Abstract
Background
Asthma is a chronic disease in which inflammation of the airways causes symptomatic wheezing, coughing and difficult breathing. Macrolides are antibiotics with antimicrobial and anti‐inflammatory activities that have been explored for the long‐term control of asthma symptoms.
Objectives
To assess the effects of macrolides compared with placebo for managing chronic asthma.
Search methods
We searched the Cochrane Airways Group Specialised Register up to March 2021. We also manually searched bibliographies of previously published reviews and conference proceedings and contacted study authors. We included records published in any language in the search.
Selection criteria
We included randomised controlled clinical trials (RCTs) involving both children and adults with asthma treated with macrolides versus placebo for four or more weeks. Primary outcomes were exacerbation requiring hospitalisation, severe exacerbations (exacerbations requiring emergency department (ED) visits or systemic steroids, or both), symptom scales, asthma control questionnaire (ACQ, score from 0 totally controlled, to 6 severely uncontrolled), Asthma Quality of Life Questionnaire (AQLQ, with score from 1 to 7 with higher scores indicating better QoL), rescue medication puffs per day, morning and evening peak expiratory flow (PEF; litres per minutes), forced expiratory volume in one second (FEV1; litres), bronchial hyperresponsiveness, and oral corticosteroid dose. Secondary outcomes were adverse events (including mortality), withdrawal, blood eosinophils, sputum eosinophils, eosinophil cationic protein (ECP) in serum, and ECP in sputum.
Data collection and analysis
Two review authors independently examined all records identified in the searches then reviewed the full text of all potentially relevant articles before extracting data in duplicate from all included studies. As per protocol, we used a fixed‐effect model. We conducted a sensitivity analysis for analyses with high heterogeneity (I2 greater than 30%). GRADE was used to assess the certainty of the body of evidence.
Main results
Twenty‐five studies met the inclusion criteria, randomising 1973 participants to receive macrolide or placebo for at least four weeks. Most of the included studies reported data from adults (mean age 21 to 61 years) with persistent or severe asthma, while four studies included children. All participants were recruited in outpatient settings. Inclusion criteria, interventions and outcomes were highly variable.
The evidence suggests macrolides probably deliver a moderately sized reduction in exacerbations requiring hospitalisations compared to placebo (odds ratio (OR) 0.47, 95% confidence interval (CI) 0.20 to 1.12; studies = 2, participants = 529; moderate‐certainty evidence). Macrolides probably reduce exacerbations requiring ED visits and/or treatment with systemic steroids (rate ratio (RaR) 0.65, 95% CI 0.53 to 0.80; studies = 4, participants = 640; moderate‐certainty evidence). Macrolides may reduce symptoms (as measured on symptom scales) (standardised mean difference (SMD) −0.46, 95% CI −0.81 to −0.11; studies = 4, participants = 136 ; very low‐certainty evidence). Macrolides may result in a little improvement in ACQ (SMD −0.17, 95% CI −0.31 to −0.03; studies = 5, participants = 773; low‐certainty evidence). Macrolides may have little to no effect on AQLQ (mean difference (MD) 0.24, 95% CI 0.12 to 0.35; studies = 6, participants = 802; very low‐certainty evidence). For both the ACQ and the AQLQ the suggested effect of macrolides versus placebo did not reach a minimal clinically important difference (MCID, 0.5 for ACQ and AQLQ) (ACQ: low‐certainty evidence; AQLQ: very low‐certainty evidence). Due to high heterogeneity (I2 > 30%), we conducted sensitivity analyses on the above results, which reduced the size of the suggested effects by reducing the weighting on the large, high quality studies.
Macrolides may result in a small effect compared to placebo in reducing need for rescue medication (MD −0.43 puffs/day, 95% CI −0.81 to −0.04; studies = 4, participants = 314; low‐certainty evidence). Macrolides may increase FEV1, but the effect is almost certainly below a level discernible to patients (MD 0.04 L, 95% CI 0 to 0.08; studies = 10, participants = 1046; low‐certainty evidence). It was not possible to pool outcomes for non‐specific bronchial hyperresponsiveness or lowest tolerated oral corticosteroid dose (in people requiring oral corticosteroids at baseline). There was no evidence of a difference in severe adverse events (including mortality), although less than half of the studies reported the outcome (OR 0.80, 95% CI 0.49 to 1.31; studies = 8, participants = 854; low‐certainty evidence). Reporting of specific adverse effects was too inconsistent across studies for a meaningful analysis.
Authors' conclusions
Existing evidence suggests an effect of macrolides compared with placebo on the rate of exacerbations requiring hospitalisation. Macrolides probably reduce severe exacerbations (requiring ED visit and/or treatment with systemic steroids) and may reduce symptoms. However, we cannot rule out the possibility of other benefits or harms because the evidence is of very low quality due to heterogeneity among patients and interventions, imprecision and reporting biases. The results were mostly driven by a well‐designed, well powered RCT, indicating that azithromycin may reduce exacerbation rate and improve symptom scores in severe asthma.
The review highlights the need for researchers to report outcomes accurately and according to standard definitions. Macrolides can reduce exacerbation rate in people with severe asthma. Future trials could evaluate if this effect is sustained across all the severe asthma phenotypes, the comparison with newer biological drugs, whether effects persist or wane after treatment cessation and whether effects are associated with infection biomarkers.
Plain language summary
Should macrolides be used for chronic asthma?
Main point: the existing evidence suggests a benefit of macrolides compared to placebo for reducing exacerbations requiring hospitalisation and severe exacerbations (defined as exacerbations requiring emergency department visit/treatment with systemic steroids). The effect of macrolides on other relevant clinical outcomes such as symptom scales and lung function is still unclear.
Background
Asthma is a chronic disease in which inflammation of the airways leads to coughing, wheezing and breathing problems. There are probably different reasons for this inflammation and why it persists, and these may require different treatments. Infection in the lungs may be one cause, and macrolides are a type of antibiotic that may be used long term as a way of improving symptoms for these people.
How we answered the question
We looked for studies on adults or children with asthma who were either given a macrolide or placebo (pretend treatment) for at least four weeks to see if it improved their symptoms and made it less likely for them to have an asthma attack, often referred to as an 'exacerbation'. We carried out our most recent search for studies in March 2021. After finding all the relevant studies, we collected information about asthma attacks requiring hospital admission, asthma attacks that needed to be treated with oral steroids, symptom scores, asthma control, quality of life, several measures of lung function, the need for rescue inhalers, serious side effects and measures of asthma activity in blood and sputum (mucous).
What we found
We found 25 studies, including two new ones that had been published since the last search was done in 2015. Overall, almost 2000 people received either macrolides or placebo. There were many problems in the way studies were described and how well they reported data, which made us consider the overall evidence to be low quality, undermining our confidence in most of the results. The studies were quite different from each other, for example in the severity of people's asthma, the type of macrolide they were given and the length of the treatment period.
Our review showed that macrolides were better than placebo in reducing exacerbations and may have benefits for some people in improving asthma symptoms, asthma control, asthma quality of life and some measures of lung function, but how much benefit and for whom are uncertain. Based on one well conducted study, the macrolide azithromycin may have some benefit for people with severe asthma, but overall the findings of this review do not support the use of macrolides for all asthma of any grade or severity. There were no reports of serious side effects of macrolides, but 16 studies did not report whether any occurred.
Summary of findings
Summary of findings 1. Macrolides compared to placebo for chronic asthma.
| Macrolide versus placebo for chronic asthma | ||||||
|
Patient or population: adults and children with chronic asthma
Settings: outpatient
Intervention: macrolide Drugs used were clarithromycin, azithromycin, roxithromycin and troleandomycin. Macrolide was given once or twice daily in most studies for 4–52 weeks (median 8 weeks). Comparison: placebo Treatment durations were calculated as weighted means of the studies included in each analysis. | ||||||
| Outcomesa | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence | Comments | |
| Assumed comparator risk** | Corresponding risk | |||||
| Placebo | Macrolide | |||||
|
Exacerbation requiring hospitalisation Weighted mean study duration: 45 weeks |
61 per 1000 | 29 per 1000 (13 to 68) |
OR 0.47 (0.20 to 1.12) |
529 (2 RCTs) |
⊕⊕⊕⊝ Moderateb |
— |
|
Severe exacerbations (requiring ED visits or systemic steroids, or both) Number of people having ≥ 1 exacerbations requiring an ED visit or systemic steroids, or both. Classification varied across studies. Weighted mean study duration: 35 weeks |
410 per 1000 | 311 per 1000 (269 to 357) | Rate ratio 0.65 (0.53 to 0.80) | 640 (4 RCTs) | ⊕⊕⊕⊝ Moderateb | — |
|
Asthma symptoms – symptom scales (various scales; lower score = better) Weighted mean study duration: 10 weeks |
The mean change in symptom scales in the intervention group compared to the control group was a reduction; 0.46 SD lower (0.81 SD lower to 0.11 SD lower) | — | 136 (4 RCTs) | ⊕⊝⊝⊝ Very lowe,f,g | The SMD is a Cohen's effect size and can be interpreted as moderate (< 0.4 = small, 0.40–0.70 = moderate, > 0.70 = large). | |
|
Asthma control (Asthma Control Questionnaire) Scored 0–6 (lower scores indicate improvement in asthma control) Weighted mean study duration: 34 weeks |
The mean change in asthma control in the intervention group compared to the mean change in control group was a greater reduction;0.17 SD lower (0.31 SD lower to 0.03 SD lower) | — | 773 (5 RCTs) | ⊕⊕⊝⊝ Lowd,h | The SMD is a Cohen's effect size and can be interpreted as small. | |
|
Asthma quality of life (AQLQ) Scored 1–7 (higher scores indicate improvement in quality of life) Weighted mean study duration: 35 weeks |
The mean change on the AQLQ scale in the control group was an increase from baseline; 0.31 points higher** | The mean change in AQLQ in the intervention group compared to the mean change in the control group was an increase; 0.24 points higher (0.12 higher to 0.35 higher) | — | 802 (6 RCTs) | ⊕⊝⊝⊝ Very lowc,d,h |
MCID: 0.5 points |
|
Rescue medication (puffs/day) Weighted mean study duration: 17 weeks |
The mean rescue medication use in the control group was 1.08 puffs/day** | The mean change in rescue medication puffs/day in the intervention group compared to the mean change in the control group was reduction; 0.43 fewer puffs (0.81 fewer to 0.04 fewer) | — | 314 (4 RCTs) | ⊕⊕⊝⊝ Lowd,h | — |
|
FEV1 (L) Weighted mean study duration: 28 weeks |
The mean FEV1 in the control group was 2.49 L** | The mean change in FEV1 (L) the intervention group compared to the control group was an increase; 0.04 L higher (0 L to 0.08 L higher) | — | 1046 (10 RCTs) | ⊕⊕⊝⊝ Lowh,i,j | Although there is no universally accepted MCID for FEV1 in asthma, variability within a single testing session can be up to 0.12 L (data from a mixed pool of respiratory patients; Enright 2004). |
|
Serious adverse events (including mortality) Weighted mean study duration: 16 weeks |
93 per 1000 | 76 per 1000 (50 to 118) | OR 0.80 (0.49 to 1.31) | 854 (8 RCTs) | ⊕⊕⊝⊝ Lowi,k | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). **Assumed risk for continuous outcomes were calculated as weighted means of the scores in the control group. Note: Sutherland 2010 could not be included in the rescue medication or quality of life calculations because they reported only mean difference between groups; Brusselle 2013 was not included in the FEV1 calculation because it was the only change score; Cameron 2013 was not included in the asthma control or quality of life calculations because it was the only study reporting absolute endpoint scores rather than change from baseline. AQLQ: Asthma Quality of Life Questionnaire; CI: confidence interval; ED: emergency department; FEV1: forced expiratory volume in one second; MCID: minimal clinically important difference; OR: odds ratio; RCT: randomised controlled trial; SD: standard deviation. | ||||||
| GRADE domains: study limitations, consistency of effect, imprecision, indirectness and publication bias. GRADE Working Group grades of evidence (Schünemann 2021). High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aTwo primary outcomes (morning and evening peak expiratory flow) are not presented. Bronchial hyperresponsiveness could not be pooled in a meta‐analysis and is described narratively in the review. Studies did not report lowest tolerated oral corticosteroid dose well and there were no data to analyse. bDowngraded one level for indirectness due to differences in the recruited populations and in the criteria used to define 'severe exacerbations'. cDowngraded one level for imprecision as among the included studies, one reported an important benefit of macrolide and another possible benefit of placebo. dDowngraded one level due to uncertainties with randomisation procedures and high risk of attrition bias in some studies included in the analysis. eDowngraded one level for inconsistency due to high heterogeneity (I2 = 70%) mainly due to one cross‐over study. fDowngraded one level for indirectness. Symptom scales were often invalidated and highly variable across studies, and we chose not to pool most in a meta‐analysis using standard mean differences, as this would lead to a result that would have been much more difficult to interpret. gDowngraded one level for imprecision due to small number of participants in the analysis; it was difficult to judge precision due to different scales. hDowngraded one level for indirectness as studies in the analysis recruited different populations with regard to severity of asthma, and one study only recruited smokers. iDowngraded one level for risk of bias as four studies that we were unable to properly assess for risk of bias were included in this analysis, and we were uncertain of how and when the measurement was taken in some cases. jNo change in grade: there was uncertainty in several domains across studies, but the two studies carrying most of the weight were well conducted. kDowngraded one level for imprecision; eight studies reported the outcomes, but only four studies observed events, leading to very wide confidence intervals that included important benefit and harm of macrolide treatment.
Background
Description of the condition
Asthma is an inflammatory disease of the airways characterised by chronic inflammation, bronchial hyperresponsiveness and paroxysmal attacks of wheezing. It affects people of every age, but frequently the disease occurs in childhood, especially in those who are atopic. It is estimated that asthma may affect between 1% and 18% of the general population, and it represents a significant cause of morbidity and costs for healthcare systems. Furthermore, the control of the disease is difficult to achieve in people with severe asthma, and even in people with milder asthma it may be hampered by poor adherence to treatments and lack of access to healthcare (GINA 2021).
Different phenotypes of the disease are recognised and under investigation. Current guidelines recommend tailoring asthma treatment according to a stepwise approach, considering severity of symptoms and response to treatment (GINA 2021).
Recently, the role of short‐acting bronchodilators in intermittent asthma was revised, and a combination of inhaled corticosteroids (ICS) and formoterol as needed is now recommended in people with mild asthma. Persistent asthma is treated with regular ICS, longer‐acting bronchodilators, or both (GINA 2021). More recent therapies include anti‐leukotrienes in mild‐to‐moderate asthma, humanised antibodies targeting immunoglobulin E (omalizumab), interleukin (IL)‐5 (mepolizumab, reslizumab, benralizumab), and IL‐4/‐13 (dupilumab), which are currently only recommended in severe asthma with markers of a phenotype likely to respond (e.g. raised blood eosinophils for the anti‐IL‐5 agents) (GINA 2021; Olin 2014).
Description of the intervention
Macrolides are a class of antibiotics that are widely used in the treatment of various infectious diseases, including respiratory tract infections (Alvarez‐Elcoro 1999). The first studies on macrolides in people with asthma suggested a steroid‐sparing effect (Nelson 1993), while other reports have demonstrated an anti‐inflammatory effect of this class of antibiotics, whereby macrolides seem to decrease bronchial hyperresponsiveness associated with eosinophilic inflammation (Amayasu 2000). A host‐directed anti‐inflammatory effects was also postulated (Spagnolo 2013). Macrolides are effective in the long‐term treatment of cystic fibrosis, diffuse panbronchiolitis and chronic obstructive pulmonary disease (COPD), and they are not associated with an increased risk of adverse events (Cai 2011; Spagnolo 2013).
However, a potential drawback of longer‐term antibiotic use for asthma is the development of bacterial resistance by strains that normally colonise the airways. Macrolide use in healthy volunteers led to pharyngeal carriage of macrolide‐resistant streptococci (Malhotra‐Kumar 2007), which is of particular concern for the wider community. Similar concerns were raised by studies in COPD (Brill 2015). Furthermore, the potential for arrhythmias due to QTc prolongation, potential ototoxicity and hepatotoxicity from macrolide long‐term use was highlighted in a British Thoracic Society document (BTS 2020).
How the intervention might work
Macrolides have anti‐inflammatory and antimicrobial properties that may improve asthma symptoms in two ways: by reducing airways inflammation directly and by controlling intracellular infection, which may trigger and maintain inflammation (Black 1997; Black 2000; Kawasaki 1998). Their anti‐inflammatory potential has been linked to their action on pro‐inflammatory cytokines and chemokines causing inflammation, which was highlighted by the results of the previous versions of this systematic review (Richeldi 2002; Richeldi 2005; Kew 2015). In vivo and in vitro studies of human and animal models have demonstrated that macrolides suppress the production of cytokines such as ILs and inhibit neutrophil adhesion to epithelial cells, the respiratory burst of neutrophils and the secretion of mucous from human airways (Adachi 1996; Hinks 2021; Konno 1994; Koyama 1998).
Older macrolides such as troleandomycin were investigated for a steroid‐sparing effect, related to reduced hepatic glucocorticoid metabolism (Nelson 1993).
The potential benefit of their antimicrobial action for people with asthma was suggested after observational studies identified intracellular bacterial infection (i.e. Chlamydophila pneumoniae or Mycoplasma pneumoniae) as a possible trigger of bronchial inflammation (Kraft 1998). Gencay 2001 subsequently demonstrated that people with asthma had a higher frequency of C pneumoniae antibodies than matched controls. Longitudinal studies showed no clear effect of infection with C pneumoniae on the incidence of asthma, but people who had an infection and developed asthma showed a faster decline in lung function (Pasternack 2005). Furthermore, in children with asthma, M pneumoniae detection in respiratory samples was associated with poorer asthma control (Wood 2013). Studies in animal models seem to point to an important role of the infection with C pneumoniae in the early phases of life in the pathogenesis of severe asthma (Essilfie 2015; Hansbro 2014).
Why it is important to do this review
Macrolides represent a relatively inexpensive intervention that may improve control of inflammation and clinical outcomes in people with chronic asthma.
Objectives
To assess the effects of macrolides compared with placebo for managing chronic asthma.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel and cross‐over randomised controlled trials (RCTs).
Types of participants
Children and adults with chronic asthma.
Types of interventions
Macrolides, administered for four or more weeks versus placebo. We pooled data from studies comparing different macrolide therapies.
Types of outcome measures
Primary outcomes
Exacerbations requiring hospitalisation.
Severe exacerbations (defined as requiring an emergency department (ED) visits or short‐course of systemic steroids, or both).
Asthma symptoms, control and quality of life scores.
Asthma medication requirements (need for rescue medications).
Lung function, including morning and evening peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1).
Non‐specific bronchial hyperresponsiveness (to histamine or methacholine).
Lowest tolerated oral corticosteroid dose (in people requiring oral corticosteroids at baseline).
Secondary outcomes
Number and type of serious adverse events (including mortality).
Number of study withdrawals.
Eosinophil count in peripheral blood samples, sputum samples or both.
Eosinophilic cationic protein (ECP) measurements in serum and sputum.
Search methods for identification of studies
Electronic searches
Search methods used in the previous version of this review are detailed in Appendix 1. The previously published version included searches up to April 2015. The search period for this update was April 2015 to 31 March 2021.
We searched the Cochrane Airways Trials Register on 31 March 2021. At that time the Register contained studies identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org), all years to Issue 3, 2021;
weekly searches of MEDLINE (OvidSP), 1946 to 26 March 2021;
weekly searches of Embase (OvidSP), 1974 to week 12 2021;
monthly searches of PsycINFO (OvidSP), 1967 to March week 4 2021;
monthly searches of CINAHL (EBSCO) (Cumulative Index to Nursing and Allied Health Literature), 1937 to 15 March 2021;
monthly searches of AMED (EBSCO) (Allied and Complementary Medicine), all years to 11 March 2021;
handsearches of the proceedings of major respiratory conferences.
Studies contained in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings are in Appendix 2. See Appendix 3 for search terms used to identify studies for this review. We did not restrict our search by language or type of publication.
We also searched the following trials registries on 31 March 2021:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch).
Searching other resources
We surveyed review articles and bibliographies identified from the primary papers for additional references and RCTs.
Data collection and analysis
Selection of studies
Two review authors (KU and GF) independently screened the abstracts of articles identified using the search strategy above, retrieving the full text for articles that appeared to fulfil the inclusion criteria. Two review authors (KU and GF) independently reviewed and categorised each article identified as included or excluded. When there was disagreement or doubt, a third review author (KK) assessed the article and helped to reach a consensus. We presented a PRISMA diagram to illustrate the flow of studies through the selection process (Moher 2009).
Data extraction and management
We used a data collection form to collect study characteristics and outcome data. We piloted the form on at least one study in the review. Two review authors (KU and GF) extracted the following study characteristics from included studies, when available.
Methods: study design, total duration of study, details of any run‐in period, number of study centres and location, study setting, withdrawals and date of study.
Participants: number, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria and exclusion criteria.
Interventions: intervention, comparison, concomitant medications and excluded medications.
Outcomes: primary and secondary outcomes specified and collected, and time points reported.
Notes: funding for trial, and notable conflicts of interest of trial authors.
Two review authors (KU and GF) independently extracted outcome data from included studies. We noted in the Characteristics of included studies table if outcome data were not reported in a usable way. We resolved disagreements by involving a third review author (KK). Two review authors (KK and KU) transferred data into the Review Manager 5 (Review Manager 2014). Three review authors (KU, LG and GF) double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports.
Assessment of risk of bias in included studies
Two review authors (KK and GF) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion and by involving another review author (KU). We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
Each potential source of bias was graded as high, low or unclear and justified with a quote from the study report in the risk of bias table. We summarised the risk of bias judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different from for a participant‐reported pain scale). Where information on risk of bias related to unpublished data or correspondence with a trial list, we noted this in the risk of bias table.
For treatment effects, we considered the risk of bias for the studies that contributed to that outcome.
Measures of treatment effect
We analysed dichotomous data as odds ratios (OR), incidence rate data as rate ratio (RaR) and continuous data as mean difference (MD; where studies used the same scales) or standardised mean difference (SMD; where studies used different scales). We entered data presented as a scale with a consistent direction of effect. We narratively described skewed data reported as medians and interquartile ranges. We analysed data from cross‐over trials using generic inverse variance (GIV). We pooled results from cross‐over trials and parallel trials. Where studies presented raw data and adjusted analyses (e.g. accounting for baseline differences), we used the adjusted analyses.
We undertook meta‐analyses only where meaningful, that is, if the treatments, participants and the underlying clinical question were similar enough for pooling to make sense and made decisions about this by consensus among review authors.
Where a trial reported multiple arms, we included only the relevant arms but reported all arms in the Characteristics of included studies table. If two comparisons (e.g. drug A versus placebo and drug B versus placebo) were combined in the same meta‐analysis, we halved the control group to avoid double‐counting.
If change from baseline and endpoint scores were available for continuous data, we used change from baseline unless most studies reported endpoint scores. If a study reported outcomes at multiple time points, we used the end‐of‐study treatment measurement.
When both an analysis using only participants who completed the trial and an analysis that imputed data for participants who were randomised but did not provide endpoint data (e.g. last observation carried forward) were available, we used the latter.
Unit of analysis issues
We combined events data using ORs or RaRs (number of participants or number of events) according to which measure would allow us to include the most studies. We used ORs for exacerbations requiring hospitalisation, serious adverse events (including mortality) (Peto OR) and withdrawal. We used RaRs for severe exacerbations (defined as exacerbations requiring ED visits or systemic steroids, or both). For continuous data in cross‐over trials, we entered data using GIV from suitable adjusted analyses to account for the trial's design.
Dealing with missing data
We assessed the potential for bias in each trial as a result of participants dropping out of the intervention prematurely. Where this was thought to introduce serious bias, we removed the studies in a sensitivity analysis.
Assessment of heterogeneity
We used the I2 statistic to measure heterogeneity among the trials in each analysis. If we identified high heterogeneity (e.g. I2 greater than 30%), we reported it and performed a sensitivity analysis with a random‐effects model.
Assessment of reporting biases
We were unable to pool more than 10 trials for any of the primary outcomes, so were unable to examine a funnel plot to explore possible small‐study and publication biases.
Data synthesis
We used a fixed‐effect model for all analyses, as we expected limited variation in effects due to differences in study populations and methods.
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses based on serological response or positivity to polymerase chain reaction (PCR) for C pneumoniae.
Sensitivity analysis
We performed a sensitivity analysis with a random‐effects model in case of high heterogeneity (I2 greater than 30%).
Summary of findings and assessment of the certainty of the evidence
The summary of findings table included the following outcomes: number of exacerbations requiring hospitalisation; severe exacerbations (requiring ED visits or short‐course systemic steroids, or both); asthma symptoms (including symptom scores, asthma control and Asthma Quality of Life Questionnaire (AQLQ)); asthma medication requirements (as reliever); lung function (including morning and evening PEF and FEV1); non‐specific bronchial hyperresponsiveness; serious adverse events; withdrawal; blood and sputum eosinophils; and ECP in serum and sputum.
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of the body of evidence as it related to the studies that contributed data to the meta‐analyses for the prespecified outcomes. Except for serious adverse events, we did not perform GRADE ratings on the secondary outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) using GRADEpro software (GRADEpro GDT). We justified all decisions to downgrade or upgrade the certainty of the evidence using footnotes and made comments to aid reader's understanding of the review where necessary.
Results
Description of studies
Results of the search
The literature search of previous versions of this review up to April 2015 identified 137 citations. Out of the 38 references identified in the search between 2007 and 2015, duplicate sifting of the titles and abstracts alone identified 33 potentially eligible studies for inclusion in the systematic review. Among them, review authors were concordant in identifying 16 RCTs to be included in the previous update of the systematic review (Kew 2015). Six of the 16 RCTs were identified in a previous meta‐analysis (Tong 2015); these Chinese trials were only listed in China's biomedical databases. The authors of this review were able to confirm key study characteristics in order to include them, although risk of bias could not be properly assessed.
For this updated review, the search extended to March 2021. We identified 55 new references. Seven titles referring to abstracts presented at congresses were duplicates of other studies already included in the review, while one title (Gibson 2019) was a subgroup analysis of another RCT (Gibson 2017) included in this update, leaving 20 references for screening. We excluded four based on the abstract alone and 13 after screening the full‐text of the original manuscripts, leaving two new studies eligible for inclusion in the systematic review and meta‐analyses (Wan 2016; Gibson 2017). One study is ongoing, no results available. See Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies tables. The study flow of the new included studies is presented in Figure 1.
1.

Study flow diagram.
Included studies
We included 25 RCTs (Amayasu 2000; Belotserkovskaya 2007; Black 2001; Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; He 2009; Kamada 1993; Kapoor 2010; Kostadima 2004; Kraft 2002; Nelson 1993; Piacentini 2007; Shoji 1999; Simpson 2008; Strunk 2008; Sutherland 2010; Wan 2016; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013). For brief descriptions of the included studies, refer to the Characteristics of included studies table. For a summary of study characteristics and a narrative on the main results of each study, see Table 2 and Appendix 4.
1. Summary characteristics of included studies at baseline.
| Study ID | Country | Number of participants | Design | Duration (weeks) | Macrolide dose and schedule | Mean age (years) | % Male | % on ICS | % Predicted FEV1 |
| Amayasu 2000 | Japan and USA | 17 | C, R, DB, PC | 8 | Clarithromycin 200 mg twice daily | 38.5 | 52.9 | 0.0 | 76.2 |
| Belotserkovskaya 2007 | Russia | 51 | P, R | 8 | Azithromycin (unknown dose) | NR | NR | NR | NR |
| Black 2001 | Multinational | 219 | P, R, DB, PC | 6 | Roxithromycin 150 mg twice daily | 41.0 | 47.5 | 80.8 | 77.1 |
| Brusselle 2013 | Belgium | 109 | P, R, DB, PC | 26 | Azithromycin 250 mg once daily for 5 days then 3 times per week | 53.0 (median) | 38.5 | 100a | 82.5 |
| Cameron 2013 | UK | 77 | P, R, DB, PC | 12 | Azithromycin 250 mg once daily | 44.6 | 48.1 | 85.7 | 78.3 |
| Gibson 2017 | Australia | 420 | P, R, DB, PC | 48 | Azithromycin 500 mg 3 times per week | 60.5 | 39.3 | 99.8 | 72.9 |
| Hahn 2006 | USA, Canada | 45 | P, R, DB, PC | 6 | Azithromycin 600 mg once daily for 3 days then weekly | 47.7 | 48.9 | 80.0 | NR |
| Hahn 2012 | USA | 75 | P, R, DB, PC | 12 | Azithromycin 600 mg once daily for 3 days then weekly | 46.6 | 32.0 | 72.0 | NR |
| He 2009 | China | 40 | P, R, PC | 12 | Azithromycin 250 mg twice weekly | 34.5 | NR | NR | NR |
| Kamada 1993 | USA | 19 | P, R, DB, PC | 12 | Troleandomycin 250 µg once daily + OCS | 12.5 | 63.2 | 100 | NR |
| Kapoor 2010 | India | 40 | C, R, DB, PC | 6 | Roxithromycin 150 mg once daily | NR | NR | NR | NR |
| Kostadima 2004 | Greece | 75 | P, R, DB, PC | 8 | Clarithromycin 250 mg twice daily or 3 times daily | 43.7 | 47.1 | 100 | 85.3 |
| Kraft 2002 | USA | 55 | P, R, DB, PC | 6 | Clarithromycin 500 mg twice daily | 33.4 | 49.1 | 32.7 | 69.3 |
| Nelson 1993 | USA | 75 | P, R, DB, PC | 52 | Troleandomycin 250 mg once daily + OCS | NR | 33.3 | 0 | NR |
| Piacentini 2007 | Italy | 16 | P, R, DB, PC | 8 | Azithromycin 10 mg/kg once daily 3 days per week | 13.4 | 75 | 100 | 78.9 |
| Shoji 1999 | Japan | 14 | C, R, DB, PC | 8 | Roxithromycin 150 mg twice daily | 39.6 | 42.9 | 0.0 | 75.0 |
| Simpson 2008 | Australia | 45 | P, R, DB, PC | 8 | Clarithromycin 500 mg twice daily | 57.6 | 48.9 | NRb | 70.7 |
| Strunk 2008 | USA | 55c | P, R, DB, PC | 30 | Azithromycin 250 mg or 500 mg once daily | 11.2 | 58.2 | 100a | 101.9 |
| Sutherland 2010 | USA | 92 | P, R, DB, PC | 16 | Clarithromycin 500 mg twice daily | 39.4 | 43.5 | NR | 76.0 |
| Wan 2016 | Taiwan | 58 | P, R, PC | 4 | Clarithromycin 5 mg/kg daily | 10.1 | 60.3 | 100 | 79.7 |
| Wang 2012 | China | 45 | P, R, PC | 8 | Clarithromycin 500 mg twice daily | NR | NR | NR | NR |
| Wang 2014 | China | 58 | P, R, PC | 52 | Azithromycin 250 mg twice weekly | 29.0 | NR | NR | NR |
| Xiao 2013 | China | 210 | P, R, PC | 12 | Roxithromycin 150 mg twice daily | 34.1 | NR | NR | NR |
| Yan 2008 | China | 40 | P, R, PC | 4 | Roxithromycin 150 mg twice daily | 38.5 | NR | NR | NR |
| Zhang 2013 | China | 60 | P, R, PC | 9 | Azithromycin 100 mg once daily | NR | NR | NR | NR |
C: cross‐over; DB: double‐blind; FEV1: forced expiratory volume in one second; ICS: inhaled corticosteroid; NR: not reported; OCS: oral corticosteroids; P: parallel; PC: placebo‐controlled; R: randomised.
aAll participants were taking long‐acting beta2‐agonist + ICS combination. b82.2% were taking long‐acting beta2‐agonist + ICS combination. c19 participants were not included in the review because they were randomised to a third group who received montelukast.
The 25 included studies reported a great variability in type of participants (ranging from intermittent aspirin‐induced asthma to severe asthma), interventions (different type of macrolides, administration scheme and doses in most of the studies) and outcomes recorded.
Design
All studies were RCTs using placebo controls, and most were described as double‐blind. There were 22 parallel group studies and three cross‐over studies (Amayasu 2000; Kapoor 2010; Shoji 1999). Median study duration was 15.2 weeks (range four to 52 weeks). Two studies were reported in the form of abstracts from congresses, with a very limited amount of data available (Belotserkovskaya 2007; Kapoor 2010); the results of one new included study could not be used due to very poor reporting (Wan 2016), and only basic information was available from six Chinese studies (He 2009; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013) included in the previous version of this review (Kew 2015).
Participants
The studies included 1991 participants of whom 1973 were relevant to this review (Strunk 2008 included a third group of 18 people receiving a treatment that was outside the protocol of this review). All participants had an asthma diagnosis, which was generally established according to the guidelines in use at the time of the studies (ATS 1987; GINA 1995; GINA 2002; GINA 2007; GINA 2010; GINA 2014); these are similar to the current international guidelines for what concerns main diagnosis and grading of severity of asthma (GINA 2021).
Four studies assessed the effects of macrolide treatment in children with asthma (Kamada 1993; Piacentini 2007; Strunk 2008; Wan 2016), and the rest recruited adults with asthma (aged over 18 years). The studies varied according to GINA 2014/GINA 2020/GINA 2021 criteria for asthma severity, and often there was very little information about baseline severity.
Most studies included participants with persistent mild‐to‐severe asthma, while one included participants with mild asthma (step 1 according to GINA 2021) (Amayasu 2000), and one used people with aspirin‐induced intermittent asthma (Shoji 1999).
Five studies investigated the role of macrolides in people with evidence of C pneumoniae or M pneumoniae infection, based on serological (Black 2001; Hahn 2006; Wan 2016) or molecular (Kraft 2002; Sutherland 2010) methods. The remaining studies did not investigate the presence of these co‐infections or of other concomitant co‐infections, although we could not confirm this in the non‐English language papers. Cameron 2013 investigated the effect of macrolides in adult smokers with persistent asthma, while Brusselle 2013, Simpson 2008, and Gibson 2017 considered the effect of macrolides in people with eosinophilic and non‐eosinophilic asthma.
Interventions
Five studies compared roxithromycin with placebo (Black 2001; Kapoor 2010; Shoji 1999; Xiao 2013; Yan 2008); seven studies compared clarithromycin with placebo (Amayasu 2000; Kostadima 2004; Kraft 2002; Simpson 2008; Sutherland 2010; Wang 2014; Wan 2016); 11 studies investigated the effect of azithromycin (Belotserkovskaya 2007; Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; He 2009; Piacentini 2007; Strunk 2008; Wang 2012; Zhang 2013), and two studies assessed the effects of troleandomycin in addition to oral steroid therapy as part of a steroid‐tapering protocol (Kamada 1993; Nelson 1993).
Outcomes
Six studies did not appear in any of the quantitative syntheses (Belotserkovskaya 2007; Black 2001; Kapoor 2010; Wan 2016; Wang 2012; Zhang 2013), and two more only contributed to the bronchial hyperresponsiveness summary of results and withdrawal (Piacentini 2007; Simpson 2008).
Two studies reported data on exacerbations requiring hospitalisation (Brusselle 2013; Gibson 2017), and four on severe exacerbations (defined as exacerbations requiring ED visits or systemic steroids, or both) as an outcome, but the definition of 'severe exacerbation' used in the different studies was variable and sometimes unclear (Brusselle 2013; Gibson 2017; Kostadima 2004; Strunk 2008). The meta‐analysis of Tong 2015 did not include exacerbations as an outcome but explicitly confirmed that the Chinese studies did not report this outcome either. Data from these studies only contributed to one meta‐analysis (FEV1). We narratively summarised data that could not be meta‐analysed for the relevant outcomes.
Most studies reported measures of symptoms, asthma control or quality of life, but the analyses were limited by the way data were reported and by the use of different scales. We did not consider a meta‐analysis of all these measures to be valid or the subsequent results to be interpretable in any meaningful way, so we chose only to meta‐analyse those that we knew would be similar. We used SMDs for the 'symptom scale' meta‐analysis, which still made the effect and its precision difficult to interpret.
Four studies reported data about change in rescue medication as puffs per day in a way that could be included in meta‐analysis (Brusselle 2013; Cameron 2013; Hahn 2006; Sutherland 2010).
Most of the studies reported measures of lung function such as FEV1 or PEF, but only 10 reported data for FEV1 (Amayasu 2000; Cameron 2013; Gibson 2017; He 2009; Kraft 2002; Shoji 1999; Sutherland 2010; Wang 2014; Xiao 2013; Yan 2008), four reported morning PEF (Brusselle 2013; Cameron 2013; Kamada 1993; Sutherland 2010), and three reported for evening PEF (Brusselle 2013; Kamada 1993; Sutherland 2010) that could be pooled. There were some issues with selective reporting that prevented studies from being included in the analyses, such as data only being presented graphically or without a measure of variance (e.g. Black 2001; Wan 2016). It was often unclear when the measures were taken (i.e. pre‐ or post‐bronchodilator), but when the information was available, we recorded it in the analysis footnotes. Brusselle 2013 reported percentage FEV1, but their data could not be combined with the other studies, which reported the outcome in litres. We combined the data made available to us from Tong 2015 for He 2009, Wang 2014, Xiao 2013, and Yan 2008. We were also provided with data for peak flow for Wang 2014, Xiao 2013, and Yan 2008, but the data were a different order of magnitude to the other studies, and it did not make sense to pool them.
Nine studies considered bronchial hyperresponsiveness, but there was variation in the measures used and the way the data were reported, which meant it was not possible to meta‐analyse the data (Amayasu 2000; Cameron 2013; Kamada 1993; Kostadima 2004; Nelson 1993; Piacentini 2007; Shoji 1999; Simpson 2008; Sutherland 2010).
Most studies considered adverse events, but only eight explicitly reported serious adverse events (Amayasu 2000; Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; Kamada 1993; Sutherland 2010). While it was not ideal to include the dichotomous cross‐over data without adjusting them to account for matched pairs, there were no events in Amayasu 2000, so it did not contribute to the pooled effect.
Ten studies reported study withdrawal (Brusselle 2013; Gibson 2017; Hahn 2006; Hahn 2012; Kamada 1993; Kostadima 2004; Nelson 1993; Simpson 2008; Strunk 2008; Sutherland 2010).
Eight studies reported the effect of macrolides on markers of inflammation related to asthma activity, but they used different measures, which could not be pooled in one analysis (Amayasu 2000; Cameron 2013; Kraft 2002; Nelson 1993; Piacentini 2007; Shoji 1999; Simpson 2008; Yan 2008). There were also some issues with data accuracy or incomplete reporting that reduced our confidence in the reliability of the data. The separate analyses include very small participant numbers, mostly from the two cross‐over studies.
Two studies considered the steroid‐sparing effect of macrolides (Kamada 1993; Nelson 1993).
Excluded studies
We excluded 14 studies from the review after viewing the full papers. Reasons for exclusion are reported in the Characteristics of excluded studies table and Figure 1.
Previous versions of this systematic review excluded 17 studies after reading the full papers (Kew 2015; Richeldi 2005), so a total of 31 studies are excluded.
Studies awaiting classification
There are no studies awaiting classification.
Ongoing studies
We found one ongoing study (NCT02517099).
Risk of bias in included studies
There was considerable uncertainty relating to study methodology due to insufficient reporting in the published reports. This was particularly true for the selection bias domains, but also for blinding of outcome assessment and attrition bias. We had concerns about incomplete and selective reporting of the results for most of the studies and generally considered there to be a high risk for bias because only a few studies reported data in a way that could be pooled in meta‐analysis. Summaries of the risk of bias judgements for each study are presented in Figure 2 and Figure 3.
2.
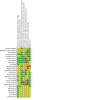
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Pharmaceutical industries financed at least five included studies (Amayasu 2000; Cameron 2013; Hahn 2006; Hahn 2012; Kamada 1993); which could raise the risk of publication bias; this could not be ascertained in the non‐English language papers. The authors of Tong 2015 provided us with information about study quality for the studies that were not available in English.
Allocation
We deemed 13 studies at low risk of bias for random sequence generation, including seven of the English language studies (Brusselle 2013; Gibson 2017; Hahn 2006; Hahn 2012; Piacentini 2007; Simpson 2008; Wan 2016) and six in Tong 2015 (He 2009; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013). For the rest, the methods for random sequence generation was unclear.
Only five studies were at low risk for adequate allocation concealment (Brusselle 2013; Gibson 2017; Hahn 2006; Hahn 2012; Wan 2016); the studies from the Tong 2015 review were not assessed for this criterion because it is not considered in the Jadad 1996 system, so we had to rate those studies as unclear, and the 14 other studies did not adequately describe the methods used.
Blinding
Most studies described as double‐blind and placebo‐controlled contained adequate descriptions of the blinding of participants and personnel, but methods were unclear in nine studies (He 2009; Wan 2016; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013, including two in an abstract form: Belotserkovskaya 2007; Kapoor 2010). Blinding of outcome assessment was adequate in seven studies (Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; Kraft 2002; Piacentini 2007; Sutherland 2010).
The same study that we rated high for performance bias also carried a high risk for detection bias (Strunk 2008).
Incomplete outcome data
Six studies had a high risk of attrition bias (Gibson 2017; Hahn 2006; Hahn 2012; Kostadima 2004; Nelson 1993; Sutherland 2010), five carried a low risk (Black 2001; Brusselle 2013; Kraft 2002; Simpson 2008; Strunk 2008), and the risk was unclear for the other 14 studies.
Selective reporting
We considered three studies at low risk of bias (Brusselle 2013; Hahn 2006; Hahn 2012). We judged eight studies at high risk of selective reporting (Belotserkovskaya 2007; Black 2001; Cameron 2013; Kamada 1993; Kapoor 2010; Simpson 2008; Strunk 2008; Sutherland 2010). This was mostly due to insufficient reporting of numerical data, which meant they could not be pooled in meta‐analysis. We rated 14 studies as unclear for this domain, including the six non‐English language studies, which we could not assess fully.
Overall, it is likely that reporting biases had a significant effect on the completeness of the meta‐analyses in this systematic review.
Other potential sources of bias
We judged Kamada 1993 to be at high risk of bias because the report showed significant baseline imbalances between groups, and this may have been an issue in some of the other trials that included very small number of participants. We judged eight studies to be at unclear risk of bias (Hahn 2012; He 2009; Kapoor 2010; Kostadima 2004; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013).
Effects of interventions
See: Table 1
We present the data with the order of outcomes listed in the methods. Evidence certainty was varied. We downgraded most for indirectness due to differences in the study populations and the way outcomes were defined, and for risk of bias due to uncertainty of randomisation procedures and high risk of attrition bias. Appendix 4 presents a narrative on each study, except for the six that we could not assess fully (He 2009; Wang 2012; Wang 2014; Xiao 2013; Yan 2008; Zhang 2013).
Primary outcomes
Exacerbations requiring hospitalisation
Two studies reported exacerbations requiring hospitalisation, with 24 events (four recorded in Brusselle 2013; 20 recorded in Gibson 2017). The meta‐analysis suggests macrolides make a moderately sized but non‐significant reduction in exacerbation requiring hospitalisation compared to placebo (OR 0.47, 95% CI 0.20 to 1.12; I2 = 0%; participants = 529; Analysis 1.1; Figure 4) (95% CI cross the line of zero effect). One study is equivocal and this effect is driven by the larger study. The evidence was of moderate certainty.
1.1. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 1: Exacerbation requiring hospitalisation
4.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.1 Exacerbation requiring hospitalisation.
Severe exacerbations
Four studies reported data on severe exacerbations (defined as exacerbations requiring ED visits or short‐course of systemic steroids, or both) (Brusselle 2013; Gibson 2017; Kostadima 2004; Strunk 2008). The pooled effect of these studies showed a benefit of macrolides over placebo (RaR 0.65, 95% CI 0.53 to 0.80; I2 = 37%; participants = 640; Analysis 1.2; Figure 5). The results were mostly driven by the data from Gibson 2017 (weight 81.6%). Apart from this study, the evidence from the other studies was very low quality, being downgraded for indirectness and imprecision. Overall the evidence was of moderate certainty.
1.2. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 2: Severe exacerbations: exacerbations requiring emergency department visits/systemic steroids
5.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.2 Severe exacerbations: exacerbations requiring emergency department visits/systemic steroids.
Asthma symptoms, control and quality of life scores
Symptom scales used across studies varied and were mostly not psychometrically validated. Data from four studies could be combined in meta‐analysis (Amayasu 2000; Hahn 2006; Hahn 2012; Kamada 1993). There was suggestion of a benefit of macrolides compared with placebo (SMD −0.46, 95% CI −0.81 to −0.11; I2 = 70%; participants = 156; Analysis 1.3; Figure 6). We downgraded the evidence for high heterogeneity (I2 = 70%), use of scales that were not psychometrically validated and small numbers in the analysis, meaning the evidence was of very low certainty.
1.3. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 3: Asthma symptom scales
6.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.3 Symptom scales.
Five studies reported measures of asthma control, mostly the Asthma Control Questionnaire (ACQ) (Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2012; Sutherland 2010). There was a small benefit of macrolide over placebo in reducing symptoms (SMD −0.17, 95% CI −0.31 to −0.03; I2 = 35%; participants = 773; Analysis 1.4; Figure 7), although the decrease in the symptom score did not reach the minimal clinically important difference (MCID) (0.5 for the ACQ, Juniper 2005). We considered the evidence to be low after downgrading for uncertainties with randomisation procedures and different populations with regards to severity of asthma.
1.4. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 4: Asthma control
7.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.4 Asthma Control.
Six studies reported quality of life measured with the AQLQ (Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; Sutherland 2010). There was an improvement of quality of life with macrolides over placebo, but it was under the MCID (MD 0.24, 95% CI 0.12 to 0.35; I2 = 55%; participants = 802; Analysis 1.5; Figure 8) (MCID: 0.5; Juniper 1994). We considered the evidence to be very low certainty after downgrading it for imprecision, uncertainties with randomisation procedures and different populations with regards to severity of asthma.
1.5. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 5: Asthma Quality of Life Questionnaire (AQLQ)
8.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.5 Asthma Quality of Life Questionnaire (AQLQ).
Need for rescue medications
Four studies reported need for rescue medication (Brusselle 2013; Cameron 2013; Hahn 2006; Sutherland 2010). Analysis indicated macrolides reduced in the need for rescue medications compared to placebo (MD −0.43 puffs per day, 95% CI −0.81 to −0.04; I2 = 0%; participants = 314; Analysis 1.6; Figure 9). The evidence was low certainty, being downgraded for uncertainties in the randomisation procedure and indirectness.
1.6. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 6: Need for rescue medication puffs/day
9.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.6 Rescue medication puffs/day.
Lung function (morning and evening peak expiratory flow and forced expiratory volume in one second)
Four studies reported morning PEF (Brusselle 2013; Cameron 2013; Kamada 1993; Sutherland 2010), and three studies reported evening PEF (Brusselle 2013; Cameron 2013; Kamada 1993; Sutherland 2010). The data for morning and evening PEF did not suggest a benefit of macrolide over placebo, and the evidence was very low certainty (morning PEF: MD 1.60 L/minute, 95% CI −10.35 to 13.56; I2 = 0%; participants = 289; Analysis 1.7; Figure 10; evening PEF: MD 1.00, 95% CI −13.65 to 15.65; I2 = 0%; participants = 212; Analysis 1.8; Figure 11). The evidence for both measures was downgraded due to issues with risk of bias, indirectness and imprecision.
1.7. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 7: Morning PEF (L/minute)
10.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.7 Morning PEF (L/minute).
1.8. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 8: Evening PEF (L/minute)
11.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.8 Evening PEF (L/minute).
Tong 2015 provided data for three additional studies, but it was not clear if they were morning or evening measurements (Wang 2014; Xiao 2013; Yan 2008). Moreover, the data were in a different order of magnitude to the other studies and had been combined using SMD, so we could not combine them. These three studies showed a benefit of macrolide over placebo, but the method of analysis meant it was difficult to contextualise.
Ten studies reported data on FEV1, that could be aggregated in a meta‐analysis (Amayasu 2000; Cameron 2013; Gibson 2017; He 2009; Kraft 2002; Shoji 1999; Sutherland 2010; Wang 2014; Xiao 2013; Yan 2008). There was a benefit of macrolide over placebo on FEV1 (MD 0.04 L, 95% CI 0 to 0.008; I2 = 66%; participants = 1046; Analysis 1.9; Figure 12). The evidence was of low certainty due to indirectness and four studies for which we were unable to properly assess risk of bias. It was not always clear whether the measurement was taken before or after a bronchodilator.
1.9. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 9: Forced expiratory volume in 1 second (FEV 1; L)
12.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.9 FEV1 (L).
Non‐specific bronchial hyperresponsiveness
We could not compare the results reported for bronchial hyperresponsiveness in nine studies due to differences in the challenge agent (e.g. methacholine, hypertonic solution) and measurement (histamine provocative concentration causing a 20% (PC20) or 15% (PC15) drop in FEV1, results expressed as log) in the different studies. We present the unpooled data in Analysis 1.10. Three studies reported an effect of macrolides in reducing bronchial hyperresponsiveness compared to placebo (Amayasu 2000; Kostadima 2004; Sutherland 2010), while six studies reported no effect compared with placebo (Cameron 2013; Kamada 1993; Nelson 1993; Piacentini 2007; Shoji 1999; Simpson 2008).
1.10. Analysis.
Comparison 1: Macrolide versus placebo, Outcome 10: Bronchial hyperresponsiveness (BHR)
| Bronchial hyperresponsiveness (BHR) | |||
| Study | Measure of BHR (units) | Results | Conclusions |
| Amayasu 2000 | Methacholine challenge test (log PC20) | Clarithromycin: 2.96, standard deviation (SD) 0.57 Placebo: 2.60, SD 0.51 (P < 0.01) |
Clarithromycin significantly reduced BHR in people with allergic intermittent asthma. |
| Cameron 2013 | Methacholine challenge test (log PC20) | Azithromycin: 0.20, SD 1.52 Placebo: 0.19, SD 1.29 (P < 0.93) |
No effect of azithromycin in smokers with persistent asthma. |
| Kamada 1993 | Methacholine challenge test (PC20) | 16/19 participants completed the test at the beginning and end of the analysis. Data were reported graphically and not included in the main analysis | No significant difference at the end of the treatment was recorded among the 3 arms of the study. |
| Kostadima 2004 | Methacholine challenge test (PC20) | Median before and after the treatment: Clarithromycin 250 mg twice daily: 0.3 mg (interquartile range (IQR) 0.1 to 1) and 1.3 mg (IQR 0.6 to 2) mg (P < 0.001) Clarithromycin 250 mg 3 times daily: 0.4 mg (IQR 0.1 to 0.9) and 2.0 mg (IQR 2.0 to 2.0) (P < 0.001) Placebo: 0.4 mg (IQR 0.1 to 0.9) and 0.3 mg (IQR 0.1 to 0.6) mg (P not significant) |
Compared to the baseline, there was a significant increase in the median PC20 in the 2 macrolide groups but not in the placebo group. |
| Nelson 1993 | Methacholine challenge test (PC20) | 11/27 participants in placebo group and 13/30 participants in troleandomycin group completed the test at the start and end of the study. Troleandomycin: +1.89 mg/mL Placebo: +0.55 mg/mL |
No significant effect of troleandomycin was recorded in comparisons within and between the study groups. |
| Piacentini 2007 | Hypertonic saline challenge (dose–response slope) | Azithromycin: 2.75, SD 2.12 to 1.42, SD 1.54 (P < 0.02) Placebo: 1.48, SD 1.75 to 1.01, SD 1.38 (P = 0.21) |
The reduction of BHR in the treatment group was driven by the change from the baseline in 3/9 participants. No significant difference observed in a comparison between the groups. Study in children. |
| Shoji 1999 | Sulpyrine inhalation testing (log PC20‐sulpyrine) | Roxithromycin: 1.18, SD 0.40 Placebo: 1.15, SD 0.43 |
No significant improvement of BHR recorded within and between group comparisons. |
| Simpson 2008 | Hypertonic saline challenge (dose–response slope; DSR) | DSR before: 1.8 (IQR 0.6 to 6.4) and after clarithromycin: 1 (IQR 0.5 to 4.2) DSR before: 1 (IQR 0.6 to 3.2) and after placebo: 1 (IQR 0.5 to 3.3) |
No significant improvement of BHR within and between group comparisons. |
| Sutherland 2010 | Methacholine challenge test (PC20 doubling dose) Analysis stratified for polymerase chain reaction (PCR) positivity for M pneumoniae or C pneumonia |
Difference between clarithromycin and placebo groups: Irrespective of PCR status: +1.2, SD 0.5 (P = 0.01) In participants with positive PCR status: +0.9, SD 1.8 (P = 0.6) In participants with negative PCR status: +1.2, SD 0.5 (P = 0.02) |
BHR was significantly improved by clarithromycin compared to placebo in the whole population and in the PCR‐negative groups, but not among the PCR‐positive participants. |
Lowest tolerated oral corticosteroid dose (in people requiring oral corticosteroids at baseline)
Most studies either excluded people taking oral corticosteroids or recruited people who did not take them regularly. Two studies that recruited people taking regular oral corticosteroids reported that macrolides had a steroid‐sparing benefit (Analysis 1.11; Figure 13; Kamada 1993; Nelson 1993). However, there was a baseline imbalance in corticosteroid dose in Nelson 1993, which overstated the difference at endpoint. We chose not to combine the study results because it was unclear if the ways the doses were calculated were sufficiently similar for pooling to make sense.
1.11. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 11: Oral corticosteroid dose
13.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.11 Oral corticosteroid dose.
Secondary outcomes
Serious adverse events
In general, macrolides were well tolerated, and there were no recorded deaths due to treatment with macrolides. Eight studies reported SAEs (Amayasu 2000; Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2006; Hahn 2012; Kamada 1993; Sutherland 2010). Meta‐analysis found no clear difference in the likelihood of SAEs in the treatment and placebo groups, but the effect was imprecise due to the rarity of events (Peto OR 0.80, 95% CI 0.49 to 1.31; I2 = 41%; participants = 854; Analysis 1.12; Figure 14).
1.12. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 12: Serious adverse events (including mortality)
14.

Forest plot of comparison: 1 Macrolide versus placebo, outcome: 1.12 Serious adverse events (including mortality).
We rated the evidence to be of low certainty due to very serious imprecision in the estimate, risk of bias issues and possible indirectness.
Study withdrawals/dropouts
Ten studies reported withdrawals/dropouts (Brusselle 2013; Gibson 2017; Hahn 2006; Hahn 2012; Kamada 1993; Kostadima 2004; Nelson 1993; Simpson 2008; Strunk 2008; Sutherland 2010). Analysis suggested the likelihood of withdrawal from the studies was similar between participants taking macrolide and placebo (OR 1.06, 95% CI 0.76 to 1.48; I2 = 0%; participants = 984; Analysis 1.13).
1.13. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 13: Withdrawal
Eosinophil counts in blood and sputum
One study reported blood eosinophils (Yan 2008). There was no difference between macrolide and placebo in blood eosinophils, but analysed data were only available as SMD, so we did not enter it with the two existing studies (Amayasu 2000; Shoji 1999). A meta‐analysis of these two small cross‐over studies showed a reduction of eosinophils in the blood of people with asthma treated with macrolides (MD −32.16, 95% CI −34.77 to −29.56; I2 = 12%; participants = 62; Analysis 1.14). Cameron 2013 investigated the effect of macrolides in sputum eosinophils in current smokers with asthma, and found a vastly different result from the two trials previously included in the analysis. The highly significant heterogeneity suggested that there was a data error (I2 = 97%). For this reason, data for the three studies have been displayed but not pooled (Analysis 1.15).
1.14. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 14: Blood eosinophils
1.15. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 15: Sputum eosinophils
Eosinophil cationic protein in serum and sputum
Two studies reported serum and sputum ECP (Amayasu 2000; Shoji 1999). Macrolides appear to reduce the concentration of ECP both in serum and sputum (serum: MD −12.07, 95% CI −14.90 to −9.24; I2 = 0%; participants = 62; Analysis 1.16; sputum: MD −1.35, 95% CI −1.69 to −1.01; I2 = 0%; participants = 62; Analysis 1.17).
1.16. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 16: Eosinophil cationic protein (ECP) in serum
1.17. Analysis.

Comparison 1: Macrolide versus placebo, Outcome 17: ECP in sputum
Subgroup analysis
Subgroup analysis based on serological response or positivity to PCR for C pneumoniae was not possible due to the scarcity and heterogeneity of data and methods.
Sensitivity analysis
Primary or secondary outcomes with high heterogeneity (I2 greater than 30%) were taken into the consideration for conducting the sensitivity analysis with a random‐effects model. The outcomes with high heterogeneity that suggested a beneficial effect of macrolide in primary analyses such as severe exacerbations: exacerbations requiring ED visits/systemic steroids (Analysis 1.2 versus Analysis 2.1), symptom scales (Analysis 1.3 versus Analysis 2.2), asthma control (Analysis 1.4 versus Analysis 2.3), AQLQ (Analysis 1.5 versus Analysis 2.4), and FEV1 (Analysis 1.9 versus Analysis 2.5) became analyses in which the 95% CIs crossed the line of no effect by changing the model to random‐effects. The reason for the change in effect estimate is decreasing the weighting of large studies such as Gibson 2017 (Analysis 2.1; Analysis 2.3; Analysis 2.4) and Hahn 2012 (Analysis 2.2) by changing the model to random effects.
2.1. Analysis.

Comparison 2: Sensitivity analysis, Outcome 1: Severe exacerbations: exacerbations requiring emergency department visits/systemic steroids
2.2. Analysis.

Comparison 2: Sensitivity analysis, Outcome 2: Symptom scales
2.3. Analysis.

Comparison 2: Sensitivity analysis, Outcome 3: Asthma control
2.4. Analysis.

Comparison 2: Sensitivity analysis, Outcome 4: Asthma Quality of Life Questionnaire (AQLQ)
2.5. Analysis.

Comparison 2: Sensitivity analysis, Outcome 5: Forced expiratory volume in 1 second (FEV 1; L)
Discussion
Summary of main results
Twenty‐five studies, involving 1973 participants given macrolide or placebo, met the inclusion criteria. The certainty of the evidence was generally low due to incomplete reporting of study methodology and clinical data, indirectness of study populations, risk of bias, and imprecision caused by small numbers of participants and events. Most studies reported data from people with persistent or severe asthma, but inclusion criteria, interventions and outcomes were highly variable, and there may have been selective or incomplete reporting.
Macrolides led to a moderately sized but non‐significant improvement compared to placebo when this was defined as exacerbations requiring hospital admission (OR 0.47, 95% CI 0.20 to 1.12; I2 = 0%; studies = 2, participants = 529), but this was driven by one study and the 95% CIs did not exclude the possibility of no effect. Not considering the heterogeneity among the studies, macrolides appeared beneficial compared to placebo for severe exacerbations (defined as requiring ED visits or systemic steroids, or both) (RaR 0.65, 95% CI 0.53 to 0.80; I2 = 37%; studies = 4, participants = 640), improvement on symptom scales (SMD −0.46, 95% CI −0.81 to −0.11; I2 = 70%, studies = 4, participants = 136), rescue medication use (MD −0.43 puffs per day, 95% CI −0.81 to −0.04), ACQ (SMD −0.17, 95% CI −0.31 to −0.03) and AQLQ (MD 0.24, 95% CI 0.12 to 0.35), although the variation in ACQ and AQLQ did not reach the MCID (for both scores, MCID = 0.50) (Juniper 2005; Juniper 1994). The improvement in FEV1 (MD 0.04 L, 95% CI 0.03 to 0.08) was very small and of doubtful clinical relevance. There is no agreed MCID for FEV1 but this is below any likely MCID. The other outcomes such as lung function were of very low quality and did not show a benefit of macrolide treatment (morning PEF: MD 1.60 L/minute, 95% CI −10.35 to 13.56; evening PEF: MD 1.00 L/minute, 95% CI −13.65 to 15.65). Measures of bronchial hyperresponsiveness were too varied to pool, but most studies showed no clear benefit of macrolide over placebo. Two studies with people taking regular oral corticosteroids suggested macrolides may have a steroid‐sparing effect in this population. Macrolides were well tolerated with respect to severe adverse events (Peto OR 0.80, 95% CI 0.49 to 1.31; I2 = 41%; studies = 8, participants = 854), although less than half of the studies reported the outcome which was approaching 10% in each group. Reporting of specific adverse effects was too patchy across studies to be analysed meaningfully. Number of withdrawals from the study was near to equal in both macrolide and placebo groups (OR 1.06, 95% CI 0.76 to 1.48; I2 = 0%; studies = 10, participants = 984), and quite high in both group (almost 20%). Biomarkers of asthma activity such as sputum and serum ECP, sputum and serum eosinophils were lower in people treated with macrolides, but this was not associated with clinical benefits.
Overall completeness and applicability of evidence
The available data do not support any generalised use of macrolides in clinical practice to improve clinical outcomes in people with persistent asthma, but we cannot rule out the possibility of benefit due to several shortcomings in the available studies. The potential benefit of macrolides for the wide range of phenotypes and for clinically relevant groups (e.g. smokers) remains to be confirmed.
The available data from the 25 RCTs included in the present review are difficult to interpret for several reasons. First, four different types of macrolides were used across the studies (roxithromycin, clarithromycin, azithromycin and troleandomycin), often with differences in dosage and frequency of administration. Second, participants with different severities of asthma were included: the oldest studies included participants who were taking long‐term oral steroids (Kamada 1993; Nelson 1993), which could reflect a severe population or outdated prescribing practice. One study included people with aspirin‐intolerant asthma (Shoji 1999), one included people with intermittent allergic asthma (Amayasu 2000), and another exclusively recruited smokers with asthma (Cameron 2013); all the other studies enrolled people with mild‐to‐severe persistent asthma, and we could not properly assess the populations of six Chinese studies. Seven studies tested participants for C pneumoniae or M pneumoniae infection, but all with different techniques and very different results (Black 2001; Hahn 2006; Kraft 2002; Simpson 2008; Strunk 2008; Sutherland 2010; Wan 2016). The scarcity of data in the primary analyses precluded any meaningful subgroup analyses to assess the possible effect of these factors. Third and perhaps most importantly, the outcomes measured were heterogeneous; reporting of exacerbations and definitions for exacerbations and their severity varied across the studies; asthma symptoms were recorded using a variety of non‐validated scales as well as the ACQ and AQLQ, with a great variability across the studies. Lung function and bronchial hyperresponsiveness were often assessed and reported using different methodologies or parameters.
Two studies showing some effect on symptoms and markers of eosinophil inflammation were unusual both in the participants they recruited and in their design. Both were cross‐over studies, one recruited people with allergic intermittent asthma (Amayasu 2000), and the other enrolled people whose asthma was aspirin‐induced (Shoji 1999).
Only four studies investigated the role of macrolides in children with asthma (Kamada 1993; Piacentini 2007; Strunk 2008; Wan 2016); unfortunately the great variability in the interventions, measurements and outcomes makes any firm conclusion on the role of macrolides in children impossible. Kamada 1993 suggested a potential role for troleandomycin as steroid‐sparing agent, while Strunk 2008 seemed instead to exclude any role of macrolides used in this way.
Since the last version of this review, two RCTs were published (Gibson 2017; Wan 2016). Wan 2016 explored the effect of macrolides versus placebo on lung function and eosinophil inflammation (measured as exhaled nitric oxide, peripheral blood eosinophil count and ECP). Unfortunately, the quality of reporting of this study did not allow us to include its results in any meta‐analysis. Nevertheless, the fact that Wan 2016 included only 58 participants mitigates the impact of the exclusion of its results on the overall conclusions of this review. In contrast, Gibson 2017 was a very well‐designed and conducted study, with a large sample‐size of well‐selected participants, most of them on high‐dose ICS and long‐acting beta‐agonist (LABA)/long‐acting muscarinic antagonists (LAMA), falling in the category severe asthma of the current GINA 2021 guidelines. A number of biological drugs such as mepolizumab, reslizumab, benralizumab (Farne 2017) and dupilumab (Castro 2018; Rabe 2018) have entered the market since 2015 and, together with omalizumab (Normansell 2014), are routinely used in clinical practice; their use is now recommended in severe eosinophilic asthma (GINA 2021).
The results of Gibson 2017 and of a subgroup analysis from the same study (Gibson 2019) may indicate that macrolides could be an alternative to biological drugs for severe forms of asthma: that would be valuable especially in low‐income countries, although the potential risk of resistance development would remain a serious caveat to their wide use.
Despite all the limitations and considering the heterogeneity, our systematic review and meta‐analysis found no benefit of macrolides over placebo on lung function. As discussed, this does not rule out the possibility for significant benefit or harm of macrolides given the shortcomings of the evidence described above. The results of this review might change if further well‐designed and appropriately powered RCTs are conducted, but at present, the evidence is not promising enough to support further research for a general use of macrolides, while there is a suggestion that research targeted at specific phenotypes (i.e. severe or non‐eosinophilic (or both) asthma) may be warranted.
Overall, the use of macrolides for at least four continuous weeks of treatment proved safe, with similar rates of severe adverse events when macrolides were compared with placebo. There were no reported deaths. Unfortunately, this outcome was not consistently reported across the studies, and internationally approved scales such as the Common Terminology Criteria for Adverse Events were not used (CTCAE 2020). Therefore, the evidence for this outcome was low.
Antibiotic resistance is of increasing concern and only two included studies investigated this (Brusselle 2013; Gibson 2017). Brusselle 2013 reported that 87% of azithromycin‐treated participants were colonised with erythromycin‐resistant streptococci, a statistically significant increase from baseline and in comparison with the placebo group, while Gibson 2017 reported no significant change on the occurrence of resistant strains.
These results suggest that spread of resistant strain is a real concern, and any further research should clearly measure and report resistance as an outcome.
Alongside this, the case for macrolide therapy contributing to better outcomes in those testing positive for C pneumoniae or M pneumoniae infection was mostly unconvincing (Belotserkovskaya 2007; Black 2001; Kraft 2002; Strunk 2008; Sutherland 2010; Wan 2016). The number of participants testing positive was much lower than expected in several studies, and subgroup analyses were often underpowered or post hoc.
Quality of the evidence
The overall certainty of the evidence is low. We had serious concerns about selective or incomplete reporting, under‐reporting or variation of study results; there was uncertainty regarding allocation procedures and blinding of outcome assessment, and all but four trials recruited fewer than 100 people.
Few studies reported clinical data well enough to be included in a meta‐analysis. Some studies reported outcomes of interest but not in a format that allowed the data to be combined with other studies, and other studies focused on non‐clinical outcomes when the use of macrolides was being tested to assess their mechanism of action and effect on biomarkers. Most outcomes were also downgraded for indirectness because some studies focused on specific populations, such as smokers or people with asthma of a particular severity, which varied across studies. Inconsistencies in the scales used or description of outcomes also made it difficult to meta‐analyse the data and reduced our confidence in the conclusions that could be drawn. Risk of bias was also an issue across most of the analyses, largely due to uncertainty as a result of insufficient reporting of methodology, but also as a result of failure to prevent or account for high or unbalanced dropout.
Evidence for outcomes such as exacerbations requiring hospitalisation and serious adverse events was very imprecise due to the length of the studies and the rarity of this type of events, so it was difficult to reach meaningful conclusions for these outcomes. Several studies excluded people at higher risk of adverse events including prolonged corrected QT interval on electrocardiogram (Brusselle 2013; Cameron 2013; Gibson 2017; Hahn 2012; Sutherland 2010; Wan 2016), abnormal liver function tests (Black 2001; Cameron 2013; Hahn 2012; Sutherland 2010), and hearing impairment (Gibson 2017); the effect of excluding these potential participants is uncertain. For other outcomes such as symptoms, quality of life and FEV1, the reporting made it difficult for us to assess the amount of variation in scales, properties, time of measurement, etc., and this uncertainty made the data difficult to interpret.
Potential biases in the review process
We did not contact most trial authors to obtain unpublished data or to clarify methodology. Only two of the studies were conducted in the last five years, and 14 were conducted over 10 years ago. We judged that the time taken to contact all authors and the anticipated low response rate due to study age would delay the publication of this update.
We found six studies listed in an existing systematic review conducted in China that did not appear in our searches (Tong 2015). While we did not limit our searches by language, they did not cover studies that are indexed in non‐English language databases. Since the Tong 2015 systematic review was published in English, we were able to contact the authors and extract sufficient information to confirm the eligibility of these trials. However, we did not have the resources to personally extract data or assess for risk of bias in these studies, and the information we were able to include were kindly provided by the authors of that systematic review and not directly from the studies themselves. The review authors were able to answer the questions we had about the studies and their outcomes, but these studies could not be assessed as rigorously as the other 19 included studies and we could not be certain that all data relevant to this review were included.
The definitions of severe exacerbation, symptom scales and quality of life were not always consistent across studies. This required a significant post‐hoc assessment of which outcomes could be pooled.
For peak flow and blood eosinophils, some of these studies could not be pooled with the others because they used a different unit of analysis. In these cases, we reported the results alongside the meta‐analysis results narratively. The main benefit of including these studies is the completeness of the evidence base, and checking study lists of existing meta‐analyses is part of the standard search procedures for Cochrane Reviews. Subtle differences in the methods between our own review and that of Tong 2015 (e.g. the way data were extracted, application of trial eligibility criteria) may also have introduced a potential bias, meaning we cannot be sure that all studies relevant to our review were identified and analysed in the same way. We considered the overall benefit of inclusion to outweigh the potential biases in light of the help provided to us by Hon Fang and the other authors of that review (Fan 2015).
Agreements and disagreements with other studies or reviews
Four other meta‐analyses have evaluated the treatment of asthma with long‐term macrolides (Hiles 2019; Reiter 2013; Tong 2015; Wang 2019). There are noticeable differences across the systematic reviews and meta‐analyses in the conclusions drawn, and this is likely a reflection of the choice of outcomes and methods of analysis. In particular, we chose not to pool results where we were uncertain of scale or measurement similarity in order to make the results as clinically meaningful as possible. Furthermore, more subtle differences in the eligibility criteria and the way scores were aggregated are likely to have contributed to differences in the results and conclusions, such as using SMD or MD, fixed or random effects, change from baseline or endpoint scores, merging multiple relevant study arms, etc. These differences entail difficulties with meta‐analysing and interpreting the body of evidence, which is quite heterogeneous.
The analysis by Reiter 2013 included 12 RCTs with a minimum treatment duration of three weeks, and reported a positive effect of macrolides on symptoms scores, quality of life, peak flow and bronchial hyperresponsiveness. Tong 2015 included 18 studies, including the six Chinese studies that were not identified by our search, and it reported a positive effect on several measures of lung function (FEV1, PEF and forced vital capacity (FVC)) and airways hyperresponsiveness, but not on other measures of lung function (percentage predicted FEV1 and percentage predicted FVC), symptoms, or quality of life. Wang 2019 explored only studies conducted with azithromycin and for at least three weeks of duration. This systematic review and meta‐analysis included eight RCTs, reporting a small but statistically significant increase in FEV1, but no change in exacerbation rate, quality of life measures, PEF or fractional exhaled nitric oxide (FeNO) in the treatment group compared to placebo.
Hiles 2019 performed an individual participant data meta‐analysis of three studies comparing azithromycin (treatment duration of at least eight weeks) versus placebo. The studies had to include data on exacerbations for a follow‐up of at least six months. Exacerbations were defined as need for at least three days of oral corticosteroids or antibiotic course, or visit to the ED, or admission to hospital. Most of the participants included in this meta‐analysis had severe asthma (320/529 participants, 60.5%). The meta‐analysis showed a reduction of exacerbations in this population, and in people an eosinophilic or non‐eosinophilic phenotype. Azithromycin did not have beneficial effects for secondary outcomes such as quality of life, lung function or biomarkers.
Reiter 2013 and Tong 2015 did not formally assess exacerbations, either because they were not included as an outcome (Tong 2015) or because the data were considered insufficient to do so (Reiter 2013). Wang 2019 explored the exacerbation frequency among the studies they included, but they did not report which definition they used for their analysis. Therefore, the results were difficult to contextualise. The results of Hiles 2019 were limited to people with severe asthma, and seem to confirm the findings of our systematic review and meta‐analysis for this specific group of patients.
The lack of hospitalisation and exacerbation data is a major shortcoming of the evidence base, considering that reducing the frequency of these events is the main premise of long‐term macrolides treatment.
Authors' conclusions
Implications for practice.
Existing evidence suggests an effect of macrolides compared with placebo on the rate of exacerbations requiring hospitalisation. Macrolides probably reduce exacerbations requiring emergency department visit/treatment with systemic steroids and may reduce symptoms. Based on one well‐designed and powered randomised controlled trial, azithromycin may reduce exacerbation rate and improve symptom scales in people with severe asthma but overall we cannot rule out the possibility of other benefits or harms because the evidence is of low certainty due to heterogeneity among participants and interventions, imprecision and reporting biases (Gibson 2017).
Implications for research.
The review highlights the need for researchers to report clinically relevant outcomes accurately and completely using guideline definitions of exacerbations, validated symptoms and quality of life scales, as well as international scales for adverse effects. The review and meta‐analysis showed that macrolides can lead to a reduction of exacerbation rate and future trials could evaluate if this effect is sustained across all the severe asthma phenotypes and in comparison with newer biological drugs, whether effects persist or wane after treatment cessation, and are associated with infection biomarkers. Trials with prespecified subgroup analyses by asthma severity or phenotype would usefully contribute to the literature.
Feedback
Feedback concerning presentation of data, 16 April 2016
Summary
As primary author of two RCTs included in your recent review of macrolides for asthma, I would like to question the presentation of data from one of my studies (Hahn 2006) that I feel may affect the interpretation of review findings for two outcomes.
The symptom scale forest plot (Analysis 1.3) placed the central point for overall symptoms for our RCT on the “favors placebo” side whereas our results favored macrolide, as stated in our abstract and as illustrated in our Figure 2. It is possible the problem arose during the examination of Table 2 in which we described a symptom change score difference with a (+) result indicating improvement, as noted in our footnote. We also reported that the overall symptom score change favoring azithromycin was statistically significant (0.68, 95% CI 0.1 to 1.3).
The AQLQ forest plot (Analysis 1.5) likewise placed the central point for AQLQ change score for our RCT (2) on the “Favors placebo” side whereas our results favored macrolide, as stated in our abstract. In this case the sign of the positive result was not changed because a positive score already reflected improvement. The review accurately presented the midpoint data from our Table 2 but report different confidence intervals.
I advocate for Analyses 1.3 & 1.5 to be amended in the interest of correct data.
Highest regards for the work you do,
Dr. Hahn.
Reply
Dear Dr Hahn,
We are very grateful for your helpful feedback regarding the accuracy of data pertaining to your study (Hahn 2006).
Regarding Analysis 1.3, we agree data from your study have been misinterpreted, causing the effect to lie in the opposite direction. This has now been amended in the review to correctly represent your symptom scale data in the meta‐analysis, and in the interpretation of the results. There may be differences between the methods we have used and your own which make the data look slightly different. For example, we had to use a standardised mean difference analysis because the scales were not the same across studies, meaning your raw data were transformed and displayed as standard deviation units. Importantly, the pooled result for symptom scales now favours macrolide.
Regarding Analysis 1.5, while the effect for Hahn 2006 lies to the right of the line of no difference, this indicates ‘favours macrolide’ on the forest plot. As is standard practice for scales where higher scores indicate improvement, the labels of the plot were swapped to represent correctly the direction of effect. As above, the confidence intervals may differ slightly as a result of the method of analysis used. We used the mean change scores and standard deviations presented in Table 2 (0.59 (0.8) n = 19 azithromycin; 0.34 (1.0) n = 17 placebo), entered in a generic inverse variance (GIV) analysis in Review Manager 2014. We have not altered this analysis but hope this clarification satisfies you that these data have been interpreted correctly.
Many thanks again for the time and consideration taken to submit these comments.
Kayleigh Kew on behalf of the authors for the review.
Contributors
David L Hang, MD MS email: dlhahn@wic.edu, Affiliation: Wisconsin Research & Education Network (WREN)
What's new
| Date | Event | Description |
|---|---|---|
| 31 March 2021 | New search has been performed | New literature search run. |
| 31 March 2021 | New citation required but conclusions have not changed | Main conclusions not changed from the previous version. Based on a single, high‐quality RCT, there is a potential benefit of macrolides in the treatment of people with severe asthma. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 3, 2001
| Date | Event | Description |
|---|---|---|
| 5 November 2019 | New search has been performed | New literature search run |
| 13 May 2016 | Feedback has been incorporated | Hahn 2006 data corrected in Symptom scales analysis 1.3 after receiving feedback. New pooled result carried through text. Overall conclusions not affected. |
| 15 April 2015 | New search has been performed | New literature search run |
| 15 April 2015 | New citation required and conclusions have changed | Sixteen new RCTs have been included. No real advantage of the use of macrolides in patients with asthma was demonstrated. The review was redrafted for this update. We added a 'Summary of findings' table and used the current methodology recommended by Cochrane. We re‐extracted data from primary studies for the studies included in the previous version, including applying the new 'Risk of bias' tool. |
| 7 August 2008 | Amended | Converted to new review format. |
| 6 June 2005 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors express sincere thanks Hon Fang and the other authors of Tong 2015 for sharing information about the non‐English language studies from their systematic review and helping us incorporate them into our meta‐analyses. We would like to thank Dr Peter Gibson for providing additional data from his randomised controlled trial published in 2017 (Gibson 2017), which has been added to this version of the systematic review and meta‐analysis.
The authors and Cochrane Airways' Editorial Team are grateful to the following peer and consumer reviewers for their time and comments: Rama Lakshman (UK); David L Hahn (USA); Hugo Farne (UK) and Sarah Hiles (Australia).
We would like to thank Luca Richeldi who wrote the original protocol and conducted the 2005 version of this review as lead author. We also thank other authors of the 2005 version of this review: Leonardi Fabbri, Toby Lasserson and Peter Gibson.
Rebecca Normansell was the Editor for this review and commented critically on its development.
The Background and Methods sections of this updated review are based on a standard template used by Cochrane Airways.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health and Social Care.
Appendices
Appendix 1. Search methods up to April 2015
Trials were identified using the Cochrane Airways Group Specialised Register, which is derived from systematic searching of electronic databases including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase and CINAHL, and handsearching of respiratory journals and meeting abstracts. All records in the Specialised Register coded as 'asthma' were searched using the following terms:
macrolide* OR clarithromycin OR troleandomycin OR erythromycin OR josamycin OR azithromycin OR roxithromycin
Review articles and bibliographies identified from these primary papers were surveyed for additional citations and randomised controlled trials.
Appendix 2. Sources and search methods for the Cochrane Airways Trials Register
Electronic searches: core databases
| Database | Dates searched | Frequency of search |
| CENTRAL (via the Cochrane Register of Studies) | From inception | Monthly |
| MEDLINE (Ovid) | 1946 onwards | Weekly |
| Embase (Ovid) | 1974 onwards | Weekly |
| PsycINFO (Ovid) | 1967 onwards | Monthly |
| CINAHL (EBSCO) | 1937 onwards | Monthly |
| AMED (EBSCO) | From inception | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
Asthma search
1. exp Asthma/
2. asthma$.mp.
3. (antiasthma$ or anti‐asthma$).mp.
4. Respiratory Sounds/
5. wheez$.mp.
6. Bronchial Spasm/
7. bronchospas$.mp.
8. (bronch$ adj3 spasm$).mp.
9. bronchoconstrict$.mp.
10. exp Bronchoconstriction/
11. (bronch$ adj3 constrict$).mp.
12. Bronchial Hyperreactivity/
13. Respiratory Hypersensitivity/
14. ((bronchial$ or respiratory or airway$ or lung$) adj3 (hypersensitiv$ or hyperreactiv$ or allerg$ or insufficiency)).mp.
15. ((dust or mite$) adj3 (allerg$ or hypersensitiv$)).mp.
16. or/1‐15
Filter to identify randomised controlled trials
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter were adapted to identify trials in other electronic databases.
Appendix 3. Search strategies for the Cochrane Airways Trials Register, ClinicalTrials.gov, and the WHO ICTRP portal
Cochrane Airways Trials Register (via Cochrane Register of Studies)
#1 AST:MISC1
#2 MeSH DESCRIPTOR Asthma Explode All
#3 asthma*:ti,ab
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Macrolides Explode 1 2 3
#6 macrolide*
#7 azithromycin*
#8 clarithromycin*
#9 erythromycin*
#10 roxithromycin*
#11 spiramycin*
#12 telithromycin*
#13 troleandomycin*
#14 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13
#15 #4 and #14
[In search line #1, MISC1 denotes the field where the reference has been coded for condition, in this case, asthma]
ClinicalTrials.gov
Condition: asthma Study type: interventional Intervention: azithromycin OR clarithromycin OR erythromycin OR roxithromycin OR spiramycin OR telithromycin OR troleandomycin
World Health Organization International Clinical Trials Registry Platform
Condition: asthma Intervention: azithromycin OR clarithromycin OR erythromycin OR roxithromycin OR spiramycin OR telithromycin OR troleandomycin
Appendix 4. Narrative of individual study results
| Study ID | Detail of results |
| Amayasu 2000 |
|
| Belotserkovskaya 2007 |
|
| Black 2001 |
|
| Brusselle 2013 |
|
| Cameron 2013 |
|
| Gibson 2017 |
|
| Hahn 2006 |
|
| Hahn 2012 |
|
| Kamada 1993 |
|
| Kapoor 2010 |
|
| Kostadima 2004 |
|
| Kraft 2002 |
|
| Nelson 1993 |
|
| Piacentini 2007 |
|
| Shoji 1999 |
|
| Simpson 2008 |
|
| Strunk 2008 |
|
| Sutherland 2010 |
|
| Wan 2016 |
|
| ACQ: Asthma Control Questionnaire; ACT: Asthma Control Test; AQLQ: Asthma Quality of Life Questionnaire; BAL: bronchoalveolar lavage; CI: confidence interval; CT: computed tomography; DRS: dose–response slope; ECP: eosinophil cationic protein; ED: emergency department; ERS: European Respiratory Society; FEF25‐75: the average forced expiratory flow during the mid (25% to 75%) portion of the FVC; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; HR: hazard ratio; ICS: inhaled corticosteroid: IgG: immunoglobulin G; IL: interleukin; IQR: interquartile range; IRR: incidence rate ratio: LABA: long‐acting beta‐agonists; LAMA: long‐acting muscarinic antagonists; MMP: matrix metallopeptidase; mRNA: messenger ribonucleic acid; n: number of participants; NS: not significant; PCR: polymerase chain reaction; PEF: peak expiratory flow; PC20 or PD20: provocative concentration (or dose) causing a 20% fall in forced expiratory volume in 1 second (FEV1); SD: standard deviation; TNF‐alpha: tumour necrosis factor alpha. | |
Data and analyses
Comparison 1. Macrolide versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Exacerbation requiring hospitalisation | 2 | 529 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.20, 1.12] |
| 1.2 Severe exacerbations: exacerbations requiring emergency department visits/systemic steroids | 4 | 640 | Rate Ratio (IV, Fixed, 95% CI) | 0.65 [0.53, 0.80] |
| 1.3 Asthma symptom scales | 4 | 136 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.81, ‐0.11] |
| 1.4 Asthma control | 5 | 773 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.31, ‐0.03] |
| 1.5 Asthma Quality of Life Questionnaire (AQLQ) | 6 | 802 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.12, 0.35] |
| 1.6 Need for rescue medication puffs/day | 4 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐0.43 [‐0.81, ‐0.04] |
| 1.7 Morning PEF (L/minute) | 4 | 289 | Mean Difference (IV, Fixed, 95% CI) | 1.60 [‐10.35, 13.56] |
| 1.8 Evening PEF (L/minute) | 3 | 212 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐13.65, 15.65] |
| 1.9 Forced expiratory volume in 1 second (FEV 1; L) | 10 | 1046 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [0.00, 0.08] |
| 1.10 Bronchial hyperresponsiveness (BHR) | 9 | Other data | No numeric data | |
| 1.11 Oral corticosteroid dose | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12 Serious adverse events (including mortality) | 8 | 854 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.80 [0.49, 1.31] |
| 1.13 Withdrawal | 10 | 984 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.76, 1.48] |
| 1.14 Blood eosinophils | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐32.16 [‐34.77, ‐29.56] |
| 1.15 Sputum eosinophils | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.16 Eosinophil cationic protein (ECP) in serum | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐12.07 [‐14.90, ‐9.24] |
| 1.17 ECP in sputum | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐1.35 [‐1.69, ‐1.01] |
Comparison 2. Sensitivity analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Severe exacerbations: exacerbations requiring emergency department visits/systemic steroids | 4 | 640 | Rate Ratio (IV, Random, 95% CI) | 0.72 [0.48, 1.08] |
| 2.2 Symptom scales | 4 | 156 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.27, 0.11] |
| 2.3 Asthma control | 5 | 773 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.33, 0.06] |
| 2.4 Asthma Quality of Life Questionnaire (AQLQ) | 6 | 802 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.06, 0.36] |
| 2.5 Forced expiratory volume in 1 second (FEV 1; L) | 10 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.01, 0.15] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amayasu 2000.
| Study characteristics | ||
| Methods |
Design: randomised controlled, double‐blind, cross‐over study Statistical analysis: Student's paired T‐test Duration: 8 weeks per treatment with 4‐week washout Conducted in Yokohama, Japan, and Boston, USA |
|
| Participants |
Population: 17 participants randomised to 2 treatment sequences (clarithromycin‐placebo and placebo‐clarithromycin) Baseline characteristics: reported for population as a whole, since the study was a cross‐over design % male: 52.9 Mean age, years: 38.5 % on maintenance ICS: 0 % on maintenance LABA/ICS: 0 Mean % predicted FEV1: 76.2 Mean daily ICS dose, µg: 0 Chlamydophila infection: not reported Inclusion criteria: non‐smokers, aspirin tolerant, with mild or moderate asthma diagnosed according to the criteria of the ATS. All were in stable condition and had been free of symptoms for respiratory infections for ≥ 6 weeks. Exclusion criteria: people using oral or ICSs, theophylline, any anti‐leukotriene drug, any other anti‐inflammatory agents or clarithromycin |
|
| Interventions |
Run‐in: wash‐out period ≥ 4 weeks between cross‐over Intervention: clarithromycin 200 mg twice per day Control: matching placebo |
|
| Outcomes | Blood eosinophils, blood neutrophils, serum ECP, sputum eosinophils, sputum neutrophils, sputum ECP, symptom score, FVC, FEV1, methacholine challenge | |
| Notes |
Funding: Aoki International Co, Ltd Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, no details. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo of identical appearance used; described as double‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of dropouts. |
| Selective reporting (reporting bias) | Unclear risk | Reported outcomes could be used in analysis, but unclear if others were missing (protocol registration not reported). |
| Other bias | Low risk | None noted. |
Belotserkovskaya 2007.
| Study characteristics | ||
| Methods |
Design: parallel randomised trial (blinding and type of control unclear) Duration: 8 weeks Location unclear |
|
| Participants |
Population: 51 adults with chronic stable asthma randomised to azithromycin (n = 28) or 'control' (n = 23) Baseline characteristics: none reported Inclusion criteria: adults with chronic stable asthma. No other details Exclusion criteria: not described |
|
| Interventions |
Run‐in: 24‐week open‐label period before randomisation Intervention: azithromycin (dose not reported) Control: 'control' not described |
|
| Outcomes | FEV1 and PEF (not suitable for analysis) | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only, no information. |
| Allocation concealment (selection bias) | Unclear risk | Abstract only, no information. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of withdrawals not given. |
| Selective reporting (reporting bias) | High risk | No full text found; minimal information about methodology and no analysable results. |
| Other bias | Low risk | None noted. |
Black 2001.
| Study characteristics | ||
| Methods |
Design: parallel randomised, double‐blind, placebo‐controlled, multicentre, multinational study Duration: 6 weeks' treatment with 24 weeks' follow‐up Conducted in Australia, New Zealand, Italy and Argentina |
|
| Participants |
Population: 219 participants with asthma randomised to roxithromycin (n = 105) or placebo (n = 114) Baseline characteristics % male: roxithromycin, 44.8; placebo, 50.0 Mean age, years: roxithromycin, 40 (SD 11.6); placebo, 42 (SD 11.9) % on maintenance ICS: roxithromycin, 77.1; placebo, 84.2 % on maintenance LABA/ICS: not reported Mean % predicted FEV1: roxithromycin, 79.0 (SD 19.3); placebo, 75.3 (SD 17.4) Mean daily ICS dose, µg: not reported Chlamydophila infection: reported according to serological tests Inclusion criteria: aged 18–60 years, physician diagnosis of asthma, FEV1 ≥ 50% of predicted and either > 15% increase in FEV1 following inhaled salbutamol or a > 15% diurnal variation in PEF on 7 of 14 days during the run‐in period. Participants also needed to have IgG titres to C pneumonia > 1:64,or IgA titres > 1:16, and a daytime symptom score ≥ 2 or night‐time symptom score ≥ 1, on 7 of the 14 days of the run‐in period Exclusion criteria: treatment with any macrolide, quinolone or tetracycline in the 4 weeks before study entry or over > 3 weeks in the preceding 4 months; other medicines that were not permitted were ergot alkaloids, terfenadine and astemizole; smoking history > 20 pack‐years; bronchiectasis; any other serious systemic diseases; hypersensitivity to macrolides or any significant change in asthma medication in previous month, including a course of OCS; respiratory tract infection during run‐in or if they had abnormal liver function tests or serum creatinine > 200 μmol/L |
|
| Interventions |
Run‐in: 2 weeks Intervention: roxithromycin 150 mg twice per day Control: matching placebo Treatments for asthma other than OCSs were permitted if the dose had not changed in the previous month. |
|
| Outcomes | Symptoms, PEF, FEV1, reliever medication | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as double‐blind, with matching placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis. This did not include 12 people who withdrew from the study within a few days of randomisation, without recording any diary card data, or a 13th person who was withdrawn because of nausea and vomiting and did not record any diary card data after the first 10 days of treatment. Did not state from which groups but represented < 6% of overall population. |
| Selective reporting (reporting bias) | High risk | Outcomes were poorly reported. FEV1, PEF morning and evening, symptoms and quality of life all reported without variance. |
| Other bias | Low risk | None noted. |
Brusselle 2013.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled, multicentre study Duration: 26 weeks Locations not described in detail; appears to be mostly conducted Belgium |
|
| Participants |
Population: 109 participants randomised to azithromycin (n = 55) or placebo (n = 54) Baseline characteristics % male: azithromycin, 47; placebo, 30 Median age, years: azithromycin, 53; placebo, 53 % on maintenance ICS: not reported % on maintenance LABA/ICS: azithromycin, 100; placebo, 100 Mean % predicted FEV1: azithromycin, 80.1 (SD 21.9); placebo, 84.8 (SD 20.7) Mean daily ICS dose, µg: azithromycin, 2000; placebo, 2000 Chlamydophila infection: not reported Inclusion criteria: aged 18–75 years; diagnosis of persistent asthma; history consistent with GINA step 4 or 5 clinical features; received high doses of ICS (≥ 1000 mg fluticasone or equivalent) plus inhaled LABA for ≥ 6 months prior to screening and had ≥ 2 independent severe asthma exacerbations requiring systemic corticosteroids, LRTI requiring antibiotics or both within the previous 12 months; never smokers or ex‐smokers with a smoking history ≤ 10 pack‐years; FeNO level below ULN Exclusion criteria: prolonged corrected QT interval, severe bronchiectasis, significant medical conditions or significant laboratory abnormalities that might interfere with the study conduct or patient's safety, pregnancy or breastfeeding, prohibited concomitant medication including anti‐IgE treatment and treatment with macrolide antibiotics within the last 3 months |
|
| Interventions |
Run‐in: 2 weeks Intervention: azithromycin 250 mg per day for 5 days and then 1 capsule 3 times per week Control: matching placebo All participants received high‐dose combination therapy of ICS and LABA for ≥ 6 months prior to study entry and continued this treatment throughout study |
|
| Outcomes | ACQ, AQLQ, rescue medication use, FEV1, morning and evening PEF, adverse events, withdrawals Severe asthma exacerbations defined as deterioration in asthma leading to ≥ 1 of: hospitalisation, ED visit or need for systemic corticosteroids for ≥ 3 days during the 26‐week treatment phase |
|
| Notes |
Funding: academic trial, no industry funding. Agency for Innovation by Science and Technology Study ID(s): NCT00760838 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned in a 1:1 ratio to receive add‐on treatment with azithromycin or placebo using a central web‐based randomisation tool. |
| Allocation concealment (selection bias) | Low risk | Web‐based randomisation and the concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind design (presumably participants and investigators). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout in both groups, but higher in placebo (3.6% with azithromycin vs 9.3% with placebo). ITT analysis used. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the prospectively registered protocol were well reported. |
| Other bias | Low risk | None noted. |
Cameron 2013.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 12 weeks Conducted at 2 hospitals in the UK |
|
| Participants |
Population: 77 participants were randomised to azithromycin (n = 39) or placebo (n = 38) Baseline characteristics % male: azithromycin, 51.3; placebo, 44.7 Mean age, years: azithromycin, 46.4 (SD 8.8); placebo, 42.8 (SD 9.4) % on maintenance ICS: azithromycin, 89.7; placebo, 81.6 % on maintenance LABA/ICS: azithromycin, 38.5; placebo, 47.4 Mean % predicted FEV1: 78.3 (prebronchodilator) Mean daily ICS dose, µg: azithromycin, 603 (SD 457); placebo, 709 (SD 564) Chlamydophila infection: not reported Inclusion criteria: aged 18–70 years, current smokers (≥ 5 pack‐years history) with chronic asthma (> 1 year' duration); free of exacerbations and respiratory tract infections for ≥ 6 weeks; able to maintain asthma without exacerbations during run‐in period and able to wean off other asthma medication Exclusion criteria: ex‐smokers or never smokers; planning to quit smoking during duration of trial; unstable asthma; current epilepsy, psychosis or history of significant atrial or ventricular tachyarrhythmia; corrected QT interval > 450 ms in women or 430 ms in men; low potassium levels (if this can be corrected, screening can continue with confirmation of normal levels prior to taking study medication); liver disease (levels for ALT, AST or both ≥ 2 times ULN); significant renal disease (creatinine or urea levels ≥ 2 times ULN); any previous severe adverse reactions to macrolides; known to have specific IgE sensitivity or skin test positivity to grass pollen and a history of worsening of asthma due to hay fever will not be recruited from mid‐May to the end of July; URTI or LRTI in the 4 weeks prior to randomisation (run‐in period can be prolonged in this situation to have 4 weeks with no respiratory infection prior to randomisation); require medications known to interact with azithromycin; on other immunosuppressants or chronic antibiotics; weight < 45 kg; frequent asthma exacerbations (> 4) requiring OCS in the year prior to randomisation; current or past diagnosis of allergic‐bronchopulmonary‐aspergillosis; pregnancy and breastfeeding; mental impairment or language difficulties that makes informed consent impossible |
|
| Interventions |
Run‐in: 4 weeks (on ICS equivalent to beclomethasone 400 µg ± a LABA) Intervention: azithromycin 250 mg per day Control: matching placebo |
|
| Outcomes | Change in ACQ, AQLQ, LCQ, diary symptom score, change in morning PEF, airways responsiveness methacholine PC20, differential cell counts, colony counts, antibody status, FeNO, exacerbation rates | |
| Notes |
Funding: Medical Research Council UK and supported financially by NHS Research Scotland (NRS), through the Scottish Primary Care Research Network. Study medication (budesonide Easyhalers; Orion Pharma, Newbury, UK) was purchased with an educational grant from AstraZeneca (London, UK). Study ID(s): NCT00852579 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but no details of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Masking: double‐blind (participant, carer, investigator, outcomes assessor). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Masking: double‐blind (participant, carer, investigator, outcomes assessor). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6 participants dropped out, but details not mentioned. |
| Selective reporting (reporting bias) | High risk | Exacerbations were not reported in either of the published reports. Other outcomes were well reported at each of the stated time points. |
| Other bias | Low risk | None noted. |
Gibson 2017.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 48 weeks Conducted at 8 centres in Australia |
|
| Participants |
Population: 420 participants were randomised to azithromycin (n = 213) or placebo (n = 207) Baseline characteristics % male: azithromycin, 37; placebo, 42 Mean age, years: azithromycin, 61.0; placebo, 60.0 % on maintenance ICS: azithromycin, 100; placebo, 99.5 % on maintenance LABA/ICS: azithromycin, 98; placebo, 99 Mean % predicted FEV1: azithromycin, 72.3; placebo, 73.6 Mean daily ICS dose, µg: not reported, but reported > 85% of participants were on beclomethasone dipropionate ≥ 800 μg equivalent in both groups Chlamydophila infection: not reported Inclusion criteria: asthma defined as a compatible history and documented objective evidence of variable airflow obstruction from bronchodilator response (with postbronchodilator reversibility of ≥ 12% and FEV1 > 200 mL, airway hyperresponsiveness, or increased peak flow variability (> 12% of amplitude above the lowest PEF over ≥ 1 week of monitoring); currently symptomatic with at least partial loss of asthma control (ACQ6 ≥ 0.75) despite treatment with maintenance ICSs or long‐acting bronchodilators; clinically stable with no recent exacerbations, infections or changes in maintenance medication for ≥ 4 weeks before study entry; non‐smokers confirmed by exhaled carbon monoxide < 10 ppm Exclusion criteria: substantial parenchymal lung disease, such as emphysema; ex‐smokers with > 10 pack‐years of smoking if their diffusing capacity for carbon monoxide (gas transfer corrected for effective alveolar volume) was < 70% of the predicted value; hearing impairment; abnormally prolonged QTc interval |
|
| Interventions |
Run‐in: 2 weeks after screening visit Intervention: azithromycin 500 mg 3 times per week Control: matching placebo |
|
| Outcomes | Total number of asthma exacerbations (severe and moderate) over 48 weeks (Severe exacerbations defined as need of hospitalisation or ED visit or need for ≥ 3 systemic steroids or increase of a stable oral steroids dose. Moderate exacerbation defined as increase of inhaled steroids or oral antibiotics without systemic steroids, or increased beta‐agonists or ED visit without hospitalisation and without systemic steroids) Change in AQLQ and ACQ6, lung function, adverse events, antibiotic courses for respiratory infection, induced sputum cell counts |
|
| Notes |
Funding: Australian Government's National Health and Medical Research Council (NHMRC) and John Hunter Charitable Trust; no commercial input into any aspect of the trial. Study ID(s): ANZCTR 12609000197235 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation from a computer‐generated random numbers table with permuted blocks of 4 or 6 and stratification for centre and past smoking. |
| Allocation concealment (selection bias) | Low risk | Study packs were labelled with the allocated randomisation number and bottle numbers. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All investigators, study research staff and participants' treating doctors were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Researchers and treating physicians blinded to the treatment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | ITT analysis included participants with no follow‐up data as no change. |
| Selective reporting (reporting bias) | Unclear risk | Exacerbations were grouped (e.g. severe exacerbations = ED + short course steroids + hospitalisation) and separate data were not available. Severe exacerbations were analysed as number per participant‐year but were available as events in an associated abstract. |
| Other bias | Low risk | None noted. |
Hahn 2006.
| Study characteristics | ||
| Methods |
Design: community‐based, parallel multisite, double‐blind, randomised, placebo‐controlled trial Duration: 6 weeks of treatment; outcomes measured at 3 months Conducted in community‐based healthcare settings located in 4 US states and 1 Canadian province |
|
| Participants |
Population: 45 participants randomised to azithromycin (n = 24) or placebo (n = 21) Baseline characteristics % male: azithromycin, 33; placebo, 67 Mean age, years: azithromycin, 50 (SD 14); placebo, 45 (SD 12) % on maintenance ICS: azithromycin, 83; placebo, 76 % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: azithromycin, 33%; placebo, 52% Inclusion criteria: aged ≥ 18 years with diagnosis of current asthma that was persistent, stable and present for > 3 months prior to enrolment, stability assessed during 2–3 week run‐in period, during which eligible patients remained in the same severity class (mild, moderate or severe) and had no acute exacerbations; documented objective evidence for reversible airway obstruction, either spontaneously or after treatment, was also required prior to randomisation, either FEV1 change 12% (and > 200 mL) or PEF change 25% (and > 60 L/minute) Exclusion criteria: ingestion of any macrolide, tetracycline or quinolone in the 6 weeks before randomisation; macrolide allergy; any unstable illness or other cause for symptoms; use of coumadin, anticonvulsants or digoxin; and pregnancy or lactation Note: asthma defined as variable symptoms of wheeze, chest tightness, cough or shortness of breath triggered by a variety of stimuli |
|
| Interventions |
Run‐in: 2‐ to 3‐week run‐in period, during which eligible patients remained in the same severity class (mild, moderate or severe) and had no acute exacerbations Intervention: azithromycin, 1 × 600 mg tablet daily for 3 days, followed by 600 mg weekly for an additional 5 weeks Control: matching placebo All participants continued to receive usual care for asthma from their primary physician, who was blinded to treatment allocation |
|
| Outcomes | Symptoms, adverse events, withdrawals | |
| Notes |
Funding: Pfizer Study ID(s): NCT00245908 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | At randomisation, participants meeting final eligibility criteria were allocated to study medication bottles that were coded centrally using a computerised 1:1 allocation ratio blocked by site. Block size was 6. An independent statistician, who had no further contact with study conduct, generated the randomisation sequences. |
| Allocation concealment (selection bias) | Low risk | Study physicians, research staff, participants and data analysts were unaware of allocation due to central randomisation and coding. Emergency unblinding envelopes were available, but study sites did not report opening any of them. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinded (participant, physician, data collector, data analyst). Bulk study medication tablets were bottled, labelled and distributed by an independent pharmaceutical service that had no further role in study conduct. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded (participant, physician, data collector, data analyst). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Used ITT principle. Did not impute values for missing data. Approximate 20% dropout in both groups unaccounted for. |
| Selective reporting (reporting bias) | Low risk | Prospectively registered pilot study. Specified outcomes were reported. |
| Other bias | Low risk | None noted. |
Hahn 2012.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, placebo‐controlled, double‐blind trial Duration: 12 weeks of treatment with 1 year off‐treatment follow‐up Conducted in the USA. Study clinician members, staff of 5 PBRNs and 1 community‐based allergist enrolled patients from their practices |
|
| Participants |
Population: 75 participants randomised to azithromycin (n = 38) or placebo (n = 37) Baseline characteristics % male: azithromycin, 29; placebo, 35 Mean age, years: azithromycin, 45.7 (SD 15.5); placebo, 47.4 (SD 14.2) % on maintenance ICS: azithromycin, 63; placebo, 81 % on maintenance LABA/ICS: azithromycin, 37; placebo, 70 Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: adults aged ≥ 18 years with physician‐diagnosed asthma (symptomatic > 2 days per week, > 2 nights a month, in exacerbation, or a combination of these characteristics); objective evidence for reversible airway obstruction (> 12% and > 200 mL change in FEV1, a 25% and 60 L/min change in PEF or both) either spontaneously or after treatment; asthma for ≥ 6 months before enrolment. Exclusion criteria: not English literate or had no email address or Internet access; macrolide allergy; pregnant or lactating; 4 weeks of continuous use of macrolides, tetracyclines or quinolones within 6 months of randomisation; asthma symptoms < 6 months' duration; unstable asthma requiring immediate emergency care; comorbidities likely to interfere with study assessments or follow‐up (e.g. cystic fibrosis, obstructive sleep apnoea requiring CPAP, cardiomyopathy, congestive heart failure, terminal cancer, alcoholism or other substance addiction, or any other serious medical condition that, in the opinion of the study physician, would seriously interfere with or preclude assessment of study outcomes or completion of study assessments); medical conditions for which macrolide administration may possibly be hazardous (e.g. acute or chronic hepatitis, cirrhosis or other liver disease; chronic kidney disease; history of prolonged cardiac repolarisation and QT interval or torsades de pointes); specified medications for which close monitoring has been recommended in the setting of macrolide administration (digoxin, theophylline, warfarin, ergotamine or dihydroergotamine, triazolam, carbamazepine, ciclosporin, hexobarbital, or phenytoin) |
|
| Interventions |
Run‐in: unclear Intervention: azithromycin 600 mg, 1 tablet per day for 3 days followed by 1 tablet per week for 11 weeks Control: matching placebo |
|
| Outcomes | Symptoms, ACQ, changes in asthma medications, withdrawals, quality of life, exacerbations Exacerbations recorded separately for those requiring a steroid burst, an unscheduled or emergency visit or a hospitalisation for asthma |
|
| Notes |
Funding: Pfizer, Inc., donated identical matching azithromycin and placebo. The Wisconsin Academy of Family Physicians; the American Academy of Family Physicians Foundation, under the auspices of the Joint Grant Awards Program; the Dean Foundation for Health Research and Education; and private donors provided financial support for direct costs of AZMATICS trial. Study ID(s): NCT00266851 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent statistician prepared the randomisation codes used for participant assignment to the azithromycin or placebo study arms. |
| Allocation concealment (selection bias) | Low risk | The investigators, participants and study site personnel were blinded to treatment allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Each study site received coded study medication bottles (1:1 allocation) in blocks of 6 and was instructed to distribute them (numbered 1–6) in numerical ascending order to eligible consenting study participants. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The investigators, participants, and study site personnel were blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All ITT analyses, and no participants with available data were excluded from any analysis. Withdrawal was high and quite uneven between groups (42% with azithromycin and 30% with placebo ). |
| Selective reporting (reporting bias) | Low risk | Prospectively registered outcomes reported fully. |
| Other bias | Unclear risk | More participants in the placebo group were taking regular ICS or ICS/LABA combination. |
He 2009.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 12 weeks Conducted in China |
|
| Participants |
Population: 40 participants were randomised to azithromycin (n = 20) or placebo (n = 20) Baseline characteristics % male: not reported Mean age, years: azithromycin, 35 (SD 7.3); placebo, 34 (SD 5.6) % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported |
|
| Interventions |
Run‐in: unknown Intervention: azithromycin 250 mg twice weekly Control: placebo |
|
| Outcomes | FEV1, FEV1/FVC, symptoms | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain, suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was unavailable. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study, although a placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Tong 2015 noted that withdrawals and dropouts were not adequately described in the study. |
| Selective reporting (reporting bias) | Unclear risk | Information was unavailable. |
| Other bias | Unclear risk | Information was unavailable. |
Kamada 1993.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 12 weeks Conducted in Denver, USA |
|
| Participants |
Population: 19 participants randomised to troleandomycin + methylprednisolone (n = 6), troleandomycin + prednisone (n = 8) or placebo + methylprednisolone (n = 5) Baseline characteristics % male: troleandomycin + methylprednisolone, 16.7; troleandomycin + prednisone, 100; placebo + methylprednisolone, 60 Mean age, years: troleandomycin + methylprednisolone, 14.3 (SD 2.9); troleandomycin + prednisone, 11.9 (SD 2.6); placebo + methylprednisolone, 11.3 (SD 2.7) % on maintenance ICS: troleandomycin + methylprednisolone, 100; troleandomycin + prednisone, 100; placebo + methylprednisolone, 100 % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: aged 6–17 years meeting ATS criteria for reversible obstructive airways disease, requiring prednisone in doses of ≥ 20 mg every other day, using inhaled bronchodilators ≥ 4 times per day, taking theophylline with daytime peak serum concentrations > 10 µg/mL, and having previously failed treatment with or were receiving cromolyn sodium at the time of screening Exclusion criteria: pregnant, smoker, viral upper respiratory infection within 4 weeks of enrolment |
|
| Interventions |
Run‐in: single‐blind run‐in period of ≥ 1 week Intervention 1: troleandomycin 250 µg + methylprednisolone once daily Intervention 2: troleandomycin 250 µg + prednisolone once daily (data not used in this review) Control: placebo + methylprednisolone once daily All participants required OCS, given as part of the randomised treatment. The mean daily dose was 34.2 mg in intervention group 1, 21.3 mg in intervention group 2 and 23.5 mg in control group |
|
| Outcomes | Symptoms score, methacholine PD20, glucocorticoid dose reduction, FEV1, PEF | |
| Notes |
Funding: FDA grant FD‐R 000278 Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stratified on 2 levels of severity of asthma. Methods unclear. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All participants received identically appearing study medications in the form of 2 blue capsules, which contained either prednisolone or methylprednisolone, and 1 white capsule, which contained either troleandomycin or placebo, daily. Described as double‐blind. Investigators who were not blinded to data tapered doses as tolerated by participants on the recommendations of investigators who were blinded to data. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear who measured outcomes and whether they were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 participants dropped out of the troleandomycin‐prednisone group, 1 of whom could not be included in the final analysis (representing 14% dropout due to small randomisation numbers). |
| Selective reporting (reporting bias) | High risk | Several measures were only reported graphically and could not be analysed. |
| Other bias | High risk | Baseline characteristics were unbalanced due to the very small numbers per group. |
Kapoor 2010.
| Study characteristics | ||
| Methods |
Design: cross‐over, randomised, double‐blind, placebo‐controlled trial Duration: 6 weeks per treatment with 3‐week washout Conducted in India |
|
| Participants |
Population: 40 participants randomised to the 2 treatment sequences (roxithromycin‐placebo and placebo‐roxithromycin) Baseline characteristics: none reported Inclusion criteria: stable, mild‐to‐moderate asthma Exclusion criteria: not described |
|
| Interventions |
Run‐in: not described Intervention: roxithromycin 150 mg once daily Control: matching placebo |
|
| Outcomes | ACT, spirometric indices, impulse oscillometry parameters | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as double‐blind, no other details. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | High risk | Only abstract available, no published report. Minimal details of study characteristics, participants or outcomes. |
| Other bias | Unclear risk | Impossible to assess. |
Kostadima 2004.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 8 weeks Conducted in Greece |
|
| Participants |
Population: 75 participants randomised to clarithromycin twice daily (n = 25), 3 times daily (n = 25) or placebo (n = 25) Baseline characteristics % male: clarithromycin twice daily, 72.7; clarithromycin 3 times daily, 40; placebo, 28.6 Mean age, years: clarithromycin twice daily, 48 (SD 16); clarithromycin 3 times daily, 42 (SD 12); placebo, 41 (SD 16) % on maintenance ICS: clarithromycin twice daily, 100; clarithromycin 3 times daily, 100; placebo, 100 % on maintenance LABA/ICS: not reported Mean % predicted FEV1: clarithromycin twice daily, 85 (SD 14); clarithromycin 3 times daily, 85 (SD 13); placebo, 86 (SD 14) Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: aged 18–70 years; established diagnosis of bronchial asthma for 1 year; treatment with budesonide 400 mg twice daily and salbutamol 200 mg taken as needed less than twice weekly for ≥ 1 month prior to recruitment; PD20 < 2 mg Exclusion criteria: history of allergic rhinitis or occupational asthma; history of smoking (past or current); treatment with systemic corticosteroids or history of URTI over the 4 weeks prior to participation in the trial; FEV1 < 50% of the predicted value or < 1 L at baseline; URTI or asthma exacerbation during the study period; history of systemic diseases (i.e. myocardial infarction or stroke in previous 3 months, uncontrolled hypertension, known aortic aneurysm, epilepsy requiring drug treatment or peptic ulcer disease); treatment with beta‐blockers; pregnancy or lactation |
|
| Interventions |
Run‐in: not described Intervention 1: clarithromycin 250 mg twice daily Intervention 2: clarithromycin 250 mg 3 times daily Control: matching placebo dextrose During the study, participants continued their treatment with budesonide and salbutamol. No other medication was allowed. We grouped the results for clarithromycin 250 mg twice daily and clarithromycin 250 mg 3 times daily and compared them with placebo. |
|
| Outcomes | Methacholine PD20 | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No specific details. |
| Allocation concealment (selection bias) | Unclear risk | Randomised to 1 of the study groups by a research nurse who played no further role in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and investigators were blinded with regard to the type of treatment received. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear who measured outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants who dropped out were not represented in the analysis; varied across groups from 12% to 20%. |
| Selective reporting (reporting bias) | Unclear risk | Several key outcomes were not reported; report did not give details of a study protocol to check that all planned outcomes were reported. |
| Other bias | Unclear risk | % male was unbalanced across groups, but other measures were well balanced (included age and baseline lung function). |
Kraft 2002.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 6 weeks Conducted in Denver, USA |
|
| Participants |
Population: 55 participants randomised to clarithromycin (n = 26) or placebo (n = 26); 3 withdrew due to scheduling conflicts (n = 1) and non‐compliance (n = 2) (treatment groups unknown) Baseline characteristics: reported for the population as a whole, not for each group % male: 49.1 Mean age, years: 33.4 (SD 8.9) % on maintenance ICS: 32.7 % on maintenance LABA/ICS: 100 Mean % predicted FEV1: 69.3 (SD 15.6) Mean daily ICS dose, µg: not reported Chlamydophila infection: 56.4% had evidence of C pneumoniae or M pneumoniae infection Inclusion criteria: fulfilled criteria for asthma, exhibited a provocative concentration of methacholine causing a 20% decline in FEV1 < 8 mg/mL, and reversibility of lung function by ≥ 12% with bronchodilator Exclusion criteria: inpatient status; URTI or LRTI within previous 3 months; use of macrolides, tetracyclines or quinolones within previous 3 months; smoking history > 5 pack‐years or any cigarettes within the previous 2 years; and significant non‐asthma pulmonary disease or other medical problems |
|
| Interventions |
Run‐in: not described Intervention: clarithromycin 500 mg twice daily Control: matching placebo |
|
| Outcomes | Lung function, cytokine in situ production | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind randomisation to treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind randomisation to treatment. The individual who performed the analysis was blinded to participants' Mycoplasma/Chlamydophila status, and those counting were blinded to treatment status. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants (treatment groups unknown) underwent analysis for Mycoplasma and Chlamydophila but were excluded from the treatment analysis due to scheduling difficulties (n = 1) and non‐compliance (n = 2). |
| Selective reporting (reporting bias) | Unclear risk | Mostly non‐clinical outcomes. No preregistered protocol mentioned to cross‐check. |
| Other bias | Low risk | None noted. |
Nelson 1993.
| Study characteristics | ||
| Methods |
Design: prospective, parallel, randomised, double‐blind, placebo‐controlled trial Duration: 1–2 years (variable) Conducted in Denver, USA |
|
| Participants |
Population: 75 participants randomised to troleandomycin + methylprednisolone (n = 37) or placebo + methylprednisolone (n = 38) Baseline characteristics % male: troleandomycin + methylprednisolone, 36.7; placebo + methylprednisolone, 29.6 Age range, years: troleandomycin + methylprednisolone, 21–75; placebo + methylprednisolone, 22–62 % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: diagnosis of asthma with demonstrated fluctuation in the FEV1 ≥ 15% of the predicted value occurring either spontaneously or as a result of therapy. They were required to have received a minimum of prednisone 15 mg per day or an equivalent dose of another corticosteroid over the preceding 3 months with history that lower doses resulted in deterioration of asthma control and pulmonary function. They were also required to be unable to achieve alternate‐day corticosteroid therapy, be receiving theophylline, if tolerated, with a peak serum value of > 10 µg/mL and inhaled β‐adrenergic bronchodilator therapy ≥ 4 times daily. People using inhaled sodium cromolyn or ICS were required to discontinue these medications before enrolment. Women of child‐bearing age were required to have a negative pregnancy test and agree to avoid pregnancy during the duration of possible troleandomycin therapy Exclusion criteria: receiving anticonvulsant therapy, had significant hepatic disease, current smokers |
|
| Interventions |
Run‐in: before entry, each participant's medication was optimally adjusted and often had received a transient increase in corticosteroid dose. Therefore, each participant's asthma was under good control when they were randomised, and steroids were tapered only in a way consistent with maintenance of continued good control Intervention: troleandomycin 250 µg once daily + methylprednisolone Control: matching placebo + methylprednisolone All participants required OCS, which were given as part of the randomised treatment. Mean daily doses were 30.8 mg for the intervention group and 32.0 mg for the control group. |
|
| Outcomes | Symptoms score, corticosteroid dose, blood eosinophil count, IgG, fasting blood sugar, methacholine PD20 | |
| Notes |
Funding: grant from the Clinical Investigation Committee, National Jewish Centre for Immunology and Respiratory Medicine Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised; no details. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind (presumably participants and personnel/investigators). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear who performed the evaluations. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout higher in placebo group; data not accounted for. |
| Selective reporting (reporting bias) | Unclear risk | Most outcome data were reported; study predated requirement to register a protocol. |
| Other bias | Low risk | None noted. |
Piacentini 2007.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 8 weeks Conducted at the residential house of the Istituto Pio XII for asthma in Italy |
|
| Participants |
Population: 16 participants randomised to azithromycin (n = 8) or placebo (n = 8) Baseline characteristics % male: azithromycin, 75; placebo, 75 Mean age, years: azithromycin, 13.9 (SD 2.4); placebo, 12.9 (SD 2.4) % on maintenance ICS: azithromycin, 100; placebo, 100 % on maintenance LABA/ICS: not reported Mean % predicted FEV1: azithromycin, 73.5; placebo, 84.3 Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: children with asthma (age not specified) according to ATS criteria Exclusion criteria: not described in detail |
|
| Interventions |
Run‐in: not stated Intervention: azithromycin once per day for 3 consecutive days every week, at 10 mg/kg bodyweight Control: matching placebo All participants continued their long‐term treatment for asthma with low‐dose ICS: either fluticasone 100–200 μg/day, or beclomethasone dipropionate 200–400 μg/day. Oral steroids were not allowed in the 3 months preceding enrolment. |
|
| Outcomes | Lung function, bronchial hyperresponsiveness expressed as the DRS of FEV1 fall after hypertonic saline inhalation and induced sputum | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Active or placebo treatment randomly attributed using a computer‐generated randomisation code. |
| Allocation concealment (selection bias) | Unclear risk | No details. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Active treatment and placebo were stored in identical bottles, and nursing staff not involved in any part of the study administered the drug to the children. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Active treatment and placebo were stored in identical bottles, and nursing staff not involved in any part of the study administered the drug to the children. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of dropout. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration number reported; could not check if outcomes were missing. |
| Other bias | Low risk | None noted. |
Shoji 1999.
| Study characteristics | ||
| Methods |
Design: cross‐over, randomised, double‐blind, placebo‐controlled trial Statistical analysis: Student's paired T‐test Duration: 8 weeks per treatment with 4‐week washout Conducted at 1 centre in Japan |
|
| Participants |
Population: 14 participants randomised to the 2 treatment sequences (roxithromycin‐placebo and placebo‐roxithromycin) Baseline characteristics: presented for the whole population due to the cross‐over design % male: 42.9 Mean age, years: 39.6 % on maintenance ICS: 0 % on maintenance LABA/ICS: 0 Mean % predicted FEV1: 75 Mean daily ICS dose, µg: 0 Chlamydophila infection: not reported Inclusion criteria: adults with clinical histories of aspirin‐intolerant asthma; positive sulpyrine or lysine aspirin provocation test; non‐smokers diagnosed with mild or moderate asthma according to ATS criteria. The participants were in a stable condition and had been free of symptoms of respiratory infection for at least 6 weeks. Exclusion criteria: people using OCS or ICSs, theophylline, any anti‐leukotriene drug, such as pranlukast, or any other anti‐allergic agents as well as roxithromycin |
|
| Interventions |
Run‐in: washout period ≥ 4 weeks Intervention: roxithromycin 150 mg twice daily Control: matching placebo |
|
| Outcomes | Blood eosinophils, blood neutrophils, serum ECP, sputum eosinophils, sputum neutrophils, sputum ECP, symptom score, FVC, FEV1, methacholine challenge | |
| Notes |
Funding: grants‐in‐aid from Aoki International Co Ltd for Dr T Shoji Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no details. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind (presumably participants and personnel); matching placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear who performed the assessments and whether they were blind. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details of dropout. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes were well reported. No details of trial registration to cross‐check. |
| Other bias | Low risk | None noted. |
Simpson 2008.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 8 weeks Participants recruited from the Ambulatory Care Service of the Department of Respiratory and Sleep Medicine at the John Hunter Hospital, New Lambton, Australia |
|
| Participants |
Population: 45 participants randomised to clarithromycin (n = 23) or placebo (n = 22) Baseline characteristics % male: clarithromycin, 43.5; placebo, 54.5 Mean age, years: clarithromycin, 60; placebo, 55 % on maintenance ICS: not reported % on maintenance LABA/ICS: clarithromycin, 83; placebo, 82 Mean % predicted FEV1: clarithromycin, 73.6 (SD 15.8); placebo, 67.6 (SD 18.8) Mean daily ICS dose, µg: clarithromycin, 2000; placebo, 2000 Chlamydophila infection: not reported Inclusion criteria: non‐smoking adults with symptomatic refractory asthma according to GINA. Antihistamine therapies were ceased for the duration of the study Exclusion criteria: smoked > 5 pack‐years or if they had any known sensitivity to macrolide antibiotics |
|
| Interventions |
Run‐in: mentioned but not described Intervention: clarithromycin 500 mg twice daily Control: matching placebo During the study, participants continued with their baseline medications as prescribed by their physician. |
|
| Outcomes | Sputum IL‐8 concentration, sputum neutrophil numbers and concentrations of neutrophil elastase and matrix metalloprotein‐9, lung function, airway hyperresponsiveness to hypertonic saline, asthma control, quality of life, symptoms | |
| Notes |
Funding: not stated Study ID(s): ACTR12605000318684 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐numbers table was computer generated for treatment allocation using permuted blocks of 4. Randomisation was stratified according to those with high (≥ 61%) and low neutrophil proportions at screening. Treatment was assigned randomly for each group separately to ensure equal numbers of participants with high neutrophil proportions in each of the 2 treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | A blinded staff member, who took no further part in the study, performed randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo and active medication were packaged identically by the hospital pharmacy department, which dispensed treatments according to the random‐numbers table. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts reported in the study. |
| Selective reporting (reporting bias) | High risk | Data reported in the paper could not be meta‐analysed (median, IQR). |
| Other bias | Low risk | None noted. |
Strunk 2008.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled multicentre trial Duration: 30 weeks, depending on asthma control Recruited from 5 CARE Network centres in the USA |
|
| Participants |
Population: 55 participants randomised to azithromycin (n = 17), placebo (n = 19), or montelukast (n = 19; not relevant to this review) Baseline characteristics: presented for the whole population % male: 58.2 Mean age, years: 11.2 (SD 2.6) % on maintenance ICS: not reported % on maintenance LABA/ICS: 100 Mean % predicted FEV1: 101.9 (SD 13.7) Mean daily ICS dose, µg: 60% were taking budesonide 800 µg per day at randomisation Chlamydophila infection: nasal washes were obtained at randomisation, at week 18 and at end of trial (either after the last planned visit or at time of treatment failure) Inclusion criteria: aged 6–17 years, and demonstration of moderate‐to‐severe persistent asthma; prebronchodilator values of FEV1 ≥ 80% predicted for consideration of step‐down at enrolment, or ≥ 50% predicted if inadequately controlled and step‐up planned; children demonstrated ability to perform reproducible spirometry and had airway lability demonstrated either by an improvement in FEV1 ≥ 12% after 4 puffs of albuterol or airway hyperresponsiveness, reflected by ≥ 20% fall in FEV1 after a methacholine dose of ≤ 12.5 mg/mL Exclusion criteria: very severe asthma, as indicated by > 3 hospitalisations in the preceding 12 months, history of intubation or mechanical ventilation within the last year, or any history of hypoxic seizure due to asthma; history of severe sinusitis requiring sinus surgery within the past 12 months; use of maintenance oral or systemic antibiotics for treatment of an ongoing condition; contraindication for use of azithromycin or montelukast; presence of lung disease other than asthma; use of digoxin, ergotamine or dihydroergotamine, triazolam, carbamazepine, ciclosporin, hexobarbital, phenytoin and other macrolides |
|
| Interventions |
Run‐in: budesonide‐stable period of 6 weeks (with salmeterol 50 µg). During the run‐in, participants demonstrated evidence of inadequate control on ICS + salmeterol, with subsequent documentation that step‐up to a higher dose of ICS (to a maximum of 1600 µg daily, with salmeterol) established control. Participants were excluded if they were unable to use the study drug delivery systems or to adhere to ≥ 80% of days with use of salmeterol Diskus and oral capsules and of diary card completion during the run‐in (prerandomisation) period. Intervention: azithromycin 250 mg (25–40 kg bodyweight) or 500 mg (> 40 kg bodyweight) once daily + placebo montelukast tablet Control: 1 or 2 placebo capsules once daily plus 1 placebo tablet The treatment arms were stratified according to clinical centre and dose of budesonide (800 µg/day vs 1600 µg/day) that achieved asthma control during run‐in. Participants were provided with albuterol MDI (Ventolin, GSK), prednisone (10 mg tablets) and a written asthma action plan. |
|
| Outcomes | Exacerbations requiring OCSs, PEF, nocturnal awakenings, rescue medication use | |
| Notes |
Funding: not stated Study ID(s): not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stratified according to clinical centre and dose of budesonide (800 µg/day vs 1600 µg/day) that achieved asthma control during run‐in. Sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Double‐blind. After the lowest dose was achieved and control maintained for an additional 6 weeks, the active study medication was changed to placebo (blinded to participant). Investigators appear not to be blind after this stage. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Double‐blind. After the lowest dose was achieved and control maintained for an additional 6 weeks, the active study medication was changed to placebo (blinded to participant). Investigators appear not to be blind after this stage. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout in active and placebo groups. |
| Selective reporting (reporting bias) | High risk | Registration number not reported. Outcomes could not be included in meta‐analysis, and several were reported for the population as a whole so groups could not be compared. |
| Other bias | Low risk | None noted. |
Sutherland 2010.
| Study characteristics | ||
| Methods |
Design: parallel, randomised, double‐blind, placebo‐controlled trial Duration: 16 weeks Recruited from 10 hospitals and medical centres in the USA |
|
| Participants |
Population: 92 participants randomised to clarithromycin (n = 47) or placebo (n = 45) Baseline characteristics % male: clarithromycin, 42.6; placebo, 44.4 Mean age, years: clarithromycin, 41.3 (SD 12.5); placebo, 37.5 (SD 10.5) % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: 76.0 (whole population) Mean daily ICS dose, µg: not reported Chlamydophila infection: 6 participants in each group were PCR positive for M pneumoniae or C pneumoniae Inclusion criteria: history of physician‐diagnosed asthma; methacholine PC20 ≤ 16 mg/mL, FEV1 improvement ≥ 12% in response to albuterol 180 µg, or both; stable asthma for ≥ 6 weeks prior to study entry; FEV1 ≥ 60% of predicted result following albuterol 180 µg; Juniper ACQ score ≥ 1.5 (optimal ACQ score cut‐off point for asthma that is 'not well controlled' by NIH/GINA guidelines); non‐smoker (less than 10 pack‐per‐year lifetime smoking history and no smoking in the year prior to study entry); able to perform spirometry, as per ATS criteria; 75% adherence with diary cards, fluticasone (monitored with Doser), and placebo tablet trial (monitored electronically with electronic Drug Exposure Monitor (eDEM) tablet dose counter) for the final 2 weeks of the 4‐week run‐in period; at visit 1, in steroid‐naive participants, no significant adrenal suppression, defined as a plasma cortisol concentration < 5 µg/dL (if adrenal suppression occurs, ACTH 250 µg stimulation test was performed. Plasma cortisol levels were collected at baseline, and 30 and 60 minutes after the ACTH stimulation test. Participants must have had a cortisol concentration > 20 µg/dL on ≥ 1 of the post‐ACTH time points); absence of bronchoscopy‐induced exacerbation (if bronchoscopy‐induced exacerbation had occurred, prednisone therapy must have stopped ≥ 6 weeks prior to study entry); absence of respiratory tract infection (if infection had occurred, infection‐related symptoms must have stopped ≥ 6 weeks prior to study entry); had experienced ≤ 2 exacerbations or respiratory tract infections prior to study entry; if female and able to conceive, willing to utilise 2 medically acceptable forms of contraception (1 non‐barrier method with single barrier method or a double barrier method) Exclusion criteria: presence of lung disease other than asthma; presence of vocal cord dysfunction, due to potential confounding of ACQ score; significant medical illness other than asthma; history of atrial or ventricular tachyarrhythmia; use of any medication that has a significant interaction with clarithromycin, including herbal or alternative therapies; asthma exacerbation within 6 weeks of the screening visit or during the run‐in period prior to bronchoscopy; use of systemic steroids or change in dose of controller therapy within 6 weeks of the screening visit; inability, in the opinion of the study investigator, to co‐ordinate use of dry powder or MDI or to comply with medication regimens; inability or unwillingness to perform required study procedures; prolonged heart rate corrected QT interval (> 450 ms in women and > 430 ms in men) on ECG at study entry; low potassium or magnesium levels (based on local Asthma Clinical Research Network laboratory definitions); abnormal elevation of liver function tests (AST, ALT, total bilirubin or alkaline phosphatase); abnormal prothrombin time or partial thromboplastin time results; reduced creatinine clearance; contraindication to bronchoscopy, as determined by medical history or physical examination; regular consumption of grapefruit or grapefruit juice; pregnant or breastfeeding |
|
| Interventions |
Run‐in: 4‐week run‐in period, in which participants were treated with CFC‐fluticasone propionate MDI 88 µg inhaled regularly twice daily, and inhaled CFC‐albuterol sulphate 180 µg as needed every 4–6 hours for relief of acute symptoms. If, at the end of the 4‐week run‐in, participants demonstrated an ACQ score ≥ 1.25, they were eligible to proceed to fibreoptic bronchoscopy for the purposes of endobronchial biopsy for characterisation of lower airway PCR status for M pneumoniae or C pneumoniae. Intervention: clarithromycin 500 mg twice daily + fluticasone propionate 88 µg twice daily (Flovent HFA 44 µg 2 puffs twice daily) Control: placebo + fluticasone propionate 88 µg twice daily (Flovent HFA 44 µg 2 puffs twice daily) |
|
| Outcomes | ACQ total score and MCID for treatment response, rescue albuterol use, morning and evening PEF, FEV1, PC20, change in exacerbation number and frequency PC20 and change in FeNO | |
| Notes |
Funding: Milton S Hershey Medical Center with collaboration from the National Heart, Lung, and Blood Institute (NHLBI) Study ID(s): NCT00318708 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Based on the results of PCR testing, participants were stratified into 2 groups, either PCR positive or PCR negative for both M pneumoniae and C pneumoniae. Within these 2 strata, participants were randomly allocated in a 1:1 distribution to the addition of either clarithromycin, 500 mg capsule by mouth twice daily, or matched placebo. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both participants and study personnel were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind (participant, carer, investigator, outcomes assessor) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All analyses invoked the ITT paradigm, with truncation at the time of exacerbation or treatment failure in relevant analyses. Dropout was 17% in clarithromycin group and 11% in placebo group, and the primary outcome reported on ClinicalTrials.gov does not appear to have imputed for missing participants. |
| Selective reporting (reporting bias) | High risk | Only group contrasts available for some outcomes in the published paper, and only the primary outcome and adverse events were uploaded to ClinicalTrials.gov. |
| Other bias | Low risk | None noted. |
Wan 2016.
| Study characteristics | ||
| Methods |
Design: randomised, placebo‐controlled trial (assumed parallel assignment; unconfirmed) Duration: 4 weeks Conducted in Taipei |
|
| Participants |
Population: 58 children randomised to clarithromycin (n = 36) or placebo (n = 22) Baseline characteristics % male: clarithromycin, 66.6; placebo, 50 Mean age, years: clarithromycin, 10.1 (SD 3.1); placebo, 10.2 (SD 3.1) % on maintenance ICS: 100% according to protocol % on maintenance LABA/ICS: 0 in both groups Mean % predicted FEV1: clarithromycin, 79.4; placebo, 80.1 Mean daily ICS dose, µg: budesonide dipropionate 200 Chlamydophila infection: clarithromycin, 58% IgG, 41.7% IgM; placebo, 65% IgG, 35% IgM Inclusion criteria: persistent asthma according to GINA guidelines; positivity to ≥ 2 common inhaled allergens; consent given by parents Exclusion criteria: < 2 antigens; no consent obtained; congenital long QT‐syndrome or prolonged QT |
|
| Interventions |
Run‐in: 1‐week washout systemic steroids and montelukast Intervention: clarithromycin orally 5 mg/kg daily for 4 weeks Control: placebo matching orally for 4 weekly |
|
| Outcomes | Childhood ACT, FEV1%, forced expiratory flow at 25–75% of the pulmonary volume, FeNO, total IgE, absolute eosinophil count, ECP | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Sealed envelope for allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported, but placebo used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reported 2 withdrawals in the control group, but rate of completion of investigations not reported. |
| Selective reporting (reporting bias) | Unclear risk | Childhood ACT not reported at end of study. Rate of completion of investigations not reported. |
| Other bias | Low risk | None noted. |
Wang 2012.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 8 weeks Conducted in China |
|
| Participants |
Population: 45 participants randomised to clarithromycin (n = 23) or placebo (n = 22) Baseline characteristics % male: not reported Mean age: not reported % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported. |
|
| Interventions |
Run‐in: unknown Intervention: clarithromycin 500 mg twice daily Control: placebo |
|
| Outcomes | Trough FEV1, cell counts, symptoms | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain, suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were reported but not in detail. A placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Tong 2015 noted that withdrawals and dropouts were not adequately described in the study. |
| Selective reporting (reporting bias) | Unclear risk | Information was not available. |
| Other bias | Unclear risk | Information was not available. |
Wang 2014.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 52 weeks Conducted in China |
|
| Participants |
Population: 58 participants randomised to azithromycin (n = 29) or placebo (n = 29) Baseline characteristics % male: not reported Mean age, years: azithromycin, 28.4 (SD 16.0); placebo, 29.6 (SD 14.2) % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported |
|
| Interventions |
Run‐in: unknown Intervention: azithromycin 250 mg twice weekly Control: placebo |
|
| Outcomes | FEV1, PEF | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain, suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study, although a placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Tong 2015 noted that withdrawals and dropouts were not adequately described in the study. |
| Selective reporting (reporting bias) | Unclear risk | Information was not available. |
| Other bias | Unclear risk | Information was not available. |
Xiao 2013.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 12 weeks Conducted in China |
|
| Participants |
Population: 210 participants randomised to roxithromycin (n = 106) or placebo (n = 104) Baseline characteristics % male: not reported Mean age, years: roxithromycin, 34.5 (SD 7.2); placebo, 33.7 (SD 8.3) % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported |
|
| Interventions |
Run‐in: unknown Intervention: roxithromycin 150 mg twice daily Control: placebo |
|
| Outcomes | FEV1, FVC, PEF | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain, suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study, although a placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was not available. |
| Selective reporting (reporting bias) | Unclear risk | Information was not available. |
| Other bias | Unclear risk | Information was not available. |
Yan 2008.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 4 weeks Conducted in China |
|
| Participants |
Population: 40 participants randomised to roxithromycin (n = 20) or placebo (n = 20) Baseline characteristics % male: not reported Mean age: not reported % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported |
|
| Interventions |
Run‐in: unknown Intervention: roxithromycin 150 mg twice daily Control: placebo |
|
| Outcomes | Trough FEV1, FEV1, PEF, cell counts, symptoms | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study, although a placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Tong 2015 noted that there was a detailed report of withdrawals and dropouts in the study, but we were unable to assess the level of dropout and how this might have affected the results. |
| Selective reporting (reporting bias) | Unclear risk | Information was not available. |
| Other bias | Unclear risk | Information was not available. |
Zhang 2013.
| Study characteristics | ||
| Methods |
Design: randomised controlled trial (assumed parallel assignment; unconfirmed) Duration: 60 days (8.7 weeks) Conducted in China |
|
| Participants |
Population: 60 participants randomised to azithromycin (n = 30) or placebo (n = 30) Baseline characteristics % male: not reported Mean age: not reported % on maintenance ICS: not reported % on maintenance LABA/ICS: not reported Mean % predicted FEV1: not reported Mean daily ICS dose, µg: not reported Chlamydophila infection: not reported Inclusion criteria: we were unable to detail the specific inclusion and exclusion criteria for this trial because it was included from an existing systematic review (Tong 2015). The inclusion criteria of the review required that the study be designed to evaluate the "efficacy of prolonged treatment with macrolide antibiotics in adult patients with asthma". Exclusion criteria: not reported |
|
| Interventions |
Run‐in: unknown Intervention: azithromycin 100 mg once daily Control: placebo |
|
| Outcomes | Trough FEV1 | |
| Notes |
Funding: unknown Study ID(s): unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tong 2015 awarded 2 points for this domain, suggesting well‐reported and acceptable methods of random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Information was not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study, although a placebo control was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tong 2015 noted that methods of blinding were not adequately described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Tong 2015 noted that withdrawals and dropouts were not adequately described in the study. |
| Selective reporting (reporting bias) | Unclear risk | Information was not available. |
| Other bias | Unclear risk | Information was not available. |
ACQ: Asthma Control Questionnaire; ACT: Asthma Control Test; ACTH; adrenocorticotropic hormone; ALT: alanine aminotransferase; AQLQ: Asthma Quality of Life Questionnaire; AST: aspartate aminotransferase;ATS: American Thoracic Society; CFC: chlorofluorocarbon; CPAP: continuous positive airway pressure; DRS: dose–response slope; ECG: electrocardiography;ECP: eosinophil cationic protein; ED: emergency department; FDA: Food and Drug Administration (USA); FeNO: fractional exhaled nitric oxide; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; GINA: Global Initiative for Asthma;ICS: inhaled corticosteroid;IgA: immunoglobulin A; IgE: immunoglobulin E; IgG: immunoglobulin G; IL‐8: interleukin‐8; IQR: interquartile range; ITT: intention‐to‐treat; LABA: long‐acting beta2‐agonist; LCQ: Leicester Cough Questionnaire; LRTI: lower respiratory tract infection; n: number of participants; NIH: National Institutes of Health (USA) MCID: minimal clinically important difference; MDI: metred dose inhaler; OCS: oral corticosteroid; PC20 or PD20: provocative concentration (or dose) causing a 20% fall in forced expiratory volume in 1 second (FEV1); Log PC20: logarithm to the base 10 of PC20; PCR: polymerase chain reaction; PEF: peak expiratory flow; PBRN: practice‐based research network; QT interval: measure of the time between the start of the Q wave and the end of the T wave in the heart's electrical cycle; SD: standard deviation; ULN: upper limit normal; URTI: upper respiratory tract infection.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andrade 1983 | Study period too short (6 days) and randomisation method not adequate. |
| Anon 2009 | Commentary. Not an RCT. |
| Bacharier 2015 | Participants not affected by asthma. |
| Baigelman 2015 | Participants not affected by asthma. |
| Ball 1990 | Study period too short (2 weeks). |
| Cogo 1994 | Study of inadequate duration. |
| D'Azevedo Silveira 2016 | Participants not affected by asthma. |
| Ebling 1984 | Basic science study. |
| Feldman 1997 | Basic science in vitro study. |
| Gong 2016 | Missing a control group without macrolides. Classification of the participants unclear. |
| Gotfried 2004 | Study was suspended because the slow enrolment of participants. The clarithromycin and placebo groups were unequal in size, and the final analysis was performed only within the treatment group, analysing data before and after the macrolide therapy within the same participants. Therefore, the study was excluded because there were no between‐study comparisons. |
| Hodgson 2016 | Participants affected by chronic cough, not asthma. |
| Hueston 1991 | Participants not affected by asthma. |
| Itkin 1970 | Treatment duration < 4 weeks. |
| Johnston 2016 | Treatment duration < 4 weeks. |
| Kaplan 1958 | Not an RCT. |
| Koh 1997 | Participants were children with bronchiectasis; 7 children had asthma and insufficient data were reported for these children separately. |
| Koutsoubari 2012 | Acute exacerbations in children, trial < 4 weeks. |
| Lee 1998 | Study on the pharmacokinetics of theophylline during macrolides administration. |
| Mandhane 2017 | Treatment duration < 4 weeks. |
| Oldach 2015 | Target condition not asthma. |
| Ram 2016 | Target condition not asthma. Intervention not a macrolide. |
| Spector 1974 | Not an RCT. |
| Stokholm 2016 | Treatment duration < 4 weeks. |
| Szefler 1980 | Not an RCT. |
| Szefler 1982a | Not an RCT. |
| Szefler 1982b | Not an RCT. |
| Takamura 2001 | Not an RCT. |
| Wald 1986 | Not an RCT. |
| Weinberger 1977 | Not an RCT. |
| Zeiger 1980 | Not an RCT. |
RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
NCT02517099.
| Study name | Preschool Wheeze: Inflammation/Infection Guided Management (PrIGMa) |
| Methods | Randomised controlled trial |
| Participants | Children aged 1–5 years |
| Interventions | Regular inhaled steroids (beclometasone dipropionate 200 μg twice for 4 months) or antibiotic therapy (co‐amoxiclav 0.3 mL/kg twice daily or azithromycin 10 mg/kg once daily for 4 weeks). |
| Outcomes | Number of unscheduled healthcare visits at 4 months Health‐related quality of life at 4 months and up to 1 year later Number of hospital admissions at 4 months and up to 1 year later Number of days of oral steroids at 4 months and up to 1 year later |
| Starting date | 5 June 2015 |
| Contact information | Imperial College London, UK |
| Notes |
Differences between protocol and review
We updated the review to conform with current methodology and reporting. We used GRADE to assess the certainty of the evidence for the primary outcomes, and modified the summary of findings table to the current standard format. We explained methods for data synthesis in more detail. There are no major changes in methodology in this updated version of the review.
Contributions of authors
KU: data extraction, entry and analysis, interpretation, drafting of the review.
LG: entry and data analysis, interpretation, revision of the review.
KK: data extraction, entry and analysis.
GF: data extraction, entry, interpretation, drafting of the review.
Contributions of editorial team
Rebecca Fortescue (Co‐ordinating Editor) edited the protocol; advised on methodology; approved the protocol prior to publication.
Christian Osadnik (Contact Editor): edited the review; advised on methodology, interpretation and content.
Emma Dennett (Managing Editor): co‐ordinated the editorial process; advised on interpretation and content; edited the review.
Emma Jackson (Assistant Managing Editor): conducted peer review and edited the references and other sections of the protocol and review.
Elizabeth Stovold (Information Specialist): designed the search strategy; ran the searches; edited the search methods section.
Sources of support
Internal sources
-
All, Other
The authors declare that no funding was received for this systematic review.
External sources
-
All, Other
The authors declare that no funding was received for this systematic review.
Declarations of interest
KU: none.
LG: I was the statistical Editor at Cochrane Airways Group and checked the data and then joined the team after providing extensive help.
KK: I was a paid researcher on a National Institute for Health Research (NIHR) Cochrane Programme Grant until December 2016, during which time I contributed to the first version of this review. The grant was awarded to the Cochrane Airways review group at St George's, University of London, where I continued as an honorary research assistant until April 2017. I am currently an employee of the Cochrane Central Executive Team and my contribution to the update for this review is not subject to any funding.
GF: I received fees for lectures (AstraZeneca) and advisory boards/lectures (Boehringer Ingelheim and Roche) for topics not related to and outside the work of this systematic review and meta‐analysis.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Amayasu 2000 {published data only}
- Amayasu H, Yashida S, Ebana S, Yamamoto Y, Nishikawa T, Shoji T, et al. Clarithromycin suppress bronchial hyperresponsiveness associated with eosinophilic inflammation in patients with asthma. Annals of Allergy, Asthma and Immunology 2000;84(6):594-8. [DOI] [PubMed] [Google Scholar]
Belotserkovskaya 2007 {published and unpublished data}
- Belotserkovskaya Y, Sinopalnikov A. Open-trial randomized comparative trial of the efficacy of the azithromycin in the 8 week treatment of mild to moderate asthma. European Respiratory Journal 2007;30(Suppl 51):358s. [Google Scholar]
Black 2001 {published data only}
- Black P, Jenkins CR, Scicchitano R, Blasi F, Allegra L, Mills G, et al. Randomised, controlled trial of roxithromycin for the treatment of asthma in subjects with serological evidence of infection with Chlamydia pneumoniae. American Journal of Respiratory and Critical Care Medicine 2001;164(4):536-41. [DOI] [PubMed] [Google Scholar]
Brusselle 2013 {published and unpublished data}
- Brusselle GG, Vanderstichele C, Jordens P, Deman R, Slabbynck H, Ringoet V, et al. Azithromycin for prevention of exacerbations in severe asthma (AZISAST): a multicentre randomised double-blind placebo-controlled trial. Thorax 2013;68(4):322-9. [DOI] [PubMed] [Google Scholar]
Cameron 2013 {published data only}
- Cameron EJ, Chaudhuri R, Mair F, McSharry C, Greenlaw N, Weir CJ, et al. Randomised controlled trial of azithromycin in smokers with asthma. European Respiratory Journal 2013;42(5):1412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibson 2017 {published and unpublished data}
- ACTRN12609000197235. The AMAZES study: Asthma and macrolides: the Azithromycin Efficacy and Safety Study [A large-scale, multicentre, double-blind, placebo controlled randomised trial to compare the efficacy (and safety) of the addition of oral low dose azithromycin for 48 weeks with fixed dose maintenance therapy on the incidence of asthma exacerbations and clinical asthma status in people with persistent asthma]. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=ACTRN12609000197235 (first received 20 April 2009).
- Gibson PG, Yang IA, Upham JW, Reynolds PN, Hidge S, James AL, et al. Azithromycin reduces exacerbations in adults with persistent symptomatic eosinophilic asthma. American Journal of Respiratory and Critical Care Medicine 2017;195:A4679. [Google Scholar]
- Gibson PG, Yang IA, Upham PN, Hodge S, James AL, Jenkins C, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial. Lancet 2017;390(10095):659-68. [DOI] [PubMed] [Google Scholar]
Hahn 2006 {published and unpublished data}
- Hahn DL, Plane MB, Mahdi OS, Byrne GI. Secondary outcomes of a pilot randomized trial of azithromycin treatment for asthma. PLoS Clinical Trials 2006;1(2):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hahn 2012 {published and unpublished data}
- Hahn D, Grasmick M, Hetzel S. Pragmatic controlled trial of azithromycin for asthma in adults. European Respiratory Journal 2011;38:322s. [Google Scholar]
- Hahn DL, Grasmick M, Hetzel S, Yale S. Azithromycin for bronchial asthma in adults: an effectiveness trial. Journal of the American Board of Family Medicine 2012;25(4):442-59. [DOI] [PubMed] [Google Scholar]
He 2009 {published data only}
- He J, Zhu N, Chen XD. Clinical impacts of azithromycin on lung function and cytokines for asthmatic patients. Fudan University Journal of Medical Science 2009;36(6):719-22. [Google Scholar]
Kamada 1993 {published data only}
- Kamada AK, Hill MR, Iklé DN, Brenner AM, Szefler SJ. Efficacy and safety of low-dose troleandomycin therapy in children with severe, steroid-requiring asthma. Journal of Allergy and Clinical Immunology 1993;91(4):873-82. [DOI] [PubMed] [Google Scholar]
Kapoor 2010 {published and unpublished data}
- Kapoor S, Brashier B, Udupa A, Pawar R, Kodgule R, Limaye S, et al. Therapeutic effect of low dose roxithromycin in chronic stable mild-to-moderate asthma. European Respiratory Journal 2010;36(suppl 54):P1176. [Google Scholar]
Kostadima 2004 {published data only}
- Kostadima E, Tsiodras S, Alexopoulos EI, Kaditis AG, Mavrou I, Georgatou N, et al. Clarithromycin reduces the severity of bronchial hyperresponsiveness in patients with asthma. European Respiratory Journal 2004;23(5):714-7. [DOI] [PubMed] [Google Scholar]
Kraft 2002 {published data only}
- Kraft M, Cassell GH, Pak J, Martin RJ. Mycoplasma pneumoniae and Chlamydia pneumoniae in asthma: effect of clarithromycin. Chest 2002;121(6):1782-8. [DOI] [PubMed] [Google Scholar]
Nelson 1993 {published data only}
- Nelson HS, Hamilos DL, Corsello PR, Levesque NV, Buchmeier AD, Bucker BL. A double-blind study of troleandomycin and methylprednisolone in asthmatic subjects who require daily corticosteroids. American Review of Respiratory Disease 1993;147(2):398-404. [DOI] [PubMed] [Google Scholar]
Piacentini 2007 {published and unpublished data}
- Piacentini GL, Peroni DG, Bodini A, Pigozzi R, Costella S, Loiacono A, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy and Asthma Proceedings 2007;28(2):194-8. [DOI] [PubMed] [Google Scholar]
Shoji 1999 {published data only}
- Shoji T, Yoshida S, Sakamoto H, Hasegawa H, Nakagawa H, Amayasu H. Anti-inflammatory effect of roxithromycin in patients with aspirin-intolerant asthma. Clinical and Experimental Allergy 1999;29(7):950-6. [DOI] [PubMed] [Google Scholar]
Simpson 2008 {published and unpublished data}
- Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Anti-inflammatory effects of clarithromycin in refractory non-eosinophilic asthma. American Thoracic Society International Conference; 2007 May 18-23; San Francisco (CA).
- Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Anti-inflammatory effects of clarithromycin in refractory non-eosinophilic asthma. Respirology 2007;12:A120. [Google Scholar]
- Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Anti-inflammatory effects of clarithromycin in refractory non-eosinophilic asthma. Thoracic Society of Australia and New Zealand Annual Scientific Meeting; 2007 Mar 25-28; Auckland:Abstract TO13.
- Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Clarithromycin targets neutrophilic airway inflammation in refractory asthma. American Journal of Respiratory and Critical Care Medicine 2008;177(2):148-55. [DOI] [PubMed] [Google Scholar]
Strunk 2008 {published and unpublished data}
- Strunk RC, Bacharier LB, Phillips BR, Szefler SJ, Zeiger RS, Chinchilli VM, et al. Azithromycin or montelukast as inhaled corticosteroid-sparing agents in moderate-to-severe childhood asthma study. Journal of Allergy and Clinical Immunology 2008;122(6):1138-44.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sutherland 2010 {published data only}
- Sutherland ER, King TS, Icitovic N, Ameredes BT, Bleecker E, Boushey HA, et al. A trial of clarithromycin for the treatment of suboptimally controlled asthma. Journal of Allergy and Clinical Immunology 2010;126(4):747-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wan 2016 {published and unpublished data}
- Wan K-S, Liu Y-C, Huang C-S, Su Y-M. Effects of low-dose clarithromycin added to fluticasone on inflammatory markers and pulmonary function among children with asthma: a randomized clinical trial. Allergy and Rhinology 2016;7(3):e131-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2012 {published data only}
- Wang Y, Zhang SL, Qu Y. Effect of clarithromycin on non-eosinophilic refractory asthma [克拉霉素治疗非嗜酸粒细胞型难治性哮喘的疗效分析]. Journal of Clinical Pulmonary Medicine 2012;17(11):1948-51. [Google Scholar]
Wang 2014 {published data only}
- Wang T, Pei FY, Song XP, Wang Q. Clinical impacts of low-dose azithromycin on lung function and fraction of exhaled nitric oxide concentration in bronchial asthma [小剂量阿奇霉素对支气管哮喘患者呼出气NO浓度及肺功能的影响]. Medical Innovation China 2014;11(9):122-4. [Google Scholar]
Xiao 2013 {published data only}
- Xiao KA. The study on effect of roxithromycin combined with budesonide in therapy in patients with asthma. Guide of Chinese Medicine 2013;11:119-20. [Google Scholar]
Yan 2008 {published data only}
- Yan XQ, Wu LQ, Lin J, Xiao XD, Dai YR. Clinical study on efficacy of roxithromycin combined with inhaled budesonide dry powder inhalation on asthma [罗红霉素与布地奈德干粉吸入剂联用治疗哮喘的临床研究]. Chinese Journal of Pharmacology and Therapeutics 2008;13(2):184-7. [Google Scholar]
Zhang 2013 {published data only}
- Zhang LY, Qian Q. Clinical effect of azithromycin combined with Seretide for asthma. Strait Pharmaceutical Journal 2013;25:159-60. [Google Scholar]
References to studies excluded from this review
Andrade 1983 {published data only}
- Andrade WP, Renard RL, Nelson HS. The effect of troleandomycin and methylprednisolone alone and in combination on bronchial sensitivity to methacholine. Annals of Allergy 1983;51(5):515-7. [PubMed] [Google Scholar]
Anon 2009 {published data only}
- Anonymous. Bronchial asthma – clarithromycin depresses neutrophil inflammation [Asthma bronchiale – clarithromycin senkt die neutrophile Entzündung]. Pneumologie 2009;63(1):2. [DOI] [PubMed] [Google Scholar]
Bacharier 2015 {published data only}
- Bacharier LB, Guilbert TW, Mauger DT, Boehmer S, Beigelman A, Fitzpatrick AM, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: a randomized clinical trial. JAMA 2015;19:2034-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baigelman 2015 {published data only}
- Beigelman A, Isaacson-Schmid M, Sajol G, Baty J, Rodriguez OM, Leege E, et al. Randomized trial to evaluate azithromycin's effects on serum and upper airway IL-8 levels and recurrent wheezing in infants with respiratory syncytial virus bronchiolitis. Journal of Allergy and Clinical Immunology 2015;135(5):1171-78e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ball 1990 {published data only}
- Ball BD, Hill MR, Brenner M, Sanks R, Szefler SJ. Effect of low-dose troleandromycin on glucocorticoid pharmacokinetics and airway hyperresponsiveness in severely asthmatic children. Annals of Allergy 1990;65(1):37-45. [PubMed] [Google Scholar]
Cogo 1994 {published data only}
- Cogo R, Caiazzo G, De Luca P, Boddi V, De Luca M, Casini A. Effect of miocamycin and amoxicillin/clavulonate on total serum immunoglobulin E levels in patients with infectious exacerbations of allergic asthma: a crossover trial. Current Therapeutic Research 1994;55(2):184-98. [Google Scholar]
D'Azevedo Silveira 2016 {published data only}5639760
- D'Azevedo Silveira V, Roza CA, Luisi F, Pitrez PM, Stein RT, Pinto LA. Azithromycin therapy in infants with bronchiolitis reduces recurrent wheezing 3 months after hospitalization: a randomized, placebo-controlled trial. Pediatric Pulmonology 2016;S9:59. [Google Scholar]
Ebling 1984 {published data only}
- Ebling WF, Szefler SJ, WJ Jusko. Analysis of cortisol, methylprednisolone, and methylprednisolone hemisuccinate. Absence of effects of troleandomycin on ester hydrolysis. Journal of Chromatography 1984;305(2):271-80. [PubMed] [Google Scholar]
Feldman 1997 {published data only}
- Feldman C, Anderson R, Theron AJ, Ramafi G, Cole PJ, Wilson R. Roxithromycin, clarithromycin, and azithromycin attenuate the injurious effects of bioactive phospholipids on human respiratory epithelium in vitro. Inflammation 1997;21(6):655-65. [DOI] [PubMed] [Google Scholar]
Gong 2016 {published data only}5639762
- Gong L, Xu L, Diao M, Guo F, Bian FF, Min J, et al. Clinical effect of treating secondary asthma attacks of children Mycoplasma pneumoniae with combined therapy of montelukast and azithromycin. European Review for Medical and Pharmacological Sciences 2016;20(24):5256-60. [PubMed] [Google Scholar]
Gotfried 2004 {published data only}
- Gotfried MH, Jung R, Messick CR, Rubinstein I, Garey KW, Rodvold KA, et al. Effects of six-week clarithromycin therapy in corticosteroid-dependent asthma: a randomized, double-blind, placebo-controlled pilot study. Current Therapeutic Research 2004;65(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodgson 2016 {published data only}
- Hodgson D, Anderson J, Reynolds C, Oborne J, Meakin G, Bailey H, et al. The effects of azithromycin in treatment-resistant cough: a randomized, double-blind, placebo-controlled trial. Chest 2016;149(4):1052-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hueston 1991 {published data only}
- Hueston WJ. A comparison of albuterol and erythromycin for the treatment of acute bronchitis. Journal of Family Practice 1991;33:476-80. [PubMed] [Google Scholar]
Itkin 1970 {published data only}
- Itkin IH, Menzel ML. The use of macrolide antibiotic substances in the treatment of asthma. Journal of Allergy 1970;45(3):146-62. [DOI] [PubMed] [Google Scholar]
Johnston 2016 {published data only}
- Johnston SL, Szigeti M, Cross M, Brightling C, Chaudhuri R, Harrison T, et al. Azithromycin for acute exacerbations of asthma: the AZALEA randomized clinical trial. JAMA Internal Medicine 2016;176(11):1630-7. [DOI] [PubMed] [Google Scholar]
Kaplan 1958 {published data only}
- Kaplan MA, Goldin M. The use of triacetyloleandomycin in chronic infectious asthma. Antibiotics Annual 1958;6:273-6. [PubMed] [Google Scholar]
Koh 1997 {published data only}
- Koh YY, Lee MH, Sun YH, Sung KW, Chae JH. Effect of roxithromycin on airway responsiveness in children with bronchiectasis: a double-blind, placebo-controlled study. European Respiratory Journal 1997;10(5):994-9. [DOI] [PubMed] [Google Scholar]
Koutsoubari 2012 {published data only}
- Koutsoubari I, Papaevangelou V, Konstantinou GN, Makrinioti H, Xepapadaki P, Kafetzis D, et al. Effect of clarithromycin on acute asthma exacerbations in children: an open randomized study. Pediatric Allergy and Immunology 2012;23(4):385-90. [DOI] [PubMed] [Google Scholar]
Lee 1998 {published data only}
- Lee HB, Lee YC, Rhee YK. Effects of erythromycin and new macrolides on the serum theophylline level and clearance. Tuberculosis and Respiratory Diseases 1998;3:546-52. [Google Scholar]
Mandhane 2017 {published data only}
- Mandhane PJ, Paredes Zambrano de Silbernagel P, Aung YN, Williamson J, Lee BE, Spier S, et al. Treatment of preschool children presenting to the emergency department with wheeze with azithromycin: a placebo-controlled randomized trial. PloS One 2017;12(8):e0182411. [DOI: 10.1371/journal.pone.0182411] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oldach 2015 {published data only}5639703
- Oldach D, Luna C, Szabo P, Mitha I, Tanaseanu C, Doreski A, et al. Oral solithromycin has a favorable profile versus oral moxifloxacin for treatment of adult community-acquired pneumonia (CABP) in elderly patients and those with COPD or asthma. European Respiratory Journal 2015;Suppl 59:PA2655. [Google Scholar]
Ram 2016 {published data only}
- Ram B, Aggarwal AN, Dhooria S, Sehgal IS, Garg M, Behera D, et al. A pilot RCT of nebulized amphotericin for maintenance of remission in patients with allergic bronchopulmonary aspergillosis. Journal of Asthma 2016;5:517-24. [DOI] [PubMed] [Google Scholar]
Spector 1974 {published data only}
- Spector SL, Katz FH, Farr RS. Troleandomycin: effectiveness in steroid-dependent asthma and bronchitis. Journal of Allergy and Clinical Immunology 1974;54(6):367-79. [Google Scholar]
Stokholm 2016 {published data only}
- Stokholm J, Chawes BL, Vissing NH, Bjarnadottir E, Pedersen TM, Vinding RK, et al. Azithromycin for episodes with asthma-like symptoms in young children aged 1-3 years: a randomised, double-blind, placebo-controlled trial. Lancet Respiratory Medicine 2016;4(1):19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Szefler 1980 {published data only}
- Szefler SJ, Rose JQ, Ellis EF, Spector SL, Green AW, Jusko WJ. The effect of troleandomycin on methylprednisolone elimination. Journal of Allergy and Clinical Immunology 1980;66(6):447-51. [DOI] [PubMed] [Google Scholar]
Szefler 1982a {published data only}
- Szefler SJ, Brenner M, Jusko WJ, Spector SL, Flesher KA, Ellis EF. Dose- and time-related effect of troleandomycin on methylprednisolone elimination. Clinical Pharmacology and Therapeutics 1982;32(2):166-71. [DOI] [PubMed] [Google Scholar]
Szefler 1982b {published data only}
- Szefler SJ, Ellis EF, Brenner M, Rose JQ, Spector SL, Yurchak AM, et al. Steroid-specific and anticonvulsant interaction aspects of troleandomycin-steroid therapy. Journal of Allergy and Clinical Immunology 1982;69(5):455-60. [DOI] [PubMed] [Google Scholar]
Takamura 2001 {published data only}
- Takamura M, Odashima Y, Iikura H. Continuous low-dosage macrolide therapy in children with bronchial asthma. Japanese Journal of Antibiotics 2001;54(Suppl C):9-11. [PubMed] [Google Scholar]
Wald 1986 {published data only}
- Wald JA, Friedman BF, Farr RS. An improved protocol for the use of troleandomycin (TAO) in the treatment of steroid-requiring asthma. Journal of Allergy and Clinical Immunology 1986;78(1 Pt 1):36-43. [DOI] [PubMed] [Google Scholar]
Weinberger 1977 {published data only}
- Weinberger MW, Hudgel D, Spector S, Chidsey C. Inhibition of theophylline clearance by troleandomycin. Journal of Allergy and Clinical Immunology 1977;59(3):228-31. [DOI] [PubMed] [Google Scholar]
Zeiger 1980 {published data only}
- Zeiger RS, Schatz M, Sperling W, Simon RA, Stevenson DD. Efficacy of troleandomycin in outpatients with severe, corticosteroid-dependent asthma. Journal of Allergy and Clinical Immunology 1980;66(6):438-46. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02517099 {published data only}
- NCT02517099. Preschool wheeze: Inflammation/Infection Guided Management (PrIGMa) [Use of pathological phenotype to determine optimal management for moderate to severe preschool wheeze]. www.clinicaltrials.gov/ct2/show/NCT02517099 (first received 6 August 2015).
Additional references
Adachi 1996
- Adachi T, Motojima S, Hirata A. Eosinophil apoptosis caused by theophylline, glucocorticoids, and macrolides after stimulation with IL-5. Journal of Allergy and Clinical Immunology 1996;98(6 Pt 2):S207-15. [DOI] [PubMed] [Google Scholar]
Alvarez‐Elcoro 1999
- Alvarez-Elcoro S, Enzler MJ. The macrolides: erythromycin, clarithromycin, and azithromycin. Mayo Clinic Proceedings 1999;74(6):613-34. [DOI] [PubMed] [Google Scholar]
ATS 1987
- ATS Scientific Assembly on Clinical Problems. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. American Review of Respiratory Disease 1987;136(1):225-44. [DOI] [PubMed] [Google Scholar]
Black 1997
- Black PN. Anti-inflammatory effects of macrolide antibiotics. European Respiratory Journal 1997;10:971-2. [DOI] [PubMed] [Google Scholar]
Black 2000
- Black PN, Scicchitano R, Jenkins CR, Blasi F, Allegra L, Wlodarczyk J, et al. Serological evidence of infection with Chlamidia pneumoniae is related to the severity of asthma. European Respiratory Journal 2000;15(2):254-9. [DOI] [PubMed] [Google Scholar]
Brill 2015
- Brill SE, Law M, El-Emir E, Allinson JP, James P, Maddox V, et al. Effects of different antibiotic classes on airway bacteria in stable COPD using culture and molecular techniques: a randomised controlled trial. Thorax 2015;70(10):930-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
BTS 2020
- Smith D, Du Rand I, Addy CL, Collyns T, Hart SP, Mitchelmore PJ, et al. British Thoracic Society guideline for the use of long-term macrolides in adults with respiratory disease. Thorax 2020;75:370-404. [DOI] [PubMed] [Google Scholar]
Cai 2011
- Cai Y, Chai D, Wang R, Bai N, Liang BB, Liu Y. Effectiveness and safety of macrolides in cystic fibrosis patients: a meta-analysis and systematic review. Journal of Antimicrobial Chemotherapy 2011;66(5):968-78. [DOI] [PubMed] [Google Scholar]
Castro 2018
- Castro M, Corren J, Pavord ID, Maspero J, Wenzel S, Rabe KF, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. New England Journal of Medicine 2018;378(26):2486-96. [DOI] [PubMed] [Google Scholar]
CTCAE 2020
- National Cancer Institute. Common Terminology Criteria for Adverse Events v.6. ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm (accessed prior to 14 November 2021).
Enright 2004
- Enright PL, Beck KC, Sherrill DL. Repeatability of spirometry in 18,000 adult patients. American Journal of Respiratory and Critical Care Medicine 2004;169:235-8. [DOI: 10.1164/rccm.200204-347OC] [DOI] [PubMed] [Google Scholar]
Essilfie 2015
- Essilfie AT, Horvat JC, Kim RY, Mayall JR, Pinkerton JW, Beckett EL, et al. Macrolide therapy suppresses key features of experimental steroid-sensitive and steroid-insensitive asthma. Thorax 2015;70:458-67. [DOI] [PubMed] [Google Scholar]
Fan 2015
- Fan H. Macrolides for asthma [personal communication]. Email to: Kayleigh Kew 30 July 2015.
Farne 2017
- Farne HA, Wilson A, Powell C, Bax L, Milan SJ. Anti-IL5 therapies for asthma. Cochrane Database of Systematic Reviews 2017, Issue 9. Art. No: CD010834. [DOI: 10.1002/14651858.CD010834.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gencay 2001
- Gencay M, Rudiger JJ, Tamm M, Solér M, Perruchoud AP, Roth M. Increased frequency of Chlamydia pneumoniae antibodies in patients with asthma. American Journal of Respiratory and Critical Care Medicine 2001;163(5):1097-100. [DOI] [PubMed] [Google Scholar]
Gibson 2019
- Gibson PG, Yang IA, Upham JW, Reynolds PN, Hodge S, James AL, et al. Efficacy of azithromycin in severe asthma from the AMAZES randomised trial. ERJ Open Research 2019;5:00056-2019. [DOI: 10.1183/23120541.00056-2019] [DOI] [PMC free article] [PubMed] [Google Scholar]
GINA 1995
- Global Initiative for Asthma. Global strategy for asthma management and prevention (1995 version). ginasthma.org/wp-content/uploads/2019/01/1995-GINA.pdf (accessed 8 April 2015).
GINA 2002
- Global Initiative for Asthma. Global strategy for asthma management and prevention (2002 version). ginasthma.org/wp-content/uploads/2019/01/2002-GINA.pdf (accessed 8 April 2015).
GINA 2007
- Global Initiative for Asthma. Global strategy for asthma management and prevention (2007 update). ginasthma.org/wp-content/uploads/2019/01/2007-GINA.pdf (accessed 8 April 2015).
GINA 2010
- Global Initiative for Asthma. Global strategy for asthma management and prevention (update 2010). ginasthma.org/wp-content/uploads/2019/01/2010-GINA.pdf (accessed 8 April 2015).
GINA 2014
- Global Initiative for Asthma. Global strategy for asthma management and prevention (update 2014). ginasthma.org/wp-content/uploads/2019/01/2014-GINA.pdf (accessed 8 April 2015).
GINA 2020
- Global Initiative for Asthma. Global strategy for asthma management and prevention 2020. ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf (accessed prior to 20 May 2021).
GINA 2021
- Global Initiative for Asthma. Global strategy for asthma management and prevention 2021. ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf (accessed prior to 14 November 2021.
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org (accessed 27 June 2021).
Hansbro 2014
- Hansbro PM, Starkey MR, Mattes J, Horvat JC. Pulmonary immunity during respiratory infections in early life and the development of severe asthma. Annals of the American Thoracic Society 2014;11(Suppl 5):S297-302. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Hiles 2019
- Hiles SA, McDonald VM, Guilhermino M, Bruselle GG, Gibson PG. Does maintenance azithromycin reduce asthma exacerbations? An individual participant data meta-analysis. European Respiratory Journal 2019;54(5):1901381. [DOI: 10.1183/13993003.01381-2019] [DOI] [PubMed] [Google Scholar]
Hinks 2021
- Hinks T, Levine SJ, Brusselle GG. Treatment options in type-2 low asthma. European Respiratory Journal 2012;57(1):2000528. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jadad 1996
- Jadad A, Moore RA, Carroll D, Jenkson C, Reynolds JM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials 1996;17(1):1-12. [DOI] [PubMed] [Google Scholar]
Juniper 1994
- Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. Journal of Clinical Epidemiology 1994;47(1):81-7. [DOI] [PubMed] [Google Scholar]
Juniper 2005
- Juniper EF, Svensson K, Mork AC, Stahl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respiratory Medicine 2005;99:553-8. [DOI] [PubMed] [Google Scholar]
Kawasaki 1998
- Kawasaki S, Takizawa H, Ohtoshi T, Takeuchi N, Kohyama T, Nakamura H, et al. Roxithromycin inhibits cytokine production by and neutrophil attachment to human bronchial epithelial cells in vitro. Antimicrobial Agents and Chemotherapy 1998;42(6):1499-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Konno 1994
- Konno S, Asano K, Kurokawa M, Ikeda K, Okamoto K, Adachi M. Antiasthmatic activity of a macrolide antibiotic, roxithromycin: analysis of possible mechanisms in vitro and in vivo. International Archives of Allergy and Immunology 1994;105(3):308-16. [DOI] [PubMed] [Google Scholar]
Koyama 1998
- Koyama T, Takizawa H, Kawasaki S, Takami K, Otoshi T, Ito K. Effects of various drugs on IL-8 production by eosinophils collected from patients with allergic inflammation. Japanese Journal of Antibiotics 1998;51(Suppl A):131-3. [PubMed] [Google Scholar]
Kraft 1998
- Kraft M, Cassell GH, Henson JE, Watson H, Williamson J, Marmion BP, et al. Detection of Mycoplasma pneumoniae in the airways of adults with chronic asthma. American Journal of Respiratory and Critical Care Medicine 1998;158(3):998-1001. [DOI] [PubMed] [Google Scholar]
Malhotra‐Kumar 2007
- Malhotra-Kumar S, Lammens C, Coenen S, Herck K, Goossens H. Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet 2007;369(9560):482-90. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Normansell 2014
- Normansell R, Walker S, Milan SJ, Walters EH, Nair P. Omalizumab for asthma in adults and children. Cochrane Database of Systematic Reviews 2014, Issue 1. Art. No: CD003559. [DOI: 10.1002/14651858.CD003559.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olin 2014
- Olin JT, Wechsler ME. Asthma: pathogenesis and novel drugs for treatment. BMJ 2014;349:g5517. [DOI] [PubMed] [Google Scholar]
Pasternack 2005
- Pasternack R, Huhtala H, Karjalainen J. Chlamydophila (Chlamydia) pneumoniae serology and asthma in adults: a longitudinal analysis. Journal of Allergy and Clinical Immunology 2005;116(5):1123-8. [DOI] [PubMed] [Google Scholar]
Rabe 2018
- Rabe KF, Nair P, Brusselle G, Maspero JF, Castro M, Sher L, et al. Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. New England Journal of Medicine 2018;378(26):2475-85. [DOI] [PubMed] [Google Scholar]
Reiter 2013
- Reiter J, Demirel N, Mendy A, Gasana J, Vieira ER, Colin AA, et al. Macrolides for the long-term management of asthma – a meta-analysis of randomized clinical trials. Allergy 2013;68(8):1040-9. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schünemann 2021
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing 'Summary of findings' tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). In: Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Spagnolo 2013
- Spagnolo P, Fabbri LM, Bush A. Long-term macrolide treatment for chronic respiratory disease. European Respiratory Journal 2013;42(1):239-51. [DOI] [PubMed] [Google Scholar]
Tong 2015
- Tong X, Guo T, Liu S, Peng S, Yan S, Yang X, et al. Macrolide antibiotics for treatment of asthma in adults: a meta-analysis of 18 randomized controlled clinical studies. Pulmonary Pharmacology and Therapeutics 2015;31:99-108. [DOI] [PubMed] [Google Scholar]
Wang 2019
- Wang X, Luo J, Wang D, Liu B, Liu C. The efficacy and safety of long-term add-on treatment of azithromycin in asthma: a systematic review and meta-analysis. Medicine 2019;98(38):e17190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wood 2013
- Wood PR, Hill VL, Burks ML, Peters JI, Singh H, Kannan TR, et al. Mycoplasma pneumoniae in children with acute and refractory asthma. Annals of Allergy, Asthma and Immunology 2013;110(5):328-334.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Kew 2015
- Kew KM, Undela K, Kotortsi I, Ferrara G. Macrolides for chronic asthma. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No: CD002997. [DOI: 10.1002/14651858.CD002997.pub4] [DOI] [PubMed] [Google Scholar]
Richeldi 2002
- Richeldi L, Ferrara G, Fabbri LM, Gibson PG. Macrolides for chronic asthma. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No: CD002997. [DOI: 10.1002/14651858.CD002997] [DOI] [PubMed] [Google Scholar]
Richeldi 2005
- Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG. Macrolides for chronic asthma. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD002997. [DOI: 10.1002/14651858.CD002997.pub2] [DOI] [PubMed] [Google Scholar]


