Abstract
Objective
This study identifies trajectories of parent depressive symptoms after having a child born with genital atypia due to a disorder/difference of sex development (DSD) or congenital adrenal hyperplasia (CAH) and across the first year postgenitoplasty (for parents who opted for surgery) or postbaseline (for parents who elected against surgery for their child). Hypotheses for four trajectory classes were guided by parent distress patterns previously identified among other medical conditions.
Methods
Participants included 70 mothers and 50 fathers of 71 children diagnosed with a DSD or CAH with reported moderate to high genital atypia. Parents were recruited from 11 US DSD specialty clinics within 2 years of the child’s birth and prior to genitoplasty. A growth mixture model (GMM) was conducted to identify classes of parent depressive symptoms over time.
Results
The best fitting model was a five-class linear GMM with freely estimated intercept variance. The classes identified were termed “Resilient,” “Recovery,” “Chronic,” “Escalating,” and “Elevated Partial Recovery.” Four classes have previously been identified for other pediatric illnesses; however, a fifth class was also identified. The majority of parents were classified in the “Resilient” class (67.6%).
Conclusions
This study provides new knowledge about the trajectories of depressive symptoms for parents of children with DSD. Future studies are needed to identify developmental, medical, or familial predictors of these trajectories.
Keywords: differences of sex development, DSD, intersex, parents, psychosocial, psychological distress
Introduction
Most parents of children with chronic medical conditions appear to cope well over time with the stressors that arise from their child’s illness and subsequent treatments (Katz et al., 2018; Price et al., 2016). However, the literature on adjustment for parents of children diagnosed with a disorder/difference of sex development (DSD) remains limited (Sandberg et al., 2017a). Only recently has research begun to systematically explore the impact of a DSD diagnosis on family psychological adjustment using reliable and valid measures, and prospective analyses of parental adjustment remain few for these rare diagnoses (Sandberg et al., 2017a).
After receiving a diagnosis of DSD with genital atypia for their child, parents face decisions concerning sex of rearing, genital surgery, and with whom to share information about the child’s diagnosis (Crissman et al., 2011). Although a DSD diagnosis does not ubiquitously result in distress for parents, a subset of parents are at risk for clinical distress (Perez et al., 2019; Sandberg et al., 2017b). Recent research has begun to quantify parent distress levels following the birth of a child with DSD (Ellens et al., 2017; Pasterski et al., 2014; Perez et al., 2019). These cross-sectional analyses identified average parental levels of depressive symptoms comparable to population norms, yet approximately a quarter of the parents endorsed clinically significant levels of depressive symptoms early on (Perez et al., 2019).
To date, our preliminary findings report that parent depressive symptoms are maintained 6 months postsurgery (Wolfe-Christensen et al., 2017), with a decrease by 12 months postsurgery compared with presurgery levels (Ellens et al., 2017). Although mean rates of depressive symptoms reduce across time, a subset of parents continue to endorse moderate to severe symptoms (Ellens et al., 2017; Wolfe-Christensen et al., 2017). These initial findings indicate potential trends in parental distress; however, because these results only report mean levels, they do not depict the full variability in individual parent experiences and differences in distress over time according to parent gender. Additionally, current findings of parent sex differences are mixed in the context of DSD, with some studies identifying mothers with greater distress than fathers, whereas other studies report no differences (Delozier et al., 2019; Pasterski et al., 2014; Wolfe-Christensen et al., 2014). Time of assessment may be a factor in discrepant results, since parent sex differences appear to decrease across time (Ellens et al., 2017). Further research is needed to ascertain sex differences in parent psychological distress, including whether such differences change or emerge over time.
The Integrative Trajectory Model of Pediatric Medical Traumatic Stress is a theoretical framework that conceptualizes family trauma experienced in medical illness populations (Kazak et al., 2006; Price et al., 2016). Although this model has not been examined in DSD populations, the model was conceptualized in the context of several pediatric illnesses (e.g., cancer, cardiac surgeries, transplants), in which similarities in adjustment were identified across illnesses (Price et al., 2016). Four trajectory classes of pediatric medical traumatic stress are identified in the model, including Resilient, Recovery, Chronic, and Escalating classes (Price et al., 2016). The Resilient trajectory characterizes the majority of families and includes consistently low levels of symptoms across time. Recovery is a trajectory in which early distress occurs, but it reduces to low levels across time. Last, the Chronic trajectory includes maintenance of high levels across time; whereas, the Escalating trajectory report an increase in distress across time (Price et al., 2016). The trajectories of traumatic stress in this model potentially describe the experiences of parents of children with DSD.
In sum, little empirical literature exists on the experience of distress in parents of a child with a DSD. Previous assessment of mean scores across time identified an overall mean trend of parent symptoms, yet concealed nuances of individual trajectories of distress. Analysis of early individual trajectories of distress can provide important insight into parent psychological adjustment and identify similar trajectory patterns (i.e., latent classes) across parents. Moreover, determination of classes will allow for examination of potential gender differences in parent trajectories. The primary aim of this study was to identify individual trajectories and latent classes of parent depressive symptoms starting prior to surgical interventions through 1 year postsurgery/postbaseline. It was hypothesized that four classes would emerge (Resilient, Recovery, Chronic, and Escalating), reflecting classes described in the Integrative Trajectory Model of Pediatric Medical Traumatic Stress (Price et al., 2016). Similar to previous findings, it was expected that the majority of parents would be placed in the Resilient class, with low levels of distress. A secondary aim was to evaluate gender as a predictor of class membership. No hypotheses were made concerning gender given previous discrepant findings.
Materials and Methods
Participants and Procedures
Participants included parents (70 mothers and 50 fathers) of a child (N = 71) diagnosed with a DSD resulting in moderate to high stage of genital atypia. Demographic information is in Table I. Participants were recruited and consented from 11 sites across the United States between September 2013 and November 2017 as part of an ongoing prospective longitudinal study evaluating parental psychosocial adjustment to their child’s DSD diagnosis. Approval was obtained from institutional review boards at each site prior to participant consent. Participants were eligible if they: (a) were a caregiver of a child diagnosed with genital atypia, due to DSD or congenital adrenal hyperplasia, as defined by a Prader rating of 3–5 in children with 46, XX DSD or a Quigley rating 3–6 in children with 46, XY DSD or 45, X/46, XY sex chromosome DSD, (b) were English-speaking, (c) were at least 18 years old, and (d) had a child within 2 years of birth who had not yet undergone genitoplasty. Children with other comorbid medical conditions were deemed ineligible. Families were recruited and gave consent at regularly scheduled clinic visits. All parent participants included a mother or father (i.e., biological, step, or adoptive). One secondary caregiver identified as a grandmother. However, the child’s mother also completed measures; therefore, the current analyses removed the grandmother in order to focus on mother and father trajectories. Parents completed baseline measures prior to the child undergoing genitoplasty, and then at approximately 6 months (M = 5.70, SD = 1.73) and 12 months (M = 12.90, SD = 2.43) postsurgery, or postbaseline for parents who opted against surgery for their children. Participants were compensated $50 for participation.
Table I.
Demographics
| Children | Mothers | Fathers | |
|---|---|---|---|
| N | 71 | 70 | 50 |
| Age M (SD) | 9.03 months (6.90) | 31.92 (5.34) | 34.36 (7.07) |
| Sex of rearing N (%) | |||
| Girl | 44 (62.0) | ||
| Boy | 25 (35.2) | ||
| Unsure/non-designated | 2 (2.8) | ||
| Sex of rearing aligns with karyotype N (%) | 62 (88.6) | ||
| Diagnosis N (%) | |||
| 46, XX | 42 (59.2) | ||
| 21-hydroxylase deficiency | 35 (49.3 | ||
| 11-hydroxylase deficiency | 1 (1.4 | ||
| Ovotesticular DSD | 1 (1.4) | ||
| Unknown/unclassified | 1 (1.4) | ||
| Other | 2 (2.8) | ||
| 46, XY or 45, X/46, XY | 27 (38) | ||
| 5-Alpha reductase deficiency | 1 (1.4) | ||
| Androgen insensitivity syndrome | 2 (2.8) | ||
| Gonadal dysgenesis | 6 (8.5) | ||
| Ovotesticular DSD | 1 (1.4) | ||
| Unknown/unclassified | 15 (21.1) | ||
| Other | 1 (1.4) | ||
| Received genitoplasty N (%) | 65 (91.5) | ||
| Parent status | 69 (98.6) | 49 (98.0) | |
| Biological | 69 (98.6) | 49 (98.0) | |
| Adoptive | 1 (1.4) | 1 (2.0) | |
| Child had genitoplasty N (%) | |||
| Race/ethnicity N (%) | |||
| Hispanic | 16 (22.9) | 7 (14.0) | |
| Black/African American | 3 (4.3) | 3 (6.0) | |
| White/Caucasian | 46 (65.7) | 34 (68.0) | |
| Asian/Pacific Islander | 4 (5.7) | 4 (8.0) | |
| Multiracial | 3 (4.3) | 1 (2.0) | |
| Other | 5 (7.1) | 5 (10.0) | |
| Marital status N (%) | |||
| Single, never married | 10 (14.3) | 2 (4.0) | |
| Divorced | 2 (2.9) | 0 (0.0) | |
| Married to parent of child with DSD | 53 (75.7) | 43 (86.0) | |
| Living with parent of child with DSD | 7 (10.0) | 5 (10.0) | |
| Not living with, but partnered with parent of child with DSD | 1 (1.4) | 0 (0.0) | |
| Highest education attained N (%) | 2 (2.9) | 1 (2.0) | |
| Some high school or less | 2 (2.9) | 1 (2.0) | |
| Finished high school/GED | 8 (11.4) | 7 (14.0) | |
| Some college or associates degree | 19 (27.14) | 15 (30.0) | |
| Bachelor’s degree | 24 (34.3) | 17 (34.0) | |
| Graduate degree | 12 (17.1) | 9 (18.0) | |
| Household income N (%) | 12 (17.1) | 3 (6.0) | |
| $0–19,999a | 12 (17.1) | 3 (6.0) | |
| $20,000–39,999 | 12 (17.1) | 9 (18.0) | |
| $40,000–59,999 | 6 (8.6) | 5 (10.0) | |
| $60,000–79,999 | 7 (10.0) | 5 (10.0) | |
| $80,000–99,999 | 7 (10.0) | 6 (12.0) | |
| $100,000+ | 22 (31.4) | 21 (42.0) |
Note. The sum for participant race and marital status is greater than the sample due to participants being able to select Hispanic as ethnicity as well as a race.
Below the federal poverty line for a family of 3.
Materials
Demographic Questionnaire
A demographic questionnaire gathered child and parent information including child age, sex of rearing, type of DSD, and diagnosis (if known), as well as parent age, sex, marital status, race/ethnicity, education, employment status, and household income.
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996) is a 21-item self-report measure of depressive symptoms. Parents responded to multiple-choice items with scores ranging from 0 to 3. Higher total scores represent greater depressive symptoms. Total scores of 0–13 indicate minimal depression, 14–19 mild, 20–28 moderate, and 29–63 severe. Total scores of 14 or greater are considered clinically significant (Viinamäki et al., 2004). Internal consistency in the current sample was excellent (αBaseline= .93; α6 months = .94; α12 months = .93).
Statistical Analysis
Determination of sample size is complex for a growth mixture model (GMM; Berlin et al., 2014b). Moreover, the current sample was previously established and post-hoc power analyses can provided unwarranted confidence in the results (Wolf et al., 2013). In consideration of this, a power analysis was not conducted. Over the three timepoints for the 120 parents, 54 parents had data at all three timepoints, 39 had data at two timepoints, and 27 had data at one timepoint. Missing data analyses assessed for associations between demographic variables and depressive symptoms and their associated missing-data indicators (missing vs. not missing) at each time point. No timepoint was identified in which demographic variables were related to both depressive symptoms and to the missing data indicators. Full-information maximum-likelihood estimation was used to address missing data. This method can effectively estimate parameters using all available information and is recommended for smaller sample sizes (Berlin et al., 2014b; Enders, 2011; Preacher et al., 2008).
A GMM was conducted to evaluate parent depressive symptoms across the three timepoints. GMM is a type of latent growth modeling that assesses changes in individual outcomes across time, and identifies unobserved (latent) classes of individuals who have similar trajectories (Berlin et al., 2014b). Theory, previous literature, and analyses of descriptive characteristics were used to create hypotheses about growth trajectories and number of classes. It was hypothesized that the data would be best described as linear, and that four classes would emerge. To account for the nonindependence in observations due to mothers and fathers parenting the same child, standard errors were adjusted using complex analyses in the estimated models (TYPE=COMPLEX syntax in Mplus, which accounts for clustering; Muthén & Muthén, 2017) in which the child variable was identified for clustering.
First, a latent growth curve model (LGCM) was conducted to determine the best single-group representation of change, in which an intercept only and linear growth curve model were tested. Goodness of fit for the nonmixture model was assessed utilizing recommended fit statistics; excellent models result in CFI ≥ 0.95, RMSEA < 0.05, and SRMR < 0.05 (comparative fit index, root mean square error approximation, and standardized root mean residual, respectively; Berlin et al., 2014b; Hu & Bentler, 1999). Further, models with lower Bayesian Information Criteria (BIC), Akaike Information Criteria (AIC), and the Sample Size Adjusted BIC (SSA-BIC) are indicative of a better model fit (Berlin et al., 2014a; Geiser, 2013; Jung & Wickrama, 2008).
Next, a model building approach was used to identify the optimal number of latent classes. First, a latent class growth analysis (LCGA) was conducted. LCGA is a type of GMM in which the intercept and slope variances are fixed to zero within classes, and only between-class variance is allowed (Berlin et al., 2014b; Jung & Wickrama, 2008). Starting with fixed within-class variance (i.e., LCGA) reduces the number of estimated parameters, which can assist with convergence for smaller samples (Berlin et al., 2014b). Next, GMMs were conducted in which variances were systematically allowed to be freely estimated to evaluate if models with freed variances were a better fit to the data. (i.e., freed intercept for each class, then intercept and slope for each class). Analyses were conducted to at least one class greater than the four expected classes.
All models were estimated using Mplus (version 8.3; Muthén & Muthén, 2017), utilizing maximum-likelihood estimation with robust standard errors and chi-squared test statistics (MLR) to account for data skewness and nonindependence (Muthén & Muthén, 2017). Starting values were initially set at default and systematically increased to optimize replication and ensure global rather than local maxima. The optimal number of latent classes was assessed using information-criteria indices (i.e., AIC, BIC, and SSA-BIC; Geiser, 2013; Jung & Wickrama, 2008). The Lo, Mendell, and Rubin test (LMR) compares a model with G classes to a model with G-1 classes. A significant LMR suggests model G is the better model (Geiser, 2013). The bootstrap likelihood ratio test (BLRT) is considered a better indicator of model fit compared with LMR; however, the BLRT is not available with TYPE=COMPLEX. Entropy was used to determine the accuracy of participant classification into a class, with numbers closer to 1 representing better accuracy (Geiser, 2013). The final model included no <1% in each class (Jung & Wickrama, 2008), and theory and prior research were utilized in conjunction with model-fit information to deem the best fitting model (Berlin et al., 2014b).
Between-class differences based on parent gender were assessed using R3STEP, which assesses for the association between covariates and classes without changing class structure (Asparouhov & Muthén, 2014). The reference group for analyses was selected as the class with the lowest distress across time. Additionally, most-likely class membership was exported to SPSS and used to descriptively report parent class membership.
Results
Observed symptom means were below clinical cutoffs at each timepoint (MBaseline = 9.04, VarBaseline = 89.55; M6 months = 7.09, Var6 months = 68.21; M12 months = 5.78, Var12 months = 49.65).
Growth Modeling
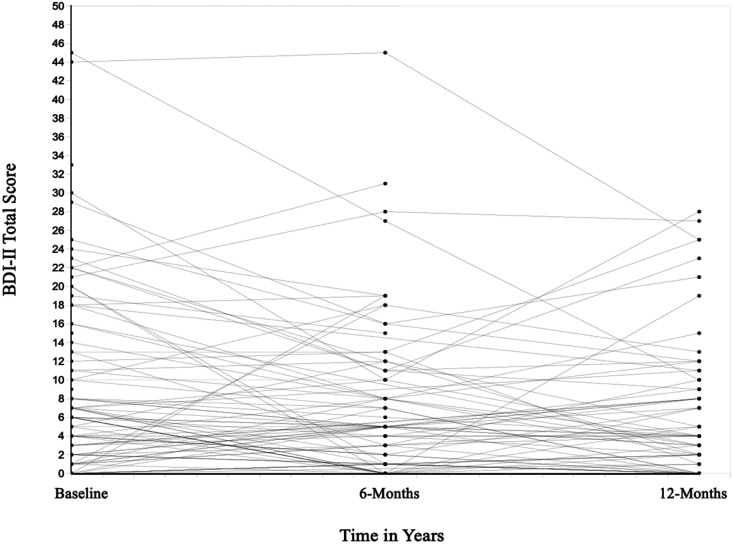
A linear growth model was selected as the best fitting growth model (MIntercept = 8.83, p < .001; VarIntercept = 64.05, p = .017; MSlope = −1.39, p < .001; VarSlope = 3.03, p = .730; see Table II). See Figure 1 for plot of raw scores. Mixture models were then systematically tested, estimating two to five classes and adjusting for clustered data. A review of model information criteria demonstrated a five-class LCGA model was similar to a four-class, so a sixth class was evaluated (see Table II). For the LCGA estimation, increase in classes resulted in lower AICs, BICs, and SSA-BIC up to six classes. Next, GMMs estimating two to six classes with freely estimated intercept variances were conducted; however, the six-class model produced errors of negative residual variance. Problems with parameter estimates occurred (i.e., negative residual variance error messages) in models in which intercept and slope variances freely estimated.
Table II.
Loglikelihood, Information Criteria, and Entropy Tests for Latent Class Growth Analysis and Growth Mixture Models
| Measure | Intercept | Linear | 1 Class | 2 Classes | 3 Classes | 4 Classes | 5 Classes | 6 Classes |
|---|---|---|---|---|---|---|---|---|
| LGCM | ||||||||
| CFI | 0.89 | 1.00 | ||||||
| TLI | 0.92 | 1.03 | ||||||
| RMSEA | 0.10 | 0.00 | ||||||
| SRMR | 0.11 | 0.02 | ||||||
| χ2 | 9.01 | 0.52 | ||||||
| df | 4 | 1 | ||||||
| χ2/df | 2.25 | 0.52 | ||||||
| AIC | 1,822.53 | 1,812.45 | ||||||
| BIC | 1,836.46 | 1,834.75 | ||||||
| SSA-BIC | 1,820.66 | 1,809.45 | ||||||
| LCGA | ||||||||
| Loglikelihood | −945.49 | −885.95 | −878.44 | −859.57 | −855.34 | −855.34 | ||
| AIC | 1,900.99 | 1,787.89 | 1,778.87 | 1,747.14 | 1,744.69 | 1,750.69 | ||
| BIC | 1,914.92 | 1,810.19 | 1,809.53 | 1,786.17 | 1,792.08 | 1,806.44 | ||
| SSA-BIC | 1,899.12 | 1,784.90 | 1,774.76 | 1,741.91 | 1,738.33 | 1,743.21 | ||
| Entropy | — | 0.91 | 0.80 | 0.88 | 0.82 | 0.83 | ||
| LMR test | — | 111.34 | 14.04 | 19.72 | 7.91 | −0.66 | ||
| LMR, p-value | — | .11 | .46 | .13 | .83 | .77 | ||
| GMM | ||||||||
| Loglikelihood | −901.78 | −881.00 | −867.25 | −856.58 | −849.92 | — | ||
| AIC | 1,815.57 | 1,780.00 | 1,758.50 | 1,743.15 | 1,735.85 | — | ||
| BIC | 1,832.29 | 1,805.09 | 1,791.95 | 1,784.96 | 1,786.03 | — | ||
| SSA-BIC | 1,813.32 | 1,776.63 | 1,754.02 | 1,737.54 | 1,729.12 | — | ||
| Entropy | — | 0.90 | 0.93 | 0.89 | 0.87 | — | ||
| LMR test | — | 38.86 | 25.71 | 19.96 | 12.43 | — | ||
| LMR, p-value | — | 0.28 | 0.29 | 0.12 | 0.38 | — | ||
Note. AIC = Akaike Information Criteria; BIC = Bayesian information criteria; LGCM = latent growth curve model.
Figure 1.
Plot of Participant Raw Scores.
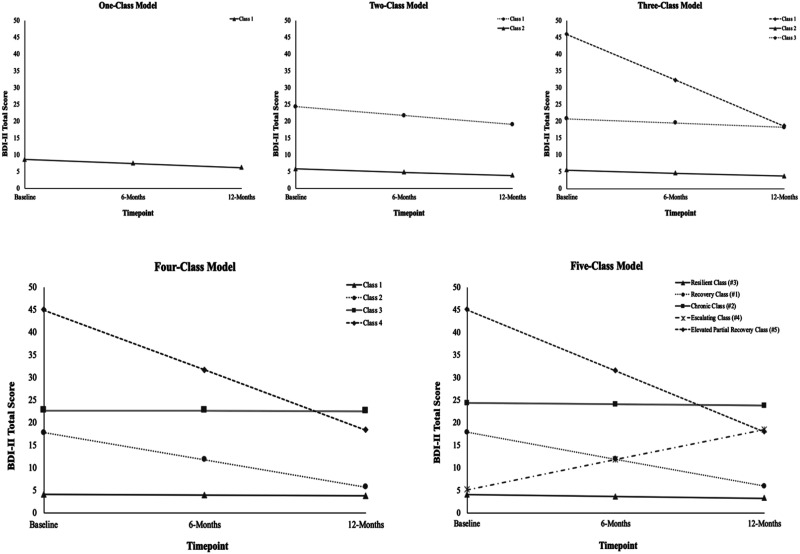
Comparison of fit statistics between the LCGAs and GMMs indicated the GMMs with estimated intercept variances produced better model fit (Table II). Analysis of fit indices across all classes demonstrated similarity between the four- and five-class GMMs with intercept variances estimated. The five-class model had a lower Loglikelihood, AIC, and SSA-BIC, with and a slightly higher BIC compared with the four-class model. Review of the estimated means and observed data within each class demonstrated the five-class model allowed for individuals with increasing levels of depressive symptoms to be placed within their own class and made distinct from the low-mean across time class (see Figure 2); therefore, the addition of that class made theoretical and meaningful sense. As such, a five-class GMM with an estimated intercept variance was selected as the best fitting mixture model (Figure 2).
Figure 2.
Growth mixture models of parent depressive symptoms.
Identified Latent Classes
Individual class estimated means per timepoint based on the model can be seen in Table IV, and are depicted in Figure 2. The BDI-II clinical cutoff score of ≥ 14 was used descriptively to gauge severity of symptoms within classes. The intercept and slope variance were the same across all classes, so it is only provided in the first described class below. The number of parents placed within each class is based off of a probability of class membership, which does not always result in a probability of 1.0. Therefore, the number of parents presented within each class will not be a whole number, and is represented as a decimal. Accuracy of class membership can be found in Table II (Entropy).
Table IV.
Individual Class Estimated Means of BDI-II Scores at Each Timepoint
| Baseline | 6 months | 12 months | |
|---|---|---|---|
| Resilient class (3) | 4.11 | 3.72 | 3.33 |
| Recovery class (1) | 17.92 | 11.94 | 5.97 |
| Chronic class (2) | 24.40 | 24.12 | 23.86 |
| Escalating class (4) | 5.22 | 11.88 | 18.55 |
| Elevated partial recovery class (5) | 45.12 | 31.58 | 18.04 |
Resilient Class
The largest class (3; 67.6%; N = 81.09) presented with low initial depressive symptoms (MIntercept = 4.11, p < .001; VarIntercept = 6.24, p = .003) that remained low over time (MSlope = −0.78, p = .132; VarIntercept = 0.00, p = 999.00). Given the low levels across time and using names already described in the literature (see Price et al., 2016), this class was termed “Resilient”.
Recovery Class
The next largest class (1; 18.1%; N = 21.78) presented with mean levels of depressive symptoms above the clinically significant cutoff at baseline (MIntercept = 17.92, p < .001). As can be seen in Figure 2, this class had a significant decrease in distress over time (MSlope = −11.95, p < .001), resulting in non-clinical levels of depressive symptoms at the last time point. This pattern is comparable with the “Recovery” class described in the literature.
Chronic Class
The third class (2) included 7.4% of parents (N = 8.91). This class had clinically significant initial levels (MIntercept = 24.40, p < .001), with no significant changes in symptoms across time (MSlope = −0.54, p = .831), suggesting chronic clinical distress. Given this pattern of symptoms, this class was named the “Chronic” class.
Escalating Class
The second-to-smallest group class (4; 5.2%; N = 6.19) included parents who reported low but statistically different from zero, levels of distress at baseline (MIntercept = 5.22, p = .033); however, their depressive symptoms significantly increased over time (MSlope = 13.34, p < .001) to clinically significant mean levels by the 12-month assessment. This pattern was named the “Escalating” class due to evidence of increasing symptoms over time.
Elevated Partial Recovery Class
Last, the smallest class (5; 1.7%; N = 2.04) included parents who reported the highest baseline symptoms (MIntercept = 45.12, p < .001) with the largest negative slope over time (MSlope = −27.08, p < .001). Despite this significant decline, these parents continued to endorse clinically significant levels at 12 months. As this class was not previously described in the literature, it was named the “Elevated Partial Recovery” class. (Note this class first emerged in the three-class model, see Figure 2).
Parent Sex Differences
Based on multinomial logistic regressions from R3STEP, and using the Resilient class as the reference group (the class with the lowest distress), fathers were less likely than mothers to be in the Recovery and Elevated Partial Recovery classes (Table III).
Table III.
Categorical Latent Variable Multinomial Logistic Regressions Using Three-Step Procedure
| Reference class | |||||
|---|---|---|---|---|---|
| Comparison class | B | SE | p | OR | 95% CI |
| Resilient (class 3) | |||||
| Recovery (class 1) | −1.34 | 0.67 | .045 | 0.26 | 0.071, 0.969 |
| Chronic (class 2) | −2.18 | 1.35 | .107 | 0.11 | 0.008, 1.598 |
| Escalating (class 4) | −1.98 | 1.61 | .218 | 0.14 | 0.006, 3.217 |
| Elevated partial recovery (class 5) | −20.84 | 1.61 | <.001 | 0.00 | 0.000, 0.000 |
Note. Mothers = 0; Fathers = 1. Negative coefficients indicate fathers were less likely than mothers to fall within the comparison class relative to the reference class.
To further describe gender differences in class membership, participants most likely class membership was exported and descriptive statistics were run: The majority of fathers (86%) were in the Resilient class, with 10% in the Recovery class, 2% in Chronic class, and 2% in the Escalating class. For mothers, the majority (58.6%) fell in the Resilient class, with 22.6% in the Recovery class, 10% in Chronic class, 5.7% in the Escalating class, and 2.8% in Elevated Partial Recovery class.
Discussion
This study examined trajectories of parental depressive symptoms across time, and identified four classes similar to classes identified in the previous research in other chronic illness conditions (i.e., Resilient, Escalating, Recovery, and Chronic classes; Price et al., 2016), as well as a fifth but very small class (i.e., Elevated Partial Recovery). Although small in size, this new class emerged as the third class within the statistical modeling, suggesting a significant difference from the other classes. The majority of parents fell within the Resilient class, indicating that most parents adjusted well to their child’s diagnosis and their depressive symptoms remained low across time. However, the emergence of the Escalating class highlights the importance of routine ongoing screening (e.g., Ernst et al., 2018; Sandberg et al., 2017a) to identify the subset of parents who initially adjust well but experience clinically increased depressive symptoms over time. Future studies are needed to discern stressors or developmental challenges that may trigger late onset of parental distress.
Although the majority of parents endorsed nonclinical levels of depressive symptoms, the Recovery class represents a subset of parents who reported early clinical distress that reduced over time and fell below clinical significance by 1 year. These findings suggest that stress abates as these parents move beyond difficult decisions or medical interventions for their child. Although speculative, another potential explanation is that parents’ symptoms may lessen when their child’s external genital appearance more closely aligns with sex of rearing (Wisniewski, 2017). Moreover, these parents may have received support or resources (e.g., behavioral health services) that may alleviate stress and enhance psychological adjustment over time. It is not known, however, to what extent behavioral health services or other support services were actually received that could account for the decrease in symptoms.
Similarly, a very small class, referred to as Elevated Partial Recovery, was identified. This class is distinguishable from the Recovery class due to very high baseline levels of depressive symptoms; however, these parents also had a significant reduction in symptoms across time, but not below thresholds for clinical significance. This lessening of symptoms may signify a form of recovery for these parents; yet, symptoms remain clinically significant at 1 year. Further information is needed to discern factors related to such high early distress, such as familial or medical factors. Moreover, because these parents continue to endorse clinical levels of depressive symptoms, ongoing screening is warranted.
Conversely, a small subset of parents endorsed clinical levels of depressive symptoms that persisted across time (Chronic class). Perhaps these parents encounter challenges across their child’s treatment, such as medical complications, complexity of treatment, or increased financial burden from medical treatments (Ellens et al., 2017; Perez et al., 2019). Moreover, these parents may have negative cognitive appraisals about their child’s diagnosis and treatment, such as perceived stigma towards their child or themselves concerning their child’s DSD (Rolston et al., 2015), perceived intrusiveness of the child’s illness into their work, family, or personal life, or greater perceived illness uncertainty, or appraisals of ambiguity or lack of information concerning their child’s diagnosis and treatment (Roberts et al., 2020).
The current results also identified that fathers are more likely than mothers to fall within the Resilient class as compared with Recovery or Elevated Partial Recovery classes. Although more than half of mothers fall in the Resilient class as well, 41% also evidence distress trajectories in one of the other four classes, suggesting greater variability in mothers’ distress than fathers. Moreover, mothers represent the majority of parents who endorse clinically significant symptoms at 1 year.
Strengths and Limitations
There are several strengths to this study. First, the prospective, longitudinal design offers insight into the changing aspects of parental psychological adjustment previously not captured for these families. Second, the person-centered statistical analyses distinguished individual parent experiences over time. Further, this study included a large sample of fathers, who have previously not been well represented in the DSD literature. Finally, the multi-site design across the US offered analyses of a large geographic area, which enhances generalizability.
This study should be considered in light of limitations. First, this study included an ethnically homogenous sample who speaks English, who also had relatively higher education levels and incomes. Thus, these results may not generalize to parents of other socioeconomic backgrounds and races. Recruitment also occurred exclusively at DSD specialty clinics. Future studies are needed to understand parent distress for families who receive services at smaller clinics without access to a multidisciplinary team or expertise in DSD. Further, the sample predominantly included parents who elected surgery for their child; thus, future studies are needed to evaluate potential differences between those who elect surgery and those who do not. Finally, due to the rarity of DSD with genital atypia, the sample size of this study was relatively small for the statistical analyses conducted. As such, the sample size of the Elevated Partial Recovery class, although meeting the requirement for at least one percent of the total sample, was a small class of only two parents. Future studies are recommended to confirm the current class findings and address generalizability of these results (Ram & Grimm, 2009).
Clinical Implications and Future Directions
The current findings indicate that the majority of parents fall within the Resilient or Recovery classes and do not have clinically significant depressive symptoms by 1-year postgenitoplasty/postbaseline. However, the challenge for clinicians will be to identify parents who fall within the Chronic, Escalating, and Elevated Partial Recovery classes, as these parents are experiencing clinically significant levels of depressive symptoms over time. Early and ongoing screening (e.g., Ernst et al., 2018; Sandberg et al., 2017a) will be needed to identify parents with elevated distress. Although currently there are no evidence-based interventions targeting distress in parents of children with DSD (Gardner & Sandberg, 2018), cognitive behavioral and problem solving interventions have shown positive results in reducing distress in parents of children with cancer (e.g., Kazak et al., 1999, 2005; Sahler et al., 2013). Interventions aimed at reducing illness uncertainty have also reduced distress for parents of children with cancer (Fedele et al., 2013; Hoff et al., 2005; Mullins et al., 2012). These interventions may similarly benefit parents of children with DSD.
With the establishment of depressive symptom trajectories for parents of children with DSD, future studies are needed to identify predictors of class membership for parents, particularly predictors of risk and resilience. Such studies should evaluate for medical risk factors including those associated with diagnoses, medical procedures, and complications, as well as levels of social support and mental health services (e.g., Ellens et al., 2017; Wolfe-Christensen et al., 2017). Future studies should also evaluate trajectories of distress as the child ages through developmental stages, such as gender expression (e.g., Crissman et al., 2011), starting school, puberty, and dating. Moreover, risk factors for mothers and fathers may differ, particularly across these developmental stages, medical treatment outcomes, or parenting roles.
Acknowledgments
We thank the families involved in this project for their time. All procedures complied with APA ethical standards. All individuals who have contributed significantly to this work have been acknowledged.
Funding
This work was funded by National Institutes of Health Grant NICHD R01HD074579 and the Vaughn Vennerberg II Endowment at Oklahoma State University.
Conflicts of interest: Dr Paul Austin—Pediatric advisory group & clinical investigator for Allergan. Dr Natalie Nokoff and Dr. Ming Chan—advisory group and clinical investigator for Neurocrine Biosciences.
References
- Asparouhov T., Muthén B. (2014). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes, 21(2), 1–22. [Google Scholar]
- Beck A. T., Steer R. A., Brown G. K. (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation.
- Berlin K. S., Williams N. A., Parra G. R. (2014a). An introduction to latent variable mixture modeling (Part 1): Overview and cross-sectional latent class and latent profile analyses. Journal of Pediatric Psychology, 39(2), 174–187. 10.1093/jpepsy/jst084 [DOI] [PubMed] [Google Scholar]
- Berlin, K. S., Williams, N. A., & Parra, G. R. (2014b). An introduction to latent variable mixture modeling (Part 2): Overview and cross-sectional latent class and latent profile analyses. Journal of Pediatric Psychology, 39(2), 174–187. http://doi.org/10.1093/jpepsy/jst085 [DOI] [PubMed] [Google Scholar]
- Crissman H. P., Warner L., Gardner M., Carr M., Schast A., Quittner A. L., Kogan B., Sandberg D. E. (2011). Children with disorders of sex development: A qualitative study of early parental experience. International Journal of Pediatric Endocrinology, 2011(1), 10. 10.1186/1687-9856-2011-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delozier A. M., Gamwell K. L., Sharkey C., Bakula D. M., Perez M. N., Wolfe-Christensen C., Austin P., Baskin L., Bernabé K. J., Chan Y.-M., Cheng E. Y., Diamond D. A., Ellens R. E. H., Fried A., Galan D., Greenfield S., Kolon T., Kropp B., Lakshmanan Y., Mullins L. L. (2019). Uncertainty and posttraumatic stress: Differences between mothers and fathers of infants with Disorders/Differences of Sex Development (DSD). Archives of Sexual Behavior, 48(5), 1617–1624. 10.1007/s10508-018-1357-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellens R. E. H., Bakula D. M., Mullins A. J., Scott Reyes K. J., Austin P., Baskin L., Bernabé K., Cheng E. Y., Fried A., Frimberger D., Galan D., Gonzalez L., Greenfield S., Kolon T., Kropp B., Lakshmanan Y., Meyer S., Meyer T., Mullins L. L., Wolfe-Christensen C. (2017). Psychological adjustment of parents of children born with atypical genitalia 1 year after genitoplasty. Journal of Urology, 198(4), 914–920. 10.1016/j.juro.2017.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C. K. (2011). Analyzing Longitudinal Data With Missing Values. Rehabilitation Psychology, 56(4), 267–288. 10.1037/a0025579 [DOI] [PubMed] [Google Scholar]
- Ernst M. M., Gardner M., Mara C. A., Délot E. C., Fechner P. Y., Fox M., Rutter M. M., Speiser P. W., Vilain E., Weidler E. M., Sandberg D. E.; The DSD-Translational Research Network Leadership Group and Psychosocial Workgroup. (2018). Psychosocial screening in disorders/differences of sex development: Psychometric evaluation of the Psychosocial Assessment Tool. Hormone Research in Paediatrics, 90(6), 368–313. 10.1159/000496114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedele D. A., Hullmann S. E., Chaffin M., Kenner C., Fisher M. J., Kirk K., Eddington A. R., Phipps S., Mcnall-Knapp R. Y., Mullins L. L. (2013). Impact of a parent-based interdisciplinary intervention for mothers on adjustment in children newly diagnosed with cancer. Journal of Pediatric Psychology, 38(5), 531–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner M., Sandberg D. E. (2018). Navigating surgical decision making in disorders of sex development (DSD). Frontiers in Pediatrics, 6(November), 1–9. 10.3389/fped.2018.00339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiser C. (2013). Data analysis with MPlus. The Guilford Press. [Google Scholar]
- Hoff A. L., Mullins L. L., Gillaspy S. R., Page M. C., Van Pelt J. C., Chaney J. M. (2005). An intervention to decrease uncertainly and distress among parents of children newly diagnosed with diabetes: A pilot study. Families, Systems and Health, 23(3), 329–342. 10.1037/1091-7527.23.3.329 [DOI] [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jung T., Wickrama K. A. S. (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. 10.1111/j.1751-9004.2007.00054.x [DOI] [Google Scholar]
- Katz L. F., Fladeboe K., King K., Gurtovenko K., Kawamura J., Friedman D., Compas B., Gruhn M., Breiger D., Lengua L., Lavi I., Stettler N. (2018). Trajectories of child and caregiver psychological adjustment in families of children with cancer. Health Psychology, 37(8), 725–735. 10.1037/hea0000619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A. E., Kassam-Adams N., Schneider S., Zelikovsky N., Alderfer M. A., Rourke M. (2006). An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology, 31(4), 343–355. http://doi.org/10.1093/jpepsy/jsj054 [DOI] [PubMed] [Google Scholar]
- Kazak A. E., Simms S., Alderfer M. A., Rourke M. T., Crump T., McClure K., Jones P., Rodriguez A., Boeving A., Hwang W.-T., Reilly A. (2005). Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. Journal of Pediatric Psychology, 30(8), 644–655. 10.1093/jpepsy/jsi051 [DOI] [PubMed] [Google Scholar]
- Kazak A. E., Simms S., Barakat L., Hobbie W., Foley B., Golomb V., Best M. (1999). Surviving Cancer Competently Intervention Program (SCCIP): A Cognitive-Behavioral and Family Therapy intervention for adolescent survivors of childhood cancer and their families. Family Process, 38(2), 176–191. 10.1111/j.1545-5300.1999.00176.x [DOI] [PubMed] [Google Scholar]
- Mullins L. L., Fedele D. A., Chaffin M., Hullmann S. E., Kenner C., Eddington A. R., Phipps S., Mcnall-Knapp R. Y. (2012). A clinic-based interdisciplinary intervention for mothers of children newly diagnosed with cancer: A pilot study. Journal of Pediatric Psychology, 37(10), 1104–1112. 10.1093/jpepsy/jss093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (2017). Mplus User’s Guide. Eighth Edition (8th ed.). Muthén & Muthén.
- Pasterski V., Mastroyannopoulou K., Wright D., Zucker K. J., Hughes I. A. (2014). Predictors of posttraumatic stress in parents of children diagnosed with a disorder of sex development. Archives of Sexual Behavior, 43(2), 369–375. 10.1007/s10508-013-0196-8 [DOI] [PubMed] [Google Scholar]
- Perez M. N., Delozier A. M., Aston C. E., Austin P., Baskin L., Chan Y.-M., Cheng E. Y., Diamond D. A., Fried A., Greenfield S., Kolon T., Kropp B., Lakshmanan Y., Meyer S., Meyer T., Nokoff N., Palmer B., Paradis A., Poppas D., Mullins L. L. (2019). Predictors of psychosocial distress in parents of young children with disorders of sex development. The Journal of Urology, 202(5), 1046–1051. 10.1097/ju.0000000000000424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., Wichman A. L., Maccallum R. C., Briggs N. E. (2008). Latent growth curve modeling. Sage Publication, Inc. 10.4135/9781412984737.n1 [DOI] [Google Scholar]
- Price J., Kassam-Adams N., Alderfer M. A., Christofferson J., Kazak A. E. (2016). Systematic review: A reevaluation and update of the Integrative (Trajectory) Model of Pediatric Medical Traumatic Stress. Journal of Pediatric Psychology, 41(1), 86–97. 10.1093/jpepsy/jsv074 [DOI] [PubMed] [Google Scholar]
- RamN., & , Grimm K. J. (2009). Methods and Measures: Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International Journal of Behavioral Development, 33(6), 565–576. 10.1177/0165025409343765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts C. M., Sharkey C. M., Bakula D. M., Perez M. N., Delozier A. J., Austin P. F., Baskin L. S., Chan Y.-M., Cheng E. Y., Diamond D. A., Fried A. J., Kropp B., Lakshmanan Y., Meyer S. Z., Meyer T., Nokoff N. J., Palmer B. W., Paradis A., Reyes K. J. S., Mullins L. L. (2020). Uncertainty as a longitudinal predictor of distress among caregivers of children born with DSD. Journal of Pediatric Psychology, 45(9), 1053–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolston A. M., Gardner M., Vilain E., Sandberg D. E. (2015). Parental reports of stigma associated with child’s disorder of sex development. International Journal of Endocrinology, 2015, 1–15. 10.1155/2015/980121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahler O. J. Z., Dolgin M. J., Phipps S., Fairclough D. L., Askins M. A., Katz E. R., Noll R. B., Butler R. W. (2013). Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: Results of a multisite randomized clinical trial. Journal of Clinical Oncology, 31(10), 1329–1335. 10.1200/JCO.2011.39.1870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg D. E., Gardner M., Callens N., Mazur T.; DSD-TRN PsycholocialWorkgroup, DSD-TRN Advocacy Advisory Network, & Accord Allliance. (2017). Interdisciplinary care in disorders/differences of sex development (DSD): The psychosocial component of the DSD – Translational Research Network. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(2), 279–292. 10.1002/ajmg.c.31561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg D. E., Pasterski V., Callens N. (2017). Introduction to the special section: Disorders of Sex Development. Journal of Pediatric Psychology, 42(5), 487–495. 10.1093/jpepsy/jsx065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viinamäki H., Tanskanen A., Honkalampi K., Koivumaa-Honkanen H., Haatainen K., Kaustio O., Hintikka J. (2004). Is the Beck Depression Inventory suitable for screening major depression in different phases of the disease? Nordic Journal of Psychiatry, 58(1), 49–53. 10.1080/08039480310000798 [DOI] [PubMed] [Google Scholar]
- Wisniewski A. B. (2017). Psychosocial implications of disorders of sex development treatment for parents. Current Opinion in Urology, 27(1), 11–13. 10.1097/MOU.0000000000000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf E. J., Harrington K. M., Clark S. L., Miller M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 73(6), 913–934. 10.1177/0013164413495237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe-Christensen C., Fedele D. A., Mullins L. L., Lakshmanan Y., Wisniewski A. B. (2014). Differences in anxiety and depression between male and female caregivers of children with a disorder of sex development. Journal of Pediatric Endocrinology and Metabolism, 27(7-8), 617–621. 10.1515/jpem-2014-0102 [DOI] [PubMed] [Google Scholar]
- Wolfe-Christensen C., Wisniewski A. B., Mullins A. J., Reyes K. J., Austin P., Baskin L., Bernabé K., Cheng E., Fried A., Frimberger D., Galan D., Gonzalez L., Greenfield S., Kolon T., Kropp B., Lakshmanan Y., Meyer S., Meyer T., Nokoff N. J., Mullins L. L. (2017). Changes in levels of parental distress after their child with atypical genitalia undergoes genitoplasty. Journal of Pediatric Urology, 13(1), 32.e1–32e6. 10.1016/j.jpurol.2016.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]