Abstract
Objective:
Negative and positive urgency, anxiety, and depressive symptoms are significant factors of disordered eating (DE) symptoms in early adolescence through young adulthood. However, it is unclear how puberty – a critical developmental milestone that is associated with increased risk for DE symptoms – affects the relationship between these factors and DE symptoms, given that the role of pubertal status has rarely been considered in relation to these associations. Thus, the present study examined whether puberty moderates associations between mood/personality factors and DE in pre-adolescent and adolescent girls.
Method:
Participants included 981 girls (aged 8–16 years) from the Michigan State University Twin Registry. Mood/personality factors, pubertal status, and DE were assessed with self-report questionnaires.
Results:
Puberty significantly moderated associations between several factors (negative urgency, positive urgency, trait anxiety, depressive symptoms) and the cognitive symptoms of DE (e.g., shape/weight concerns, body dissatisfaction). Associations between mood/personality factors and cognitive DE were stronger in girls with more advanced pubertal status. By contrast, no significant moderation effects were detected for mood/personality-dysregulated eating (e.g., binge eating, emotional eating) associations.
Discussion:
Findings identify pubertal development as an important moderator of mood/personality-DE symptom associations, especially for cognitive DE symptoms that are known to predict the later onset of clinical pathology.
Keywords: puberty, negative urgency, positive urgency, trait anxiety, depressive symptoms, shape/weight concerns, body dissatisfaction, dietary restraint
Introduction
Past research has identified numerous factors for clinical eating disorders (i.e., anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder) and their component symptoms (e.g., dietary restraint, binge eating, weight/shape concerns) in females. Some of the strongest factors include mood symptoms and personality characteristics, including anxiety (Kaye et al., 2004), depressive symptoms (Pearson et al., 2017), and negative and positive urgency (the tendency to engage in rash actions in the presence of extreme negative and extreme positive emotions, respectively; Culbert et al., 2015; Kenny et al., 2019; Shope et al., 2020). These factors have been linked to disordered eating (DE) symptoms in both cross-sectional (Booth et al., 2018; Kaye et al., 2004; Schulze et al., 2009; Wallin & Råstam, 2016) and longitudinal research (Davis & Smith, 2018; Le Grange et al., 2014; Pearson et al., 2012).
Although levels of DE symptoms are highest in late adolescence (i.e., ages 16–18) and adulthood (Verschueren et al., 2020), DE symptoms are present earlier in childhood and adolescence and show substantial increases in prevalence across pubertal development (Hildebrandt et al., 2010; Klump et al., 2017; Vannucci et al., 2014). Pubertal development is defined as the relatively brief (i.e., two-to-four-year) timespan in which youth develop primary and secondary sexual characteristics (e.g., breast development), reach skeletal maturity (e.g., growth spurts), and attain reproductive capability (Rogol et al., 2002; Sheehy et al., 1999). Pubertal status refers to an individual’s current phase of pubertal development (e.g., pre-puberty, puberty, post-puberty). The median age of pubertal onset (based on breast gland development) in girls is 8.8–10.3 years of age (Camilla Eckert-Lind et al., 2020), while the median age of menarche (occurs in the last stage of puberty; Petersen et al., 1988) for girls in the United States is 12.25–12.43 years, with earlier ages of onset for girls identifying as Black and Hispanic (Biro et al., 2018; Chumlea et al., 2003). Notably, remarkably little research has examined whether associations between DE symptoms and mood/personality factors also shift across the pubertal period. The lack of research has led to knowledge gaps regarding potential changes in the strength of mood/personality-DE associations and when mood/personality factors are most likely to predict DE symptoms. It may be that mood/personality factors predict DE in post-puberty, but are not predictive in pre-puberty. In this case, additional studies would be critically needed to identify the key, early developmental factors that contribute to DE in pre-puberty, as well as how they might differ from developmental factors that contribute to DE during or after puberty.
To our knowledge, no studies have directly examined differences in mood/personality-DE associations across pubertal development. However, related studies support differential associations (Adams et al., 1993; Davis & Smith, 2018) and DE symptom changes across pubertal development (e.g., Culbert et al., 2009; Klump et al., 2017; Pearson et al., 2012; Vanucci et al., 2014). For example, girls in the 8th and 12th grades reported higher levels of depression and symptoms of DE (e.g., body dissatisfaction) than girls in the 5th grade (Adams et al., 1993). Likewise, Vanucci et al. (2014) found stronger associations between loss of control over eating and weight/shape concerns in girls who were post-pubertal versus pre-pubertal. Although this study did not examine mood/personality factors per se, the observed stronger associations between loss of control eating and DE attitudes across pubertal phases support the possible presence of developmental differences for mood/personality factors as well. Finally, twin research has consistently shown significant shifts in genetic and environmental influences on DE across pubertal development in girls (i.e., increasing genetic and decreasing shared environmental influences; Culbert et al., 2009; Klump, 2013; Klump et al., 2017). These findings further highlight the likely presence of pubertal differences in mood/personality-DE associations, as genetic factors also account for these associations (Racine et al., 2013; Slane et al., 2011).
Given the above, the present study aimed to examine potential differences in associations between mood/personality factors and DE across pubertal status in a large, population-based sample of girls. Various DE symptoms were examined to identify potential differential effects of puberty across symptom type (e.g., cognitive symptoms such as body dissatisfaction/weight concerns and dysregulated eating symptoms such as binge eating), and we examined a range of mood (e.g., anxiety symptoms, depressive symptoms) and personality factors (i.e., negative and positive urgency). Based on past research (e.g., Klump, 2013; Klump et al., 2017; Vanucci et al., 2014), we expected to find stronger associations between DE symptoms and mood/personality factors in girls in later versus earlier pubertal status.
Methods
Participants
The sample consisted of 981 female twins ages 8 to 16 (M(SD) = 11.75 (2.03)) from the Michigan State University Twin Registry (MSUTR). Twins were recruited into the MSUTR using birth records in collaboration with the Michigan Department of Health and Human Services (see Klump & Burt, 2006; Burt & Klump, 2012; Burt & Klump, 2019). The present study used archival data from the Twin Study of Mood, Behavior, and Hormones during Puberty (see O’Connor et al., 2016) within the MSUTR. Because the primary aim of this MSUTR study was to examine ovarian hormone influences on DE, twin participants had to meet several inclusion/exclusion criteria (e.g., no recent psychotropic, steroid, or other medication use that is known to influence hormone functioning). Past studies have shown that MSUTR twins who met inclusion/exclusion criteria for this and other studies (Klump et al., 2013a; 2013b; 2015) are not significantly different from non-participating MSUTR twins in terms of DE symptoms (e.g., weight/shape concerns, body dissatisfaction, over-evaluation of weight/shape, etc.; d’s = .02–.14, all p > .05). The racial/ethnic identification of the current sample (White (83.6%), Black (7.8%), Asian (0.6%), American Indian/Alaskan Native (0.2%), multiracial (7.8%), Latinx/Hispanic (3.8%)) is also representative of the Michigan population, while the median family income (~$60,000-$100,000) is slightly higher (United States Census Bureau, 2019). The university Institutional Review Board approved this study, and all participants provided informed assent and parental consent.
Measures
Disordered Eating Symptoms
Cognitive DE Symptoms were assessed using the body dissatisfaction (BD) and weight preoccupation (WP) subscales from the Minnesota Eating Behavior Survey (MEBS; von Ranson et al., 2005)1, and the dietary restraint and shape/weight concerns subscales from the Youth Eating Disorder Examination-Questionnaire ((Y)EDE-Q; Fairburn & Beglin, 1994; Goldschmidt et al., 2007). We examined both MEBS and EDEQ constructs given previous studies (including in this dataset – see Klump et al., 2010; Klump et al., 2012; O’Connor et al., 2020) suggesting differential associations between weight/shape concerns and other factors in analyses of the MEBS versus YEDE-Q scales.
The MEBS 6-item BD subscale assesses discontent with body shape and size (e.g., feeling parts of body are too big) and 8-item WP subscale assesses cognitions and behaviors related to weight concerns (e.g., fear and monitoring of weight gain). The MEBS is appropriate for use in children as young as eight years old (e.g., Luo et al., 2016; O’Connor et al., 2016). Moreover, individuals with diagnosable eating disorders (e.g., AN, BN) score significantly higher on the MEBS than controls (von Ranson et al., 2005). The BD and WP subscales had internal consistency of .70–.85 in previous studies (von Ranson et al., 2005) and internal consistency of .77 and .78, respectively, in the present sample.
The 36-item YEDE-Q assesses cognitive DE symptoms over the past 28 days, and includes a shape concerns (i.e., dissatisfaction and discomfort with body shape), a weight concerns (i.e., dissatisfaction with weight and desire to lose weight), and a dietary restraint (i.e., avoidance of eating and having dietary rules) subscale. In adolescent samples, the YEDE-Q subscales had internal consistency values of .63–.95 (Jennings & Phillips, 2017; Wade et al., 2008) and correlated highly with scores from the EDE (Binford et al., 2005). Based on prior research (Klump et al., 2010; Wade et al., 2008) and the high correlation (r = .90, p < .001) between the shape concerns and weight concerns subscale, we combined them by averaging their items into one shape/weight concerns subscale for all analyses. Internal consistency was .79 for dietary restraint and .94 for shape/weight concerns in the present sample.
Dysregulated Eating Symptoms were assessed using the MEBS binge eating (BE) subscale (von Ranson et al., 2005), the Eating in the Absence of Hunger for Children (EAH-C) questionnaire (Tanofsky-Kraff et al., 2008), and the Emotional Eating Scale-Adapted for Children and Adolescents (EES-C; Tanofsky-Kraff et al., 2007). We examined all three scales to ensure that we captured the differential expression of dysregulated eating across development (e.g., more emotional eating and loss of control over eating than binge eating in younger versus older children/adolescents; Tanofsky-Kraff et al., 2009; Tanofsky-Kraff, Schvey, & Grilo, 2020).
The 7-item MEBS-BE subscale assesses thoughts about and engagement in BE.. The BE subscale showed internal consistency of .65–.69 in past samples (von Ranson et al., 2005) and internal consistency of .68 in the present sample.
The 14-item EAH-C questionnaire (for individuals ages 6–19) assesses internal and external reasons for eating unrelated to hunger, including negative affect (e.g., feeling sad, angry, anxious), external cues (e.g., eating when others are eating), and fatigue/boredom. Eating in the absence of hunger predicted higher self-reported binge eating during adolescence (Balantekin et al., 2017; Tanofsky-Kraff et al., 2008). Internal consistency ranged from .80–.88 in previous work (Tanofsky-Kraff et al., 2008) and was .87 in the present sample.
The 26-item EES-C assesses the urge to eat to cope with negative emotions (e.g., feeling depressed, unsettled, anxious, angry, and frustrated) and has been validated for use with children ages 8–17 years old. The EES-C demonstrated good convergent and discriminant validity and good test-retest reliability, with internal consistency for the subscales ranging from .83–.95 (Tanofsky-Kraff et al., 2007). Emotional eating scores correlate with established measures of binge eating (r’s = .55–.69) (Racine et al., 2009; van Strien, 2000). Internal consistency for the overall EES-C was .95 in the present sample.
Mood/Personality Factors
Trait anxiety was assessed using the State-Trait Anxiety Inventory for Children (STAI-CH; Spielberger et al., 1983). The STAI-CH is split into the State Anxiety and Trait Anxiety subscales. We examined only the 20-item trait anxiety subscale to capture general proneness to anxious thoughts and behavior (e.g., worries about making mistakes, generally feels troubled, etc.). The trait anxiety subscale had test-retest reliability of .86 and internal consistency ranging from .59–.89 in previous work (Papay & Hedl, 1978; Papay & Spielberger, 1986). Internal consistency for this scale was .88 in the present sample.
Depressive symptoms were assessed using the 27-item Children’s Depression Inventory (CDI; Kovacs, 1985; 1992). Participants endorsed one of three descriptions (for each symptom) that best applied to them during the past two weeks (e.g., sad once in a while, sad many times, or sad all the time). The CDI showed good test-retest reliability and construct validity, with internal consistency ranging from .71–.89 in previous work (Kovacs, 1992; Sitarenios & Kovacs, 1999) and internal consistency at .87 in the present sample. The suicidal ideation item was omitted from this scale.
Negative urgency and positive urgency were assessed using the 40-item UPPS-P Impulsive Behavior Scale for Children (Zapolski et al., 2010), which was derived from the original 59-item UPPS-P scale (Cyders et al., 2007; Whiteside & Lyman, 2001). Although the UPPS-P assesses five impulsive personality trait facets, we focused on negative and positive urgency, as these trait facets have shown the strongest associations with DE symptoms (e.g., Claes et al., 2015; Shope et al., 2020). Internal consistency for these subscales ranged from .80–.95 in previous work (Gunn & Smith, 2010; Kenny et al., 2019; Zapolski & Smith, 2013), and was at .84 for negative urgency and .89 for positive urgency in the present sample.
Pubertal Development
Pubertal development was measured with the self-report Pubertal Development Scale (Petersen et al., 1988) that assesses secondary sex characteristics (e.g., breast development, body hair). Aside from menses, which was coded dichotomously (i.e., 1 or 4), all other items were coded using a 4-point scale (i.e., development (1) has not yet begun, (2) has barely started, (3) is definitely underway, or (4) seems complete). PDS items were averaged to create a continuous PDS total score for all analyses (Culbert et al., 2009; O’Connor et al., 2020). Following previous work (Klump et al., 2017), maternal reports on the PDS were used for participants with missing PDS scores because they responded “don’t know” to any item on the PDS (n = 103, 10.5 % of total sample; the majority between the ages of 8–10); maternal- and child-reported PDS scores correlated highly in our sample (r = .88). PDS scores correlate with physician ratings (r = .61–.67) and exhibited internal consistency between .76–.83 in past studies (Petersen et al., 1988) and internal consistency of .84 in the present sample.
Covariate
Body mass index (BMI) was included as a covariate, as it is associated with DE symptoms (Jones et al., 2001; Keel et al., 1997). BMI was calculated (weight in kg/height in m2) using height and weight measured with a wall-mounted ruler and digital scale, respectively.
Statistical Analyses
Except for the EAH-C questionnaire, all scores were log transformed prior to analysis due to positive skew. A square root transformation was applied to the EAH-C questionnaire, as the log transformation did not normalize positive skew for this measure. Measures that had ≤10% missing items were prorated, and measures with >10% missing items or measures that had any missing items but had fewer than 10 items overall were coded as missing. However, for the MEBS subscales, prorated values were used rather than coded as missing, as there were very few missing values (< 1%), and an examination of the subscale scores with and without prorated scores showed nearly identical means and standard deviations.
Multilevel models (MLMs) were used to examine the moderating effects of pubertal status on associations between the mood/personality factors and each DE outcome. Family relatedness was accounted for in MLMs by nesting a level 1 variable (individual twin) within a level 2 unit (family). Each model included the main effect of the mood/personality factor (e.g., trait anxiety), the main effect of the continuous PDS score, and the interaction between the mood/personality factor and PDS score (e.g., trait anxiety x PDS score interaction). Consistent with previous studies (e.g., Culbert et al., 2009; Klump et al., 2017; O’Connor et al., 2020), BMI was included as a covariate in the MLMs. All variables were standardized prior to analysis to ease interpretation of model estimates. Significant moderation effects were further probed by conducting simple slopes analyses (i.e., examining the relationship between the mood/personality factors and DE symptoms at different levels of pubertal development) using the online tool specific to MLMs (see Preacher et al., 2006). Significance was set at p < .01 for all models due to the number of MLMs conducted.
Results
Descriptive Statistics and Pearson Correlations
Table 1 shows descriptive statistics for all variables. There was adequate variability and severity in the level and range of DE symptoms. Means and SDs for dietary restraint and shape/weight concerns are in line with past studies (Forsén Mantilla et al., 2017; Wade et al., 2008), especially those that included a large age range spanning middle childhood into adolescence. Additionally, 3.8% (2.6% in pre-puberty vs. 6.2% in puberty and/or post-puberty) of participants scored above the MEBS total score clinical cutoff (i.e., total score ≥ 15.55; von Ranson et al., 2005). The percentages of girls in pre-puberty versus puberty/post-puberty were determined using previously established (Culbert et al., 2009; Klump et al., 2003; Petersen et al., 1988) PDS cut points, such that those who had an average PDS score of ≥ 2.5 were considered to be in puberty and post-puberty and those with an average score of < 2.5 were considered to be in pre-puberty. However, it should be noted that the PDS scores were only categorized as such to examine how our data compare to past research that have examined how MEBS scores vary by pubertal status. Otherwise, PDS scores were examined as a continuous variable in all other analyses. The percentages in our data are in line with previously published data for similar age groups but are, understandably, slightly lower than data using higher starting age ranges (e.g., 10 or 11 years) (Culbert et al., 2009; Klump et al., 2010; O’Connor et al., 2020; Spanos et al., 2010).
Table 1.
Descriptive statistics
| Study Measures | Mean | SD | Possible Range | Observed Range |
|---|---|---|---|---|
| Covariate and Moderator | ||||
| Body Mass Index | 19.49 | 4.47 | -- | 11–47 |
| Pubertal Development Scale | 2.23 | 0.89 | 1–4 | 1–4 |
| Cognitive Symptoms | ||||
| Dietary Restraint (YEDE-Q) | 0.47 | 0.80 | 0–6 | 0–5.4 |
| Shape/Weight Concerns (YEDE-Q) | 0.75 | 1.06 | 0–6 | 0–5.58 |
| Body Dissatisfaction (MEBS) | 0.93 | 1.46 | 0–6 | 0–6 |
| Weight Preoccupation (MEBS) | 1.71 | 1.99 | 0–8 | 0–8 |
| Dysregulated Eating Symptoms | ||||
| Binge Eating (MEBS) | 0.88 | 1.32 | 0–7 | 0–7 |
| Emotional Eating Total Score | 0.50 | 0.44 | 1–5 | 0–2.27 |
| Eating in the Absence of Hunger Total Score | 1.16 | 0.28 | 1–5 | 0–1.99 |
| Mood/Personality Factors | ||||
| Negative Urgency | 2.02 | 0.65 | 1–4 | 1–3.88 |
| Positive Urgency | 1.99 | 0.68 | 1–4 | 1–4 |
| Trait Anxiety | 33.15 | 7.39 | 20–60 | 20–60 |
| Depressive Symptoms | 6.90 | 6.57 | 0–52 | 0–42.58 |
Note. SD = Standard Deviation; YEDE-Q = Youth Eating Disorder Examination-Questionnaire; MEBS = Minnesota Eating Behavior Survey
Pearson correlations were computed to provide an initial indication of associations among pubertal status, mood/personality factors, and DE symptoms (Table 2). Pubertal status was significantly, positively correlated with all variables (e.g., BMI, mood/personality factors, and DE symptoms; r’s = .07–.79; p’s < .05–.001). Although associations were mainly in the small-to-medium effect size range, this is consistent with prior studies showing that girls who are further along in their pubertal development report higher DE symptom levels (e.g., Culbert et al., 2013; Klump et al., 2017; O’Connor et al., 2020; Pearson et al., 2012). All predictor variables were also significantly and positively correlated with all DE symptoms (r’s = .18–.47; p’s < .001). Moreover, the intercorrelations among cognitive DE scales (r = .46–.70, 21–48% shared variance) and dysregulated eating scales (r = .41–.45 (17%−20% shared variance) were moderate-to-large in magnitude. This indicates that the various measures used capture both shared and unique variance for the different DE symptoms assessed.
Table 2.
Pearson correlations
| Study Measures | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | |||||||||||||
| 2. BMI | .44** | -- | ||||||||||||
| 3. Pubertal Development Scale | .79** | .52** | -- | |||||||||||
| 4. Dietary Restraint (YEDE-Q) | .03 | .31** | .16** | -- | ||||||||||
| 5. Shape/Weight Concerns (YEDE-Q) | .20** | .46** | .30** | .70** | -- | |||||||||
| 6. Body Dissatisfaction (MEBS) | .19** | .45** | .24** | .46** | .68** | -- | ||||||||
| 7. Weight Preoccupation (MEBS) | .04 | .29** | .14** | .60** | .67** | .54** | -- | |||||||
| 8. Binge Eating (MEBS) | .04 | .14** | .12** | .38** | .49** | .34** | .44** | -- | ||||||
| 9. Emotional Eating | .05 | .06 | .12** | .15** | .25** | .16** | .19** | .41** | -- | |||||
| 10. Eating in the Absence of Hunger | .12** | .12** | .19** | .13** | .29** | .22** | .23** | .45** | .43** | -- | ||||
| 11. Negative Urgency | .12** | .10** | .16** | .26** | .37** | .29** | .36** | .47** | .32** | .34** | -- | |||
| 12. Positive Urgency | .02 | .06 | .07* | .23** | .30** | .18** | .32** | .42** | .26** | .28** | .67** | -- | ||
| 13. Trait Anxiety | .12** | .07* | .18** | .26** | .34** | .20** | .35** | .39** | .29** | .30** | .43** | .38** | -- | |
| 14. Depressive Symptoms | .08* | .15** | .13** | .35** | .44** | .39** | .40** | .44** | .29** | .33** | .44** | .40** | .59** | -- |
Note. BMI = Body Mass Index; PDS = Pubertal Development Scale; YEDE-Q = Youth Eating Disorders Examination-Questionnaire; MEBS = Minnesota Eating Behavior Survey-Binge Eating.
p < .05,
p < .01
Moderation Models
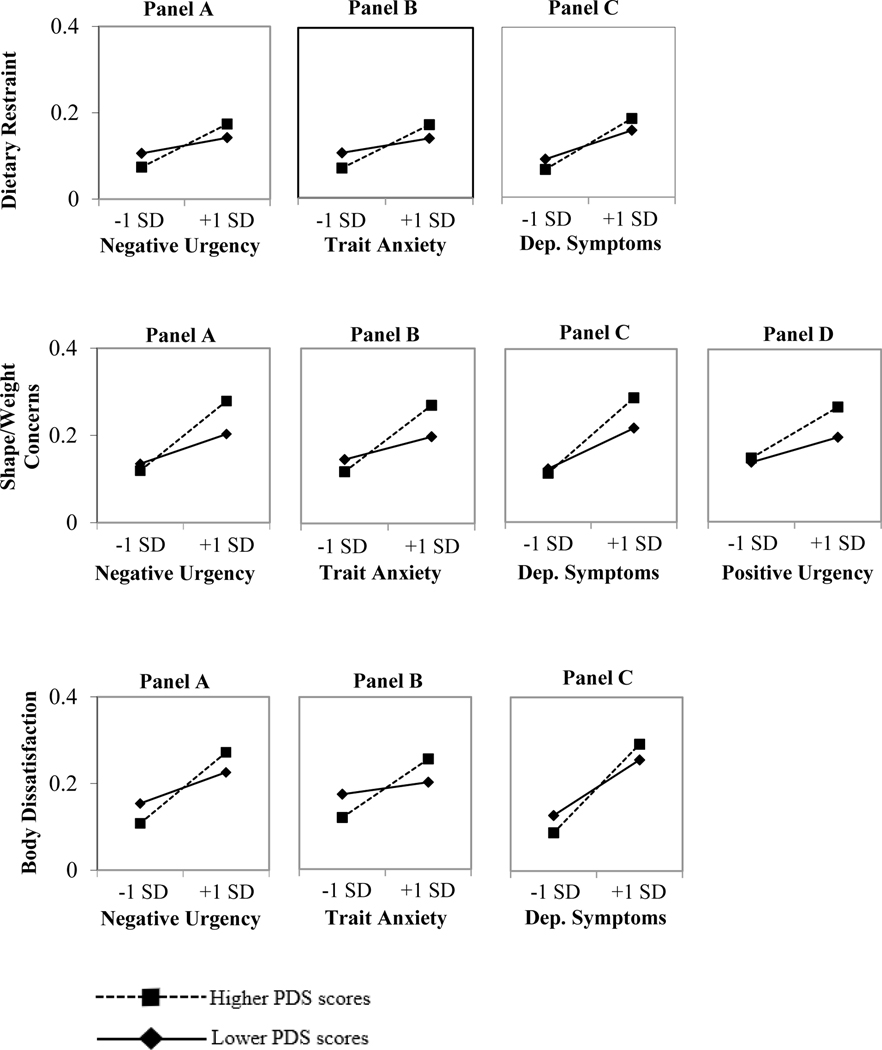
Overall, puberty was found to be a stronger moderator of associations between mood/personality factors and the cognitive DE symptoms than the dysregulated eating symptoms (see Tables 3–4). Although there were no statistically significant effects for weight preoccupation, pubertal status was a significant moderator of associations between dietary restraint, shape/weight concerns, and body dissatisfaction and negative urgency, trait anxiety, and depressive symptoms (Table 3). There was also a statistically significant pubertal status by positive urgency interaction in the prediction of shape/weight concerns. All statistically significant interaction effects were in the expected direction, such that girls who were at more advanced pubertal status and reported higher scores on the mood/personality factors reported the highest levels of cognitive DE symptoms (Figure 1). Surprisingly, there were no statistically significant interactive effects between pubertal status and the mood/personality factors for any of the dysregulated eating symptoms of binge eating, emotional eating, and eating in the absence of hunger (Table 4), although the main effects of mood/personality factors on the dysregulated eating symptoms were all statistically significant.
Table 3.
Moderating effects of pubertal status on associations between mood/personality factors and cognitive disordered eating symptoms (N = 981)
| Dietary Restraint (YEDE-Q) | Shape/Weight Concerns (YEDE-Q) | Body Dissatisfaction (MEBS) | Weight Preoccupation (MEBS) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Model Predictors | b (SE) | t (df) | b (SE) | t (df) | b (SE) | t (df) | b (SE) | t (df) | ||||
| Negative Urgency | ||||||||||||
| BMI | .29 (.04) | 7.62 (797.64) | *** | .39 (.03) | 11.59 (825.80) | *** | .41 (.03) | 11.86 (758.98) | *** | .27 (.04) | 7.31 (824.41) | *** |
| PDS | .00 (.04) | 0.13 (775.24) | .07 (.03) | 2.11 (798.55) | * | .00 (.04) | −0.11 (738.44) | −.03 (.03) | −0.86 (791.85) | |||
| Negative Urgency | .20 (.03) | 6.57 (951.23) | *** | .28 (.03) | 10.54 (948.12) | *** | .23 (.03) | 7.94 (947.90) | *** | .30 (.03) | 10.34 (946.85) | *** |
| PDS × Negative Urgency | .09 (.03) | 3.14 (934.61) | ** | .12 (.03) | 4.43 (921.76) | *** | .09 (.03) | 3.10 (950.74) | ** | .06 (.03) | 2.23 (925.66) | * |
| Positive Urgency | ||||||||||||
| BMI | .28 (.04) | 7.45 (818.30) | *** | .38 (.03) | 10.97 (851.51) | *** | .41 (.04) | 11.48 (788.55) | *** | .27 (.04) | 7.21 (823.40) | *** |
| PDS | .01 (.04) | 0.39 (769.22) | .10 (.04) | 2.85 (797.64) | ** | .03 (.04) | 0.80 (739.14) | −.01 (.04) | −0.34 (771.51) | |||
| Positive Urgency | .18 (.03) | 6.05 (931.94) | *** | .22 (.03) | 8.27 (914.11) | *** | .13 (.03) | 4.56 (947.75) | *** | .26 (.03) | 9.06 (931.27) | *** |
| PDS × Positive Urgency | .07 (.03) | 2.49 (915.94) | * | .07 (.03) | 2.78 (893.79) | ** | .03 (.03) | 0.96 (939.06) | .00 (.03) | 0.08 (913.03) | ||
| Trait Anxiety | ||||||||||||
| BMI | .30 (.04) | 8.03 (785.22) | *** | .41 (.03) | 12.27 (808.77) | *** | .43 (.03) | 12.48 (749.41) | *** | .30 (.04) | 8.24 (807.07) | *** |
| PDS | −.01 (.04) | −0.14 (762.71) | .06 (.03) | 1.65 (781.84) | .00 (.04) | −0.03 (729.95) | −.06 (.04) | −1.59 (775.62) | ||||
| Trait Anxiety | .20 (.03) | 6.58 (949.83) | *** | .25 (.03) | 9.38 (949.67) | *** | .16 (.03) | 5.51 (946.76) | *** | .30 (.03) | 10.17 (948.31) | *** |
| PDS × Trait Anxiety | .10 (.03) | 3.50 (943.93) | *** | .12 (.03) | 4.70 (940.20) | *** | .10 (.03) | 3.69 (950.44) | *** | .05 (.03) | 1.61 (942.87) | |
| Depressive Symptoms | ||||||||||||
| BMI | .26 (.04) | 6.99 (792.50) | *** | .36 (.03) | 11.18 (808.03) | *** | .40 (.03) | 12.03 (743.92) | *** | .25 (.04) | 6.84 (800.78) | *** |
| PDS | .00 (.04) | 0.10 (764.70) | .07 (.03) | 2.20 (774.22) | * | −.01 (.03) | −0.17 (717.15) | −.03 (.04) | −0.72 (763.75) | |||
| Depressive Sx | .27 (.03) | 9.21 (936.95) | *** | .33 (.03) | 12.59 (939.93) | *** | .32 (.03) | 11.55 (923.08) | *** | .33 (.03) | 11.39 (934.69) | *** |
| PDS x Depressive Sx | .07 (.03) | 2.63 (925.59) | ** | .10 (.03) | 3.98 (917.69) | *** | .07 (.03) | 2.73 (936.93) | ** | .02 (.03) | 0.80 (923.94) | |
Note. YEDE-Q = Youth Eating Disorder Examination-Questionnaire; MEBS = Minnesota Eating Behavior Survey; BMI = Body Mass Index; PDS = Pubertal Development Scale; Depressive Sx = Depressive Symptoms. Both statistically significant (p < .01) and trend level (p < .05) models are denoted with asterisks, but those with p < .01 are also bolded for clarity.
p < .05,
p < .01,
p < .001.
Table 4.
Moderating effects of pubertal status on associations between mood/personality factors and dysregulated eating symptoms (N = 981)
| Binge Eating (MEBS) | Emotional Eating (Full Scale) | Eating in the Absence of Hunger (Full Scale) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Model Predictors | b (SE) | t (df) | b (SE) | t (df) | b (SE) | t (df) | |||
| Negative Urgency | |||||||||
| BMI | .09 (.04) | 2.37 (758.49) | * | −.01 (.04) | −0.36 (702.23) | .02 (.04) | 0.53 (899.19) | ||
| PDS | .01 (.04) | 0.19 (736.26) | .08 (.04) | 2.10 (660.89) | * | .12 (.04) | 3.20 (875.51) | *** | |
| Negative Urgency | .44 (.03) | 14.89 (950.26) | *** | .30 (.03) | 9.17 (883.96) | *** | .29 (.03) | 10.24 (886.79) | *** |
| PDS × Negative Urgency | .05 (.03) | 1.60 (953.86) | .01 (.03) | 0.24 (904.03) | .02 (.03) | 0.81 (840.22) | |||
| Positive Urgency | |||||||||
| BMI | .07 (.04) | 1.98 (773.79) | * | −.02 (.04) | −0.46 (728.37) | .03 (.04) | 0.87 (898.71) | ||
| PDS | .05 (.04) | 1.40 (725.56) | .11 (.04) | 2.90 (667.49) | ** | .15 (.04) | 3.79 (852.90) | *** | |
| Positive Urgency | .38 (.03) | 12.92 (955.44) | *** | .24 (.03) | 7.42 (909.37) | *** | .23 (.03) | 8.22 (855.33) | *** |
| PDS × Positive Urgency | .00 (.03) | 0.16 (948.34) | * | −.02 (.03) | −0.48 (911.86) | −.04 (.03) | −1.42 (834.70) | ||
| Trait Anxiety | |||||||||
| BMI | .11 (.04) | 3.05 (762.39) | ** | .00 (.04) | −0.10 (711.60) | .06 (.04) | 1.54 (897.68) | ||
| PDS | .00 (.04) | −0.05 (740.07) | .07 (.04) | 1.93 (671.30) | * | .11 (.04) | 2.74 (874.91) | ** | |
| Trait Anxiety | .35 (.03) | 11.57 (953.37) | *** | .26 (.03) | 8.12 (904.05) | *** | .26 (.03) | 8.94 (883.33) | *** |
| PDS × Trait Anxiety | .07 (.03) | 2.33 (954.95) | * | .04 (.03) | 1.33 (913.31) | .05 (.03) | 1.91 (861.31) | ||
| Depressive Symptoms | |||||||||
| BMI | .05 (.04) | 1.29 (766.35) | −.05 (.04) | −1.38 (722.86) | .01 (.04) | 0.30 (879.67) | |||
| PDS | .03 (.04) | 0.72 (736.58) | .10 (.04) | 2.62 (679.08) | ** | .12 (.04) | 3.25 (851.38) | ** | |
| Depressive Sx | .41 (.03) | 13.63 (935.91) | *** | .28 (.03) | 8.68 (885.28) | *** | .28 (.03) | 9.67 (897.87) | *** |
| PDS × Depressive Sx | .06 (.03) | 2.17 (938.78) | * | .07 (.03) | 2.28 (909.18) | * | .06 (.03) | 2.15 (853.73) | * |
Note. MEBS = Minnesota Eating Behavior Survey; BMI = Body Mass Index; PDS = Pubertal Development Scale; Depressive Sx = Depressive Symptoms. Both statistically significant (p < .01) and trend level (p < .05) models are denoted with asterisks, but those with p < .01 are also bolded for clarity.
p < .05,
p < .01,
p < .001.
Figure 1.
Pubertal status interacting with negative urgency (A Panels), trait anxiety (B Panels), depressive symptoms (C Panels), and positive urgency (D Panel) in predicting cognitive disordered eating symptoms
Simple slopes analyses were conducted to further probe the interaction effects and determine whether the associations were only present in one developmental period (e.g., more advanced pubertal status) or were present across the pubertal development period, but stronger or weaker in one or the other. All simple slopes were statistically significant at p < .001, suggesting that the mood/personality factors were significantly related to the cognitive DE symptoms across the full range of pubertal development. These significant associations highlight the strength of the main effect of these factors (particularly negative urgency, trait anxiety, and depressive symptoms) on cognitive DE symptoms. Nonetheless, results of the simple slopes analyses (and significant interaction effects – see Tables 3–4) indicated that associations between the mood/personality factors and the cognitive DE symptoms were stronger with advancing pubertal development. These data suggest that girls who endorsed higher levels of the mood/personality factors and were at more advanced pubertal status exhibited the highest levels of cognitive DE symptoms.
Discussion
This is the first study to test pubertal status as a moderator of the relationship between key mood/personality factors (i.e., negative and positive urgency, trait anxiety, and depressive symptoms) and various cognitive and dysregulated DE symptoms using a population-based sample of girls. Our analyses revealed three important findings. First, the mood/personality variables were significant factors of cognitive and dysregulated DE symptoms across all stages of pubertal development. These data are consistent with past studies that have shown that some of the factors (particularly negative urgency) identified in late adolescence/early adulthood are also important during pre-adolescence and adolescence in girls. Second, our analyses also revealed that pubertal status significantly moderated associations between mood/personality effects and cognitive DE symptoms, such that girls at more advanced pubertal status and greater negative and positive urgency, trait anxiety, or depressive symptoms showed higher levels of cognitive DE symptoms (i.e., dietary restraint, shape/weight concerns, and body dissatisfaction). And third, puberty did not moderate associations between mood/personality factors and dysregulated eating symptoms, suggesting a specific effect of puberty on the cognitive symptoms of DE. Taken together, our findings underscore the need to consider mood/personality factors in prevention and intervention programs for youth of all ages, but also highlight the importance of puberty for specific types of cognitive DE symptoms that are strong predictors of the later development of clinical eating pathology (e.g., AN, BN; Jacobi, 2005; Stice & Shaw, 2002).
Moving forward, it will be important to identify the mechanisms underlying the differential effects of pubertal status on mood/personality-DE associations. Stronger pubertal moderation for the cognitive symptoms suggests that psychosocial, psychological, and/or biological processes associated with puberty enhance existing mood/personality-DE associations and lead to increased body weight/shape concerns in girls during/after puberty. Puberty is associated with a myriad of physical (e.g., increased adiposity; Bucchianeri et al., 2013; Siervogel et al., 2003), psychological (e.g., increased negative affect; Allen & Matthews, 1997; Spear, 2000), and psychosocial (e.g., increased awareness of culturally-based ideals of thinness; Croll et al., 2002; Knauss et al., 2007) changes that could theoretically potentiate existing mood/personality-DE associations. For example, while negative affect may be associated with body weight/shape concerns in pre-puberty, these associations may be even stronger during/after puberty when awareness of pressures for thinness increases and bodily changes move girls away from Western ideals of beauty. Indeed, the “perfect storm” of increased pressures for thinness and increased negative affect during puberty may strengthen mood/personality-DE associations and increase levels of body weight/shape concerns and dietary restraint in girls. Clearly, these theories are speculative, but they offer one set of potential explanations for the highly specific effects of puberty on mood/personality-DE associations for the DE symptoms (i.e., weight/shape concerns, restraint) that would seemingly be most directly affected by physical and psychosocial changes of puberty.
They also provide some initial insight as to why puberty does not moderate associations between mood/personality factors and dysregulated eating symptoms. The physical and psychosocial changes of puberty may be less directly linked to dysregulated eating symptoms, especially since many types of dysregulated eating (e.g., eating in the absence of hunger, loss of control over eating) are present in children and pre-pubertal girls (Balantekin et al., 2017; Tanofsky-Kraff et al., 2020) prior to the onset of weight/shape concerns (Jacobi et al., 2004; O’Dea & Abraham, 1999) and increased pressures for thinness (Killen et al., 1994; Keel & Forney, 2013; Stice & Shaw, 2002). Thus, the mechanisms of negative affect/personality factor associations with dysregulated eating may be different and less tied to the sociocultural changes of puberty.
One possibility is that the conceptual/empirical model of associations between puberty and mood/personality factors is different for dysregulated eating. An alternative model examined by others (e.g., Combs et al., 2011; Davis & Smith, 2018, Pearson et al., 2012) is that there are mediating (instead of moderating) associations between puberty, mood/personality factors, and dysregulated eating in girls, such that the changes of puberty lead directly to increases in negative affect/impulsivity, which then lead to increases in dysregulated eating. Our data are cross-sectional and are therefore not ideal for examining these hypotheses. Nonetheless, to explore this possibility, we conducted post-hoc mediation analyses and found that negative urgency and trait anxiety were significant, partial mediators of the relationship between pubertal status and the dysregulated eating symptoms of emotional eating and eating in the absence of hunger (On-line Supplemental Material Tables 1–2 and Figure 1). Significant mediation effects were also observed for shape/weight concerns; however, model fit comparisons for this cognitive DE symptom showed that the moderation, rather than mediation, models fit these data best (Supplemental Table 2).
Together, these findings highlight differential effects of puberty across DE symptom type, and although exploratory, they support the possibility that puberty may lead to changes in affect/personality characteristics that then lead to dysregulated (but not cognitive) symptoms of DE in girls. The partial mediation effects also suggest that other (unexamined) factors play a role in the effects of puberty on dysregulated eating. Ovarian hormones (e.g., estrogen, progesterone) are one set of biological factors that may be particularly important, given that they are activated during puberty in girls and have significant effects on anxiety, impulsivity, and dysregulated eating symptoms (Colzato et al., 2010; Diekhof, 2015; Derntl et al., 2014; Hoyt & Falconi, 2015; Reardon et al., 2009; Klump et al., 2018; Zerwas et al., 2014). Furthermore, past data in women demonstrate stronger ovarian hormone effects on binge eating than cognitive weight/shape concerns (Hildebrandt et al., 2015). It may be that ovarian hormones are driving pubertal effects on impulsivity/anxiety and dysregulated eating. This possibility warrants additional study using longitudinal research that can replicate our preliminary mediation models and more clearly identify the factors that may underlie these mediating effects.
Nonetheless, the present study may have some initial implications for clinical practice. The differential effects of puberty across DE symptom type suggest that clinicians may want to more strongly target mood and personality factors in older adolescent clients to enhance outcomes for body weight and shape concerns specifically. By contrast, clinicians should be aware that interventions for dysregulated eating more generally should target mood and personality symptoms regardless of the child’s developmental stage, as these symptoms contribute to dysregulated eating in girls across development. Incorporating these types of developmentally tailored interventions may enhance treatment outcomes and contribute to more personalized medicine approaches to client care.
Before ending, we note a few limitations. First, we cannot make conclusions regarding causality and/or the direction of effects given our use of cross-sectional data. Longitudinal and prospective studies are a critical next step for replicating and extending our data to examine potential risk factor/causation models. Second, we examined a population-based sample of girls, and thus, it is unclear whether results generalize to clinical populations. Given the very low prevalence of clinical eating pathology (e.g., AN and BN) in pre- and early adolescence (Bulik, 2002), it would be difficult to examine our hypotheses in a purely clinical sample of young girls. Our sample exhibited a wide range of DE attitudes and behaviors (including clinical levels of these characteristics). Thus, these findings likely speak to the range of DE present in the population at large. Nonetheless, additional work in clinical samples is needed to determine the generalizability of the findings to clinical eating disorders. Third, our sample was predominantly white and middle class and only included girls. Additional studies of more diverse samples in terms of race, ethnicity, socioeconomic status, and gender are needed to determine if our findings generalize across the myriad of stressors (e.g., discrimination, disadvantage) that contribute to DE in youth.
Supplementary Material
Acknowledgements
This work was supported by a grant awarded to KLK by the National Institute of Mental Health (NIMH) (R01 MH092377). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH.
Footnotes
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The Minnesota Eating Behavior Survey (MEBS; previously known as the Minnesota Eating Disorder Inventory [M-EDI]) was adapted and reproduced by special permission of Psychological Assessment Resources, Inc., 16204 North Florida Avenue, Lutz, FL 33549, from the Eating Disorder Inventory (collectively, EDI and EDI-2) by Garner, Olmstead, and Polivy (1983) by the Psychological Assessment Resources, Inc. Further reproduction of the MEBS is prohibited without prior permission from Psychological Assessment Resources, Inc.
References
- Adams PJ, Katz RC, Beauchamp K, Cohen E, & Zavis D. (1993). Body dissatisfaction, eating disorders, and depression: A developmental perspective. Journal of Child and Family Studies, 2(1), 37–46. doi: 10.1007/BF01321299 [DOI] [Google Scholar]
- Allen MT, & Matthews KA (1997). Hemodynamic responses to laboratory stressors in children and adolescents: The influences of age, race, and gender. Psychophysiology, 34(3), 329–339. doi: 10.1111/j.1469-8986.1997.tb02403.x14 [DOI] [PubMed] [Google Scholar]
- Balantekin KN, Birch LL, & Savage JS (2017). Eating in the absence of hunger during childhood predicts self-reported binge eating in adolescence. Eating Behaviors, 24, 7–10. doi: 10.1016/j.eatbeh.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binford RB, Le Grange D, & Jellar CC (2004). Eating Disorders Examination versus Eating Disorders Examination-Questionnaire in adolescents with full and partial-syndrome bulimia nervosa and anorexia nervosa. International Journal of Eating Disorders, 37(1), 44–49. doi: 10.1002/eat.20062 [DOI] [PubMed] [Google Scholar]
- Biro FM, Pajak A, Wolff MS, Pinney SM, Windham GC, Galvez MP, … Teitelbaum SL (2018). Age of menarche in a longitudinal US cohort. Journal of Pediatric and Adolescent Gynecology, 31(4), 339–345. doi: 10.1016/j.jpag.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth C, Spronk D, Grol M, & Fox E. (2018). Uncontrolled eating in adolescents: The role of impulsivity and automatic approach bias for food. Appetite, 120, 636–643. doi: 10.1016/j.appet.2017.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucchianeri MM, Arikian AJ, Hannan PJ, Eisenberg ME, & Neumark-Sztainer D. (2013). Body dissatisfaction from adolescence to young adulthood: Findings from a 10-year longitudinal study. Body Image, 10, 1–7. doi: 10.1016/j.bodyim.2012.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM (2002). Eating disorders in adolescents and young adults. Child and Adolescent Psychiatric Clinics, 11, 201–218. doi: 10.1016/s1056-4993(01)00004-9 [DOI] [PubMed] [Google Scholar]
- Burt SA, & Klump KL (2012). The Michigan State University Twin Registry (MSUTR): An Update. Twin Research and Human Genetics, 16(1), 344–350. doi: 10.1017/thg.2012.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA, & Klump KL (2019). The Michigan State University Twin Registry (MSUTR): 15 years of twin and family research. Twin Research and Human Genetics, 1–5. doi: 10.1017/thg.2019.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chumlea WC, Schubert CM, Roche AF, Kulin HE, Lee PA, Himes JH, & Sun SS (2003). Age at menarche and racial comparisons in US girls. Pediatrics, 111(1), 110–113. doi: 10.1542/peds.111.1.110 [DOI] [PubMed] [Google Scholar]
- Claes L, Islam MA, Fagundo AB, Jimenez-Murcia S, Granero R, Agüera Z, … Fernández-Aranda F. (2015). The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLOS ONE, 10(5), e0126083. doi: 10.1371/journal.pone.0126083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colzato LS, Hertsig G, van denWildenberg WP, & Hommel B. (2010). Estrogen modulates inhibitory control in healthy human females: Evidence from the stop-signal paradigm. Neuroscience, 167, 709–715. doi: 10.1016/j.neuroscience.2010.02.029 [DOI] [PubMed] [Google Scholar]
- Combs JL, Pearson CM, & Smith GT (2011). A risk model for preadolescent disordered eating. International Journal of Eating Disorders, 44(7), 596–604. doi: 10.1002/eat.20851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croll J, Neumark-Sztainer D, Story M, & Ireland M. (2002). Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: Relationship to gender and ethnicity. Journal of Adolescent Health, 31, 166–175. doi: 10.1016/S1054-139X(02)00368-3 [DOI] [PubMed] [Google Scholar]
- Culbert KM, Breedlove SM, Sisk CL, Burt SA, & Klump KL (2013). The emergence of sex differences in risk for disordered eating attitudes during puberty: A role for prenatal testosterone exposure. Journal of Abnormal Psychology, 122(2), 420–432. doi: 10.1037/a0031791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Burt SA, McGue M, Iacono WG, Klump KL (2009). Puberty and the genetic diathesis of disordered eating attitudes and behaviors. Journal of Abnormal Psychology, 118(4), 788–796. doi: 10.1037/a0017207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Racine SE, & Klump KL (2015). Research Review: What we have learned about the causes of eating disorders - a synthesis of sociocultural, psychological, and biological research. Journal of Child Psychology and Psychiatry, 56(11), 1141–1164. doi: 10.1111/jcpp.12441 [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, & Peterson C. (2007). Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment, 19(1), 107–118. doi: 10.1037/1040-3590.19.1.107 [DOI] [PubMed] [Google Scholar]
- Davis HA, & Smith GT (2018). An integrative model of risk for high school disordered eating. Journal of Abnormal Psychology, 127(6), 559–570. doi: 10.1037/abn0000365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derntl B, Pintzinger N, Kryspin-Exner I, & Schöpf V. (2014). The impact of sex hormone concentrations on decision-making in females and males. Frontiers in Neuroscience, 8, 352. doi: 10.3389/fnins.2014.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diekhof EK (2015). Be quick about it. Endogenous estradiol level, menstrual cycle phase and trait impulsiveness predict impulsive choice in the context of reward acquisition. Hormones and Behavior, 74, 186–193. doi: 10.1016/j.yhbeh.2015.06.001 [DOI] [PubMed] [Google Scholar]
- Eckert-Lind C, Busch AS, Petersen JH, Biro FM, Butler G, Bräuner EV, & Juul A. (2020). Worldwide secular trends in age at pubertal onset assessed by breast development among girls: A systematic review and meta-analysis. JAMA Pediatrics, 174(4), e195881. doi: 10.1001/jamapediatrics.2019.5881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or Self-Report Questionnaire? International Journal of Eating Disorders, 16, 363–370. [PubMed] [Google Scholar]
- Forsén Mantilla E, Birgegård A, & Clinton D. (2017). Factor analysis of the adolescent version of the Eating Disorders Examination Questionnaire (EDE-Q): Results from Swedish general population and clinical samples. Journal of Eating Disorders, 5(1). doi: 10.1186/s40337-017-0140-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, & Polivy J. (1983). Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2(2), 15–34. doi: [DOI] [Google Scholar]
- Goldschmidt AB, Doyle AC, & Wilfley DE (2007). Assessment of binge eating in overweight youth using a questionnaire version of the Child Eating Disorder Examination with Instructions. International Journal of Eating Disorders, 40, 460–467. doi: 10.1002/eat.20387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, & Smith GT (2010). Risk factors for elementary school drinking: pubertal status, personality, and alcohol expectancies concurrently predict fifth grade alcohol consumption. Psychology of Addictive Behaviors, 24(4), 617–627. doi: 10.1037/a0020334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt T, Alfano L, Tricamo M, & Pfaff DW (2010). Conceptualizing the role of estrogens and serotonin in the development and maintenance of bulimia nervosa. Clinical Psychology Review, 30, 655–668. doi: 10.1016/j.cpr.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt BA, Racine SA, Keel PK, Burt SA, Neale M, Boker S, Sisk CL, & Klump KL (2015). The effects of ovarian hormones and emotional eating on changes in weight preoccupation across the menstrual cycle. International Journal of Eating Disorders, 48(5), 477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt LT, & Falconi AM (2015). Puberty and perimenopause: Reproductive transitions and their implications for women’s health. Social Science Medicine, 132, 103–112. doi: 10.1016/j.socscimed.2015.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, 2005. Psychosocial risk factors for eating disorders. In: Wonderlich SA, Mitchell JE, deZwaan M, Steiger H. (Eds.), Eating Disorders Review. Radcliffe Publishing Ltd, Oxford, UK, pp. 59–85. [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19–65. doi: 10.1037/0033-2909.130.1.19 [DOI] [PubMed] [Google Scholar]
- Jennings KM, & Phillips KE (2017). Eating Disorder Examination-Questionnaire (EDE-Q): Norms for clinical sample of female adolescents with anorexia nervosa. Archives of psychiatric nursing, 31(6), 578–581. doi: 10.1016/j.apnu.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JM, Bennett S, Olmsted MP, Lawson ML, Rodin G. (2001). Disordered eating attitudes and behaviours in teenaged girls: A school-based study. Canadian Medical Association Journal, 165(5), 547–552. [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, & Masters K. (2004). Comorbidity of Anxiety Disorders with Anorexia and Bulimia Nervosa. American Journal of Psychiatry, 161(12), 2215–2221. doi: 10.1176/appi.ajp.161.12.2215 [DOI] [PubMed] [Google Scholar]
- Keel PK, & Forney KJ (2013). Psychosocial risk factors for eating disorders. International Journal of Eating Disorders, 46(5), 433–439. doi: 10.1002/eat.22094 [DOI] [PubMed] [Google Scholar]
- Keel PK, Fulkerson JA & Leon GR (1997). Disordered eating precursors in pre- and early adolescent girls and boys. Journal of Youth and Adolescence, 26, 203–216. doi: 10.1023/A:1024504615742 [DOI] [Google Scholar]
- Kenny TE, Singleton C, & Carter JC (2019). An examination of emotion-related facets of impulsivity in binge eating disorder. Eating Behaviors, 32, 74–77. doi: 10.1016/j.eatbeh.2018.12.006 [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, Simmonds B, Robinson TN, Litt I, Varady A, et al. (1994). Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders, 16(3), 227–238. doi: [DOI] [PubMed] [Google Scholar]
- Klump KL (2013). Puberty as a critical risk period for eating disorders: A review of human and animal studies. Hormones and Behavior, 64(2), 399–410. doi: 10.1016/j.yhbeh.2013.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, & Burt SA (2006). The Michigan State University Twin Registry (MSUTR): Genetic, environmental and neurobiological influences on behavior across development. Twin Research and Human Genetics, 9(6), 971–977. doi: 10.1375/183242706779462868 [DOI] [PubMed] [Google Scholar]
- Klump KL, Burt SA, Spanos A, McGue M, Iacono WG, & Wade TD (2010). Age differences in genetic and environmental influences on weight and shape concerns. International Journal of Eating Disorders, 43(8), 679–688. doi: 10.1002/eat.20772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Culbert KM, O’Connor S, Fowler N, & Burt SA (2017). The significant effects of puberty on the genetic diathesis of binge eating in girls. International Journal of Eating Disorders, 50, 984–989. doi: 10.1002/eat.22727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Culbert KM, Slane JD, Burt SA, Sisk CL, & Nigg JT (2012). The effects of puberty on genetic risk for disordered eating: Evidence for a sex difference. Psychological Medicine, 42(3), 627–637. doi: 10.1017/s0033291711001541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Fowler N, Mayhall L, Sisk CL, Culbert KM, & Burt SA (2018). Estrogen moderates genetic influences on binge eating during puberty: Disruption of normative processes? Journal of Abnormal Psychology, 127(5), 458–470. doi: 10.1037/abn0000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Hildebrandt BA, O’Connor SM, Keel PK, Neale M, Sisk CL, Boker S, & Burt SA (2015). Changes in genetic risk for emotional eating across the menstrual cycle: A longitudinal study. Psychological Medicine, 45(15), 3227–3237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Keel PK, Burt SA, Racine SE, Neale MC, Sisk CL, & Boker S. (2013a). Ovarian hormones and emotional eating associations across the menstrual cycle: An examination of the potential moderating effects of body mass index and dietary restraint. International Journal of Eating Disorders, 46(3), 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Keel PK, Racine SE, Burt SA, Sisk CL, Neale M, Boker S, & Hu JY (2013b). The interactive effects of estrogen and progesterone on changes in emotional eating across the menstrual cycle. Journal of Abnormal Psychology, 122(1), 131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Keel PK, Sisk C, & Burt SA (2010). Preliminary evidence that estradiol moderates genetic influences on disordered eating attitudes and behaviors during puberty. Psychological Medication, 40(10), 1745–1753. doi: 10.1017/S0033291709992236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, McGue M, & Iacono WG (2003). Differential heritability of eating pathology in pre-pubertal versus pubertal twins. International Journal of Eating Disorders, 33(3), 287–292. doi: 10.1002/eat.10151 [DOI] [PubMed] [Google Scholar]
- Knauss C, Paxton SJ, & Alsaker FD (2007). Relationships amongst body dissatisfaction, internalisation of the media body ideal and perceived pressure from media in adolescent girls and boys. Body Image, 4, 353–360. doi: 10.1016/j.bodyim.2007.06.007 [DOI] [PubMed] [Google Scholar]
- Kovacs M. (1985). The Children’s Depression Inventory (CDI). Psychopharmacology Bulletin, 21, 995–998. [PubMed] [Google Scholar]
- Kovacs M. (1992). Manual for the Children’s Depression Inventory. North Tonawanda, NJ: Multi-Health Systems. [Google Scholar]
- Le Grange D, O’Connor M, Hughes EK, Macdonald J, Little K, & Olsson CA (2014). Developmental antecedents of abnormal eating attitudes and behaviors in adolescence. International Journal of Eating Disorders, 47(7), 813–824. doi: 10.1002/eat.22331 [DOI] [PubMed] [Google Scholar]
- Luo X, Donnellan MB, Burt SA, & Klump KL (2016). The dimensional nature of eating pathology: Evidence from a direct comparison of categorical, dimensional, and hybrid models. Journal of Abnormal Psychology, 125(5), 715–726. doi: 10.1037/abn0000174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor SM, Burt SA, VanHuysse JL, & Klump KL (2016). What drives the association between weight-conscious peer groups and disordered eating? Disentangling genetic and environmental selection from pure socialization effects. Journal of Abnormal Psychology, 125(3), 356–368. doi: 10.1037/abn0000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor SM, Culbert KM, Mayhall LA, Burt SA, & Klump KL (2020). Differences in genetic and environmental influences on body weight and shape concerns across pubertal development in females. Journal of Psychiatric Research, 121, 39–46. doi: 10.1016/j.jpsychires.2019.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dea JA, & Abraham S. (1999). Onset of disordered eating attitudes and behaviors in early adolescence: Interplay of pubertal status, gender, weight, and age. Adolescence, 34(136), 671–679. [PubMed] [Google Scholar]
- Papay J, & Spielberger CD (1986). Assessment of anxiety and achievement in kindergarten and first- and second-grade children. Journal of Abnormal Child Psychology, 14, 279–286. [DOI] [PubMed] [Google Scholar]
- Papay JP, & Hedl JJ Jr. (1978). Psychometric characteristics and norms for disadvantaged third and fourth grade children on the State-Anxiety Inventory for Children. Journal of Abnormal Child Psychology, 6, 115–120. [DOI] [PubMed] [Google Scholar]
- Pearson CM, Combs JL, Zapolski TCB, & Smith GT (2012). A longitudinal transactional risk model for early eating disorder onset. Journal of Abnormal Psychology, 121(3), 707–718. doi: 10.1037/a0027567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Miller J, Ackard DM, Loth KA, Wall MM, Haynos AF, & Neumark SD (2017). Stability and change in patterns of eating disorder symptoms from adolescence to young adulthood. International Journal of Eating Disorders, 50(7), 748–757. doi: 10.1002/eat.22692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, & Boxer A. (1988). A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence, 17(2), 117–133. doi: 10.1007/BF01537962 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. doi: 10.3102/10769986031004437 [DOI] [Google Scholar]
- Racine SE, Culbert KM, Larson CL, & Klump KL (2009). The possible influence of impulsivity and dietary restraint on associations between serotonin genes and binge eating. Journal of Psychiatric Research, 43(16), 1278–1286. doi: 10.1016/j.jpsychires.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine SE, Keel PK, Burt SA, Sisk CL, Neale M, Boker S, & Klump KL (2013). Exploring the relationship between negative urgency and dysregulated eating: Etiologic associations and the role of negative affect. Journal of Abnormal Psychology, 122(2), 433–444. doi: 10.1037/a0031250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon LE, Leen-Feldner EW, & Hayward C. (2009). A critical review of the empirical literature on the relation between anxiety and puberty. Clinical Psychology Review, 29(1), 1–23. doi: 10.1016/j.cpr.2008.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogol AD, Roemmich JN, & Clark PA (2002). Growth at puberty. Journal of Adolescent Health, 31, 192−200. doi: 10.1016/s1054-139x(02)00485-8 [DOI] [PubMed] [Google Scholar]
- Schulze UM, Calame S, Keller F, Mehler-Wex C. (2009). Trait anxiety in children and adolescents with anorexia nervosa. Eating and Weight Disorders, 14, e163–e168. doi: 10.1007/BF03327817. [DOI] [PubMed] [Google Scholar]
- Sheehy A, Gasser T, Molinari L, & Largo RH (1999). An analysis of variance of the pubertal and mid-growth spurts for length and width. Annals of Human Biology, 26, 309–331. doi: 10.1080/030144699282642 [DOI] [PubMed] [Google Scholar]
- Shope MM, Prows SD, Racine SE, & Culbert KM (2020). Examining associations between emotion-based rash action and dysregulated eating symptoms in men and women. Eating Behaviors, 37, 101379. doi: 10.1016/j.eatbeh.2020.101379 [DOI] [PubMed] [Google Scholar]
- Siervogel RM, Demerath EW, Schubert C, Remsberg KE, Chumlea WC, Sun S, & Towne B. (2003). Puberty and body composition. Hormone Research in Paediatrics, 60, 36–45. doi: 10.1159/000071224 [DOI] [PubMed] [Google Scholar]
- Sitarenios G, & Kovacs M. (1999). Use of the Children’s Depression Inventory. In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment (2nd ed., pp. 267–298). Mahwah, NJ: Erlbaum. [Google Scholar]
- Slane JD, Burt SA, & Klump KL (2011). Genetic and environmental influences on disordered eating and depressive symptoms. International Journal of Eating Disorders, 44(7), 605–611. doi: 10.1002/eat.20867 [DOI] [PubMed] [Google Scholar]
- Spear LP (2000). Neurobehavioral changes in adolescence. Current Directions in Psychological Science, 9(4), 111–114. doi: 10.1111/1467-8721.00072 [DOI] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, & Jacobs GA (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Spanos A, Klump KL, Burt SA, McGue M, & Iacono WG (2010). A longitudinal investigation of the relationship between disordered eating attitudes and behaviors and parent–child conflict: A monozygotic twin differences design. Journal of Abnormal Psychology, 119(2), 293–299. doi: 10.1037/a0019028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw HE, 2002. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research, 53, 985–993. doi: 10.1016/s0022-3999(02)00488-9 [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, & Yanovski JA (2008). Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite, 51, 148–155. doi: 10.1016/j.appet.2008.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Schvey NA, & Grilo CM (2020). A developmental framework of binge-eating disorder based on pediatric loss of control eating. American Psychologist, 75(2), 189–203. doi: 10.1037/amp0000592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, … Yanovski JA (2007). Validation of the Emotional Eating Scale Adapted for use in Children and Adolescents (EES-C). International Journal of Eating Disorders, 40, 232–240. doi: 10.1002/eat.20362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, & Yanovski JA (2009). A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders, 42(1), 26–30. doi: 10.1002/eat.20580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2019). QuickFacts Michigan. https://www.census.gov/quickfacts/MI [Google Scholar]
- Vannucci A, Tanofsky-Kraff M, Ranzenhofer LM, Kelly NR, Hannallah LM, Pickworth CK, … Yanovski JA (2014). Puberty and the manifestations of loss of control eating in children and adolescents. International Journal of Eating Disorders, 47(7), 738–747. doi: 10.1002/eat.22305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T. (2000). Ice-cream consumption, tendency toward overeating, and personality. International Journal of Eating Disorders, 28(4), 460–464. doi: [DOI] [PubMed] [Google Scholar]
- Verschueren M, Claes L, Palmeroni N, Bogaerts A, Gandhi A, Moons P, & Luyckx K. (2019). Eating disorder symptomatology in adolescent boys and girls: Identifying distinct developmental trajectory classes. Journal of Youth and Adolescence, 49(2), 410–426. doi: 10.1007/s10964-019-01174-0 [DOI] [PubMed] [Google Scholar]
- von Ranson KM, Klump KL, Iacono WG, & McGue M. (2005). The Minnesota Eating Behavior Survey: A brief measure of disordered eating attitudes and behaviors. Eating Behaviors, 6, 373–392. doi: 10.1016/j.eatbeh.2004.12.002 [DOI] [PubMed] [Google Scholar]
- Wade TD, Byrne S, & Bryant-Waugh R. (2008). The eating disorder examination: Norms and construct validity with young and middle adolescent girls. International Journal of Eating Disorders, 41(6), 551–558. doi: 10.1002/eat.20526 [DOI] [PubMed] [Google Scholar]
- Wallin U, & Råstam M. (2016). Childhood anorexia nervosa compared with low weight food intake disorder without weight and shape‐related psychopathology: A retrospective study of 102 patients. European Eating Disorders Review, 24(4), 329–333. doi: 10.1002/erv.2447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. doi: 10.1016/s0191-8869(00)00064-7 [DOI] [Google Scholar]
- Zapolski TCB, & Smith GT (2013). Comparison of parent versus child-report of child impulsivity traits and prediction of outcome variables. Journal of Psychopathology and Behavioral Assessment, 35(3), 301–313. doi: 10.1007/s10862-013-9349-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TCB, Stairs AM, Settles RF, Combs JL, Smith GT (2010). The measurement of dispositions to rash action in children. Assessment, 17(1), 116–125. doi: 10.1177/1073191109351372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerwas S, Holle AV, Watson H, Gottfredson N, & Bulik CM (2014). Childhood anxiety trajectories and adolescent disordered eating: Findings from the NICHD study of early child care and youth development. International Journal of Eating Disorders, 47(7), 784–792. doi: 10.1002/eat.22318 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.