Abstract
Background:
In the setting of kidney transplantation, histopathology of kidney biopsies is a key element in the organ assessment and allocation. Despite the broad diffusion of the Remuzzi–Karpinski score on preimplantation kidney biopsies, scientific evidence of its correlation to the transplantation outcome is controversial. The main issues affecting the prognostic value of histopathology are the referral to general on-call pathologists and the semiquantitative feature of the score, which can raise issues of interpretation. Digital pathology has shown very reliable and effective in the oncological diagnosis and treatment; however, the spread of such technologies is lagging behind in the field of transplantation. The aim of our study was to create a digital online platform where whole-slide images (WSI) of preimplantation kidney biopsies could be uploaded and stored.
Methods:
We included 210 kidney biopsies collected between January 2015 and December 2019 from the joint collaboration of the transplantation centers of Padua and Verona. The selected slides, stained with hematoxylin and eosin, were digitized and uploaded on a shared web platform. For each case, the on-call pathologists' Remuzzi grades were obtained from the original report, together with the clinical data and the posttransplantation follow-up.
Results:
The storage of WSI of preimplantation kidney biopsies would have several clinical, scientific, and educational advantages. The clinical utility relies on the possibility to consult online expert pathologists and real-time quality checks of diagnosis. From the perspective of follow-up, the archived digitized biopsies can offer a useful comparison to posttransplantation biopsies. In addition, the digital online platform is a precious tool for multidisciplinary meetings aimed both at the clinical discussion and at the design of research projects. Furthermore, this archive of readily available WSI is an important educational resource for the training of professionals.
Conclusions:
Finally, the web platform lays the foundation for the introduction of artificial intelligence in the field of transplantation that would help create new diagnostic algorithms and tools with the final aim of increasing the precision of organ assessment and its predictive value for transplant outcome.
Keywords: Digital pathology, innovation technology, preimplantation biopsy
INTRODUCTION
While the population with end-stage renal disease is growing and aging, kidney transplantation remains the best treatment strategy in most categories of patients.[1] The utilization policy of kidneys from expanded criteria donors (ECDs) has allowed a significant and beneficial expansion in the number of kidney transplantations, allowing some reduction in the time on the waiting list as well.[2]
In 1999, Remuzzi and a panel of international pathologists proposed the use of a histopathological score of preimplantation renal biopsies in order to detect significant chronic morphological changes and decide for discarding the organs or for proceeding with a single or dual transplantation.[3] This allocation protocol was prospectively validated in 2006, showing the correlation of this score with the graft survival.[4] Despite no agreement has been reached on the “best” grading system for preimplantation biopsies,[5,6,7,8] from that publication, the Remuzzi–Karpinski score has been widely adopted.[9,10] Although preimplantation biopsy may generate data for accepting or rejecting an organ, it represents a controversial issue. The major issue that undermines the reliability of histopathology is the low rate of agreement between pathologists on the Remuzzi–Karpinski score.[11] Some authors claim that biopsies are not representative of the organ status and suboptimal scoring leads to suboptimal usage of organs.[12] Furthermore, there is a wide variability and subjectivity among pathologists, pointing out that interobserver variability in biopsy scoring constitutes an important issue.[13] Indeed, as reported by Azancot et al., donor histology and graft outcome were correlated when the biopsy was evaluated by renal pathologists, but not when they were evaluated by on-call pathologists. The assessment of preimplantation kidney biopsies requires specialized training, while in most occasions, it is relied on the on-call general pathologist without the possibility of a second opinion from expert consultants. Indeed, the usual setting of transplant biopsy assessment involves the on-call pathologist and requires the biopsy to be examined with rapid embedding and fixation with microwave instrument, which is considered the gold standard. The possibility that the pathologist on-call may be a nephropathologist is unlikely due to the scarcity with such an expertise in most institutions. Therefore, slides of kidney biopsy are generally reviewed as part of laboratory checks or second opinion consultation, among which the most promising exploit/use digital pathology. In addition, the quantification of the chronic changes for each histological parameter is often subject to the judgment of the pathologist, lacking therefore in standardization and reproducibility. Poor concordance has been shown among general pathologists, who tend to give higher scores, especially for glomerulosclerosis and arterial thickness, which are the most important parameters for the assessment of chronic kidney damage.[12]
This conservative attitude of general pathologists, related to a lower familiarity with the specific type of assessment, has great consequences because the allocation of the organs is largely based on histopathology. On the one hand, we are therefore underutilizing the donor pool when a double kidney transplantation is inappropriately performed based on a high Remuzzi score; on the other side, a lack of uniformity in the judgment over pathology weakens the correlation between the time-zero biopsy and the transplantation outcome.[14]
The Banff working group, who gathered in 2017 to discuss the criteria for preimplantation kidney biopsy analysis, suggested that rigidly defined histologic cutoffs such as 20% glomerulosclerosis should not be used in isolation to discard kidneys. Other parameters including arteriolar hyalinosis, acute tubular injury, thrombotic microangiopathy, and diabetic nephropathy should also be included in a histopathologic donor biopsy scoring form as checkmarks.[15] However, prospective controlled studies are necessary in order to investigate new histopathological scores and validate them on the organ viability assessment.
Anyway, although the role of preimplantation kidney biopsies is nowadays questioned, their importance is undeniable. Together with the clinico-laboratory donor data, histopathology is essential in the global assessment of the organ condition for a more accurate prognostic evaluation of the long-term graft function. In addition, time-zero biopsies can be a baseline reference that, compared to posttransplant samples, can guide the identification of signs of rejection as opposed to chronic injuries prior to procurement. Within the Nord Italian transplant (NIT) area, kidneys procured from ECDs (over 70 years or between 60 and 70 with one risk factor among creatinine clearance <60 ml/min, proteinuria, diabetes, severe hypertension, and cardiovascular complication) are subject to biopsy which is analyzed according to the histologic Remuzzi/Karpinski score. The score is a combination of glomerular, vascular, interstitial, and tubular scores. For each component, the score could range from 0 to 3. When the vessel-wall thickness exceeds the luminal diameter or the lumen is entirely occluded, the score is 3. For the glomerular sclerosis, tubular atrophy, and interstitial fibrosis, when more than 50% is counted, the score is 3 for each parameter. Thus, the global score could range from a minimum of 0 to a maximum of 12.[4] The NITp dual kidney transplant protocol has changed in the last decade from the initial allocation strategy designed by Remuzzi; at the moment, kidneys are allocated to single KT with a score from 0 to 4, to dual KT when the score is 5–7, while they are discarded when the score exceeds 7.[16,17]
New medical and scientific technologies such as digital pathology and artificial intelligence (AI) are available nowadays allowing extraordinary benefits.[18] The fast, easy, and standardized analysis of specimens and the potential consult from distant specialists are some of the advantages of these technologies and represent the frontline diagnostic tools in oncology.[19] Although promising, digital approaches to transplant pathology are limited and scattered;[20,21] these resources have not been as extensively employed in the field of transplantation pathology and, in particular, to the preimplantation biopsies.[17,22]
The aim of this project was to create a digital platform of whole-slide images (WSI) taken from preimplantation kidney biopsies, highlighting the advantages in terms of clinical, scientific, and educational purposes, to improve prospects for management of kidney transplant.
PREIMPLANTATION KIDNEY CASE SERIES AND WEB PLATFORM
We considered consecutive preimplantation kidney biopsies performed at either the Hospital of Padua or Verona between January 2015 December 2019, and resulting in a single kidney transplantation. We retrieved a total of 210 kidney biopsies, 53 wedge and 157 needle biopsies, accompanied by clinical data. All biopsies were reported as adequate with at least 25 evaluable glomeruli and 2 arteries present, according to Banff.[15] The initial on-call pathologists' Remuzzi grades were obtained from the original reports for indexing, teaching, and multidisciplinary meeting purposes. The cases (hematoxylin and eosin) were digitized with a Hamamatsu NanoZoomer scanner at ×40, uploaded on a shared web platform provided by Nikon [Figure 1], and viewed with NDP.view2 software.[23] Digital slide size ranged from 200 megabytes to 1,5 gigabytes. For scanning procedure, there was a first-scan success rate of 93%, then all the remaining cases were successfully digitized with a second scan. The platform allows at present a basic set of annotation functionalities, such as the possibility to draw region of interest, to post comments on the image to highlight a specific feature, and a linear and square measurement tool. Screenshot function is obviously present. A present time, it is not allowed to all members to upload new cases, nor to professional external to our institutions to view cases, but we intend to open soon the consultation also to other pathologists, clinicians, and nonmedical professional for research purposes. Indeed, one of the main aims of the project is to constitute a body of digitized high-quality cases to be used to develop an AI tool which could help assessing the score.
Figure 1.
Platform for the digital archive of whole-slide images
All professionals involved from the two institutions received a permanent link with meeting ID and password for all online materials. The additional goal of the project is a validation of the digital system according to the newest CAP guidelines[24] and pathologists of our centers with different level of expertise, but all available for on-call service, and fewer expert nephropathologists are currently reviewing cases both on the platform and on glass slide to assess and ensure the concordance rates between digital and glass slide.
Multidisciplinary meetings were supported by Zoom videoconferencing software (Zoom Video Communications, Inc., San Jose, CA, USA). The platform was available from October 2020 offering the opportunity to organize three multidisciplinary meetings between pathologists, nephrologists, and surgeons from the centers of Padua and Verona. During the meetings, 10 cases were discussed via teleconference by the team and thus enabling to take multidisciplinary decisions for management of transplanted patients. Indeed, the cases concerned patients which had undergone subsequent biopsy for clinical reasons and the baseline histological picture was reviewed. We also collected feedback from the participants in terms of usability of the platform, satisfaction in viewing and navigating the cases, and issues, for example, lagging or slow uploading. For the multidisciplinary meeting, the person showing the digital slide sharing the screen kept the webcam on, while the others briefly turned it off, in order to minimize potential issue in quality of transmission of images. We underline that all the participants viewed the cases with their own workstations, hence there was great variability in terms of monitors and hardware, but we did not receive any significant report of relevant issues in terms of lagging or difficulties in navigating the slides. We have, however, less information concerning the viewing with tablets or smartphones.
Two training events were held for residents with the purpose to teach to recognize and quantify pathognomonic lesions of kidney preimplantation biopsies. In these events, about six clear-cut cases were used for teaching, but all the residents received access link to the platform to view cases. Moreover, the pathologist personnel involved in on-call rotation at our institution had the possibility to access the cases as an offer of self-learning collaterally to the teaching events organized for the residency program.
DISCUSSION
Digital pathology provides innovative tools that are being increasingly exploited to improve cancer care and discovery.[25] The adoption of digital pathology in several clinical and surgical fields has proven valuable in the review of difficult cases by experts, easy case archiving, consultation, and research activities.[19,20,21] However, its employment in the field of transplantation is lagging behind, partially due to the cost of the equipment, but mostly for the perception of low utility of pathology in assessing the organ viability and predicting the transplant outcome. Another major barrier to taking on WSI for primary diagnosis is the cultural resistance experienced by a pathologist.[26] A large-scale adoption of WSI should be encouraged, particularly in the assessment of transplant biopsies, as the advantages pertain not only to clinical practice but also to scientific development and finally to the educational area.
For what concerns the clinical utility, the diagnostic value of such a tool is precious in a setting such that of transplantation, where clinicians need the expertise of a dedicated pathologist in a contingency of time.[27] It allows online consultation of a specialist neuropathologist reducing the geographical and logistic barriers.[28] The prognostic value of the Remuzzi–Karpinski score in predicting the renal functional reserve of kidneys procured from expanded criteria deceased donors is significantly influenced by the specific expertise of the pathologist.[5] The lack of confidence of general on-call pathologists in analyzing the preimplantation kidney biopsies has also consequences in overestimating the degree of chronic injury which causes an increased rate of organ discard.[12] The digital platform allows a multidisciplinary approach, where clinicians and transplant surgeons can discuss together the cases, shaping a more direct and evidence-based opinion on the organ before making a final decision. The overscoring is the most frequent bias in the assessment by the general than by the specialist pathologists, suggesting that there is a risk of more organs being turned down or used for a double kidney transplantation. The platform, for example, can allow to properly frame the issue of suboptimal score due to subcapsular overrepresentation of glomerulosclerosis [Figure 2].[29] Indicating the precise percentage of glomerulosclerosis in addition to the specific locations, instead of indicating approximately the range (20%–50%), may be decisive in the organ allocation. Furthermore, while transplantation carries an unavoidable risk of transmission of malignant diseases from donor to recipient,[30,31] the digital system opens the way to a real-time, fast, and reliable consultation and quality control assessment of diagnoses provided by pathologists in the time constraints of transplant.
Figure 2.
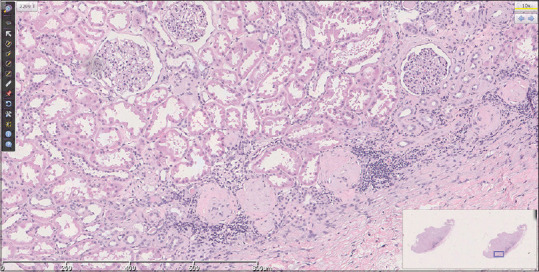
Example of subcapsular overrepresentation of glomerulosclerosis
In addition to the potential share of the images among colleagues, the digital platform provides informatics tools to give a quantitative description of features. The semiquantitative score may not be a sufficiently refined tool to guide the decision process in those gray-zone cases over two thresholds. As an instance, the arteriolar wall-to-lumen ratio can be exactly and easily quantified [Figure 3]. Furthermore, once digital pathology is adopted, there may be several new software-driven opportunities to increase workflow efficiency and facilitate precision diagnoses. In line with this necessity, the digital diagnostic platform could not only facilitate the analysis of the preimplantation biopsies but also help in making a semiquantitative histological assessment more objective and reproducible.[21] Indeed, one of the main goals of the project is to constitute a body of digitized high-quality cases to be used to develop an AI tool which could help assessing the score and which could be handy for on-call pathologist. With this in mind, we intend to open soon the consultation also to other nonmedical professional, such as computer scientists, engineers, and statisticians. As in the work by Hermsen et al.,[32] AI tool for preimplantation kidney biopsy exists but still needs validation and application on real-life cases outside academic institutions, with real general pathologists using the tool in their routine activity, and our interest is also in contributing to be part of this development.
Figure 3.
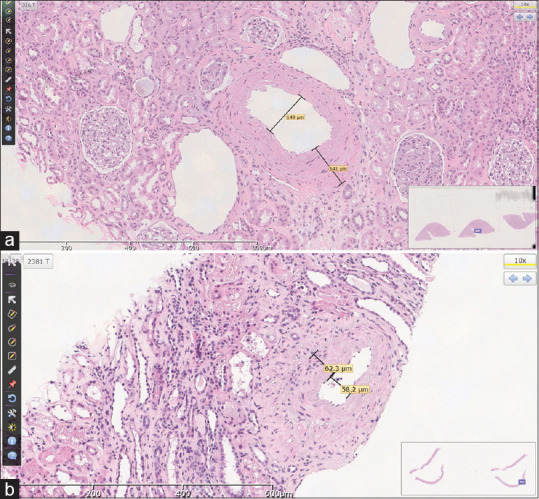
Assessment of arteriolar wall-to-lumen ratio through digital measurements in a wedge (a) and needle core (B) biopsy.
From a diagnostic perspective, a digital archive of these time-zero biopsies could facilitate their comparison against samples taken at posttransplantation time points. The critical issue in these situations is generally the different and distant locations of the transplantation centers, where the preimplantation biopsy is stored, and the peripheral hospital, where the clinicians can manage the patients and perform a follow-up biopsy. It is often useful to have a control biopsy taken at time zero, through which the pathologist can identify whether a particular scenario of chronic damage was partially present at baseline or it is entirely new and related to immunological causes.[33] The creation of a digital platform enables an easier and faster accessibility to preimplantation and follow-up kidney biopsies, possibly increasing the prognostic meaning of the first and the diagnostic value of the latter.
The digital platform has a role in scientific research as well. WSI of donor kidney biopsies can be a priceless opportunity to start collaborations and share opinions on the management of preimplantation biopsy procedure and evaluation. It could also be the groundwork for a more ambitious project of prospective collection of data on the outcome of kidney transplantations with the aim to implement the prognostic value of the histological analysis and multidisciplinary approach.[34,35]
Finally, the application of such computer-based technology in the field of donor assessment pathology has a valuable educational purpose as well. The sharing of WSI through multimedia lessons is a valuable resource for the training of residents, physicians, and medical students.[36] Human kidney specimens with or without pathological lesions are hardly available in clinical practice and could therefore offer a teaching tool for young and inexperienced professionals.
FUTURE DIRECTIONS
Digital pathology plays an important role in accelerating advances in health care by supporting collaboration. Notably, there is an emerging need in transplantation to enhance and standardize the diagnosis, and in this scenario, the employment of AI may allow a standardization in the organ assessment of the conventionally analyzed parameters/alterations. The integration of computer algorithms into digital pathology workflow could support diagnosis, resulting in significant improvement of standardization and safety for patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2021/12/1/4/307702
REFERENCES
- 1.Maenosono R, Tullius SG. Saving lives by saving kidneys for transplant. JAMA Intern Med. 2019;179:1374. doi: 10.1001/jamainternmed.2019.2609. [DOI] [PubMed] [Google Scholar]
- 2.Massie AB, Luo X, Chow EK, Alejo JL, Desai NM, Segev DL. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am J Transplant. 2014;14:2310–6. doi: 10.1111/ajt.12830. [DOI] [PubMed] [Google Scholar]
- 3.Remuzzi G, Grinyò J, Ruggenenti P, Beatini M, Cole EH, Milford EL, et al. Early experience with dual kidney transplantation in adults using expanded donor criteria. J Am Soc Nephrol. 1999;10:2591–8. doi: 10.1681/ASN.V10122591. [DOI] [PubMed] [Google Scholar]
- 4.Remuzzi G, Cravedi P, Perna A, Dimitrov BD, Turturro M, Locatelli G, et al. Long-term outcome of renal transplantation from older donors. N Engl J Med. 2006;354:343–52. doi: 10.1056/NEJMoa052891. [DOI] [PubMed] [Google Scholar]
- 5.Antonieta Azancot M, Moreso F, Salcedo M, Cantarell C, Perello M, Torres IB, et al. The reproducibility and predictive value on outcome of renal biopsies from expanded criteria donors. Kidney Int. 2014;85:1161–8. doi: 10.1038/ki.2013.461. [DOI] [PubMed] [Google Scholar]
- 6.Karpinski J, Lajoie G, Cattran D, Fenton S, Zaltzman J, Cardella C, et al. Outcome of kidney transplantation from high-risk donors is determined by both structure and function. Transplantation. 1999;67:1162–7. doi: 10.1097/00007890-199904270-00013. [DOI] [PubMed] [Google Scholar]
- 7.Munivenkatappa RB, Schweitzer EJ, Papadimitriou JC, Drachenberg CB, Thom KA, Perencevich EN, et al. The Maryland Aggregate Pathology Index: A deceased donor kidney biopsy scoring system for predicting graft failure. Am J Transplant. 2008;8:2316–24. doi: 10.1111/j.1600-6143.2008.02370.x. [DOI] [PubMed] [Google Scholar]
- 8.Lopes JA, Moreso F, Riera L, Carrera M, Ibernon M, Fulladosa X, et al. Evaluation of pre-implantation kidney biopsies: Comparison of Banff criteria to a morphometric approach. Kidney Int. 2005;67:1595–600. doi: 10.1111/j.1523-1755.2005.00241.x. [DOI] [PubMed] [Google Scholar]
- 9.Yap YT, Ho QY, Kee T, Ng CY, Chionh CY. Impact of pre-transplant biopsy on 5-year outcomes of expanded criteria donor kidney transplantation. Nephrology. 2021;26:70–7. doi: 10.1111/nep.13788. [DOI] [PubMed] [Google Scholar]
- 10.Carrara C, Cravedi P, Perna A, Peraro F, Villa A, Carrara F, et al. Preimplantation histological score associates with 6-month GFR in recipients of perfused, older kidney grafts: Results from a pilot study. Nephron. 2021;145((2)):137–149. doi: 10.1159/000512341. [DOI] [PubMed] [Google Scholar]
- 11.Husain SA, Shah V, Alvarado Verduzco H, King KL, Brennan C, Batal I, et al. Impact of deceased donor kidney procurement biopsy technique on histologic accuracy. Kidney Int Rep. 2020;5:1906–13. doi: 10.1016/j.ekir.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Girolami I, Gambaro G, Ghimenton C, Beccari S, Caliò A, Brunelli M, et al. Pre-implantation kidney biopsy: Value of the expertise in determining histological score and comparison with the whole organ on a series of discarded kidneys. Nephrol. 2020;33:167–76. doi: 10.1007/s40620-019-00638-7. [DOI] [PubMed] [Google Scholar]
- 13.Kasiske BL, Stewart DE, Bista BR, Salkowski N, Snyder JJ, Israni AK, et al. The role of procurement biopsies in acceptance decisions for kidneys retrieved for transplant. Clin J Am Soc Nephrol. 2014;9:562–71. doi: 10.2215/CJN.07610713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mallon DH, Riddiough GE, Summers DM, Butler AJ, Callaghan CJ, Bradbury LL, et al. Successful transplantation of kidneys from elderly circulatory death donors by using microscopic and macroscopic characteristics to guide single or dual implantation. Am J Transplant. 2015;15:2931–9. doi: 10.1111/ajt.13349. [DOI] [PubMed] [Google Scholar]
- 15.Liapis H, Gaut JP, Klein C, Bagnasco S, Kraus E, Farris AB, et al. Banff histopathological consensus criteria for preimplantation kidney biopsies. Am J Transplant. 2017;17:140–50. doi: 10.1111/ajt.13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nord Italian Transplant Program. Protocollo Reni da Donatori Anziani. 2013. [Accessed 2021 Mar 30]]. Available from: https://www.policlinico.mi.it/AMM/nitp/area_operatore/protocolli/02/PT06580_protocollo-reni-donatori-anziani_rev0.pdf .
- 17.Eccher A, Neil D, Ciangherotti A, Cima L, Boschiero L, Martignoni G, et al. Digital reporting of whole-slide images is safe and suitable for assessing organ quality in preimplantation renal biopsies. Hum Pathol. 2016;47:115–20. doi: 10.1016/j.humpath.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Pantanowitz L, Farahani N, Parwani A. Whole slide imaging in pathology: Advantages, limitations, and emerging perspectives. Pathol Lab Med Int. 2015;7:23–33. [Google Scholar]
- 19.Niazi MK, Parwani AV, Gurcan MN. Digital pathology and artificial intelligence. Lancet Oncol. 2019;20:e253–61. doi: 10.1016/S1470-2045(19)30154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eccher A, Girolami I, Brunelli M, Novelli L, Mescoli C, Malvi D, et al. Digital pathology for second opinion consultation and donor assessment during organ procurement: Review of the literature and guidance for deployment in transplant practice. Transplant Rev. 2020;34:100562. doi: 10.1016/j.trre.2020.100562. [DOI] [PubMed] [Google Scholar]
- 21.Girolami I, Parwani A, Barresi V, Marletta S, Ammendola S, Stefanizzi L, et al. The landscape of digital pathology in transplantation: From the beginning to the virtual E-slide. Pathol Inform. 2019;10:21. doi: 10.4103/jpi.jpi_27_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cima L, Brunelli M, Parwani A, Girolami I, Ciangherotti A, Riva G, et al. Validation of remote digital frozen sections for cancer and transplant intraoperative services. Pathol Inform. 2018;9:34. doi: 10.4103/jpi.jpi_52_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamamatsu. NDP.view2 Software. [Accessed 2021 Mar 30]]. Available from: https://www.hamamatsu.com/resources/pdf/sys/SBIS0066E_NDPVIEW2.pdf .
- 24.Evans AJ, Brown RW, Bui MM, Chlipala EA, Lacchetti C, Milner DA, et al. Validating whole slide imaging systems for diagnostic purposes in pathology: Guideline update from the College of American Pathologists in Collaboration with the American Society for Clinical Pathology and the Association for Pathology Informatics. Arch Pathol Lab Med. 2021 [Online ahead of print] [Google Scholar]
- 25.Browning L, Colling R, Rittscher J, Winter L, McEntyre N, Verrill C. Implementation of digital pathology into diagnostic practice: Perceptions and opinions of histopathology trainees and implications for training. J Clin Pathol. 2020;73:223–7. doi: 10.1136/jclinpath-2019-206137. [DOI] [PubMed] [Google Scholar]
- 26.Eccher A, Girolami I. Current state of whole slide imaging use in cytopathology: Pros and pitfalls. Cytopathology. 2020;31:372–8. doi: 10.1111/cyt.12806. [DOI] [PubMed] [Google Scholar]
- 27.Haas M. Donor kidney biopsies: Pathology matters, and so does the pathologist. Kidney Int. 2014;85:1016–9. doi: 10.1038/ki.2013.439. [DOI] [PubMed] [Google Scholar]
- 28.Wilbur D, Pettus J, Smith M, Cornell L, Andryushkin A, Wingard R, et al. Using image registration and machine learning to develop a workstation tool for rapid analysis of glomeruli in medical renal biopsies. Pathol Inform. 2020;11:37. doi: 10.4103/jpi.jpi_49_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muruve NA, Steinbecker KM, Luger AM. Are wedge biopsies of cadaveric kidneys obtained at procurement reliable? Transplantation. 2000;69:2384–8. doi: 10.1097/00007890-200006150-00029. [DOI] [PubMed] [Google Scholar]
- 30.Eccher A, Girolami I, Motter JD, Marletta S, Gambaro G, Momo RE, et al. Donor-transmitted cancer in kidney transplant recipients: A systematic review. Nephrol. 2020;33((6)):1321–1332. doi: 10.1007/s40620-020-00775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eccher A, Girolami I, Marletta S, Brunelli M, Carraro A, Montin U, et al. Donor-transmitted cancers in transplanted livers: Analysis of clinical outcomes. Liver Transplant 2020. 2021;27((1)):55–66. doi: 10.1002/lt.25858. [DOI] [PubMed] [Google Scholar]
- 32.Hermsen M, de Bel T, den Boer M, Steenbergen EJ, Kers J, Florquin S, et al. Deep learning–based histopathologic assessment of kidney tissue. J Am Soc Nephrol. 2019;30:1968–79. doi: 10.1681/ASN.2019020144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood-Trageser MA, Lesniak AJ, Demetris AJ. Enhancing the value of histopathological assessment of allograft biopsy monitoring. Transplantation. 2019;103((7)):1306–1322. doi: 10.1097/TP.0000000000002656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carpenter D, Husain SA, Brennan C, Batal I, Hall IE, Santoriello D, et al. Procurement biopsies in the evaluation of deceased donor kidneys. Clin J Am Soc Nephrol. 2018;13:1876–85. doi: 10.2215/CJN.04150418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Angeletti A, Cravedi P. Making procurement biopsies important again for kidney transplant allocation. Nephron. 2019;142:34–9. doi: 10.1159/000499452. [DOI] [PubMed] [Google Scholar]
- 36.Pantanowitz L, Wiley CA, Demetris A, Lesniak A, Ahmed I, Cable W, et al. Experience with multimodality telepathology at the University of Pittsburgh Medical Center. Pathol Inform. 2012;3:45. doi: 10.4103/2153-3539.104907. [DOI] [PMC free article] [PubMed] [Google Scholar]


