Abstract
Objective:
To determine if interproximal reduction of teeth (IPR) is perceived differently by orthodontists and general dentists.
Materials and Methods:
A Web-based survey containing statements about IPR was developed and randomly distributed to orthodontists and general dentists.
Results:
The majority of orthodontists and general dentists strongly agreed that IPR is a minimally invasive procedure that poses little risk for the development of interproximal decay. However, general dentists were more likely to perform post-IPR polishing and to apply topical fluoride than are orthodontists (P < .0001). A greater percentage of orthodontists strongly believed that the esthetic and occlusal benefits of IPR outweigh the potential risk of tooth decay when IPR was performed (P < .0001). A greater percentage of general dentists were hesitant to perform IPR, despite research supporting that IPR has little negative effect on the health of teeth.
Conclusions:
The results of this study disproved the null hypothesis that orthodontists and general dentists share similar views regarding the use of IPR during orthodontic treatment. General dentists were more conservative in their views of IPR and were less comfortable with performing IPR as a routine procedure. General dentists felt more strongly about the importance of post-IPR polishing and application of topical fluoride. Orthodontists were more likely to have researched the long-term effects of IPR on the health of teeth and therefore felt more comfortable performing IPR during orthodontic treatment.
Keywords: Interproximal reduction, Perception, Orthodontists, Dentists
INTRODUCTION
Interproximal reduction (IPR) of enamel involves the removal of outer enamel (0.3–0.5 mm) on the interproximal surfaces of teeth.1 IPR is one of the techniques that may be used during orthodontic treatment to provide extra intra-arch space in patients with mild to moderate crowding and when extraction therapy is undesirable.2,3 Other advantages of IPR include decreased treatment time1 and prevention of interdental gingival retraction.4 The procedure can be performed using several methods: (1) air rotor stripping with fine tungsten-carbide or diamond burs, (2) the use of diamond-coated stripping disks, or (3) the use of hand-held or motor-driven abrasive strips.1,5–7
Widespread acceptance of IPR has been hindered by the overarching notion that abraded enamel may be more susceptible to caries formation, despite the lack of evidence demonstrating an increased risk of caries on reduced teeth.1 In a clinical study that involved IPR followed by polishing, Zachrisson et al.8 concluded that IPR does not negatively affect the health of the reduced teeth. Jarjoura et al.9 supported this conclusion and demonstrated that the application of fluoride after IPR provided little additional benefit to the patient. Undoubtedly, improper IPR techniques could result in a rough enamel surface, which could increase plaque accumulation10 and consequently lead to an increased risk of developing caries. However, as long as IPR is properly performed on tooth surfaces with sufficient enamel thickness,11 it can result in many potential benefits for the patient and clinician, including relief of mild-moderate crowding2,3 and shortening of treatment time.1
As researchers continue to study the long-term effects of IPR, the perception of IPR varies among clinicians. General dentists may be more conservative than orthodontists in their use of IPR since preservation of healthy tooth structure is an important principle in cavity preparations.12 Conversely, orthodontists may be more proactive in performing IPR as a result of the multiple studies failing to demonstrate significant risks on the long-term health of the reduced teeth.8,9 None of the previous IPR studies have compared the perception of IPR between orthodontists and general dentists. The aim of this study was to test the null hypothesis that orthodontists and general dentists share similar perceptions regarding the interproximal reduction of permanent teeth to gain space during orthodontic therapy.
MATERIALS AND METHODS
Approval to conduct this study was obtained from the Institutional Review Board of the Virginia Commonwealth University. A Web-based survey was developed for orthodontists and general dentists to respond to statements about the perceived advantages and disadvantages of IPR of permanent teeth.
The initial series of statements to which invited participants were asked to respond focused on the circumstances for performing IPR and whether clinicians preferred to use alternatives to IPR. The second part of the survey contained statements regarding IPR protocol to determine if there was a preference to follow IPR with polishing and topical fluoride application. The last section of the survey assessed clinicians' subjective opinions regarding IPR. Demographic information was collected at the end of the survey.
The American Association of Orthodontists delivered the Web-based survey electronically to all members across the United States. The data were collected over the course of 8 weeks from July 2012 to September 2012 using REDCap electronic data capture tools hosted at the Virginia Commonwealth University.13 REDCap (Research Electronic Data Capture) is a secure, Web-based application designed to support data capture for research studies. The Virginia Dental Association, Maryland State Dental Association, and South Carolina Dental Association agreed to participate and subsequently placed the REDCap online survey link in a monthly electronic newsletter that was sent to their members during the same period of time.
Groups were compared initially using analysis of variance (ANOVA) or chi-square test, as appropriate. Comparisons among items were done using repeated-measures, mixed-model ANOVA. Relationships among items were summarized using Pearson's correlation. All analyses were accomplished using SAS software (JMP version 10, SAS Institute Inc, Cary, NC). Statistical significance was set at α < .05.
RESULTS
A total of 132 general dentists and 873 orthodontists responded to the survey. Table 1 shows that both groups had similar gender and race characteristics (approximately 80% were males and 90% white) but that they differed in age (P < .0001). Responding orthodontists were generally younger than general dentists, with a mean of 48.2 vs 53.2 years of age.
Table 1.
Demographic Characteristics
Responses related to clinicians' use of IPR are summarized in Table 2. More orthodontists (66%) reported performing IPR on a routine basis to gain intra-arch space, compared to 46% of general dentists (P < .0001). Nearly half (49.8%) of the orthodontists reported a preference for performing IPR on anterior teeth over posterior teeth, while general dentists had no preference (P = .0021). Both orthodontists and general dentists agreed that performing IPR was better than leaving incisors flared (P = .118).
Table 2.
Use of Interproximal Reduction of Teeth (IPR)
Responses related to practitioners' protocols for implementing IPR are summarized in Table 3. The majority of orthodontists and general dentists agreed that IPR was a minimally invasive procedure that posed little risk for the development of interproximal caries, but a greater percentage of general dentists than orthodontists reported applying topical fluoride (37.9% vs 11.5%, P < .0001) and polishing the reduced tooth surfaces (78.1% vs 45.7%, P < .0001) after IPR (Figures 1 and 2).
Table 3.
Interproximal Reduction of Teeth (IPR) Protocol and Personal Opinions of IPRa
Figure 1.
Opinions of orthodontists and general dentists on polishing teeth post-IPR.
Figure 2.
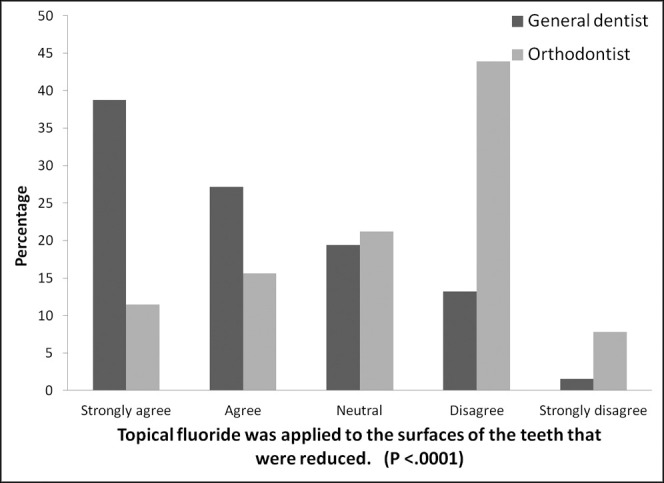
Opinions of orthodontists and general dentists on applying topical fluoride post-IPR.
Responses related to practitioners' personal opinions regarding IPR are also summarized in Table 3. Orthodontists more strongly supported the esthetic and occlusal benefits of IPR and agreed that the benefits outweigh the potential risk of tooth decay (P < .0001).The majority of orthodontists (92.1%) and general dentists (75%) were willing to have IPR performed on their own teeth, but 45.9% of orthodontists expressed the strongest level of willingness, compared to 19.7% of general dentists. A greater percentage of general dentists (16.7% vs 3.4%) were unwilling to have IPR altogether (P < .0001). The large majority of orthodontists (80%) reported having researched the effects of IPR on the health of teeth, compared to only 33% of general dentists (P < .0001). While the majority of orthodontists (89.4%) and general dentists (65.9%) reported being comfortable with performing IPR on patients, more orthodontists reported a stronger level of comfort (44.7% vs 19.7%, P < .0001). Lastly, the majority of clinicians denied being hesitant to perform IPR, but a greater percentage of general dentists reported hesitation (25% vs 7%, P < .0001).
DISCUSSION
IPR is a common procedure in orthodontics, employed to alleviate various problems, such as crowding, increased incisor flare, and tooth size discrepancies. In this study, the majority of both general dentists and orthodontists reported routinely performing IPR to gain intra-arch space. Because the survey was not limited to only general dentists who perform orthodontic treatment, it was surprising to learn that 46% of the general dentists reported routinely performing IPR. This could be a reflection of an increasing percentage of general dentists integrating simple orthodontic treatment into their practice, namely through clear aligner systems.
Previous studies have shown that IPR can create deep surface irregularities that cannot be removed by polishing alone.14,15 Some clinicians believe the resulting enamel roughness can promote plaque accumulation and, further, lead to an increased risk of developing interproximal caries, gingival inflammation, gingival recession, and increased sensitivity to hot and cold temperatures.16 Despite these risks, this study showed that both general dentists and orthodontists prefer performing IPR over leaving incisors flared. However, the decision to perform IPR rather than flaring incisors or extracting premolars depends on multiple factors and varies among patients. The statements utilized in this study's survey did not relate the use of IPR to specific clinical scenarios, but rather they were intentionally phrased in such a way that general perceptions regarding IPR could be captured.
The results showed that general dentists were more likely than orthodontists to perform post-IPR polishing and topical fluoride application. This implies that general dentists are more likely to perceive an increased risk of caries development in areas where IPR has been performed if such a post-IPR protocol is not followed. Despite differences in post-IPR protocol, the majority of both general dentists and orthodontists agreed IPR was a minimally invasive procedure.
A greater percentage of orthodontists agreed that IPR poses little risk for the development of interproximal caries and, further, agreed that the esthetic and occlusal benefits of IPR outweigh the potential risk of tooth decay when IPR is performed. A greater percentage of orthodontists were also more willing to have IPR performed on their own teeth than were general dentists. It is possible that general dentists are less comfortable with the idea of performing IPR routinely because of a lack of familiarity with IPR, or their reluctance may stem from a basic tendency to adhere to the modern general dental principle to preserve healthy tooth structure.17
The results of this study showed that more orthodontists than general dentists have researched the long-term effects of IPR. This may be because the majority of IPR studies have been published in the orthodontic rather than the dental literature. General dentists may be more hesitant to perform IPR because they are unaware of the studies that have failed to show that interproximally reduced teeth have higher caries rates.
The type of method used to perform IPR may also have an influence on a practitioner's decision to polish or to apply topical fluoride post–enamel reduction. Only one study has compared various methods of IPR and their effect on the enamel surface.18 This study reported an increase in enamel roughness postreduction and recommended polishing following IPR. However, it did not explore the relationship between enamel roughness and an increased risk for interproximal caries. To the best of our knowledge, no study has investigated the influence of the different methods used for IPR on the potential increase in caries risk. Our study also showed that orthodontists are less likely than general dentists to apply fluoride after performing IPR. This may be because separate studies have concluded that topical fluoride application on an abraded enamel surface has limited beneficial value in preventing caries formation in patients exposed to other sources of fluoride, such as fluoridated water and toothpaste.9 Therefore, because the majority of orthodontists reported having researched the long-term effects of IPR on the health of teeth, it is no surprise that orthodontists were less likely to have applied topical fluoride post-IPR. A future study could be performed to investigate the differences in views between general dentists that perform IPR and those that do not.
CONCLUSIONS
Orthodontists and general dentists agree that IPR is a minimally invasive procedure.
General dentists are more conservative in their views of IPR and are less comfortable with IPR as a routine procedure.
General dentists feel more strongly about post-IPR polishing and topical fluoride application.
A greater percentage of orthodontists have researched the long-term effects of IPR on the health of teeth.
ACKNOWLEDGMENTS
This study was supported in part by the AD Williams Summer Research Fellowship Program of the Virginia Commonwealth University and by the Virginia Orthodontic Education and Research Foundation.
REFERENCES
- 1.Zachrisson BU, Minster L, Ogaard B, Birkhed D. Dental health assessed after interproximal enamel reduction: caries risk in posterior teeth. Am J Orthod Dentofacial Orthop. 2011;139:90–98. doi: 10.1016/j.ajodo.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Sheridan JJ. Guidelines for contemporary air-rotor stripping. J Clin Orthod. 2007;41:315–320. [PubMed] [Google Scholar]
- 3.Sheridan JJ. The physiologic rationale for air-rotor stripping. J Clin Orthod. 1997;31:609–612. [PubMed] [Google Scholar]
- 4.Zachrisson BU. Interdental papilla reconstruction in adult orthodontics. World J Orthod. 2004;5:67–73. [PubMed] [Google Scholar]
- 5.Zachrisson BU. Stripping. In: Rakosi T, Graber TM, editors. Orthodontic and Dentofacial Orthopedic Treatment. Stuttgart, Germany: Thieme; 2010. pp. 289–312. [Google Scholar]
- 6.Arman A, Cehreli SB, Ozel E, Arhun N, Cetinsahin A, Soyman M. Qualitative and quantitative evaluation of enamel after various stripping methods. Am J Orthod Dentofacial Orthop. 2006;130:131:e7–131.e14. doi: 10.1016/j.ajodo.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Keim RG, Gottlieb EL, Nelson AH, Vogels DS. 2008 JCO study of orthodontic diagnosis and treatment procedures. J Clin Orthod. 2008;42:625–640. [PubMed] [Google Scholar]
- 8.Zachrisson BU, Nyoygaard L, Mobarak K. Dental health assessed more than 10 years after interproximal enamel reduction of mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2007;131:162–169. doi: 10.1016/j.ajodo.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Jarjoura K, Gagnon G, Neiberg L. Caries risk after interproximal reduction. Am J Orthod Dentofacial Orthop. 2006;130:26–30. doi: 10.1016/j.ajodo.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 10.Radlanski RJ, Jager A, Schwestka R, Bertzbach F. Plaque accumulations caused by interdental stripping. Am J Orthod Dentofacial Orthop. 1989;95:27. doi: 10.1016/0889-5406(88)90131-x. [DOI] [PubMed] [Google Scholar]
- 11.Hall NE, Lindauer SJ, Tufekci E, Shroff B. Predictors of variation in mandibular incisor enamel thickness. J Am Dent Assoc. 2007;138:809–815. doi: 10.14219/jada.archive.2007.0270. [DOI] [PubMed] [Google Scholar]
- 12.Dennison JB, Hamilton JC. Treatment decisions and conservation of tooth structure. Dent Clin North Am. 2005;49:825–845, vii. doi: 10.1016/j.cden.2005.05.007. [Review] [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joseph VP, Rossouw PE, Basson NJ. Orthodontic microabrasive reproximation. Am J Orthod Dentofacial Orthop. 1992;102:351–359. doi: 10.1016/0889-5406(92)70051-B. [DOI] [PubMed] [Google Scholar]
- 15.Lundgren T, Milleding P, Mohlin B, Nannmark U. Restitution of enamel after interdental stripping. Swed Dent J. 1993;17:217–224. [PubMed] [Google Scholar]
- 16.Zachrisson BU. Actual damage to teeth and periodontal tissues with mesiodistal enamel reduction (“stripping”) World J Orthod. 2003;5:178–183. [PubMed] [Google Scholar]
- 17.White JM, Eakle WS. Rationale and treatment approach in minimally invasive dentistry. J Am Dent Assoc. 2000;131(suppl):13S–19S. doi: 10.14219/jada.archive.2000.0394. [Review] [DOI] [PubMed] [Google Scholar]
- 18.Danesh G, Hellak A, Lippold C, Ziebura T, Schafer E. Enamel surfaces following interproximal reduction with different methods. Angle Orthod. 2007;77:1004–1010. doi: 10.2319/041806-165.1. [DOI] [PubMed] [Google Scholar]