Abstract
Sjögren's syndrome is a chronic autoimmune disorder characterized by mononuclear infiltration of exocrine glands, most commonly the lacrimal and salivary glands. While up to 34% of patients report bilateral parotid swelling, bilateral parotid sialolithiasis remains an exceptionally rare symptom. Here we present a patient who presents to the otolaryngology clinic with presentation of bilateral punctate parotid gland sialolithiasis prior to diagnosis of Sjögren's syndrome. Due to a wide array of clinical presentations frequently affecting the head and neck, otolaryngologists are often the initial providers for patients suffering from Sjögren's syndrome.
Keywords: Sialolithiasis, parotid gland, Salivary stones, Sjogren's Syndrome, Xerostomia
Introduction
Sjögren's syndrome is a chronic autoimmune disorder characterized by mononuclear infiltration of exocrine glands, most commonly the lacrimal and salivary glands. Resultant symptoms include keratoconjunctivitis sicca and xerostomia, which are often the initial presenting complaints of a patient with Sjögren's syndrome.
Furthermore, the disease can be associated with lithiasis of the major salivary glands occurring mainly in the submandibular gland (72%-94%) [1]. A much less common presentation includes bilateral parotid sialolithiasis with only a few case reports appearing in the current literature. The differential diagnosis for an adult with bilateral parotid sialolithiasis should include Sjögren's syndrome to aid in early recognition of the disease.
We present a new case of Sjögren's disease manifesting as bilateral calculi of the parotids, review clinical characteristics important for diagnosis, and discuss management as it relates to otolaryngology.
Case presentation
A 41-year-old female presented to the ENT clinic with a 2-year history of bilateral facial pain and swelling which worsens when eating. She attempted using warm compresses on her face with little relief of pain and swelling. She additionally reported a recent onset of dryness of the mouth and eyes. Her medical history was significant for hypothyroidism treated with Armour Thyroid medication. Family history included severe rheumatoid arthritis in her mother. She received no prior diagnosis or treatment related to her facial pain, keratoconjunctivitis sicca and xerostomia.
On physical examination, bilateral parotid regions were swollen without tenderness to palpation. Halitosis was appreciated with a paucity of saliva from the right or left Stensen's duct ostium upon bilateral parotid gland massage. She had no hearing loss, events of epistaxis, dental caries, or cervical lymphadenopathy. The rest of her ear, nose, and throat examination was largely unremarkable.
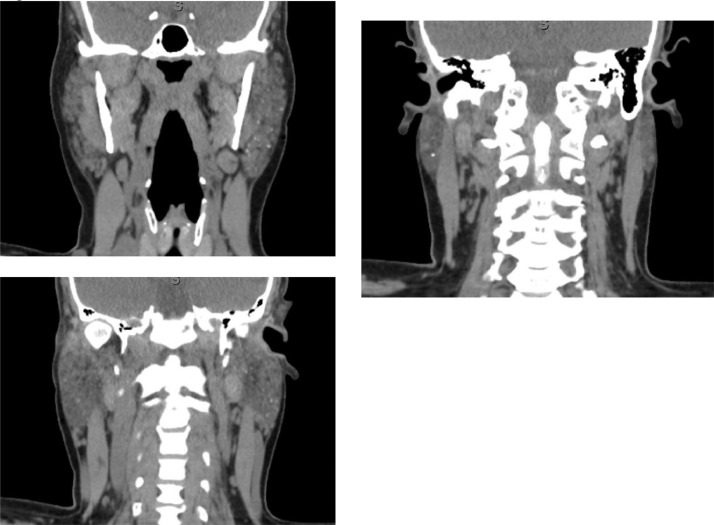
The patient brought in a recent set of laboratory blood tests and a computed tomography (CT) of her head for review, ordered previously by her primary care physician and outside otolaryngologist. Her lab report was remarkable for elevated levels of ANA 1:640 with a speckled pattern, anti-Ro/SSA and anti-La/SSB antibodies >8.0 and 0, respectively, ESR 32, and CRP 1.5. CT scan revealed the presence of multiple punctate calculi in bilateral parotid glands (Fig. 1).
Fig. 1.
CT soft-tissue neck revealing bilateral parotid gland sialolithiasis.
A presumptive diagnosis of Sjögren's syndrome was made based on the American-European Consensus Criteria for Sjögren's Syndrome. The patient's symptoms were managed conservatively with sialagogues and artificial tear drops, and she was advised to follow-up with a rheumatologist for further management of the disease. The patient was informed that she may return to the office should her rheumatologist require a minor salivary gland biopsy for diagnosis confirmation.
Discussion
Sjögren's syndrome is a chronic inflammatory autoimmune disease with a global prevalence of 61 per 100,000 people. The highest prevalence of the disease exists in Europe with 72 cases per 100,000 people. Women develop the disease much more frequently than men with an estimated ratio of 9:1. The mean age of disease diagnosis is 56, and another peak exists between ages 20 and 40. Due to the various manifestations of the disease, symptoms often occur years prior to the diagnosis.
The most common clinical manifestations of Sjogren's syndrome includes dry eyes and dry mouth which are reported in up to 98% of patients with the disease. Patients may also complain of a foreign-body sensation in the eyes, sensitivity to light and difficulty chewing due salivary gland dysfunction [2]. Compared with the general population, patients with Sjögren's syndrome have an increased prevalence of dental caries and early tooth decay due to the decrease in salivary amylase and carbonic anhydrase concentrations [3]. While up to 34% of patients report bilateral parotid swelling, bilateral parotid sialolithiasis remains an exceptionally rare symptom; however, it occurs with greater frequency in Sjögren's syndrome patients than in the public [1].
The American-European Consensus Group provides international classification criteria for the diagnosis of Sjögren's syndrome. Classification requires the presence of four out of the six criteria: ocular signs, ocular symptoms, oral signs, oral symptoms, salivary gland involvement, autoantibodies and/or histopathology of a lip biopsy showing focal lymphocytic sialadenitis for diagnosis [4]. Our patient presented with bilateral parotid sialolithiasis, xerostomia, keratoconjunctivitis sicca and positive serology for anti-Ro/SSa and anti-La/SSB. Four out of the six criteria were met making the diagnosis of Sjögren's syndrome likely.
Targeted therapy of Sjögren's syndrome is not presently available, and treatment is mainly symptomatic. Management typically involves sialagogues, secretagogues such as pilocarpine and short-term topical corticosteroids to relieve sicca symptoms [2]. Parotid gland sialolithiasis is initially managed conservatively, but surgical management may be required if initial treatment fails to improve symptoms. Surgical intervention consists of stone removal under sialendoscopy and shock-wave lithotripsy under ultrasound guidance [5]. Parotidectomy should be considered a last resort treatment and reserved for patients with refractory symptoms or failed minimally invasive techniques [1].
Conclusion
Because of the variation in presentation with frequent head and neck involvement, otolaryngologists are often the initial providers for patients with Sjögren's disease. Early recognition of the disease with treatment provided by an interdisciplinary team of rheumatologists, ophthalmologists, ENTs, and dentists improves long-term outcomes and reduces complications.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Konstantinidis I, Paschaloudi S, Triaridis S, Fyrmpas G, Sechlidis S, Constantinidis J. Bilateral multiple sialolithiasis of the parotid gland in a patient with Sjögren's syndrome. Acta Otorhinolaryngol Ital. 2007;27(1):41–44. [PMC free article] [PubMed] [Google Scholar]
- 2.Stefanski A.L., Tomiak C., Pleyer U., Dietrich T., Burmester G.R., Dörner T. The diagnosis and treatment of Sjögren's Syndrome. Deutsches Arzteblatt international. 2017;114(20):354–361. doi: 10.3238/arztebl.2017.0354. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathews S.A., Kurien B.T., Scofield R.H. Oral manifestations of Sjögren's syndrome. J dental res. 2008;87(4):308–318. doi: 10.1177/154405910808700411. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- 4.Vitali C. Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Annals of the Rheumatic Diseases. 2002;61(6):554–558. doi: 10.1136/ard.61.6.554. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samani M., Hills A.J., Holden A.M., Man C.B., McGurk M. Minimally-invasive surgery in the management of symptomatic parotid stones. The Br j oral & maxillofacial surg. 2016;54(4):438–442. doi: 10.1016/j.bjoms.2016.01.033. https://doi.org/ [DOI] [PubMed] [Google Scholar]