Abstract
Background:
Mortality in single ventricle cohorts remains high with multiple associated factors. The effect of heart block during stage I palliation remains unclear.
Objectives:
To study patient and surgical risks for heart block and its effect on transplant-free 12-month survival in single ventricle patients.
Methods:
Patient, surgical, outcome data and heart block status (transient and permanent) were obtained from the NPC-QIC single-ventricle database. Bivariate analysis was performed comparing patients with and without heart block and multivariable modelling used to identify variables associated with block. One year outcomes were analyzed to identify variables associated with lower 12 month transplant-free survival.
Results:
In total, 1,423 patients were identified, of which 28 (2%) developed heart block (second degree or complete) during their surgical admission. Associated risk factors for block included heterotaxy syndrome (OR 6.4) and atrial flutter/fibrillation (OR 3.8). Patients with heart block had lower 12 month survival though only in patients with complete heart block as opposed to second degree block. At 12 months of age, 39% of heart block patients died and were more likely to experience mortality at 12 months compared to patients without block (OR 4.9, 95%CI 1.4,17.5, p=0.01).
Conclusions:
Though rare, complete heart block following stage I palliation represents an additional risk for poor outcomes among this high risk patient population. Heterotaxy syndrome was the most significant risk factor for development of heart block following stage 1 palliation. The role of transient block on outcomes and potential rescue with long term pacing remains unknown and requires additional study.
Keywords: Heart block, Hypoplastic left heart syndrome, Pediatric cardiology, Stage I Palliation, Survival
Introduction
Staged surgical palliation of patients with single ventricle has undergone significant advancement over the past decades, though morbidity and mortality remain significant.(1–3) Although rare in single ventricle patients, concomitant heart block adds complexity and potential risks for pediatric patients with congenital heart disease. The incidence of heart block in large single ventricle populations is poorly defined, but in the literature has been reported in ~ 4–11%.(4,5) Surgical and patient characteristics such as heterotaxy syndrome and the need for additional atrioventricular valve surgery have been postulated mechanistic drivers associated with heart block in single ventricle populations but data remains sparse in large cohorts, particularly surrounding Stage I palliation (S1P).(6–8) Patients with permanent heart block typically require long term ventricular pacing and pacemaker implantation which has been associated with progressive ventricular dysfunction in older age Fontan cohorts.(7,9) In younger single ventricle cohorts, the associated consequences of heart block and the deleterious effects of chronic ventricular pacing is unknown. In recent data from the Pediatric Heart Network and additional small retrospective studies, patients with perioperative heart block have had decreased transplant free survival to Stage II palliation compared to those without heart block, though the mechanisms are unclear and survival past the second stage palliation is unknown.(4,5,10,11) This study seeks to address the current gaps in the literature surrounding the risk and long term outcomes for patients with single ventricle heart disease with post/perioperative heart block following S1P to inform care for this high risk population.
Methods
The National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) is a learning health network composed of over 60 pediatric care centers developed to improve outcomes for patients with hypoplastic left heart syndrome (HLHS) and variants. The NPC-QIC includes a voluntary registry with a standard dataset with data definitions, online web-based data entry, and data quality checks. Institutional review board approval and parental consent or waiver of consent is maintained by individual centers participating in the NPC-QIC database. Additional approval was obtained at Cincinnati Children’s Hospital Medical Center for this study #2020–0001 (4/22/2020). The research reported in this paper adhered to Helsinki Declaration guidelines. Phase I NPC-QIC data captures patient, surgical and outcome data from birth through the interstage period and admission for Stage II palliation for patients discharged after S1P. Phase II data includes all variables from phase I and expands upon this data with additional patient data through 12 months of age including all patients deemed to need a S1P, regardless of discharge status.
Study Population
All patients included in the NPC-QIC with phase II data were included in the initial analysis. To be included in the data set patients must: 1) have HLHS or variant single ventricle disease and 2) need either Norwood procedure (BT shunt, central shunt or RV-PA conduit), Damus-Kaye-Stansel (DKS) or hybrid procedure.
Perioperative Stage I Palliation and Interstage Variables
Data were collected for all patients from birth through admission for second stage palliation including variables in the interstage time period. Patient characteristics including sex, race, primary cardiac diagnosis, additional major congenital anomalies, and heterotaxy status were collected. Surgical and perioperative variables were collected including type of surgical palliation, requirement for additional AV valve repair. Post-surgical and interstage variables were collected including patient ventricular function on the echocardiogram prior to discharge, hospital length of stay (LOS) and whether a patient required readmission following discharge from their stage I surgical palliation and prior to their second stage palliation. Patients with heart block were noted during the initial hospital admission for stage I surgical palliation. The database included variables for heart block, including a separate variable for second and third degree heart block, and patients could have both occur during their hospitalization. Data on first degree heart block was not collected. The registry does not denote whether heart block was permanent or transient only that it was present at some point following stage I surgical palliation. Patients with perioperative heart block were defined as having either second or third degree heart block, with additional sub-analysis performed based on heart block type. Separate discrete variables for pacemaker implant during or after stage I surgical admission were collected.
12 Month Patient Outcome Data
Patients equal to or greater than one year from the date of birth were identified and discrete outcome variables are denoted in the database including: survival, death prior to discharge from stage I palliation, interstage death, death following stage II palliation, heart transplantation and “other death”. Only patients with this outcome variable at 1 year of age were included in this 12 month analysis and data is censored at 12 months. Peri-operative data including patient age, weight and length of stay were collected in the cohort of patients surviving to 12 months of age.
Statistics
Data were examined for feasibility and correctness, and any data point which was not possible, or feasible was set to missing. Bivariate analysis was initially performed to compare patients with and without heart block to identify patient, surgical and outcome differences between the patient cohorts and variables associated with heart block. Additional bivariate analyses were performed to evaluate survival to stage II palliation as well 12 month survival in the sub-cohort of patients 1 year of age or greater. Χ2 test or Fisher’s exact test were used for categorical variables and Student’s t test or Wilcoxon rank sums test was used for continuous variables as appropriate. Based on bivariate analyses, separate models for risk of heart block during stage I admission and risk of death prior to 12 months were created. Survival analysis was performed, comparing survival in patients with/without HB, and also comparing pacemaker placement/not in patients having HB. Logrank tests for equality over strata were performed, and Kaplan-Meier curves were plotted for visual display of this analysis. All analyses were performed using SAS Version 9.4 (SAS®Institute Inc., Cary, NC, USA).
Results
Patient and Surgical Factors Associated with Heart Block
In total, 1,423 single ventricle patients were identified having undergone stage I palliation within the phase II cohort contained in the NPC-QIC database (July 2008 - August 2020). Heart block was seen in 2% (28 patients) of this cohort.(Table 1) Of the patients with heart block, 14 had second degree block, 12 had complete heart block and 2 patients had both second and complete heart block seen during their admission. In general, patients with heart block were less frequently black/African American, were less likely on digoxin at time of discharge and were older at the time of Stage I discharge (p≤0.05). Heart block patients were more likely to have heterotaxy syndrome and atrial flutter and had an increased mortality compared to patients without heart block (p=0.001). Of the 28 patients with heart block, 8 patients (29%) underwent pacemaker implant prior to stage I discharge. Of the 8 patients with heart block who underwent pacemaker implantation, 4 patients had second degree heart block and 4 had complete heart block. Twenty patients with heart block did not have pacemaker implantation including 10 patients with complete heart block. Three patients underwent pacemaker implantation without heart block. One patient had atrial tachycardia and the remaining 2 patients had no additional arrhythmia coding. Pacemaker implantation was more frequent in patients with heart block (8 patients (29%)) vs. those without heart block (3 patients, (0.2%, p=<0.0001)). One additional patient was readmitted in the interstage period for pacemaker implant in each cohort.
Table 1.
Patient and Surgical Characteristics in Patients with and without Heart Block
| Heart Block (n=28) |
No Heart Block (n=1395) |
P-value | |
|---|---|---|---|
| Stage I Palliation Data, mean±SD | |||
| Age at time of Stage I Palliation (days) | 13.7±18 | 9.6±16 | 0.08 |
| Weight at Stage I Palliation (kg) | 3.2±0.6 | 3.3±0.6 | 0.8 |
|
| |||
| Stage II Palliation Data, mean±SD | |||
| Age at time of Stage II Palliation (days) | 183.3±67 | 152.6±45 | 0.03 |
| Weight at Stage II Palliation (kg) | 6.5±1 | 6.2±1 | 0.2 |
|
| |||
| Female, n (%) | 12 (43%) | 554 (40%) | 0.9 |
|
| |||
| Race, n (%) | |||
| White | 18 (64%) | 958 (69%) | |
| Black-African American | 2 (7%) | 214 (15%) | |
| Asian | 2 (7%) | 8 (1%) | 0.05 |
| American Indian | 1 (4%) | 10 (1%) | |
| Other | 5 (18%) | 213 (15%) | |
|
| |||
| Primary Diagnosis, n (%) | |||
| Hypoplastic Left Heart Syndrome | 19 (68%) | 1037 (74%) | |
| Double Inlet Left Ventricle | 2 (7%) | 69 (5%) | |
| Double Inlet Right Ventrcle | 0 (0%) | 4 (0%) | |
| Mitral Atresia | 0 (0%) | 29 (2%) | |
| Tricuspid Atresia | 0 (0%) | 44 (3%) | 0.6 |
| Unbalanced Atrio-ventricular Canal | 2 (7%) | 76 (5%) | |
| Doutlet Outlet Right Ventrcle | 0 (0%) | 12 (1%) | |
| Single Ventricle Other | 1 (4%) | 46 (3%) | |
| Other | 4 (14%) | 86 (6%) | |
|
| |||
| Heterotaxy Syndrome, n (%) | 3 (11%) | 26 (2%) | 0.02 |
|
| |||
| Major Congenital Anomaly of Other Organ, n (%) | 4 (14%) | 92 (7%) | 0.2 |
|
| |||
| Type of Surgery, n (%) | |||
| Norwood with BTS | 6 (21%) | 379 (27%) | |
| Norwood with RV-PA Conduit | 18 (64%) | 776 (56%) | |
| Hybrid Procedure | 2 (7%) | 106 (8%) | |
| Norwood Central Shunt | 0 (0%) | 15 (1%) | 0.6 |
| DKS with BT Shunt | 0 (0%) | 27 (2%) | |
| DKS with RV-PA Conduit | 2 (7%) | 50 (4%) | |
| Other | 0 (0%) | 42 (3%) | |
|
| |||
| Additional AV Valve Repair, n (%) | 2 (7%) | 34 (2%) | 0.2 |
|
| |||
| Post Operative Rhythm Abnormalities, n (%) | |||
| Atrial Flutter | 3 (11%) | 44 (3%) | 0.03 |
| Chaotic Atrial Rhythm | 0 (0%) | 9 (1%) | 0.6 |
| Ectopic Atrial Tachycardia | 3 (11%) | 135 (10%) | 0.8 |
| Junctional Ectopic Atrial Tachycardia | 1 (4%) | 66 (5%) | 0.8 |
| Re-entrant SVT | 3 (11%) | 152 (11%) | 1 |
| Sinus Bradycardia | 0 (0%) | 50 (4%) | 0.3 |
| Ventricular Fibrillation | 0 (0%) | 12 (1%) | 0.6 |
| Ventricular Tachycardia | 3 (11%) | 58 (4%) | 0.2 |
|
| |||
| Pacemaker Implant Prior to Discharge, n (%) | 8 (29%) | 3 (0%) | <0.0001 |
|
| |||
| Ventricular Function Prior to Stage I Discharge, n (%) | |||
| Normal or low normal | 11 (39%) | 997 (71%) | |
| Mild Dysfunction | 1 (4%) | 63 (5%) | |
| Moderate Dysfunction | 0 (0%) | 18 (1%) | 0.7 |
| Severe Dysfunction | 0 (0%) | 4 (0%) | |
| No information | 1 (4%) | 15 (1%) | |
|
| |||
| Digoxin at Discharge, n (%) | 9 (32%) | 755 (54%) | 0.02 |
|
| |||
| Death, n (%) | 11 (39%) | 225 (16%) | 0.001 |
Based on bivariate modelling and plausible relationship to heart block, race (black/African American), presence of heterotaxy syndrome and history of atrial flutter/fibrillation were included in the initial multivarible logistic regression modelling for heart block. Heterotaxy syndrome (OR 6.4(1.8–22.7), p=0.005) and history of atrial flutter/fibrillation (OR 3.8(1.1–13.0), p=0.04) were independently associated with heart block during stage I admission while race was not. (Table 2)
Table 2.
Multivariable Model of Associated Risks of Heart Block and Death Prior to 12 Months
| Odds Ratio (95%CI) | p-value | |
|---|---|---|
| Associated Risk for Heart Block During Stage I Admission | ||
| Heterotaxy Syndrome | 6.4 (1.8–22.7) | 0.004 |
| Atrial Flutter/fibrillation | 3.8 (1.1–13.0) | 0.04 |
|
| ||
| Associated Risk of Death Prior to 12 Months | ||
| Heart Block | 4.9 (1.4–17.5) | 0.01 |
| Non-cardiac Syndrome | 1.7 (1.1–2.5) | 0.01 |
| Hybrid Procedure | 2.4 (1.5–3.7) | <0.001 |
| Digoxin Usage | −3.8 (2.9–5.1) | <0.001 |
Associated Outcomes of Patients with Heart Block
In the cohort of patients with heart block, death or transplant prior to Stage II palliation was 39%, with the majority of those deaths occurring prior to stage I discharge (21%). (Table 3) Comparing patients with heart block to those without, patients with heart block were older at the time of stage I discharge (62.4 vs. 38 days, p=0.05) but had similar Stage 1 LOS (p=0.1). Patients with heart block were more likely to be admitted through the interstage period (p=0.003) and have an unanticipated readmission in the interstage period for pacemaker implantation (4% vs. 0%, p=<0.0001). Patients with heart block were more likely to have an outcome of death (39% vs. 16%, p=0.001) but not transplantation (4% vs. 4%, p=0.9) compared to those patients without heart block. In addition to a lower associated survival, patients with heart block were also more likely to have death prior to discharge from Stage I palliation (21% vs. 9%, p=0.02) than patients without heart block.(Figures 1 and 2) Despite the presence of heart block, no patient in the heart block group was felt to have an ultimate cause of death directly attributable to arrhythmia.
Table 3.
Outcomes Based on the Presence/Absence of Heart Block
| Heart Block | No Heart Block | P-value | |
|---|---|---|---|
| Stage I Palliation Length of Stay | 45.2+30 | 38.2+27 | 0.1 |
|
| |||
| Age at Discharge Stage I (days) | 62.4±40 | 47±31 | 0.05 |
|
| |||
| Patient Weight At Discharge Stage I (kg) | 3.9±1 | 3.8±1 | 0.3 |
|
| |||
| Sage II Palliation Length of Stay | 31.0+63 | 18.7+23 | 0.4 |
|
| |||
| Remained Inpatient to Stage II Palliation | 8 (29%) | 152 (11%) | 0.003 |
|
| |||
| Unanticipated Interstage Readmission | 5 (18%) | 485 (35%) | 0.4 |
|
| |||
| Admission with PCM Implant | 1 (4%) | 1 (0%) | <0.0001 |
|
| |||
| Outcomes | |||
| Survive to 12 months | 16 (57%) | 1100 (79%) | 0.002 |
| Heart Transplant | 1 (4%) | 59 (4%) | 0.9 |
|
| |||
| Survival Outcome Comparison | |||
| Survive to 12 months | 16 (57%) | 1100 (79%) | 0.002 |
| Death Prior to Discharge | 6 (21%) | 127 (9%) | |
| Interstage Death | 1 (4%) | 48 (3%) | |
| Death post Stage II | 0 (0%) | 14 (1%) | |
| Heart Transplant | 1 (4%) | 59 (4%) | |
| Other death | 4 (14%) | 36 (3%) | |
|
| |||
| Cause of Death Arrhythmia, n (%) | 0 (0%) | 9 (1%) | 0.5 |
Figure 1.
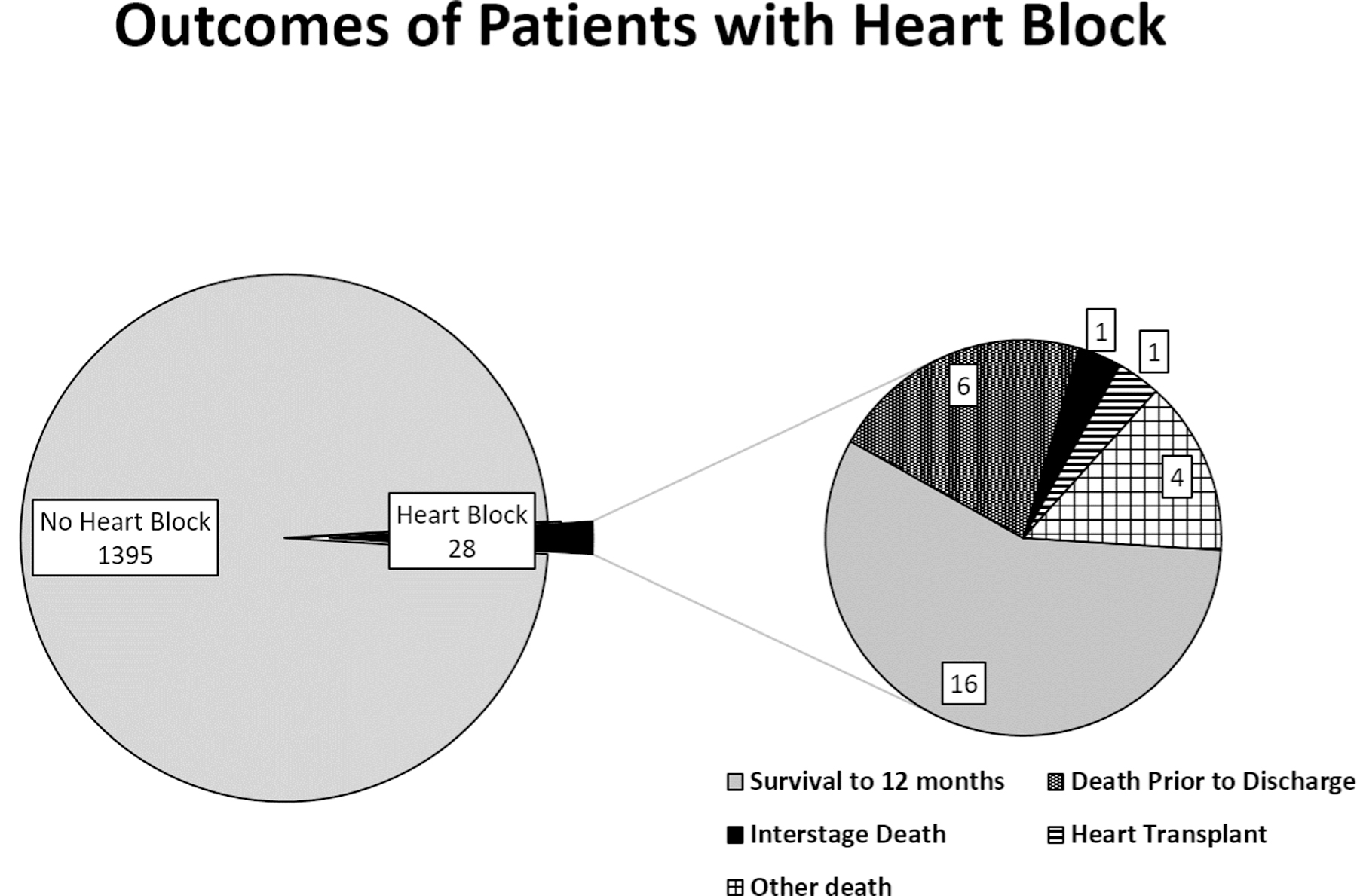
Outcomes of Patients with Heart Block
The orange wedge represents the 2% of the total population with heart block at Stage I palliation.
Figure 2.
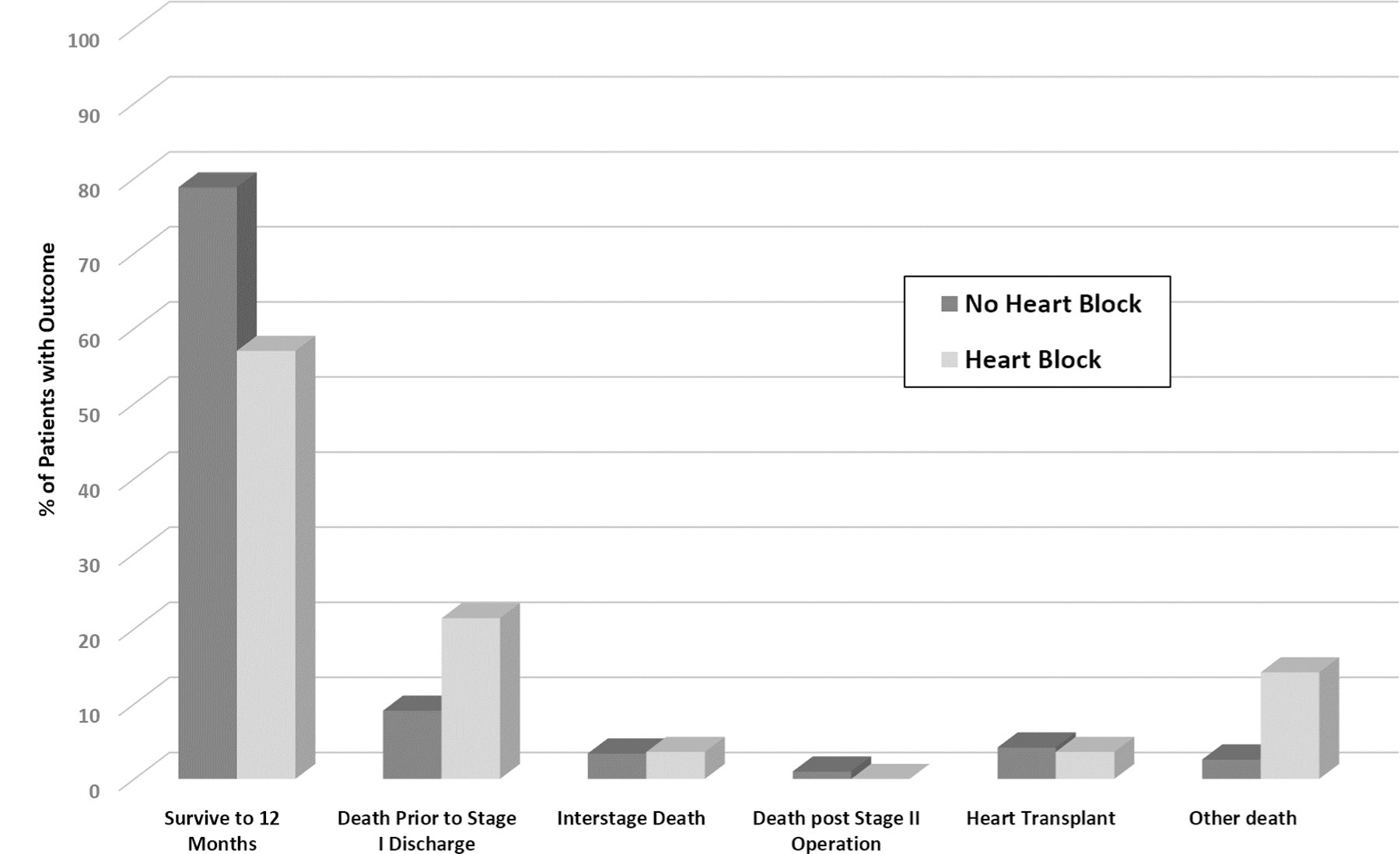
Comparative Outcomes in Patients with and without Heart Block
The blue bar represents patients with no heart block. The orange bar represents patients with heart block during stage I palliation.
Variables Associated with Death or Transplant at 12 Months of Life
A total of 1,195 patients were 12 months or older at the time of analysis. In total, 24% (288 individuals) either died or were transplanted prior to the first year of life. Survival to 12 months of life was seen in only 57% in the cohort of patients with heart block compared to 79% in those without heart block. (Figure 3a) Heart block was seen more frequently in the death/transplant population than surviving patients (4% vs 1%, p=0.006).(Table 4) In comparison of heart block type, third degree heart block was associated with death or transplant (3% vs. 0.4%, p=0.0007) though second degree heart block was not (2% vs. 1%, p=0.3). Patients with third degree heart block had worse survival compared to those with second degree heart block. (Figure 3b) Heart block patients with a pacing system had slightly lower mortality than those without, though not statistically significant. In addition to heart block, primary diagnosis, the presence of a major syndrome or congenital anomaly, and surgical type were associated with death or transplantation prior to 12 months of age. A total of 10 pacemakers were implanted during stage I admission and 1 implanted in the interstage period, with no difference in associated transplant free 12 month survival (p=0.3).(Figure 3c) On multivariable analysis, heart block (OR 4.9 (1.8–17.5), p=0.01), the presence of an additional non-cardiac syndrome (OR 1.7 (1.1–2.5, p=0.01) and hybrid procedure (OR 2.4 (1.5–3.7), p=0.0001) were associated with increased risk of death while the use of digoxin at Stage I discharge (OR 3.8(2.9–5.1), p=<0.0001) was associated with increased survival. (Table 2)
Figure 3.
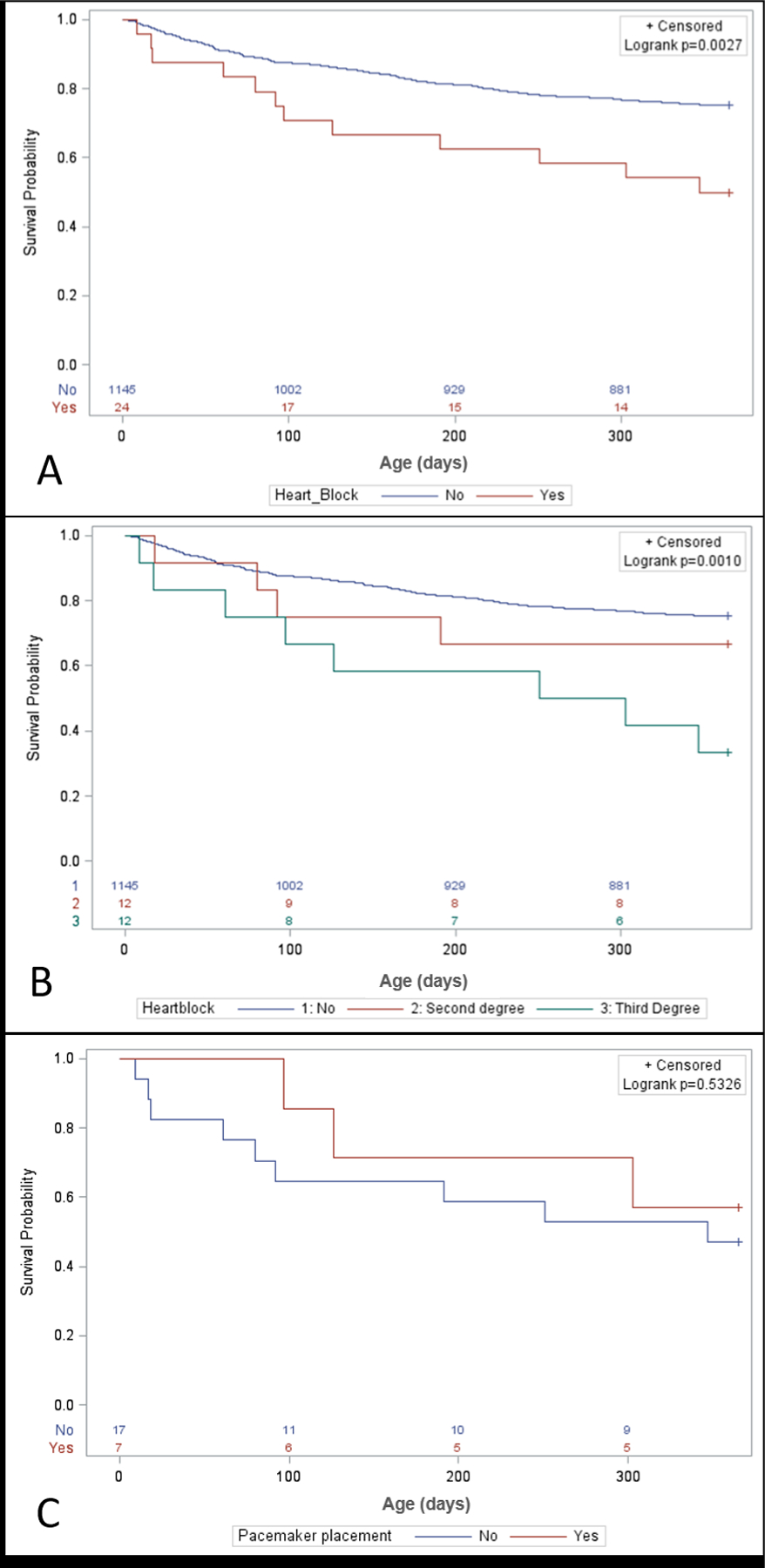
Outcomes of Patients with Heart Block by Heart Block Type and Pacemaker
A. Kaplan Meier Curve comparing patients with and without heart block over the first 12 months of life.
B. Kaplan Meier Curve comparing patients by degree of heart block.
C. Kaplan Meier Curve comparing heart block patients by the presence or absence of a permanent pacing system.
D. Kaplan Meier Curve comparing patients with 1) heterotaxy syndrome with no heart block; 2) patients with second degree heart block and 3) patients with third degree heart block.
Table 4.
Survival Comparison at 12 Months of Life
| - | Survival (n=907) |
Death/ Transplant (n=288) |
P-value |
|---|---|---|---|
| Female, n(%) | 344 (38%) | 132 (46%) | 0.1 |
|
| |||
| Race | |||
| White | 629 (69%) | 193 (67%) | 0.1 |
| Black-African American | 143 (16%) | 40 (14%) | |
| Asian | 5 (1%) | 3 (1%) | |
| American Indian | 5 (1%) | 4 (1%) | |
| Other | 125 (14%) | 56 (19%) | |
|
| |||
| Primary Diagnosis | |||
| Hypoplastic Left Heart Syndrome | 664 (73%) | 227 (79%) | 0.02 |
| Double Inlet Left Ventricle | 49 (5%) | 5 (2%) | |
| Double Inlet Right Ventricle | 2 (2%) | 1 (0%) | |
| Mitral Atresia | 18 (2%) | 6 (2%) | |
| Tricuspid Atresia | 31 (3%) | 4 (1%) | |
| Unbalanced Atrioventricular Canal | 43 (5%) | 24 (8%) | |
| Double Outlet Right Ventricle | 2 (0%) | 2 (1%) | |
| Single Ventricle Other | 35 (39%) | 7 (2%) | |
| Other | 63 (7%) | 20 (7%) | |
|
| |||
| Major Syndrome | 88 (10%) | 56 (19%) | <0.0001 |
|
| |||
| Heterotaxy Syndrome | 19 (2%) | 7 (2%) | 0.8 |
|
| |||
| Major Congenital Anomaly of Other Organ | 51 (6%) | 36 (13%) | 0.0002 |
|
| |||
| Type of Surgery | |||
| Norwood with BTS | 259 (29%) | 64 (22%) | <0.0001 |
| Norwood with RV-PA Conduit | 500 (55%) | 147 (51%) | |
| Norwood Central Shunt | 8 (1%) | 3 (1%) | |
| Hybrid Norwood | 58 (6%) | 47 (16%) | |
| DKS with BT Shunt | 22 (2%) | 4 (1%) | |
| DKS with RV-PA Conduit | 39 (4%) | 9 (3%) | |
| Other | 21 (3%) | 14 (5%) | |
|
| |||
| Additional AV Valve Repair (Y/N) | 18 (2%) | 13 (1%) | 0.02 |
|
| |||
| Post Operative Rhythm Abnormalities Heart Block | 282 (31%) | 130 (45%) | <0.0001 |
| Any Heart Block | 13 (1%) | 12 (4%) | 0.006 |
| 2nd degree | 9 (1%) | 5 (2%) | 0.3 |
| 3rd degree | 4 (0.4%) | 8 (3%) | 0.0007 |
|
| |||
| Pacemaker Implant | 6 (1%) | 4 (1%) | 0.3 |
|
| |||
| Ventricular Function Prior to Stage I Discharge | |||
| Normal or low normal | 729 (80%) | 99 (34%) | |
| Mild Dysfunction | 50 (6%) | 10 (3%) | |
| Moderate Dysfunction | 18 (2%) | 2 (1%) | 0.3 |
| Severe Dysfunction | 2 (0%) | 1 (0%) | |
| No information | 16 (2%) | 0 (0%) | |
|
| |||
| Digoxin at Discharge | 550 (61%) | 79 (27%) | <0.0001 |
|
| |||
| Readmission after Stage I Discharge for PCM | 0 | 1 | 0.1 |
Discussion
Perioperative heart block in single ventricle patients is relatively rare but is associated with significant potential morbidity and mortality.(12) Patients with permanent heart block require long term ventricular pacing and pacemaker implantation, which has been associated with long term ventricular dysfunction in older age Fontan cohorts.(7,9) Additionally, in those patients with early recovery of AV nodal function after transient heart block, the recurrence risk of heart block is unknown. In this study, the overall risk of heart block in this large cohort of patients was ~2% and associated with markedly lower 12 month survival particularly in patients with complete heart block as opposed to second degree block. In this diverse population, heterotaxy and atrial arrhythmias were associated with heart block surrounding stage I palliation.
While the exact incidence of heart block in larger single ventricle populations is unclear, in the reported literature it has been seen in 4–11%.(4) In this study of patients from a diverse hospital and regional mix, the incidence of heart block was slightly lower than previously reported at ~ 2%. Whether this difference is secondary to the larger cohort size and more diverse patient make up is unknown, but is likely to represent a reasonable incidence of heart block in the current era. Interestingly, this data also differed from prior studies with regard to factors associated with heart block around stage I palliation. In recent data from the Pediatric Heart Network, the need for additional AV valve surgery during the stage I admission was found to be associated with heart block, though this association was not seen in the single ventricle sub population.(4–6) Despite a similar incidence in need for additional tricuspid valve surgery, it accounted for only 7% of heart block patients in this cohort as compared to 15% in the previous studies.(4,5) Similarly, while heterotaxy syndrome in non-single ventricle populations has been demonstrated to be associated with a variety of conduction system diseases, smaller studies have not demonstrated a link between heart block and heterotaxy, and larger studies have not evaluated the relationship in this population. This study demonstrated a strong relationship between heterotaxy syndrome and heart block and future studies evaluating the mechanistic drivers may be warranted.(6) The relationship between heart block and atrial arrhythmias is of interest though the cause/effect relationship is unclear. Whether heart block is driving secondary atrial arrhythmias or there is a yet undetermined secondary factor driving the relationship is difficult to determine. While patients with heart block may be more likely to have atrial arrhythmias secondary to resultant hemodynamic embarrassment or possibly secondary to the need for associated pacing, a direct cause and effect cannot be determined from this dataset and requires additional study.
The deleterious effects of heart block and chronic ventricular pacing have been difficult to delineate in the early care of single ventricle populations secondary to small patient cohorts. In several smaller studies, heart block and requirement for pacing has been evaluated in the interstage period but this has not been studied at later time points. In addition to worse survival, heart block was also associated with interstage readmission underscoring the increased complexity of this population throughout their care cycle. Difference between this and prior data may stem from prior studies’ significant limitation of using a broad definition of heart block without delineation between second and third degree heart block.(4,9) In this study, early heart block during stage I palliation was found to have increased risk for death out to 12 months of life, but of importance, this risk seemed to be restricted to patients with complete or third degree heart block rather than in patients with second degree block.
Interestingly, only 29% of patients with heart block underwent permanent pacemaker implant. The placement of a permanent pacing system was not statistically significant, but did show a non-significant improved 12 month outcome. This sub-cohort comparison was extremely small and not adequately powered and given pacing is the only current feasible treatment option, this needs further study. Unfortunately, transient heart block with return of normal AV nodal conduction is not specifically captured in the database. What role transient heart block or the recurrence of transient heart block plays in 12 month outcomes remains unknown, though only a single patient in the heart block cohort was readmitted after stage 1 discharge for pacemaker implantation. While it would be assumed that single ventricle patients with complete heart block were not discharged to home without stable pacing, a greater proportion of patients with heart block did remain admitted through the interstage period. What role heart block played in that decision and whether the presence of transient heart block or persistent second degree heart block was felt to place patients at high risk and led to lack of interstage discharge is unknown and requires additional study.
Limitations
There are several limitations, primarily related to use of large databases and the rarity of heart block. While allowing for a broad perspective of patients from different centers, analysis is limited to collected data fields. Several variables of interest were unable to be analyzed. One of these variables was the duration and persistence (transient vs. permanent) of 3rd degree heart block, particularly in patients who did not receive pacemaker implantation. While we would presume it unlikely for a single ventricle patient to be discharged with complete heart block without stable pacing, the duration of the heart block would be of interest and will require additional evaluation. Due to the low rate of heart block, confidence intervals around the odds ratios remain wide.
Conclusions
Single ventricle patients with complete heart block during stage I palliation are a particularly high risk group of patients. The presence of heterotaxy syndrome was the only identified mechanistic driver associated with heart block in this cohort and adds to the complexity of this patient population. Heart block was associated with lower transplant free survival though only in the sub-cohort of patients with third degree heart block as opposed to patients with second degree block. The role of transient heart block in deleterious outcomes and potential rescue with long term pacing remains unknown and requires additional study.
Acknowledgements
1. Current funding sources for National Pediatric Cardiology Quality Improvement Collaborative include (1) participation fees from enrolled centers; (2) a grant from the Children’s Heart Association of Cincinnati; (3) a federal grant to the pediatric Center for Education and Research in Therapeutics at Cincinnati Children’s Hospital Medical Center, funded by the federal Agency for Healthcare, Research and Quality [#U19HS021114 AHRQ]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
2. This work was conducted with support from the Heart Institute Research Core (HIRC) at Cincinnati Children’s Hospital.
3. Dr. Jayaram is supported by a CTSA grant from NCATS awarded to the University of Kansas for Frontiers: University of Kansas Clinical and Translational Science Institute # KL2TR002367. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or NCATS.
Abbreviations/Glossary
- NPC-QIC
National Pediatric Cardiology Quality Improvement Collaborative
- S1P
Stage 1 palliation
- HLHS
hypoplastic left heart syndrome
- LOS
Length of stay
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COI/Disclosures: None of the authors have financial disclosures of conflicts or industry relationships of interest with the given manuscript.
References
- 1.Brown DW, Mangeot C, Anderson JB et al. Digoxin Use Is Associated With Reduced Interstage Mortality in Patients With No History of Arrhythmia After Stage I Palliation for Single Ventricle Heart Disease. J Am Heart Assoc 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahle WT, Spray TL, Wernovsky G, Gaynor JW, Clark BJ 3rd. Survival after reconstructive surgery for hypoplastic left heart syndrome: A 15-year experience from a single institution. Circulation 2000;102:III136–41. [DOI] [PubMed] [Google Scholar]
- 3.Frommelt PC, Guey LT, Minich LL et al. Does initial shunt type for the Norwood procedure affect echocardiographic measures of cardiac size and function during infancy?: the Single Vventricle Reconstruction trial. Circulation 2012;125:2630–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oster ME, Chen S, Dagincourt N et al. Development and impact of arrhythmias after the Norwood procedure: A report from the Pediatric Heart Network. J Thorac Cardiovasc Surg 2017;153:638–645 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mah DY, Cheng H, Alexander ME et al. Heart block following stage 1 palliation of hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 2016;152:189–94. [DOI] [PubMed] [Google Scholar]
- 6.Niu MC, Dickerson HA, Moore JA et al. Heterotaxy syndrome and associated arrhythmias in pediatric patients. Heart Rhythm 2018;15:548–554. [DOI] [PubMed] [Google Scholar]
- 7.Kodama Y, Kuraoka A, Ishikawa Y et al. Outcome of patients with functional single ventricular heart after pacemaker implantation: What makes it poor, and what can we do? Heart Rhythm 2019;16:1870–1874. [DOI] [PubMed] [Google Scholar]
- 8.Alsoufi B, McCracken C, Schlosser B et al. Outcomes of multistage palliation of infants with functional single ventricle and heterotaxy syndrome. J Thorac Cardiovasc Surg 2016;151:1369–77 e2. [DOI] [PubMed] [Google Scholar]
- 9.Hall SJ, Cullington D, Thomson JDR, Bentham JR. Permanent pacing post-Fontan is not associated with reduced long-term survival. Cardiol Young 2019:1–3. [DOI] [PubMed]
- 10.Trivedi B, Smith PB, Barker PC, Jaggers J, Lodge AJ, Kanter RJ. Arrhythmias in patients with hypoplastic left heart syndrome. Am Heart J 2011;161:138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilhelm CM, Paulus D, Cua CL et al. Arrhythmias Following Comprehensive Stage II Surgical Palliation in Single Ventricle Patients. Pediatr Cardiol 2016;37:552–7. [DOI] [PubMed] [Google Scholar]
- 12.Buelow MW, Rudd N, Tanem J, Simpson P, Bartz P, Hill G. Reintervention following stage 1 palliation: A report from the NPC-QIC Registry. Congenit Heart Dis 2018;13:919–926. [DOI] [PubMed] [Google Scholar]


