ABSTRACT
Pneumoperitoneum is a known complication of percutaneous endoscopic gastrostomy tube placement that typically resolves spontaneously with conservative management. We describe the case of a 72-year-old man who developed abdominal pain and distention after percutaneous endoscopic gastrostomy tube placement who was subsequently found to have a moderate-sized pneumoperitoneum. Despite supportive care, his abdominal pain failed to improve. We report paracentesis with air aspiration as an intervention for benign pneumoperitoneum resulting in rapid and durable resolution of abdominal complaints.
INTRODUCTION
Percutaneous endoscopic gastrostomy (PEG) tube placement is a common procedure used to provide nutrition to patients who are not candidates for oral intake and those needing gastric decompression.1 Some complications of PEG placement include bleeding, PEG site infection, aspiration, buried bumper, tube dislodgement, and pneumoperitoneum. Pneumoperitoneum, the presence of air in the peritoneal cavity, has been reported with varying frequencies depending on the patient population and period of the study. In 2006, a prospective study of 65 patients showed an incidence of 20% of patients with pneumoperitoneum on x-ray.2 Further literature review revealed a range of 4.6% in a retrospective review by Park et al to 38% in an older prospective study by Gottfried et al.3,4 Pneumoperitoneum will typically self-resolve within 72 hours because of resorption of air. The pneumoperitoneum will persist more than 72 hours in some cases, but this generally is not of clinical significance. We present a case of a patient with persistent and clinically significant pneumoperitoneum managed by paracentesis with air evacuation, a previously unreported intervention in this clinical setting.
CASE REPORT
Our patient is a 72-year-old man with a relevant medical history of tongue cancer treated with chemoradiation 9 years previously. He subsequently developed dysphagia with recurrent esophageal strictures requiring dilation. This resulted in progressive weight loss despite nutritional supplements. After discussing risks and benefits, the patient opted for PEG tube placement for long-term enteral nutrition. An esophagogastroduodenoscopy with 20 French Cook PEG tube placement was performed through the “pull” technique. Excellent finger indentation and transillumination occurred during the procedure to identify the placement site. The patient tolerated the procedure with no immediate complications and was admitted to the hospital for observation.
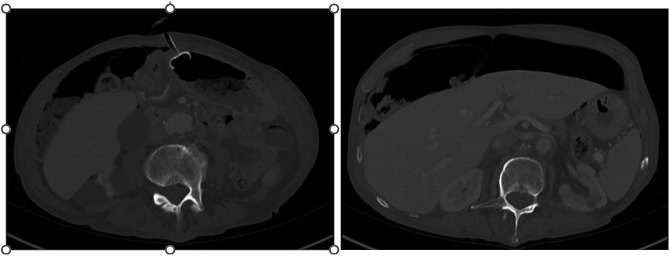
Overnight, the patient developed fever (101°F) but remained hemodynamically stable. The patient reported mild abdominal pain around the PEG site. An examination showed a mildly distended and tender abdomen with normal bowel sounds while the PEG site looked healthy without erythema, warmth, or exudate. Tube feeds were started the day after PEG tube placement. Over the course of that day, he developed worsening abdominal pain and distention. Laboratory test results showed new leukocytosis with no changes in other laboratory parameters. Tube feeds were then paused. Abdominal computed tomography (CT) was obtained and showed an appropriately placed PEG tube in the gastric body as well as moderate pneumoperitoneum (Figure 1). Two days later, an abdominal radiograph was obtained because of lack of improvement in his symptoms. The radiograph showed persistent moderate-sized pneumoperitoneum (Figure 2). Six days after the PEG tube placement, the patient's symptoms had still not improved with conservative measures, including treatment of constipation. Interventional radiology was consulted for paracentesis with air evacuation and aspirated air from the peritoneal cavity. After air evacuation, abdominal pain immediately resolved, and tube feeds were advanced to goal infusion rate without issue. The patient was seen 2 months later in the outpatient clinic, denying any further issues with abdominal symptoms, and was gaining weight with PEG tube feeding.
Figure 1.
Computed tomography of the abdomen shows percutaneous endoscopic gastrostomy tube in the stomach and moderate-sized pneumoperitoneum.
Figure 2.
The radiograph showed persistent moderate-sized pneumoperitoneum.
DISCUSSION
Pneumoperitoneum, the presence of free air in the abdominal cavity, after PEG tube placement is typically considered a benign and self-limited finding. The etiology is likely related to elevated intragastric air pressures from the endoscope and escape of air from the stomach after needle puncture.3,4 In addition, the pneumoperitoneum may also occur because of incomplete fixation of the PEG tube against the abdominal wall. A recent randomized trial showed that patients who had insufflation with carbon dioxide had more rapid reabsorption and resolution of their pneumoperitoneum than those who received ambient air.5 Although pneumoperitoneum in these patients is typically benign, the risk cannot be neglected because in the presence of peritoneal signs, it may indicate intestinal perforation, which would necessitate exploratory laparotomy.6
If patients are asymptomatic without any signs of peritonitis, no further intervention is typically necessary other than monitoring. However, other more sinister causes of pneumoperitoneum such as perforated viscus should be ruled out. An upright posteroanterior chest radiograph is typically the initial imaging examination of choice when assessing patients for pneumoperitoneum.7 However, CT scan is more sensitive than conventional radiography in the diagnosis of pneumoperitoneum and is also more capable of identifying a particular organ of concern in cases of abdominal pain of unknown origin.8 Thus, abdominal CT was a reasonable initial study for this patient.
In our case, imaging and laboratory tests did not indicate any cause for his abdominal pain other than the known pneumoperitoneum, but his symptoms failed to improve with conservative management. Thus, decision was made to proceed with paracentesis with air evacuation by interventional radiology, resulting in the resolution of both the pneumoperitoneum and the patient's symptoms. A literature review using PubMed, Cochrane, and MEDLINE uncovered no other cases of pneumoperitoneum after PEG tube placement that was managed with air evacuation. In conclusion, rare cases of persistent abdominal pain in association with moderate-sized pneumoperitoneum after PEG tube placement may benefit decompression through interventional radiology–guided pneumocentesis.
DISCLOSURES
Author contributions: T. Brotherton and A. Chhaparia wrote the manuscript. G. Sayuk, M. Presti, and J. Elwing edited the manuscript and revised the manuscript for intellectual content. T. Brotherton is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Anuj Chhaparia, Email: Anuj.Chapparia@health.slu.edu.
Michael Presti, Email: Michael.Presti@va.gov.
Gregory Sayuk, Email: gsayuk@wustl.edu.
Jill Elwing, Email: Jill.Elwing@va.gov.
REFERENCES
- 1.Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20(24):7739–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiesen AJ, Sideridis K, Fernandes A, et al. True incidence and clinical significance of pneumoperitoneum after PEG placement: A prospective study. Gastrointest Endosc. 2006;64(6):886–9. [DOI] [PubMed] [Google Scholar]
- 3.Park WY, Lee TH, Lee JS, et al. Reappraisal of pneumoperitoneum after percutaneous endoscopic gastrostomy. Intest Res. 2015;13(4):313–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gottfried EB, Plumser AB, Clair MR. Pneumoperitoneum following percutaneous endoscopic gastrostomy. A prospective study. Gastrointest Endosc. 1986;32:397–9. [DOI] [PubMed] [Google Scholar]
- 5.Murphy CJ, Adler DG, Cox K, Sommers DN, Fang JC. Insufflation with carbon dioxide reduces pneumoperitoneum after percutaneous endoscopic gastrostomy (PEG): A randomized controlled trial. Endosc Int Open. 2016;4(3):E292–E295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Snape J, Poon M, Green J, et al. Pneumo-peritoneum following PEG insertion: A clinical dilemma. JE Acute Med. 2010;9(3):120–1. [PubMed] [Google Scholar]
- 7.Roh JJ, Thompson JS, Harned RK, et al. Value of pneumoperitoneum in the diagnosis of visceral perforation. Am J Surg. 1983;146(pp):830–3. [DOI] [PubMed] [Google Scholar]
- 8.Pinto A, Miele V, Schillirò ML, et al. Spectrum of signs of pneumoperitoneum. Semin Ultrasound CT MR. 2016;37(1):3–9. [DOI] [PubMed] [Google Scholar]