Keywords: FMT, live biotherapeutic product, engineered microbes, microbiome, therapeutics
Abstract
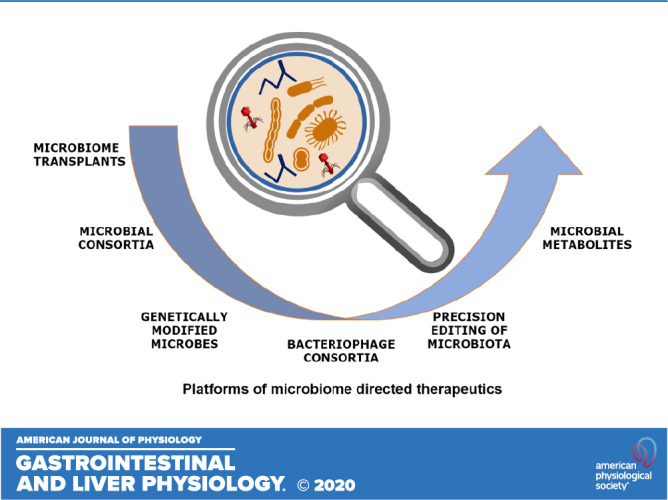
The extensive investigation of the human microbiome and the accumulating evidence regarding its critical relationship to human health and disease has advanced recognition of its potential as the next frontier of drug development. The rapid development of technologies, directed at understanding the compositional and functional dynamics of the human microbiome, and the ability to mine for novel therapeutic targets and biomarkers are leading innovative efforts to develop microbe-derived drugs that can prevent and treat autoimmune, metabolic, and infectious diseases. Increasingly, academics, biotechs, investors, and large pharmaceutical companies are partnering to collectively advance various therapeutic modalities ranging from live bacteria to small molecules. We review the leading platforms in current development focusing on live microbial consortia, engineered microbes, and microbial-derived metabolites. We will also touch on how the field is addressing and challenging the traditional definitions of pharmacokinetics and pharmacodynamics, dosing, toxicity, and safety to advance the development of these novel and cutting-edge therapeutics into the clinic.
INTRODUCTION
Research discoveries interrogating the human intestinal microbiome have revealed a huge potential to design therapeutics by leveraging mechanisms evolved by microbes for human-host interactions (1). Collectively, these discoveries support the premise that the introduction or restoration of specific microbes into complex microbial ecosystems such as the gastrointestinal tract or restoration of complex microbial community diversity may reverse diseased pathology returning it toward homeostasis and health (2). While compositional shifts in the abundance of microbial species may be one route to therapeutic benefit, it is also recognized that the functional metabolic shifts in the microbiome, resulting from changes in small molecule outputs, or the metabolome, are also an important route to therapy (3). The scientific advances emerging from research into the human microbiome is supporting development of three leading platforms in drug design and development: 1) “bugs as drugs” or consortia of microbes and engineered microbes, 2) “drugs from bugs” or metabolites that modulate host physiological pathways, and 3) “drugging the bugs” or strategies that selectively target or eliminate disease-causing microbes (e.g., phage therapeutics). The number of diseases amenable to treatment by these various strategies is considerable and includes inflammatory, autoimmune, metabolic, neurodegenerative diseases, and cancer (4–8).
PROGRESS IN UNDERSTANDING GASTROINTESTINAL MICROBIAL DIVERSITY
Much of the early work on the gastrointestinal microbiome was focused on defining the compositional complexity of the healthy gastrointestinal tract and then contrasting it, with the compositional shifts observed in diseased states. Indeed, initiatives such as the Human Microbiome Project (HMP), the Integrative Human Microbiome Project (iHMP), and Metagenomics of the Human Intestinal Tract (MetaHit) have contributed a wealth of DNA sequencing information and when interrogated using computational tools and machine learning algorithms have identified changes in specific taxa or altered community stability in healthy control and disease cohorts (9). With the increased adoption of shotgun metagenomic sequencing, microbial composition is being characterized with increasing taxonomic precision and resolution, such that species-level and strain-level shifts are now being documented (10). Collectively, these data have fueled scientific interest in identifying microbes that may either have a causal role in driving disease or actively contribute to health and homeostasis. Extensive efforts to cultivate previously unculturable human gastrointestinal bacterial isolates are also ongoing (11), enabling the establishment of both publicly available and proprietary bacterial culture collections/stool banks. The adoption of multiomic approaches including metatranscriptomics and metabolomics is providing greater insight into the physiological properties of bacteria. Over the past decade, emerging academic and industry approaches focused on the manipulation of the human microbiome have given rise to a number of therapeutic platforms and modalities directed toward treating and curing noncommunicable diseases, which have escalated in the Westernized world.
BUGS AS DRUGS: CONSORTIA OF MICROBES
The success of fecal microbial transplantation (FMT) in treating Clostridioides difficile has served as proof of concept that a resetting of the diseased microbiome to a healthy state is a therapeutic approach with great potential (12, 13). However, FMT may not have long-term feasibility as a reproducible therapeutic approach, since FMT involves an undefined and inconsistent consortia of microbes with significant safety risks associated with its use, particularly in immune-compromised subjects (https://bit.ly/39py5T7). Recently, a number of serious adverse events, due to transmission of donor-derived drug-resistant enteropathogenic bacteria associated with FMT resulted in significant morbidity and one mortality (14). The risk associated with FMT is further under scrutiny, with recent positive detection of SARS-CoV-2 in the stool of infected individuals. An alternative to FMT is the use of either a single bacterial strain or consortia of defined bacterial strains that exhibit favorable properties to treat disease. Such a defined microbial consortium provides a more rational basis for microbial drug development and offers a potentially safer and more effective treatment of disease, particularly in those indications where FMT has demonstrated clinical success [e.g., ulcerative colitis (UC), recurrent C. difficile infection]. Thus, restoring a microbiome with a subset of commensal bacteria that provide functional synergy reflective of a healthy state may lend itself to success. Success of a Phase III trial using a defined consortium of commensal bacteria (Ser 109; Table 1) to treat recurrent C. difficile infection is the first example of the potential for an LBP in this setting (19).
Table 1.
Summary of microbiome-based therapeutics targeting GI indications currently in development by stage
| Drug Development Phase |
|||
|---|---|---|---|
| Mode of Action | Discovery/Preclinical | Phase 1a/1b | Phase 2/3 |
| Live microbial therapeutics (various proprietary approaches) | |||
| Rationally selected live multistrain microbiota drug; 11 and 16 clonal human commensal bacteria strain LBPs | Drug name: VE202 Indication: Crohn’s Disease Company/sponsor: Vedanta Biosciences/Janssen R&D ClinicalTrials.gov: NCT03723746 |
||
| Rationally selected live multistrain microbiota drug; 8 clonal human commensal bacteria strain LBP | Drug name: VE303 Indication: Clostridium difficile Company/Sponsor: Vedanta Biosciences CONSORTIUM study ClinicalTrials.gov: NCT03788434 (15, 16) |
||
| Rationally selected live multistrain microbiota drug; blend of spore and fermented nonspore, vegetative forms of bacteria | Drug name: Ser 301 Indication: ulcerative colitis Company/sponsor: Seres Therapeutics |
||
| Rationally selected live multistrain microbiota drug | Drug name: FIN 524 Indication: ulcerative colitis Company/sponsor: Finch/Takeda |
||
| Rationally selected live multistrain microbiota drug | Drug name: FIN 525 Indication: Crohn’s disease Company/sponsor: Finch/Takeda |
||
| Rationally selected live multistrain microbiota drug | Drug name: ABI-M301 Indication: Crohn’s disease Company/sponsor: Assembly |
||
| Rationally selected live multistrain microbiota drug | Drug name: ABI-M201 Indication: ulcerative colitis Company/sponsor: Assembly ClinicalTrials.gov: NCT03923478 |
||
| Single-strain live biotherapeutic product; Bacteroides thetaiotaomicron | Drug name: Thetanix Pediatric indication: Crohn’s disease Company/sponsor: 4D Pharma plc ClinicalTrials.gov: NCT02704728 (17) |
||
| Single-strain live biotherapeutic product | Drug name: Rosburix Indication: pediatric ulcerative colitis Company/sponsor: 4D Pharma plc |
||
| Single-strain live biotherapeutic product | Drug name: Blautix Indications: irritable bowel syndrome Company/sponsor: 4D Pharma plc ClinicalTrials.gov: NCT03721107 |
||
| Multistrain donor-derived microbiota drug product; fecal microbial transplant (FMT) | FMTIndications: ulcerative colitis and Clostridium difficile Investigator initiated studiesmultiple |
||
| Multistrain donor-derived microbiota drug product; consortium of Firmicute bacterial spores from healthy donors | Drug name: Ser 287 Indication: ulcerative colitis Company/sponsor: Seres/NestleECO-RESET trial ClinicalTrials.gov: NCT03759041 (18) |
||
| Multistrain donor derived-microbiota drug product; consortium of bacterial spores from healthy donors | Drug name: Ser 109 Indication: Clostridium difficile Company/sponsor: Seres/Nestle ECOSPOR III trialClinicalTrials.gov: NCT03183128 (19, 20) |
||
| Multistrain donor-derived microbiota/ FMT drug product | Drug name: CP101 Indication: Clostridium difficile Company/sponsor: Crestovo/Finch PRISM 3 trial ClinicalTrials.gov: NCT03110133 |
||
| Multistrain donor-derived microbiota drug product;proprietary Microbiota Restoration Therapy drug platform | Drug name: RBX7455 Indication: Clostridium difficile Company/sponsor: Rebiotix, Inc/Ferring ClinicalTrials.gov: NCT02981316 |
||
| Multistrain donor-derived microbiota drug product;proprietary Microbiota Restoration Therapy drug platform | Drug name: RBX2660 (enema)Indication: Clostridium difficile Company/sponsor: Rebiotix, Inc/Ferring PUNCH trials ClinicalTrials.gov: NCT03244644 (21) |
||
| Targeted gut delivery of a Lactococcus lactis strain engineered to express gliadin peptide in combination with an immunomodulating cytokine | Drug name: AG017 Indication: celiac disease Company/sponsor: ActoBio Therapeutics (22) |
||
| Bacterial strains engineered to produce targeted therapeutic drug combined with prebiotic to regulate colonization | Drug name: TBD Indication: irritable bowel syndrome Company/sponsor: Novome (23) |
||
| Bacteriophage | |||
| Customized phage cocktail designed to eliminate specific disease-associated bacterial targets in the gut | Drug name: BX002 Indication: inflammatory bowel disease Company/sponsor: BiomX, Ltd |
||
| Customized phage cocktail designed to eliminate specific disease-associated bacterial targets in the gut; targets adherent-invasive Escherichia coli (AIEC) | EcoActiveIndication: Crohn’s disease Company/sponsor: Intralytix/Ferring ClinicalTrials.gov: NCT03808103 (24) |
||
| Customized phage cocktail designed to eliminate specific disease-associated bacterial targets in the gut; targets Klebsiella pneumonia strains | Drug name: BX003Indication: primary sclerosing cholangitis Company/sponsor: BiomX Ltd |
||
| Engineered bacteriophage using CRISPR-Cas technology | EligobioticsCompany/sponsor: Eligo Bioscience (25) | ||
| Small molecules/microbial-derived metabolites | |||
| Polysaccharide A; Treg induction | Drug nameSYMB104 Indication: inflammatory bowel disease Company/sponsor: Symbiotix Biotherapies, Inc |
||
| FimH adhesin inhibitor; blocks pathogen adhesion | Drug name:EB8018 (Sibofimloc) AEIC in Indication: Crohn’s disease Company/sponsor: Enterome/Takeda ClinicalTrials.gov: NCT03709628 |
||
| Enzymedegrades β-lactam antibiotics in vivo | Drug name:SYN004 (Ribaximase) Indication: Clostridium difficile Company/sponsor: Synthetic Biologics ClinicalTrials.gov: NCT02563106 (26) |
||
| Therapeutic microbiome-derived molecule reported to promote mucosal healing of damaged epithelial surfaces | Drug name: SG-2-0776 Indication: inflammatory bowel disease Company/sponsor: Second Genome |
||
Data are current as of October 1, 2020. C. difficile, Clostridium difficile; GI indications, gastrointestinal disease indications; IBS, irritable bowel syndrome; LBP, live biotherapeutic product.
The rational design of defined microbial consortia for drug development has been driven by the extensive microbial community profiling and sequencing studies of clinical samples that have compared healthy individuals and subjects with immune-mediated disease (27). By harnessing the evolving insights from host microbial interactions and expanding the availability of taxonomically diverse libraries of human-derived bacterial strains, it is now possible to construct tailored consortia that are designed to reprogram a dysfunctional disease-associated microbial ecology (28). For example, to treat inflammatory bowel disease (IBD), specific microbial strains can be selected that augment colonic T regulatory cell (Treg) activity (29) or negatively regulate mucosal T helper cell (Th1, Th17) function (30), with the goal of reducing inflammation and restoring mucosal immune homeostasis.
Developing live microbial consortia, “bugs as drugs,” is currently a therapeutic strategy at the forefront of microbiome drug development platforms. These consortia developed as drugs are defined by the FDA as a live biotherapeutic product (LBP), a biological product that 1) contains live organisms, such as bacteria; 2) is applicable to the prevention, treatment, or cure of a disease or condition of human beings; and 3) is not a vaccine (https://bit.ly/2QyvPQK; https://www.fda.gov/media/82945/download). LBPs can also include genetically modified microorganisms, termed recombinant LBPs, that contain microbes with purposeful addition, deletion, or modification of genetic material.
There are advantages to developing a defined consortium of microbes. Consortia can be numerically reduced in size to include only those strains that are well characterized, can be easily or reproducibly manufactured at scale, and exhibit functional properties or mechanism of action that is hypothesized to impact disease biology. These living drugs are orally delivered, thus providing the advantage of being targeted to the gastrointestinal tract but with the potential for systemic impact via direct or indirect modulation of host cellular targets, for instance, via induction or elaboration of host or microbial-derived metabolites. Additionally, consortia that promote expansion of CD8 T cells and NK cells can be used in combination with existing drug therapies (e.g., immune checkpoint inhibitors) to augment their efficacy (31).
The traditional small and large molecule drug development requirements are not wholly applicable to LBPs, and the regulatory framework is currently being developed as these products progress through the development lifecycle and into patient trials. Live microbial therapeutics often do not require traditional drug toxicology studies since they are recognized as natural inhabitants of human body. Human donor strains are extensively screened to mitigate against the risk of transmitting disease and single strains may undergo extensive metagenomic sequencing to identify any potential bacterial toxins or antibiotic resistance genes. Preclinical toxicology studies are not readily applicable since in vitro assays are challenging with live microbes and the normal resident microbiome of rodents, dogs, or small primates typically used for toxicology studies cannot appropriately replicate that of the human microbiome. To date, there have been no serious safety events reported for trials involving single or defined consortia LBPs, and they seem to be well tolerated. However, it must be noted that the majority of trials have been conducted in healthy volunteers although a few are in progress or progressing into larger patient Phase 2 and 3 trials, which will provide the opportunity to observe any major safety effects.
The concepts of dose, pharmacokinetics (PK), and pharmacodynamics (PD) have required new thinking and frameworks for live microbes, which do not remain static in the host and for which inherent interindividual gut microbiome variability may influence bacterial colonization dynamics and targeted “drug” activity. Traditional small and large molecule preclinical human dose modeling does not translate to microbial products, and dose ranging experiments based on product CFU counts are thus conducted first in human healthy volunteer trials (16). How dose-dependent colonization in a healthy individual translates to patients is being evaluated in ongoing patient trials, and what is learned from these studies is expected to provide insight to support dose modeling algorithms for future trials. PK for a live microbe may be defined by strain-specific colonization kinetics (i.e., numbers of, and abundance of, strain colonization). PD may be defined by the LBPs’ detectable and measurable impact on individual gut microbiome composition or on modulation of gut metabolic function (i.e., stool metabolites).
One example of the development of LBPs is those targeting inflammatory bowel disease (IBD). Patients with IBD exhibit gastrointestinal microbial dysbiosis that includes reduced microbial diversity, deficiency of Clostridia cluster species, and an overgrowth of Proteobacteria, in addition to mucosal immune dysregulation (28, 32). In experiments conducted in the laboratory of Kenya Honda, Clostridium species were identified as specific microbial drivers of accumulation and function of colonic T regulatory cells (33). His laboratory further demonstrated that a minimum number of Clostridium strains in combination were required to drive this effect (29). The identified consortium was shown to be effective in treating inflammation and preventing disease-associated mortality in a preclinical model of colitis. Thus, this rational approach to selecting commensal bacteria from Clostridium clusters IV, XIVa, and XVIII identified specific strains with potent immune regulatory properties that are also relevant to controlling disease in IBD: biological effects included the induction of colonic lamina propria regulatory T cells, induction of immunoregulatory molecules indolamine dioxygenase and transforming growth factor-β1 (TGF-β1), production of short-chain fatty acids (SCFA) that promote mucosal barrier integrity, and modulation of macrophages through inhibition of histone deacetylase (33–37). These fundamental scientific findings are being exploited in the design and development of a rational LBP for the treatment of IBD (Vedanta Biosciences and others).
The number of microbiome-focused efforts to design unique LBPs for treating infectious, inflammatory, autoimmune, and metabolic diseases has grown significantly over the past 5 years (refer to Table 1 for a representative list of therapeutics targeting gastrointestinal disease indications). A few LBPs have reached Phase 1 and Phase 2 trials in healthy volunteers and target patient populations. A human-derived multibacterial FMT-derived spore-based drug product (SER-287, Seres Therapeutics) completed a Phase 1 b randomized, double-blinded, placebo-controlled, multiple-dose, induction study in 58 patients with mild-to-moderate UC in January 2018. Efficacy results of this product suggested that clinical and endoscopic remission was achieved in 15 subjects for up to 6 mo. This response was correlated with both durable colonization of a subset of species in the product and an elaboration of microbial metabolites (secondary bile acids). The product has progressed to a Phase 2 b three-arm placebo-controlled trial of ∼200 patients with active mild-to-moderate UC (Table 1). The study’s primary end point is clinical remission measured after 10 wk of drug administration. Endoscopic improvement will be measured as a secondary efficacy measure. A second-generation product (Ser-301) is in preclinical development and conforms with a rational design approach derived from identifying specific species that engraft in remitting patients and hence associated with treatment efficacy in the Phase 1 b study. Another rationally designed LBPs (ABI-M201, Abbvie and Assembly Biosciences; Table 1) intended to treat UC and Crohn’s disease (CD) respectively has entered a Phase 1 b clinical trial in patients with mild to moderate UC and will test the safety and efficacy of this LBP in patients with concurrent mesalamine therapy.
In addition to the consortia products, the single-strain approach to LBP drug development has also been adopted. This approach undoubtedly simplifies the manufacture and clinical development path over that for consortia-based products, but whether a single bacterium is sufficient to treat disease over ecosystem approaches awaits clinical readouts, as trials progress beyond Phase 2. An additional point worth mentioning is the emerging notion that clinical success may equate with durable colonization, also referred to as engraftment, of product/donor strains and which, in some circumstances, may require addition of specific substrates such as prebiotics to enhance the colonization potential of exogenously introduced strains. Hence, efforts leading to the identification of specific prebiotics that confer a competitive growth advantage of drug-product bacterial strains over preexisting gut-resident strains are also being advanced.
ENGINEERED MICROBES AS DRUGS
In addition to the development of LBPs containing either a single or a consortium of strains, a second approach to manipulating live microbes for LBPs is by targeted genetic modification of single-strain bacteria. This requires engineering strategies that alter the functionality of the engineered bacterium and requires a sound understanding of disease biology, microbial genomics, and synthetic biology. The resulting bacterial strains are engineered to produce molecules of interest and with specific colonization properties that can be manipulated (i.e., short- vs. long-term engraftment potential) (38). For this product modality, there are significant drug development, regulatory, public, and ethical hurdles that must be overcome before such genetically modified bacteria are approved as clinical treatments. These include the potential for gene transfer, acquisition of antibiotic resistance in the recipient microbiome, and biocontainment. Nevertheless, novel product approaches are in development and include transfer of specific nutrient utilization genes to control the abundance and metabolic function of transferred microbial strains (39). Additional examples of this approach to engineer bacterial strains include 1) a commensal Escherichia coli strain to produce enzymes for rare genetic disorders in which enzyme deficiency leads to toxic accumulation of normally metabolized products (Synlogic); 2) a probiotic strain of Lactococcus lactis for local gut delivery of IL-10 to treat IBD (22) or peptides for tolerance induction in Celiac disease (40) (ActoBio Therapeutics; Table 1); 3) a strain of Clostridium to restore colonic epithelial barrier homeostasis and mucosal immune function for the treatment of IBD by targeted delivery of butyrate-related molecules to the colon (41) (Chain Biotech).
DRUGS FROM BUGS: MICROBIAL MOLECULES AND METABOLITES
Microbiome-focused studies are also embracing the important aspect of functionality. The human gastrointestinal microbiome, like that of environmental microbiomes such as soil, has a vast metabolic capacity and is able to generate thousands of diverse bioactive molecules and metabolites (natural products). These products map to very diverse chemical and biological groups including amino acid derivatives, oligosaccharides, lipids, glycolipids, polyketides, benzenoids, peptides (e.g., nonribosomal peptides and ribosomal and posttranslationally modified peptides), glycopeptides, etc. (42). These products are produced at physiologically relevant concentrations, function both locally in the gastrointestinal tract and systemically, and have been shown to impact human host physiology including immunity, metabolism, and even gut-brain signaling (27, 42, 43). They also function in microbe-microbe interactions and in niche protection (44).
Until recently, most studies of microbiome-derived metabolites have focused on the known metabolites such as SCFAs, particularly butyrate. However, research efforts to identify other biologically and clinically important microbially derived products, such as bile acids and tryptophan-derived metabolites/mimetics, have intensified. In addition, the immune regulatory function of cell surface molecules such as polysaccharide A (PSA) from Bacteroides fragilis has also been demonstrated (45). Its clinical utility is being pursued in development of a microbial drug that can modulate regulatory T cell (TREG) activity as a therapeutic approach to treat autoimmune and inflammatory diseases (Symbiotix Biotherapies, Inc). A range of methodologies including sequenced-based, molecular-based, and metabolomic-based approaches have been exploited to expand the repertoire of novel functional metabolites and products generated by microbes. These include 1) mining of microbial community metagenomic sequence data and use of computational algorithms, in combination with heterologous expression/synthetic biology, to identify novel functional metabolic features or biosynthetic gene clusters (BGCs) (44, 46, 47); 2) target-driven functional screening of cosmid or fosmid metagenomic libraries (48); 3) target-screening of supernatants derived from diverse bacterial isolates (49); and more recently, 4) the application of high-throughput untargeted metabolomics combined with high-resolution analytical chemistry.
Estimates of around 10,000 BGCs present in the human gastrointestinal metagenome have been proposed (42). Very recent work has uncovered a completely new family of bioactive metabolites. These metabolites, derived from a peptide aldehyde scaffold, have been found to inhibit human cathepsins and are thought to regulate antigen presentation and immune recognition, thereby contributing to commensal immune tolerance mechanisms (50).
Similarly, evidence that other novel classes of metabolites derived from commensal bacterial effector genes (Cbegs), found in the human gastrointestinal microbiome, impact important host signaling pathways has also been demonstrated. One such molecule, a member of a structurally diverse group of long-chain N-acyl amide (N-acyl-3-hydroxy palmitoyl glycine), referred to as commendamide, was found to activate human host G protein-coupled receptors (GPCRs) (48). Following on from this finding, a family of six distinct N-acyl molecules have since been reported and are enriched in the Bacteroides phyla (51). Interestingly, the close similarity between bacterially derived and endogenous human ligands has led to speculation that bacterial ligands are essentially mimetic drugs with potent host effects (43).
The finding that certain bacterial phyla in the human gastrointestinal tract appear to generate unique bioactive moieties is intriguing. For example, Bacteriodetes have been known to synthesize and produce sphingolipids, which modulate host immunity and inflammation (52). The physiological importance of these molecules has been highlighted in recent work demonstrating that host and bacterial sphingolipid metabolism is altered in IBD and that Bacteroidetes sphingolipids are important in maintaining host immune homeostasis (6, 53).
Our understanding of the biosynthesis of microbial molecules and metabolites and their functional importance in the context of human biology is growing rapidly. The motivation to continue to drive this discovery path forward is driven by two clear goals: first, to clarify the molecular mechanisms that govern host-microbial symbiosis and pathogenesis, and second, to drive novel drug discovery and development. As with the development of therapeutic bacterial consortia, several efforts are underway to advance small molecule/metabolite discovery pipelines to advance this development work into the clinic (Table 1).
A novel protein (SG-2-0776) derived from the microbiome that promotes mucosal healing will be evaluated in patients with IBD with plans to initiate clinical trials in 2020 (Second Genome, Table 1). Utilization of the vast resources of multiomic data sets combined with machine learning algorithms has been applied to identify and develop precision enteric medicines for IBD and other diseases. In addition to identifying small microbial-derived molecules as therapies, this approach also is also leading to the identification of small molecule inhibitors of bacterial metabolite production that are associated with disease pathogenesis and progression.
DRUGGING THE BUGS: SELECTIVE TARGETING OF PATHOBIONTS
The ability to selectively target and eliminate disease-causing bacteria is a further microbiome approach gaining traction for the treatment of human gastrointestinal diseases. These targeted approaches also referred to as microbiome engineering strategies range from interfering with pathobiont (e.g., commensal microbes with pathogenic microbe virulence mechanisms) gastrointestinal epithelial attachment mechanisms, bacterial metabolism, direct killing via targeted phage therapies, and the use of narrow spectrum antimicrobials such as bacteriocins.
FimH-expressing bacteria are increased in a subset of patients with CD and are thought to have a causal role (24). Thus, a small molecule inhibitor approach to target the specific class of pathobionts expressing FimH surface adhesins [e.g., adherent-invasive E. coli (AIEC)] has been developed. This lead molecule, called EB8018, is a gut-restricted oral FimH antagonist and is currently in Phase 1 and 2 trials for the treatment of active CD and postoperative CD, respectively (Enterome; Table 1).
The identification of small molecule inhibitors of bacterial metabolite production that are associated with disease pathogenesis and progression is also yielding progress. Such identified inhibitors include those targeting bacterial β-glucuronidase (54) to enhance cancer drug efficacy and limit inherent toxicity and others being developed to inhibit bacterial metabolites implicated in chronic kidney disease (49).
There is significant interest in developing targeted phage therapies for the treatment of gastrointestinal diseases such as IBD and colorectal cancer. Bacteriophages, viruses that infect bacteria, can induce lysis and killing of target bacteria. They have a narrow bacterial host range and therefore avoid the collateral damage induced by broad-spectrum antibodies. Hence, they preserve overall microbiome diversity and reduce the risk of promoting antibiotic resistance mechanisms by targeting microorganisms as a strategy to also control chronic inflammation mediated by them. However, these microbiome-targeting interventions require knowledge of the causal microorganism. Examples include a bacteriophage therapy targeting AIEC in patients with CD that is currently in Phase 1/2a clinical trials (Intralytix Inc; Table 1); another is the pathobiont Klebsiella pneumoniae, which has been implicated in IBD and primary sclerosing cholangitis disease pathogenesis (30, 55), which is also in development (BiomX; Table 1). Additional platforms are in preclinical development and take advantage of CRISPR-Cas technology as engineering approaches for phage genome editing that may further refine specificity and selectivity of bacterial targets. Thus far, development has focused on infectious disease pathogens, especially multidrug resistant targets including C. difficile. The first Phase 1 b clinical trial began in 2020 using a CRISPR-Cas3 engineered phage cocktail targeting urinary tract infection-causing E. coli (https://clinicaltrials.gov/show/NCT04191148).
CONCLUSIONS: CHALLENGES AND OPPORTUNITIES
The pharmaceutical development of microbial therapeutics links research and development at the cutting edge of discovery in research fields that encompass immunology, oncology, microbiology, genomics, and systems biology. An understanding of how exogenously derived microbes interact, colonize, and engraft once introduced into a new host microenvironment and the nature of the chemical mediators that they produce to mediate drug-like efficacy are areas of intense exploration with novel and extensive drug development potential.
The successes of FMT in C. difficile infection and UC have shown promise and support the potential of microbial-based approaches in the treatment of disease. Recent work investigating FMT for recurrent C. difficile has established that microbial composition and diversity significantly increased in responders (56). However, in launching into this new frontier of microbiome-based drug development, several questions and potential hurdles are revealed that still need to be addressed as the field evolves.
A defined bacterial consortium, even if its constituents are phylogenetically diverse, does not provide the microbial diversity of FMT, and it is yet to be demonstrated whether the scientific rationale for any given consortia will prove efficacious in the clinic. The reliance on preclinical animal model testing for efficacy and mode of action readouts is also challenging and will require testing and validation in humanized mouse or other small animal models and human subjects. For LBPs, assays and algorithms that will improve our insight into host receptivity to transient or durable bacterial colonization that may be required for drug efficacy are needed to help with defining pharmacokinetics, dose prediction modeling, and translation of the pharmacodynamic effect in modulating target pathways relevant to disease. No microbiome-based therapeutic has been yet approved by the FDA, and regulatory requirements are thus likely to evolve including in considerations regarding the evidence required to justify redundancy of strains in a consortium-based drug, antibiotic sensitivity characteristics, and definitions of potency that are likely required for later-stage drug development.
DISCLOSURES
E. Lamousé-Smith is employed by Janssen Pharmaceutical R&D, LLC. D. Kelly is employed by Seventure Partners, and I. De Cremoux is the CEO of Seventure Partners.
AUTHOR CONTRIBUTIONS
E.L-S., D.K., and I.D.C. prepared figures; E.L-S. and D.K. drafted manuscript; E.L-S. and D.K. edited and revised manuscript; E.L-S., D.K., and I.D.C. approved final version of manuscript.
REFERENCES
- 1.Cullen CM, Aneja KK, Beyhan S, Cho CE, Woloszynek S, Convertino M, McCoy SJ, Zhang Y, Anderson MZ, Alvarez-Ponce D, Smirnova E, Karstens L, Dorrestein PC, Li H, Sen Gupta A, Cheung K, Powers JG, Zhao Z, Rosen GL. Emerging priorities for microbiome research. Front Microbiol 11: 136, 2020. doi: 10.3389/fmicb.2020.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. Current understanding of the human microbiome. Nat Med 24: 392–400, 2018. doi: 10.1038/nm.4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turroni S, Brigidi P, Cavalli A, Candela M. Microbiota-host transgenomic metabolism, bioactive molecules from the inside. J Med Chem 61: 47–61, 2018. doi: 10.1021/acs.jmedchem.7b00244. [DOI] [PubMed] [Google Scholar]
- 4.Abdel-Haq R, Schlachetzki JCM, Glass CK, Mazmanian SK. Microbiome-microglia connections via the gut-brain axis. J Exp Med 216: 41–59, 2019. doi: 10.1084/jem.20180794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cani PD. Microbiota and metabolites in metabolic diseases. Nat Rev Endocrinol 15: 69–70, 2019. doi: 10.1038/s41574-018-0143-9. [DOI] [PubMed] [Google Scholar]
- 6.Franzosa EA, Sirota-Madi A, Avila-Pacheco J, Fornelos N, Haiser HJ, Reinker S, Vatanen T, Hall AB, Mallick H, McIver LJ, Sauk JS, Wilson RG, Stevens BW, Scott JM, Pierce K, Deik AA, Bullock K, Imhann F, Porter JA, Zhernakova A, Fu J, Weersma RK, Wijmenga C, Clish CB, Vlamakis H, Huttenhower C, Xavier RJ. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat Microbiol 4: 293–305, 2019. [Erratum in Nat Microbiol 4:898, 2019]. doi: 10.1038/s41564-018-0306-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marietta E, Horwath I, Balakrishnan B, Taneja V. Role of the intestinal microbiome in autoimmune diseases and its use in treatments. Cell Immunol 339: 50–58, 2019. doi: 10.1016/j.cellimm.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Toker J, Arora R, Wargo JA. The microbiome in immuno-oncology. Adv Exp Med Biol 1244: 325–334, 2020. doi: 10.1007/978-3-030-41008-7_19. [DOI] [PubMed] [Google Scholar]
- 9.Knight R, Vrbanac A, Taylor BC, Aksenov A, Callewaert C, Debelius J, Gonzalez A, Kosciolek T, McCall LI, McDonald D, Melnik AV, Morton JT, Navas J, Quinn RA, Sanders JG, Swafford AD, Thompson LR, Tripathi A, Xu ZZ, Zaneveld JR, Zhu Q, Caporaso JG, Dorrestein PC. Best practices for analysing microbiomes. Nat Rev Microbiol 16: 410–422, 2018. doi: 10.1038/s41579-018-0029-9. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd-Price J, Arze C, Ananthakrishnan AN, Schirmer M, Avila-Pacheco J, Poon TW, IBDMDB Investigators, , et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature 569: 655–662, 2019. doi: 10.1038/s41586-019-1237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Browne HP, Forster SC, Anonye BO, Kumar N, Neville BA, Stares MD, Goulding D, Lawley TD. Culturing of 'unculturable' human microbiota reveals novel taxa and extensive sporulation. Nature 533: 543–546, 2016. doi: 10.1038/nature17645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costello SP, Hughes PA, Waters O, Bryant RV, Vincent AD, Blatchford P, Katsikeros R, Makanyanga J, Campaniello MA, Mavrangelos C, Rosewarne CP, Bickley C, Peters C, Schoeman MN, Conlon MA, Roberts-Thomson IC, Andrews JM. Effect of fecal microbiota transplantation on 8-week remission in patients with ulcerative colitis: a randomized clinical trial. JAMA 321: 156–164, 2019. doi: 10.1001/jama.2018.20046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paramsothy S, Kamm MA, Kaakoush NO, Walsh AJ, van den Bogaerde J, Samuel D, Leong RWL, Connor S, Ng W, Paramsothy R, Xuan W, Lin E, Mitchell HM, Borody TJ. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet 389: 1218–1228, 2017. doi: 10.1016/S0140-6736(17)30182-4. [DOI] [PubMed] [Google Scholar]
- 14.DeFilipp Z, Bloom PP, Torres Soto M, Mansour MK, Sater MRA, Huntley MH, Turbett S, Chung RT, Chen YB, Hohmann EL. Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med 381: 2043–2050, 2019. doi: 10.1056/NEJMoa1910437. [DOI] [PubMed] [Google Scholar]
- 15.Bobilev D, Bhattarai S, Menon R, Klein B, Reddy S, Olle B, Roberts B, Bucci V, Norman J. VE303, a rationally designed bacterial consortium for prevention of recurrent Clostridioides difficile (C. difficile) infection (rCDI), stably restores the gut microbiota after vancomycin (vanco)-induced dysbiosis in adult healthy volunteers (HV). Open Forum Infect Dis 6: S60, 2019. doi: 10.1093/ofid/ofz359.130. [DOI] [Google Scholar]
- 16.Bobilev D, Vaickus L, Depetrillo P, Klein B, Reddy S, Olle B, Roberts B, Norman J. Mo1955 – Ve303, a live biotherapeutic product for prevention of recurrent Clostridioides difficile (C. difficile) infection. Preliminary results of a phase 1, open-label healthy volunteers study of oral Ve303 after vancomycin. Gastroenterology 156: S-899–S-900, 2019. doi: 10.1016/S0016-5085(19)39218-2. [DOI] [Google Scholar]
- 17.Hansen R, Sanderson I, Muhammed R, Allen S, Tzivinikos C, Henderson P, Gervais L, Jeffery IB, Mullins DP, O‘Herlihy EA, Weinberg JD, Kitson G, Russell RK, Wilson D. A phase I randomized, double-blind, placebo-controlled study to assess the safety and tolerability of (Thetanix®) Bacteroides thetaiotaomicron in adolescents with stable Crohn’s disease. Gastroenterology 156: S447, 2019. doi: 10.1016/S0016-5085(19)37969-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henn MR, O’Brien EJ, Diao L, Feagan BG, Sandborn WJ, Huttenhower C, Wortman JR, McGovern BH, Wang-Weigand S, Lichter DI, Chafee M, Ford CB, Bernardo P, Zhao P, Simmons S, Tomlinson AD, Cook DN, Pomerantz RJ, Misra BK, Auninš JG, Trucksis M. A Phase 1b safety study of SER-287, a spore-based microbiome therapeutic for active mild to moderate ulcerative colitis. Gastroenterology 160: 115–127.e30, 2021. doi: 10.1053/j.gastro.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garber K. First microbiome-based drug clears phase III, in clinical trial turnaround. Nat Rev Drug Discov 19: 655–656, 2020. doi: 10.1038/d41573-020-00163-4. [DOI] [PubMed] [Google Scholar]
- 20.McGovern BH, Ford CB, Henn MR, Pardi DS, Khanna S, Hohmann EL, O'Brien EJ, Desjardins CA, Bernardo P, Wortman JR, Lombardo MJ, Litcofsky KD, Winkler JA, McChalicher CWJ, Li SS, Tomlinson AD, Nandakumar M, Cook DN, Pomerantz RJ, Aunins JG, Trucksis M. SER-109, an investigational microbiome drug to reduce recurrence after Clostridioides difficile infection: lessons learned from a phase 2 trial. Clin Infect Dis, ciaa387, 2020. doi: 10.1093/cid/ciaa387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dubberke ER, Lee CH, Orenstein R, Khanna S, Hecht G, Gerding DN. Results from a randomized, placebo-controlled clinical trial of a RBX2660-A microbiota-based drug for the prevention of recurrent Clostridium difficile infection. Clin Infect Dis 67: 1198–1204, 2018. doi: 10.1093/cid/ciy259. [DOI] [PubMed] [Google Scholar]
- 22.Huibregtse IL, Zaat SA, Kapsenberg ML, Sartori da Silva MA, Peppelenbosch MP, van Deventer SJ, Braat H. Genetically modified Lactococcus lactis for delivery of human interleukin-10 to dendritic cells. Gastroenterol Res Pract 2012: 1–7, 2012. doi: 10.1155/2012/639291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Whitaker WR, Shepherd ES, Sonnenburg JL. Tunable expression tools enable single-cell strain distinction in the gut microbiome. Cell 169: 538–546 e512, 2017. doi: 10.1016/j.cell.2017.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmela C, Chevarin C, Xu Z, Torres J, Sevrin G, Hirten R, Barnich N, Ng SC, Colombel JF. Adherent-invasive Escherichia coli in inflammatory bowel disease. Gut 67: 574–587, 2018. doi: 10.1136/gutjnl-2017-314903. [DOI] [PubMed] [Google Scholar]
- 25.Citorik RJ, Mimee M, Lu TK. Sequence-specific antimicrobials using efficiently delivered RNA-guided nucleases. Nat Biotechnol 32: 1141–1145, 2014. doi: 10.1038/nbt.3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kokai-Kun JF, Roberts T, Coughlin O, Le C, Whalen H, Stevenson R, Wacher VJ, Sliman J. Use of ribaxamase (SYN-004), a beta-lactamase, to prevent Clostridium difficile infection in beta-lactam-treated patients: a double-blind, phase 2b, randomised placebo-controlled trial. Lancet Infect Dis 19: 487–496, 2019. doi: 10.1016/S1473-3099(18)30731-X. [DOI] [PubMed] [Google Scholar]
- 27.Fischbach MA. Microbiome: focus on causation and mechanism. Cell 174: 785–790, 2018. doi: 10.1016/j.cell.2018.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Britton GJ, Contijoch EJ, Mogno I, Vennaro OH, Llewellyn SR, Ng R, Li Z, Mortha A, Merad M, Das A, Gevers D, McGovern DPB, Singh N, Braun J, Jacobs JP, Clemente JC, Grinspan A, Sands BE, Colombel JF, Dubinsky MC, Faith JJ. Microbiotas from humans with inflammatory bowel disease alter the balance of Gut Th17 and RORgammat(+) regulatory T cells and exacerbate colitis in mice. Immunity 50: 212–224 e214, 2019. doi: 10.1016/j.immuni.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atarashi K, Tanoue T, Oshima K, Suda W, Nagano Y, Nishikawa H, Fukuda S, Saito T, Narushima S, Hase K, Kim S, Fritz JV, Wilmes P, Ueha S, Matsushima K, Ohno H, Olle B, Sakaguchi S, Taniguchi T, Morita H, Hattori M, Honda K. Treg induction by a rationally selected mixture of Clostridia strains from the human microbiota. Nature 500: 232–236, 2013. doi: 10.1038/nature12331. [DOI] [PubMed] [Google Scholar]
- 30.Atarashi K, Suda W, Luo C, Kawaguchi T, Motoo I, Narushima S, Kiguchi Y, Yasuma K, Watanabe E, Tanoue T, Thaiss CA, Sato M, Toyooka K, Said HS, Yamagami H, Rice SA, Gevers D, Johnson RC, Segre JA, Chen K, Kolls JK, Elinav E, Morita H, Xavier RJ, Hattori M, Honda K. Ectopic colonization of oral bacteria in the intestine drives TH1 cell induction and inflammation. Science 358: 359–365, 2017. doi: 10.1126/science.aan4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y, Wiesnoski DH, Helmink BA, Gopalakrishnan V, Choi K, DuPont HL, Jiang ZD, Abu-Sbeih H, Sanchez CA, Chang CC, Parra ER, Francisco-Cruz A, Raju GS, Stroehlein JR, Campbell MT, Gao J, Subudhi SK, Maru DM, Blando JM, Lazar AJ, Allison JP, Sharma P, Tetzlaff MT, Wargo JA, Jenq RR. Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nat Med 24: 1804–1808, 2018. [Erratum in Nat Med 25: 188, 2019]. doi: 10.1038/s41591-018-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen LJ, Cho JH, Gevers D, Chu H. Genetic factors and the intestinal microbiome guide development of microbe-based therapies for inflammatory bowel diseases. Gastroenterology 156: 2174–2189, 2019. doi: 10.1053/j.gastro.2019.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atarashi K, Tanoue T, Shima T, Imaoka A, Kuwahara T, Momose Y, Cheng G, Yamasaki S, Saito T, Ohba Y, Taniguchi T, Takeda K, Hori S, Ivanov II, Umesaki Y, Itoh K, Honda K. Induction of colonic regulatory T cells by indigenous Clostridium species. Science 331: 337–341, 2011. doi: 10.1126/science.1198469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, Liu H, Cross JR, Pfeffer K, Coffer PJ, Rudensky AY. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504: 451–455, 2013. doi: 10.1038/nature12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang PV, Hao L, Offermanns S, Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci USA 111: 2247–2252, 2014. doi: 10.1073/pnas.1322269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Furusawa C, Horinouchi T, Hirasawa T, Shimizu H. Systems metabolic engineering: the creation of microbial cell factories by rational metabolic design and evolution. Adv Biochem Eng Biotechnol 131: 1–23, 2013. [DOI] [PubMed] [Google Scholar]
- 37.Mortha A, Chudnovskiy A, Hashimoto D, Bogunovic M, Spencer SP, Belkaid Y, Merad M. Microbiota-dependent crosstalk between macrophages and ILC3 promotes intestinal homeostasis. Science 343: 1249288, 2014. doi: 10.1126/science.1249288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Costello SP, Soo W, Bryant RV, Jairath V, Hart AL, Andrews JM. Systematic review with meta-analysis: faecal microbiota transplantation for the induction of remission for active ulcerative colitis. Aliment Pharmacol Ther 46: 213–224, 2017. doi: 10.1111/apt.14173. [DOI] [PubMed] [Google Scholar]
- 39.Shepherd ES, DeLoache WC, Pruss KM, Whitaker WR, Sonnenburg JL. An exclusive metabolic niche enables strain engraftment in the gut microbiota. Nature 557: 434–438, 2018. doi: 10.1038/s41586-018-0092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huibregtse IL, Marietta EV, Rashtak S, Koning F, Rottiers P, David CS, van Deventer SJ, Murray JA. Induction of antigen-specific tolerance by oral administration of Lactococcus lactis delivered immunodominant DQ8-restricted gliadin peptide in sensitized nonobese diabetic Abo Dq8 transgenic mice. J Immunol 183: 2390–2396, 2009. doi: 10.4049/jimmunol.0802891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parada Venegas D, De la Fuente MK, Landskron G, Gonzalez MJ, Quera R, Dijkstra G, Harmsen HJM, Faber KN, Hermoso MA. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol 10: 277, 2019. [Erratum in Front Immunol 10: 1486, 2019]. doi: 10.3389/fimmu.2019.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Donia MS, Fischbach MA. Human microbiota. Small molecules from the human microbiota. Science 349: 1254766, 2015. doi: 10.1126/science.1254766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen LJ, Esterhazy D, Kim SH, Lemetre C, Aguilar RR, Gordon EA, Pickard AJ, Cross JR, Emiliano AB, Han SM, Chu J, Vila-Farres X, Kaplitt J, Rogoz A, Calle PY, Hunter C, Bitok JK, Brady SF. Commensal bacteria make GPCR ligands that mimic human signalling molecules. Nature 549: 48–53, 2017. doi: 10.1038/nature23874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sugimoto Y, Camacho FR, Wang S, Chankhamjon P, Odabas A, Biswas A, Jeffrey PD, Donia MS. A metagenomic strategy for harnessing the chemical repertoire of the human microbiome. Science 366: eaax9176, 2019. doi: 10.1126/science.aax9176. [DOI] [PubMed] [Google Scholar]
- 45.Song X, Sun X, Oh SF, Wu M, Zhang Y, Zheng W, Geva-Zatorsky N, Jupp R, Mathis D, Benoist C, Kasper DL. Microbial bile acid metabolites modulate gut RORgamma(+) regulatory T cell homeostasis. Nature 577: 410–415, 2020. doi: 10.1038/s41586-019-1865-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mallick H, Franzosa EA, McLver LJ, Banerjee S, Sirota-Madi A, Kostic AD, Clish CB, Vlamakis H, Xavier RJ, Huttenhower C. Predictive metabolomic profiling of microbial communities using amplicon or metagenomic sequences. Nat Commun 10: 3136, 2019. doi: 10.1038/s41467-019-10927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Medema MH, Fischbach MA. Computational approaches to natural product discovery. Nat Chem Biol 11: 639–648, 2015. doi: 10.1038/nchembio.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cohen LJ, Kang HS, Chu J, Huang YH, Gordon EA, Reddy BV, Ternei MA, Craig JW, Brady SF. Functional metagenomic discovery of bacterial effectors in the human microbiome and isolation of commendamide, a GPCR G2A/132 agonist. Proc Natl Acad Sci USA 112: E4825–4834, 2015. doi: 10.1073/pnas.1508737112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Y-Y, Chen D-Q, Chen L, Liu J-R, Vaziri ND, Guo Y, Zhao Y-Y. Microbiome–metabolome reveals the contribution of gut–kidney axis on kidney disease. J Transl Med 17: 5, 2019. doi: 10.1186/s12967-018-1756-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo CJ, Chang FY, Wyche TP, Backus KM, Acker TM, Funabashi M, Taketani M, Donia MS, Nayfach S, Pollard KS, Craik CS, Cravatt BF, Clardy J, Voigt CA, Fischbach MA. Discovery of reactive microbiota-derived metabolites that inhibit host proteases. Cell 168: 517–526 e518, 2017. doi: 10.1016/j.cell.2016.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Milshteyn A, Colosimo DA, Brady SF. Accessing bioactive natural products from the human microbiome. Cell Host Microbe 23: 725–736, 2018. doi: 10.1016/j.chom.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.An D, Oh SF, Olszak T, Neves JF, Avci FY, Erturk-Hasdemir D, Lu X, Zeissig S, Blumberg RS, Kasper DL. Sphingolipids from a symbiotic microbe regulate homeostasis of host intestinal natural killer T cells. Cell 156: 123–133, 2014. doi: 10.1016/j.cell.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brown EM, Ke X, Hitchcock D, Jeanfavre S, Avila-Pacheco J, Nakata T, Arthur TD, Fornelos N, Heim C, Franzosa EA, Watson N, Huttenhower C, Haiser HJ, Dillow G, Graham DB, Finlay BB, Kostic AD, Porter JA, Vlamakis H, Clish CB, Xavier RJ. Bacteroides-derived sphingolipids are critical for maintaining intestinal homeostasis and symbiosis. Cell Host Microbe 25: 668–680.e7, 2019. doi: 10.1016/j.chom.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bhatt AP, Pellock SJ, Biernat KA, Walton WG, Wallace BD, Creekmore BC, Letertre MM, Swann JR, Wilson ID, Roques JR, Darr DB, Bailey ST, Montgomery SA, Roach JM, Azcarate-Peril MA, Sartor RB, Gharaibeh RZ, Bultman SJ, Redinbo MR. Targeted inhibition of gut bacterial beta-glucuronidase activity enhances anticancer drug efficacy. Proc Natl Acad Sci USA 117: 7374–7381, 2020. doi: 10.1073/pnas.1918095117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakamoto N, Sasaki N, Aoki R, Miyamoto K, Suda W, Teratani T, Suzuki T, Koda Y, Chu P-S, Taniki N, Yamaguchi A, Kanamori M, Kamada N, Hattori M, Ashida H, Sakamoto M, Atarashi K, Narushima S, Yoshimura A, Honda K, Sato T, Kanai T. Gut pathobionts underlie intestinal barrier dysfunction and liver T helper 17 cell immune response in primary sclerosing cholangitis. Nat Microbiol 4: 492–503, 2019. doi: 10.1038/s41564-018-0333-1. [DOI] [PubMed] [Google Scholar]
- 56.Blount KF, Shannon WD, Deych E, Jones C. Restoration of bacterial microbiome composition and diversity among treatment responders in a phase 2 trial of RBX2660: an investigational microbiome restoration therapeutic. Open Forum Infect Dis 6: ofz095, 2019. 10.1093/ofid/ofz095. [DOI] [PMC free article] [PubMed] [Google Scholar]


