Abstract
American Indian communities in Minnesota have been disproportionately impacted by the opioid use disorder (OUD) epidemic, which tribal communities have taken numerous steps to address. The Cascade of Care is a public health framework for measuring population-level OUD risk, treatment engagement, treatment retention, and recovery outcomes, which can help communities monitor the impact of responses to the OUD epidemic and identify where treatment- and recovery-related barriers and facilitators may exist. However, no studies have quantified the Cascade of Care stages within tribal communities and the extent to which these stages can be quantified using existing data sources is unknown. We utilized data from the Minnesota Drug and Alcohol Abuse Normative Evaluation System (DAANES) to quantify OUD Cascade of Care stages for an American Indian tribal nation in Minnesota and for the entire state. DAANES data indicated 269 individuals in the tribal community received treatment for opioid-related problems in 2018. Among them, an estimated 65–99% initiated medications for OUD and an estimated 13–41% were retained in treatment for at least 180 days. Existing state-level data can provide information about Cascade of Care stages for American Indian communities, particularly with regard to treatment admission, initiation of medications for OUD, and treatment retention. Additional data sources are needed to measure population-level OUD risk, recovery, and cultural and contextual factors that may impact treatment and recovery.
Keywords: cascade of care, medications for opioid use disorder, opioid use disorder, substance use disorder treatment
1.0. Land Acknowledgement
We collectively acknowledge that this research was conducted on the traditional, ancestral, and contemporary lands of Native people. This land holds great historical, spiritual, and personal significance for the Ojibwe people, before them the Dakota people, and other Native people from time immemorial. With this land acknowledgment, we affirm tribal sovereignty of the Native nations in this area and beyond (University of Minnesota Duluth, 2020).
2.0. Introduction
The opioid epidemic has disproportionately impacted American Indian communities, especially in Minnesota. Minnesota American Indian communities have declared public health emergencies, implemented comprehensive treatment programs, and become resilient leaders in addressing the opioid epidemic. These actions are warranted as American Indians in Minnesota have opioid overdose death rates that are six times higher than non-Hispanic whites in Minnesota (Tipps et al, 2018). This disproportionality is one manifestation of the perpetuation of structural racism, defined by Lawrence and Keleher (2004, p. 01) as “an array of dynamics – historical, cultural, institutional and interpersonal that routinely advantage whites while producing cumulative and chronic adverse outcomes for people of color.”
Manifestations of structural racism, including indigenous historical trauma, undermine health and exacerbate the opioid epidemic in American Indian communities (Gone et al., 2019; Skewes & Blume, 2019). Stark inadequacies in funding and conflicting federal policies have contributed to long-standing health inequities, despite a trust responsibility rooted in treaties that mandates that the United States provide health care services to American Indians in exchange for land and resources (Warne & Frizell, 2014). Contemporary efforts to improve access to health services and health outcomes for American Indians, such as the Indian Self-Determination and Education Assistance Act (ISDEAA) of 1975 and the Indian Health Care Improvement Act, have not been fully successful because of persistent underfunding (Warne & Frizzell, 2014). For example, in 2017, the Indian Health Service per capita expenditures for health care services was $4,078, compared to the national average of $9,726 per person (Government Accountability Office, 2018), thus perpetuating health inequities, including the impact of the opioid epidemic. Opioid prescribing and dispensing practices have further amplified these federal policy failures, including a lack of oversight of opioid prescribing within Indian Health Service (Office of Inspector General, 2019).
Medications for opioid use disorders (MOUD) can decrease the risk of overdose and improve psychosocial functioning, making them critical public health tools for addressing the opioid epidemic (National Academy of Sciences, Engineering, and Medicine, 2019). However, a lack of access to culturally appropriate MOUD care may prolong the opioid epidemic for American Indian communities. For example, standardized implementation of programs that offer MOUD often lack an explicit integration of spirituality and culture that honor the American Indian emphasis on spirituality, holistic healing, and wellness. In 2017, only 22% of American Indian and Alaskan Native-serving substance use treatment facilities in the US offered opioid agonist treatment and in 2018 only 40% of American Indian and Alaskan Native individuals in specialty OUD treatment in the US received MOUD (Krawczyk et al., 2021). This cautious reception toward MOUD in many American Indian populations may be due in part to the perceived lack of fit with staff expertise and training, stigma toward substance use and treatment, and misperceptions about MOUD (Venner et al., 2018). In contrast, MOUD with culturally-specific implementation approaches, integrated care, focus on family and community wellness, and adjunctive psychosocial counseling is hypothesized to facilitate greater acceptance of MOUD and better treatment outcomes (Venner et al., 2018).
The OUD Cascade of Care (Socias et al., 2016; Williams et al., 2018, 2019; Yedinak et al., 2019) has been developed as a framework that can help quantify the extent to which individuals with OUD within identified populations achieve key treatment stages, with an emphasis on MOUD engagement, treatment retention, and recovery or remission outcomes. Quantifying treatment stages this way can in turn help identify the nature of treatment barriers, optimize the implementation of OUD services, measure and reduce opioid-related health inequities, and monitor population-level changes in service engagement and population outcomes over time. Although the specific measures at each stage in the Cascade of Care have varied across studies based on available data and the clinical issues being addressed (Piske et al., 2020; Socias et al., 2016; Williams et al., 2018, 2019; Yedinak et al., 2019), the Cascade of Care typically includes population-level estimates for the number of people who: have harmful opioid use or are at risk for OUD (stage 1), have had OUD diagnosed by a healthcare provider and/or engaged in OUD care (stage 2), have initiated MOUD (stage 3), have been retained in OUD treatment for at least 6 months (stage 4), and have achieved remission or consider themselves to be in recovery (stage 5). Previous studies have utilized the Cascade of Care to characterize OUD services and clinical outcomes at national (Williams et al., 2019), state (Johnson et al., 2020; Yedinak et al., 2019), and provincial levels (Piske et al., 2020) and to evaluate the impact of policy and program development (Piske et al., 2020; Scott et al., 2020).
No research to our awareness has evaluated Cascade of Care stages within tribal communities. Moreover, most previous studies that have quantified Cascade of Care stages have done so using national-, state-, or provincial-level datasets that may not be capable of quantifying these stages within individual tribal communities (e.g., specific tribal communities often cannot be distinguished in existing datasets, smaller populations may yield insufficient sample sizes for obtaining community-level population estimates). Nonetheless, tribal communities could potentially benefit from utilizing the Cascade of Care framework to assess OUD treatment engagement and outcomes within their communities, shape interventions using data-driven strategies, and identify key priorities for public health policies as they respond to the opioid epidemic. For example, as part of the key provisions of the ISDEAA of 1975, tribes can exercise control over health care delivery services, with greater flexibility in the development of comprehensive behavioral health prevention and treatment services, and generate third-party revenue to offset inadequate funding (Warne, 2011). This flexibility provides a contextual framework for tribes to exercise their sovereign right to implement comprehensive OUD treatment services that reflect a holistic approach, encompassing the praxes of ancestral cultural knowledge and wisdom. In particular, the partner tribe of this research has implemented culturally driven models of prevention and treatment that honor sacred ancestral teachings while incorporating ceremonies and traditional practices that support their collective resiliency. The Cascade of Care has potential to guide the further development of strategies to address factors that contribute to improved health by providing an additional framework to monitor OUD treatment engagement, outcomes, and other efforts to address the impact of the opioid epidemic.
Efforts to address this gap and to support the commitment of the tribal nation described in this research in addressing the opioid crisis led to the current collaborative tribal-university research partnership that uses the OUD Cascade of Care framework to understand and tailor tribally-delivered OUD services. Specifically, the aims of this study were to (1) use data routinely collected by the state to quantify Cascade of Care stages for American Indians seeking treatment in a rural tribal nation in Minnesota and (2) compare the Cascade of Care for the tribal nation to a Cascade of Care representing the adult population of Minnesota.
In addressing these aims, we worked from a framework that emphasizes Indigenous data sovereignty and governance. Indigenous peoples “have always been data creators, data users, and data stewards” (Carroll et al, 2019, p. 02). However, a legacy of colonialism in the United States has led to many tribes relying on external sources of information about their communities’ economic, environmental, and health status (Carroll et al, 2019). In this study we employ a community-based participatory research (CBPR) framework that prioritized Indigenous data sovereignty by working with a community advisory board throughout the research process, with whom we co-designed and collaboratively interpreted the findings.
3.0. Methods
3.1. Approval and Partnership
This research was approved by the tribal Institutional Review Board (IRB) and the University of Minnesota IRB; the release of this paper was approved by the tribal IRB. The community in this study is an American Indian Tribal Nation in Minnesota. Out of respect for the wishes of the Anji’bide community advisory board (composed of members and descendants of the partnering tribal nation), the specific community will remain anonymous. The Anji’bide (Changing our Paths) project uses a CBPR approach where those directly affected by a topic are equal partners throughout the research endeavor (Wallerstein & Duran, 2006). Our team includes a community advisory board composed of individuals from the tribal nation who have lived experience with opioid use, work in opioid treatment, and/or have other relevant cultural or community experience. In line with CBPR principles, the research team shared the findings of this paper with the community advisory board for their interpretation, as part of an effort toward “decolonizing of Indigenous minds by re-centering Indigenous values and cultural practices within research practice… an essential piece is an Indigenous peoples’ struggle for self-determination” (Hisgun, as cited in Meuers, 2012). Their insights are included in the discussion section, along with those of the study authors.
Several OUD-related services available in the tribal nation are provided by Tribal Health programs and joint partnerships between the tribe and state. Services provided are tailored to be culturally appropriate and to empower tribal members. OUD-related services include (but are not limited to) syringe exchange services, pre-arrest diversion, home health, rapid screening tests, services for mothers and children, first responder (naloxone), and intensive treatment services including MOUD (buprenorphine) offered through tribally-run clinics. Inherent in the tribe’s culture is an understanding of the interconnectedness between people and the world around them. Nature is seen as an important teacher and the Earth is viewed as if a sentient being itself, deserving of gratitude for its gifts and deserving our nurturance to ensure sustainable abundance. Culture and spirituality are viewed as strengths that teach adaptability and harmony.
3.2. Data Source
Through meetings with the Minnesota Department of Health and Department of Human Services, it was determined that data from the Drug and Alcohol Abuse Normative Evaluation System (DAANES; Minnesota Department of Human Services, 2015) was a suitable data source for quantifying some stages of the Cascade of Care. All treatment providers who receive federal or state funding in Minnesota are required to enter information into the DAANES for all clients upon their admission to and discharge from substance use treatment programs, regardless of the funding source of the client.
The DAANES data received by the research team included clients who were: (1) admitted to substance use treatment programs in 2018, (2) 18 years or older, (3) identified opioids as a primary, secondary, or tertiary substance needing to be addressed at treatment admission, (4) reported American Indian race, and (5) were admitted to a tribally-run treatment clinic located within the reservation. To compare the Cascade of Care stage estimates from the tribal community to the general adult population in Minnesota, our team also received DAANES data for all adults in Minnesota who met criteria 1–3 above (all clients in the tribal community sample were also included in this sample).
3.3. Measures
The DAANES data had information that could inform several stages on the Cascade of Care, including the number of individuals who identified opioids (including heroin, non-prescribed methadone, or other opioids) as a primary, secondary, or tertiary problem upon admission to a substance use treatment facility (stage 2), the number of individuals who were reported to have received MOUD including methadone, naltrexone, or “other opioid replacement” (i.e., buprenorphine), or “other anti-craving medication” during treatment (stage 3), and the number of individuals who were retained in treatment for at least six months, indicated by a discharge date that was at least 180 days after the admission date (stage 4).
Notably, these measures differed somewhat from measures defined in previous Cascade of Care research (although specific measures used in the Cascade of Care have also varied across previous studies; Piske et al., 2020; Socias et al., 2016; Williams et al., 2018, 2019; Yedinak et al., 2019). Specifically, our measure for stage 2 characterized the number of individuals who had opioids identified as a primary, secondary, or tertiary substance addressed in treatment, which differed from the more typically reported Cascade of Care stage of being diagnosed with OUD. Additionally, for stage 4, we could only identify retention in treatment when individuals had an admission and discharge date that were at least 180 days apart, which did not include individuals who were admitted but did not have a discharge date entered. Unfortunately, the DAANES data had no measures that mapped onto Cascade of Care stage 1 (number of people at risk for OUD) or stage 5 (number of people who achieved remission or recovery).
3.4. Analysis Plan
Our first analytic aim was to quantify the Cascade of Care for the tribal community to the extent possible using the existing data source. Analyses for this aim were performed using DAANES data representing the tribal community, which was extracted by a representative from the Minnesota Department of Human Services and shared with the research team in a de-identified, aggregated format. Frequency tables were computed using Statistical Package for the Social Sciences software (IBM Corp, 2019) by tabulating the number of unique individuals1 meeting stages 2, 3, and 4 on the Cascade of Care for the tribal community, as defined in the Measures section above. Our second aim was to compare rates of MOUD initiation (stage 3) and retention in treatment for 180 days or more (stage 4) for members of the tribal community versus all adults in Minnesota. Chi-square tests were used to evaluate differences in the proportions of individuals reaching these subsequent stages (stages 3 and 4) among those who initiated treatment for an opioid problem (stage 2), using separate chi-square tests for the stage 3 and stage 4 tests. When outcomes were unknown due to missing discharge data, a plausible range of outcomes was estimated by generating an interval of plausible outcomes between the best-case scenario (i.e., all individuals with missing data achieved the positive outcome) and the worst-case scenario (i.e., no individuals with missing data achieved the positive outcome), with the actual outcome expected to be present somewhere within the interval between these two extreme scenarios.
4.0. Results
4.1. The Cascade of Care Quantified
4.1.1. Stage 2: OUD treatment initiation.
Based on DAANES admission records, there were 269 tribal members who were admitted to substance use treatment programs in 2018 who had opioids identified as a primary, secondary, or tertiary substance addressed during treatment (stage 2). Of note, other co-occurring substance problems were common, with 203 of these clients (76%) also reporting methamphetamine as a primary, secondary, or tertiary substance and 78–83 (29–31%) and 15–25 (6–9%) reporting the marijuana and alcohol, respectively, as substances.2
4.1.2. Stage 3: MOUD initiation.
DAANES discharge data was available for 195 (72%) of the 269 individuals included in the sample. Of the 195 individuals with discharge data, 171 received “other opioid replacement” medications (i.e., buprenorphine) and 21 received “other anti-craving medication”. No individuals received methadone or naltrexone. Therefore, we estimate that 171–192 individuals with discharge data initiated some form of MOUD (stage 3), or 88–99% of clients who had discharge data available. However, because it is unknown whether individuals without discharge data received MOUD, the rate of MOUD initiation could have ranged from as low as 64% (i.e., if none of the individuals with missing discharge initiated MOUD) to as high as 99% (i.e., if all of the individuals with missing discharge data initiated MOUD).
4.1.3. Stage 4: Treatment retention for 180 days.
The duration between DAANES admission and discharge dates were used to identify the number of clients known to be retained in treatment for at least 180 days (stage 4). There were 36 individuals meeting this criteria, reflecting 18% of the 195 clients with discharge data available. However, because the retention for individuals with missing discharge data could not be known, the rate of 180-day treatment retention could have ranged from as low as 13% (i.e., if none of the individuals with missing discharge data were retained for 180 days or longer) to as high as 41% (i.e., if all of the individuals with missing discharge data were retained for 180 days or longer).
The quantified Cascade of Care, along with the limitations of the data as described above, are depicted for the tribal community in Figure 1.
Figure 1.
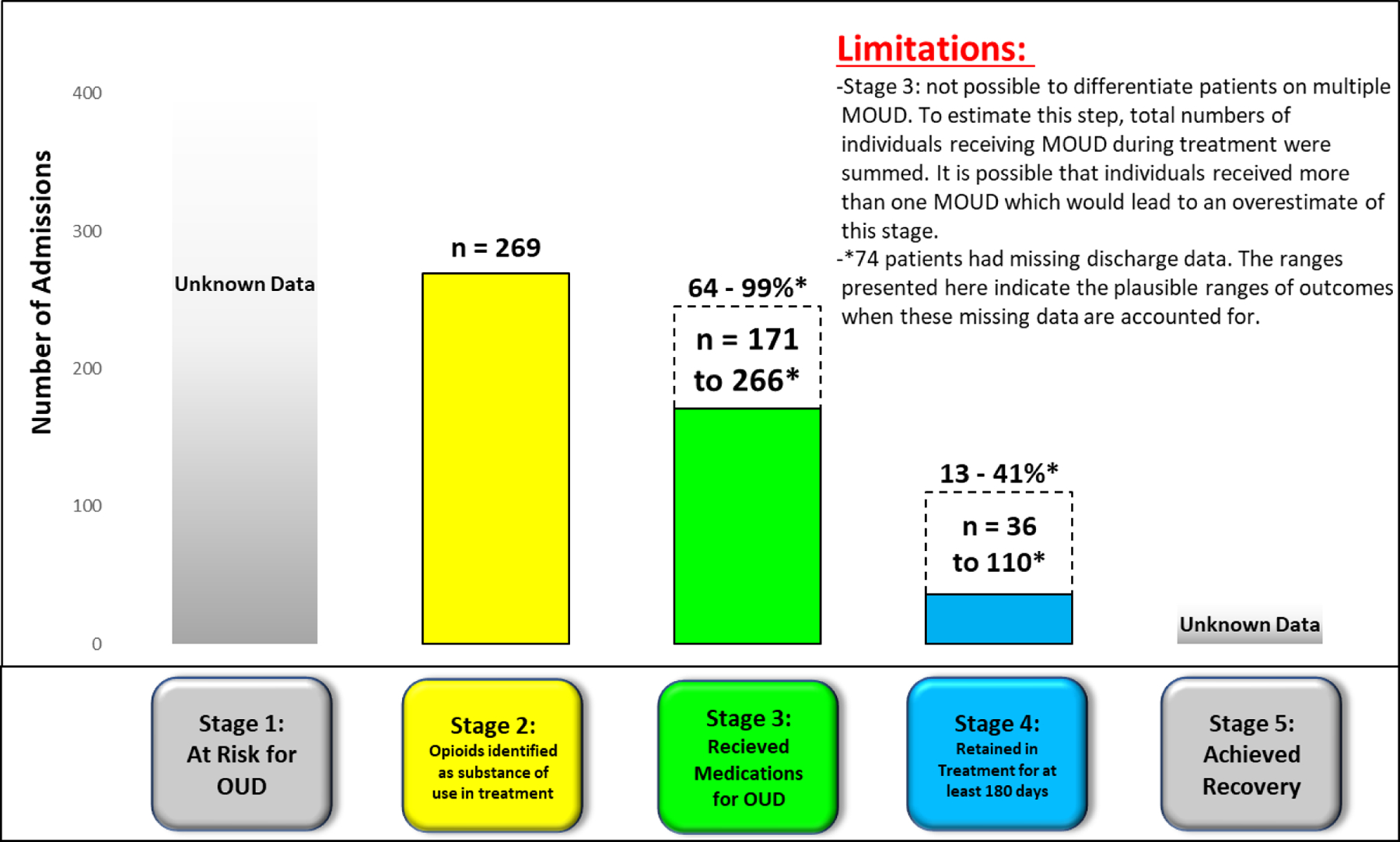
Preliminary Cascade of Care for adults in the tribal community who received treatment for an opioid use problem in 2018.
4.2. Comparison to the State-level Cascade of Care
Figure 2 displays a Cascade of Care for all adults in Minnesota, regardless of race or ethnicity, who were admitted to treatment with a primary, secondary, or tertiary problem (stage 2). The DAANES data received for this sample only included people with discharge data available, and thus these values may not reflect outcomes for individuals with missing discharge data. As shown in Figure 2, there were 10,111 individuals in this sample who had opioids identified as a primary, secondary, or tertiary problem (stage 2). Among them, 2298 (22.7%) received methadone, 214 (2.1%) received naltrexone, 1939 (19.2%) received “other opioid replacement” medication, and 296 (2.9%) received “other anti-craving” medication, suggesting a total of 4744 (46.9%) who received any type of MOUD (stage 3). There were 1218 (12.0%) individuals in this sample retained in treatment for 180 days or longer (stage 4). Chi-square tests indicated that a larger percentage of the tribal community sample received MOUD compared to the all-Minnesota sample (χ2(1)≥28.5, p<.001 for both the highest and lowest ends of the estimated interval for stage 3 in the tribal sample). Chi-square testing did not yield conclusive information about differences between the tribal community sample and the all-Minnesota sample in 180-day retention, as the test suggested higher rates of 180-day retention when missing discharge data were assumed to indicate 180-day retention (χ2(1)=192.8, p<.001), but the test suggested there was no difference in rates of 180-day retention when missing discharge data were assumed to indicate less than 180-day retention (χ2(1)=0.3, p=.57).
Figure 2.
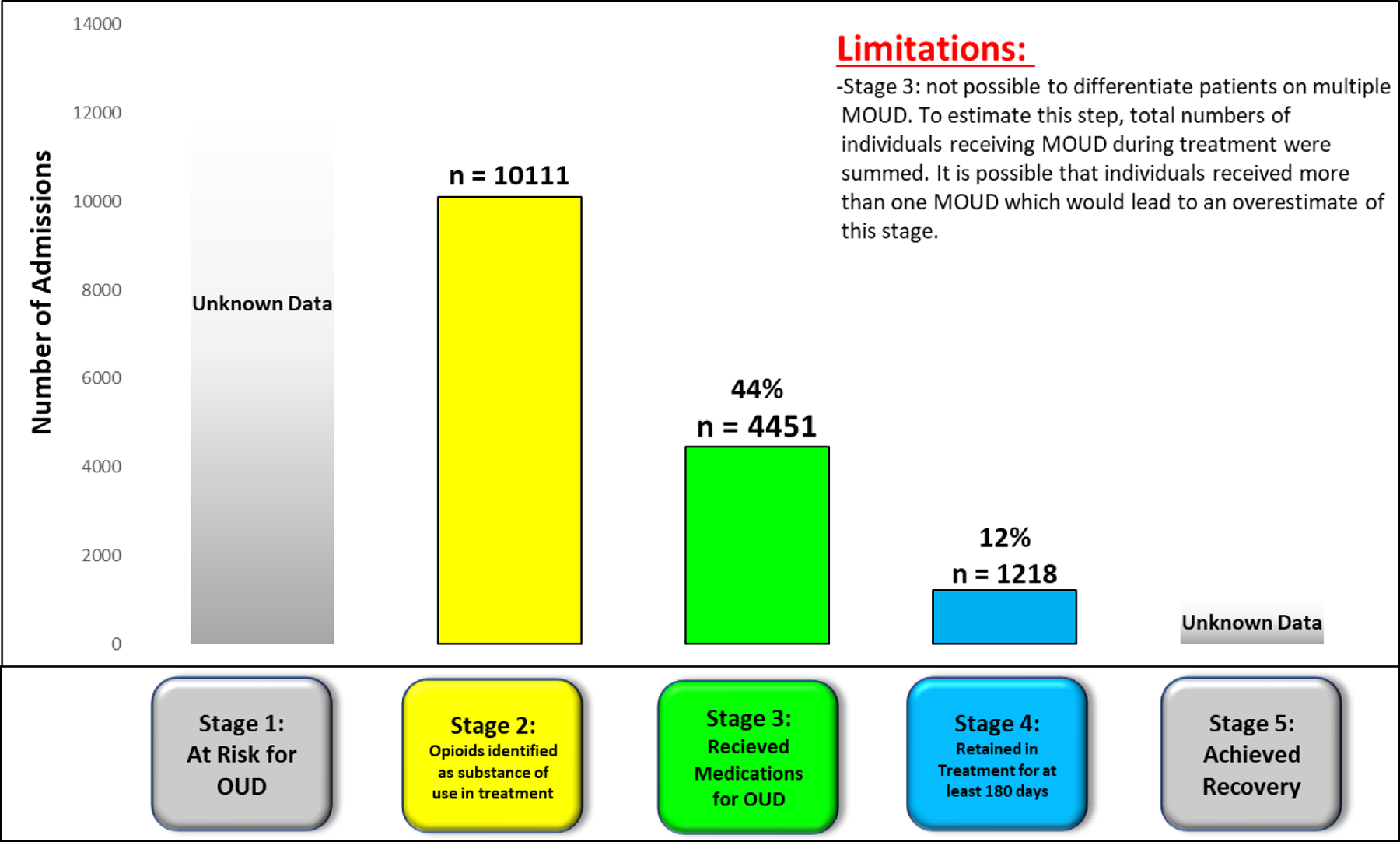
Preliminary Cascade of Care for all adults in Minnesota who received treatment for an opioid use problem in 2018.
5.0. Discussion
This study aimed to understand the extent to which the OUD Cascade of Care stages could be quantified for a specific tribal nation in Minnesota using existing data sources and to compare the Cascade of Care for that tribal nation to the entire state of Minnesota. While the Cascade of Care has been proposed as a valuable public health tool (Williams et al., 2019) and has been used to quantify OUD services and outcomes at state and provincial levels (Johnson et al., 2020; Piske et al., 2020; Yedinak et al., 2019), the ability to adequately quantify the Cascade of Care stages within specific tribal communities has not been explored until now.
Using a state-level dataset, we were able to quantify Cascade of Care stages reflecting admission to specialty substance use treatment to address a primary, secondary, or tertiary opioid problem (stage 2), initiation of MOUD (stage 3), and retention in treatment for at least 180 days (stage 4). These data had limitations, including a lack of information about cultural practices and engagement in specific services within the community that could support the treatment and recovery process despite not being explicitly part of the Cascade of Care. Additionally, 28% of clients in the tribal community sample did not have discharge data, therefore some stages had to be estimated across an interval of possible outcomes to account for these unknown outcomes. The sample only included clients who were in substance use treatment programs (i.e., not other clinical settings, such as primary care, hospitals, etc.) and we lacked data that could quantify the number of people in the community who were at risk for OUD but not yet diagnosed by a healthcare provider (stage 1) and data on rates of OUD remission and recovery (stage 5). Of note, our research team sought additional data sources that could potentially fill these gaps (e.g., National Survey on Drug Use and Health, SAMHSA, 2017; Behavioral Risk Factor Surveillance System, Centers for Disease Control, 2018); however, the number of American Indian individuals within these samples was relatively small and it was not possible to examine individuals in specific tribal communities within them. Future efforts to conduct population-based surveys in the tribal nation could be used to quantify the prevalence of risk for OUD among people in the community who have not yet been diagnosed by a healthcare provider. These surveys could assess the use of prescribed opioids for pain, use of non-medical use of opioids (prescribed or illicitly obtained), and other risk factors such as family history of substance use or psychiatric disorders (Williams et al., 2019). OUD recovery (stage 5) is also difficult to quantify, in part because definitions of recovery vary across individuals and communities. Future work should identify ways to measure these stages within tribal communities.
We also analyzed data on the Cascade of Care stages for the entire state of Minnesota. A larger percentage of individuals who initiated OUD treatment in the tribal nation initiated MOUD (stage 3) compared to the general adult population in Minnesota. Although Venner and colleagues (2018) note a preference among some American Indian communities for OUD treatment without medications, in this sample MOUD was more widely used in the tribal community than in the full-state sample. We were unable to conclude whether individuals in the tribal nation sample differed from the general adult population on the outcome of 180-day treatment retention. However, rates of 180-day retention based on available data (i.e., only including clients with discharge data) were 18% and 12% for the tribal community and full state samples, respectively, suggesting that efforts to promote longer-term treatment retention are warranted within the tribal nation and the state as a whole to improve clinical outcomes and reduce risk of overdose (Lander et al., 2020).
Access to substance use treatment outcome metrics is important for monitoring population health within tribal communities, evaluating barriers and facilitators associated with clinical services, and guiding the delivery and modification of treatment service models. Incorporating measures that can more directly quantify the Cascade of Care stages (e.g., receipt of MOUD, achieving recovery) and improving tribal communities’ access to existing data sources that can quantify these stages may help communities address the opioid epidemic in a more informed manner and aligns with principles of Indigenous data sovereignty (Carroll et al., 2019). Unfortunately, existing datasets also have limitations for tribal nations, including those discussed here (e.g., lack of measures related to culturally relevant factors).
The data presented here help quantify the extent to which gaps may exist between being diagnosed with OUD, initiating MOUD, and continuing treatment for 180 days. When reviewing the OUD Cascade of Care, the Anji’bide community advisory board discussed the historical context of distrust and fear of the healthcare system, rooted deeply within the same foundations associated with the oppressive system that directly and indirectly is seen as the cause of historical and contemporary trauma. This system of care does not always acknowledge the importance of traditional American Indian practices.
When considering the Cascade of Care, the Anji’bide community advisory board that partnered in this research highlighted the important role of Anishinaabe culture in OUD treatment, including (but not limited to) the use of tobacco, thanking the spirits for every new morning, drum and sweat lodge ceremonies, and adopting a medicine wheel approach that emphasizes a balance between physical, mental, emotional, and spiritual dimensions of wellness. These insights have also been voiced in previous research: for example, Donovan et al. (2015) found that a culturally-tailored prevention program was associated with increased hope, optimism, self-efficacy, and cultural identity, as well as reduced substance use among tribal youth, and Venner et al. (2018) have reviewed importance of culturally tailored treatments in OUD treatment for American Indians, including adopting a holistic “medicine wheel” approach.
There is little research on specific culturally tailored OUD treatments (Venner et al., 2018), although research on culturally tailored treatments for other substance use disorders may provide some guidance (McDonell, 2015). Future studies should evaluate culturally tailored treatment approaches, as well as culturally tailored versions of the Cascade of Care that account for cultural practices and tribal views of recovery, which in turn may require additional measurement methods and data sources. Future research should also address co-occurring substance use and mental health conditions, including service models for addressing these problems in tribal communities due to the additional barriers they impose on treatment initiation and retention and their associations with higher mortality (Jones & Mccance-Katz, 2019).
Along with culturally tailored treatment, having a community-based approach for both OUD treatment and research surrounding OUD treatment is important. Such an approach actively involves communities in identifying and addressing issues of concern (Hubberstey et al., 2016). MOUD programs with community support can improve community-level outcomes, such as lowering the amount of child protection cases, increasing school and community event attendance, and increasing influenza immunizations (Kanate et al., 2015). Mamakwa and colleagues (2017) found that community-based MOUD programs that used traditional healing in combination with MOUD had higher retention rates and more negative urine drug screenings than most other MOUD programs, even though those communities faced systemic racism and numerous other barriers.
In addition, the COVID pandemic has brought other challenges to the OUD epidemic and affected how tribal communities interact and provide substance use treatment. The pandemic has changed how people access healthcare, social support, and medications; many services have been reduced while telehealth has become a primary mode of treatment delivery. Identifying ways in which to incorporate culturally tailored treatment into telehealth poses a unique challenge.
6.0. Limitations and Strengths
There are noteworthy limitations of this study. The Cascade of Care stages are centered on a Euro-American medical model of OUD treatment and do not necessarily reflect cultural or tribal definitions of substance use treatment, nor do they reflect non-linear indigenous worldviews or holistic concepts of healing and health. As with any research regarding tribal communities, the results that were obtained may not be generalizable beyond the community studied here; there are over five hundred federally and state recognized tribes in the United States alone, all of which exhibit great cultural diversity.
Potential reliability limitations may exist from the data collection methods, which rely on clinician reports at substance use treatment admission and discharge. Missing data was also common and limited the precision of some results. There are many important factors that should be considered when examining treatment outcomes that could not be accounted for statistically, including those tied to structural racism (e.g., availability of services, poverty, underfunded health and human service systems, travel, distrust, isolation, housing).
Strengths of the study include the use of a data system with required data entry for all clients who are admitted to substance use treatment programs in Minnesota, which may provide a best-available estimate of OUD treatment services for the community. The use of CBPR methods is also a strength as these methods may help bridge cultural differences between researchers and the community members, empower community members, and expand the usefulness of study outcomes.
7.0. Conclusion
American Indian communities in Minnesota have been disproportionately impacted by the opioid epidemic. The OUD Cascade of Care offers unique ways to help quantify community efforts to address the opioid epidemic and can be beneficial for identifying priorities for interventions and policy changes needed to address systemic failures. Existing datasets may be able to provide information about the Cascade of Care for American Indian communities, particularly with regard to treatment admission, initiation of medications for OUD, and treatment retention; however, tribes may require additional data to more fully understand factors that facilitate or hinder treatment engagement and recovery.
Tribes continue to show resilience, strength, and leadership in addressing the opioid epidemic and increasing balance, health, and seeking minobimaadiziwin (Good Life). Federal and state partners can join in these efforts by funding health care systems at the level of need or higher, thus upholding treaty responsibilities and taking a key step towards decreasing racial health inequities.
Highlights.
OUD treatment engagement and outcomes measures are quantified in a tribal community
Clients in the tribal community being treated for OUD received MOUD at high rates
The Cascade of Care may highlight where service delivery changes are needed
Modifying the Cascade of Care may identify relevant cultural information for tribes
Acknowledgements
We wish to thank the Tribal Nation Community Advisory Board for their knowledge, help, and feedback. We want to thank the Minnesota Department of Human Services and the Minnesota Department of Health for their help with data acquisition.
Role of Funding Source
Funding for this study was provided by the National Institute on Drug Abuse (R61DA049386). NIDA played no role in study design, data collection, analysis, or interpretation, manuscript preparation, or in the decision to submit this manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare no conflicts of interest.
When an individual was admitted to more than one program in 2018, we only utilized data from their first admission.
Ranges are given for these measures because the aggregate data received by the research team provided an interval (1 to 5) instead of an exact number if the number of individuals endorsing a substance as a primary, secondary, or tertiary treatment target was less than 5.
8.0 References
- Alexander C (2020). Sharing our Knowledge Makes us Stronger. Powerpoint.
- Carroll SR, Rodriguez-Lonebear D and Martinez A, 2019. Indigenous Data Governance: Strategies from United States Native Nations. Data Science Journal, 18(1), p.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormack D, Reid P, & Kukutai T (2019). Indigenous data and health: Critical approaches to ‘race’/ethnicity and Indigenous data governance. Public Health, 172, 116–118. doi: 10.1016/j.puhe.2019.03.026 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2018. [Google Scholar]
- Donovan DM, Thomas LR, Sigo RL, Price L, Lonczak H, Lawrence N, Ahvakana K, Austin L, Lawrence A, Price J, Purser A, Bagley L. Healing of the canoe: preliminary results of a culturally tailored intervention to prevent substance abuse and promote tribal identity for Native youth in two Pacific Northwest tribes. Am Indian Alsk Native Ment Health Res. 2015;22(1):42–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, & Burrage RL (2019). The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: A systematic review. American Psychologist, 74(1), 20–35. [DOI] [PubMed] [Google Scholar]
- Government Accountability Office. (2018). Indian Health Service: Spending Levels and Characteristics of IHS and Three Other Federal Health Care Programs. GAO-19–74R: Published: Dec 10, 2018. Publicly Released: Dec 10, 2018.
- Hubberstey C, Rutman D, Hume S, Bibber MV, & Poole N (2016). Toward an Evaluation Framework for Community- Based FASD Prevention Programs. The Canadian Journal of Program Evaluation.
- IBM Corp. (2019). IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp. [Google Scholar]
- Johnson K, Hills H, Ma J, Brown CH, & McGovern M (2020). Treatment for opioid use disorder in the Florida medicaid population: Using a cascade of care model to evaluate quality. The American Journal of Drug and Alcohol Abuse, 1–9. [DOI] [PMC free article] [PubMed]
- Jones CM, & Mccance-Katz EF (2019). Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug and Alcohol Dependence, 197, 78–82. [DOI] [PubMed] [Google Scholar]
- Kanate D, Folk D, Cirone S, Gordon J, Kirlew M, Veale T, Bocking N, Rea S, Kelly L. Community-wide measures of wellness in a remote First Nations community experiencing opioid dependence: evaluating outpatient buprenorphine-naloxone substitution therapy in the context of a First Nations healing program. Can Fam Physician. 2015. February;61(2):160–5. [PMC free article] [PubMed] [Google Scholar]
- Kirmayer LJ, & Valaskakis GG (Eds.). (2009). Healing traditions: The mental health of Aboriginal peoples in Canada. UBC press. [Google Scholar]
- Krawczyk N, Garrett B, Ahmad NJ, Patel E, Solomon K, Stuart EA, & Saloner B (2021). Medications for Opioid Use Disorder among American Indians and Alaska Natives: Availability and Use Across a National Sample. Drug and Alcohol Dependence, 220. [DOI] [PubMed] [Google Scholar]
- Lander LR, Zheng W, Hustead JD, Mahoney JJ, Berry JH, Marshalek P, & Winstanley EL (2020). Long-term treatment retention in West Virginia’s comprehensive opioid addiction treatment (COAT) program. Journal of the Neurological Sciences, 411, 116712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence K, & Keleher T (2004). Structural Racism. Retrieved October 05, 2020, from http://www.intergroupresources.com/rc/Definitions%20of%20Racism.pdf
- Lavallée LF (2009). Practical Application of an Indigenous Research Framework and Two Qualitative Indigenous Research Methods: Sharing Circles and Anishnaabe Symbol-Based Reflection. International Journal of Qualitative Methods, 8(1). [Google Scholar]
- Legha R, Raleigh-Cohn A, Fickenscher A, & Novins D (2014). Challenges to providing quality substance abuse treatment services for American Indian and Alaska Native communities: perspectives of staff from 18 treatment centers. BMC Psychiatry, 14, 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamakwa S, Kahan M, Kanate D, Kirlew M, Folk D, Cirone S, Rea S, Parsons P, Edwards C, Gordon J, Main F, Kelly L. Evaluation of 6 remote First Nations community-based buprenorphine programs in northwestern Ontario: Retrospective study. Can Fam Physician. 2017. February;63(2):137–145. [PMC free article] [PubMed] [Google Scholar]
- McDonell Michael G, Nepom Jenny R, Leickly Emily, Suchy-Dicey Astrid, Hirchak Kait, Echo-Hawk Abigail, . . . Buchwald Dedra. (2015). A culturally-tailored behavioral intervention trial for alcohol use disorders in three American Indian communities: Rationale, design, and methods. Contemporary Clinical Trials, 47, 93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuers M (2012). Sixth annual drug and gang summit held at Red Lake. Red Lake Nation News. https://www.redlakenationnews.com/story/2012/02/27/news/sixth-annual-drug-and-gang-summit-held-at-redlake/022720120107991789514.html?fbclid=IwAR38AZaSz-8y-YJ0QII5Ga9VighvtvywukeAHNYiaYHk6y5oRWIzLEuX1T8 [Google Scholar]
- Minnesota Department of Human Services (2015). DAANES web user manual for chemical dependency treatment programs. Available at https://mn.gov/dhs/assets/daanes-web-user-manual_tcm1053-342025.pdf
- National Academies of Sciences, Engineering, and Medicine. (2019). Medications for opioid use disorder save lives. [PubMed]
- Office of Inspector General. (2019). IHS needs to improve oversight of its hospitals’ opioid prescribing and dispensing practices and consider centralizing its information technology functions. (2019, July 17). Retrieved February 25, 2021, from https://oig.hhs.gov/oas/reports/region18/181711400.asp
- Piske M, Zhou H, Min JE, Hongdilokkul N, Pearce LA, Homayra F, … & Nosyk B (2020). The cascade of care for opioid use disorder: a retrospective study in British Columbia, Canada. Addiction. [DOI] [PubMed]
- Rodriguez-Lonebear D (2016). Building a data revolution in Indian country. In KUKUTAI T & TAYLOR J (Eds.), Indigenous Data Sovereignty: Toward an agenda (pp. 253–272). Acton ACT,Australia: ANU Press. Retrieved October 7, 2020, from http://www.jstor.org/stable/j.ctt1q1crgf.21 [Google Scholar]
- SAMHSA. (2020, August 19). MAT Medications, Counseling, and Related Conditions. Retrieved October 06, 2020, from https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions
- SAMHSA Substance Abuse and Mental Health Services Administration (2017). Results from the 2016 National Survey on Drug Use and Health. Rockville, MD: HHS. SMA17–5044. [Google Scholar]
- Scott CK, Dennis ML, Grella CE, Kurz R, Sumpter J, Nicholson L, & Funk RR (2020). A community outreach intervention to link individuals with opioid use disorders to medication-assisted treatment. Journal of Substance Abuse Treatment, 108, 75–81. [DOI] [PubMed] [Google Scholar]
- Skewes MC, & Blume AW (2019). Understanding the link between racial trauma and substance use among American Indians. American Psychologist, 74(1), 88–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socías ME, Wood E, Kerr T, Nolan S, Hayashi K, Nosova E, Montaner J, & Milloy MJ (2018). Trends in engagement in the cascade of care for opioid use disorder, Vancouver, Canada, 2006–2016. Drug and alcohol dependence, 189, 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tipps RT, Buzzard GT, & McDougall JA (2018). The Opioid Epidemic in Indian Country. The Journal of Law, Medicine & Ethics, 46(2), 422–436. [DOI] [PubMed] [Google Scholar]
- Torres A, Joseph V, & Abrahamson G (2020). Reclaiming Tribal Health: A National Budget Plan to Rise Above Failed Policies and Fulfill Trust Obligations to Tribal Nations The National Tribal Budget Formulation Workgroup’s Recommendations on the Indian Health Service Fiscal Year 2022 Budget. Retrieved October 5, 2020, from https://www.nihb.org/docs/05042020/FINAL_FY22%20IHS%20Budget%20Book.pdf
- University of Minnesota Duluth. (2020, January 24). Land Acknowledgment. Retrieved October 06, 2020, from https://www.d.umn.edu/about-umd/campus-history/land
- Venner KL, Donovan DM, Campbell ANC, Wendt DC, Rieckmann T, Radin SM, Momper SL, Rosa CL. Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska Natives. Addict Behav. 2018. November;86:111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein NB, & Duran B (2006). Using community-based participatory research to address health disparities. Health promotion practice, 7(3), 312–323. [DOI] [PubMed] [Google Scholar]
- Warne D (2011). Policy issues in American Indian health governance. Journal of Law, Medicine, and Ethics, 39 (suppl. 1), 42–45. [DOI] [PubMed] [Google Scholar]
- Warne D, & Frizzell LB (2014). American Indian health policy: historical trends and contemporary issues. American Journal of Public Health, 104(S3), S263–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AR, Nunes EV, Bisaga A, Levin FR, & Olfson M (2019). Development of a cascade of care for responding to the opioid epidemic. The American Journal of Drug and Alcohol Abuse, 45(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yedinak JL, Goedel WC, Paull K, Lebeau R, Krieger MS, Thompson C, et al. (2019) Defining a recovery-oriented cascade of care for opioid use disorder: A community-driven, statewide cross-sectional assessment. PLoS Med 16(11): e1002963. [DOI] [PMC free article] [PubMed] [Google Scholar]


