Abstract
Objective:
To evaluate the effect of dental crowding and lip protrusion on self-esteem and quality of life (QOL) in female orthodontic patients with Class I malocclusion.
Materials and Methods:
The study sample consisted of 201 patients (mean age 22.6 ± 3.0 years) who sought orthodontic treatment. All the patients were evaluated before treatment in terms of their degree of dental crowding and lip protrusion. Rosenberg's Self-Esteem Scale and the Orthognathic Quality of Life Questionnaire (OQLQ) were used to determine self-esteem and QOL and to evaluate whether these values were related to malocclusion severity.
Results:
The results indicated that severe crowding and severe protrusion can result in lower self-esteem and poorer QOL (P < .05) than mild crowding and protrusion in Class I malocclusion. In the oral function component of the OQLQ, the severity of protrusion did not have significant effect.
Conclusions:
In Class I malocclusion, patients with mild crowding or protrusion had significantly better self-esteem and QOL scores than severe crowding or protrusion patients.
Keywords: Self-esteem, Quality of life, Protrusion, Crowding
INTRODUCTION
Recently there has been increasing recognition of the effect of dentofacial problems on social and psychological well-being.1,2 This has resulted in a greater clinical focus on improving quality of life (QOL) and other psychological measures in cases of dental conditions that are not life threatening, and thus the psychological aspects of malocclusion and orthodontic treatment have become a popular topic in modern orthodontics.3,4
Malocclusion represents only one dimension of the complex nature of oral health. However, malocclusion can affect self-satisfaction, and as a result, impair psychological and social functioning.2 Evidence has suggested that malocclusion can be associated with self-esteem (SE)5 and QOL issues.6
There have been inconsistencies between the severity of malocclusion and the reported QOL or patients' perception of their occlusion.7 Patient concerns regarding malocclusion are frequently different from those of the orthodontist; patients typically have high levels of concern for noticeable problems such as dental crowding, overjet, or lip profile, but are tolerant of less noticeable malocclusion such as Class II or Class III molar relationship.8 In other words, many malocclusion patients consider esthetic impairment very important. Therefore, to evaluate the psychological impact of malocclusion, measures of impact need to be focused on esthetic problems.
The severity of esthetic impairment varies among orthodontic patients, and we can assume that the psychological impact of malocclusion can also vary among malocclusion patients. The objective of this study was to evaluate whether there is any difference in SE and QOL using Rosenberg's Self-Esteem Scale (RSE)9 and the Orthognathic Quality of Life Questionnaire (OQLQ)10 in crowding and protrusion patients with differing severity. I chose the OQLQ for QOL measurement because it focuses more on esthetic impairment than do other QOL measures such as the Oral Health Impact Profile (OHIP)11 and the Oral Health-Related Quality of Life (OHRQoL).12
MATERIALS AND METHODS
The study group was chosen among female orthodontic patients at the Department of Orthodontics, Seoul National University Dental Hospital, Korea. To be included in the study group, the patients had to satisfy all of the following criteria: (1) age between 18 and 30 years; (2) no craniofacial anomalies, including cleft lip and/or palate; (3) Class I molar relationship without spacing or noticeable facial asymmetry; (4) normal overbite and overjet (0 mm ≤ 4 mm); (5) no missing or impacted teeth except third molars; (6) no reported medical problem or temporomandibular joint pain; (7) no orthodontic treatment experience; (8) no untreated caries or periodontal disease. The patients were enrolled over an 18-month period.
Sample size was calculated with the data from a previous study13 using the Sample Size Determination Program Ver. 2.0.1 (Seoul National University Dental Hospital, Seoul, Korea) with α = 0.05 and a power of 90%. A sample size of 27 in each group was required to detect a significant difference.
Each patient signed a consent form and agreed to participate in the study. The Seoul National University Dental Hospital Institutional Review Board approved all the study procedures. After a brief explanation about the questionnaire, each participant completed the RSE and OQLQ during a clinical examination before orthodontic treatment.
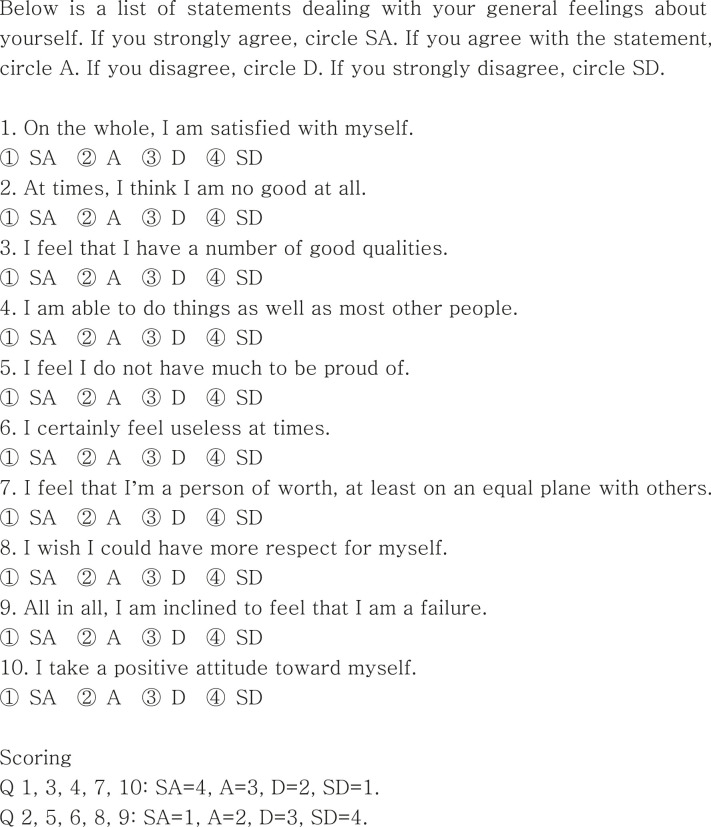
The RSE is a Likert scale in which a positive or a negative response is weighed with a four-point scale, ranging from “strongly agree” to “strongly disagree,” and consists of 10 questions (Figure 1). The RSE was between 10 and 40, and a higher RSE score indicates greater SE. This scale has been used for both the general population14 and orthodontic patients.5,15
Figure 1.
Rosenberg's Self-Esteem Scale (RSE).9
The OQLQ was originally developed to assess QOL in dentofacial deformity patients.10,16 It consists of 22 questions that measure four principal components (social aspects, facial esthetics, function, and awareness of facial deformity) using a four-point scale according to how much the issue covered by a particular statement bothers the respondent (Figure 2). OQLQ dimensions are scored so that lower scores indicate better QOL, and the scores range between 0 and 88. This scale has been used to evaluate orthognathic surgery patients in several countries.17,18
Figure 2.
Orthognathic Quality of Life Questionnaire (OQLQ).10
Figure 2.
Continued.
Protrusive lip profile and maxillary anterior crowding are easily noticeable features, and are common reasons for seeking orthodontic treatment.19,20 Thus, the psychological influences of these two conditions were evaluated in female orthodontic patients. The study sample was divided into four groups. If the sum of upper and lower lip protrusion to the E-line was 4 mm or more, and the irregularity index (II) of the maxillary anterior teeth was less than 5 mm, the subject was placed in the protrusion group (PG). If the exhibited score was higher than 8 mm on the II without lip protrusion, the subject was placed in the crowding group (CG). If the II was less than 5 mm and the sum of upper and lower lip protrusion was less than 4 mm, the subject was placed in the minor malocclusion group (MMG). Subjects who showed both maxillary anterior crowding and lip protrusion were classified as belonging to the crowding and protrusion group (CPG). Detailed group descriptions are given in Table 1.
Table 1.
Characteristics of Each Group
To assess test-retest reliability, 20 consecutively selected patients were asked to complete an identical questionnaire 3 to 4 weeks after the first questionnaire. This time interval was selected because these patients had not started treatment by the time of the second survey and it was long enough to expect that they would forget their previous answers.
All sets of cephalograms were traced at the same time by one investigator, and cephalometric values were calculated with the V-ceph Program (Cybermed, Seoul, Korea). Before data analysis, 15 randomly selected cephalograms were retraced and measured twice, 4 weeks apart, and the measurement error was calculated using Dahlberg's formula.21 The error ranged between 0.1 mm and 0.8 mm for linear measurements and between 0.1° and 0.9° for angular measurements.
Statistical analysis was conducted using SPSS (version 17.0, SPSS, Chicago, Ill). The results of the Shapiro-Wilk test confirmed that all the variables followed a normal distribution. The RSE and OQLQ measurements of each group were compared using 1-way ANOVA and Scheffe's multiple comparison. The level of significance for all tests was set at α = 0.05.
RESULTS
Sample Characteristics
A total of 2046 patients were screened. Among the 211 patients who met the inclusion criteria, 6 patients failed to complete the questionnaire and 4 of them declined to participate. Finally, 201 patients were included in the study. The mean age of these patients was 22.6 years, and there was no significant difference in age between the groups (Table 2).
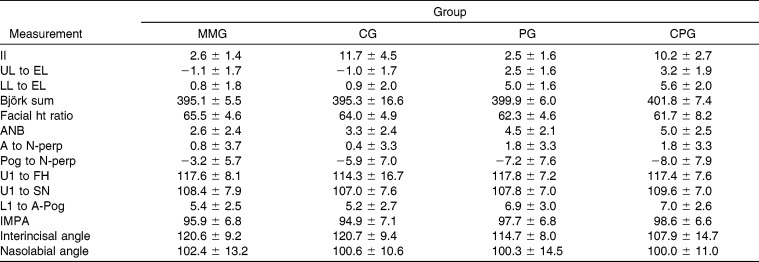
Table 2.
Comparison of Age in Each Groupa
There was no significant difference in the II between the MMG and PG, or between the CG and CPG (Table 3). While the amount of lip protrusion was greater in the PG and CPG than in the MMG and CG, maxillary incisor inclination was not significantly different in these groups. There was no significant difference in the distance, lip protrusion to the esthetic line, between the PG and CPG, as well as between the MMG and CG. Facial height ratio was smaller, ANB was greater, and the chin position was more retrusive in the PG and CPG than in the MMG. The CPG showed more of a vertical skeletal pattern than did the MMG or CG.
Table 3.
Mean and Standard Deviation in the Measurements of Each Group
Comparison of RSE and OQLQ Values
The test-retest analysis was performed by comparing the two sets of scores using the intraclass correlation analysis. Correlation coefficients of each principal component, RSE, and OQLQ are shown in Table 4. The intraclass correlation coefficient was between 0.863–0.974 and all the measurements were significantly correlated between the initial and retest questionnaire.
Table 4.
Reliability Test; Intraclass Correlation Coefficient (ICC) in Test-Retesta
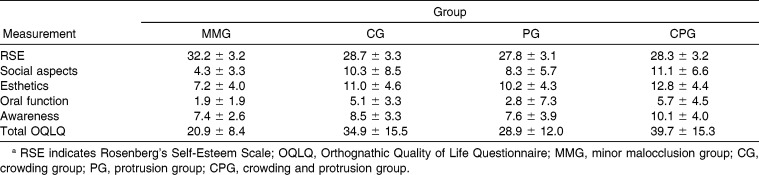
There was no significant difference in the level of self-esteem between the CG, PG, and CPG (Table 5); only the MMG exhibited higher RSE.
Table 5.
Mean and Standard Deviations of RSE and OQLQ of Each Groupa
The OQLQ score was lower (better QOL) in the MMG and higher in the CPG. Scores in social aspects were not significantly different between CG, PG, and CPG. In the esthetic component, the CPG showed a greater effect in QOL, while the MMG showed the lowest score. In the oral function component, the PG had a score similar to that of the MMG. On the other hand, the CG and CPG had higher scores than did the MMG or PG in the oral function component. In the awareness component, only the CPG exhibited a lower QOL.
DISCUSSION
Sample Selection
The smile has been reported to be the secondmost important facial characteristic associated with physical attractiveness,22 and previous research suggests that malocclusion might negatively affect self-satisfaction and impair social functioning.2,23 However, because there are many other factors that can influence psychological aspects, including characteristics of the hair, skin, eyes, body shape, and socioeconomic status, the psychological impact of a single factor can be limited. For that reason, only one-third of malocclusion patients having an Index of Orthodontic Treatment Need (IOTN) of grade 4 or 5 showed a significantly impacted QOL.24 I assumed that the severe and easily noticeable features of malocclusion would have significant psychosocial effect, and the results of this study supported my hypothesis.
The characteristics of malocclusion patients vary widely and, because of increased knowledge about orthodontic treatment and esthetic concerns, even some patients having a very mild malocclusion seek orthodontic treatment. In this study, we tried to evaluate the psychological impact of crowding and protrusion using mild and severe crowding or protrusion patients. Because malocclusion patients seeking orthodontic treatment may have lower QOL than those who do not,6 orthodontic patients rather than normal occlusion subjects were used as a control group.
Patients whose sum of upper and lower lip protrusion exceeded 4 mm were designated as the PG. This is because the average measurement of lip protrusion to Ricketts' E-line in Korean adult females is −0.86 ± 2.15 mm (upper) and 0.56 ± 2.30 mm (lower).25 Therefore, lip protrusion greater than 4 mm represents a value that is similar to or greater than one standard deviation.
The United States Public Health Service determined the standard of crowding as being greater than 6 on the II. Between the ages of 12 years and 17 years, 32.5% of adolescents demonstrated values of greater than 6.26 This percentage seems to be too high to evaluate the psychological influence of crowding. In this study, an II score greater than 8 of the maxillary arch was chosen as the standard for the CG and CPG. To observe the impact more clearly, we excluded patients with moderate crowding (II: 5 mm ≤ 8 mm). Most CG and CPG patients had a crossbite of the maxillary lateral incisors or a high canine, which are easily detected by a layperson.
Previous research showed sex-based differences on the RSE5,27 and the oral health–related QOL.6,28,29 There also can be differences based on the age of the study population.5,13,30 To minimize the influence of sex and age, only adult females under 30 years of age were included. In addition, Angle Class I malocclusion patients without noticeable asymmetry were used to minimize the influence of various skeletal malocclusions.
RSE and OQLQ Values
The RSE value of this study was similar to the result of the previous study on female university students.13 The OQLQ measurement of CPG was 39.7, similar to the OQLQ value of orthognathic surgery patients (37.63–42.53).17,31,32 Therefore, it can be assumed that severe crowding and protrusion have a great impact on QOL, as does a dentofacial deformity requiring orthognathic surgery.
The OQLQ score of the MMG (20.9) was similar to that of the nonsurgical control group of a previous study (21.37),32 which suggests that mild occlusal problems would have only a mild effect on QOL. Another interesting finding of this study was that in the PG, there was no significant impact on the “oral function” component. Such a result is reasonable, as the PG had only minor crowding; their major problem was lip protrusion. Previous studies showed that, in the jaw deformity patients without occlusal problem did not have significant impact in oral function component of OQLQ and OQLQ value of these patients (26.34) was similar to the value of PG in this study (27.8). Even in the patients without functional problems, malocclusion can influence the QOL to a certain degree by esthetic impairment.
The CG experienced slightly greater QOL impairment than did the PG, and the CPG showed the greatest impairment of QOL. Because the CG and CPG contend with not only the esthetic problems but amount of QOL impairment in CPG seems to be greater than that caused by the malocclusion without significant functional problems like MMG and PG.
The desire for esthetic improvement is an important motivating factor in seeking orthodontic treatment. Most oral health measures are difficult to apply in some orthodontic patients because many of their complaints are asymptomatic and esthetic in nature.33 For example, the OHIP questionnaire examines mainly “physical health”–related problems such as functional limitation, physical pain, and physical disability.11 Previous research using the OHIP reported that some of the questions did not show significant improvement by orthodontic treatment34 or significant difference between the orthodontically treated group and the untreated group.28 In our specialty, we need more condition-specific measures that focus on esthetic impairment.
In previous research on an adolescent population, protrusion was a less noticeable feature than anterior crowding, and the RSE was not lower in the protrusion group.5 My results indicated that in adult female orthodontic patients, both lip protrusion and anterior crowding led to a lower RSE and OQLQ. This was similar to the results found in a previous study using female Asian university students.13 The esthetic concerns of adult females seem to be greater than those of adolescent females. Among Asians, the percentage of patients whose chief complaint is lip fullness or protrusion is greater in adult patients than in adolescent patients.35
The OQLQ was originally developed to assess QOL in dentofacial deformity patients, but it is not necessary to limit its indication to surgical cases. Previous research has shown that patients with a prominent zygoma or square face—but no significant functional occlusal problem—who want to undergo zygomatic osteotomy or mandibular angle ostectomy do not have significant QOL impairment.17 As this study has shown, the OQLQ seems to be suitable for evaluating the psychological effects of malocclusion that causes esthetic problems. Future studies need to address differences in OQLQ of diverse malocclusions and changes in the OQLQ after orthodontic treatment.
CONCLUSION
In this psychological assessment of adult female orthodontic patients, I found that patients with severe anterior crowding and/or severely protrusive lip profile may have lower SE and QOL than those with minor crowding and/or protrusion.
REFERENCES
- 1.Fernandes MJ, Ruta DA, Ogden GR, Pitts NB, Ogston SA. Assessing oral health-related quality of life in general dental practice in Scotland: validation of the OHIP-14. Community Dent Oral Epidemiol. 2006;34:53–62. doi: 10.1111/j.1600-0528.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 2.de Oliveira CM, Sheiham A. The relationship between normative orthodontic treatment need and oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:426–436. doi: 10.1046/j.1600-0528.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 3.Shaw WC, Addy M, Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dent Oral Epidemiol. 1980;8:36–45. doi: 10.1111/j.1600-0528.1980.tb01252.x. [DOI] [PubMed] [Google Scholar]
- 4.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–27. doi: 10.1179/146531204225011364. discussion 15. [DOI] [PubMed] [Google Scholar]
- 5.Jung MH. Evaluation of the effects of malocclusion and orthodontic treatment on self-esteem in an adolescent population. Am J Orthod Dentofacial Orthop. 2010;138:160–166. doi: 10.1016/j.ajodo.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 6.Feu D, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JA. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–159. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Kok YV, Mageson P, Harradine NW, Sprod AJ. Comparing a quality of life measure and the Aesthetic Component of the Index of Orthodontic Treatment Need (IOTN) in assessing orthodontic treatment need and concern. J Orthod. 2004;31:312–318. doi: 10.1179/146531204225020625. discussion 300–311. [DOI] [PubMed] [Google Scholar]
- 8.Graber LW, Lucker GW. Dental esthetic self-evaluation and satisfaction. Am J Orthod. 1980;77:163–173. doi: 10.1016/0002-9416(80)90004-4. [DOI] [PubMed] [Google Scholar]
- 9.Rosenberg M. Society and the Adolescent SelfImage Rev ed. Middletown, Conn: Wesleyan University Press; 1989. pp. xxxii–347. [Google Scholar]
- 10.Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Community Dent Oral Epidemiol. 2000;28:195–201. doi: 10.1034/j.1600-0528.2000.280305.x. [DOI] [PubMed] [Google Scholar]
- 11.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 12.Kressin N, Spiro A, III, Bosse R, Garcia R, Kazis L. Assessing oral health-related quality of life: findings from the normative aging study. Med Care. 1996;34:416–427. doi: 10.1097/00005650-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Jung MH. Effects of malocclusion on the self-esteem of female university students. Korean J Orthod. 2008;38:388–396. [Google Scholar]
- 14.Tao FB, Xu ML, Kim SD, Sun Y, Su PY, Huang K. Physical activity might not be the protective factor for health risk behaviours and psychopathological symptoms in adolescents. J Paediatr Child Health. 2007;43:762–767. doi: 10.1111/j.1440-1754.2007.01217.x. [DOI] [PubMed] [Google Scholar]
- 15.Shaw WC, Richmond S, Kenealy PM, Kingdon A, Worthington H. A 20-year cohort study of health gain from orthodontic treatment: psychological outcome. Am J Orthod Dentofacial Orthop. 2007;132:146–157. doi: 10.1016/j.ajodo.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dent Oral Epidemiol. 2002;30:81–90. doi: 10.1034/j.1600-0528.2002.300201.x. [DOI] [PubMed] [Google Scholar]
- 17.Khadka A, Liu Y, Li J, et al. Changes in quality of life after orthognathic surgery: a comparison based on the involvement of the occlusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:719–725. doi: 10.1016/j.tripleo.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Al-Bitar ZB, Al-Omari IK, Al-Ahmad HT, El Maaytah MA, Cunningham SJ. A comparison of health-related quality of life between Jordanian and British orthognathic patients. Eur J Orthod. 2009;31:485–489. doi: 10.1093/ejo/cjp034. [DOI] [PubMed] [Google Scholar]
- 19.Dann CT, Phillips C, Broder HL, Tulloch JF. Self-concept, Class II malocclusion, and early treatment. Angle Orthod. 1995;65:411–416. doi: 10.1043/0003-3219(1995)065<0411:SCIMAE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Shaw WC, Meek SC, Jones DS. Nicknames, teasing, harassment and the salience of dental features among school children. Br J Orthod. 1980;7:75–80. doi: 10.1179/bjo.7.2.75. [DOI] [PubMed] [Google Scholar]
- 21.Dahlberg G. Statistical methods for medical and biological students. London: George Allen & Unwin; 1940. pp. 122–132. [Google Scholar]
- 22.Hassebrauck M. The visual process method: a new method to study physical attractiveness. Evol Hum Behav. 1998;19:111–123. [Google Scholar]
- 23.Klages U, Bruckner A, Guld Y, Zentner A. Dental esthetics, orthodontic treatment, and oral-health attitudes in young adults. Am J Orthod Dentofacial Orthop. 2005;128:442–449. doi: 10.1016/j.ajodo.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 24.Gherunpong S, Tsakos G, Sheiham A. A socio-dental approach to assessing children's orthodontic needs. Eur J Orthod. 2006;28:393–399. doi: 10.1093/ejo/cji114. [DOI] [PubMed] [Google Scholar]
- 25.Malocclusion Research Committee of Korean Association of Orthodontists. Korean Norm of Lateral Cephalometric Radiograph. Seoul: Korean Association of Orthodontists; 1997. [Google Scholar]
- 26.Kelly JE, Harvey CR. An assessment of the occlusion of the teeth of youths 12–17 years. Vital Health Stat 11. 1977:1–65. [PubMed] [Google Scholar]
- 27.Onyeaso CO. An assessment of relationship between self-esteem, orthodontic concern, and Dental Aesthetic Index (DAI) scores among secondary school students in Ibadan, Nigeria. Int Dent J. 2003;53:79–84. doi: 10.1111/j.1875-595x.2003.tb00663.x. [DOI] [PubMed] [Google Scholar]
- 28.Palomares NB, Celeste RK, Oliveira BH, Miguel JA. How does orthodontic treatment affect young adults' oral health-related quality of life. Am J Orthod Dentofacial Orthop. 2012;141:751–758. doi: 10.1016/j.ajodo.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 29.Esperao PT, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JA. Oral health-related quality of life in orthognathic surgery patients. Am J Orthod Dentofacial Orthop. 2010;137:790–795. doi: 10.1016/j.ajodo.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 30.Marshman Z, Robinson PG. Child and adolescent oral health-related quality of life. Semin Orthod. 2007;13:88–95. [Google Scholar]
- 31.Lee S, McGrath C, Samman N. Impact of orthognathic surgery on quality of life. J Oral Maxillofac Surg. 2008;66:1194–1199. doi: 10.1016/j.joms.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 32.Lee S, McGrath C, Samman N. Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int J Oral Maxillofac Surg. 2007;36:488–492. doi: 10.1016/j.ijom.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien K, Kay L, Fox D, Mandall N. Assessing oral health outcomes for orthodontics—measuring health status and quality of life. Community Dent Health. 1998;15:22–26. [PubMed] [Google Scholar]
- 34.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–898. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Im DH, Kim TW, Nahm DS, Chang YI. Current trends in orthodontic patients in Seoul National University Dental Hospital. Korean J Orthod. 2003;33:63–72. [Google Scholar]