Abstract
IMPORTANCE
Medical overuse is an important cause of patient harm and medical waste.
OBSERVATION
This structured literature review of English-language articles supplemented by examination of tables of contents of high-impact journals published in 2018 identified articles related to medical overuse. Articles were appraised for their methodologic quality, clinical relevance, and influence on patients. Of 1499 candidate articles, 839 addressed medical overuse. Of these, 117 were deemed to be most significant, with the 10 highest-ranking articles selected by author consensus. The most important articles on medical overuse identified issues with testing, including that procalcitonin does not affect antibiotic duration in patients with lower respiratory tract infection (4.2 vs 4.3 days); incidentalomas are present in 22% to 38% of common magnetic resonance imaging or computed tomography studies; 9% of women dying of stage IV cancer are still screened with mammography; and computed tomography lung cancer screening offers stable benefit and higher rates of harm for patients at lower risk. Articles related to overtreatment reported that urgent care clinics commonly overprescribe antibiotics (in 39% of all visits, patients received antibiotics) and that treatment of subclinical hypothyroidism had no effect on clinical outcomes. Three studies highlighted services that should be questioned, including using opioids for chronic noncancer pain (meta-analysis found no clinically significant benefit), stress ulcer prophylaxis for intensive care unit patients (mortality, 31.1% with pantoprazole vs 30.4% with placebo), and supplemental oxygen for patients with normal oxygen levels (mortality relative risk, 1.21; 95% CI, 1.03–1.43). A policy article found that state medical liability reform was associated with reduced invasive testing for coronary artery disease, including 24% fewer angiograms.
CONCLUSIONS AND RELEVANCE
The findings suggest that many tests are overused, overtreatment is common, and unnecessary care can lead to patient harm. This review of these 2018 findings aims to inform practitioners who wish to reduce overuse and improve patient care.
Medical overuse has gained traction in the national health care conversation.1 In the United States, deeper understanding about the contributions of medical overuse to the opioid epidemic2,3 has led to reduced prescribing by practitioners. The public is also learning about harms from inappropriate use of medical devices through articles that detail large investigations,4 books,5 and even film.6
The burgeoning public conversation about overuse has been accompanied by continued efforts within the medical community to address it. Initiatives have included professional meetings (such as the Preventing Overdiagnosis7 and High Value Practice Academic Alliance conferences)8; quality improvement initiatives at the institutional, payer, and state levels9,10; and targeted collections in medical journals, such as the Less is More series in JAMA Internal Medicine. The present series of updates in overuse in adult medicine11–15 has given rise to updates in pediatric16–18 and dermatology overuse (unpublished data, Arash Mostaghimi, Ashley Pournamdari, Elizabeth Tkachenko, John Barbieri, and Adewole Adamson, 2019). Additional consequences of overuse receiving attention is how overuse affects practitioners. A 2018 survey19 of physicians, nurses, and advanced practice practitioners found that self-reported provision of inappropriate or futile care was common and associated with burnout. This finding replicated previous studies of critical care practitioners20,21 and implies that reducing overuse could enhance practitioner wellness.19
This article examines and describes 10 of the most important studies published in 2018 concerning medical overuse in the care of adult patients. We divided the articles into the following categories: overtesting, overdiagnosis, services to question, and methods to reduce overuse.
Methods
Literature Search and Article Selection
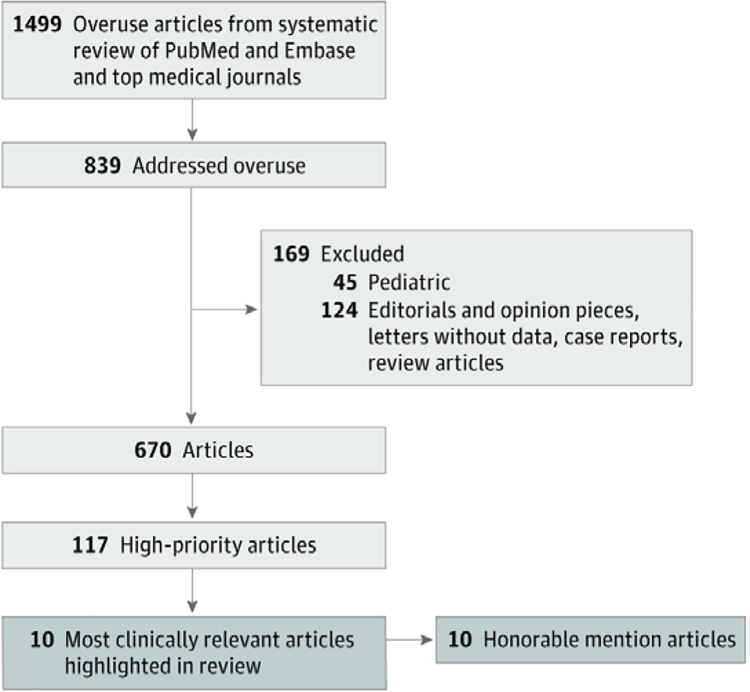
We selected articles through a structured review of studies published in 2018 that were indexed in PubMed under the Medical Subject Headings term health services misuse or with any of the following words in the title: overuse, overtreatment, overdiagnosis, inappropriate, and unnecessary. In Embase, we performed a search using these same terms with the additional Emtree term unnecessary procedure. We excluded articles with overuse injury in the title. Searches were limited to humans and English language. One of us (D.J.M., S.S.D., E.R.C., and D.K.) reviewed all titles for relevance to medical overuse. One of the same 4 authors reviewed all 2018 titles from 10 major medical journals (Figure) and read abstracts and full journal articles for those of potential relevance. We based our search methods on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.22
Figure. Review Process for All 12018 Articles From 10 Major Journals.
Major journals include Lancet, JAMA, JAMA Internal Medicine, Annals of Internal Medicine, Medical Care, PLoS Medicine, Journal of General Internal Medicine, and Journal of Hospital Medicine
The structured literature review identified 1499 articles, 839 of which addressed medical overuse. After excluding 45 pediatric articles and 124 editorials, opinion pieces, letters without data, case reports, or review articles, 670 articles remained (Figure). Of these, 117 (17.5%) were ranked as most relevant by at least 1 of us based on methodologic quality, clinical relevance, and influence on patients. From these 117 highest-rated articles, the 10 most relevant were selected by consensus among all authors and are highlighted in this article. These articles are organized into the categories of overtesting, overdiagnosis, overtreatment, services to question, and methods to reduce overuse. The 10 next most influential articles are listed for honorary mention (Table).23–32
Table.
Honorary Mention Articles
| Journal | Article | Article Title |
|---|---|---|
| JAMA Internal Medicine | Dvorin et al23 | High Frequency of Systemic Corticosteroid Use for Acute Respiratory Tract Illnesses in Ambulatory Settings |
| BMJ | Gafoor et al24 | Antidepressant Utilisation and Incidence of Weight Gain During 10 Years’ Follow-up: Population Based Cohort Study |
| BMJ | Khera et al25 | Impact of 2017 ACC/AHA Guidelines on Prevalence of Hypertension and Eligibility for Antihypertensive Treatment in United States and China: Nationally Representative Cross Sectional Study |
| American Journal of Hospice and Palliative Care | Lambden et al26 | Association of Perceived Futile or Potentially Inappropriate Care With Burnout and Thoughts of Quitting Among Health-Care Providers |
| BMJ | Paalova et al27 | Subacromial Decompression Versus Diagnostic Arthroscopy for Shoulder Impingement: Randomised, Placebo Surgery Controlled Clinical Trial |
| JAMA | Salminen et al28 | Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial |
| Journal of Preventive Medicine & Public Health | Seo and Langabeer29 | Determinants of Potentially Unnecessary Cervical Cancer Screenings in American Women |
| American Journal of Clinical Pathology | Sun et al30 | Repeating Critical Hematology and Coagulation Values Wastes Resources, Lengthens Turnaround Time, and Delays Clinical Action |
| Journal of General Internal Medicine | Zhou et al31 | Regional Supply of Medical Resources and Systemic Overuse of Health Care Among Medicare Beneficiaries |
| Journal of Emergency Medicine | Zitek et al32 | Most Transfers From Urgent Care Centers to Emergency Departments Are Discharged and ManyAre Unnecessary |
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; APPAC, Appendicitis Acuta.
Results
Overtesting
Association of Procalcitonin Measurement With Duration of Antibiotic Prescriptions Under Real-world Conditions
Huang et al33 found that procalcitonin measurement does not reduce duration of antibiotic prescriptions under real-world conditions.
Background
Procalcitonin is a peptide that is associated with bacterial infections. A prior randomized clinical trial34 found that a mandated procalcitonin guideline decreased antibiotic prescribing for acute lower respiratory tract infection (LRTI) in Europe. Less is known about how procalcitonin measurement affects antibiotic prescribing and duration in the real world.
Results
A total of 1656 patients presenting to 14 US emergency departments with acute LRTI were randomized to procalcitonin measurement with treatment threshold suggestions and an improvement bundle (education, prompts, and feedback) or usual care. An intention-to-treat analysis demonstrated no difference in days of antibiotic use (mean, 4.2 days for the treatment group and 4.3 days for the usual care group; difference, −0.05 day; 95% CI, −0.6 to 0.5 days) or adverse outcomes attributable to withholding antibiotics at 30 days (11.7% for the treatment group and 13.1% for the usual care group; difference, −1.5 percentage points; 95% CI, −4.6 to 1.7 percentage points). Similarly, a per-guideline subgroup analysis of patients for whom practitioners were completely adherent to procalcitonin guideline recommendations demonstrated no difference in antibiotic use.
Implications
Real-time knowledge of procalcitonin values and an improvement bundle did not affect antibiotic prescribing for patients with acute lower respiratory tract infection (LRTI) (patients for whom practitioners were uncertain if they needed antibiotics). Although procalcitonin may be associated with bacterial infection, it does not improve antibiotic use by practitioners.
Comprehensive Review of Incidentalomas
In a comprehensive review, O’Sullivan et al35 found widespread detection of incidentalomas.
Background
Incidentalomas are abnormalities detected on imaging procedures unrelated to the indication for testing. As the visual resolution and use of advanced imaging have increased, the possibility of incidentally detecting abnormalities of questionable clinical significance has become more common. However, data are too sparse to guide practitioners and patients in incidentally discovered abnormalities.
Results
A systematic review and meta-analysis of 20 prior systematic reviews (involving 240 primary studies) investigating incidentaloma prevalence demonstrated high rates of incidentaloma detection across imaging modalities and organ systems. The proportion of patients who received imaging and were diagnosed with an incidentaloma was highest for computed tomographic (CT) colonography (38%; 95% CI, 21%−57%), cardiac magnetic resonance imaging (MRI) (34%; 95% CI, 22%−46%), spinal MRI (22%; 95% CI, 19%−26%), and brain MRI (22%; 95% CI, 14%−31%). Of incidentally detected abnormalities, those most likely to be malignant cancers involved the breast (42%; 95% CI, 31%−54%) and the thyroid (28%; 95% CI, 20%−37%).
Implications
Before imaging is performed, patients and their physicians should consider the high likelihood of detecting incidentalomas, which can increase patient anxiety and lead to additional testing and interventions of unknown benefit and harm.
Mammograms and Resultant Additional Testing in Women With Advanced Cancer
Sadigh et al36 found that many women with advanced cancer undergo mammography and resultant additional testing.
Background
Breast cancer screening affects mortality at approximately 10 years after its execution.37 As such, it is not recommended for women with life expectancies of fewer than 10 years because of a lack of benefit,37 which is a Choosing Wisely recommendation.38
Results
Investigators used Surveillance, Epidemiology, and End Results Medicare data to evaluate rates of screening mammography and subsequent follow-up breast imaging in women with stage IV colorectal or lung cancer. Overall, 9% of women underwent screening mammography, among whom 11% underwent subsequent follow-up breast imaging (most commonly diagnostic mammography) within 9 months. Rates of resulting invasive procedures were not reported.
Implications
A significant proportion of women with advanced cancer had unnecessary screening mammography similar to the findings of a study39 of older women with limited life expectancy. The high rate of downstream imaging implies harm and waste to patients and the health care system. Practitioners ordering screening tests should limit screening to patients with sufficient life expectancy to benefit from screening.
Overdiagnosis
Harms and Benefits of Lung Cancer Screening in Relation to Underlying Risk of Lung Cancer
Caverly et al40 reported that lung cancer screening reduced harms but diminished benefits as the risk of lung cancer decreases.
Background
Computed tomographic lung cancer screening is recommended based on the National Lung Screening Trial.41 A concurrent Veterans Health Affairs lung cancer screening project found a higher false-positive rate than the National Lung Screening Trial (58% vs 26%), and early-stage lung cancer was rarely detected.42 These findings have led to questions about patient benefit. Investigators sought to compare the expected outcomes of higher observed false-positive rates in the Veterans Health Affairs among patients of varying risk.
Results
Basing the value of screening on trials that found an approximately 20% relative risk reduction in death from lung cancer, investigators modeled benefits according to patients’ baseline lung cancer risk stratified by quintiles. Patients in the lowest risk quintile had a number needed to screen of 6903 to prevent 1 lung cancer death, and those in the highest risk quintile had a number needed to screen of 687. Harms were similar across all risk groups, with approximately 55% of false-positive results requiring tracking and 2% of these needing further diagnostic evaluation.
Implications
Screening tests, including those focused on lung cancer, have effectiveness that is dependent on the pretest risk of disease. The greatest benefit to harm ratio accrues to patients with the highest risk of having cancer. Harms are relatively stable across groups. Screening programs should be tailored to individual patient risk to achieve the desired favorable outcomes.43
Overtreatment
Association of Urgent Care With Use of Antibiotics
Palms et al44 found an association between urgent care and overuse of antibiotics.
Background
The number of urgent care centers has increased markedly, with more than 10 000 clinics nationwide.45 Urgent care generally provides immediate medical evaluation with a practitioner who does not have a relationship with the patient. Infectious symptoms are a common reason for evaluation.
Results
On the basis of the Truven administrative claims data from more than 150 million visits in 2010 to 2011, inappropriate antibiotic prescribing for patients with viral illnesses occurred most frequently in urgent care centers (in 45.7% of patient visits for viral illness [n = 201 682] compared with 24.6% of such emergency department visits and 17% of primary care office visits). Antibiotics were prescribed at 39% of all urgent care visits.
Implications
Antibiotic treatment for nonindicated conditions is among the most common forms of overuse in ambulatory care and given in more than one-third of urgent care visits. Patients should be encouraged to seek care from their primary care physicians whenever possible. Urgent care centers lack sustained relationships with patients, and although they are a convenient alternative to primary care, they should improve their tendency to overtreat.
Treatment of Subclinical Hypothyroidism Among Patients With Mild to Moderate Symptoms
Feller et al46 recommend that treatment of subclinical hypothyroidism be avoided among patients with mild to moderate symptoms.
Background
Subclinical hypothyroidism is the laboratory combination of an elevated thyrotropin level and a normal range free thyroxine level. Approximately 13 million people in the United States have subclinical hypothyroidism,47 most of whom qualify for thyroid hormone treatment based on existing guidelines.48
Results
A systematic review and meta-analysis of 21 randomized clinical trials comparing thyroid hormone therapy with placebo or no treatment among 2192 nonpregnant adults with subclinical hypothyroidism found that thyroid hormone therapy was not associated with quality of life (standardized mean difference, −0.11; 95% CI, −0.25 to 0.03) or thyroid-related symptoms (standardized mean difference, 0.01; 95% CI, −0.12 to 0.14). In addition, no significant differences were found in secondary outcomes, including mood-related outcomes, cognitive function, systolic blood pressure, or body mass index. Among the 7 trials that measured hypothyroid symptoms at enrollment, the burden of symptoms was mild to moderate.
Implications
Practitioners should not routinely prescribe thyroid hormone therapy to patients with subclinical hypothyroidism and mild to moderate symptoms. Consequently, thyrotrophin testing in patients who are asymptomatic or have nonspecific symptoms may need to be reconsidered.49
Services to Question
Effectiveness of Opioids in Patients With Chronic Noncancer Pain
Busse et al50 report that opioids may be ineffective in patients with chronic noncancer pain.
Background
The opioid crisis has focused on opioid harms, with limited attention to the potential benefits of these medications. Opioids are commonly used to treat chronic noncancer pain, but their effectiveness on pain and functioning in this population compared with alternative treatments is unclear.
Results
A systematic review and meta-analysis of 96 randomized clinical trials evaluated the association of opioids with pain and functioning in diverse patients with chronic noncancer pain. In the pooled analysis, opioids were associated with more reduced pain compared with placebo; although the reduction was statistically significant, the magnitude of effect (−0.79 cm on a 10-cm visual analog scale) did not reach the threshold for clinical significance (for all trials and those with high-quality evidence). Similarly, there was a small, statistically significant improvement in physical functioning associated with opioids compared with placebo that did not reach clinical significance. Pooled analysis of moderate-quality evidence found no difference in pain relief between nonsteroidal anti-inflammatory drugs and opioids or between tricyclic antidepressants and opioids.
Implications
In 2018, many studies focused on harm from opioids, including the risk of long-term use and overdose in patients prescribed presumably short-term opioids after dental work or surgery.51 Opioids have a small and likely clinically insignificant association with chronic noncancer pain and may not be superior to nonsteroidal anti-inflammatory drugs or tricyclic antidepressants.
Routine Stress Ulcer Prophylaxis in Patients Admitted to an Intensive Care Unit
According to Krag et al,52 the benefit of routine stress ulcer prophylaxis in patients admitted to an intensive care unit (ICU) is negligible.
Background
Because patients admitted to the ICU have increased risk for stress-related gastrointestinal bleeding, proton pump inhibitors are commonly prescribed prophylactically to reduce risk. Proton pump inhibitors have been associated with Clostridium difficile infection, pneumonia, renal failure, and other adverse events.53
Results
In this multicenter, randomized, blinded pragmatic trial, 3298 patients admitted to the ICU with at least 1 risk factor for gastrointestinal bleeding were randomly assigned to 40 mg of intravenous pantoprazole or placebo. Patients with prior treatment with acid suppressants and with gastrointestinal bleeding during the index hospital admission were excluded. At 90 days, no statistically significant difference in mortality (31.1% in the pantoprazole group and 30.4% in the placebo group) or a composite of clinically important gastrointestinal bleeding, pneumonia, C difficile infection, or myocardial ischemia (21.9% in the pantoprazole group and 22.6% in the placebo group) was found. Clinically important gastrointestinal bleeding was present in 2.5% of patients randomized to the pantoprazole group vs 4.2% of patients randomized the placebo group (relative risk, 0.58; 95% CI, 0.40–0.86).
Implications
Stress ulcer prophylaxis should not be routinely used for hospitalized patients. Patients prescribed stress ulcer prophylaxis often have the treatment continued unnecessarily past ICU admission and even after discharge.54
Association of Liberal Use of Oxygen Therapy With Risk of Mortality Among Acutely Ill Patients
Chu et al55 found that liberal use of oxygen therapy increases the risk of mortality among acutely ill patients.
Background
Supplemental oxygen is commonly provided to acutely ill, nonhypoxemic patients. There is biologic plausibility for harms associated with hyperoxia, including increased vasoconstriction, inflammation, and oxidative stress.56
Results
A systematic review and meta-analysis of 25 randomized clinical trials of 16 037 acutely ill adults found that a liberal oxygen therapy strategy (supplementing those with a median baseline oxygen saturation as measured by pulse oximetry (SpO2) of 96%; interquartile range, 96%−98%) increased in-hospital mortality (relative risk, 1.21; 95% CI, 1.03–1.43) and 30-day mortality (relative risk, 1.14; 95% CI, 1.01–1.28) compared with a conservative oxygen therapy strategy. The number of patients needed to be treated with a liberal oxygen approach to result in 1 patient death was 71 patients (95% CI, 37–1000).
Implications
Routine provision of oxygen to acutely ill adults without baseline hypoxemia increases their risk of death. Supplemental oxygen should be avoided for baseline SpO2 values higher than 94%.
Methods to Reduce Overuse
Association of Medical Liability Reform With Less Invasive Testing
According to Farmer et al,57 medical liability reform may lead to less invasive testing.
Background
Defensive medicine related to fear of malpractice is the most common explanation for overuse cited by physicians.58 Although malpractice reform has seldom reduced health care costs or general rates of use,59 the effect of malpractice reform on discretionary or unnecessary care is poorly understood. Invasive cardiac procedures are known to be overused and often of uncertain appropriateness.60
Results
A quasi-experimental study evaluated the association of state-level malpractice damage caps with diagnostic testing in Medicare patients with suspected coronary artery disease. The study included physicians in 9 states that introduced damage caps between 2002 and 2005 and 20 states with no caps. After adjusting for patient and county characteristics, physicians in new-cap states ordered 24% fewer initial coronary angiograms and performed 23% less revascularization after cap introduction. There was a trend toward more noninvasive stress tests. Appropriateness of specific services was not assessed.
Implications
Malpractice damage caps may be associated with less invasive diagnostic testing in patients with suspected coronary artery disease. Although a prior study59 suggested that malpractice reform has a mixed and generally small association with overall spending, it may be associated with reductions in overuse or a shift toward less aggressive care.57 This finding may represent a promising lever for protecting patients from unnecessary harm.
Limitations
This analysis has limitations. Only top medical journals or those with specific keywords related to medical overuse were reviewed. In addition, which articles to include and key points were subjective decisions by us.
Conclusions
In 2018, the published medical literature on overuse identified research on testing, including findings that procalcitonin does not affect antibiotic treatment duration in LRTI, incidentalomas are present in 22% to 38% of common MRI or CT studies, mammography screening is performed for 1 of 10 women with stage IV cancer, and CT lung cancer screening achieves 10-fold benefit if used in the highest-risk patients. Overtreatment was well documented, including that 39% of all patients visiting urgent care facilities received antibiotics and that detection and treatment of subclinical hypothyroidism had no effect on clinical outcomes. Three studies50,52,55 highlighted questionable services, including the use of opioids for chronic noncancer pain, stress ulcer prophylaxis in ICU patients, and supplemental oxygen for hospitalized patients with SpO2 greater than 94%. State medical liability reform was associated with reduced invasive testing for coronary artery disease.
As with past updates,11–15 this abstraction identified many routine current practices that are unequivocally unnecessary. These practices are often theoretically beneficial based on a physiologic rationale with minimal clinical evidence. Examples from this category included opioids for noncancer chronic pain, proton pump inhibitors for prophylaxis in the ICU, treatment of subclinical hypothyroidism, and liberal use of oxygen therapy. Notable additions from honorary mention articles included the commonly used subacromial decompression surgery, which was no better than sham surgery,27 and evidence that most patients with appendicitis do not need appendectomy.28 Such work highlights the peril of creating practice standards based on low-level evidence or simply on a physiologic basis and then requiring high-level evidence to question or reverse such practices.61
New models of care delivery are changing the context in which patients are interacting with the health care system and professionals. The increasing number of urgent care facilities, which provide immediate care without patient relationships, is particularly notable.44 In some ways, this is similar to past experiences of indigent populations, uninsured persons, and those without a personal physician seeking primary care in emergency departments. Urgent care often results in excessive use of antibiotics, inappropriate emergency department referrals, and likely other unnecessary tests and treatments.
Individual physicians continue to be pressured to see more patients and pushed to take on too many responsibilities to do all things well.62 In many settings, physicians are incentivized to order tests and treatments. Financial incentives for physicians may take the form of payments from pharmaceutical companies63 or fee-for-service payment or health insurance metrics that reward blanket population-level strategies and disincentivize patient-centered screening and treatment decisions.64 Because of these demands, burnout is increasing and may be associated with providing unnecessary care and overuse. Restructuring medicine to disincentivize tests and unneeded treatments may increase fulfillment in clinical practice. Decreasing the burden of documentation, increasing the time spent in patient contact, and encouraging care delivery that is aligned with patients’ goals and best evidence may optimize value in health care with rewarding experiences for both patients and physicians.
Acknowledgments
Funding/Support: This study was supported in part by Cancer Center Support Grant P30 CA008748 from the National Cancer Institute to Memorial Sloan Kettering Cancer Center (Dr Korenstein), the Department of Veterans Affairs and the Robert Wood Johnson Foundation Clinical Scholars Program (Dr Dhruva), and the Johns Hopkins Center for Innovative Medicine (Dr Wright).
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest Disclosures: Dr Morgan reported receiving grants from the Agency for Healthcare Research and Quality, the National Institutes of Health, the Centers for Disease Control and Prevention, and Veterans Affairs; receiving honoraria for journal and book editing from Springer Nature; and receiving travel expenses for meetings from the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, and Lown. Dr Coon reported receiving grants from Intermountain Healthcare and Stanford University. Dr Korenstein reported receiving other support from the National Cancer Institute. No other disclosures were reported.
Contributor Information
Daniel J. Morgan, Department of Epidemiology and Public Health, University of Maryland School of Medicine, Baltimore; Department of Hospital Epidemiology, Veterans Affairs Maryland Health Care System, Baltimore, Maryland.
Sanket S. Dhruva, Department of Medicine, School of Medicine, University of California, San Francisco; San Francisco Veterans Affairs Medical Center, San Francisco, California.
Eric R. Coon, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City.
Scott M. Wright, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Deborah Korenstein, Center for Health Policy and Outcomes, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York; Department of Medicine, Weill Cornell Medical College, New York, New York.
REFERENCES
- 1.It’s Hard for Doctors to Unlearn Things, That’s Costly for All of Us. New York Times. https://www.nytimes.com/2018/09/10/upshot/its-hard-for-doctors-to-unlearn-things-thats-costly-for-all-of-us.html. Accessed June 10, 2019.
- 2.Zhu W, Chernew ME, Sherry TB, Maestas N. Initial opioid prescriptions among U.S. commercially insured patients, 2012–2017. N Engl J Med. 2019; 380(11):1043–1052. doi: 10.1056/NEJMsa1807069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shipton EA, Shipton EE, Shipton AJ. A review of the opioid epidemic: what do we do about it? Pain Ther. 2018;7(1):23–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Consortium of Investigative Journalists. Medical devices harm patients worldwide as governments fail on safety. https://www.icij.org/investigations/implant-files/medical-devices-harm-patients-worldwide-as-governments-fail-on-safety/. Accessed June 13, 2019.
- 5.Lenzer J The Danger Within Us: America’s Untested, Unregulated Medical Device Industry and One Man’s Battle to Survive It. New York, NY: Little Brown & Co; 2017. [Google Scholar]
- 6.Netflix. The Bleeding Edge. https://www.netflix.com/title/80170862. Accessed June 25, 2019.
- 7.Welcome to Preventing Overdiagnosis. 2019. https://www.preventingoverdiagnosis.net/?p=1719. Accessed June 25, 2019.
- 8.2019 National Conference on High Value Practice Academic Alliance. http://hvpaa.org/conference/. Accessed June 25, 2019. [Google Scholar]
- 9.Pugel S, Stallworth JL, Pugh LB, et al. Choosing Wisely in Georgia: a quality improvement initiative in 25 adult ambulatory medicine offices. jt Comm J Qual Patient Saf. 2018;44(12):699–707. doi: 10.1016/j.jcjq.2018.05.010 [DOI] [PubMed] [Google Scholar]
- 10.Ellen ME, Wilson MG, Vélez M, et al. ; Synthesis Working Group. Addressing overuse of health services in health systems: a critical interpretive synthesis. Health Res Policy Syst. 2018;16(1):48. doi: 10.1186/s12961-018-0325-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan DJ, Dhruva SS, Coon ER, Wright SM, Korenstein D. 2018 Update on medical overuse. JAMA Intern Med. 2019;179(2):240–246. doi: 10.1001/jamainternmed.2018.5748 [DOI] [PubMed] [Google Scholar]
- 12.Morgan DJ, Dhruva SS, Coon ER, Wright SM, Korenstein D. 2017 Update on medical overuse: a systematic review. JAMA Intern Med. 2018;178(1): 110–115. doi: 10.1001/jamainternmed.2017.4361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. 2016 Update on medical overuse: a systematic review. JAMA Intern Med. 2016;176(11): 1687–1692. doi: 10.1001/jamainternmed.2016.5381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. Update on medical practices that should be questioned in 2015. JAMA Intern Med. 2015;175(12):1960–1964. doi: 10.1001/jamainternmed.2015.5614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgan DJ, Wright SM, Dhruva S. Update on medical overuse. JAMA Intern Med. 2015;175(1):120–124. doi: 10.1001/jamainternmed.2014.5444 [DOI] [PubMed] [Google Scholar]
- 16.Coon ER, Quinonez RA, Morgan DJ, et al. 2018 Update on pediatric medical overuse: a review. JAMA Pediatr. 2019;173(4):379–384. doi: 10.1001/jamapediatrics.2018.5550 [DOI] [PubMed] [Google Scholar]
- 17.Coon ER, Young PC, Quinonez RA, Morgan DJ, Dhruva SS, Schroeder AR. 2017 Update on pediatric medical overuse: a review. JAMA Pediatr. 2018;172 (5):482–486. doi: 10.1001/jamapediatrics.2017.5752 [DOI] [PubMed] [Google Scholar]
- 18.Coon ER, Young PC, Quinonez RA, Morgan DJ, Dhruva SS, Schroeder AR. Update on pediatric overuse. Pediatrics. 2017;139(2):e20162797. doi: 10.1542/peds.2016-2797 [DOI] [PubMed] [Google Scholar]
- 19.Chamberlin P, Lambden J, Kozlov E, et al. Clinicians’ perceptions of futile or potentially inappropriate care and associations with avoidant behaviors and burnout [published online March 15, 2019]. J Palliat Med. doi: 10.1089/jpm.2018.0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meltzer LS, Huckabay LM. Critical care nurses’ perceptions of futile care and its effect on burnout. Am J Crit Care. 2004;13(3):202–208. [PubMed] [Google Scholar]
- 21.Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, et al. Perceived nonbeneficial treatment of patients, burnout, and intention to leave the job among ICU nurses and junior and senior physicians. Crit Care Med. 2017;45(3):e265–e273. doi: 10.1097/CCM.0000000000002081 [DOI] [PubMed] [Google Scholar]
- 22.PRISMA. http://www.prisma-statement.org/. Accessed June 17, 2019.
- 23.Dvorin EL, Lamb MC, Monlezun DJ, Boese AC, Bazzano LA, Price-Haywood EG. High frequency of systemic corticosteroid use for acute respiratory tract illnesses in ambulatory settings. JAMA Intern Med. 2018;178(6):852–854. doi: 10.1001/jamainternmed.2018.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gafoor R, Booth HP, Gulliford MC. Antidepressant utilisation and incidence of weight gain during 10 years’ follow-up: population based cohort study. BMJ. 2018;361:k1951. doi: 10.1136/bmj.k1951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018;362:k2357. doi: 10.1136/bmj.k2357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lambden JP, Chamberlin P, Kozlov E, et al. Association of perceived futile or potentially inappropriate care with burnout and thoughts of quitting among health-care providers [published online August 5, 2018]. Am J Hosp Palliat Care. doi: 10.1177/1049909118792517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paavola M, Malmivaara A, Taimela S, et al. ; Finnish Subacromial Impingement Arthroscopy Controlled Trial (FIMPACT) Investigators. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: randomised, placebo surgery controlled clinical trial. BMJ. 2018;362:k2860. doi: 10.1136/bmj.k2860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018;320(12):1259–1265. doi: 10.1001/jama.2018.13201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seo M, Langabeer JR II. Determinants of potentially unnecessary cervical cancer screenings in American women. J Prev Med Public Health. 2018;51(4):181–187. doi: 10.3961/jpmph.18.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun SP, Garcia J, Hayden JA. Repeating critical hematology and coagulation values wastes resources, lengthens turnaround time, and delays clinical action. Am J Clin Pathol. 2018;149(3):247–252. doi: 10.1093/ajcp/aqx156 [DOI] [PubMed] [Google Scholar]
- 31.Zhou M, Oakes AH, Bridges JFP, Padula WV, Segal JB. Regional supply of medical resources and systemic overuse of health care among medicare beneficiaries. J Gen Intern Med. 2018;33(12):2127–2131. doi: 10.1007/s11606-018-4638-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zitek T, Tanone I, Ramos A, Fama K, Ali AS. Most transfers from urgent care centers to emergency departments are discharged and many are unnecessary. J Emerg Med. 2018;54(6):882–888. doi: 10.1016/j.jemermed.2018.01.037 [DOI] [PubMed] [Google Scholar]
- 33.Huang DT, Yealy DM, Filbin MR, et al. ; ProACT Investigators. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018;379(3):236–249. doi: 10.1056/NEJMoa1802670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schuetz P, Christ-Crain M, Thomann R, et al. ; ProHOSP Study Group. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059–1066. doi: 10.1001/jama.2009.1297 [DOI] [PubMed] [Google Scholar]
- 35.O’Sullivan JW, Muntinga T, Grigg S, Ioannidis JPA. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ. 2018;361:k2387. doi: 10.1136/bmj.k2387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sadigh G, Duszak R Jr, Ward KC, et al. Downstream breast imaging following screening mammography in medicare patients with advanced cancer: a population-based study. J Gen Intern Med. 2018;33(3):284–290. doi: 10.1007/s11606-017-4212-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oeffinger KC, Fontham ETH, Etzioni R, et al. ; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314 (15):1599–1614. doi: 10.1001/jama.2015.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choosing Wisely List. https://www.choosingwisely.org/wp-content/uploads/2015/02/SGIM-Choosing-Wisely-List.pdf. Accessed June 14, 2019.
- 39.Schonberg MA, Breslau ES, McCarthy EP. Targeting of mammography screening according to life expectancy in women aged 75 and older. J Am Geriatr Soc. 2013;61(3):388–395. doi: 10.1111/jgs.12123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caverly TJ, Fagerlin A, Wiener RS, et al. Comparison of observed harms and expected mortality benefit for persons in the Veterans Health Affairs Lung Cancer Screening Demonstration Project. JAMA Intern Med. 2018;178(3):426–428. doi: 10.1001/jamainternmed.2017.8170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.US Preventive Services Task Force. Final Update Summary: Lung Cancer: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/lungcancer-screening. Accessed June 10, 2019.
- 42.Kinsinger LS, Anderson C, Kim J, et al. Implementation of lung cancer screening in the Veterans Health Administration. JAMA Intern Med. 2017;177(3):399–406. doi: 10.1001/jamainternmed.2016.9022 [DOI] [PubMed] [Google Scholar]
- 43.Predict Breast. https://breast.predict.nhs.uk/predict_v2.1. Accessed June 17, 2019.
- 44.Palms DL, Hicks LA, Bartoces M, et al. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the United States. JAMA Intern Med. 2018;178(9):1267–1269. doi: 10.1001/jamainternmed.2018.1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Urgent Care Market (Clinic Growth, Revenues by Procedure, IVD and Vaccine Sales). KaloramaInformation. https://kaloramainformation.com/product/urgent-care-market-clinic-growth-revenues-by-procedure-ivd-and-vaccine-sales/. Accessed June 14, 2019.
- 46.Feller M, Snel M, Moutzouri E, et al. Association of thyroid hormone therapy with quality of life and thyroid-related symptoms in patients with subclinical hypothyroidism: a systematic review and meta-analysis. JAMA. 2018;320(13):1349–1359. doi: 10.1001/jama.2018.13770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489–499. doi: 10.1210/jcem.87.2.8182 [DOI] [PubMed] [Google Scholar]
- 48.Rosario PW, Calsolari MR. How selective are the new guidelines for treatment of subclinical hypothyroidism for patients with thyrotropin levels at or below 10 mIU/L? Thyroid. 2013;23(5):562–565. doi: 10.1089/thy.2012.0502 [DOI] [PubMed] [Google Scholar]
- 49.Screening for thyroid dysfunction: recommendation statement. Am Fam Physician. 2015;91(11). [Google Scholar]
- 50.Busse JW, Wang L, Kamaleldin M, et al. Opioids for chronic noncancer pain: a systematic review and meta-analysis. JAMA. 2018;320(23):2448–2460. doi: 10.1001/jama.2018.18472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. doi: 10.1136/bmj.j5790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krag M, Marker S, Perner A, et al. ; SUP-ICU trial group. Pantoprazole in patients at risk for gastrointestinal bleeding in the ICU. N Engl J Med. 2018;379(23):2199–2208. doi: 10.1056/NEJMoa1714919 [DOI] [PubMed] [Google Scholar]
- 53.Schoenfeld AJ, Grady D. Adverse effects associated with proton pump inhibitors. JAMA Intern Med. 2016;176(2):172–174. doi: 10.1001/jamainternmed.2015.7927 [DOI] [PubMed] [Google Scholar]
- 54.Wohlt PD, Hansen LA, Fish JT. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmacother. 2007;41(10): 1611–1616. doi: 10.1345/aph.1K227 [DOI] [PubMed] [Google Scholar]
- 55.Chu DK, Kim LH-Y, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–1705. doi: 10.1016/S0140-6736(18)30479-3 [DOI] [PubMed] [Google Scholar]
- 56.Hafner S, Beloncle F, Koch A, Radermacher P, Asfar P. Hyperoxia in intensive care, emergency, and peri-operative medicine: Dr. Jekyll or Mr. Hyde? a 2015 update. Ann Intensive Care. 2015;5(1):42. doi: 10.1186/s13613-015-0084-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Farmer SA, Moghtaderi A, Schilsky S, et al. Association of medical liability reform with clinician approach to coronary artery disease management. JAMA Cardiol. 2018;3(7):609–618. doi: 10.1001/jamacardio.2018.1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PLoS One. 2017;12(9):e0181970. doi: 10.1371/journal.pone.0181970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu H, Greenberg M, Haviland A. The impact of state medical malpractice reform on individual-level health care expenditures. Health Serv Res. 2017;52 (6):2018–2037. doi: 10.1111/1475-6773.12789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Desai NR, Bradley SM, Parzynski CS, et al. Appropriate use criteria for coronary revascularization and trends in utilization, patient selection, and appropriateness of percutaneous coronary intervention. JAMA. 2015;314(19):2045–2053. doi: 10.1001/jama.2015.13764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Herrera-Perez D, Haslam A, Crain T, et al. A comprehensive review of randomized clinical trials in three medical journals reveals 396 medical reversals. Elife. 2019;8:e45183. doi: 10.7554/eLife.45183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ofri D The Business of Health Care Depends on Exploiting Doctors and Nurses. New York Times. Published June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed June 25, 2019.
- 63.Hartung DM, Johnston K, Cohen DM, Nguyen T, Deodhar A, Bourdette DN. Industry payments to physician specialists who prescribe repository corticotropin. JAMA Netw Open. 2018;1 (2):e180482. doi: 10.1001/jamanetworkopen.2018.0482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.MacLean CH, Kerr EA, Qaseem A. Time out: charting a path for improving performance measurement. N Engl J Med. 2018;378(19):1757–1761. doi: 10.1056/NEJMp1802595 [DOI] [PubMed] [Google Scholar]