Abstract
Objective:
To evaluate the treatment effects of a hybrid hyrax-facemask (FM) combination in growing Class III patients.
Material and Methods:
A sample of 16 prepubertal patients (mean age, 9.5 ± 1.6 years) was investigated by means of pre- and posttreatment cephalograms. The treatment comprised rapid palatal expansion with a hybrid hyrax, a bone- and toothborne device. Simultaneously, maxillary protraction using an FM was performed. Mean treatment duration was 5.8 ± 1.6 months. The treatment group was compared with a matched control group of 16 untreated Class III subjects. Statistical comparisons were performed with the Mann-Whitney U-test.
Results:
Significant improvement in skeletal sagittal values could be observed in the treatment group over controls: SNA: 2.4°, SNB: −1.7°, Co-Gn: −2.3 mm, Wits appraisal: 4.5 mm. Regarding vertical changes, maintenance of vertical growth was obtained as shown by a small nonsignificant increase of FMA and a small significant decrease of the Co-Go-Me angle.
Conclusions:
The hybrid hyrax-FM combination was found to be effective for orthopedic treatment in growing Class III patients in the short term. Favorable skeletal changes were observed both in the maxilla and in the mandible. No dentoalveolar compensations were found.
Keywords: Hybrid hyrax, Skeletal anchorage, Class III malocclusion, RME
INTRODUCTION
Maxillary protraction using a facemask (FM), introduced by Delaire, has proven to be effective in Class III patients showing a maxillary deficiency.1–3 There is evidence that this method is particularly efficient during the early developmental phases.4–6 The most efficient treatment time seems to be in the early mixed dentition,7 although some studies also report good outcomes when treatment is started in the late mixed dentition.8
Usually, orthopedic forces for maxillary protrusion are applied via tooth-borne devices. A side effect of this approach is a mesial migration of the maxillary posterior teeth and a constriction of the space for the maxillary canines.9 This unwanted mesialization also seems to reduce the skeletal response to maxillary protraction.10
To overcome these drawbacks, application of orthopedic forces directly to the bone might be beneficial. Miniplates have already proven to be effective in maxillary protraction and to withstand the orthopedic forces in controlled studies.11,12 There is still no evidence, however, whether mini-implants are as reliable as miniplates.
FM therapy is often combined with rapid maxillary expansion (RME). Regarding the advantages of RME before maxillary protraction, the results have been controversial. Baik13 reported statistically significant differences in treatment outcomes depending on whether RME was performed in combination with FM. Larger forward (1.0 mm) and downward (0.5 mm) movement of point A was observed in the expansion group. In a meta-analysis, Jäger et al.7 identified a greater effect of maxillary protraction after RME. In a randomized clinical trial, however, Vaughn et al.14 found no statistically significant differences between groups treated with FM and with or without RME in any of the measured cephalometric variables. Similar results were reported in a recent investigation by Tortop et al.15
Skeletal anchorage of the RME device may help minimize the side effects caused by tooth-borne appliances such as buccal tipping, gingival recession, and root damage. However, the forces encountered during RME can reach very high levels that challenge the stability of skeletal anchorage devices. Some of the purely bone-borne RME devices16,17 have an unusually sturdy and bulky design. The need for invasiveness is high, since a flap has to be raised for insertion and removal. A higher risk of root lesions and infections has been described as well.16
In this study, a tooth- and bone-borne expander, the hybrid hyrax, was used.18,19 This device includes two orthodontic mini-implants in the anterior palate for skeletal anchorage and it is also attached to the first molars. By using this device, the above-mentioned side effects of RME can be minimized.19 It can be also used for maxillary expansion and simultaneous protraction.19,20 Within the limits of a pilot study, it showed high stability and efficacy.20 However, the clinical performance of mini-implant-borne devices for maxillary expansion and protraction has not yet been assessed in a controlled study.
The aim of this controlled study was to evaluate the treatment effects of a hybrid hyrax-FM combination in growing Class III patients.
MATERIALS AND METHODS
This study was approved by the ethics committee of The University of Düsseldorf. Sample size calculation (power analysis) was based on the results of a previous pilot study.20 Given a significant increase in SNA of 2.0° with a standard deviation of 1.9°, an alpha level of 0.05, and a power of 0.80, the required sample size was calculated to be 16 subjects in the treatment and control groups, respectively.
Consequently, 16 consecutively treated patients (10 males and 6 females) of white ancestry with dentoskeletal Class III malocclusion were included in the treatment group. All patients were treated in the same clinic using the hybrid hyrax-FM combination. Therapeutic success at the end of the observation period was not a determining factor for inclusion or exclusion of patients.
Lateral cephalograms were available for all subjects at the start (T1) and at the end (T2) of active treatment. Mean age at T1 was 9.5 ± 1.6 years, mean age at T2 was 10.4 ± 1.5 years, and the mean T1–T2 interval was 0.9 ± 0.4 years. At T1, all patients had a Class III malocclusion in the mixed dentition characterized by a Wits appraisal of −2 mm or less (mean, −5.6 ± 2.2 mm), anterior crossbite or incisor edge-to-edge relationship, and a Class III molar relationship. All patients showed a prepubertal stage of skeletal maturity according to the cervical vertebral maturation method (CS1-3),21 both at T1 and at T2.
A control group of 16 untreated subjects (8 males and 8 females) with dentoskeletal Class III malocclusion was obtained from the departments of orthodontics at the University of Florence, Italy, and the University of Michigan.22 The mean age at T1 was 9.4 ± 1.1 years, mean age at T2 was 10.4 ± 1.1 years, and the mean T1−T2 interval was 1.0 ± 0.3 years. The control group matched the treatment group as to type of dentoskeletal disharmony, skeletal maturation at each time point, sex distribution, and mean duration of observation intervals.
Treatment Protocol
A hybrid hyrax device was inserted in all patients of the treatment group (Figure 1a). Two 2 × 9-mm mini-implants (Benefit mini-implants; PSM Medical Solutions; Tuttlingen, Germany) were inserted in the anterior palate on both sides of the midpalatal suture. Predrilling was not necessary in these young patients.18 The implants were angled approximately parallel to each other. The laboratory-fabricated appliance comprised a split palatal screw (Hyrax, Dentaurum, Ispringen, Germany), two orthodontic bands fitted to the first molars, and two abutments screwed to mini-implants. These components were connected by rigid stainless steel wire 1.5 mm in diameter. For application of orthopedic protraction forces, rigid sectional wires were welded to the buccal side of the molar bands (stainless steel; diameter, 1.2 mm). The hooks in the canine region allowed the line of force to be close to the center of resistance of the maxilla, using the elastics for protraction.
Figure 1.
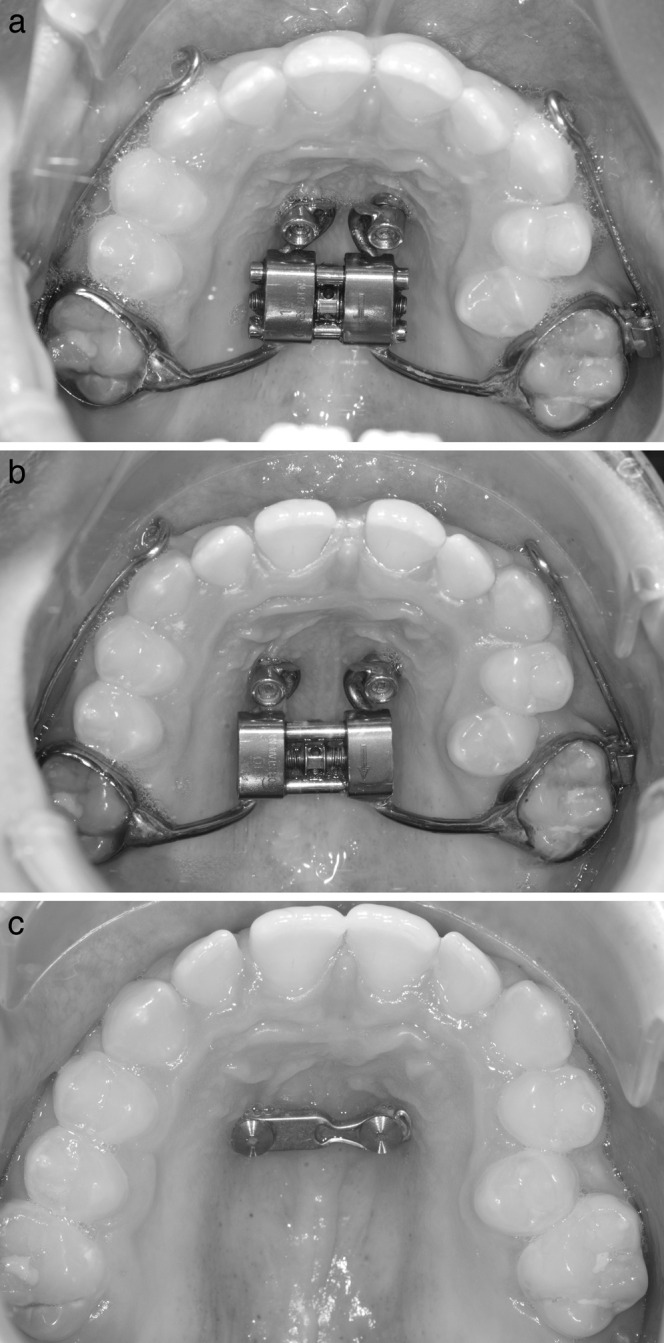
(a) Hybrid hyrax appliance in situ. Rigid sectional wires (stainless steel; diameter, 1.2 mm) were welded to the buccal side of the molar bands. A hook at the canine region enables orthopedic force application. (b) Situation after 1 week of expansion. Due to distraction of the midpalatal suture, a diastema mediale occurred. (c) Situation after removal of the hybrid hyrax. A modified plate was inserted for retention of maxillary transverse width.
Figure 2.
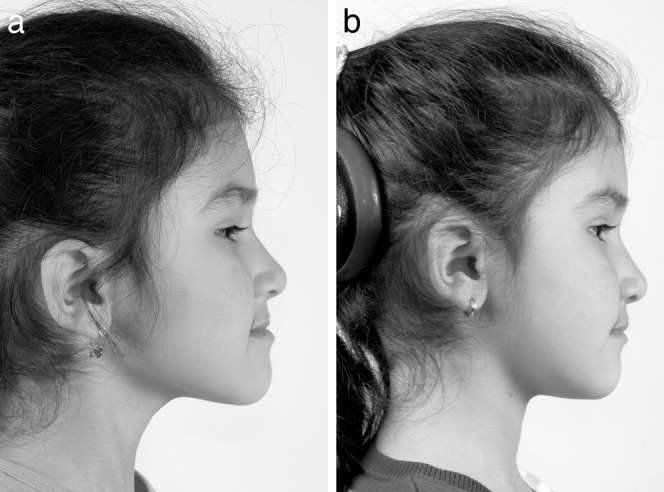
(a) Profile of an 8-year-old girl before treatment. (b) Profile after maxillary protraction of 7 months.
RME was performed by activating the split screw by 90° turns four times a day, resulting in an expansion of 0.8 mm per day (Figure 1a,b). Activation was continued until a transverse overcorrection of 30% was achieved.
Maxillary protraction was started simultaneously with the RME. The FM was adjusted and elastics were applied with a downward and forward force vector having an inclination of 20°–30° to the occlusal plane. The elastics delivered 400 g of force, controlled by a force gauge, on each side. The patients were instructed to wear the FM 16 hours per day.
Cephalometric Analysis and Method Error
A customized digitization regimen and analysis provided by Viewbox 3.0 (dHAL Software, Kifissia, Greece) was utilized for all the cephalograms examined in this study. The customized cephalometric analysis comprising measurements from the analyses of Jacobson,23 McNamara,24 and Steiner25 generated 24 variables, 11 angular and 13 linear, for each tracing.
Within a week, randomly selected cephalograms were remeasured by the same operator to determine the method error. The measurements at both times for each patient were analyzed with the intraclass coefficient correlation, which varied from 0.966 for SNB to 0.995 for the inclination of the maxillary incisor to the Frankfort horizontal plane. These values indicated a high level of intra-observer agreement. Linear measurement errors averaged 0.3 mm (SD, 0.8 mm), and angular measurements averaged 0.4° (SD, 0.6°).
Statistical Analysis
Homogeneity between the treatment and control groups allowed for comparisons without annualizing the data. In an exploratory analysis by the Shapiro-Wilk test, the data did not show normal distribution. Therefore, nonparametric statistics were applied. Significant differences between the cephalometric variables at T1 (comparison of starting forms) and during the T1–T2 interval in the treatment vs control groups were tested by means of the Mann-Whitney U-test. All statistical computations were performed using statistical software SPSS 12.0 (SPSS Inc, Chicago, Ill).
RESULTS
No significant differences were found between the demographic data of the treatment and the control groups. Comparison of the skeletal and dental characteristics between patients of the treatment and the control group showed no statistically significant differences, except for a larger Co-Go-Me angle in the control group (P < .05; Table 1).
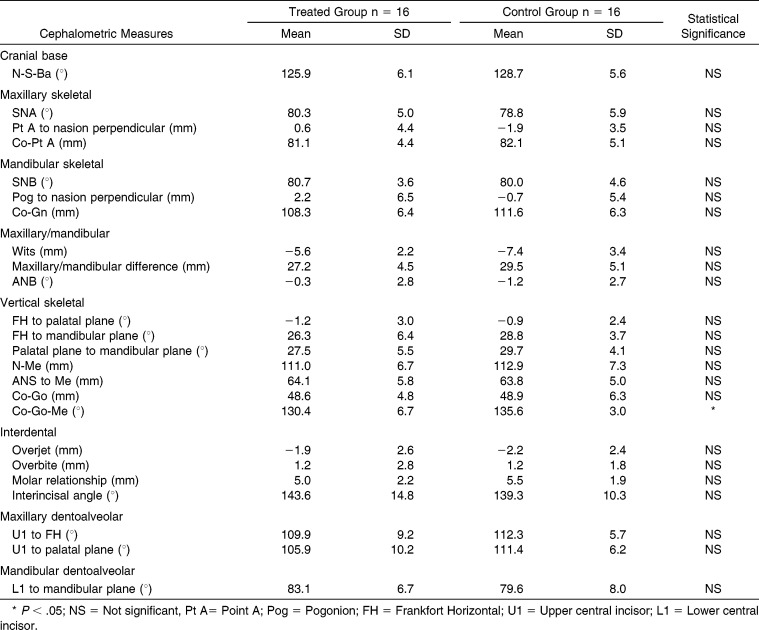
Table 1.
Comparison of Starting Forms at T1
In the treatment group, all the mini-implants remained stable throughout treatment. RME was performed without complications in all patients, with a midpalatal suture opening shown by the appearance of a midline diastema after a few days. FMs were worn without interruption by abrasions or pressure points.
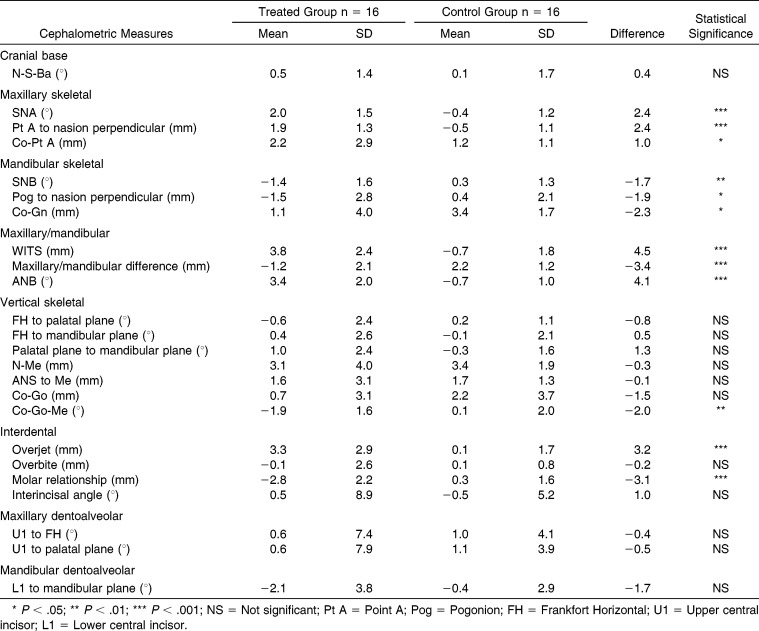
Significant differences caused by active treatment were observed between T1 and T2 by comparing the two groups (Table 2). Regarding advancement of the maxilla, SNA and Point A to nasion perpendicular showed significant increases of 2.4° and 2.4 mm, respectively, in the treatment group over the controls. Moreover, the treatment group exhibited a significant decrease in the length and sagittal position of the mandible compared with the control group (CoGn, −2.3 mm and SNB, −1.7°). Both effects led to significant changes in the sagittal maxillomandibular relationship. In the treatment group, the Wits appraisal increased by 4.5 mm and the ANB angle improved by 4.1° compared with the control group.
Table 2.
Comparison of Change During Treatment (T1–T2)
Regarding the vertical skeletal measurements, only the Co-Go-Me angle decreased significantly (2.0°) in the treatment sample vs the control sample. The other skeletal vertical values showed no significant differences between groups.
Treatment effects also occurred in the interdental measurements. Both overjet and molar relationship improved significantly (3.2 mm and −3.1 mm, respectively) in the treatment group over controls. No significant differences between groups could be found in overbite or inclination of the maxillary and mandibular incisors.
DISCUSSION
This investigation is the first controlled study evaluating the effectiveness of a Class III treatment protocol employing simultaneous mini-implant-borne maxillary expansion and protraction. Specific features of the study were (1) inclusion of consecutively treated Class III patients; (2) a control group of untreated subjects matching the treatment group as to type of dentoskeletal disharmony, skeletal maturation at each time point, sex distribution, and mean duration of observation intervals; and (3) treatment performed during the prepubertal stages of skeletal maturation.
Significant sagittal skeletal improvement was achieved, as shown by changes in SNA (2.4°) and Wits appraisal (4.5 mm) compared with the control group. These values were found to be slightly higher than those of conventional RME and FM therapy. In a controlled clinical study, Westwood et al.26 found increases of 1.6° in SNA and 4.3 mm in the Wits appraisal. A meta-analysis of conventional maxillary protraction reported a mean increase in the SNA angle of 1.4°.7
Occlusal effects related to the control group, however, appeared to be slightly higher using the conventional approach. In the study by Westwood et al.,26 the overjet improved by 4.8 mm compared with the 3.2 mm in the current investigation; the molar relationship improved by 3.8 mm compared with 3.1 mm.
But the greater occlusal effects using a dental-borne appliance are caused by a combination of sagittal skeletal improvement and mesial migration of the dentition, whereas the latter was avoided by using the hybrid hyrax. Accordingly, Celikoglu and Oktay27 observed a greater improvement of the overjet than of the WITS appraisal using a dental-borne maxillary protraction device, indicating a mesial movement of the maxillary dentition.27 Koh and Chung28 compared the treatment changes of skeletal- vs dental-anchored FM. They also found a greater skeletal improvement in young class III patients for the skeletal anchorage group. The maxillary incisors were retroclined compared with their inclination at treatment onset, whereas the incisors protruded in the dental anchorage group. All these results underline the effectiveness of skeletal anchorage. It enhances the orthopedic outcomes with a reduction in dental side effects.
No significant vertical effect was observed in the palatal or mandibular plane angle with respect to FH or in the overbite, which indicates a good adjustment of the force vector using the extended buccal sectional wires together with forward and downward force direction.
Only the Co-Go-Me angle showed a significant reduction (2.0°). This effect has already been observed in previous studies dealing with maxillary protraction and functional therapy in Class III patients.29,30 This morphogenetic anterior rotation of the mandible was effective in inducing significant decrements in mandibular length.31 The force applied to the chin in a cranial and posterior direction might be the cause. Along with a significant decrease in the SNB angle of 1.8°, the applied treatment protocol also seems to affect mandibular growth in a positive way.
Miniplates have proven to withstand orthopedic forces of maxillary protraction.12,32 In this study, the mini-implants were also found to remain stable. This stability might be related to the high bone quality of the insertion site and to the stable screw coupling to the appliance, which might lead to an increased biomechanical load capacity.33,34 Compared with miniplates, the hybrid hyrax appears to be less invasive in both insertion and removal. Mini-implants provide additional skeletal anchorage during RME, minimizing transverse and sagittal side effects.19
The results of this study represent short-term treatment effects encountered immediately after active therapy. Longitudinal studies to the end of growth are required to evaluate the long-term effects of these treatment modalities.
CONCLUSIONS
The hybrid hyrax-FM combination is an effective orthopedic treatment modality in growing Class III patients.
Significant advancement of the maxilla and significant improvement in the sagittal position of the mandible were achieved.
The need for surgical invasiveness is lower than that for purely bone-borne devices.
REFERENCES
- 1.Delaire J. Manufacture of the “orthopedic mask” [In French] Rev Stomatol Chir Maxillofac. 1971;72:579–582. [PubMed] [Google Scholar]
- 2.Mandall N, DiBiase A, Littlewood S, et al. Is early Class III protraction facemask treatment effective? A multicentre, randomized, controlled trial: 15-month follow-up. J Orthod. 2010;37:149–161. doi: 10.1179/14653121043056. [DOI] [PubMed] [Google Scholar]
- 3.Hickham JH. Maxillary protraction therapy: diagnosis and treatment. J Clin Orthod. 1991;25:102–113. [PubMed] [Google Scholar]
- 4.Takada K, Petdachai S, Sakuda M. Changes in dentofacial morphology in skeletal Class III children treated by a modified maxillary protraction headgear and a chin cup: a longitudinal cephalometric appraisal. Eur J Orthod. 1993;15:211–221. doi: 10.1093/ejo/15.3.211. [DOI] [PubMed] [Google Scholar]
- 5.Franchi L, Baccetti T, McNamara JA., Jr Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 6.Franchi L, Baccetti T, McNamara JA., Jr Shape-coordinate analysis of skeletal changes induced by rapid maxillary expansion and facial mask therapy. Am J Orthod Dentofacial Orthop. 1998;114:418–426. doi: 10.1016/s0889-5406(98)70187-8. [DOI] [PubMed] [Google Scholar]
- 7.Jager A, Braumann B, Kim C, Wahner S. Skeletal and dental effects of maxillary protraction in patients with angle class III malocclusion: a meta-analysis. J Orofac Orthop. 2001;62:275–284. doi: 10.1007/pl00001935. [DOI] [PubMed] [Google Scholar]
- 8.Yuksel S, Ucem TT, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23:559–568. doi: 10.1093/ejo/23.5.559. [DOI] [PubMed] [Google Scholar]
- 9.Ngan P, Yiu C, Hu A, Hagg U, Wei SH, Gunel E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur J Orthod. 1998;20:237–254. doi: 10.1093/ejo/20.3.237. [DOI] [PubMed] [Google Scholar]
- 10.Williams MD, Sarver DM, Sadowsky PL, Bradley E. Combined rapid maxillary expansion and protraction facemask in the treatment of Class III malocclusions in growing children: a prospective long-term study. Semin Orthod. 1997;3:265–274. doi: 10.1016/s1073-8746(97)80059-x. [DOI] [PubMed] [Google Scholar]
- 11.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sar C, Arman-Ozcirpici A, Uckan S, Yazici AC. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011;139:636–649. doi: 10.1016/j.ajodo.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 13.Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 14.Vaughn GA, Mason B, Moon HB, Turley PK. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005;128:299–309. doi: 10.1016/j.ajodo.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 15.Tortop T, Keykubat A, Yuksel S. Facemask therapy with and without expansion. Am J Orthod Dentofacial Orthop. 2007;132:467–474. doi: 10.1016/j.ajodo.2006.09.047. [DOI] [PubMed] [Google Scholar]
- 16.Mommaerts MY. Transpalatal distraction as a method of maxillary expansion. Br J Oral Maxillofac Surg. 1999;37:268–272. doi: 10.1054/bjom.1999.0127. [DOI] [PubMed] [Google Scholar]
- 17.Koudstaal MJ, van der Wal KG, Wolvius EB, Schulten AJ. The Rotterdam Palatal Distractor: introduction of the new bone-borne device and report of the pilot study. Int J Oral Maxillofac Surg. 2006;35:31–35. doi: 10.1016/j.ijom.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Wilmes B, Drescher D. A miniscrew system with interchangeable abutments. J Clin Orthod. 2008;42:574–580; quiz, 595. [PubMed] [Google Scholar]
- 19.Wilmes B, Nienkemper M, Drescher D. Application and effectiveness of a mini-implant- and tooth-borne rapid palatal expansion device: the hybrid hyrax. World J Orthod. 2010;11:323–330. [PubMed] [Google Scholar]
- 20.Ludwig B, Glasl B, Bowman SJ, Drescher D, Wilmes B. Miniscrew-supported Class III treatment with the Hybrid RPE Advancer. J Clin Orthod. 2010;44:533–539. Qui 561. [PubMed] [Google Scholar]
- 21.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 22.Alexander AEZ, McNamara JA, Jr, Franchi L, Baccetti T. Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. Am J Orthod Dentofacial Orthop. 2009;135:700–701. doi: 10.1016/j.ajodo.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 23.Jacobson A. The “Wits” appraisal of jaw disharmony. Am J Orthod. 1975;67:125–138. doi: 10.1016/0002-9416(75)90065-2. [DOI] [PubMed] [Google Scholar]
- 24.McNamara JA., Jr A method of cephalometric evaluation. Am J Orthod. 1984;86:449–469. doi: 10.1016/s0002-9416(84)90352-x. [DOI] [PubMed] [Google Scholar]
- 25.Steiner CC. Cephalometrics for you and me. Am J Orthod. 1953;39:729–755. [Google Scholar]
- 26.Westwood PV, McNamara JA, Jr, Baccetti T, Franchi L, Sarver DM. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306–320. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 27.Celikoglu M, Oktay H. Effects of maxillary protraction for early correction of class III malocclusion. Angle Orthod. 2014;84:628–633. doi: 10.1093/ejo/cjt006. [DOI] [PubMed] [Google Scholar]
- 28.Koh SD, Chung DH. Comparison of skeletal anchored facemask and tooth-boren facemask according to vertical skeletal pattern and growth stage. Eur J Orthod. 2014;36:86–92. doi: 10.2319/060313-421.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baccetti T, Franchi L, McNamara JA., Jr Thin-plate spline analysis of treatment effects of rapid maxillary expansion and face mask therapy in early Class III malocclusions. Eur J Orthod. 1999;21:275–281. doi: 10.1093/ejo/21.3.275. [DOI] [PubMed] [Google Scholar]
- 30.Tollaro I, Baccetti T, Franchi L. Mandibular skeletal changes induced by early functional treatment of Class III malocclusion: a superimposition study. Am J Orthod Dentofacial Orthop. 1995;108:525–532. doi: 10.1016/s0889-5406(95)70053-6. [DOI] [PubMed] [Google Scholar]
- 31.Lavergne J, Gasson N. Direction and intensity of mandibular rotation in the sagittal adjustment during growth of the jaws. Scand J Dent Res. 1977;85:193–196. doi: 10.1111/j.1600-0722.1977.tb00553.x. [DOI] [PubMed] [Google Scholar]
- 32.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludwig B, Glasl B, Bowman SJ, Wilmes B, Kinzinger GS, Lisson JA. Anatomical guidelines for miniscrew insertion: palatal sites. J Clin Orthod. 2011;45:433–441; quiz, 467. [PubMed] [Google Scholar]
- 34.Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop. 2007;131:74–81. doi: 10.1016/j.ajodo.2005.09.029. [DOI] [PubMed] [Google Scholar]