This cross-sectional study evaluates the role that poverty and socioeconomic disparities play in the risk of firearm-related death among children and young adults.
Key Points
Question
Is concentrated county-level poverty associated with a youth’s risk of firearm-related death?
Findings
In this cross-sectional study of 67 905 firearm-related fatalities among US youth aged 5 to 24 years, higher concentration of county-level poverty was associated with increased rates of total firearm-related deaths, homicides, suicides, and unintentional deaths. More than half of all firearm-related deaths, including two-thirds of firearm-related homicides, could be associated with living in a county with a high concentration of poverty.
Meaning
The findings suggest that high poverty concentration can have deleterious implications for the risk of youth firearm-related deaths; a multidimensional strategy that reduces poverty and firearm-related deaths among youth living in impoverished communities is urgently needed.
Abstract
Importance
Youth firearm-related deaths are a public health crisis in the US. The association between county-level poverty and the risk of firearm-related deaths among youth is unknown, however.
Objective
To examine the association between county-level poverty concentration and firearm-related mortality rates in US youth.
Design, Setting, and Participants
This cross-sectional study analyzed US firearm fatalities in children and young adults aged 5 to 24 years that occurred between January 1, 2007, and December 31, 2016. Data were obtained from the Centers for Disease Control and Prevention’s Compressed Mortality File, and annual intercensal county population data were obtained from the US Census Bureau. Data analyses were conducted between November 1, 2019, and June 30, 2020.
Exposures
County-level poverty was categorized into 5 groups: 0% to 4.9%, 5% to 9.9%, 10% to 14.9%, 15% to 19.9%, and ≥20% of the population living below the federal poverty level.
Main Outcomes and Measures
The main outcomes were firearm-related deaths in total and by specific intent (homicide, suicide, and unintentional) per 100 000 youths over the entire study period. Multivariable negative binomial regression models were used to analyze the association between firearm-related mortality rates and county poverty concentration, controlling for demographic variables, urbanicity, and statewide firearm prevalence. Adjusted incidence rate ratios (IRRs) were calculated, and statewide firearm prevalence was estimated. The population-attributable fraction (PAF) and years of potential life lost for each intent were calculated.
Results
A total of 67 905 firearm-related deaths among youth (predominantly composed of 60 164 male individuals [88.6%]) from 2007 to 2016 were analyzed. Of these deaths, 42 512 were homicides (62.6%), 23 034 were suicides (33.9%), and 1627 were unintentional (2.4%). Firearm-related mortality risk increased in a stepwise manner with increasing county poverty concentration. Compared with counties with the lowest poverty concentration, counties with the highest poverty concentration had an increased rate of total firearm-related deaths (adjusted IRR, 2.29; 95% CI, 1.96-2.67), homicides (adjusted IRR, 3.55; 95% CI, 2.80-4.51), suicides (adjusted IRR, 1.45; 95% CI, 1.20-1.75), and unintentional deaths (adjusted IRR, 9.32; 95% CI, 2.32-37.4). The PAF was 0.51 (95% CI, 0.43-0.57) for all firearm-related deaths, 0.66 (95% CI, 0.57-0.73) for homicides, 0.30 (95% CI, 0.17-0.42) for suicides, and 0.86 (95% CI, 0.46-0.97) for unintentional deaths. This calculation translated to 34 292 firearm-related deaths that would not have occurred if all counties had the same risk as counties with the lowest poverty concentration. A total of 3 833 105 years of potential life lost was observed.
Conclusions and Relevance
This study found an association between firearm-related mortality rates among youth and county-level poverty concentration. With more than half of firearm-related deaths and two-thirds of firearm-related homicides potentially associated with living in an area with a high concentration of poverty, a multidimensional strategy to reduce poverty and firearm-related deaths is urgently needed.
Introduction
Firearm-related deaths are a major public health crisis in the US. Among US children and young adults, firearm-related deaths are the second leading cause of death, accounting for 24% of all deaths in those aged 15 to 24 years in 2019.1,2,3,4 Compared with other high-income countries, the US has a youth firearm-related homicide rate that is 49 times higher than the aggregate rate of 22 countries.5,6 Globally, among children 0 to 14 years of age who were killed by firearms, 91% resided in the US in 2010.7
In the US, the risk of unintentional injury-related death is greater for those living in counties with a higher poverty concentration.8 Individual and community-level poverty have been associated with adverse child health outcomes, including injury hospitalization, asthma, and lack of school readiness.9 Furthermore, county-level poverty has been associated with increased rates of injury mortality, such as child abuse death and youth suicide.10,11
The aim of this study was to examine the association between county-level poverty concentration and firearm-related mortality rates in US youth. We hypothesized higher rates of firearm-related deaths across all intents of firearm injury in youth living in counties with the highest poverty concentrations.
Methods
Study Design and Data Sources
We conducted a retrospective, cross-sectional study of all firearm-related fatalities among US youth aged 5 to 24 years that occurred from January 1, 2007, to December 31, 2016. Given that this study analyzed only fatality data, it was deemed exempt from institutional review board review and the informed consent requirement by Boston Children's Hospital.
We used the Centers for Disease Control and Prevention’s Compressed Mortality File, an administrative database of death certificate data produced by the National Center for Health Statistics.12 This data set includes complete pooled mortality and population counts in the US by age, sex, race and ethnicity, and cause of death at the county level. Causes of death are classified according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
We obtained annual intercensal county population data from the US Census Bureau.13,14 This data set includes population counts stratified by age, sex, and race and ethnicity at the county level. We obtained county poverty estimates from the Small Area Income and Poverty Estimates data.15 Urban-rural classification was obtained from the National Center for Health Statistics 2013 urban-rural county classification, which was based on the 2010 US Census data.16 To estimate the annual statewide firearm prevalence, we used a proxy measure from the RAND Corporation17 that combined data from several surveys and administrative sources and represented the proportion of households with a firearm for each state for each year of the study period.
Study Measures
The study outcome was total firearm-related deaths in youth aged 5 to 24 years, including homicides, suicides, unintentional deaths, and deaths with undetermined intent. The codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision that were used to classify causes of death included accidental discharge of firearms (W32-W34), intentional self-harm (suicide) by discharge of firearms (X72-X74), assault (homicide) by discharge of firearms (U01.4 and X93-X95), and discharge of firearms of undetermined intent (Y22-Y24). County-level poverty concentration, which was defined as the percentage of the population living below the federal poverty level, was categorized into 5 groups (0% to 4.9%, 5% to 9.9%, 10% to 14.9%, 15% to 19.9%, and ≥20%) consistent with previous studies.8,10,11,18,19,20,21 The annual income threshold for the federal poverty level for a family of 4 was $21 027 in 2007 and was $24 339 in 2016.22 Annual county-level population estimates were stratified by sex (male or female), age (5-9, 10-14, 15-19, or 20-24 years), self-reported or self-selected race and ethnicity (Alaska Native and American Indian, Asian, Hispanic, non-Hispanic Black, non-Hispanic White, or other [Native Hawaiian or Other Pacific Islander and ≥2 races]), and county urban-rural classification (large central metropolitan, large fringe metropolitan, medium metropolitan, small metropolitan, micropolitan, or noncore).16
Statistical Analysis
We calculated the total annual firearm-related mortality rates per 100 000 youths aged 5 to 24 years and for each intent (homicide, suicide, unintentional, and undetermined) and across demographic variables, urbanicity, and county-level poverty concentration. To compare relative rates between each of these groups, we calculated incidence rate ratios (IRRs) with 95% CIs for the first (2007) and last (2016) years of the analysis. In addition, we calculated the yearly unadjusted IRRs for each county-level poverty concentration, using counties with 0% to 4.9% poverty concentration as the referent group for firearm-related total deaths, homicides, and suicides. For unintentional deaths, counties with 5% to 9.9% county-level poverty concentration were used as the referent group when calculating the unadjusted IRRs given that counties with 0% to 4.9% poverty level had 0 recorded unintentional deaths for several years.
To examine the association of county-level poverty concentration on firearm-related mortality rates, we performed a series of generalized estimating equation modeling, with each model using firearm fatalities as the dependent variable and county-level poverty concentration as the independent variable. Models used robust SE estimates clustered on panels and an unstructured within-group correlation structure. We constructed panels to account for the clustering of data within counties across all years of the study period. Each demographic group of sex, age, and race and ethnicity within each county was considered a panel. Each panel was then represented by 10 observations, 1 for each year of the study.
We estimated 3 multivariable negative binomial regression models: model 1 consisted of demographic variables as covariates, model 2 consisted of model 1 with added county urbanicity, and model 3 consisted of model 2 with statewide firearm prevalence added. Models included the log of the stratum-specific population estimate as the offset (coefficient constrained to 1) to estimate incidence rates in which strata were defined by county, year, age group, sex, and race and ethnicity. Therefore, each stratum contributed a count of firearm-related deaths and a population estimate to the calculation of incidence rates. Counties with the lowest poverty concentration (0%-4.9%) were used as a referent in the multivariable models. For these analyses, county urban-rural classification was coded as either urban (large central metropolitan, large fringe metropolitan, medium metropolitan, and small metropolitan) or rural (micropolitan or noncore).23,24 Because no firearm prevalence data were available for Washington, DC, these firearm-related deaths were not included in multivariable model 3.17 As a sensitivity analysis, we ran model 3 with the data from Washington, DC, but we observed no changes in the outcome.
The population-attributable fraction (PAF) calculated the number of youth firearm-related deaths that may not have occurred had the risk for all youth equaled the risk for those who lived in counties with the lowest poverty concentration. The PAF represents the proportion of deaths associated with a particular exposure, which was concentrated county poverty in this study. We calculated the PAF using the adjusted IRRs from model 3. We calculated years of potential life lost using annual fatality frequencies by age and sex. For each study year, we took the sex-specific life expectancy estimated by the Centers for Disease Control and Prevention and subtracted the mean age of death for each age group under study (eg, 17 years for youth who died at ages 15-19 years).25 The resulting difference was multiplied by the frequency of firearm-related deaths in each particular age and sex strata for each year and then totaled for all age and sex strata for each study year.
All analyses were performed in Stata, version 15 (StataCorp LLC). Data analyses were conducted between November 1, 2019, and June 30, 2020.
Results
Firearm-Related Deaths in US Youth
From 2007 to 2016, a total of 67 905 firearm-related deaths in youth aged 5 to 24 years occurred. This group comprised 60 164 male (88.6%) and 7741 female (11.4%) individuals.
Of the 67 905 firearm-related deaths, 42 512 were homicides (62.6%), 23 034 were suicides (33.9%), and 1627 were unintentional (2.4%). The annual rate of total firearm-related deaths was 8.5 per 100 000 youths in 2007 and increased to 9.2 per 100 000 youths in 2016, a rate difference of 0.7 per 100 000 youths (95% CI, 0.4-1.0). Those individuals who were living in counties with the highest poverty concentration (≥20% below the federal poverty level) accounted for 14 960 (22.0%) of total firearm-related deaths, 10 858 (25.5%) of homicides, 3553 (15.3%) of suicides, and 408 (25.1%) of unintentional deaths, despite representing only 15.1% (n = 127 574 665) of the US youth population. Male individuals accounted for 60 164 (88.6%) of total firearm-related deaths. Non-Hispanic Black youth accounted for 30 394 (44.8%) of total firearm-related deaths and 27 174 (63.9%) of homicides, despite representing only 14.3% (n = 120 786 590) of the US youth population (Table 1).
Table 1. Characteristics of Youth With Firearm-Related Deaths in the United States From 2007 to 2016.
| Characteristic | No. (%) | ||||
|---|---|---|---|---|---|
| US youth population (n = 846 630 376) | Total firearm-related deaths (n = 67 905) | Homicides (n = 42 512) | Suicides (n = 23 034) | Unintentional deaths (n = 1627) | |
| Age group, y | |||||
| 5-9 | 202 946 668 (24.0) | 722 (1.0) | 567 (1.3) | 5 (0.02) | 130 (8.0) |
| 10-14 | 206 835 615 (24.4) | 2521 (3.7) | 1175 (2.7) | 1052 (4.6) | 226 (13.9) |
| 15-19 | 215 975 889 (25.5) | 23 595 (34.7) | 15 178 (35.7) | 7562 (32.8) | 594 (36.5) |
| 20-24 | 220 872 204 (26.1) | 41 067 (60.5) | 25 592 (60.2) | 14 415 (62.3) | 677 (41.6) |
| Sex | |||||
| Male | 433 118 700 (51.2) | 60 164 (88.6) | 37 643 (88.5) | 20 442 (88.7) | 1459 (89.7) |
| Female | 413 511 676 (48.8) | 7741 (11.4) | 4869 (11.5) | 2592 (11.3) | 168 (10.3) |
| Race and ethnicitya | |||||
| Alaska Native or American Indian | 7 412 316 (0.9) | 866 (1.3) | 313 (0.7) | 483 (2.1) | 48 (3.0) |
| Asian | 39 862 446 (4.7) | 1015 (1.5) | 502 (1.2) | 491 (2.1) | 16 (1.0) |
| Hispanic | 185 385 811 (21.9) | 11 243 (16.6) | 8518 (20.0) | 2410 (10.4) | 219 (13.5) |
| Non-Hispanic | |||||
| Black | 120 786 590 (14.3) | 30 394 (44.8) | 27 174 (63.9) | 2569 (11.2) | 444 (27.3) |
| White | 465 395 531 (55.0) | 24 173 (35.6) | 5839 (13.7) | 17 037 (74.0) | 899 (55.3) |
| Otherb | 27 787 682 (3.3) | 214 (0.3) | 166 (0.4) | 44 (0.2) | 1 (0.1) |
| County-level poverty concentration, % | |||||
| 0-4.9 | 8 531 252 (1.0) | 248 (0.4) | 85 (0.2) | 159 (0.7) | 2 (0.1) |
| 5-9.9 | 152 172 754 (18.0) | 6841 (10.1) | 3152 (7.4) | 3484 (15.1) | 127 (7.8) |
| 10-14.9 | 269 774 510 (31.9) | 18 551 (27.3) | 10 175 (23.9) | 7707 (33.5) | 474 (29.1) |
| 15-19.9 | 288 577 195 (34.1) | 27 305 (40.2) | 18 242 (42.9) | 8151 (35.4) | 616 (37.9) |
| ≥20 | 127 574 665 (15.1) | 14 960 (22.0) | 10 858 (25.5) | 3533 (15.3) | 408 (25.1) |
| Urbanicityc | |||||
| Large central metropolitan | 257 014 048 (30.4) | 27 665 (40.7) | 22 293 (52.4) | 4868 (21.1) | 295 (18.1) |
| Large fringe metropolitan | 206 747 223 (24.4) | 11 927 (17.6) | 6957 (16.4) | 4612 (20.0) | 227 (14.0) |
| Medium metropolitan | 181 310 221 (21.4) | 13 939 (20.5) | 8043 (18.9) | 5393 (23.4) | 360 (22.1) |
| Small metropolitan | 81 013 443 (9.6) | 5413 (8.0) | 2253 (5.3) | 2867 (12.5) | 212 (13.0) |
| Micropolitan | 73 256 239 (8.7) | 5096 (7.5) | 1812 (4.3) | 2917 (12.7) | 277 (17.0) |
| Noncore | 47 289 202 (5.6) | 3865 (5.7) | 1154 (2.7) | 2377 (10.3) | 256 (15.7) |
Race and ethnicity were self-reported or self-selected.
The other category included Native Hawaiian or Other Pacific Islander and ≥2 races.
For analyses, county urbanicity was coded as a categorical variable, either urban (large central metropolitan, large fringe metropolitan, medium metropolitan, and small metropolitan) or rural (micropolitan or noncore).
Firearm-Related Deaths by Intent and Demographic Variable
Youth aged 20 to 24 years had the highest rates of total firearm-related deaths and for each intent in 2007 and 2016 (2007: 19.7 deaths per 100 000 youths; 2016: 21.4 deaths per 100 000 youths) (eTable 1 in the Supplement). Non-Hispanic Black youth had the highest rates of total firearm-related deaths (2007: 27.3 deaths per 100 000 youths; 2016: 29.9 deaths per 100 000 youths) and homicides (2007: 24.5 deaths per 100 000 youths; 2016: 26.5 deaths per 100 000 youths) in 2007 and 2016. Alaska Native or American Indian youth had the highest rates of suicides (2007: 5.7 deaths per 100 000 youths; 2016: 6.3 deaths per 100 000 youths) and unintentional deaths (2007: 0.9 deaths per 100 000 youths; 2016: 0.6 deaths per 100 000 youths) in the same periods. For Alaska Native or American Indian youth, firearm-related suicides increased 10.5% from 2007 (5.7 per 100 000 youths) to 2016 (6.3 per 100 000 youths). Firearm-related suicide rates among non-Hispanic White youth increased 55.2% from 2007 (2.9 per 100 000 youths) to 2016 (4.5 per 100 000 youths). Large central metropolitan areas had the highest rates of total firearm-related deaths (2007: 12.7 deaths per 100 000 youths; 2016: 11.8 deaths per 100 000 youths) and homicides (2007: 10.5 deaths per 100 000 youths; 2016: 9.3 deaths per 100 000 youths), whereas noncore areas that had the highest rates of suicides (2007: 4.1 deaths per 100 000 youths; 2016: 5.9 deaths per 100 000 youths) and unintentional deaths (2007: 0.8 deaths per 100 000 youths; 2016: 0.5 deaths per 100 000 youths) (Table 2).
Table 2. Mortality Rates and Incidence Rate Ratios for Total Firearm-Related Deaths and Specific Intents Stratified by Race and Ethnicity and Urbanicity .
| Characteristic | Total firearm-related deaths | Homicides | Suicides | Unintentional deaths | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | |||||||||
| 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | |
| Race and ethnicitya | ||||||||||||||||
| Alaska Native or American Indian | 11.0 | 12.0 | 2.4 (1.9-3.0) | 1.9 (1.5-2.4) | 3.8 | 4.5 | 2.7 (1.8-3.8) | 3.3 (2.2-4.7) | 5.7 | 6.3 | 2 (1.4-2.7) | 1.4 (1.0-1.9) | 0.9 | 0.6 | 4.5 (1.8-9.6) | 3.0 (0.8-7.8) |
| Asian | 3.2 | 3.4 | 0.7 (0.6-0.9) | 0.5 (0.4-0.6) | 1.7 | 1.3 | 1.1 (0.8-1.5) | 1 (0.7-1.3) | 1.5 | 2.0 | 0.5 (0.4-0.7) | 0.4 (0.4-0.5) | 0 | 0 | 0.1 (0-0.8) | 0.1 (0-0.7) |
| Hispanic | 8.2 | 6.2 | 1.8 (1.7-1.9) | 1 (0.9-1.1) | 6.6 | 4.3 | 4.5 (4.1-5.0) | 3.1 (2.8-3.4) | 1.3 | 1.7 | 0.4 (0.4-0.5) | 0.4 (0.3-0.4) | 0.2 | 0.1 | 0.9 (0.6-1.4) | 0.8 (0.5-1.2) |
| Non-Hispanic | ||||||||||||||||
| Black | 27.3 | 29.9 | 5.9 (5.6-6.2) | 4.8 (4.6-5.1) | 24.5 | 26.5 | 16.9 (15.5-18.3) | 19.1 (17.5-20.8) | 2.0 | 2.9 | 0.7 (0.6-0.8) | 0.6 (0.6-0.7) | 0.5 | 0.4 | 2.4 (1.7-3.4) | 1.9 (1.3-2.8) |
| White | 4.6 | 6.2 | 1 [Reference] | 1 [Reference] | 1.5 | 1.4 | 1 [Reference] | 1 [Reference] | 2.9 | 4.5 | 1 [Reference] | 1 [Reference] | 0.2 | 0.2 | 1 [Reference] | 1 [Reference] |
| Otherb | 1.0 | 0.4 | 0.2 (0.1-0.3) | 0.1 (0-0.1) | 0.9 | 0.3 | 0.6 (0.4-0.9) | 0.3 (0.1-0.5) | 0.2 | 0.1 | 0.1 (0-0.2) | 0 (0-0.1) | 0 | 0 | 0 (0-0.8) | 0 (0-0.6) |
| Urbanicityc | ||||||||||||||||
| Large central metropolitan | 12.7 | 11.8 | 1 [Reference] | 1 [Reference] | 10.5 | 9.3 | 1 [Reference] | 1 [Reference] | 1.9 | 2.3 | 1 [Reference] | 1 [Reference] | 0.2 | 0.1 | 1 [Reference] | 1 [Reference] |
| Large fringe metropolitan | 6.1 | 6.9 | 0.5 (0.5-0.5) | 0.6 (0.6-0.6) | 4.1 | 4.0 | 0.4 (0.4-0.4) | 0.4 (0.4-0.5) | 1.7 | 2.7 | 0.9 (0.8-1.0) | 1.2 (1.1-1.3) | 0.1 | 0.1 | 0.9 (0.5-1.5) | 0.7 (0.4-1.3) |
| Medium metropolitan | 7.5 | 9.0 | 0.6 (0.6-0.6) | 0.8 (0.7-0.8) | 4.6 | 4.9 | 0.4 (0.4-0.5) | 0.5 (0.5-0.6) | 2.5 | 3.8 | 1.3 (1.1-1.5) | 1.7 (1.5-1.9) | 0.3 | 0.2 | 1.6 (1.0-2.6) | 1.1 (0.7-1.9) |
| Small metropolitan | 5.9 | 8.2 | 0.5 (0.4-0.5) | 0.7 (0.6-0.8) | 2.8 | 3.3 | 0.3 (0.2-0.3) | 0.4 (0.3-0.4) | 2.8 | 4.6 | 1.5 (1.2-1.7) | 2.0 (1.8-2.3) | 0.2 | 0.2 | 1.5 (0.8-2.6) | 1.5 (0.8-2.7) |
| Micropolitan | 6.2 | 8.5 | 0.5 (0.4-0.5) | 0.7 (0.7-0.8) | 2.5 | 3.0 | 0.2 (0.2-0.3) | 0.3 (0.3-0.4) | 3.2 | 5.0 | 1.7 (1.4-2.0) | 2.2 (1.9-2.5) | 0.4 | 0.4 | 2.8 (1.7-4.6) | 2.7 (1.6-4.5) |
| Noncore | 7.9 | 9.5 | 0.6 (0.6-0.7) | 0.8 (0.7-0.9) | 2.8 | 3.0 | 0.3 (0.2-0.3) | 0.3 (0.3-0.4) | 4.1 | 5.9 | 2.2 (1.8-2.6) | 2.6 (2.2-3.0) | 0.8 | 0.5 | 5.2 (3.2-8.3) | 3.1 (1.7-5.4) |
Abbreviation: IRR, incidence rate ratio.
Race and ethnicity were self-reported or self-selected.
The other category included Native Hawaiian or Other Pacific Islander and ≥2 races.
For analyses, county urbanicity was coded as a categorical variable, either urban (large central metropolitan, large fringe metropolitan, medium metropolitan, and small metropolitan) or rural (micropolitan or noncore).
In 2007, non-Hispanic Black youth had a total firearm-related mortality rate that was 5.9 times (95% CI, 5.6-6.2) higher than the rate for non-Hispanic White youths; this rate narrowed to 4.8 times (95% CI, 4.6-5.1) in 2016. Among non-Hispanic Black youth, the homicide rate was 19.1 times (95% CI, 17.5-20.8) greater than that for non-Hispanic White youth in 2016 (Table 2).
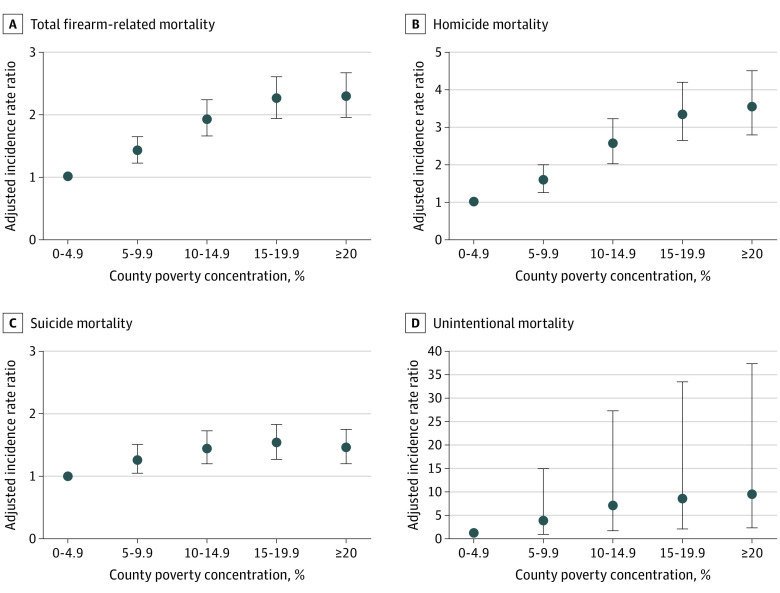
Firearm-Related Deaths and Poverty
Youth living in counties with the highest poverty concentration (≥20%) had 4.3 times (95% CI, 3.4-5.5) higher rate of total firearm-related deaths in 2007 and 4.6 times (95% CI, 2.9-7.7) higher rate in 2016 compared with those living in counties with the lowest poverty concentration (0%-4.9%). Youth in counties with the highest poverty level had 6.3 times (95% CI, 4.6-8.9) higher rate of homicides in 2007, with a greater than 3-fold increase to 20.9 times (95% CI, 7.1-101.0) higher rate in 2016 compared with the rates in counties with the lowest poverty concentration (Table 3). For firearm-related total deaths and homicides, the inequity in counties with the highest poverty concentration persisted throughout each year of the study. This inequity was less pronounced for firearm-related suicides and was not consistently detected over time. The counties with the highest poverty concentration persistently had the highest rates of unintentional firearm-related deaths (Figure 1).
Table 3. Mortality Rates and Incidence Rate Ratios for Total Firearm-Related Deaths and Specific Intents Stratified by County-Level Poverty Concentration.
| County poverty concentration, % | Total firearm-related deaths | Homicides | Suicides | Unintentional deaths | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | Rate per 100 000 youths | IRR (95% CI) | |||||||||
| 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | 2007 | 2016 | |
| 0-4.9 | 3.2 | 2.9 | 1 [Reference] | 1 [Reference] | 1.7 | 0.5 | 1 [Reference] | 1 [Reference] | 1.5 | 2.5 | [1 [Reference] | 1 [Reference] | 0 | 0 | 0.5 (0-2.8) | 0 (0-6.9) |
| 5-9.9 | 4.8 | 5.6 | 1.5 (1.2-1.9) | 1.9 (1.2-3.1) | 2.7 | 2.4 | 1.5 (1.1-2.2) | 5.2 (1.8-25.3) | 1.9 | 3.0 | 1.3 (0.9-1.9) | 1.2 (0.7-2.1) | 0.1 | 0.1 | 1 [Reference]a | 1 [Reference]a |
| 10-14.9 | 8.7 | 7.7 | 2.7 (2.1-3.4) | 2.6 (1.7-4.4) | 6.0 | 3.8 | 3.4 (2.5-4.9) | 8.1 (2.8-39.5) | 2.4 | 3.7 | 1.6 (1.2-2.4) | 1.5 (0.9-2.6) | 0.2 | 0.2 | 2.2 (1.3-3.8) | 2.0 (1.1-3.6) |
| 15-19.9 | 10.9 | 11.7 | 3.4 (2.7-4.3) | 4 (2.5-6.6) | 7.6 | 8.0 | 4.4 (3.2-6.2) | 17.3 (5.9-83.9) | 2.8 | 3.3 | 1.9 (1.3-2.8) | 1.3 (0.8-2.3) | 0.4 | 0.2 | 3.7 (2.2-6.3) | 2.4 (1.4-4.3) |
| ≥20 | 14.0 | 13.6 | 4.3 (3.4-5.5) | 4.6 (2.9-7.7) | 10.9 | 9.7 | 6.3 (4.6-8.9) | 20.9 (7.1-101.0) | 2.3 | 3.4 | 1.6 (1.1-2.4) | 1.4 (0.8-2.4) | 0.5 | 0.3 | 5.4 (3.1-9.6) | 3.2 (1.7-6.2) |
Abbreviation: IRR, incidence rate ratio.
Given the low incidence of unintentional firearm-related deaths, counties with a poverty concentration of 5% to <10% were used as a referent for unintentional firearm-related deaths.
Figure 1. Incident Rate Ratio for Youth Firearm-Related Mortality Stratified by County-Level Poverty Concentration, 2007-2016.
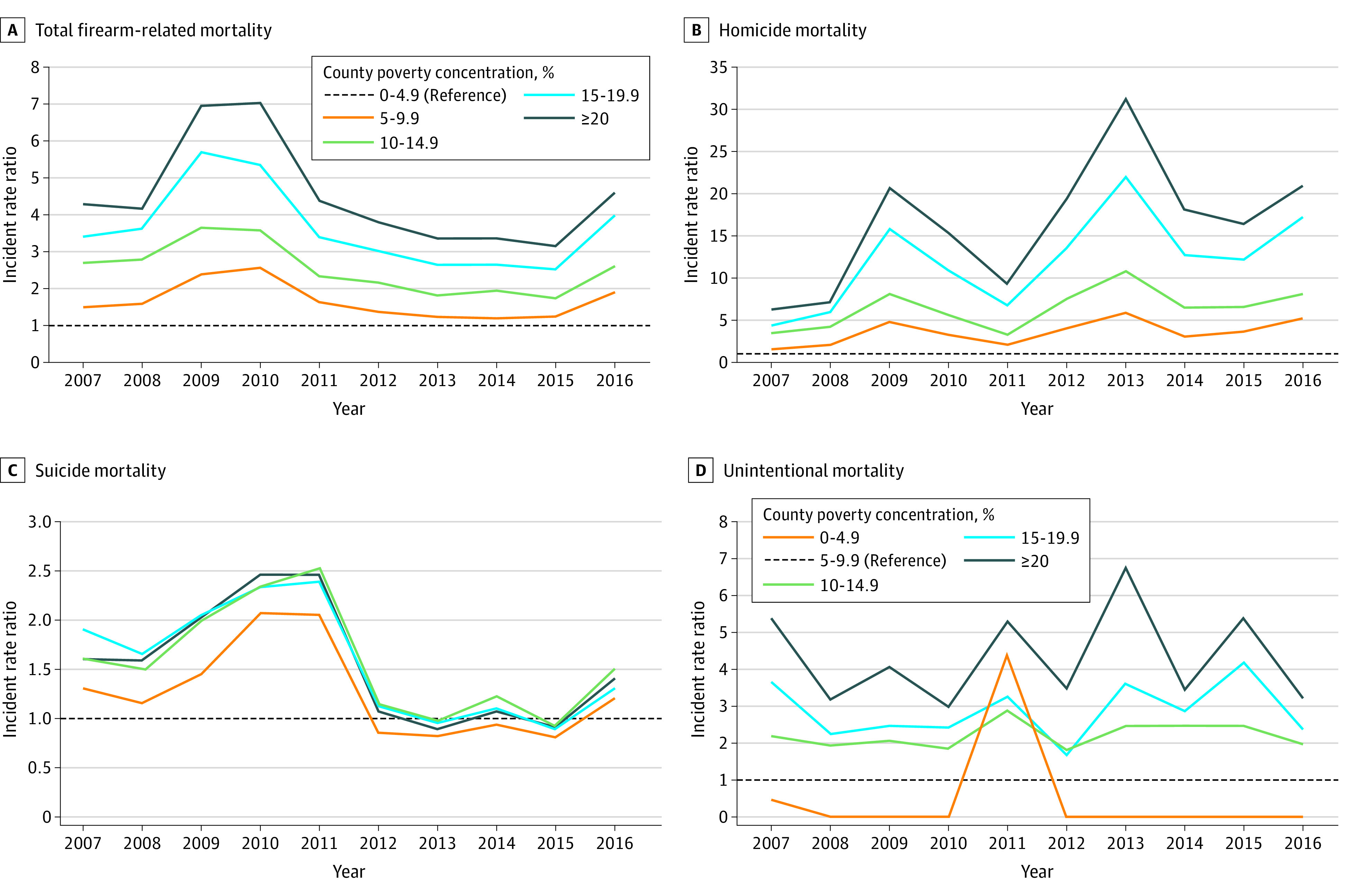
Multivariable Analysis of Firearm-Related Deaths and Poverty
In the multivariable modeling, which controlled for demographic variables, urbanicity, and statewide firearm prevalence, we observed higher rates of total firearm-related deaths, homicides, suicides, and unintentional deaths among the youth in counties with higher poverty concentration compared with counties with lower poverty concentration. These rates increased in a stepwise manner by poverty concentration level, and this same pattern was demonstrated for all intents except for a small decrease in suicide rates between the 2 most impoverished county categories. Youths who were living in counties with the highest poverty concentration compared with counties with the lowest poverty concentration had higher rates of total firearm-related deaths (adjusted IRR, 2.29; 95% CI, 1.96-2.67), homicides (adjusted IRR, 3.55; 95% CI, 2.80-4.51), suicides (adjusted IRR, 1.45; 95% CI, 1.20-1.75), and unintentional deaths (adjusted IRR, 9.32; 95% CI, 2.32-37.4) (eTable 2 in the Supplement; Figure 2).
Figure 2. Adjusted Incident Rate Ratio for Youth Firearm-Related Mortality Stratified by County-Level Poverty Concentration.
Model 3 was adjusted for demographic characteristics, county urbanicity, and statewide firearm prevalence.
PAF for Firearm-Related Deaths
To identify the percentage of deaths that may not have occurred if all US youth had the same risk as those who lived in counties with the lowest poverty concentration, we calculated the PAF for each regression model (eTable 2 in the Supplement). The PAF in model 3 was 0.51 (95% CI, 0.43-0.57) for all firearm-related deaths, 0.66 (95% CI, 0.57-0.73) for homicides, 0.30 (95% CI, 0.17-0.42) for suicides, and 0.86 (95% CI, 0.46-0.97) for unintentional deaths. This calculation represents a total of 34 292 excess firearm-related deaths associated with high level of county poverty. Over the 10-year study period, we observed 3 833 105 years of potential life lost in youth aged 5 to 24 years from firearm-related deaths, including 2 398 974 from homicides, 1 296 850 from suicides, and 95 207 from unintentional deaths.
Discussion
In this cross-sectional study of firearm-related deaths over a 10-year period, higher county poverty concentration was associated with higher rates of death from firearms among US youth, including total firearm-related deaths, homicides, suicides, and unintentional deaths. These inequities persisted throughout the study period for total firearm-related deaths and homicides.
The findings showed the association between poverty and youth firearm-related deaths across all intents and that mortality rates increased in a stepwise fashion with poverty concentration increases. In addition, this study adds to the literature by demonstrating that these mortality rates were consistent even after controlling for demographic variables, county urbanicity, and statewide firearm prevalence. These findings are consistent with the results of previous work, which found that counties with greater socioeconomic deprivation had higher all-cause youth mortality.26 The results were specific to firearm-related deaths and supported the findings of previous studies that rates of all-cause homicides, suicides, and unintentional injury mortality were higher in impoverished counties.8,10,26 To our knowledge, this study was the first to calculate a PAF to describe the firearm-related mortality inequity by poverty concentration. We estimated that more than half of all firearm-related deaths and two-thirds of all firearm-related homicides could be associated with living in a county with higher poverty concentration. In total, nearly 4 million years of potential life were lost among US youth during the 10-year study period.
Substantial inequities in firearm-related mortality rates exist among different racial and ethnic groups, especially Alaska Native or American Indian and non-Hispanic Black groups, as found in previous studies.27,28,29,30,31,32,33,34,35 Youths who were living in rural counties were at a lower risk of firearm-related homicides but a higher risk of firearm-related suicides and unintentional deaths, which is consistent with results of other studies.10,36 This inequity may be owing to limited access to mental health services, increased access to lethal means, social isolation, and changing socioeconomic factors of rural communities.10,36,37 The large 95% CIs observed in unintentional deaths were likely owing to the relatively small number of overall unintentional deaths in this study.
This study emphasized the urgency of addressing the high risk of firearm-related deaths among youth in communities with a high concentration of poverty. Poverty disproportionally affects young people in the US, wherein 1 in 6 children younger than 18 years and nearly 1 in 5 adults aged 18 to 24 years live in poverty.38 There are also pronounced poverty inequities by race and ethnicity, with 10% of Asian and non-Hispanic White children, 23% of Hispanic children, 30% of American Indian children, and 31% of non-Hispanic Black children experiencing poverty.39
The implications of poverty are complex and multifactorial at the individual, household, and societal or community levels. Children living in high poverty concentration neighborhoods often have inadequate housing and limited access to high-quality educational opportunities as well as increased exposure to toxic stress and adverse childhood experiences, which have been associated with negative child health outcomes.40,41 Historical studies have pointed more to an individual’s reaction to absolute resource deprivation than to income equality (or relative deprivation) as a factor in violent crime. Furthermore, a lack of social cohesion or social capital, often described as the level of mutual trust among members of society, has been proposed as a potential explanation for the association between poverty and firearm violence.42,43
Decreasing firearm-related deaths in youth living in poverty requires a multipronged prevention effort that addresses poverty and firearm access at all levels. At the individual level, interventions to prevent violence may include cognitive-behavioral interventions and social skills training.28 At the household and societal or community levels, interventions may include prioritizing safety-net programs, such as the Child Tax Credit; Temporary Assistance for Needy Families; Head Start; and the Special Supplemental Nutrition Program for Women, Infants, and Children. Furthermore, standardizing a living wage and strengthening the Children’s Health Insurance Program, which has been associated with better access to and improved quality of health care, are needed.44,45,46,47,48 At the state and national levels, multiple studies have reported on the success and importance of firearm regulation legislation.27,49,50,51,52,53,54,55,56
Additional research is warranted to better elucidate how the risk of firearm-related death may change along with changes in the poverty concentration of a community over time, as well as how the risk conferred by the length of time spent in a community with a high poverty level may modulate one’s risk of firearm-related death. Although this study focused on firearm-related deaths, most people who experience firearm violence survive but with substantial detrimental physical, mental health, and community-related outcomes.57,58 Survivors of firearm violence compared with the general population have higher health care and intensive care unit utilization rates, higher rates of alcohol and substance use disorder, and greater risk of posttraumatic stress disorder.57,58,59,60,61
Limitations
This study has several limitations. First, as an ecological study, it may be subject to the bias inherent to this design; thus, we reported only associations, not causation. The implications of poverty are multifactorial, and we were unable to fully account for the mechanisms through which county-level poverty concentration may lead to a higher risk of firearm-related death. Second, because the Compressed Mortality File is an administrative database, demographic variables or causes and intents of death could have been misclassified.62,63 Third, counties are often heterogenous, containing neighborhoods with varying levels of poverty. The database does not include income-related data about the youths themselves; therefore, we could not distinguish the implications of individual-level poverty vs county-level poverty. Thus, we may have underestimated or overestimated the association of county-level poverty with the risk of firearm-related death. Fourth, the RAND Corporation’s firearm prevalence estimates are statewide estimates and do not account for the variability that likely exists at the county level or for illicit firearm ownership. Fifth, the equation for PAF considers the prevalence of the exposure and the relative risk. During the study period, there was a shift in the number of counties in each poverty category. This increase in exposure can increase the PAF without changing the relative risk. Caution is advised in interpreting the PAF as a causal statement about county poverty.
Conclusions
In this 10-year analysis of firearm-related deaths among US youth aged 5 to 24 years, we found that higher county-level poverty concentration was associated with increased rates of total firearm-related deaths, homicides, suicides, and unintentional deaths. Furthermore, more than half of all firearm-related deaths and two-thirds of all firearm-related homicides in this age group could be associated with living in a county with a higher concentration of poverty. In a time of greater socioeconomic inequities, the findings highlighted the potential deleterious implications of concentrated county poverty for the risk of youth firearm-related deaths. This study adds to the growing body of evidence that shows the association between county-level poverty concentration and adverse health outcomes and that emphasizes the urgency for a multidimensional strategy for reducing poverty and firearm-related deaths among the youth population.
eTable 1. Mortality Rates and Incidence Rate Ratios for Total Firearm-Related Deaths and Specific Intents, by Age and Sex in 2007 & 2016.
eTable 2. Adjusted Incidence Rate Ratios for Total Firearm Related and Specific Causes by County-Poverty Concentration
References
- 1.Centers for Disease Control and Prevention . Wide-ranging Online Data for Epidemiologic Research (WONDER). Accessed March 31, 2021. https://wonder.cdc.gov/
- 2.Lee LK, Mannix R. Increasing fatality rates from preventable deaths in teenagers and young adults. JAMA. 2018;320(6):543-544. doi: 10.1001/jama.2018.6566 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . WISQARS (Web-Based Injury Statistics Query and Reporting System). Choice Reviews. 2011;48(08):48-4227. [Google Scholar]
- 4.Centers for Disease Control and Prevention . Leading causes of injury death highlighting violence. WISQARS. Accessed March 31, 2021. https://webappa.cdc.gov/sasweb/ncipc/mortrate.html
- 5.Richardson EG, Hemenway D. Homicide, suicide, and unintentional firearm fatality: comparing the United States with other high-income countries, 2003. J Trauma. 2011;70(1):238-243. doi: 10.1097/TA.0b013e3181dbaddf [DOI] [PubMed] [Google Scholar]
- 6.Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266-273. doi: 10.1016/j.amjmed.2015.10.025 [DOI] [PubMed] [Google Scholar]
- 7.Grinshteyn E, Hemenway D.. Chapter 6: Firearm violence in the pediatric population: an international perspective. In: Lee LK, Fleegler EW, eds. Pediatric Firearm Injuries and Fatalities: The Clinician’s Guide to Policies and Approaches to Firearm Harm Prevention. Springer International Publishing; 2021:75-85. doi: 10.1007/978-3-030-62245-9_6 [DOI] [Google Scholar]
- 8.Karb RA, Subramanian SV, Fleegler EW. County poverty concentration and disparities in unintentional injury deaths: a fourteen-year analysis of 1.6 million U.S. fatalities. PLoS One. 2016;11(5):e0153516. doi: 10.1371/journal.pone.0153516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roos LL, Wall-Wieler E, Lee JB, Lee JB. Poverty and early childhood outcomes. Pediatrics. 2019;143(6):e20183426. doi: 10.1542/peds.2018-3426 [DOI] [PubMed] [Google Scholar]
- 10.Hoffmann JA, Farrell CA, Monuteaux MC, Fleegler EW, Lee LK. Association of pediatric suicide with county-level poverty in the United States, 2007-2016. JAMA Pediatr. 2020;174(3):287-294. doi: 10.1001/jamapediatrics.2019.5678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farrell CA, Fleegler EW, Monuteaux MC, Wilson CR, Christian CW, Lee LK. Community poverty and child abuse fatalities in the United States. Pediatrics. 2017;139(5):e20161616. doi: 10.1542/peds.2016-1616 [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention, National Center for Health Statistics . Compressed Mortality File, 1999-2016. CD-ROM. Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 13.US Census Bureau . County intercensal datasets: 2000-2010. Accessed September 15, 2019. https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000-2010-counties.html
- 14.US Census Bureau . Population estimates by age, sex, race and Hispanic origin. June 21, 2018. Accessed September 15, 2019. https://www.census.gov/newsroom/press-kits/2018/estimates-characteristics.html
- 15.US Census Bureau . Small Area Income and Poverty Estimates (SAIPE) program. Accessed September 15, 2019. https://www.census.gov/programs-surveys/saipe.html
- 16.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1-73. [PubMed] [Google Scholar]
- 17.Schell TL, Peterson S, Vegetabile BG, Scherling A, Smart R, Morral AR. State-Level Estimates of Household Firearm Ownership. RAND Corporation; 2020.
- 18.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312-323. doi: 10.2105/AJPH.2003.032482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krieger N, Waterman PD, Chen JT, Soobader M-J, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US). Public Health Rep. 2003;118(3):240-260. doi: 10.1093/phr/118.3.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus ZIP code analyses. J Public Health Manag Pract. 2021;27(Suppl 1, COVID-19 and Public Health: Looking Back, Moving Forward):S43-S56. doi: 10.1097/PHH.0000000000001263 [DOI] [PubMed] [Google Scholar]
- 21.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. Am J Public Health. 2003;93(10):1655-1671. doi: 10.2105/AJPH.93.10.1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Census Bureau . Poverty thresholds. Accessed September 15, 2019. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
- 23.Probst J, Zahnd W, Breneman C. Declines in pediatric mortality fall short for rural US children. Health Aff (Millwood). 2019;38(12):2069-2076. doi: 10.1377/hlthaff.2019.00892 [DOI] [PubMed] [Google Scholar]
- 24.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: Geographic disparities in trauma mortality. Surgery. 2016;160(6):1551-1559. doi: 10.1016/j.surg.2016.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention, National Center for Health Statistics . Life expectancy. Accessed October 1, 2019. https://www.cdc.gov/nchs/fastats/life-expectancy.htm
- 26.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. J Urban Health. 2013;90(3):388-405. doi: 10.1007/s11524-012-9744-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Resnick S, Smith RN, Beard JH, et al. Firearm deaths in America: can we learn from 462,000 lives lost? Ann Surg. 2017;266(3):432-440. doi: 10.1097/SLA.0000000000002376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dahlberg LL. Youth violence in the United States. J Okla State Med Assoc. 2000;93(11):526-527. doi: 10.1016/s0749-3797(98)00009-9 [DOI] [PubMed] [Google Scholar]
- 29.Cunningham RM, Walton MA, Carter PM. The major causes of death in children and adolescents in the United States. N Engl J Med. 2018;379(25):2468-2475. doi: 10.1056/NEJMsr1804754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fowler KA, Dahlberg LL, Haileyesus T, Gutierrez C, Bacon S. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1):e20163486. doi: 10.1542/peds.2016-3486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riddell CA, Harper S, Cerdá M, Kaufman JS. Comparison of rates of firearm and nonfirearm homicide and suicide in black and white non-Hispanic men, by U.S. State. Ann Intern Med. 2018;168(10):712-720. doi: 10.7326/M17-2976 [DOI] [PubMed] [Google Scholar]
- 32.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5-14. doi: 10.1016/j.ypmed.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pressley JC, Barlow B, Kendig T, Paneth-Pollak R. Twenty-year trends in fatal injuries to very young children: the persistence of racial disparities. Pediatrics. 2007;119(4):e875-e884. doi: 10.1542/peds.2006-2412 [DOI] [PubMed] [Google Scholar]
- 34.Kalesan B, Galea S. Patterns of gun deaths across US counties 1999-2013. Ann Epidemiol. 2017;27(5):302-307.e3. doi: 10.1016/j.annepidem.2017.04.004 [DOI] [PubMed] [Google Scholar]
- 35.Herne MA, Bartholomew ML, Weahkee RL. Suicide mortality among American Indians and Alaska Natives, 1999-2009. Am J Public Health. 2014;104(suppl 3):S336-S342. doi: 10.2105/AJPH.2014.301929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fontanella CA, Hiance-Steelesmith DL, Phillips GS, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatr. 2015;169(5):466-473. doi: 10.1001/jamapediatrics.2014.3561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nance ML, Carr BG, Kallan MJ, Branas CC, Wiebe DJ. Variation in pediatric and adolescent firearm mortality rates in rural and urban US counties. Pediatrics. 2010;125(6):1112-1118. doi: 10.1542/peds.2009-3219 [DOI] [PubMed] [Google Scholar]
- 38.Statista. Poverty rate in the United States in 2019, by age and gender. Accessed March 9, 2021. https://www.statista.com/statistics/233154/us-poverty-rate-by-gender/
- 39.The Annie E. Casey Foundation, KIDS COUNT Data Center . Children in poverty by race and ethnicity in the United States. Accessed April 5, 2021. https://datacenter.kidscount.org/data/tables/44-children-in-poverty-by-race-and-ethnicity#detailed/1/any/false/1729,37,871,870,573,869,36,868,867,133/10,11,9,12,1,185,13/324,323
- 40.Pascoe JM, Wood DL, Duffee JH, Kuo A, et al; Committee on Psychosocial Aspects of Child and Family Health; Council on Community Pediatrics . Mediators and adverse effects of child poverty in the United States. Pediatrics. 2016;137(4):e20160340. doi: 10.1542/peds.2016-0340 [DOI] [PubMed] [Google Scholar]
- 41.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232-e246. doi: 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 42.Arthur JA. Socioeconomic predictors of crime in rural Georgia. Crim Justice Rev. 1991;16(1):29-41. doi: 10.1177/073401689101600106 [DOI] [Google Scholar]
- 43.Kennedy BP, Kawachi I, Prothrow-Stith D, Lochner K, Gupta V. Social capital, income inequality, and firearm violent crime. Soc Sci Med. 1998;47(1):7-17. doi: 10.1016/S0277-9536(98)00097-5 [DOI] [PubMed] [Google Scholar]
- 44.Council on Community Pediatrics . Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. doi: 10.1542/peds.2016-0339 [DOI] [PubMed] [Google Scholar]
- 45.Halfon N, Larson K, Son J, Lu M, Bethell C. Income inequality and the differential effect of adverse childhood experiences in US children. Acad Pediatr. 2017;17(7S):S70-S78. doi: 10.1016/j.acap.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 46.Dube A. Minimum wages and the distribution of family incomes. Am Econ J Appl Econ. 2019;11(4):268-304. doi: 10.1257/app.20170085 [DOI] [Google Scholar]
- 47.Feinberg E, Swartz K, Zaslavsky A, Gardner J, Walker DK. Family income and the impact of a children’s health insurance program on reported need for health services and unmet health need. Pediatrics. 2002;109(2):E29. doi: 10.1542/peds.109.2.e29 [DOI] [PubMed] [Google Scholar]
- 48.Hemenway D, Miller M. Firearm availability and homicide rates across 26 high-income countries. J Trauma. 2000;49(6):985-988. doi: 10.1097/00005373-200012000-00001 [DOI] [PubMed] [Google Scholar]
- 49.Fleegler EW, Lee LK, Monuteaux MC, Hemenway D, Mannix R. Firearm legislation and firearm-related fatalities in the United States. JAMA Intern Med. 2013;173(9):732-740. doi: 10.1001/jamainternmed.2013.1286 [DOI] [PubMed] [Google Scholar]
- 50.Lee LK, Fleegler EW, Farrell C, et al. Firearm laws and firearm homicides: a systematic review. JAMA Intern Med. 2017;177(1):106-119. doi: 10.1001/jamainternmed.2016.7051 [DOI] [PubMed] [Google Scholar]
- 51.Siegel M, Pahn M, Xuan Z, Fleegler E, Hemenway D. The impact of state firearm laws on homicide and suicide deaths in the USA, 1991-2016: a panel study. J Gen Intern Med. 2019;34(10):2021-2028. doi: 10.1007/s11606-019-04922-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Conner KR, Zhong Y. State firearm laws and rates of suicide in men and women. Am J Prev Med. 2003;25(4):320-324. doi: 10.1016/S0749-3797(03)00212-5 [DOI] [PubMed] [Google Scholar]
- 53.Azad HA, Monuteaux MC, Rees CA, et al. Child access prevention firearm laws and firearm fatalities among children aged 0 to 14 years, 1991-2016. JAMA Pediatr. 2020;174(5):463-469. doi: 10.1001/jamapediatrics.2019.6227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Monuteaux MC, Azrael D, Miller M. Association of increased safe household firearm storage with firearm suicide and unintentional death among US youths. JAMA Pediatr. 2019;173(7):657-662. doi: 10.1001/jamapediatrics.2019.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kivisto AJ, Phalen PL. Effects of risk-based firearm seizure laws in Connecticut and Indiana on suicide rates, 1981-2015. Psychiatr Serv. 2018;69(8):855-862. doi: 10.1176/appi.ps.201700250 [DOI] [PubMed] [Google Scholar]
- 56.Goyal MK, Badolato GM, Patel SJ, Iqbal SF, Parikh K, McCarter R. State gun laws and pediatric firearm-related mortality. Pediatrics. 2019;144(2):e20183283. doi: 10.1542/peds.2018-3283 [DOI] [PubMed] [Google Scholar]
- 57.Pulcini CDC, Goyal MK, Hall M, et al. Retracted nonfatal firearm injuries: utilization and expenditures for children pre- and postinjury. Acad Emerg Med. 2021. doi: 10.1111/acem.14318 [DOI] [PubMed] [Google Scholar]
- 58.Pulcini CDC, Goyal MK, Hall M, et al. Mental health utilization and expenditures for children pre-post firearm injury. Am J Prev Med. 2021;61(1):133-135. doi: 10.1016/j.amepre.2021.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vella MA, Warshauer A, Tortorello G, et al. Long-term functional, psychological, emotional, and social outcomes in survivors of firearm injuries. JAMA Surg. 2020;155(1):51-59. doi: 10.1001/jamasurg.2019.4533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Peek-Asa C, Butcher B, Cavanaugh JE. Cost of hospitalization for firearm injuries by firearm type, intent, and payer in the United States. Inj Epidemiol. 2017;4(1):20. doi: 10.1186/s40621-017-0120-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Monuteaux MC, Mannix R, Fleegler EW, Lee LK. Predictors and outcomes of pediatric firearm injuries treated in the emergency department: differences by mechanism of intent. Acad Emerg Med. 2016;23(7):790-795. doi: 10.1111/acem.12986 [DOI] [PubMed] [Google Scholar]
- 62.Arias E, Heron M, Hakes J; National Center for Health Statistics; US Census Bureau . The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat 2. 2016;(172):1-21. [PubMed] [Google Scholar]
- 63.Shain B; Committee on Adolescence . Suicide and suicide attempts in adolescents. Pediatrics. 2016;138(1):e20161420. doi: 10.1542/peds.2016-1420 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Mortality Rates and Incidence Rate Ratios for Total Firearm-Related Deaths and Specific Intents, by Age and Sex in 2007 & 2016.
eTable 2. Adjusted Incidence Rate Ratios for Total Firearm Related and Specific Causes by County-Poverty Concentration