.07 ± 5.63 | — |
| Sindel et al 48 | — |
|
|
— |
| Taser et al 50 | 132 (118-145) | 22.37 ± 2.50 | 6.75 ± 2.89 | — |
| Uğurlu et al 51 | 113 (107-123 ) | (14.38-20.84) | 7.61 | — |
| Burks and Morgan 9 | — | 24.8 b | 7.2 | — |
| Siegler et al 47 | — | 17.81 ± 3.05 | — | — |
| Buzzi et al 10 | — | 16.3 (10-28) |
|
— |
| Milner and Soames 38 | — | 13.0 ± 3.9 | 11.0 ± 3.3 | — |
| Raheem and O’Brien 43 | — | 15.5 ± 7.7 | 10 ± 7 | — |
| van den Bekerom et al 52 | — | (15-20) | (6-10) | 2 |
a Data are reported as mean or mean ± SD; numbers in parentheses are ranges. Dashes indicate data not reported. ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; Inf, inferior limb; Sup, superior limb.
b Length was defined as the longest fiber of the ATFL.
c Length was defined as the shortest length of the ATFL.
Our findings showed a much more dorsal position of the CFL attachment on the calcaneus compared with the study of Yıldız and Yalcın. 58 As the age of our specimens was similar to theirs (35-78 years), 2 factors may explain this phenomenon. One is the length and slope of the calcaneus. Although the angular difference found by Yıldız and Yalcın was about 5º to 8º, our calcaneus was longer and had a steeper angle of 10º to 15º, making its upper edge closer to the CFL. Another factor is the longer and wider CFLs in our study, with a tendency to spread dorsally; this consequently further minimizes the distance between the CFL and the upper edge of the calcaneus. These 2 possible reasons may both correlate with racial differences, as the calcaneus and CFLs of this study match those in the studies of Akatsuka et al 1 and Kakegawa et al, 28 all from Asian ethnic groups, but differ from those in the study by Yıldız and Yalcın, whose specimens were White.
There were some limitations to our study. First, though we made conjectures about ATFL and CFL from the biomechanical perspective, our study was still limited to anatomic observation, without verification by biomechanical study. Second, because the samples used to determine the origin, length, width, and thickness of the ATFL, and the ATFL-CFL angle (66 cases) were not exactly the same as those used to determine the CFL origin (73 cases), our study may not be ideal to explore the correlation between CFL origin and other parameters, as unreliable conclusion could be drawn from unequal samples. Besides, other limitations, such as no data on height, only Asian specimens, and a single observer for ATFL measurements, have possible implications for the measuring process and results and require improvement. In addition, CFL morphologic measurements and information on insertions of the ATFL on the talus or CFL on the calcaneus, which are also important for reconstruction, are still needed to complement our findings.
Conclusion
A fair amount of variability of ATFL length, width, and thickness was found in our study, with much less variability in the ATFL-CFL angle. Most CFLs attached anterior to the tip of the fibula. In addition, the measurement of distance AB varied. Knowing this anatomic information can help surgeons planning anatomic lateral ankle ligament reconstructions.
Acknowledgment
The authors acknowledge Zeyu Wu for assisting in specimen preparation and analyzing the large number of samples for this study. They also thank Xiaomei Chen for checking and recording the data.
Footnotes
Final revision submitted June 7, 2021; accepted June 16, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by the National Key R & D Program of China (No. 2017YFC1105000). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Southern Medical University (No. NFYKDXJCYXY2019031001).
References
- 1. Akatsuka Y, Teramoto A, Takashima H, Watanabe K, Yamashita T. Morphological evaluation of the calcaneofibular ligament in different ankle positions using a three-dimensional MRI sequence. Surg Radiol Anat. 2019;41(3):307–311. [DOI] [PubMed] [Google Scholar]
- 2. Anderson ME. Reconstruction of the lateral ligaments of the ankle using the plantaris tendon. J Bone Joint Surg AM. 1985;67(6):930–934. [PubMed] [Google Scholar]
- 3. Attarian DE, McCrackin HJ, Devito DP, McElhaney JH, Garrett WE, Jr. A biomechanical study of human lateral ankle ligaments and autogenous reconstructive grafts. Am J Sports Med. 1985;13(6):377–381. [DOI] [PubMed] [Google Scholar]
- 4. Balduini FC, Tetzlaff J. Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med. 1982;1(1):3–12. [PubMed] [Google Scholar]
- 5. Baumhauer JF, O’Brien T. Surgical considerations in the treatment of ankle instability. J Athl Train. 2002;37(4):458–462. [PMC free article] [PubMed] [Google Scholar]
- 6. Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34(6):975–978. [DOI] [PubMed] [Google Scholar]
- 7. Boey H, Verfaillie S, Natsakis T, Vander Sloten J, Jonkers I. Augmented ligament reconstruction partially restores hindfoot and midfoot kinematics after lateral ligament ruptures. Am J Sports Med. 2019;47(8):1921–1930. [DOI] [PubMed] [Google Scholar]
- 8. Broström L. Sprained ankles. 3. Clinical observations in recent ligament ruptures. Acta Chir Scand. 1965;130(6):560–569. [PubMed] [Google Scholar]
- 9. Burks RT, Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22(1):72–77. [DOI] [PubMed] [Google Scholar]
- 10. Buzzi R, Todescan G, Brenner E, et al. Reconstruction of the lateral ligaments of the ankle: an anatomic study with evaluation of isometry. J Sports Traumatol Relat Res. 1993;15(2):55–74. [Google Scholar]
- 11. Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69(1):17–26. [PubMed] [Google Scholar]
- 12. Chilvers M, Manoli A, 2nd. The subtle cavus foot and association with ankle instability and lateral foot overload. Foot Ankle Clin. 2008;13(2):315–324. [DOI] [PubMed] [Google Scholar]
- 13. Clanton TO, Campbell KJ, Wilson KJ, et al. Qualitative and quantitative anatomic investigation of the lateral ankle ligaments for surgical reconstruction procedures. J Bone Joint Surg Am. 2014;96(12):e98. [DOI] [PubMed] [Google Scholar]
- 14. de Vries JS, Krips R, Sierevelt IN, Blankevoort L. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2006;18(4):CD004124. [DOI] [PubMed] [Google Scholar]
- 15. Delfaut EM, Demondion X, Boutry N, et al. Multi-fasciculated anterior talo-fibular ligament: reassessment of normal findings. Eur Radiol. 2003;13(8):1836–1842. [DOI] [PubMed] [Google Scholar]
- 16. DiGiovanni CW, Brodsky A. Current concepts: lateral ankle instability. Foot Ankle Int. 2006;27(10):854–866. [DOI] [PubMed] [Google Scholar]
- 17. Edama M, Kageyama I, Kikumoto T, et al. Morphological features of the anterior talofibular ligament by the number of fiber bundles. Ann Anat. 2018;216:69–74. [DOI] [PubMed] [Google Scholar]
- 18. Edama M, Takabayashi T, Inai T, et al. Relationships between differences in the number of fiber bundles of the anterior talofibular ligament and differences in the angle of the calcaneofibular ligament and their effects on ankle-braking function. Surg Radiol Anat. 2019;41(6):675–679. [DOI] [PubMed] [Google Scholar]
- 19. Eldridge SM, Ashby D, Kerry S. Sample size for cluster randomized trials: effect of coefficient of variation of cluster size and analysis method. Int J Epidemiol. 2006;35(5):1292–1300. [DOI] [PubMed] [Google Scholar]
- 20. Erickson SJ, Smith JW, Ruiz ME, et al. MR imaging of the lateral collateral ligament of the ankle. AJR Am J Roentgenol. 1991;156(1):131–136. [DOI] [PubMed] [Google Scholar]
- 21. Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11(3):659–662. [DOI] [PubMed] [Google Scholar]
- 22. Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5(6):241–242. [DOI] [PubMed] [Google Scholar]
- 23. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. [DOI] [PubMed] [Google Scholar]
- 24. Girard P, Anderson RB, Davis WH, Isear JA, Kiebzak GM. Clinical evaluation of the modified Brostrom-Evans procedure to restore ankle stability. Foot Ankle Int. 1999;20(4):246–252. [DOI] [PubMed] [Google Scholar]
- 25. Golanó P, Vega J, de Leeuw PA, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):557–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability. A prospective, randomized comparison. Am J Sports Med. 1996;24(4):400–404. [DOI] [PubMed] [Google Scholar]
- 27. Ibrahim SA, Hamido F, AI Misfer AK, et al. Anatomical reconstruction of the lateral ligaments using Gracillis tendon in chronic ankle instability; a new technique. Foot Ankle Surg. 2011;17(4):239–246. [DOI] [PubMed] [Google Scholar]
- 28. Kakegawa A, Mori Y, Tsuchiya A, et al. Independent attachment of lateral ankle ligaments: anterior talofibular and calcaneofibular ligaments. J Foot Ankle Surg. 2019;58(4):717–722. [DOI] [PubMed] [Google Scholar]
- 29. Karlsson J, Bergsten T, Lansinger O, Peterson L. Surgical treatment of chronic lateral instability of the ankle joint. A new procedure. Am J Sports Med. 1989;17(2):268–273; discussion 273-274. [DOI] [PubMed] [Google Scholar]
- 30. Karlsson J, Eriksson BI, Bergsten T, Rudholm O, Swärd L. Comparison of two anatomic reconstructions for chronic lateral instability of the ankle joint. Am J Sports Med. 1997;25(1):48–53. [DOI] [PubMed] [Google Scholar]
- 31. Kelikian AS, Sarrafian SK. Sarrafian’s Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 32. Kirk KL, Campbell JT, Guyton GP, Parks BG, Schon LC. ATFL elongation after Brostrom procedure: a biomechanical investigation. Foot Ankle Int. 2008;29(11):1126–1130. [DOI] [PubMed] [Google Scholar]
- 33. Liu W, Li H, Hua Y. Quantitative magnetic resonance imaging (MRI) analysis of anterior talofibular ligament in lateral chronic ankle instability ankles pre- and postoperatively. BMC Musculoskelet Disord. 2017;18(1):397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lynch SA. Assessment of the injured ankle in the athlete. J Athl Train. 2002;37(4):406–412. [PMC free article] [PubMed] [Google Scholar]
- 35. MacAuley D. Ankle injuries: same joint, different sports. Med Sci Sports Exerc. 1999;31(7 suppl):S409–S411. [DOI] [PubMed] [Google Scholar]
- 36. Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16(10):608–615. [DOI] [PubMed] [Google Scholar]
- 37. Matsui K, Takao M, Tochigi Y, Ozeki S, Glazebrook M. Anatomy of anterior talofibular ligament and calcaneofibular ligament for minimally invasive surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1892–1902. [DOI] [PubMed] [Google Scholar]
- 38. Milner CE, Soames RW. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int. 1998;19(11):757–760. [DOI] [PubMed] [Google Scholar]
- 39. Neuschwander TB, Indresano AA, Hughes TH, Smith BW. Footprint of the lateral ligament complex of the ankle. Foot Ankle Int. 2013;34(4):582–586. [DOI] [PubMed] [Google Scholar]
- 40. O’Loughlin PF, Murawski CD, Egan C, Kennedy JG. Ankle instability in sports. Phys Sportsmed. 2009;37(2):93–103. [DOI] [PubMed] [Google Scholar]
- 41. Ozeki S, Yasuda K, Kaneda K, Yamakoshi K, Yamanoi T. Simultaneous strain measurement with determination of a zero strain reference for the medial and lateral ligaments of the ankle. Foot Ankle Int. 2002;23(9):825–832. [DOI] [PubMed] [Google Scholar]
- 42. Petersen W, Rembitzki IV, Koppenburg AG, et al. Treatment of acute ankle ligament injuries: a systematic review. Arch Orthop Trauma Surg. 2013;133(8):1129–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Raheem OA, O’Brien M. Anatomical review of the lateral collateral ligaments of the ankle: a cadaveric study. Anat Sci Int. 2011;86(4):189–193. [DOI] [PubMed] [Google Scholar]
- 44. Reed GF, Lynn F, Meade BD. Use of coefficient of variation in assessing variability of quantitative assays. Clin Diagn Lab Immunol. 2002;9(6):1235–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Roos KG, Kerr ZY, Mauntel TC, et al. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(1):201–209. [DOI] [PubMed] [Google Scholar]
- 46. Schenck RC, Jr, Coughlin MJ. Lateral ankle instability and revision surgery alternatives in the athlete. Foot Ankle Clin. 2009;14(2):205–214. [DOI] [PubMed] [Google Scholar]
- 47. Siegler S, Block J, Schneck CD. The mechanical characteristics of the collateral ligaments of the human ankle joint. Foot Ankle. 1988;8(5):234–242. [DOI] [PubMed] [Google Scholar]
- 48. Sindel M, Demir S, Yildirim A, Ucar Y. Anatomy of the lateral ankle ligaments. Turk J Med Sci. 1998;28(1):53–56. [Google Scholar]
- 49. Sitler M, Ryan J, Wheeler B, et al. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at West Point. Am J Sports Med. 1994;22(4):454–461. [DOI] [PubMed] [Google Scholar]
- 50. Taser F, Shafiq Q, Ebraheim NA. Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg Radiol Anat. 2006;28(4):391–397. [DOI] [PubMed] [Google Scholar]
- 51. Uğurlu M, Bozkurt M, Demirkale I, et al. Anatomy of the lateral complex of the ankle joint in relation to peroneal tendons, distal fibula and talus: a cadaveric study. Eklem Hastalik Cerrahisi. 2010;21(3):153–158. [PubMed] [Google Scholar]
- 52. van den Bekerom MP, Oostra RJ, Golanó P, van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat. 2008;21(7):619–626. [DOI] [PubMed] [Google Scholar]
- 53. Waldrop NE, 3rd, Wijdicks CA, Jansson KS, LaPrade RF, Clanton TO. Anatomic suture anchor versus the Broström technique for anterior talofibular ligament repair: a biomechanical comparison. Am J Sports Med. 2012;40(11):2590–2596. [DOI] [PubMed] [Google Scholar]
- 54. Walther M, Kriegelstein S, Altenberger S, et al. Lateral ligament injuries of the ankle joint. Unfallchirurg. 2013;116(9):776–780. [DOI] [PubMed] [Google Scholar]
- 55. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ, Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. [DOI] [PubMed] [Google Scholar]
- 56. Wenny R, Duscher D, Meytap E, Weninger P, Hirtler L. Dimensions and attachments of the ankle ligaments: evaluation for ligament reconstruction. Anat Sci Int. 2015;90(3):161–171. [DOI] [PubMed] [Google Scholar]
- 57. Woods C, Hawkins R, Hulse M, Hodson. The Football Association Medical Research Programme: an audit of injuries in professional football: an analysis of ankle sprains. Br J Sports Med. 2003;37(3):233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yıldız S, Yalcın B. The anterior talofibular and calcaneofibular ligaments: an anatomic study. Surg Radiol Anat. 2013;35(6):511–516. [DOI] [PubMed] [Google Scholar]



