Abstract
Introduction:
Physicians play a critical role in tobacco treatment, being a frequent link to smokers and a trusted source of information. Unfortunately, barriers exist that limit physicians’ implementation of evidence-based interventions. This study examines the implementation and predictors of the “5A’s” tobacco treatment clinical guidelines among U.S. physicians.
Methods:
A national sample of 1,058 U.S. physicians from 6 specialties (Family Medicine, Internal Medicine, Obstetrics and Gynecology, Cardiology, Pulmonology, and Oncology) were surveyed in 2018 (51.8% response rate). Survey domains included: demographics, awareness of guidelines, tobacco treatment practices (i.e., 5A’s), perceived barriers to treatment, and perceived efficacy of various treatments. Multiple logistic regression analyzed predictors of implementing guideline activities.
Results:
Mean age was 51.3 years, with the majority male (64.4%) and non-Hispanic White (63.9%). Nearly all physicians reported asking patients if they smoke (95.6%) and advising to stop (94.8%), slightly fewer assessed readiness to quit (86.5%), and only a minority assisted with a quit plan (27.4%), or arranged follow-up (18.6%). Only 18% reported using the U.S. Public Health Service Guidelines in clinical practice. Time-related factors were the most common barriers (53.4%), with patient factors (36.9%) and financial/resource factors (35.1%) cited less frequently. Predictors of implementing aspects of the 5A’s included physician awareness and utilization of the U.S. Public Health Service guidelines, specialty, and to a smaller degree graduating prior to 1990, not reporting time as a barrier, patient barriers, sex, and higher perceived effectiveness of pharmacotherapy.
Conclusions:
This national survey highlights the need for increased implementation of all aspects of the latest guidelines for evidence-based tobacco treatments, including community-based resources.
Keywords: smoking cessation, physician behavior, clinical guidelines
INTRODUCTION
Despite progress made in reducing tobacco use, cigarette smoking remains the leading cause of preventable disease and death in the U.S. In 2019, cigarette use was reported by 14.0% of U.S. adults, the most of any tobacco product.1 Long-term tobacco use can result in a number of illnesses including lung cancer, heart disease, and chronic obstructive pulmonary disease.2,3 In addition to the health burden, tobacco-related illnesses yield billions in healthcare expenditures.4 In order to lessen this burden on the healthcare system, effective means of cessation are vital.
Physicians have unique access to smokers, establishing provider–patient relationships with smoking patients over years. Furthermore, physician advice has been recognized as a major determinant in a patient’s decision to quit5,6 and in the U.S., 4 of the 7 Food and Drug Administration (FDA)-approved pharmacotherapies currently require a prescription. In the context of growing sources of health information, research suggests that although individuals reported receiving information from TV, Internet, and elsewhere, the most widely accessed and trusted source was their physician.7,8 Indeed, research points to smokers listing their physicians as the most credible source of tobacco-cessation information.8
In 1996, the U.S. Public Health Service (USPHS) released the “Clinical Practice Guideline for Treating Tobacco Use and Dependence.” This guideline, which has been updated throughout the years, provides key evidence-based recommendations and draws attention to the “5A’s” of clinical interventions for smoking cessation: Ask, Advise, Assess, Assist, and Arrange. These “5A’s” highlight the need to: (1) Ask every patient if they use tobacco, (2) Advise them to quit, (3) Assess willingness to quit, (4) Assist in making a quit attempt, and (5) Arrange for follow-up.5,9
Studies have explored the implementation of the 5A’s by physicians in a variety of clinical settings. Implementation results in greater satisfaction for the healthcare provider and cessation success among patients.6,10 Though physicians historically have a high rate of Asking (90%) and Advising (71%) patients,11 relatively fewer report Assessing, Assisting, and Arranging.2,12 Notably, implementation of assist and arrange were found to be highly correlated with cessation success among patients, highlighting the importance of executing all of the 5A’s.13 Barriers previously reported in fully implementing the 5A’s include lack of time, providers forgetting to complete follow-up, and lack of training.12,13
Much of the research focused on the delivery of the 5A’s by physicians have focused on primary care providers.2,6 Although internal medicine and family medicine physicians provide primary care to adult smokers and can intervene prior to the onset of disease, other specialties, such as oncologists, pulmonologists, and cardiologists, often treat smokers who already suffer with tobacco-caused disease. Additionally, obstetrician–gynecologists may provide care to pregnant smokers, a critical patient group, or deliver primary care to women of childbearing age. Thus, understanding the utilization of the 5A’s across multiple diverse specialties is critical to assess the impact that tobacco treatment interventions could have among the full spectrum of tobacco users. The current study explores the rates and predictors of practicing the 5A’s among a national sample of U.S. physicians across a variety of specialties.
METHODS
Study Sample
The physician sample was randomly drawn from the American Medical Association’s Physician Masterfile and was obtained through the licensed vendor, Medical Marketing Service. Total sample size was 3,000 distributed evenly across 6 specialties of interest (500 were randomly selected from each specialty): Family Medicine, Internal Medicine, Obstetrics and Gynecology, Cardiology, Pulmonology, and Oncology. These specialties were chosen as they are the most involved in primary patient care, tobacco cessation, and treatment of tobacco-related illnesses. Overall, 1,058 physicians participated, and 496 physicians were ineligible (e.g., not seeing outpatients). The American Association for Public Opinion Research guidelines for mail surveys were used to calculate final response rates; eligibility status of the unknown non-responders was estimated via proportional allocation using known cases.14 This yielded an overall response rate of 51.8%.15 There were no significant differences between respondents and non-respondents within specialties with respect to mean age and sex with the exception of oncologists; non-respondent oncologists were on average 2 years older than respondents (p<0.05). Overall (i.e., all 6 specialties), non-respondents were significantly more likely to be male (p<0.05) and older (1.2 years) (p<0.05) than respondents; however, the effect of male sex was non-significant when controlling for medical specialty.
Survey fielding occurred from February to July 2018. Several survey method experiments were embedded in the study. First, a split sample experiment with a subset of cases (n=1,000) to explore the feasibility of web-based survey data collection was conducted. Details on this experiment are found elsewhere.16 In brief, the web-push data collection mode obtained the same response rate as the traditional paper-and-pencil mail survey. As such, the remainder of the sample employed web-push data collection. Second, experiments that varied the survey incentive amount ($25 vs $50) were performed, and there were minimal non-significant differences in response rate by incentive amount (51.0% vs 52.4%).
An initial mailing contained a personalized introductory cover letter, an upfront incentive, and either the paper survey or instructions how to complete the web survey (i.e., the survey URL was provided with an anonymous login code). One week after the first mailing, a second mailing contact via postcard was sent to non-respondents. The third mailing to non-responders mirrored the first contact, minus the gift card. The fourth mailing to all non-responders included a paper survey as well as a cover letter with instructions on how to complete the web survey, giving all non-responders on the fourth contact a choice of data collection mode (i.e., paper survey or web survey).
Measures
The survey instrument addressed several domains focused on tobacco use and patient provider communication. Survey questions were adapted from previous surveys conducted by the authors on physicians’ tobacco treatment practices,17,18 which have been adapted by others for use with healthcare providers.19 Specific to this paper, the outcome variable was delivery of the USPHS guidelines (i.e., the 5A’s) and the predictor variables included demographics, awareness of the USPHS guidelines, perceived barriers to tobacco treatment, and perceived effectiveness of pharmacotherapy. Outcome and predictor variables are described in greater detail below.
Physicians were asked to indicate on a 5-point scale (never=1, rarely=2, some of the time=3, most of the time=4, or always=5) how often they engage in each of the 5A’s (Ask, Advise, Assess, Assist, and Arrange) in their outpatient practice. The authors operationally defined engaging in the 5A’s as responding always for Ask and Advise given the high rates of physician practice, and as always or most of the time for Assess, Assist, and Arrange, which physicians have historically engaged in less frequently.20–22 With the exception of Assist, each activity was assessed with 1 item. For Assist, physicians responded to 3 separate behaviors, each of which are considered Assisting: encouraging smokers to set a quit date, discussing medication options, and referring to treatment (e.g., quitline). Operationally, “Assisting” was defined as affirmatively responding always or most of the time to all 3 of these practices.
Barriers to providing smoking-cessation treatment were assessed using a 4-point scale (strongly agree to strongly disagree), which was collapsed into strongly agree versus all other responses. Barriers included competing priorities in the visit, lack of time, patient’s disinterest in pharmacotherapy, patient’s resistance to cessation messages, lack of community resources, cost of cessation treatment to patient, and limited provider reimbursement. Physicians were also asked to indicate how effective they thought each of 7 FDA-approved medications were in helping smokers quit cigarettes by rating them each on a 4-point scale (not at all effective to very effective).
Statistical Analyses
Analyses were conducted using Stata, version 16x. Univariate descriptive statistics were used to describe the sample in detail as well as the outcome and predictor variables. Given the large number of predictors, data reduction techniques were used prior to modeling predictors of the 5A’s. First, factor analyses were conducted (principal component analysis) of the 7 physician-perceived barriers to effective smoking cessation, which resulted in 3 categories of barriers—“Time Factors,” “Patient Factors,” and “Financial/Resource Factors”—which were used in the logistic regression. The 7 barriers are grouped under their respective category. Second, a scale reliability analysis was conducted for perceived effectiveness of the 7 pharmacotherapies, which yielded a Chronbach’s α of 0.84, suggesting high internal consistency. As such, the perceived effectiveness of 7 tobacco-cessation pharmacotherapies were averaged and treated as a continuous scale for logistic regression.
This study estimated AORs for 5 separate models, with each of the 5A’s as the outcome variables. Predictor variables in this analysis included sex, year of graduation, medical specialty/subspecialty, awareness of the guidelines, perceived barriers to effective smoking cessation, and perceived effectiveness of cessation pharmacotherapy. Additional independent variables used for adjustment purposes included physician race/ethnicity.
RESULTS
Table 1 summarizes the demographic and professional characteristics of the 1,058 respondents. The mean age was 51.3 years and the majority reported being male (64.4%) and identified their race as non-Hispanic White (63.9%). The mean medical school graduation year was 1993 and 75% of respondents graduated from a U.S. medical school.
Table 1.
Characteristics of Physician Responders
| Characteristic | Full sample n (%) n=1,058 |
|---|---|
|
| |
| Age, mean, years (SD) | 51.3 (+/− 10.6) |
| Sex | |
| Male | 681 (64.4) |
| Female | 360 (34.0) |
| No response/Other | 17 (1.6) |
| Race | |
| White, non-Hispanic | 676 (63.9) |
| Asian/Pacific Islander | 138 (13) |
| South Asian | 79 (7.5) |
| Black, non-Hispanic | 48 (4.5) |
| Hispanic | 42 (4.0) |
| Other/No response | 75 (7.1) |
| Specialty | |
| Family medicine | 208 (19.7) |
| Internal medicine | 169 (16) |
| Obstetrics/Gynecology | 203 (19.2) |
| Pulmonary | 175 (16.5) |
| Cardiology | 147 (13.9) |
| Oncology | 140 (13.23) |
| No response | 16 (1.5) |
| Medical school | |
| U.S. graduate | 790 (74.7) |
| Graduation year | |
| Before 1990 | 388 (36.7) |
| During 1990s | 293 (27.7) |
| During 2000s | 325 (30.7) |
| No response | 52 (4.9) |
| Practice type | |
| Group-single specialty | 306 (28.9) |
| Hospital or health organization | 299 (28.3) |
| Multispecialty | 132 (12.5) |
| Solo practice | 125 (11.8) |
| Academic medical center | 122 (11.5) |
| Other | 62 (5.9) |
| No response | 12 (1.1) |
Figure 1 illustrates delivery of each of the 5A’s by specialty. Overall, as expected, Ask and Advise were universally implemented (≥90%) by most specialties and there was a general decrease in percentage of physicians utilizing each activity as they moved from Ask through Arrange. In terms of specialty, pulmonologists had among the highest rates for each activity, whereas obstetrician–gynecologists and oncologists had among the lowest, especially for Assess (78.7% and 73.6%, respectively) and Assist (17.7% and 18.6%). Very few obstetrician–gynecologists (3%) Arranged follow-up. Few significant differences in the reported delivery of the 5A’s were noted by demographic characteristics. Female physicians were more likely (90.5%) than male physicians (84.4%) to report Assessing (p=0.006) and male physicans (21.8%) were more likely to report Arranging for follow-up compared with female physicans (11.7%) (p<0.0001). Additionally, those who graduated medical school before 1990 were more likely to report Arranging for follow-up (23%) than those who graduated in the 1990s (16.0%) or in the 2000s (14.7%) (p=0.009).
Figure 1.
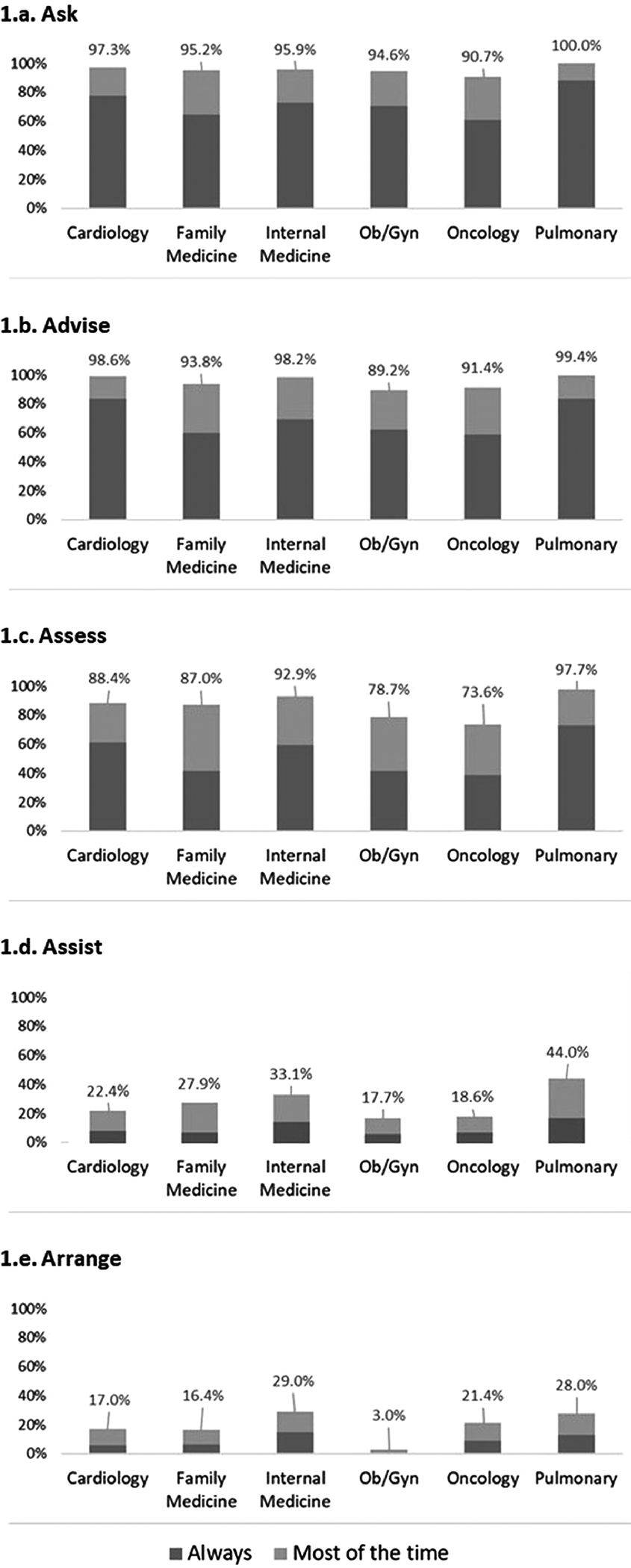
Delivery of the 5 A’s among U.S. physicians by specialty.
Tobacco treatment–related knowledge and beliefs are summarized in Table 2. Of note, only a minority of respondents (18%) reported using the USPHS Guidelines in clinical practice and 30% reported they have never heard about the guidelines. With respect to barriers to delivering cessation, the most common barriers noted were time-related factors, with 53.4% reporting that they strongly agreed that competing priority or lack of time during patient visits were barriers. Physicians also indicated that patient factors were a barrier with 36.9% strongly agreeing that patient’s disinterest in pharmacotherapy or resistance to cessation messages were barriers to effective smoking cessation in practice. Financial or resource issues were cited less frequently as barriers, with lack of community resources (19.1%) being the most common financial or resource barrier. Physician opinion diverged on the perceived efficacy of the various forms of FDA-approved pharmacotherapies. Varenicline and bupropion were viewed as most effective by a strong majority (89.9% and 75.3%, respectively) whereas among nicotine-replacement therapies (NRTs), just the nicotine patch was perceived as effective by a majority of respondents (68.2%). Nicotine gum, lozenge, inhaler, and nasal spray were all seen as less effective.
Table 2.
Tobacco Treatment Related Beliefs Among U.S. Physicians (N=1,054)
| Beliefs/Awareness | Full sample, % n=1,058 |
|---|---|
|
| |
| Awareness of USPHS guidelines | |
| Never heard about | 30.0 |
| Heard/Read about but not used | 50.0 |
| Have used in practice | 18.0 |
| Barriers to cessation deliverya,c | |
| Time factors | 53.4 |
| Competing priorities in the visit | 46.6 |
| Lack of time during patient visit | 30.3 |
| Patient factors | 36.9 |
| Patient’s disinterest in pharmacotherapy | 17.8 |
| Patient’s resistance to cessation messages | 31.6 |
| Financial/Resource factors | 35.1 |
| Lack of community resources for referral | 19.1 |
| Cost of cessation treatment to patient (e.g., medication, counseling) | 17.6 |
| No or limited provider reimbursement | 14.0 |
| Perceived effectiveness of pharmacotherapyb,c | |
| Varenicline (Chantix) | 89.9 |
| Bupropion (Zyban) | 75.3 |
| Nicotine patch | 68.2 |
| Nicotine gum | 49.8 |
| Nicotine lozenge | 41.4 |
| Nicotine oral inhaler | 37.4 |
| Nicotine nasal spray | 33.4 |
Strongly agree.
Somewhat, or very effective.
Individual barriers/pharmacotherapies were not mutually exclusive and will not sum to 100%.
USPHS, U.S. Public Health Service.
Predictors of each of the 5A’s are found in Table 3. Physician awareness and implementation of the USPHS guidelines was a robust and significant predictor of adherence to all 5 steps of the 5A’s. Additionally, specialty was significantly associated with the delivery of each of the 5A’s. Pulmonologists were significantly more likely to perform each of the 5A’s than other specialists except Arrange. Arranging for follow up, which was performed infrequently, was significantly more likely from internists and oncologists, and least likely from obstetrician–gynecologists. In addition, physicians who graduated earlier, prior to 1990, were significantly more likely to Ask or Advise. Male physicians were less likely to Assess readiness to quit. Physicians who identified time as a barrier were significantly less likely to engage in all of the 5A’s. Interestingly, physicians who identified patient factors as a barrier were significantly more likely to report they Ask about smoking status and Assist. Lastly, higher perceived effectiveness of pharmacotherapy was associated with higher rates of Arranging for follow-up.
Table 3.
Factors Associated With Delivering the 5 A’s
| Ask about smoking statusa | Advise to quit smokinga | Assess readiness to quitb | Assist with quit attemptb | Arrange for follow-upb | |
|---|---|---|---|---|---|
|
|
|||||
| Physician factor | AOR 95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% C)] | AOR (95% CI) |
|
| |||||
| Male | 0.84 (0.60, 1.17) | 0.77 (0.55, 1.06) | 0.33 (0.21, 0.54) | 0.85 (0.60, 1.22) | 1.53 (0.99, 2.38) |
| White (vs non-White) | 0.84 (0.61, 1.16) | 0.78 (0.57, 1.06) | 0.85 (0.55, 1.30) | 0.92 (0.66, 1.28) | 0.72 (0.49, 1.04) |
| When graduated | |||||
| After 1999 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| 1990s | 1.13 (0.78, 1.62) | 1.31 (0.92, 1.86) | 0.89 (0.54, 1.45) | 1.08 (0.72, 1.62) | 1.09 (0.67, 1.76) |
| Before 1990 | 1.51 (1.03, 2.20) | 2.28 (1.58, 3.30) | 1.19 (0.72, 1.98) | 1.08 (0.73, 1.60) | 1.40 (0.90, 2.20) |
| Specialty | |||||
| Family medicine | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Cardiology | 1.83 (1.08, 3.12) | 3.25 (1.85, 5.70) | 1.56 (0.78, 3.14) | 0.97 (0.54, 1.73) | 1.20 (0.62, 2.30) |
| Internal medicine | 1.27 (0.79, 2.04) | 1.38 (0.87, 2.20) | 2.14 (1.02, 4.51) | 1.49 (0.90, 2.45) | 2.33 (1.32, 4.10) |
| Ob/Gyn | 1.37 (0.88, 2.15) | 1.33 (0.86, 2.05) | 0.64 (0.36, 1.14) | 0.75 (0.44, 1.28) | 0.22 (0.09, 0.57) |
| Oncology | 1.01 (0.63, 1.64) | 1.24 (0.77, 2.00) | 0.59 (0.32, 1.06) | 0.80 (0.44, 1.45) | 1.92 (1.02, 3.60) |
| Pulmonary | 3.46 (1.97, 6.09) | 3.18 (1.90, 5.33) | 6.70 (2.25, 19.93) | 2.03 (1.26, 3.29) | 1.56 (0.90, 2.73) |
| Awareness of USPHS guidelines | |||||
| Never heard about | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Heard/Read about but not used | 1.40 (1.02, 1.93) | 1.89 (1.38, 2.60) | 1.86 (1.24, 2.80) | 1.96 (1.32, 2.91) | 1.73 (1.08, 2.76) |
| Have used in practice | 2.73 (1.64, 4.54) | 2.52 (1.59, 4.02) | 3.62 (1.63, 8.05) | 4.98 (3.13, 7.94) | 3.89 (2.28, 6.65) |
| Patient barriersc | 1.72 (1.25, 2.37) | 1.12 (0.82, 1.51) | 1.17 (0.77, 1.78) | 1.50 (1.08, 2.08) | 1.05 (0.72, 1.54) |
| Cost/Resource barriersc | 1.12 (0.82, 1.55) | 1.31 (0.96, 1.79) | 1.55 (0.99, 2.41) | 1.18 (0.85, 1.64) | 1.15 (0.79, 1.68) |
| Time barriersc | 0.71 (0.52, 0.97) | 0.60 (0.44, 0.82) | 0.45 (0.30, 0.70) | 0.47 (0.34, 0.65) | 0.37 (0.25, 0.54) |
| Perceived effectiveness of medication | 1.26 (0.89, 1.78) | 0.72 (0.51, 1.02) | 0.83 (0.52, 1.33) | 1.44 (0.99, 2.07) | 1.80 (1.18, 2.76) |
Always.
Most of the time or always.
Physician-perceived barriers aggregated into 3 factors: “Time”, “Patient”, and “Financial/resource”. Physician was considered to agree with these factors as barriers if they strongly agreed in any question belonging to that category.
USPHS, U.S. Public Health Service.
DISCUSSION
After a review of the literature, this study appears to be the first national survey of multiple physician specialties focused on physician engagement in each of the 5A’s and predictors of such practices. Although these findings are consistent with other surveys indicating that physicians generally Ask and Advise patients, this study adds: (1) differentiation of tobacco guidelines implementation by medical specialty; (2) predictors of implementation including awareness of guidelines, certain perceived barriers, and physician characteristics; and (3) the perceived effectiveness of pharmacotherapy as a predictor. The overwhelming majority of physicians reported routinely Asking their patients about smoking, Advising to stop, and Assessing their willingness to quit. Despite this encouraging finding, far fewer report that they Assist their patients with a treatment plan and Arrange follow-up visits to address cessation. These results are similar to previous studies where Asking and Advising were frequent, whereas Assisting and Arranging were quite rare.20,21 The strongest predictors of performing the 5A’s included: awareness of USPHS guidelines, not endorsing time factors as a barrier, and physician characteristics (i.e., medical specialty). Interesting findings were additionally noted with respect to patient barriers and perceived effectiveness of pharmacotherapy. Each of these merits’ further discussion.
Very few physicians (18%) reported implementing the USPHS clinical guidelines into their practice. This gap in guideline utilization contributes to fewer physicians Assisting their patients with cessation plans and following up. There is a critical need to increase awareness, and especially utilization, of these guidelines. This could be accomplished through efforts of professional organizations (e.g., American College of Physicians, American Association of Family Practice.), as well as brief physician training activities and academic detailing interventions, which have been shown to increase the use of guidelines-based strategies, such as counseling, and may improve cessation rates.23,24
Consistent with previous research, time factors (e.g., lack of time or competing priorities), were the most commonly reported barriers to treatment delivery.25 To address these, the Centers for Disease Control and Prevention’s Ask–Advise–Refer model26 or Ask–Advise–Connect27 would reduce the burden on providers to deliver treatment themselves through referral to evidence-based community resources (e.g., quitlines or in-person specialty tobacco treatment programs). Often, physicians are not fully aware of public cessation resources,25 and interventions designed to connect physicians to state-level quitlines have been shown to be feasible and potentially cost effective.28 Interestingly, patient factors (disinterest or resistance) were associated with higher rates of Asking or Assisting. It is possible that physicians faced with resistant patients could feel compelled to make a renewed effort to inquire about tobacco use and provide assistance.
Physician characteristics (e.g., specialty and graduation year) were predictors of tobacco treatment implementation. Compared with family physicians, pulmonologists reported higher rates of implementation of each of the 5A’s except Arrange, whereas cardiologists and internists had higher rates of some of these activities. Oncologists also had higher rates of Arrange. These findings are consistent with previous studies, showing some specialties having higher rates of tobacco treatment resource awareness,29 and studies done among primary care physicians showed that internists were most active in smoking-cessation counseling whereas obstetrician–gynecologists were least active.20 Perhaps specialties that treat more tobacco-related disease (pulmonologists, cardiologists, oncologists, and internists) place tobacco treatment at the forefront of their practice. Physicians graduating before 1990 had higher rates of implementation some of guideline practices. Perhaps younger physicians are entering medicine at a time when smoking rates are at their lowest levels. Those who practiced during times when smoking rates were much higher may view tobacco use as a more pressing public health crisis.
Finally, higher perceived effectiveness of pharmacotherapy correlated with higher arranging follow-up. Regarding specific pharmacotherapies, prescription NRTs (e.g., nicotine oral inhaler and nasal spray) were perceived to be the least effective despite no supporting evidence. Although varenicline has been shown in numerous studies to be the most effective single tobacco treatment medication,30 the difference in effectiveness is relatively small among NRTs. These inconsistencies in perception are unfounded in the literature and may reflect an absence of familiarity with inhaled or nasal forms of NRT.5 Previous studies have indicated that non-nicotine prescription medications, such as bupropion, were perceived as most effective, whereas nicotine nasal spray was considered least effective.18 It is vital that physicians have accurate information that all of the 7 FDA-approved pharmacotherapies are safe and effective, regardless of their market share or lack of advertising.
Limitations
This study has a few limitations. First, data are self-reported and may be subject to self-report bias. Second, delivery of the 5A’s was assessed from the perspective of the physician, which again is subject to bias, especially as physicians understand what the expected counseling behaviors should be. Other approaches to assess physician cessation practices include direct observation,31 patient self-report,32 and chart review,33 which may yield different estimates. Third, data reduction techniques were used for the logistic regression. Though data reduction increases interpretability, there is the possibility of the loss of granular detail. In addition, the questions about engagement in the 5A’s did not provide a ref period (e.g., in the past year). Fouth, although respondents differed minimally from non-respondents with respect to sex and age, non-respondents may differ from participating physicians in other ways. As sampling probabilities varied by specialty, the overall sample was not nationally representative, but was randomly drawn and analyses were adjusted by specialty. Given that topic salience is one of the strongest predictors of survey response, the findings in this study may represent an upper bound for the delivery of the 5A’s.
CONCLUSIONS
Physician knowledge, beliefs, and practices about tobacco treatment seem to deviate substantially from best practices, and vary by specialty. The results of this national survey highlight the need for increased implementation of the latest guidelines for tobacco cessation and evidence-based treatments, including community-based resources. With greater understanding and enhanced training, physicians will be more prepared to comprehensively and effectively address tobacco use.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by grant 1R01CA190444-01A1 from the National Cancer Institute. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or U.S. Food and Drug Administration.
The funder had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults—United States, 2019. MMWR Morb Mortal Wkly Rep 2020;69(46):1736–1742. 10.15585/mmwr.mm6946a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park ER, Gareen IF, Japuntich S, et al. Primary care provider-delivered smoking cessation interventions and smoking cessation among participants in the National Lung Screening Trial. JAMA Intern Med 2015;175(9):1509–1516. 10.1001/jamainternmed.2015.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rigotti NA, Thorndike AN. Reducing the health burden of tobacco use: what’s the doctor’s role? Mayo Clin Proc 2001;76(2):121–123. 10.1016/s0025-6196(11)63116-9. [DOI] [PubMed] [Google Scholar]
- 4.Franken A. Reducing the disease burden of tobacco use: the role of health reform and beyond. Am J Prev Med 2010;39(6 suppl 1):S83–S84. 10.1016/j.amepre.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: HHS; 2008. [Google Scholar]
- 6.Conroy MB, Majchrzak NE, Regan S, Silverman CB, Schneider LI, Rigotti NA. The association between patient-reported receipt of tobacco intervention at a primary care visit and smokers’ satisfaction with their health care. Nicotine Tob Res 2005;7(suppl 1):S29–S34. 10.1080/14622200500078063. [DOI] [PubMed] [Google Scholar]
- 7.Smith D. Health care consumer’s use and trust of health information sources. J Commun Healthc. 2011;4(3):200–210. 10.1179/1753807611Y.0000000010. [DOI] [Google Scholar]
- 8.Wackowski OA, Bover Manderski MT, Delnevo CD. Smokers’ sources of e-cigarette awareness and risk information. Prev Med Rep 2015;2:906–910. 10.1016/j.pmedr.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. public health service report. Am J Prev Med 2008;35(2):158–176. 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dixon LB, Medoff D, Goldberg R, et al. Is implementation of the 5 A’s of smoking cessation at community mental health centers effective for reduction of smoking by patients with serious mental illness? Am J Addict 2009;18(5):386–392. 10.3109/10550490903077747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quinn VP, Stevens VJ, Hollis JF, et al. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am J Prev Med 2005;29(2):77–84. 10.1016/j.amepre.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Chase EC, McMenamin SB, Halpin HA. Medicaid provider delivery of the 5A’s for smoking cessation counseling. Nicotine Tob Res 2007;9(11):1095–1101. 10.1080/14622200701666344. [DOI] [PubMed] [Google Scholar]
- 13.Martínez C, Castellano Y, Andrés A, et al. Factors associated with implementation of the 5A’s smoking cessation model. Tob Induc Dis 2017;15(1):41. 10.1186/s12971-017-0146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith TW. A revised review of methods to estimate the status of cases with unknown eligibility. Chicago, IL: University of Chicago, National Opinion Research Center; 2009. [Google Scholar]
- 15.The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th edition. AAPOR; 2016. [Google Scholar]
- 16.Delnevo CD, Singh B. The effect of a web-push survey on physician survey responses rates: a randomized experiment. Surv Pract 2021;14(1). 10.29115/sp-2021-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinberg MB, Zimmermann MH, Gundersen DA, Hart C, Delnevo CD. Physicians’ perceptions regarding effectiveness of tobacco cessation medications: are they aligned with the evidence? Prev Med 2011;53(6):433–434. 10.1016/j.ypmed.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Steinberg MB, Delnevo CD. Physician beliefs regarding effectiveness of tobacco dependence treatments: results from the NJ Health Care Provider Tobacco Survey. J Gen Intern Med 2007;22(10):1459–1462. 10.1007/s11606-007-0282-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of US health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res 2010;12(7):724–733. 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldstein MG, DePue JD, Monroe AD, et al. A population-based survey of physician smoking cessation counseling practices. Prev Med 1998;27(5):720–729. 10.1006/pmed.1998.0350. [DOI] [PubMed] [Google Scholar]
- 21.Solberg LI, Asche SE, Boyle RG, Boucher JL, Pronk NP. Frequency of physician-directed assistance for smoking cessation in patients receiving cessation medications. Arch Intern Med 2005;165(6):656–660. 10.1001/archinte.165.6.656. [DOI] [PubMed] [Google Scholar]
- 22.Kruger J, O’Halloran A, Rosenthal AC, Babb SD, Fiore MC. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health. 2016;16(1):141. 10.1186/s12889-016-2798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bauer A, Brenner L, Moser J, Trudzinski F, Köllner V, Bals R. The effects of a short-term physician training on smoking cessation in a university pulmonary department. Ger Med Sci 2020;18:Doc06. 10.3205/000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goldstein MG, Niaura R, Willey C, et al. An academic detailing intervention to disseminate physician-delivered smoking cessation counseling: smoking cessation outcomes of the Physicians Counseling Smokers Project. Prev Med 2003;36(2):185–196. 10.1016/s0091-7435(02)00018-x. [DOI] [PubMed] [Google Scholar]
- 25.Marcy TW, Skelly J, Shiffman RN, Flynn BS. Facilitating adherence to the tobacco use treatment guideline with computer-mediated decision support systems: physician and clinic office manager perspectives. Prev Med 2005;41(2):479–487. 10.1016/j.ypmed.2004.11.026. [DOI] [PubMed] [Google Scholar]
- 26.Clinical tools. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/basic_information/for-health-care-providers/clinical-tools/index.html. Updated 2020. Accessed January 14, 2021. [Google Scholar]
- 27.Vidrine JI, Shete S, Cao Y, et al. Ask-advise-connect: a new approach to smoking treatment delivery in health care settings. JAMA Intern Med 2013;173(6):458–464. 10.1001/jamainternmed.2013.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bentz CJ, Bayley KB, Bonin KE, Fleming L, Hollis JF, McAfee T. The feasibility of connecting physician offices to a state-level tobacco quit line. Am J Prev Med 2006;30(1):31–37. 10.1016/j.amepre.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 29.Steinberg MB, Alvarez MS, Delnevo CD, Kaufman I, Cantor JC. Disparity of physicians’ utilization of tobacco treatment services. Am J Health Behav 2006;30(4):375–386. 10.5993/ajhb.30.4.4. [DOI] [PubMed] [Google Scholar]
- 30.Leone FT, Zhang Y, Evers-Casey S, et al. Initiating pharmacologic treatment in tobacco-dependent adults. an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 2020;202(2):e5–e31. 10.1164/rccm.202005-1982st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellerbeck EF. Direct observation of smoking cessation activities in primary care practice. J Fam Pract 2001;50(8):688–693. [PubMed] [Google Scholar]
- 32.Stevens VJ, Solberg LI, Quinn VP, et al. Relationship between tobacco control policies and the delivery of smoking cessation services in nonprofit HMOs. JNCI Monographs. 2005;2005(35):75–80. 10.1093/jncimonographs/lgi042. [DOI] [PubMed] [Google Scholar]
- 33.Williams RJ, Masica AL, McBurnie MA, et al. Documentation of the 5 As for smoking cessation by PCPs across distinct health systems. Am J Manag Care. 2014;20(3):e35–e42. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


