“For he who has health has hope; and he who has hope, has everything.”
—Owen Arthur (1)
The COVID-19 pandemic has underscored many existing realities of our health care system, including how much health matters, how health and the economy are inextricably linked, and the importance of achieving health equity to realize good health for everyone.
It has been estimated before the COVID-19 pandemic that premature deaths and lost productivity associated with poor health costs the United States about $3.2 trillion (16% of GDP) annually (2). Adding to that, the Institute of Healthcare Improvement estimates that health inequities cost the United States roughly $83 billion—a figure that is anticipated to grow to $300 billion by the year 2050 (3). The COVID-19 pandemic has only served to highlight these trends, with estimates suggesting a reduction in U.S. real GDP between 4% and 11% caused by COVID-related health costs (2).
Previous conversations on how best to address these impacts have focused on controlling health care costs vs promoting health. However, a report from the McKinsey Global Institute suggests that prioritizing health care using existing approaches can present an economic opportunity of about $12 trillion by 2040 (2). Given this, maybe it is time for us to rethink health as an investment rather than just a cost and focus on how to truly optimize health care and health systems. Who can argue against the promise of improved health while accelerating economic growth?
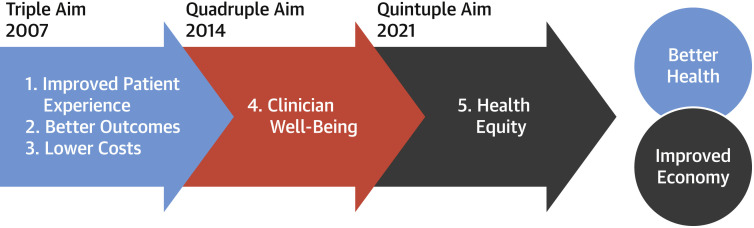
In 2007, the Institute of Healthcare Improvement introduced the Triple Aim, a concept of improved patient experience, better outcomes, and lower costs as key to health care transformation (4). A few years later, the concept evolved to become known as “the Quadruple Aim” to include clinician well-being. Research showing decreased clinician engagement and burnout directly correlated to lower patient satisfaction, reduced health outcomes, and higher costs led to the realization that achieving the initial 3 aims needed to start with the clinician (5).
Today, the concept is quickly evolving to become the “Quintuple Aim,” which incorporates health equity as another key element necessary to truly achieving improved patient care, outcomes, and costs (6). Without understanding the social determinants of health, which drive 70% of health care outcomes, and without a clear path forward to solve for health equity, all attempts to globally transform cardiovascular care will be futile (Figure 1 ).
Figure 1.
Evolution to the Quintuple Aim
Achieving this Quintuple Aim is a worthy goal that ties directly to the American College of Cardiology’s (ACC’s) mission to transform cardiovascular care and improve heart health. The College and its more than 54,000 members around the world have an opportunity to drive real solutions and lead in this area—both in the United States and globally.
For example, the ACC has an opportunity to lead on health equity by using our NCDR registry data and other data sources to try to understand the drivers of cardiovascular health. We must also find a way to use sociodemographic and clinical data at the individual and the community level to better understand the distinct needs of the populations we serve. Additionally, we can play an important role in helping combat implicit bias among clinicians with the goal of improving communication and engagement with patients and ultimately transforming the patient experience and health outcomes.
Another area of focus correlates with the intersection of cardiovascular disease with other disease states, like cancer, diabetes, renal disease, and even obstetrics. The cardiovascular profession’s natural tendency to innovate and our early work to collaborate across specialties with surgeons places us in a unique position to both convene stakeholders and to help develop and implement solutions. Already, the evolution of cardio-oncology and cardio-obstetrics as specialties and the recognition of cardio-renal, cardio-rheumatology, and cardiometabolic diseases are helping to better identify patients earlier in the spectrum for cardiovascular disease and allowing for great awareness and education across a broader array of health care providers, including primary care.
As we think about these intersections, we must also think about the health care workforce and how we deliver care and how we communicate. With far too few cardiologists to manage the epidemic of cardiovascular disease worldwide, we need to work toward building capacity and creating coordinated systems of care that leverage primary care clinicians, and every member of the health care team can help prioritize preventive care, health promotion, as well as disease care and treatment.
Harnessing technology is also essential. Digital transformation and our ability to leverage new technologies that can allow us to reach more people—clinicians and patients—with tools and education will help make the bridging of conditions easier to navigate. More than 65% of the world’s population (5.27 billion people) owns a cell phone, while roughly 60% (>4 billion people) has access to the Internet and social media, respectively, making it easier to share research and best practices and/or use technology such as telehealth to provide care quickly and efficiently and at a lower cost (7).
The ACC’s NCD Academy is one example of how we’re already making strides in this area. The education platform built for the primary care community in low- and middle-income countries uses innovative eLearning technology to equip health care providers with high-quality continuing education available anytime, anywhere on topics ranging across cardiovascular disease, cancer, respiratory disease, diabetes, and even mental health. In <12 months, >13,000 primary care clinicians have completed the NCD Academy courses.
The challenge going forward will be ensuring broadband access and access to potentially transformative technologies is scalable and sustainable so that we can try to meet patients and clinicians where they are. Finding ways to use technology to screen for social factors and/or provide nonmedical “health care” or nonacute assistance that can facilitate health services at home while at the same time combating social isolation and providing support to our aging population will also be important.
The ACC has a robust innovation program that is closely looking at the intersection of technology and health care, particularly in the areas of virtual care, remote patient monitoring, and artificial intelligence–driven care. We believe that technology and the digital transformation of health care offers the single greatest opportunity to transform the future of health care delivery in countries around the world. If we remain laser focused on building digital platforms for delivering high-quality, low-cost, personalized care, we can build a health care future that enhances, not exacerbates, our ability to provide equitable care to patients regardless of their geography or income status.
U.S. Senator Ron Wyden from Oregon has said: “Fixing health care and fixing the economy are two sides of the same coin” (8). As we build back better from the COVID-19 pandemic, we have an incredible chance to rethink our approach to health and transition to the pursuit of the Quintuple Aim, with the added focus on health equity.
Together, we must work to identify the social determinants of health; target prevention through multiple channels by identifying the intersections of various diseases; use data to understand the individuals and the populations we serve; be diligent about removing implicit bias and structural barriers; and harness technology to move health care from episodic, siloed “sick care” to continuous and integrated “health care.”
Doing this right could lead to health improvements that then would translate to tremendous economic growth, including an estimated increase in the U.S. labor force by 2 million individuals and 5% greater workplace productivity for 25 million adults, including those who previously had a disability, needed to be full-time caregivers, or had chronic conditions that interfered with employment (2). These labor force impacts could add up to an increase of $3 trillion or a 10% increase in U.S. GDP by the year 2040 (2).
Previous Surgeon General Joycelyn Elders said: “Health is more than absence of disease; it is about economics, education, environment, empowerment, and community. The health and well-being of the people is critically dependent upon the health system that serves them. It must provide the best possible health with the least disparities and respond equally well to everyone” (9).
Health has been put front and center for the entire world by the COVID pandemic. Now is the time for us to seize the opportunity and embrace health as a priority. The Quintuple Aim and its focus on health equity; clinician well-being; and the pursuit of better health, improved outcomes, and lower costs is an investment that has the potential to be a game changer, not just for society, but for the economy as well.
References
- 1.Owen Arthur Quotes . BrainyMedia Inc; 2021. BrainyQuote.com.https://www.brainyquote.com/quotes/owen_arthur_168187 [Google Scholar]
- 2.Linzer K., Remes J., Singhal S. McKinsey Global Institute; October 5, 2020. How prioritizing health is a prescription for US prosperity.https://www.mckinsey.com/∼/media/McKinsey/Industries/Healthcare%20Systems%20and%20Services/Our%20Insights/How%20prioritizing%20health%20is%20a%20prescription%20for%20US%20prosperity/How-prioritizing-health-is-a-prescription-for-US-prosperity.pdf [Google Scholar]
- 3.Enekwechi A. The Commonwealth Fund Blog; January 28, 2021. Any Medicare solvency must include advancing health.https://www.commonwealthfund.org/blog/2021/any-medicare-solvency-effort-must-include-advancing-health-equity [Google Scholar]
- 4.IHI Triple Aim Initiative Institute for Healthcare Improvement. http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx
- 5.Miller D. Healthleaders; November 8, 2016. Is it time for a quadruple aim?https://www.healthleadersmedia.com/nursing/it-time-quadruple-aim [Google Scholar]
- 6.Coleman K., Wagner E., Schaefer J., Reid R., LeRoy L. Agency for Healthcare Research and Quality; 2016. Redefining Primary Care for the 21st Century. White Paper. (Prepared by Abt Associates, in partnership with the MacColl Center for Health Care Innovation and Bailit Health Purchasing, Cambridge, MA under Contract No.290-2010-00004-I/ 290-32009-T.) AHRQ Publication No. 16(17)-0022-EF. [Google Scholar]
- 7.DATAREPORTAL Digital around the world. https://datareportal.com/global-digital-overview
- 8.Kapoor S. The Economic Tribune; July 23, 2021. Filling institution voids in India. A way to prevent COVID-19.https://www.econtribune.com/post/filling-institutional-voids-in-india-a-way-to-prevent-covid-19 [Google Scholar]
- 9.Joycelyn Elders Quotes Goodreads.com. https://www.goodreads.com/author/quotes/84684.Joycelyn_Elders