Abstract
Objective
A consortium of 8 academic child and adolescent psychiatry programs in the United States and Canada examined their pivot from in-person, clinic-based services to home-based telehealth during the COVID-19 pandemic. The aims were to document the transition across diverse sites and to present recommendations for future telehealth service planning.
Method
Consortium sites completed a Qualtrics survey assessing site characteristics, telehealth practices, service use, and barriers to and facilitators of telehealth service delivery prior to (pre) and during the early stages of (post) the COVID-19 pandemic. The design is descriptive.
Results
All sites pivoted from in-person services to home-based telehealth within 2 weeks. Some sites experienced delays in conducting new intakes, and most experienced delays establishing tele−group therapy. No-show rates and use of telephony versus videoconferencing varied by site. Changes in telehealth practices (eg, documentation requirements, safety protocols) and perceived barriers to telehealth service delivery (eg, regulatory limitations, inability to bill) occurred pre−/post−COVID-19.
Conclusion
A rapid pivot from in-person services to home-based telehealth occurred at 8 diverse academic programs in the context of a global health crisis. To promote ongoing use of home-based telehealth during future crises and usual care, academic programs should continue documenting the successes and barriers to telehealth practice to promote equitable and sustainable telehealth service delivery in the future.
Key words: COVID-19, telemedicine, videoconferencing, ambulatory care
The World Health Organization declared COVID-19 a public health emergency of international concern on January 30, 2020,1 and declared it a pandemic on March 11, 2020. In response, local, state, and provincial governments recommended restrictions on in-person gatherings, issued “shelter-in-place” orders, and provided guidelines for social distancing to slow the spread of infection. This rapid transition drove significant changes in mental health care service delivery, propelling telehealth to the forefront, as both patients and providers spent increasing amounts of time sheltering at home.
At the federal level in the United States, multiple legal, regulatory, and reimbursement changes facilitated shifts in health care service delivery. The Office for Civil Rights (OCR) of the Department of Health and Human Services announced that it would “exercise its enforcement discretion” and “not impose penalties for noncompliance with the regulatory requirements” under the Health Insurance and Portability Accountability Act (HIPAA).2 , 3 This flexibility covered health care providers in connection with the good faith provision of telehealth (ie, real-time, interactive services delivered directly to patients through telephone and/or videoconferencing) specifically during the pandemic.3 The OCR indicated, under this notice, that health care providers could use non−public facing popular applications that allow for videoconferencing to provide telehealth services without risk of the OCR seeking to impose a penalty for noncompliance with the HIPAA Rules. The Drug Enforcement Administration (DEA) adopted policies during the pandemic allowing DEA-registered providers to prescribe controlled substances without an in-person examination.4 Most states modified their licensure requirements during the crisis, with significant state-by-state variability.5 The Centers for Medicare and Medicaid Services (CMS) expanded telehealth reimbursement during the pandemic, including expanding coverage for psychotherapy, assessment, and intervention, as well as other behavioral health services to be delivered via telephone.6
In Canada, health care is primarily under the jurisdiction of the provinces, and thus similar regulatory changes were made at the provincial level. In response to the COVID-19 pandemic, all provinces made necessary regulatory changes to allow telephony and videoconferencing care from home.7 Similar to the United States, previous restrictions on the type of platform used to communicate with patients were lifted. Unlike the United States, there were no changes in restrictions related to prescribing controlled substances or interprovince licensing requirements.
The rapid transition from in-person clinic-based services to home-based telehealth, with patients and the majority of providers at home, posed significant challenges to academic psychiatry programs. Prior to COVID-19, most mental health programs in academic medical centers did not have clinic-based telehealth programs.8 , 9 Of those with established telehealth programs, most had not offered telehealth services into patients’ homes, and very few allowed both providers and patients to be at home. As such, at the onset of the COVID-19 pandemic many programs had to develop new protocols and to increase provider competency for home-based telehealth service delivery with little time or experience.
Home-based telehealth is likely a long-term model for mental health care service delivery during the COVID-19 pandemic and recovery period.10 , 11 In addition, the rapid adoption of telehealth service delivery has the potential to heavily influence the future mental health landscape. Therefore, we present here the experience of 8 diverse academic child and adolescent psychiatry programs that rapidly pivoted from outpatient, in-person, clinic-based services to home-based telehealth. We describe the chronology and rate of conversion to primarily home-based telehealth, as well as facilitators, barriers, and other challenges that programs addressed in rapidly implementing these home-based telehealth services. Our purpose is to describe “lessons learned” and to provide recommendations to support the viability of home-based telehealth going forward.
Method
Definitions
We define telehealth as real-time, interactive services delivered directly to patients through telephone and/or videoconferencing. When either of these modalities is specifically indicated, we use the terms telephony or videoconferencing, respectively. During the COVID-19 pandemic, telehealth has referred primarily to home-based telehealth in which patients are located at home or other non-clinic locations. Providers have predominately been at home as well, although some have provided care from the clinic.
Sample
The Consortium represents a non-random sample of child and adolescent psychiatry programs operating ambulatory child and adolescent psychiatry services at academic medical centers in the United States and Canada. Because of significant variability in models of care, staffing, and reimbursement offered to contracted sites outside of these medical centers, we excluded contracted services, for example, to community mental health centers or stand-alone telehealth programs. Representatives met weekly via videoconferencing to outline issues regarding the rapid transformation of clinic-based outpatient services to home-based telehealth. Programs represented include Children’s Hospital Colorado; MedStar Georgetown University Hospital; Nationwide Children’s Hospital; New York University (NYU) Langone Health; Seattle Children’s Hospital; Hospital for Sick Children (SickKids); Zucker Hillside Hospital; and Zuckerberg San Francisco General Hospital.
Measures and Procedure
Consortium members collaboratively developed a Qualtrics survey to understand implementation of home-based telehealth services specific to their geographic location and programs. One program had 2 distinct sites (NYU Langone Health private and public settings) and completed 2 separate surveys, resulting in 9 total responses. Surveys were completed by the co-authors (eg, faculty psychiatrists and psychologists, nurse practitioner) in collaboration with clinic leadership (eg, Medical Director); respondents regularly receive feedback from clinic staff related to telehealth service delivery through their supervisory and administrative roles. Institutional review boards at 2 participating institutions confirmed that approval was not required, as this does not constitute human subjects research. Topics assessed by the survey are described below.
Site Characteristics
Each site reported descriptive characteristics at the institutional level (public versus private; urban, suburban and/or rural; safety-net hospital; number of full-time equivalent staff and trainees) and patient population level (primary language spoken; racial/ethnic background).
Home-Based Telehealth Practices
Sites reported information regarding platforms used for videoconferencing and electronic medical records (EMR), and policies related to telehealth (eg, provider training and credentialing) pre− and post−COVID-19 onset.
State/Province Regulations
State- and province-level regulations and waivers related to home-based telehealth service delivery pre− and post−COVID-19 onset were reported (eg, allowable service locations, provider credentialing).
Service Use
The number of in-person and telehealth visits (videoconferencing or telephony) by service type (ie, new intakes, follow-up [medication management, individual therapy, or family therapy] and group therapy) were reported between February 16, 2020, and April 15, 2020; parallel data were collected for the same weeks in 2019 as a point of comparison. Two sites (Children’s Hospital Colorado, Medstar Georgetown) did not distinguish between telephony and videoconferencing; 1 site (Nationwide Children’s Hospital) did not provide data for intake and group therapy visits; 2 sites (Medstar Georgetown and NYU Langone Child Study Center) did not provide no-show data for 2019; and 1 site (Zuckerberg San Francisco General Hospital) did not provide use data.
Barriers to Telehealth Service Delivery
Respondents indicated whether 17 factors were perceived to be barriers to home-based telehealth service delivery (yes/no) pre− and post−COVID-19 onset. Barriers included patient (eg, age, diagnosis), technology (eg, cost to purchase and maintain equipment), and systems (eg, potential for liability) factors. Respondents could also write in any additional barriers not assessed.
Analysis Plan
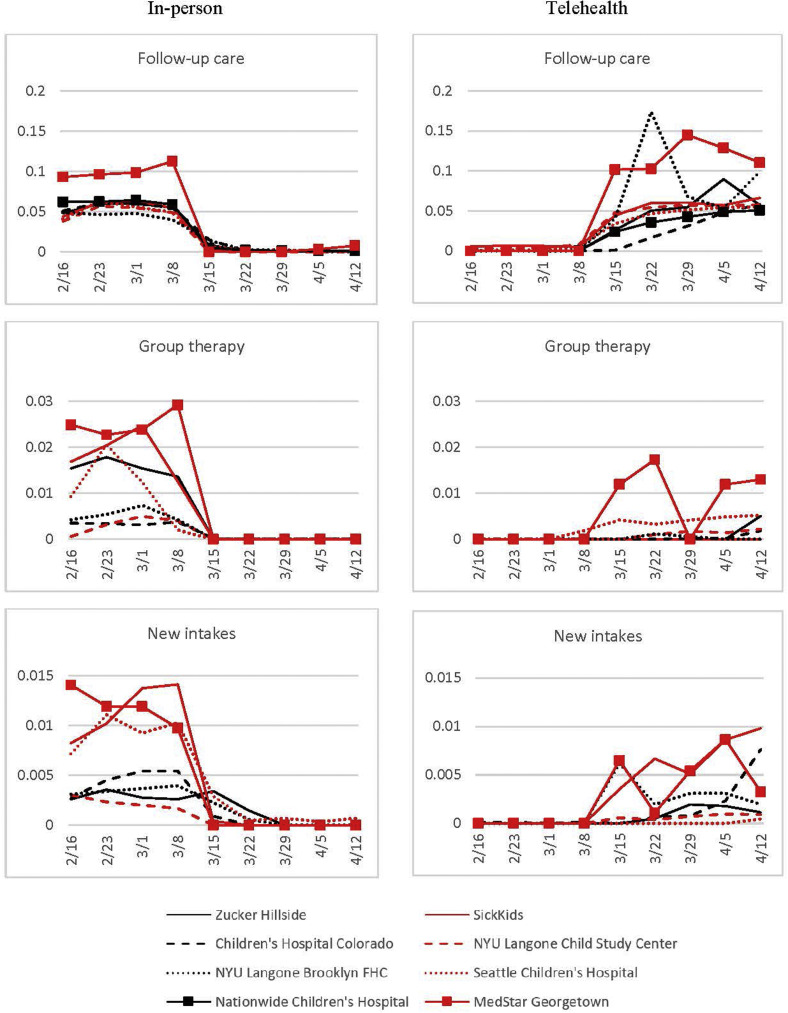
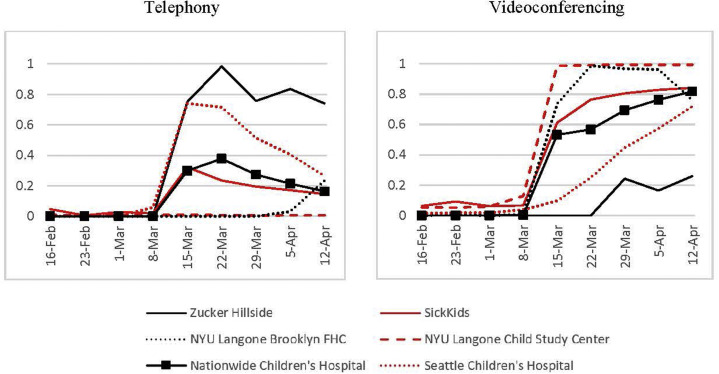
Descriptive statistics are presented to characterize changes in telehealth practices and service use. Responses were weighted equally across all sites. To examine patterns of service use across sites of different sizes, we used a proxy for site size that was calculated by summing the total number of follow-up visits at each site across February 17, 2019 to April 20 2019, and from February 16, 2020 to April 18, 2020, with 2019 data included to minimize the impact of changes in service provision already occurring by the start of data collection in 2020. All data points in Figure 1 were standardized using this proxy. To examine the use of telephony versus videoconferencing for follow-up care in 2020 (February 16, 2020 to April 18, 2020), we calculated the rate of visits using each modality as a proportion of the total follow-up visits that occurred (in-person and telehealth) (Figure 2 ).
Figure 1.
Weekly Mental Health Completed Visits From February 16, 2020, to April 18, 2020
Note:Graphs represent patterns of in-person (left) and telehealth (right) service use across sites. Data on the y-axis represent weekly completed visits (follow-up, group therapy, or new intakes) as a proportion of the total number of follow-up visits at each site from February 17, 2019 to February 20, 2019, and from February 16, 2020 to April 18, 2020 (to standardize for site size). The x-axis represents each week of the 2020 study period.Please note color figures are available online.
Figure 2.
Weekly Follow-up Telephony or Videoconferencing Visits From February 16, 2020, to April 18, 2020, as a Proportion of Total Weekly Follow-up Visits
Note:Data on the y-axis represent the percentage of follow-up visits that week (in-person, telephone, and video-conferencing) that took place by either telephony (left column) or videoconferencing (right column). The x-axis represents each week of the 2020 study period. Please note color figures are available online.
No-show rates were calculated for follow-up mental health care only, and for 3 specific time periods (February 17, 2019 to April 20, 2019; February 16, 2020 to March 14, 2020; and March 15, 2020 to April 18, 2020). This allowed for comparison of no-show rates for a comparable period in 2019, the period prior to widespread closures for COVID-19, and the period after widespread closures for COVID-19. No-show rates were calculated by dividing the number of no-show appointments for a specified time period by the sum of the no-show appointments for that time period and the completed appointments for that time period.
Results
Site Characteristics
Table 1 displays descriptive information for participating sites. Sites were 50% public and 89% hospital-based; 44% identified as a safety-net hospital.12 Most sites served urban and suburban communities, with 3 sites also providing care for rural populations. Sites served a median of 35% Medicaid-insured patients. Patient populations were diverse in race/ethnicity and primary language spoken.
Table 1.
Participating Site Characteristics
| General site information |
Patient population |
Clinical providers |
Telehealth technology |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Name and affiliation | Location | Type | Medicaid % | Race/ethnicity % | Primary language % | Primary community | FTE Staff | Trainees | Platform | EMR | IT support available | Consent method |
| Children’s Hospital Colorado; University of Colorado School of Medicine | Colorado, USA | Private hospital | 29 | 0.6 American Indian, Alaska Native; 1.7 Asian; 4.3 Black, African American; 19.0 Hispanic, Latinx; 66.7 White; 0.1 Native Hawaiian, other Pacific Islander; 7.6 other | 95.8 English; 3.6 Spanish; 0.02 French; 0.6 other | Urban, suburban, rural | 3.7 Clinical psychology; 3.3 psychiatry; 16.1 Master’s level clinician | 5.4 Other | Primary: Vidyo (HIPAA compliant; interpreter services not integrated; EMR integrated) Secondary: Zoom Tried and abandoned: Jabber; Doximity |
Epic | Providers, patients | Verbal, written |
| Medstar Georgetown University Hospital; Georgetown University School of Medicine | District of Columbia, USA | Private hospital | 20 | 5.0 Asian; 30.0 Black, African American; 15.0 Hispanic, Latinx; 50.0 White | 95.0 English; 5.0 Spanish | — | 4.0 Clinical psychology; 4.0 psychiatry; 2.0 Master’s level clinician | 1 Clinical psychology; 2 psychiatry | Primary: Webex; internal system (HIPAA compliant; interpreter services and EMR not integrated) Secondary: Zoom; Doxy.me |
Cerner | Providers, patients | Verbal, written |
| Nationwide Children’s Hospital; The Ohio State University | Ohio, USA | Public hospital; safety- net | 39 | 0.1 American Indian, Alaska Native; 2.3 Asian; 19.1 Black, African American; 5.2 Hispanic, Latinx; 63.7 White; 0.2 Native Hawaiian, other Pacific Islander; 9.4 other | 92.6 English; 3.7 Spanish, 0.2 French; 0.2 Mandarin, Cantonese; 3.3 other | Urban, suburban, rural |
74.5 Clinical psychology; 24.3 psychiatry; 15.9 psychiatric nurse practitioner; 314.0 Master’s level clinician | 15 Clinical psychology; 4 psychiatry; 2 psychiatric nurse practitioner | Primary: Zoom (HIPAA compliant; interpreter services and EMR integrated) | Epic | Providers, patients | Verbal, written |
| NYU Langone Brooklyn Family Health Centers Pediatric Behavioral Health; NYU Langone Health | New York, USA | Public hospital | 49 | 2.1 American Indian, Alaska Native; 2.3 Asian; 9.1 Black, African American; 52.0 White; 7.0 Native Hawaiian, other Pacific Islander; 27.5 other | 54.3 English; 44.9 Spanish; 0.8 Mandarin, Cantonese | Urban | 12.0 Clinical psychology; 10.5 psychiatry; 33.0 Master’s level clinician; 3.0 other | 4 Clinical psychology | Primary: Webex (HIPAA compliant; interpreter Services and EMR not integrated) Secondary: Jabber |
Epic | Providers, patients | Verbal, written (before COVID-19) |
| NYU Langone Health Child Study Center, Department of Child and Adolescent Psychiatry | New York, USA | Private hospital | — | — | 99.0 English | Urban | 44.0 Clinical psychology; 13.0 psychiatry; 1.0 psychiatric nurse practitioner; 3.0 Master’s level clinician | 19 Clinical psychology; 5 psychiatry; 0.5 psychiatry nurse practitioner; 0.5 Master’s level clinician | Primary: MyChart (HIPAA compliant; interpreter services not integrated; EMR integrated) Secondary: Webex |
Epic | Providers, patients | Verbal |
| Seattle Children’s Hospital; University of Washington School of Medicine | Washington, USA | Private hospital; safety- net | 35 | 0.7 American Indian, Alaska Native; 7.5 Asian; 6.1 Black, African American; 13.8 Hispanic, Latinx; 55.5 White; 0.4 Native Hawaiian, other Pacific Islander; 4.1 other | 92.0 English; 4.3 Spanish; 0 French; 0.3 Mandarin, Cantonese; 3.4 other | Urban, suburban, rural |
24.2 Clinical psychology; 3.2 psychiatry; 1.9 psychiatric nurse practitioner; 5.6 Master’s level clinician; 5.6 other | 0.2 Clinical psychology; 1.1 psychiatry | Primary: Zoom (HIPAA compliant; interpreter services integrated; EMR not integrated) Secondary: Webex Tried and abandoned: InTouch |
Cerner | Providers, patients | Verbal, written |
| SickKids; University of Toronto | Ontario, Canada | Public hospital | N/A | — | — | Urban, suburban | 1.2 Clinical psychology; 7.7 psychiatry; 1.psychiatric nurse practitioner; 4.4 Master’s level clinician; 3.8 other | 2 Psychiatry | Primary: Zoom (HIPAA compliant; interpreter Services and EMR not integrated) Secondary: OTN |
Epic | Providers, patients | Verbal, other (e-mail with policies) |
| Zucker Hillside Hospital, Child and Adolescent Outpatient Psychiatry Department, Northwell Health; Zucker School of Medicine at Hofstra/Northwell Health | New York, USA | Private hospital; safety- net | 30 | 1 American Indian, Alaska Native; 1 Asian; 19 Black, African American; 8 Hispanic, Latinx; 55 White; 1 Native Hawaiian, other Pacific Islander; 17 other |
96 English; 1 Spanish; 1 French; 1 Mandarin, Cantonese; 1 other | Urban, suburban | 1.3 Clinical psychology; 1.75 psychiatry; 0.7 psychiatric nurse practitioner; 4.4 Master’s level clinician; 1.0 other | 2 Clinical psychology; 6 psychiatry | Primary: Zoom (HIPAA compliant; interpreter Services and EMR not integrated) Secondary: Doximity; AmWell |
Net Smart/My Avatar | Providers | Verbal |
| Zuckerberg San Francisco General Hospital; University of California, San Francisco | California, USA | Public hospital; safety- net | 100 | 0.3 American Indian, Alaska Native; 4.6 Asian; 20.8 Black, African American; 53.4 Hispanic, Latinx; 10.4 White; 0.3 Native Hawaiian, other Pacific Islander; 10.2 other |
61.7 English; 32.4 Spanish; 0.3 Mandarin, Cantonese; 5.6 other | Urban | — | — | Primary: Zoom (HIPAA compliant; interpreter services integrated; EMR not integrated) | My Avatar | Providers, patients | Verbal, written |
Note: EMR = Electronic Medical Record; N/A = not applicable.
Home-Based Telehealth Practices
Zoom was the most commonly used videoconferencing platform (56%) and Epic the most common EMR (56%). All sites reported that their primary videoconferencing platforms were HIPAA-compliant; some were integrated with interpreter services (33%) and/or EMR (33%). One site (Zucker Hillside Hospital) provided technological support to providers only; all other sites provided technological support to both providers and patients. Two-thirds obtained both verbal and written consent for any telehealth services. Additional descriptives are presented in Table 1.
Site-specific home-based telehealth practices are shown in Table 2 . Prior to COVID-19, 78% of sites provided some videoconferencing services; 71% of these sites required providers to be in-clinic to provide videoconferencing services, and 57% required patients to be in a designated clinical location to receive services. For some sites, videoconferencing was provided in a very limited capacity pre−COVID-19. For example, Children’s Hospital Colorado had about 0.1 full-time equivalent per week for any telehealth service; SickKids limited videoconferencing to children who were aggressive in the context of neurodevelopmental disorders. Zuckerberg San Francisco General Hospital, a public safety-net hospital, had no telehealth program, as it was not covered by Medicaid. By contrast, Seattle Children’s Hospital had a robust videoconferencing program to community mental health centers and to the homes of children with autism, but offered these home-based telehealth services to only a small number of other families, depending on the specific provider’s practice.
Table 2.
Site-Specific Telehealth Practices Before and After COVID-19 Pandemic Onset
| Colorado | Medstar | Nationwide | NYU FHC | NYU CSC | Seattle | SickKids | Zucker Hillside | ZSFGH | |
|---|---|---|---|---|---|---|---|---|---|
| Provide Telehealth Services | |||||||||
| Before | X | X | X | X | X | X | X | ||
| After | X | X | X | X | X | X | X | X | X |
| Require providers to be on-site to provide videoconferencing services | |||||||||
| Before | X | X | X | X | X | n/a | n/a | ||
| After | |||||||||
| Allow providers to provide videoconferencing services from home | |||||||||
| Before | X | X | X | n/a | n/a | ||||
| After | X | X | X | X | X | X | X | X | X |
| Require patients to be in a designated clinical location to receive videoconferencing services | |||||||||
| Before | X | X | n/a | n/a | |||||
| After | |||||||||
| Allow patients to participate in videoconferencing services from home | |||||||||
| Before | X | X | X | n/a | n/a | ||||
| After | X | X | X | X | X | X | X | X | X |
| Provider training requirements | |||||||||
| Before | X | X | X | X | X | n/a | n/a | ||
| After | X | X | X | X | X | X | X | ||
| Provider credentialing requirements | |||||||||
| Before | X | X | X | X | n/a | n/a | |||
| After | X | X | X | ||||||
| Formalized safety protocols | |||||||||
| Before | X | X | X | n/a | n/a | ||||
| After | X | X | X | X | X | X | X | X | |
| Allow billing | |||||||||
| Before | X | X | X | X | X | X | n/a | n/a | |
| After | X | X | X | X | X | X | X | X | X |
| Documentation requirements | |||||||||
| Before | X | X | X | X | X | n/a | n/a | ||
| After | X | X | X | X | X | X | X | X | X |
| Train support staff to facilitate service delivery | |||||||||
| Before | X | X | X | n/a | n/a | ||||
| After | X | X | X | X | X | X | X | X | |
| Train patients to use technology | |||||||||
| Before | X | X | X | n/a | n/a | ||||
| After | X | X | X | X | X | X | |||
Note: X = Yes; Bellevue = Bellevue Hospital; Colorado = Children’s Hospital Colorado; Medstar = Medstar Georgetown University Hospital; Nationwide = Nationwide Children’s Hospital; NYU CSC = NYU Langone Health Child Study Center; NYU FHC = NYU Langone Brooklyn Family Health Centers; Seattle = Seattle Children’s Hospital; Zucker Hillside = Zucker Hillside Hospital; ZSFGH = Zuckerberg San Francisco General Hospital.
During the onset of the pandemic, software licensing was a barrier to videoconferencing ramp-up for 33% of sites. Limited software licenses initially caused some sites to schedule around lower-volume times of the day, to triage patients based on acuity, to determine which providers (trainees, faculty, non-faculty) would be able to start virtual care first, and to use telephony.13
After the onset of COVID-19, all 9 sites provided videoconferencing services, allowing providers and patients to participate from home. Changes in telehealth practices were seen pre−/post−COVID-19, respectively, across sites, in instituting provider training requirements for delivering telehealth (56%, 78%), creation/existence of formalized telehealth safety protocols (33%, 89%), allowable telehealth billing (67%, 100%), implementing telehealth-specific documentation requirements (56%, 100%), training support staff to facilitate telehealth services (33%, 89%), training patients to use technology (33%, 56%), and telehealth-specific provider credentialing requirements (44%, 33%).
State/Province Regulations
The sites were from 6 states and 1 province with differing regulations (Table S1, available online). Prior to COVID-19, 57% of the states/provinces required providers to be on-site to provide videoconferencing services, and 43% required patients to be in a designated clinical location to receive videoconferencing services; post−COVID-19, these regulations were removed, and all jurisdictions allowed both patients and providers to participate from home. State/province level requirements for provider training (New York State Office of Mental Health−regulated sites) and credentialing (District of Columbia and Ohio) were uncommon pre−COVID-19 and were lifted post−COVID-19. Except California, all states/provinces allowed billing of videoconferencing services to public insurance prior to COVID-19; post−COVID-19, California began allowing billing of videoconferencing services to public insurance. Documentation requirements shifted (71% pre− and 86% post−COVID-19), with Ontario establishing requirements post−COVID-19.
Service Use
All 8 sites with use data reduced in-person visits close to zero by March 22, 2020 (Figure 1), which corresponds with local shelter-in-place orders (Table S2, available online). The most drastic decreases in in-person visits occurred the week of March 15 to 21, 2020. At all sites, telehealth visits were rare between February 16, 2020, and March 14, 2020. Beginning the week of March 15, 2020, telehealth visit numbers began increasing, with some sites switching to telehealth more quickly than others (eg, Medstar Georgetown).
The speed at which sites switched to telehealth service delivery varied by visit type. Sites generally transitioned follow-up care (individual or family therapy; medication management) to telehealth more quickly than group therapy or new intakes. By the week of April 12, 2020, all sites were conducting a comparable number of telehealth visits per week, as they had been conducting in-person visits prior to March 15, 2020. For group therapy, no sites reached a number of telehealth visits by the week of April 12, 2020, that was comparable to in-person visits prior to March 15, 2020. Approximately half of the sites conducted a number of new intakes via telehealth the week of April 12, 2020, that was comparable to the number of intakes in-person before March 15, 2020.
Six sites provided data on the use of telephony versus videoconferencing (Figure 2). Some sites (eg, Zucker Hillside Hospital, Seattle Children’s Hospital) relied primarily on telephony in the first weeks following the onset of COVID-19, and gradually transitioned to partial use of videoconferencing by the end of the study period. Others (eg, SickKids, NYU Langone Child Study Center) used videoconferencing at low rates pre−COVID-19, and transitioned to videoconferencing for more than 80% of visits by the end of March 2020. By the end of the study, all sites were using videoconferencing for at least some follow-up care, and 5 of the 6 sites were using videoconferencing for more than 70% of visits.
Only 6 sites provided no-show data for both 2019 and 2020 (Table S3, available online). Two of these 6 sites (Children’s Hospital Colorado, Seattle Children’s Hospital) had similar no-show rates across all 3 time periods. Two of the 6 sites (Zucker Hillside Hospital, Nationwide Children’s Hospital) had higher no-show rates after March 15, 2020, than in 2019 or prior to the COVID-19 closures. An additional 2 sites (SickKids, NYU Langone Brooklyn FHC) had lower no-show rates after March 15, 2020, than in 2019 or prior to the COVID-19 closures.
Barriers to Telehealth Service Delivery
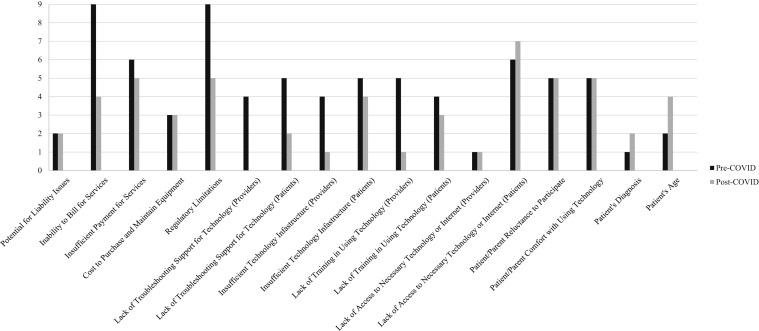
Perceived barriers to telehealth service delivery pre−/post−COVID-19 are presented in Figure 3 . Prior to COVID-19, the most common barriers to telehealth service delivery, reported by all sites, were inability to bill for service and regulatory limitations; post−COVID-19, these were barriers for 44% and 56% of sites, respectively. Post−COVID-19, the most common barrier was patient lack of access to necessary technology and/or the Internet (or reliable Internet). Although certain barriers were noted less commonly post− versus pre−COVID-19 (ie, inability to bill, inadequate reimbursement, regulatory limitations, lack of troubleshooting support for providers and patients, insufficient technology infrastructure for patients and providers, lack of training in using technology for patients and providers), many perceived barriers to telehealth implementation remained the same (potential for liability, cost to purchase and maintain equipment, patient/parent reluctance to participate, patient/parent comfort with technology) and some were more frequently noted (patient lack of training in using technology, diagnosis, and age). Additional barriers to telehealth service delivery noted by sites included the following: limited ability to e-prescribe controlled substances for some sites; limited ability to prescribe controlled substances for patients seen via telehealth for some sites because of federal and/or state regulations; language barriers for non-native English speakers; cultural barriers affecting trust in or comfort with technology; and concerns about privacy.
Figure 3.
Barriers to Telehealth Service Delivery
Note:Perceived patient-, technology-, and systems-level barriers to home-based telehealth service delivery.
Discussion
To our knowledge, this is the first description of the experience of a consortium of academic child and adolescent psychiatry outpatient programs in rapidly pivoting from traditional in-person services to home-based telehealth services during the COVID-19 pandemic, or any other crisis. Our aims were to describe telehealth service delivery before and during the early stages of the COVID-19 pandemic with respect to telehealth practices, service use, and barriers to telehealth service delivery. Based on the data and experiences of the consortium, we provide recommendations to inform and support future development and evaluation of telehealth services.
COVID-19 was a “disrupter” of child and adolescent psychiatric practice. Programs rapidly pivoted to home-based telehealth practice to continue providing care for their patients, while following site and state/province recommendations to shelter at home at the start of the pandemic. This rapid transition created new stressors for providers and families,14 including coping with stressors related to sheltering at home, managing home schooling, and, for some individuals, sharing devices and Internet bandwidth. Each program paved its own way to delivering home-based telehealth services in the context of local regulatory requirements, reimbursement environment, hospital resources, patient clinical needs, and patient and provider receptivity. As evidenced by our use data, all programs transitioned to providing home-based telehealth services, noting a decrease in some barriers (eg, billing, reimbursement, technology support) and persistence of others (eg, liability, cost of equipment, comfort with technology, cultural concerns).
Each program’s experience transitioning from in-person to telehealth service delivery varied in part because of differences in site and state/province telehealth practices pre−COVID-19. In order for some programs to offer home-based telehealth services, regulations had to change first. Most of the participating sites provided some telehealth services prior to the pandemic, but there were differences related to the amount offered, allowable locations for providers and patients, number of providers experienced with the modality, and the established infrastructure to support telehealth services. These differences likely contributed to how easily sites transitioned to home-based telehealth.
After the COVID-19 pandemic began, all sites moved to offering predominately home-based telehealth, rather than in-person, services. The majority of sites were able to bill, had specific documentation requirements, and trained their staff with regard to telehealth services and safety protocols. Not only did programs have to modify their existing practices, but many individual providers experienced abrupt changes, as many were naive to telehealth and had to learn a new skill set not only for use of the technology but also for tasks such as billing (ie, per Current Procedural Terminology [CPT]),15 documentation, safety, and secure service delivery. Regarding safety, consortium sites anecdotally noted that their providers encountered new clinical challenges in transitioning to home-based telehealth practice because of lack of familiarity with the privacy and safety of the home and the resources in the community.16 , 17 Each program developed its own approach, ranging from screening for suicidality with a rating scale, to sending explanatory letters to families regarding the technology and clinical processes, to a protocol assessing the availability of a private space as well as safety risks with documentation of community resources in case of potential harm. Going forward, safety protocols are needed to ensure a standard of care comparable to that of clinic-based telehealth, as well as to traditional in-person care.18 Programs would benefit from retaining and consistently updating telehealth practices and provider training, as this will allow for more nimble shifts between in-person and telehealth services as needed. Ongoing training of providers to master technology-mediated clinical service and to implement safety protocols should increase competence and reduce provider stress in delivering telehealth services. Safety protocols will help providers to be prepared for possible adverse events such as suicidality, aggression, or family emergencies,16 , 17 as well as “zoombombing” (ie, intrusion of uninvited individuals into sessions). In the future, telehealth experiences should ideally start during training (eg, residency and fellowship) so that new providers are ready to integrate telehealth into their practices, not only for crisis services but for routine care that diversifies their practice options and promotes access for families.
Despite the programs’ differences, all pivoted their follow-up services from in-person to home-based telehealth on the same timeline. Service use was likely underreported by sites who were not able to fully capture the amount of telephony provided because of limitations with billing codes and EMR encounter tracking. While accommodating for program-specific telehealth ramp-up considerations (eg, credentialing, training, software licensing, technology support, prescription regulations), the current study shows that sites generally prioritized transitioning established patients’ care first and had to delay enrolling new patients; about half of the sites achieved pre-pandemic intake levels within a month. No-show rates for telehealth in 2020 varied across sites but were not dramatically different from 2019 rates for traditional in-person care; this was of interest because colloquially it was perceived that telehealth no-show rates were lower.
Use data also revealed that all programs experienced a lag in establishing tele-group interventions. Establishing tele-group services requires considerable extra administrative coordination. For example, although videoconferencing platforms integrated with the EMR facilitate access to individual appointments, additional steps outside of the EMR may be required to access group appointments. Time is also required to adapt clinical interventions to the virtual modality, and some group interventions may be more adaptable to telehealth than others (eg, parent-training programs versus children’s group anxiety programs).19 No site reached pre-pandemic rates of group therapy within the study window.
Based on the Consortium’s experience and use data, we recommend that programs planning to use telehealth in the future develop sustainable data collection systems for tracking telehealth service use. Programs should build visit types in the EMR that distinguish in-clinic versus home-based videoconferencing and telephony services, as well as telephony services from nonbillable telephone encounters. These data are critical to health equity and understanding differences in the populations served (or not served) by the various types of telehealth or in-person services. In addition, we recommend developing processes to track clinical outcomes to monitor the quality and effectiveness of care provided through telehealth, to determine whether care delivered via telehealth is comparable to in-person care. This information can also clarify which patients (eg, age groups, diagnoses) and therapeutic interventions are most appropriate for telehealth service delivery. Tracking clinical outcomes is directly linked to ensuring financial sustainability. The Congressional Budget Office has often assigned telehealth legislation low scores, noting that this is due to insufficient quantitative outcomes documenting the effectiveness of telehealth interventions. An evidence base is needed to help make the case for the quality and cost-effectiveness of telehealth.
During this time of rapid transition to telehealth, participating programs noted that some barriers to care decreased whereas others persisted or became even more apparent (Figure 3). Although troubleshooting and infrastructure support for providers improved during the initial stages of the pandemic, respondents noted ongoing barriers related to patient access, comfort, and support for the use of technology. If home-based telehealth is to be accessible and equitable for patients, continued work is needed to reduce the “digital chasm” by considering how to provide families with devices and Internet resources. An Executive Order was issued on August 3, 2020, requiring the Secretary of Health and Human Services and the Secretary of Agriculture to develop and implement, within 30 days, “a strategy to improve rural health by improving the physical and communications health care infrastructure available to rural Americans.”20 This will hopefully improve connectivity, although as telehealth expands, more bandwidth is needed across the nation, not just in rural communities. The “digital chasm” is an increasingly important social determinant of health. As programs are likely to offer hybrid services (eg, part in-person and part home-based telehealth) in the future, academic child and adolescent psychiatry programs should advocate for strategies to ensure universal connectivity and devices that reach underserved populations.
Telephony was crucial to our programs’ ability to sustain care and outreach to families at the start of the pivot from in-person to home-based telehealth services until videoconferencing was available, and to continuing care for families who never had videoconferencing access. The value of telephony is emphasized by another crisis, namely, Hurricane Maria in Puerto Rico. Satellite telephone and cellular lines were reinstated much more quickly than videoconferencing capacity.21 The CMS’s relaxation of policies during the COVID-19 pandemic to allow billing for psychotherapy and Evaluation and Management codes for services conducted through telephony6 helped programs to continue providing services to families while recouping some revenue. Telephony continues to be the primary telehealth approach for patients with limited technology or Internet access (eg, unhoused individuals), low technological literacy, and other barriers faced by disenfranchised communities. Given that community health centers and public hospitals serve a disproportionate share of low-income, racial and ethnic minoritized, and immigrant populations—those hardest hit by the COVID-19 pandemic—disruptions to mental health care services have risked exacerbating these inequities.22 , 23
In addition to ensuring families have access to technology, the ongoing development of infrastructure and systems to guide patients and families in technology-facilitated protocols is necessary to optimize experience and satisfaction with telehealth services. Different approaches to training are possible. Informational sheets with written instructions or how-to-videos in the patient’s preferred language can efficiently convey information. A follow-up telephone call or test run of the video connection by support staff can be helpful for families struggling with technology. Providers should also be given tips to support patients “on the fly.”
Prior to the pandemic, all sites reported that inability to bill for services and regulatory limitations were barriers to telehealth service delivery. The COVID-19 pandemic prompted temporary regulatory and billing changes, allowing sites to provide telehealth in the context of the ongoing crisis. If telehealth is to be a feasible and sustainable service model, it will be crucial to establish a business model for financial stability for sufficient revenue to pay providers, to maintain technologies (eg, videoconferencing platforms, electronic prescribing software), and to support clinic operations; this requires alignment across states and among Medicare, Medicaid, and private insurers (ie, parity across all payers). Regulations that were modified during the pandemic to decrease barriers to telehealth care, such as the changes related to prescribing of controlled substances (eg, stimulants), will need to be reviewed once the public health crisis is over. In Canada, sustainability will depend on individual provincial health plans continuing to fund telehealth services via multiple videoconferencing platforms. Advocacy should continue to emphasize the value that telehealth brings to patients and families so that it can be used not only during crises.
This study had several limitations. The Consortium was a nonrandom sample of child and adolescent psychiatry programs at academic medical centers in the United States and Canada serving predominantly urban and suburban communities. As such, the experiences of our sites may not be representative of the experiences of all sites, particularly those serving rural communities. Another limitation was related to the inability to gather data prospectively during a crisis. All data were obtained retrospectively using data extracted from EMR visit types and billing codes, which are subject to error. Not all visit types were comparably recorded across EMRs, and some sites did not have distinct codes to differentiate videoconferencing and telephony encounter types. Data were collected in aggregate form and not from individual patient charts, preventing disaggregation of the use data by patient demographic characteristics (eg, race/ethnicity). Future studies could also include qualitative patient impressions (eg, patient-level barriers to telehealth services) or clinical patient outcomes, as such information would add to understanding the value-added benefit of home-based telehealth to the mental health care landscape for children and adolescents.
The pandemic has transformed our mental health care delivery system. The Consortium’s experiences highlight the considerable variation and rapid transformation of telehealth practices among sites in the context of changing laws and regulations. We recommend ongoing efforts to document the successes and barriers to telehealth practice to promote equitable and sustainable telehealth service delivery in the future.
Acknowledgments
The authors wish to acknowledge Douglas K. Novins, MD, at the University of Colorado Anschutz Medical Campus, for introducing consortium members, serving as a scientific advisor, and assistance with data collection. The authors would like to thank Matthew Biel, MD, MSc, at Georgetown University, for data collection and manuscript editing; James Murphy, MD, MBA, at the University of Colorado School of Medicine, for manuscript editing; and Marina Tolou-Shams, PhD, at the University of California, San Francisco, for data collection and scientific collaboration. The authors would like to thank the following individuals for their contribution to data collection: Marie Augustine, MS and Kathy Brewer, MS, at Seattle Children’s Hospital; David A. Axelson, MD, with Nationwide Children’s Hospital and The Ohio State University; Terrilyn Chow and Hiba Michael, BA, at The Hospital for Sick Children; Reena Carmen, LCSW, at Northwell Health; Claudine Higdon, MD, at Northwell Health and Zucker School of Medicine; Glenn Hirsch, MD and William Moitoza, MEd, at NYU Langone Health; Aaron Reliford, MD, at NYU Langone Health and Family Health Centers at NYU Langone; Barbara Krishna Stuart, PhD, at the University of California, San Francisco; and Giuseppa M. King, MBA, at Children’s Hospital Colorado.
Footnotes
Drs. Folk and Schiel are co-first authors of this article. Drs. Fortuna, Fornari, and Myers are co-senior authors of this article.
The authors have reported no funding for this work.
This study was presented as an abstract at the American Academy of Child and Adolescent Psychiatry 67th Annual Meeting; October 12−24, 2020; virtual.
Dr. Oblath served as the statistical expert for this research.
Author Contributions
Conceptualization: Folk, Schiel, Feuer, Sharma, Khan, Doan, Kulkarni, Ramtekkar, Hawks, Fornari, Fortuna, Myers
Data curation: Folk, Oblath, Feuer
Formal analysis: Oblath
Project administration: Schiel
Visualization: Folk, Schiel, Oblath
Writing – original draft: Folk, Schiel, Oblath, Feuer, Sharma, Khan, Doan, Kulkarni, Ramtekkar, Hawks, Fornari, Fortuna, Myers
Writing – review and editing: Folk, Schiel, Oblath, Feuer, Sharma, Khan, Doan, Kulkarni, Ramtekkar, Hawks, Fornari, Fortuna, Myers
Disclosure: Dr. Folk has received salary support from the National Institute of Mental Health (T32MH018261) and the National Institute on Drug Abuse (K23DA050798). Dr. Schiel has served on the Behavioral Health Steering Board for Epic. Drs. Feuer, Fornari, and Fortuna have received salary support from the Patient-Centered Outcomes Research Institute (PCORI). Drs. Oblath, Sharma, Khan, Kulkarni, Ramtekkar, Hawks, Myers and Ms. Doan have reported no biomedical financial interests or potential conflicts of interest.
Supplemental Material
Table S1.
State/Province Specific Telehealth Practices Before and After COVID-19 Pandemic Onset
| California | Colorado | District of Columbia | New York State | Ohio | Ontario | Washington | |
|---|---|---|---|---|---|---|---|
| Require providers to be on-site to provide services | |||||||
| Before | X | X | Xa | X | |||
| After | |||||||
| Require patients to be in a designated clinical location to receive services | |||||||
| Before | X | Xa | X | ||||
| After | |||||||
| Allow providers/patients to serve/participate at home | |||||||
| Before | X | X | X | X | |||
| After | X | X | X | X | X | X | X |
| Provider training requirements | |||||||
| Before | Xa | ||||||
| After | |||||||
| Provider credentialing requirements | |||||||
| Before | X | X | |||||
| After | |||||||
| Allow billing public insurance | |||||||
| Before | X | X | X | X | X | X | |
| After | X | X | X | X | X | Xb | X |
| Documentation requirements | |||||||
| Before | X | X | X | X | X | ||
| After | X | X | X | X | X | X | |
Note: aSpecific to New York State Office of Mental Health (OMH) regulated sites.
Expanded billing to including telephone care; California responses refer to MediCAL regulations.
Table S2.
Emergence of COVID-19 Among Consortium Sites
| Location | Date of first COVID-19 case in state/province | State and provincial “stay-at-home” orders |
|---|---|---|
| Seattle, WA | January 21, 2020 | March 23, 2020 |
| Toronto, ON, Canada | January 25, 2020 | March 17, 2020 |
| San Francisco, CA | January 26, 2020 | March 19, 2020 |
| New York, NY | March 1, 2020 | March 22, 2020 |
| Washington DC | March 5, 2020 | March 16, 2020 |
| Denver, CO | March 5, 2020 | March 26, 2020 |
| Columbus, OH | March 9, 2020 | March 23, 2020 |
Table S3.
No-Shows for Follow-up Mental Healthcare as a Proportion of Scheduled Follow-up Mental Health Visits by Site
| February 17, 2019, to April 20, 2019 | February 16, 2020, to March 14, 2020 | March 15, 2020, to April 18, 2020 | |
|---|---|---|---|
| Children’s Hospital Colorado | 0.05 | 0.04 | 0.05 |
| Nationwide Children's Hospital | 0.10 | 0.08 | 0.13 |
| MedStar Georgetown | N/A | 0.10 | 0.08 |
| NYU Langone Brooklyn Family Health Centers | 0.24 | 0.23 | 0.14 |
| NYU Langone Child Study Center | N/A | 0.06 | 0.05 |
| Seattle Children's Hospital | 0.20 | 0.26 | 0.22 |
| SickKids | 0.06 | 0.05 | 0.03 |
| Zucker Hillside | 0.03 | 0.04 | 0.07 |
Note: N/A = not available.
References
- 1.World Health Organization Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). January 30, 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov Accessed March 12, 2020.
- 2.United States Department of Health and Human Services Health Insurance Portability and Accountability Act of 1996. August 21, 1996. https://aspe.hhs.gov/report/health-insurance-portability-and-accountability-act-1996 Accessed March 29, 2020.
- 3.United States Department of Health and Human Services Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Updated March 30, 2020. Accessed September 27, 2020.
- 4.Drug Enforcement Administration Diversion Control Division How to prescribe controlled substances to patients during the COVID-19 public health emergency. https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-023)(DEA075)Decision_Tree_(Final)_33120_2007.pdf Accessed September 27, 2020.
- 5.Federation of State Medical Boards. U.S. states and territories modifying licensure requirements for physicians in response to COVID-19. https://www.fsmb.org/siteassets/advocacy/pdf/state-emergency-declarations-licensures-requirementscovid-19.pdf Updated September 22, 2020. Accessed September 27, 2020.
- 6.Centers for Medicare and Medicaid Services COVID-19 emergency declaration blanket waivers for health care providers. August 20, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf Accessed September 27, 2020.
- 7.Royal College of Physicians and Surgeons of Canada Telemedicine and virtual care guidelines (and other clinical resources for COVID-19). Updated July 6, 2020. http://www.royalcollege.ca/rcsite/documents/about/covid-19-resources-telemedicine-virtual-care-e#ab Accessed September 27, 2020.
- 8.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. August 20, 2020 [ePub]. https://doi.apa.org/fulltext/2020-61592-001.html [DOI] [PubMed]
- 9.DeJong SM, Alicata D, Brooks D, et al. Pediatric Telepsychiatry curriculum for graduate and continuing medical education. May 2020. Available online at aadprt.org/VTO/Model Curricula and at https://www.aacap.org/App_Themes/AACAP/Docs/clinical_practice_center/business_of_practice/Telepsych/Pediatric_Telepsychiatry_Curriculum_Oct_2020-web.pdf [DOI] [PubMed]
- 10.Craven J. Some telepsychiatry ‘here to stay’ post-COVID. Medscape Psychiatry. July 22, 2020. https://www.medscape.com/viewarticle/934416 Accessed September 7, 2020.
- 11.Robeznieks A. How to maintain momentum on telehealth after COVID-19 crisis ends. June 30, 2020. https://www.ama-assn.org/practice-management/digital/how-maintain-momentum-telehealth-after-covid-19-crisis-ends Accessed September 7, 2020.
- 12.Institute of Medicine . National Academies Press; Washington, DC: 2000. America’s Health Care Safety Net: Intact but Endangered. [PubMed] [Google Scholar]
- 13.Sharma A., Sasser T., Schoenfelder Gonzalez E., Vander Stoep A., Myers K. Implementation of home-based telemental health in a large child psychiatry department during the COVID-19 Crisis. J Child Adolesc Psychopharmacol. 2020;30:404–413. doi: 10.1089/cap.2020.0062. [DOI] [PubMed] [Google Scholar]
- 14.Doan B.T., Yang Y.B., Romanchych E., et al. From pandemic to progression: an educational framework for the implementation of virtual mental health care for children and youth as a response to COVID-19. J Contemp Psychother. 2020 doi: 10.1007/s10879-020-09478-0. October 23:1-7 Open Access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Medical Association CPT (Current Procedural Terminology) https://www.ama-assn.org/amaone/cpt-current-procedural-terminology Accessed August 22, 2020.
- 16.Schoenfelder Gonzalez E, Myers K, Thompson EE, King DA, Glass AM, Penfold RB. Developing home-based telemental health services for youth: practices from the SUAY Study. J Telemed Telecare. July 2019 [ePub]. Accessed April 18, 2020. 10.1177/1357633X19863208 [DOI] [PubMed]
- 17.Luxton D.D., O’Brien K., McCann R.A., Mishkind M.C. Home-based telemental health care safety planning: what you need to know. Telemed J E Health. 2012;18:629–633. doi: 10.1089/tmj.2012.0004. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Child and Adolescent Psychiatry Committee on Telepsychiatry and the Committee on Quality Issues Clinical Update for Telepsychiatry with Children and Adolescents. J Am Acad Child Adolesc Psychiatry. 2017;56:875–878. doi: 10.1016/j.jaac.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Sasser T, Rutter T, Gurtovenko K, et al. Rapid adaptation and acceptability of telegroup delivery of evidence-based treatments for youth during COVID-19. Poster presented at the American Academy of Child and Adolescent Psychiatry Annual Meeting (Virtual), October 12−24, 2020.
- 20.Trump D.J. Executive order on improving rural health and telehealth access. August 3, 2020. https://trumpwhitehouse.archives.gov/presidential-actions/executive-order-improving-rural-health-telehealth-access/ Accessed April 23, 2021.
- 21.de Arzola O.R. Emergency preparedness and Hurricane Maria: the experience of a regional academic medical center in southwest Puerto Rico. J Grad Med Educ. 2018;10:477–480. doi: 10.4300/jgme-d-18-00547.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vahidy F.S., Nicolas J.C., Meeks J.R., et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-039849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fortuna L.R., Tolou-Shams M., Robles-Ramamurthy B., Porche M.V. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: the need for a trauma-informed social justice response. Psychol Trauma. 2020;12:443–445. doi: 10.1037/tra0000889. [DOI] [PMC free article] [PubMed] [Google Scholar]