Abstract
Introduction:
A growing number of state legislatures have passed laws that restrict access to abortion care after a specified gestational age (gestational age limit laws). The impact of these laws on maternal and child population health outcomes and inequities is unknown. The objective of this study is to determine whether states that implement gestational age limit laws experience subsequent changes in rates of infant mortality.
Methods:
Using U.S. population-based data from the National Center for Health Statistics Linked Infant Birth-Death Files (2005–2017), difference-in-differences models were estimated using multivariable linear regressions to compare trends in infant mortality (all-cause and cause-specific rates) in states with gestational age limit laws relative to states without such laws. Models stratified by maternal racial/ethnic group explored racial heterogeneity in the law’s impact. Data were analyzed in 2020.
Results:
This study included 16,232,133 births in states that enacted a gestation age limit abortion law and 36,472,309 births in states that did not from 2005 to 2017. In difference-in-difference analyses, gestational age limit laws were associated with 0.23 excess infant deaths per 1,000 live births (95% CI=0.09, 0.37, p<0.01). In cause-specific analyses, gestational age limit laws were associated with 0.10 additional infant deaths due to congenital anomalies per 1,000 live births (95% CI=0.03, 0.17, p=0.01). Associations between gestational age limit laws and infant mortality in models stratified by maternal racial/ethnic group were not statistically significant.
Conclusions:
Based on data from 2005 to 2017, states that enacted gestational age limit abortion laws subsequently experienced increased infant mortality rates.
INTRODUCTION
In recent years, an unprecedented number of abortion regulations have been introduced, and passed, in state legislatures across the U.S.1 The result is an increasingly restrictive climate related to reproductive health services and a patchwork of limitations, parameters, and prohibitions that differs from state to state. One of the most commonly enacted type of regulation restricts abortion at a specific point during pregnancy, known as a gestational age limit.2 Although the U.S. Supreme Court recognizes the constitutional right to abortion, it holds that individual states may ban the procedure after fetal viability (typically ranging from 24 to 28 weeks from the last menstrual period), as determined on an individual basis and with some medical exceptions.2 To date, states that attempt to limit abortion in the first trimester have been stopped by court order. However, currently 22 states have successfully implemented laws that limit or prohibit abortion at a specified gestational age in the second trimester, most commonly after 22 weeks from the last menstrual period or 20 weeks postfertilization.2 In 2019 alone, 9 states enacted gestational age limits.1
Women who seek abortions at later gestational ages are typically those who were unable to obtain earlier care owing to lack of financial resources, transportation, child care, and other constraints.3,4 Additionally, most women who receive a diagnosis of severe fetal anomaly seek abortion care which, given the timing of diagnosis in the second trimester, may also be at later gestational ages. Previous evidence finds that gestational age limit laws effectively reduce access to abortion services and decrease the number of abortions at later gestational ages. A study using 2008 data estimated that because of gestational age limits at abortion facilities, >4,000 women annually are denied abortion and must carry unwanted pregnancies to term.5 This number is likely to have increased considerably since then, as 16 states have enacted or increased gestational age limits over the last decade. More recently, Hall et al.6 evaluated Georgia’s enactment of a gestational age limit and found it decreased abortions after 20 weeks from the last menstrual period, as was its intent. They conclude that the corresponding increase in unintended births—which have been associated with adverse maternal and infant health outcomes7,8—may be exacerbating health disparities and negatively impacting the health and economic security of women in the state.6
Infant mortality is a longstanding indicator of population health and societal well-being. In the U.S., infant mortality has steadily declined over the past decade but remains higher than almost all European countries at 5.7 deaths per 1,000 births and is accompanied by marked racial inequities.1,9 As with abortion regulations, prevalence varies dramatically by state,9 but the degree to which state abortion laws directly influence state trends in infant mortality is limited. Krieger and colleagues10 demonstrated that states that legalized abortion access in 1970 experienced more rapid decline in infant mortality between 1970 and 1973. Additionally, increased state funding for abortion services since 2000 has been shown to be associated with reduced risk of infant mortality, especially among low-income women of color.11 More recently, a cross-sectional study from 2008 to 2010 found the odds of infant mortality were higher in states with a greater number of laws that restrict access to abortion.12
The objective of this quasi-experimental study is to evaluate the association between gestational age limit laws and state-level rates of infant mortality in the U.S. over the 2005–2017 period. The primary hypothesis is that states implementing a gestational age limit law will experience subsequently higher rates of infant mortality than they would have in the absence of these laws. In addition, given that abortion restrictions disproportionately harm Black women,13,14 a secondary hypothesis anticipates increased racial inequities in states with gestational age limits relative to states without such laws.
METHODS
Study Sample
This analysis utilized the National Center for Health Statistics’ period-linked birth and infant death files for 2005–2017, which include records for all live births occurring in the U.S. and linked death records for those that ended in death within 1 year. Annual infant mortality rates were calculated as deaths per 1,000 live births by maternal state of residence and year from 2005 to 2017 for the total population as well as stratified by maternal race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic). In addition to all-cause mortality, separate models were fit for the 2 leading subgroups of cause-specific deaths: preterm-related conditions and congenital anomalies. These subgroups of death were identified by applying the updated Dollfus infant death classification scheme developed by Nakamura et al.15 based on ICD-10 codes for underlying cause of death.
Measures
The gestational age limit abortion laws were defined as any policy implemented at the state level that prohibited abortion based on gestational age. Data on whether each state had such a restriction in place in January of each year from 2005 to 2017 were abstracted from the Guttmacher Institute’s state policy status reports.16
Data on important confounding factors came from multiple sources. Controls included the percentage of women who gave birth within their state of residence and percentage of births by maternal age from annual natality files provided by the National Center for Health Statistics. Also included were the following annual state-level sociodemographic and economic characteristics obtained from the U.S. Census’ American Community Survey: total population, percentage of the population living in urban counties, median household income, percentage of the population living below the federal poverty level, and percentage of the population that is non-Hispanic White. Unemployment rate from the Bureau of Labor Statistics was included as an additional indicator of state economic conditions. Medicaid expenditures by state and year were obtained from the Regional Economic Information System of the U.S. Bureau of Economic Analysis, and annual female obesity prevalence and female smoking rates were obtained from the Behavioral Risk Surveillance System. Finally, in order to capture concurrent policy influence on the state’s maternal population health, models included an indicator for whether the state had in effect a waiver or state plan amendment to expand Medicaid eligibility for family planning services.17,18 Means for all variables were generated at the state-year level and merged using state and year indicators.
Statistical Analysis
Descriptive statistics characterized states that never enacted a gestational age law and states that ever imposed a gestational age law or always had one in effect from 2005 to 2017. The analytic approach employed a differences-in-differences design with demeaned data at the state level to control for unobserved variation between states and infant mortality, and demeaned at the year level to control for secular changes in infant mortality rates at the national level. Multivariable linear regression models estimated infant mortality rates for the total population as well as for White, Black, and Hispanic infants separately. Each model was weighted by the number of women of reproductive age represented in the regression. The coefficient of interest was an indicator variable that took the value of one when a state had a gestation age limit law. To control for the serially correlated nature of error terms when observing data over time, SEs were clustered at the state level. Results include coefficients and robust 95% CIs from both crude models (controlled only for state and year) and fully adjusted models (including state, year, and all aforementioned covariates). Coefficients can be interpreted as changes in rates of infant mortality (infant deaths per 1,000 live births) associated with implementation of the gestational age limit law.
The parallel trends assumption of differences-in-differences assumes that trends in the outcome in treated states and control states would have remained parallel in the absence of treatment (implementation of the law). To examine this assumption, infant mortality by year was plotted separately for states that imposed gestational age limits on abortion and those states that did not. A placebo test was performed by examining the association between the state gestational age limit law and infant mortality due to injury sustained in transportation accidents (ICD-10 codes V01–V99). As there is no reason to suppose a relationship between accidents and gestation age laws, a well-specified differences-in-differences model should not return a statistically significant result. All analyses were conducted in Stata, version 15 in 2020.
RESULTS
From 2005 to 2017, a total of 13 states enacted a gestational age limit abortion law and 1 (North Carolina) had the law in effect prior to 2005 (Table 1.) All prohibited abortion after 22 weeks from the last menstrual period with the exception of Florida’s law, which prohibited abortion 24 weeks after the last menstrual period. The prevalence of infant mortality was higher in states with a gestational age limit: 7.23 (SD=1.24) infant deaths per 1,000 live births compared with 6.08 (SD=1.31) infant deaths per 1,000 live births in states without such a law. Infant mortality declined over the study period for states that implemented a gestational age limit and those that did not, but mortality rates were constantly higher for states with restrictions than those without across the study years (Figure 1). Table 2 includes descriptive differences in maternal, infant, and state characteristics between states that ever enacted the law and those that did not.
Table 1.
States With a Gestational Age Limit Law and First Full Year in Effect, 2005‒2017a
| State | First full year with law in effect |
|---|---|
| Alabama | 2012 |
| Arkansas | 2013 |
| Florida | 2014 |
| Indiana | 2011 |
| Kansas | 2011 |
| Louisiana | 2012 |
| Mississippi | 2015 |
| Nebraska | 2010 |
| North Dakota | 2013 |
| Oklahoma | 2011 |
| Texas | 2013 |
| West Virginia | 2016 |
| Wisconsin | 2015 |
North Carolina had the law in effect prior to 2005, the first year of data used in this study. Births in North Carolina are included in the ever imposed a gestational age limit law group.
Figure 1.
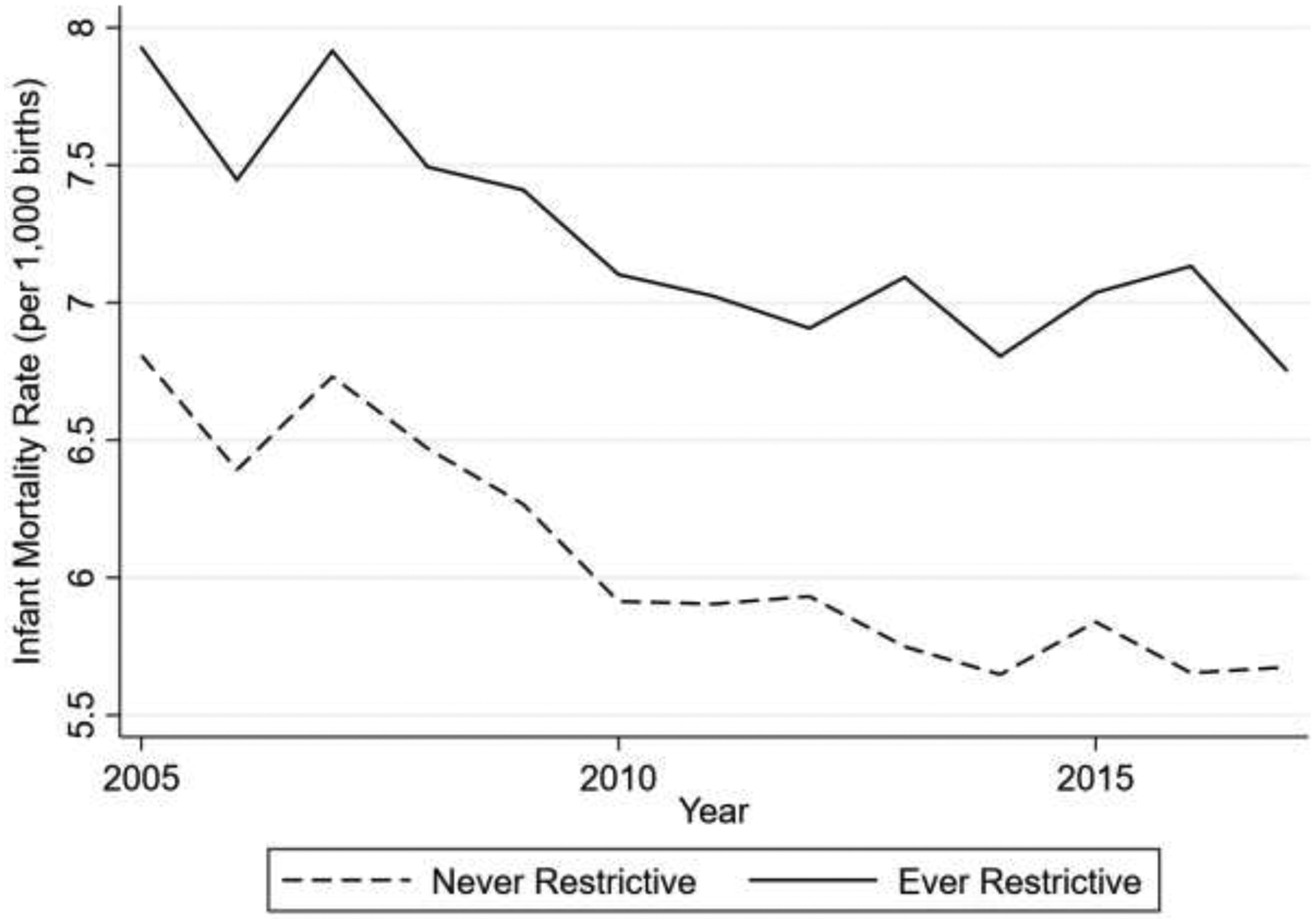
Trends in unadjusted infant mortality rates in states that enacted a gestational age limit law and states that never enacted a gestational age limit law, 2005‒2017.
Table 2.
Maternal, Infant, and State Characteristics by State Policy Status, 2005‒2017
| Characteristic | Never imposed gestational age limit (N=481 state- months, 36,472,309 total births) Mean (SD) |
Ever imposed gestational age limit (N=182 state-months, 16,232,133 total births) Mean (SD) |
|---|---|---|
| Maternal age, years (% of births) | ||
| 10–19 | 7.66 (2.68) | 9.77 (3.13) |
| 20–29 | 51.81 (5.79) | 57.35 (3.48) |
| 30–39 | 37.32 (6.80) | 31.00 (5.49) |
| 40–49 | 2.79 (0.89) | 1.89 (0.50) |
| Race (% of births) | ||
| Non-Hispanic White | 61.18 (19.20) | 63.90 (15.10) |
| Non-Hispanic Black | 11.78 (11.78) | 17.20 (12.65) |
| Hispanic | 16.27 (12.77) | 13.51 (11.87) |
| Birth occurred in maternal state of residence (% of births) | 96.28 (3.11) | 96.59 (2.78) |
| Infant mortality rate (per 1,000 births) | 6.08 (1.31) | 7.23 (1.24) |
| Infant mortality due to congenital anomalies (per 1,000 births) | 1.22 (0.33) | 1.50 (0.26) |
| Infant mortality due to preterm birth (per 1,000 births) | 1.68 (0.59) | 2.03 (0.55) |
| Infant mortality due to external causes (per 1,000 births) | 0.40 (0.25) | 0.48 (0.24) |
| Total state population | 5,898,636 (6,822,774) | 6,611,685 (6,937,908) |
| Residence in urban county (% of total population) | 76.62 (15.98) | 67.46 (11.80) |
| Non-Hispanic white (% of total population) | 76.74 (14.76) | 78.02 (10.16) |
| Female obesity prevalence | 26.07 (3.73) | 30.21 (4.02) |
| Median household income (2011 USD) | 54,966 (9,333) | 45,791 (6,031) |
| Income below Federal Poverty Level (% of total population) | 13.32 (3.01) | 15.43 (3.31) |
| Medicaid expenditure per capita (2011 USD) | 2,870 (1,143) | 2,407 (549) |
USD, U.S. Dollar.
Table 3 provides the difference-in-difference results for all-cause and cause-specific mortality in association with gestational age limit laws. These results indicated that gestational age limit laws were associated with 0.23 additional infant deaths per 1,000 live births (95% CI=0.09, 0.37, p<0.01). This represents an increase of 3.6% over the average infant mortality rate. Infant mortality due to congenital anomalies was increased by 0.10 additional infant deaths per 1,000 live births in association with enactment of a gestational age limit law (95% CI=0.03, 0.17, p=0.01). Adjusted estimates for deaths due to prematurity were not statistically significant (0.07 deaths due to prematurity and related conditions per 1,000 live births, 95% CI= −0.02, 0.16, p=0.15).
Table 3.
Associations Between Gestational Age Limit Laws and Infant Mortality (Deaths Per 1,000 Live Births)a
| Model | All-cause infant mortality | Congenital anomalies | Prematurity and related conditions | |||
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | ||||
| Crude | Adjusted | Crude | Adjusted | Crude | Adjusted | |
| Total population | 0.29 (0.18, 0.39) | 0.23 (0.08, 0.37) | 0.12 (0.05, 0.18) | 0.10 (0.03, 0.17) | 0.09 (0.02, 0.17) | 0.07 (−0.02, 0.16) |
| Baseline (mean infant mortality rate in untreated) | 6.31 | 6.31 | 1.27 | 1.27 | 1.75 | 1.75 |
| Percent increase over baseline | 4.6% | 3.6% | 9.4% | 7.9% | 5.1% | 4.0% |
| Maternal race/ethnicity | ||||||
| Non-Hispanic Black | 0.42 (0.02, 0.82) | 0.47 (−0.03, 0.96) | 0.08 (−0.09, 0.24) | 0.16 (−0.05, 0.37) | 0.07 (−0.30, 0.44) | −0.01 (−0.43, 0.40) |
| Baseline (mean infant mortality rate in untreated) | 11.24 | 11.24 | 1.63 | 1.63 | 3.82 | 3.82 |
| Percent increase over baseline | 3.7% | 4.2% | 4.9% | 9.8% | 1.8% | −0.3% |
| Hispanic | −0.27 (−0.93, 0.39) | −0.08 (−0.83, 0.67) | 0.04 (−0.43, 0.51) | ≤0.01 (−0.51, 0.51) | 0.02 (−0.17, 0.20) | 0.08 (−0.09, 0.26) |
| Baseline (mean infant mortality rate in untreated) | 5.69 | 5.69 | 2.34 | 2.34 | 1.66 | 1.66 |
| Percent increase over baseline | −4.7% | −1.6% | 1.7% | 0.8% | 1.2% | 4.8% |
| Non-Hispanic White | 0.14 (−0.01, 0.28) | 0.10 (−0.07, 0.28) | 0.05 (−0.02, 0.13) | 0.05 (−0.03, 0.14) | 0.06 (−0.02, 0.13) | 0.04 (−0.05, 0.13) |
| Baseline (mean infant mortality rate in untreated) | 5.12 | 5.12 | 1.14 | 1.14 | 1.28 | 1.28 |
| Percent increase over baseline | 2.7% | 2.1% | 4.4% | 4.4% | 4.7% | 3.1% |
Beta coefficients were calculated using linear regression models (N=663). Crude regressions controlled for state and year only. Adjusted regressions additionally included all state-level sociodemographic and economic characteristics outlined in Table 1 with SEs clustered at the state level.
Table 3 additionally provides difference-in-difference estimates for models stratified by maternal race/ethnicity. Coefficients for non-Hispanic Black and non-Hispanic White infant mortality remained positive but were not statistically significant (0.47 non-Hispanic Black infant deaths per 1,000 live births, 95% CI=0.02, 0.82, p=0.06; 0.14 non-Hispanic White infant deaths per 1,000 live births, 95% CI= −0.01, 0.28, p=0.09). There were no statistically significant associations with cause-specific mortality for any racial/ethnic subgroup.
Figure 1 shows parallel trends between states that enacted gestational age restrictions on abortion access and states that did not. The first full-year change in policy status was Nebraska in 2010, showing a parallel trend between treatment and control states before this date. Finally, the placebo tests examining associations between gestational age restrictions and mortality due to transportation accidents resulted in coefficients that were not statistically significant (Appendix Table 1), as expected.
DISCUSSION
This study evaluated state laws that restrict access to abortion based on gestational age and found that these policies are associated with increased infant mortality. There was no evidence of heterogeneity by maternal race/ethnicity, indicating that the policy’s association with infant mortality was not specific to 1 racial/ethnic group.
The total additional infant deaths associated with these laws can be estimated by applying the marginal estimates to the number of infant births in affected states. In 2017, there were 1,209,752 births in states with gestational age limits. Applying the main estimate of 0.23 excess infant deaths per 1,000 live births arrives at (0.23 × 1,209,752/1,000) 278 additional infant deaths in 2017 attributable to gestational age limits on access to abortion care.
Research on the population health impact of laws that prohibit abortion after a specified gestational age is sparse, but is beginning to reveal the adverse consequences for both maternal and child health. The landmark Turnaway Study, which compared the experience of people denied an abortion owing to a 20-week gestational limit to those who received an abortion at just before 20 weeks, documented elevated risk for numerous social, economic, physical, and mental health adversities as a result.19,20 Women denied an abortion after a gestational age limit were forced to continue the pregnancy, placing them at risk for morbidities and mortality associated with pregnancy and childbearing that they would not have otherwise experienced.21 Applying the same quasi-experimental design as the present study, Hawkins and colleagues22 evaluated the impact of gestational age limit laws on state trends in maternal mortality and found a 38% increase post-implementation. They reported an association driven by non-Hispanic White women in particular, although mortality rates were elevated across all racial/ethnic groups.22
Coupled with the evidence that gestational age limit laws restrict access to wanted and needed abortions,6 these findings suggest infants born as a result of these laws are at greater risk of death. Mechanistically, these laws may be linked to increased rates of infant mortality in several ways. Research suggests that women most likely to be impacted by gestational age limit laws are those that lack the resources and opportunities to access abortion as early as desired, owing to financial, logistical, and other social constraints.3,4 These same hardships are likely to persist into and be exacerbated by maternity, such that many women forced to continue unwanted pregnancies as a result of these laws may experience multiple barriers to adequate prenatal, postpartum, and other health care for themselves and their infants, and may lack sufficient income to cover living expenses and other resources necessary to support the optimal health of a newborn.12,23 Compounding these material hardships are the psychosocial stress and other detrimental mental health consequences of constrained choice. Evidence highlights elevated psychological distress and overall mental health impact of navigating barriers to abortion access, particularly among those denied abortion.4,19,24 A large body of literature links the physiological response to psychosocial stress during pregnancy with adverse reproductive health outcomes25–30 and postpartum depression—shown to be higher in states that restrict funding for abortion31—has been linked to infant mortality. Finally, these laws may be directly linked to infant mortality due to congenital anomalies by restricting access to abortion among women who receive a diagnosis of fetal anomaly at or around the time of the gestational limit.
Limitations
This study must be interpreted in the light of its limitations. The state-year data structure allowed for meaningfully control for variables that reflect overall states’ social and health environments; however, it was not possible to control for individual income, family income, or other individual-level sociodemographic characteristics and economic circumstances that may be related to risk of infant death but are not available on birth or infant death records. Although models included controls for state population-level economic conditions that may influence financial access to abortion care independent of state law, there are additional components of access (such as number of clinics and their geographic accessibility) that may impact women’s ability to obtain an abortion regardless of gestational age limits that were not included. As hypothesized, there is a significant crude association between the gestational age limit laws and infant deaths due to prematurity. Following addition of a rich set of controls, this association is no longer significant as the SE window expands. The point estimates of the models with and without controls are similar, suggesting that this may be due to a lack of power to estimate these effects in the version of the model that includes controls. Missing values in the vital records data may have generated selection bias; however, this process led to the exclusion of a negligible proportion of the total observations (<0.5%) and no significant differences were observed in missing value rates between states that enacted and those that never enacted restrictions based on gestational age. Further, if states often enact other legislation inimical to infant health at the same time they pass restrictions on abortion care based on gestational age estimates may recover the effect of this bundle of policies. Finally, exposure to the policy was defined as the first full year the policy was in effect. This may have introduced misclassification bias in cases where the effective date was mid-year, or in cases where providers began adhering to the law as soon as it was enacted but before it was in effect. This potentiality would bias the estimations toward 0, and away from finding any impact of the laws on infant health.
CONCLUSIONS
Based on data from 2005 to 2017, state laws that restrict access to abortion based on gestational age are significantly associated with infant mortality. With a direct and negative influence on trends in infant mortality, this evidence is relevant to the growing number of state legislative and judicial actions focusing on gestational age limit policies and efforts aimed at improving maternal and child population health in the U.S.
Supplementary Material
ACKNOWLEDGMENTS
The research presented in this paper is that of the authors and does not reflect the official policy of NIH. This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant number R01HD096070. The funding source had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication. All authors had full access to all the data in the study and M. Wallace takes responsibility for the integrity of the data and the accuracy of the data analysis. MW, KT, and CS conceived of and designed the study, DK and CS lead the analysis, DK, CS, MW, DV, and KT interpreted analytic results. MW and DK and DV drafted the initial manuscript. All authors reviewed and revised the manuscript and approved the final version. No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Nash E, Mohammed L, Cappello O, Naide S. State policy trends 2019: a wave of abortion bans, but some states are fighting back. https://www.guttmacher.org/article/2019/12/state-policy-trends-2019-wave-abortion-bans-some-states-are-fighting-back. Published 2019. Accessed January 13, 2021.
- 2.Guttmacher Institute. State bans on abortion throughout pregnancy. https://www.guttmacher.org/state-policy/explore/state-policies-later-abortions#. Published 2021. Accessed January 13, 2021.
- 3.Foster DG, Kimport K. Who seeks abortions at or after 20 weeks? Perspect Sex Reprod Health. 2013;45(4):210‒218. 10.1363/4521013. [DOI] [PubMed] [Google Scholar]
- 4.Foster DG. The Turnaway Study: Ten Years, a Thousand Women, and the Consequences of Having—or Being Denied—an Abortion. New York, NY: Scribner; 2020. [Google Scholar]
- 5.Upadhyay UD, Weitz TA, Jones RK, Barar RE, Foster DG. Denial of abortion because of provider gestational age limits in the United States. Am J Public Health. 2014;104(9):1687‒1694. 10.2105/ajph.2013.301378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall KS, Redd S, Narasimhan S, et al. Abortion trends in Georgia following enactment of the 22-week gestational age limit, 2007‒2017. Am J Public Health. 2020;110(7):1034‒1038. 10.2105/ajph.2020.305653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohllajee AP, Curtis KM, Morrow B, Marchbanks PA. Pregnancy intention and its relationship to birth and maternal outcomes. Obstet Gynecol. 2007;109(3):678‒686. 10.1097/01.aog.0000255666.78427.c5. [DOI] [PubMed] [Google Scholar]
- 8.Orr ST, Miller CA, James SA, Babones S. Unintended pregnancy and preterm birth. Paediatr Perinat Epidemiol. 2000;14(4):309‒313. 10.1046/j.1365-3016.2000.00289.x. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Infant Mortality. 2020; https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm. Published 2020. Accessed January 13, 2021.
- 10.Krieger N, Gruskin S, Singh N, et al. Reproductive justice and the pace of change: socioeconomic trends in US infant death rates by legal status of abortion, 1960‒1980. Am J Public Health. 2015;105(4):680‒682. 10.2105/ajph.2014.302401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger N, Gruskin S, Singh N, et al. Reproductive justice & preventable deaths: state funding, family planning, abortion, and infant mortality, US 1980‒2010. SSM Popul Health. 2016;2:277‒293. 10.1016/j.ssmph.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pabayo R, Ehntholt A, Cook DM, Reynolds M, Muennig P, Liu SY. Laws restricting access to abortion services and infant mortality risk in the United States. Int J Environ Res Public Health. 2020;17(11):3773. 10.3390/ijerph17113773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dehlendorf C, Harris LH, Weitz TA. Disparities in abortion rates: a public health approach. Am J Public Health. 2013;103(10):1772‒1779. 10.2105/ajph.2013.301339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen SA. Abortion and women of color: the bigger picture. Guttmacher Policy Review. 2008;11(3):2‒12. [Google Scholar]
- 15.Nakamura AM, Dove MS, Minnal A, Damesyn M, Curtis MP. Infant mortality: development of a proposed update to the Dollfus Classification of Infant Deaths. Public Health Rep. 2015;130(6):632‒642. 10.1177/003335491513000613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guttmacher Institute. An Overview of Abortion Laws. https://www.guttmacher.org/state-policy/explore/overview-abortion-laws. Published 2021. Accessed January 20, 2021.
- 17.Guttmacher Institute. Medicaid Family Planning Eligibility Expansions. https://www.guttmacher.org/state-policy/explore/medicaid-family-planning-eligibility-expansions#. Published 2021. Accessed April 5, 2021.
- 18.Kaiser Family Foundation. States that have expanded eligibility for coverage of family planning services under Medicaid. https://www.kff.org/medicaid/state-indicator/family-planning-services-waivers/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Published 2020. Accessed April 5, 2021.
- 19.Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74(2):169‒178. 10.1001/jamapsychiatry.2016.3478. [DOI] [PubMed] [Google Scholar]
- 20.Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts S, Glymour MM. Socioeconomic outcomes of women who receive and women who are denied wanted abortions in the United States. Am J Public Health. 2018;108(3):407‒413. 10.2105/ajph.2017.304247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerdts C, Dobkin L, Foster DG, Schwarz EB. Side effects, physical health consequences, and mortality associated with abortion and birth after an unwanted pregnancy. Womens Health Issues. 2016;26(1):55‒59. 10.1016/j.whi.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Hawkins SS, Ghiani M, Harper S, Baum CF, Kaufman JS. Impact of state-level changes on maternal mortality: a population-based, quasi-experimental study. Am J Prev Med. 2020;58(2):165‒174. 10.1016/j.amepre.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Muennig P, Reynolds M, Jiao B, Pabayo R. Why is infant mortality in the United States so comparatively high? Some possible answers. J Health Polit Policy Law. 2018;43(5):877‒895. 10.1215/03616878-6951223. [DOI] [Google Scholar]
- 24.Biggs MA, Kaller S Ralph L Barriers accessing abortion care and their association with psychological well-being. Contraception. 2020;101(5):355. 10.1016/j.contraception.2020.03.010. [DOI] [Google Scholar]
- 25.Phelan AL, DiBenedetto MR, Paul IM, Zhu J, Kjerulff KH. Psychosocial stress during first pregnancy predicts infant health outcomes in the first postnatal year. Matern Child Health J. 2015;19(12):2587‒2597. 10.1007/s10995-015-1777-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shapiro GD, Fraser WD, Frasch MG, Seguin JR. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J Perinat Med. 2013;41(6):631‒645. 10.1515/jpm-2012-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hobel CJ. Stress and preterm birth. Clin Obstet Gynecol. 2004;47(4):856‒880. 10.1097/01.grf.0000142512.38733.8c. [DOI] [PubMed] [Google Scholar]
- 28.Harron K, Gilbert R, Fagg J, Guttmann A, van der Meulen J. Associations between pre-pregnancy psychosocial risk factors and infant outcomes: a population-based cohort study in England. Lancet Public Health. 2021;6(2):e97‒e105. 10.1016/s2468-2667(20)30210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White SE, Gladden RW. Maternal mental health and infant mortality for healthy-weight infants. Am J Manag Care. 2016;22(11):e389‒e392. [PubMed] [Google Scholar]
- 30.Sanderson CA, Cowden B, Hall DM, Taylor EM, Carpenter RG, Cox JL. Is postnatal depression a risk factor for sudden infant death? Br J Gen Pract. 2002;52(481):636‒640. [PMC free article] [PubMed] [Google Scholar]
- 31.Medoff MH. The relationship between restrictive state abortion laws and postpartum depression. Soc Work Public Health. 2014;29(5):481‒490. 10.1080/19371918.2013.873997. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


