Abstract
Background
In December 2020, Israel began a mass vaccination campaign against coronavirus disease 2019 (Covid-19) by administering the BNT162b2 vaccine, which led to a sharp curtailing of the outbreak. After a period with almost no cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, a resurgent Covid-19 outbreak began in mid-June 2021. Possible reasons for the resurgence were reduced vaccine effectiveness against the delta (B.1.617.2) variant and waning immunity. The extent of waning immunity of the vaccine against the delta variant in Israel is unclear.
Methods
We used data on confirmed infection and severe disease collected from an Israeli national database for the period of July 11 to 31, 2021, for all Israeli residents who had been fully vaccinated before June 2021. We used a Poisson regression model to compare rates of confirmed SARS-CoV-2 infection and severe Covid-19 among persons vaccinated during different time periods, with stratification according to age group and with adjustment for possible confounding factors.
Results
Among persons 60 years of age or older, the rate of infection in the July 11–31 period was higher among persons who became fully vaccinated in January 2021 (when they were first eligible) than among those fully vaccinated 2 months later, in March (rate ratio, 1.6; 95% confidence interval [CI], 1.3 to 2.0). Among persons 40 to 59 years of age, the rate ratio for infection among those fully vaccinated in February (when they were first eligible), as compared with 2 months later, in April, was 1.7 (95% CI, 1.4 to 2.1). Among persons 16 to 39 years of age, the rate ratio for infection among those fully vaccinated in March (when they were first eligible), as compared with 2 months later, in May, was 1.6 (95% CI, 1.3 to 2.0). The rate ratio for severe disease among persons fully vaccinated in the month when they were first eligible, as compared with those fully vaccinated in March, was 1.8 (95% CI, 1.1 to 2.9) among persons 60 years of age or older and 2.2 (95% CI, 0.6 to 7.7) among those 40 to 59 years of age; owing to small numbers, the rate ratio could not be calculated among persons 16 to 39 years of age.
Conclusions
These findings indicate that immunity against the delta variant of SARS-CoV-2 waned in all age groups a few months after receipt of the second dose of vaccine.
A key to the containment of the coronavirus disease 2019 (Covid-19) pandemic is mass vaccination of the population. However, the success of this policy is challenged by breakthrough infection and disease in fully vaccinated persons. One potential cause of breakthrough infection is the emergence of new variants of concern1 that escape immunity, thus reducing the effectiveness of the vaccine. Several studies investigating the effectiveness of the BNT162b2 vaccine (Pfizer–BioNTech) against the beta (B.1.351)2,3 and delta (B.1.617.2)4-6 variants showed only modest rates of breakthrough infection and disease, whereas other studies showed higher rates.7,8
A second potential cause of breakthrough infection is waning of the immunity conferred by the vaccine. Mass vaccination with the BNT162b2 vaccine began in December 2020, and little is known about waning immunity over time. A recent study on longer-term follow-up of the participants in the phase 2–3 randomized trial of the BNT162b2 vaccine9 showed a reduction in vaccine efficacy from 96% (in the period of 7 days to <2 months after receipt of the second dose) to 84% (in the period of 4 months to approximately 7 months after receipt of the second dose), which indicated a decrease in protection by a factor of four (i.e., [100−84]÷[100−96]). Preliminary reports of waning effectiveness of the same vaccine have come from a health maintenance organization in Israel10 and from the United States,11 and a decrease in vaccine-induced neutralization titers during the first 6 months after receipt of the second dose of vaccine has been reported.12
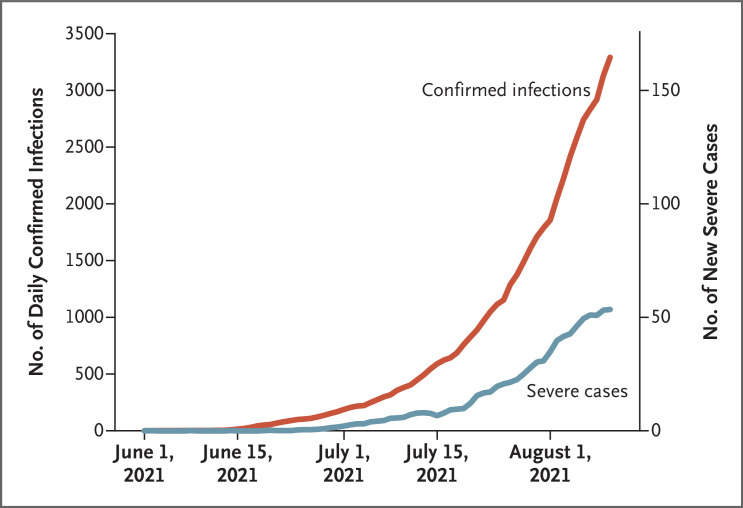
Israel conducted a very successful vaccination campaign using the BNT162b2 vaccine.13-15 Starting in December 2020, more than half the adult population received two doses of vaccine within 3 months. The vaccination campaign, together with social measures, led to a sharp curtailing of the outbreak. By May 2021, infection rates had decreased to a few dozen cases daily, most of which were in unvaccinated persons or in persons returning from abroad. However, the number of polymerase-chain-reaction (PCR) tests that were positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) started to rise exponentially in June 2021, with a substantial number of infections being reported in vaccinated persons (Figure 1). This rise in community transmission was followed by a concomitant increase in the numbers of severe cases and deaths, in both the vaccinated and unvaccinated populations. Genetic analysis showed that as of June 2021, more than 98% of the positive cases in Israel were attributed to the delta variant.16 In this study, we estimated the role of waning immunity in the observed breakthrough against the delta variant.
Figure 1. Daily Confirmed SARS-CoV-2 Infections and New Cases of Severe Covid-19 among Fully Vaccinated Persons in Israel, June through Early August 2021.
The graph shows increases in the numbers of daily severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and new cases of severe coronavirus disease 2019 (Covid-19), on different scales, during the delta variant wave among persons who had received two doses of vaccine.
Methods
Data Source
Data on all residents of Israel who had been fully vaccinated before June 1, 2021, and who had not been infected before the study period were extracted from the Israeli Ministry of Health database on September 2, 2021. We defined fully vaccinated persons as those for whom 7 days or more had passed since receipt of the second dose of the BNT162b2 vaccine. We used the Ministry of Health official database that contains all information regarding Covid-19 (see Supplementary Methods 1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). We extracted from the database information on all documented SARS-CoV-2 infections (i.e., positive result on PCR assay) and on the severity of the disease after infection. We focused on infections that had been documented in the period from July 11 through 31, 2021 (study period), removing from the data all confirmed cases that had been documented before that period. The start date was selected as a time when the virus had already spread throughout the entire country and across population sectors. The end date was just after Israel had initiated a campaign regarding the use of a booster vaccine (third dose). The study period happened to coincide with the school summer vacation.
We omitted from all the analyses children and adolescents younger than 16 years of age (most of whom were unvaccinated or had been recently vaccinated). Only persons 40 years of age or older were included in the analysis of severe disease because severe disease was rare in the younger population. Severe disease was defined as a resting respiratory rate of more than 30 breaths per minute, oxygen saturation of less than 94% while the person was breathing ambient air, or a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen of less than 300.14 Persons who died from Covid-19 during the follow-up period were included in the study and categorized as having had severe disease.
During the study period, approximately 10% of the detected infections were in residents of Israel returning from abroad. Most residents who traveled abroad had been vaccinated and were exposed to different populations, so their risk of infection differed from that in the rest of the study population. We therefore removed from the analysis all residents who had returned from abroad in July.
Vaccination Schedule
The official vaccination regimen in Israel involved the administration of the second dose 3 weeks after the first dose. All residents 60 years of age or older were eligible for vaccination starting on December 20, 2020, thus becoming fully vaccinated starting in mid-January 2021. At that time, younger persons were eligible for vaccination only if they belonged to designated groups (e.g., health care workers and severely immunocompromised adults). The eligibility age was reduced to 55 years on January 12, 2021, and to 40 years on January 19, 2021. On February 4, 2021, all persons 16 years of age or older became eligible for vaccination. Thus, if they did not belong to a designated group, persons 40 to 59 years of age received the second dose starting in mid-February, and those 16 to 39 years of age received the second dose starting in the beginning of March. On the basis of these dates, we defined our periods of interest in half months starting from January 16; vaccination periods for individual persons were determined according to the time that they had become fully vaccinated (i.e., 1 week after receipt of the second dose). All the analyses were stratified according to vaccination period and to age group (16 to 39 years, 40 to 59 years, and ≥60 years).
Statistical Analysis
The association between the rate of confirmed infections and the period of vaccination provides a measure of waning immunity. Without waning of immunity, one would expect to see no differences in infection rates among persons vaccinated at different times. To examine the effect of waning immunity during the period when the delta variant was predominant, we compared the rate of confirmed infections (per 1000 persons) during the study period (July 11 to 31, 2021) among persons who became fully vaccinated during various periods. The 95% confidence intervals for the rates were calculated by multiplying the standard confidence intervals for proportions by 1000. A similar analysis was performed to compare the association between the rate of severe Covid-19 and the vaccination period, but for this outcome we used periods of entire months because there were fewer cases of severe disease.
To account for possible confounders, we fitted Poisson regressions. The outcome variable was the number of documented SARS-CoV-2 infections or cases of severe Covid-19 during the study period. The period of vaccination, which was defined as 7 days after receipt of the second dose of the Covid-19 vaccine, was the primary exposure of interest. The models compared the rates per 1000 persons between different vaccination periods, in which the reference period for each age group was set according to the time at which all persons in that group first became eligible for vaccination. A differential effect of the vaccination period for each age group was allowed by the inclusion of an interaction term between age and vaccination period. Additional potential confounders were added as covariates, as described below, and the natural logarithm of the number of persons was added as an offset. For each vaccination period and age group, an adjusted rate was calculated as the expected number of weekly events per 100,000 persons if all the persons in that age group had been vaccinated in that period. All the analyses were performed with the use of the glm function in the R statistical software package.17
In addition to age and sex, the regression analysis included as covariates the following confounders. First, because the event rates were rising rapidly during the study period (Figure 1), we included the week in which the event was recorded. Second, although PCR testing is free in Israel for all residents, compliance with PCR-testing recommendations is variable and is a possible source of detection bias. To partially account for this, we stratified persons according to the number of PCR tests that had been performed during the period of March 1 to November 31, 2020, which was before the initiation of the vaccination campaign. We defined three levels of use: zero, one, and two or more PCR tests. Finally, the three major population groups in Israel (general Jewish, Arab, and ultra-Orthodox Jewish) have varying risk factors for infection. The proportion of vaccinated persons, as well as the level of exposure to the virus, differed among these groups.18 Although we restricted the study to dates when the virus was found throughout the country, we included population sector as a covariate to control for any residual confounding effect.
We conducted several secondary analyses to test the robustness of the results, including calculation of the rate of confirmed infection in a finer, 10-year age grouping and an analysis restricted to the general Jewish population (in which the delta outbreak began), which comprises the majority of persons in Israel. In addition, a model including a measure of socioeconomic status as a covariate was fitted to the data, because this was an important risk factor in a previous study.18 Since socioeconomic status was unknown for 5% of the persons in our study and the missingness of the data seemed to be informative, and also owing to concern regarding nondifferential misclassification (persons with unknown socioeconomic status may have had different rates of vaccination, infection, and severe disease), we did not include socioeconomic status in the main analysis. Finally, we compared the association between the number of PCR tests that had been conducted before the vaccination campaign (i.e., before December 2020) with the number that were conducted during the study period in order to evaluate the possible magnitude of detection bias in our analysis. A good correlation between past behavior regarding PCR testing and behavior during the study period would provide reassurance that the inclusion of past behavior as a covariate in the model would control, at least in part, for detection bias.
Results
Study Population
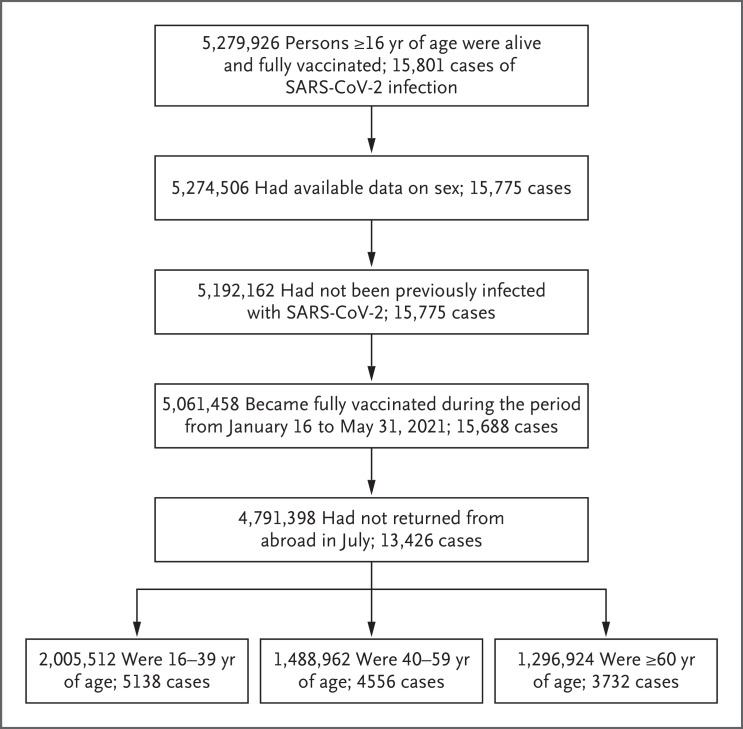
Among 5,279,926 fully vaccinated adults, we retained data on 4,791,398 persons for the main analysis (Figure 2). Among these persons, 13,426 had a positive PCR test (confirmed SARS-CoV-2 infection) and 403 had severe Covid-19. Table 1 provides the number of events according to vaccination period, and Table S1 in the Supplementary Appendix provides a more detailed summary according to vaccination period and age group. Table 1 shows the characteristics of the study population according to vaccination period; Tables S2 through S4 show these data for each of the three age groups.
Figure 2. Study Population.
The population included persons who were fully vaccinated before June 1, 2021, were not abroad during July 2021, and had no documented SARS-CoV-2 infection according to polymerase-chain-reaction assay before July 11, 2021.
Table 1. Demographic and Clinical Characteristics of the Study Population According to Vaccination Period.*.
| Variable | Vaccination Period | ||||||
|---|---|---|---|---|---|---|---|
| Jan. 16–31 (N=1,076,708) |
Feb. 1–15 (N=972,835) |
Feb. 16–28 (N=747,788) |
March 1–15 (N=819,040) |
March 16–31 (N=749,422) |
April 1–30 (N=325,201) |
May 1–31 (N=100,404) |
|
| No. of positive SARS-CoV-2 PCR tests | 3779 | 3182 | 2259 | 2146 | 1459 | 459 | 142 |
| No. of cases of severe Covid-19 | 251 | 108 | 16 | 17 | 5 | 5 | 1 |
| Male sex — no. (%) | 518,196 (48) | 459,251 (47) | 380,135 (51) | 410,371 (50) | 358,398 (48) | 153,619 (47) | 46,352 (46) |
| Age group — no. (%) | |||||||
| 16–39 yr | 125,977 (12) | 195,961 (20) | 352,722 (47) | 549,090 (67) | 496,779 (66) | 217,731 (67) | 67,252 (67) |
| 40–59 yr | 243,741 (23) | 418,282 (43) | 328,038 (44) | 208,064 (25) | 190,326 (25) | 78,281 (24) | 22,230 (22) |
| ≥60 yr | 706,990 (66) | 358,592 (37) | 67,028 (9) | 61,886 (8) | 62,317 (8) | 29,189 (9) | 10,922 (11) |
| No. of previous SARS-CoV-2 PCR tests — no. (%)† | |||||||
| 0 | 700,766 (65) | 655,201 (67) | 502,035 (67) | 564,855 (69) | 536,943 (72) | 240,548 (74) | 75,696 (75) |
| 1 | 204,238 (19) | 197,137 (20) | 163,752 (22) | 172,576 (21) | 144,087 (19) | 56,873 (17) | 16,320 (16) |
| ≥2 | 171,704 (16) | 120,497 (12) | 82,001 (11) | 81,609 (10) | 68,392 (9) | 27,780 (9) | 8,388 (8) |
| Population sector — no. (%)‡ | |||||||
| General Jewish | 970,782 (90) | 826,783 (85) | 617,113 (83) | 656,786 (80) | 506,554 (68) | 201,850 (62) | 72,292 (72) |
| Arab | 62,003 (6) | 107,704 (11) | 90,289 (12) | 115,399 (14) | 198,375 (26) | 102,798 (32) | 20,740 (21) |
| Ultra-Orthodox Jewish | 43,923 (4) | 38,348 (4) | 40,386 (5) | 46,855 (6) | 44,493 (6) | 20,553 (6) | 7,372 (7) |
The numbers of persons in the column heads represent the numbers of persons who were fully vaccinated during that period. Positivity on the polymerase-chain-reaction (PCR) assay for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; i.e., confirmed infection) and cases of severe coronavirus disease 2019 (Covid-19) were assessed in the study period of July 11 to 31, 2021. Percentages may not total 100 because of rounding.
Shown are the numbers of PCR tests that had been performed during the period of March 1 to November 31, 2020, which was before the initiation of the vaccination campaign.
Population sector was determined on the basis of the area of residency, with the use of classifications provided by the Israeli Bureau of Statistics.
Because of the risk-based vaccination policy in Israel, persons who were vaccinated in January were older than those who were vaccinated later. In addition, the lower risk of Covid-19–related complications among younger persons may have caused a belief that vaccination was not urgent or even necessary, which also affected the age distribution of vaccination over the months.19 The distribution of the number of previous PCR tests changed slightly between the periods, with 65% of the persons who became fully vaccinated in the second half of January having had no previous tests, as compared with 75% of those fully vaccinated in May. The number of tests seemed to be inversely correlated with age. A considerable difference was noted in the time of vaccination among the main population sectors: Arabs and ultra-Orthodox Jewish persons received vaccines later than did persons in the general Jewish population. Age and cultural differences contribute to these disparities.18 (These differences in risk factors were adjusted for by their inclusion as covariates in the Poisson regression analysis.)
Descriptive Analysis
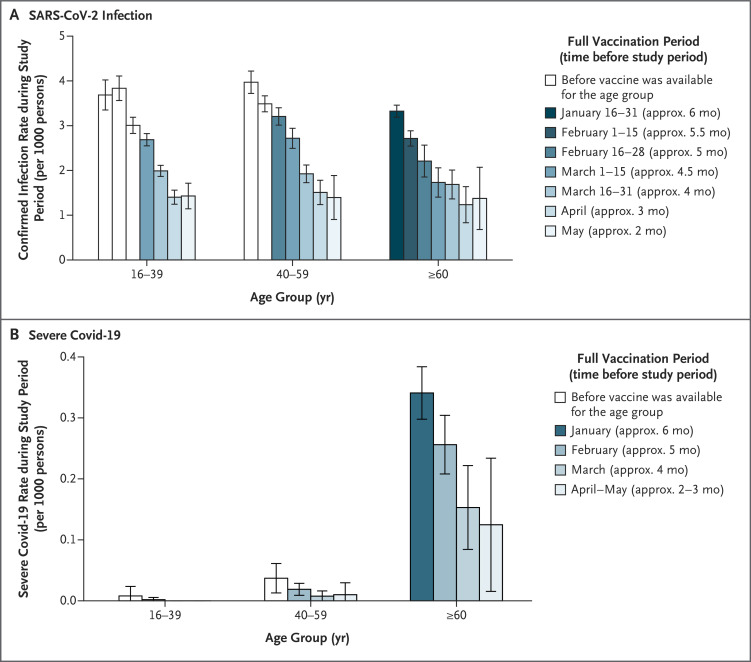
The rate of confirmed SARS-CoV-2 infection showed a clear increase as a function of time from vaccination. Among persons 60 years of age or older who were fully vaccinated in the second half of January, the rate was 3.3 confirmed infections per 1000 persons during the study period, as compared with 2.2 confirmed infections per 1000 persons who became fully vaccinated in the second half of February and 1.7 confirmed infections per 1000 persons fully vaccinated in the second half of March (Figure 3A). Similar results were observed in the other age groups and when the analysis was categorized according to age in decades (Figure 3A and S1). However, primarily health care workers and severely immunocompromised adults became fully vaccinated during the first three vaccination periods (January 16 to February 28) in the 16–39-year-old group and during the first two vaccination periods (January 16 to February 15) in the 40–59-year-old group; thus, the results for those vaccination periods in these age groups may be biased owing to selective samples and should be interpreted with caution.
Figure 3. Rates of Documented SARS-CoV-2 Infection and Severe Covid-19, July 11 to 31, 2021.
Shown are the rates of documented infection per 1000 persons (Panel A) and rates of severe Covid-19 per 1000 persons (Panel B), according to period of second dose of Covid-19 vaccine and age group. In the analyses in the age groups younger than 60 years, white bars represent periods during which vaccination was restricted to only designated groups (e.g., health care workers and severely immunocompromised adults). 𝙸 bars represent 95% confidence intervals, which are not adjusted for multiplicity. In Panel A, white bars represent half a month; in Panel B, white bars represent a month.
A similar pattern was observed in the analysis of severe Covid-19 in the group of persons 60 years of age or older (Figure 3B). In this analysis, vaccination periods were defined as January, February, March, and the combined April–May period because of the small numbers of severe cases in each age group. The rate of severe Covid-19 among persons 60 years of age or older who were fully vaccinated in January was 0.34 cases per 1000 persons over the study period and decreased to 0.26 cases per 1000 persons among those who were fully vaccinated in February, 0.15 cases per 1000 persons fully vaccinated in March, and 0.12 cases per 1000 persons fully vaccinated in the April–May period. The numbers of severe cases in the younger age groups were too small for conclusions to be drawn.
Regression Analysis
Table 2 and Table 3 present the results of the regression analyses regarding confirmed SARS-CoV-2 infection and severe Covid-19, respectively; the complete set of estimated coefficients is provided in Tables S5 and S6. For each age group, the numbers in the tables show the ratios between the estimated rates in the first period when the persons in that group were eligible to become fully vaccinated (i.e., the second half of January for persons ≥60 years of age, the second half of February for those 40 to 59 years of age, and the first half of March for those 16 to 39 years of age) and the estimated rates in the other periods. The tables also include the adjusted rates for each vaccination period. In the group of persons 60 years of age or older, the rate of confirmed infection among those vaccinated in the second half of January was 1.1 times as high as the rate among those vaccinated in the first half of February. The rate ratio increased to 1.6 and 2.2 when comparing January vaccinees with those who were vaccinated in March and in April, respectively. The same phenomenon, of an increasing rate of confirmed infection with increased time since vaccination, was observed in all age groups.
Table 2. Rate Ratios of Confirmed SARS-CoV-2 Infection According to Age Group and Vaccination Period.*.
| Age Group | Vaccination Period | ||||||
|---|---|---|---|---|---|---|---|
| Jan. 16–31 | Feb. 1–15 | Feb. 16–28 | March 1–15 | March 16–31 | April 1–30 | May 1–31 | |
| 16–39 Yr | |||||||
| Rate ratio of reference vs. period (95% CI) | 0.8 (0.7–0.9) | 0.7 (0.7–0.8) | 0.9 (0.8–1.0) | Reference | 1.2 (1.1–1.3) | 1.5 (1.4–1.8) | 1.6 (1.3–2.0) |
| Adjusted rate — no. of events/wk/100,000 persons | 108.7 | 117.9 | 93.4 | 85.7 | 72.7 | 55.4 | 52.1 |
| 40–59 Yr | |||||||
| Rate ratio of reference vs. period (95% CI) | 0.9 (0.8–1.0) | 1.0 (0.9–1.0) | Reference | 1.1 (1.0–1.2) | 1.4 (1.3–1.6) | 1.7 (1.4–2.1) | 2.1 (1.4–3.0) |
| Adjusted rate — no. of events/wk/100,000 persons | 117.2 | 110.7 | 106.0 | 95.9 | 75.0 | 61.3 | 51.2 |
| ≥60 Yr | |||||||
| Rate ratio of reference vs. period (95% CI) | Reference | 1.1 (1.1–1.2) | 1.3 (1.1–1.5) | 1.6 (1.4–2.0) | 1.6 (1.3–2.0) | 2.2 (1.6–3.1) | 2.2 (1.3–3.6) |
| Adjusted rate — no. of events/wk/100,000 persons | 105.7 | 92.4 | 82.3 | 64.3 | 65.2 | 47.9 | 49.1 |
Analyses were adjusted for week of infection, number of previous PCR tests (0, 1, or ≥2), population sector, and sex. Shown are rate ratios for confirmed SARS-CoV-2 infection during the period of July 11 through 31, 2021 (study period), as a function of time since full vaccination. We defined fully vaccinated persons as those for whom 7 days or more had passed since receipt of the second dose of the BNT162b2 vaccine. The comparison was between the estimated rate among persons who became fully vaccinated during the first vaccination period in which their age group was eligible (reference; i.e., January 16 to 31 for persons ≥60 years of age, February 16 to 28 for persons 40 to 59 years of age, and March 1 to 15 for persons 16 to 39 years of age) and the estimated rate among persons who became fully vaccinated in another vaccination period. For example, among persons 60 years of age or older, the rate of confirmed SARS-CoV-2 infection during the July 11–31 period among those vaccinated in January (105.7 events per week per 100,000 persons) was divided by the rate among those vaccinated in the second half of March (65.2 events per week per 100,000), yielding a rate ratio of 1.6. The 95% confidence intervals are not adjusted for multiplicity.
Table 3. Rate Ratios of Severe Covid-19 According to Age Group and Vaccination Period.*.
| Age Group | Vaccination Period | ||
|---|---|---|---|
| January | February | March | |
| 40–59 Yr | |||
| Rate ratio of reference vs. period (95% CI) | 0.6 (0.3–1.4) | Reference | 2.2 (0.6–7.7) |
| Adjusted rate — no. of events/wk/100,000 persons | 1.0 | 0.6 | 0.3 |
| ≥60 Yr | |||
| Rate ratio of reference vs. period (95% CI) | Reference | 1.2 (1.0–1.5) | 1.8 (1.1–2.9) |
| Adjusted rate — no. of events/wk/100,000 persons | 10.7 | 9.0 | 5.9 |
For severe Covid-19, estimates are provided for the whole months of January, February, and March. Estimates are not provided for the youngest age group (16 to 39 years of age) and for the latest vaccination periods (April and May) because of very low case numbers. Analyses were adjusted for week of infection, number of previous PCR tests (0, 1, or ≥2), population sector, and sex. Shown are rate ratios during the period of July 11 through 31, 2021, as a function of time since full vaccination. The numbers in each age group are the ratios between the estimated rates in the first period when persons in that group were eligible to receive vaccination and the estimated rates in the other periods. The 95% confidence intervals are not adjusted for multiplicity.
Fewer cases of severe Covid-19 were noted in persons younger than 60 years of age, especially in the group of persons 16 to 39 years of age (Table S1), so the model could be fitted only to the groups of persons 40 to 59 years of age and those 60 years of age or older and only for the vaccination months of January through March. The confidence intervals were wide; however, the results suggest a monotonic increase in the rate of severe disease as time since vaccination increased.
The analysis was repeated with socioeconomic status as an additional covariate, with the use of four categories (0 to 3 [indicating low socioeconomic level], 4 to 6 [indicating medium socioeconomic level], 7 to 10 [indicating high socioeconomic level], and unknown) and yielded similar results with only slightly smaller rate ratios (Table S8). Similar results were obtained when the analysis was restricted to the general Jewish population (Table S9).
Discussion
The centralized health care system in Israel succeeded in vaccinating most of the Israeli population relatively early and in a short time.13-15 This population is, therefore, useful for studying the effects of the BNT162b2 vaccine on the spread of SARS-CoV-2 infection and severity of Covid-19, as well as for studying the waning of vaccine protection over time. The appearance and rapid predominance of the delta variant in June 2021 resulted in a dramatic increase in the number of new SARS-CoV-2 infections among fully vaccinated persons, which aroused concern regarding decreased efficacy of the vaccine over time (Figure 1).
A comparison of the rate of confirmed infection among persons vaccinated at different times revealed a clear increase in the rate as the time from vaccination increased in all age groups, with and without correction for measured confounding factors (Figure 3A and Table 2). The rate of confirmed infection among persons 60 years of age or older who became fully vaccinated in the second half of January was 1.6 times as high as that among persons in the same age group who became fully vaccinated in March. The data show a similar increase in rate with increasing time since vaccination in the other age groups. The rate of severe Covid-19 cases also increased as a function of time from vaccination. Serologic studies in Israel have shown a correlated time-dependent reduction in neutralization titers,12,20 which might be the biologic mechanism governing the observed waning immunity, and thus support the finding in this population-based research.
In contrast to early findings from the United Kingdom,5 approximately two thirds of the cases of severe Covid-19 in Israel during the study period occurred in persons who had received two doses of the BNT162b2 vaccine. Two major differences exist between the studies. First, the current analysis used data from July 2021, a time when, for most of the Israeli population, at least 5 months had passed since receipt of their second dose of vaccine. The U.K. data were collected during the period of April through June 2021, with a much shorter time from vaccination to infection. Second, Israel has followed the original Pfizer–BioNTech protocol of administering the second dose 3 weeks (21 days) after the initial injection in most recipients, whereas the time between doses in the United Kingdom has typically been longer.6
A comparison of vaccinated persons with unvaccinated persons is of interest in order to predict the future burden on the health system. We therefore obtained data on the entire Israeli population from the Israeli Central Bureau of Statistics and calculated the number of unvaccinated persons indirectly. Moreover, unvaccinated persons might differ from the vaccinated population in important characteristics that could result in biased estimates. Nevertheless, we estimated the effectiveness of the vaccine against confirmed SARS-CoV-2 infection (see Supplementary Analysis 1). Vaccinated persons were found to be protected even after 6 months, as compared with unvaccinated persons. However, vaccine effectiveness was considerably lower than it had been closer to the vaccination date. Our findings are in line with findings from the randomized trial of the BNT162b2 vaccine, which showed a reduction in vaccine efficacy against symptomatic infection from 96% in the first 2 months after vaccination to 84% at 4 to 7 months after vaccination, when averaged over all age groups combined.9
Observational studies are subject to confounding bias and detection bias. We examined these biases by using different sensitivity analyses (see Supplementary Analysis 2) and obtained similar results. Nevertheless, some sources of bias might remain; for instance, any effects that were due to differences in coexisting conditions between the vaccination periods could not be controlled for, because coexisting conditions are not recorded in the national database.
We did not separate the contribution of vaccine breakthrough due to waning immunity from the contribution due to the change in the dominant variant from alpha (B.1.1.7) to delta. Our analysis showed only the clear effect of waning vaccine-induced immunity against the delta variant. In addition, we were not able to quantify the extent of waning in the months immediately after vaccination (when the prevalence was extremely low in Israel).
Understanding the extent of waning immunity is critical for policy making, especially regarding vaccination strategies. The results presented here provided an epidemiologic basis for the decision by the Israeli Ministry of Health on July 30, 2021, to approve the administration of a booster (third dose) of Covid-19 vaccine to persons who had been vaccinated at least 5 months previously. The findings also suggest the need to follow the effects of waning immunity closely and to inform policymakers worldwide who are facing decisions regarding the administration of booster vaccinations.
Acknowledgments
We thank Ofra Amir, Ronen Fluss, Sarah Goldberg, Boaz Lev, Ami Mizrahi, Geert Molenberghs, Rami Yaari, and Arnona Ziv for fruitful discussions.
Supplementary Appendix
Disclosure Forms
This article was published on October 27, 2021, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Centers for Disease Control and Prevention. SARS-CoV-2 variant classifications and definitions. 2021. (https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html).
- 2.Mor O, Zuckerman NS, Hazan I, et al. BNT162b2 vaccination efficacy is marginally affected by the SARS-CoV-2 B.1.351 variant in fully vaccinated individuals. July 19, 2021. (https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3878825). preprint.
- 3.Abu-Raddad LJ, Chemaitelly H, Butt AA, et al. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med 2021;385:187-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med 2021;385:585-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheikh A, McMenamin J, Taylor B, Robertson C. SARS-CoV-2 delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021;397:2461-2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pouwels KB, Pritchard E, Matthews PC, et al. Effect of delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nat Med 2021. October 14 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang P, Hasan MR, Chemaitelly H, et al. BNT162b2 and mRNA-1273 COVID-19 vaccine effectiveness against the Delta (B.1.617.2) variant in Qatar. August 11, 2021. (https://www.medrxiv.org/content/10.1101/2021.08.11.21261885v1). preprint. [DOI] [PubMed]
- 8.Puranik A, Lenehan PJ, Silvert E, et al. Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. August 21, 2021. (https://www.medrxiv.org/content/10.1101/2021.08.06.21261707v3). preprint.
- 9.Thomas SJ, Moreira ED Jr, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. DOI: 10.1056/NEJMoa2110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mizrahi B, Lotan R, Kalkstein N, et al. Correlation of SARS-CoV-2 breakthrough infections to time-from-vaccine; preliminary study. July 31, 2021. (https://www.medrxiv.org/content/10.1101/2021.07.29.21261317v1). preprint. [DOI] [PMC free article] [PubMed]
- 11.Puranik A, Lenehan PJ, O’Horo JC, et al. Durability analysis of the highly effective BNT162b2 vaccine against COVID-19. September 7, 2021. (https://www.medrxiv.org/content/10.1101/2021.09.04.21263115v1). preprint. [DOI] [PMC free article] [PubMed]
- 12.Khoury DS, Cromer D, Reynaldi A, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med 2021;27:1205-1211. [DOI] [PubMed] [Google Scholar]
- 13.Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021;384:1412-1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet 2021;397:1819-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg Y, Mandel M, Woodbridge Y, et al. Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: a three-month nationwide experience from Israel. April 24, 2021. (https://www.medrxiv.org/content/10.1101/2021.04.20.21255670v1). preprint. [DOI] [PMC free article] [PubMed]
- 16.Nextstrain: real-time tracking of pathogen evolution (https://nextstrain.org/). [DOI] [PMC free article] [PubMed]
- 17.The R Foundation. The R project for statistical computing. 2020. (https://www.R-project.org/).
- 18.Muhsen K, Na’aminh W, Lapidot Y, et al. A nationwide analysis of population group differences in the COVID-19 epidemic in Israel, February 2020–February 2021. Lancet Reg Health Eur 2021;7:100130-100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Delphi Group at Carnegie Mellon University in partnership with Facebook. COVID-19 symptom survey: topline report on COVID-19 vaccination in the United States, survey waves 6–8, January 10–February 27, 2021. (https://www.cmu.edu/delphi-web/surveys/CMU_Topline_Vaccine_Report_20210312.pdf).
- 20.Wall EC, Wu M, Harvey R, et al. Neutralising antibody activity against SARS-CoV-2 VOCs B.1.617.2 and B.1.351 by BNT162b2 vaccination. Lancet 2021;397:2331-2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.