ABSTRACT
Coronavirus disease-2019 (COVID-19)-associated mucormycosis is on the rise in the Indian subcontinent. We report a unique case of cutaneous mucormycosis in a case of newly diagnosed young diabetic patient with severe COVID-19 pneumonia with post-COVID lung fibrosis. Neither did he have any preceding trauma or wound, nor was there any evidence of any secondary dissemination. Cutaneous mucormycosis without evidence of either is unheard off. Possible risk factors in this case were multiple bacterial secondary infections with the use of higher antibiotics, use of voriconazole for possible aspergillosis, and steroid use.
How to cite this article
Tambe RR, Hinduja A, Sunil S, Varaiya A, Joshi A. Cutaneous Mucormycosis in a Patient of Severe COVID-19 Pneumonia: A Rarer than Rare Case Report. Indian J Crit Care Med 2021;25(11):1318–1319.
Keywords: COVID-19 and mucormycosis, COVID-19-associated mucormycosis, Cutaneous mucormycosis, Secondary invasive fungal infection
INTRODUCTION
Secondary infections are common in many viral illnesses. Fifty-eight percent of severe and critical coronavirus disease-2019 (COVID-19) patients had secondary infections.1 In India, there are rising reports of COVID-associated mucormycosis infections (CAM) with a prevalence of 0.27%.2 Like non-CAM, CAM commonly affects rhino-orbital followed by rhino-orbital-cerebral site followed by pulmonary followed by other sites.2 Of these cases, cutaneous mucormycosis was less than 0.026%.2
Mucormycosis is a rare but serious invasive fungal infection.3 Cutaneous mucormycosis lesions present as indurated plaques that are erythematous to purple. These become necrotic with an erythematous halo that can develop into an eschar. Other presentations include blisters, cellulitis, tender nodules, ulcers, and purpuric lesions.4 Unlike other forms of mucormycosis, cutaneous mucormycosis can occur in the immunocompetent host.4 Cutaneous mucormycosis occurs secondary to inoculation of spores in cuts or open wounds. It could rarely also be secondary to dissemination from another site. We present a unique case that had neither any preceding trauma nor a source of secondary dissemination and was found to have cutaneous mucormycosis near the anterior axillary fold. So far we have not come across any patient with cutaneous mucormycosis in the absence of trauma or the absence of secondary dissemination. This makes it a unique case.
AIM AND OBJECTIVE
To report a unique case of cutaneous mucormycosis in a young man with severe COVID-19 pneumonia.
CASE DESCRIPTION
A 32-year-old premorbid healthy male was presented on April 28, 2021, with fever, loose motions, and breathlessness. High resolution computed tomography (HRCT) revealed more than 75% lung involvement with CORAD-5. The patient was admitted to COVID intensive care unit (ICU) requiring invasive ventilation. His COVID-19 test and rapid antigen test were negative. He had high titers of COVID antibodies with no COVID vaccination history. Treatment was initiated with enoxaparin, remdesivir, ceftriaxone, and prednisolone (60 mg twice a day). Antibiotics were escalated to injection meropenem and teicoplanin for persistent fever with rising trend of procalcitonin, total leukocyte count and interleukin-6. Blood cultures were negative. Gradually his fever subsided. Steroids were tapered and stopped by day 10. The patient underwent tracheostomy on day 10. On day 13, fever recurred with inotropic support requirement. Galactomannan levels were raised, hence voriconazole was started. Repeat cultures grew carbapenemase-producing Acinetobacter baumannii in blood, hence antibiotics switched to polymyxin and minocycline. Later pirfenidone was added as repeat HRCT showed interstitial septal thickening. The Patient developed weakness of all four limbs. Evaluation with electromyography and nerve conduction studies revealed critical illness myopathy. Glycosylated hemoglobin was 8.8 mg/dL. On day 33, the patient had fever recurrence with increased mucopurulent tracheal secretions. Repeat blood culture (two sets) and tracheostomy culture grew pan sensitive Klebsiella pneumoniae, appropriate antibiotics added. Fever persisted. The patient developed a painful hemorrhagic bulla at the left anterior axillary fold with an erythematous halo (Fig. 1). Patient denied any trauma to the abovementioned site. No procedure, dressing, or needlestick injury occurred at that site. Electrocardiogram chest leads were also far from the lesion ruling out iatrogenic trauma as the possible source of the cutaneous mucormycosis. Ultrasonography (USG) done to understand the depth of the lesion revealed evolving abscess (Fig. 2). Surgical debridement and aspiration was done and cultures were sent, which grew Mucor species. Injection liposomal amphotericin-B was started. His fever settled thereafter. In view of no obvious prior trauma or wound, the possibility of dissemination or other sources of Mucor was considered. Magnetic resonance imaging of brain orbits with paranasal sinus and otolaryngological evaluation did not reveal anything suggestive of Mucor infection. HRCT chest was repeated which revealed a cavity in the right lobe of the lung. Three sets of tracheostomy cultures revealed no evidence of Mucor. Hence, it was concluded that the cavity is secondary to Klebsiella pneumoniae infection. Patient received twenty-one doses of liposomal amphotericin-B and later was continued on isavuconazole on discharge for a total of 60 days. Patient recovered and regained mobility with good healing of the wound.
Fig. 1.

Hemorrhagic bullae near anterior axillary fold—later diagnosed as cutaneous mucormycosis on culture of aspirate
Fig. 2.
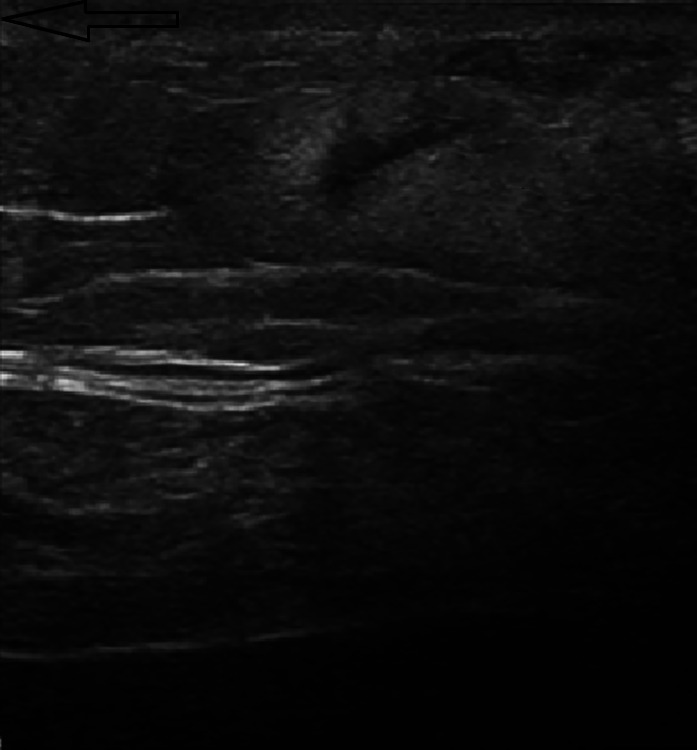
USG image of the evolving abscess
DISCUSSION
In view of the increased incidence of mucormycosis seen in COVID-19 patients, a direct correlation between the two needs to be evaluated further. There are several potential mechanisms, which may have contributed to the development of mucormycosis in our patient:
He is an undiagnosed case of diabetes mellitus.
COVID-19 is associated with severe immune system abnormalities.1
He had severe COVID-19 infection requiring prolonged ICU stay. He also received multiple higher antibiotics. These may predispose to bacterial and fungal coinfections.1
He received steroids for COVID-19 and voriconazole for suspected invasive aspergillosis; both these medications are known to increase the risk of mucormycosis.
In cases of cutaneous mucormycosis, infection develops when spores enter the body through a cut or open wound. This did not seem to be the cause in the present case and the source of mucormycosis remains unidentified. In view of the absence of any trauma, a possibility of secondary dissemination from an unknown primary cannot be entirely ruled out.
To the best of our knowledge, this is the first documented case of COVID-19-associated cutaneous mucormycosis without any trauma, burns, or other possible sources of direct inoculation.
Learning Points
Cutaneous mucormycosis should be considered as a possible infection in patients of COVID-19 infection having unusual skin lesions, especially with other comorbidities even in the absence of any other sources or dissemination. All skin lesions should be evaluated and if possible subjected to a biopsy to rule out cutaneous mucormycosis.
CONCLUSION
To conclude that cutaneous mucormycosis although a rare disorder should be considered as a differential possibility in COVID-19 infection patients with unusual cutaneous lesions.
Footnotes
Source of support: Nil
Conflict of interest: None
ORCID
Rahul R Tambe https://orcid.org/0000-0002-2003-1352
Anupa Hinduja https://orcid.org/0000-0002-8000-3265
Suchithra Sunil https://orcid.org/0000-0001-6720-1083
Ami Varaiya https://orcid.org/0000-0001-8367-8826
Amol Joshi https://orcid.org/0000-0003-3034-478X
REFERENCES
- 1.Zhang H, Zhang Y, Wu J, Li Y, Zhou X, Li X, et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020;9(1):1958–1964. doi: 10.1080/22221751.2020.1812437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel A, Agarwal R, Rudramurthy SM, Shevkani M, Xess I, Sharma R, et al. Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis. 2021;27(9):2349–2359. doi: 10.3201/eid2709.210934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Mucormycosis. Who.Int. WHO – South East Asia – India; 2021. Available from: https://www.who.int/india/emergencies/coronavirus-disease-(covid-19)/mucormycosis.
- 4.Castrejón-Pérez AD, Miranda I, Welsh O, Welsh EC, Ocampo-Candiani J. Cutaneous mucormycosis. An Bras Dermatol. 2017;92(3):304–311. doi: 10.1590/abd1806-4841.20176614. [DOI] [PMC free article] [PubMed] [Google Scholar]


