Abstract
Objective:
To evaluate the changes in soft tissue around the lips after orthodontic bracket debonding using three-dimensional (3-D) stereophotogrammetry.
Materials and Methods:
3-D facial images of 20 subjects (10 men and 10 women; mean age, 26.81 ± 7.23 years) were taken with a white light scanner before and after debonding the labial brackets. Two images acquired from each subject were superimposed, and 15 soft tissue landmarks around the lips were plotted and analyzed. Statistical analysis was performed using both paired and independent t-tests (P < .05).
Results:
There were no significant changes in position of any landmark on the x (left-right)- or y (vertical)-axes after removal of the brackets. However, the landmarks in the oral commissures and lower lip (LLP, −0.55 mm; Li, −0.44 mm; Ch-L, −0.56 mm, all P < .05) on the z (anteroposterior)-axis showed statistically significant differences. There were no significant positional changes of most landmarks on the x-, y-, or z- axes after bracket removal among the various genders and lip thicknesses.
Conclusions:
There was a slight retrusion in the oral commissure and lower lip areas after debonding, but no changes were found in the upper lip area. This study showed that 3-D stereophotogrammetry can be useful in evaluating facial soft tissue changes in orthodontic patients.
Keywords: 3-D stereophotogrammetry, White light scanner, Debonding, Soft tissue changes
INTRODUCTION
Orthodontic treatment seeks to restore not only occlusal function but also esthetics by improving facial harmony.1 To achieve this, treatment based on proper orthodontic diagnosis and planning is necessary. Considering the growing interest in facial esthetics and patients' awareness of even slight lip changes at the end of treatment, there is a need to anticipate changes in the lip and perioral soft tissues after bracket removal.
Research on the influence of orthodontic appliances on changes around the lips has been limited to assessing the soft tissues of the midsagittal area using two-dimensional (2-D) cephalograms or photographs.2,3 Recently, different methods of evaluating 3-D soft tissue changes such as 3-D cone-beam computed tomography (CBCT), laser scanning, and stereophotogrammetry have been reported with the development of digital technology.4–9 3-D CBCT can create high quality images of soft tissue but is unpleasant for the patient to be repeatedly subjected to radiation exposure, noise generated on the skin of the cone beam's boundary, and long scan time.4 On the other hand, 3-D laser scanning does not discharge radiation, and it can reproduce the detailed color and texture of soft tissue with a relatively short scan time. However, laser scanning still has limitations because it needs to be processed with the patient's eyes closed, and it cannot perfectly represent the texture and color of the scanned skin.6 Hence, 3-D stereophotogrammetry, which photographs an object using white light–scanning equipment at various angles with one or more cameras and composes a 3-D photograph with computer software, was developed. Its advantages, such as repetitive exposures with the eyes open and excellent reproducibility, reliability, and representation of soft tissue texture and color, have been proven.5,7,10,11
Most of the studies using 3-D facial imaging technologies in orthodontics have dealt with the changes achieved by orthognathic surgery6,8,9 and various types of orthodontic treatment.12,13 However, there have been only a few 3-D photographic studies on soft tissue changes around the lips by orthodontic appliances5 after debonding. Therefore, the purpose of this study was to evaluate the changes in soft tissues around the lips after removing brackets using 3-D light stereophotogrammetry.
MATERIALS AND METHODS
Twenty subjects (10 men and 10 women; mean age, 26.81 ± 7.23 years) were recruited from the patient population in the Department of Orthodontics at Seoul National University Bundang Hospital (Seongnam, Korea). The patients completed their orthodontic treatment with Class I molar and canine relationships and were willing to participate in the study. We used the following inclusion criteria: (1) lip competence, (2) facial symmetry, (3) no craniofacial syndromes, and (4) adult. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1312-230-101).
Imaging Methods (Acquisition and Registration)
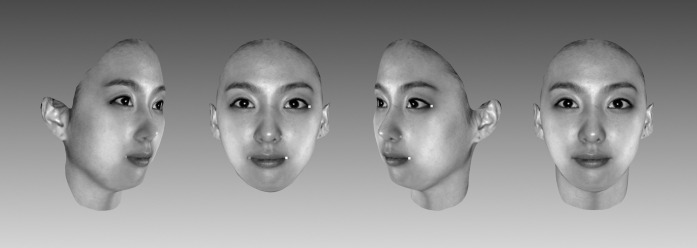
A 3-D optical scanning system (Morpheus 3-D; Morpheus Co, Gyeonggi, Korea) with computer software (Facemaker; Morpheus) was used to capture 3-D facial photographs of the patients. This system utilizes light-emitting diodes as a source of white light. Two images were acquired: before and after removal of the brackets in all patients. For every photo session, three photographs were taken, from (1) the front, (2) 45° to the left, and (3) 45° to the right. The patients' forehead, ears, and neck were exposed; patients were asked to keep the teeth in occlusion after swallowing in the natural head position and to relax their facial muscles with eyes open during the scan.10 All photos were taken under the same conditions to minimize effects from variables such as lighting, makeup, and facial expression. In addition, the collection and analysis of data were done by an experienced investigator. Labial self-ligating brackets (Damon Clear brackets in the maxillary arch and Damon Q brackets in the mandibular arch; Ormco, Glendora, Calif) were used. Maxillary (mandibular) incisor brackets had 0.105-inch (0.081-inch) thickness, 0.156-inch (0.123-inch) height, and 0.138-inch (0.110-inch) width.
As shown in Figure 1, three photographs were registered using Facemaker software. Registration is a process of converting data obtained from various points of time into a single coordinate system using iterative closest point (ICP) algorithms.14 These algorithms repeat the process to determine a pair of points closest to the predefined, overlapped area between the inputted two data and calculate the 3-D conversion parameter that minimizes the distance between the points.
Figure 1.
The process of three-dimensional photograph taking and registration.
Superimposition
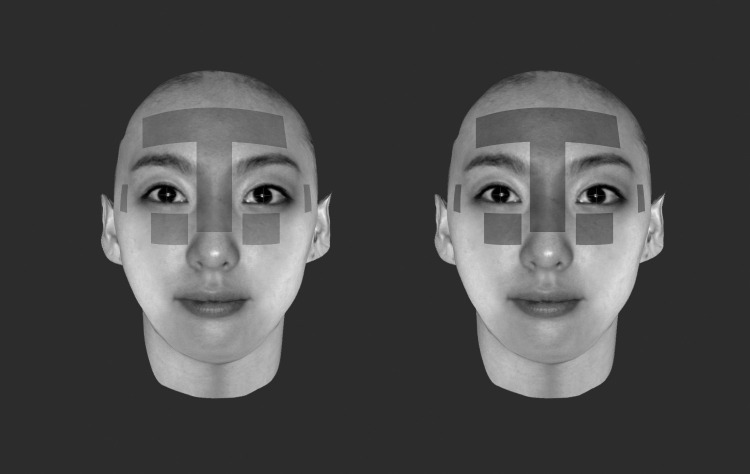
On two 3-D images acquired before and after debonding in each patient, locations of left and right pupil and nose tip points were automatically determined. The left and right forehead, bridge of the nose, temples, and area below the eyes were detected automatically based on the locations of pupil and nasal tip points (Figure 2). For each point cloud within the facial area, ICP algorithms were applied. Based on the result, the conversion value of movement and rotation that minimizes the average distance of point clouds is calculated and overlapped automatically and subsequently revised with a manual correction.14
Figure 2.
Superimposition of photographs taken before and after removal of orthodontic brackets. The locations of pupil and nose tip points, left and right foreheads, bridge of the nose, temple, and area below the eyes are auto-detected.
3-D Coordinate System Setting
The segment connecting the left and right pupil points becomes the x (left-right)-axis. The plane consisting of perpendicular bisectors that pass through the center of the segment connecting the left and right pupil points (midinterpupil point) becomes the yz plane. The z-axis is defined as the anteroposterior axis of the face on the yz plane. The y (vertical)-axis is the superoinferior axis of the face on the yz plane. The imaginary center point of 3-D facial geometry on the bases of the y- and z-axes on the yz plane becomes the zero points (0, 0, and 0). The xz plane is set perpendicular to the yz plane, passing through the zero points. The xy plane is the plane perpendicular to the yz and xz planes, passing through the zero points (Figure 3). The 3-D coordinate values (x, y, and z) of the landmarks were acquired using the coordinate system of the imaginary center of facial geometry.
Figure 3.
Soft tissue landmarks and three-dimensional coordinate system: x-axis (left-right axis; left [+], right [−]), y-axis (vertical axis; superior [+], inferior [−]), and z-axis (anteroposterior axis; anterior [+], posterior [−]).
Landmark Identification
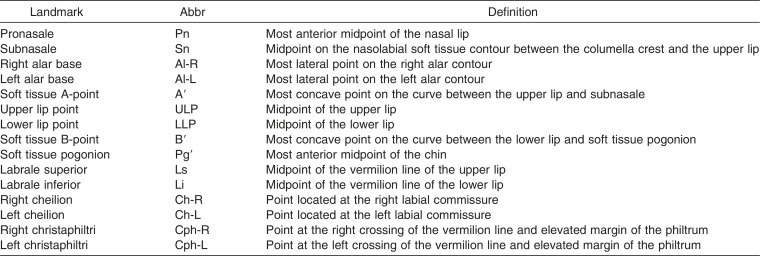
The landmarks of the 3-D image generated by Facemaker are identified using Morpheus 3-D computer software. Fifteen landmarks are plotted with the autodetection function, but can be easily adjusted manually (Table 1, Figure 3).
Table 1.
Definitions of 15 Facial Soft Tissue Landmarks for 3-D Photography
Statistical Analysis
The paired t-test was used to evaluate changes in the x, y, and z coordinate values in 15 perioral soft tissue landmarks between the two images taken before and after bracket removal. In addition, an independent t-test was used to compare changes in the 3-D coordinate values between each soft tissue landmark before and after debonding in different genders and lip thicknesses. Lip thickness, which is the distance between the incisal tip of the maxillary (mandibular) incisor and the most anterior point of the upper (lower) lip, was measured on the pretreatment lateral cephalograms. Statistical analysis was performed with SPSS 20.0 for Windows (PASW, Chicago, Ill). Differences were considered significant at a P-value less than .05.
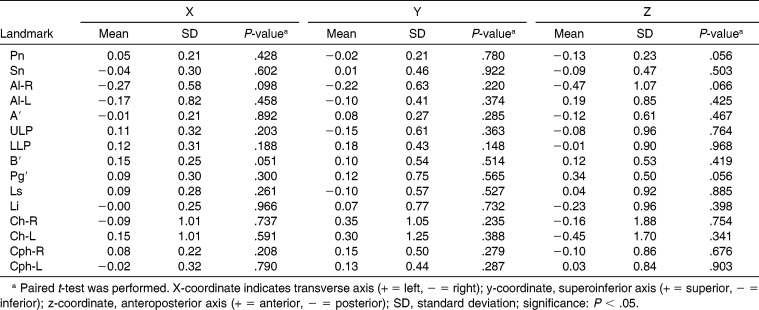
For the reproducibility of images taken by 3-D stereophotogrammetry, we confirmed that there were no significant differences in the x-, y-, or z-coordinate values of any landmark between the two repeated images taken at 2-week intervals before debonding in 15 randomly selected patients (P > .05) (Table 2).
Table 2.
Mean Differences in 3-D Coordinates Between Each Landmark of 2 Images Acquired at 2-Week Intervals Before Debonding
RESULTS
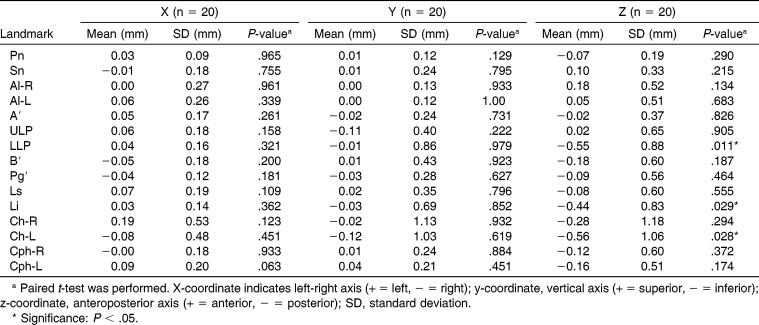
As presented in Table 3, no significant difference was found in the position of any landmark on the x- or y-axes after bracket removal. However, LLP, Li, and Ch-L (−0.55 mm; −0.44 mm; −0.56 mm, respectively, all P < .05) on the z-axis showed statistically significant differences.
Table 3.
Mean Differences in 3-D Coordinates Between Each Landmark of Two Images Before and After Removal of Brackets
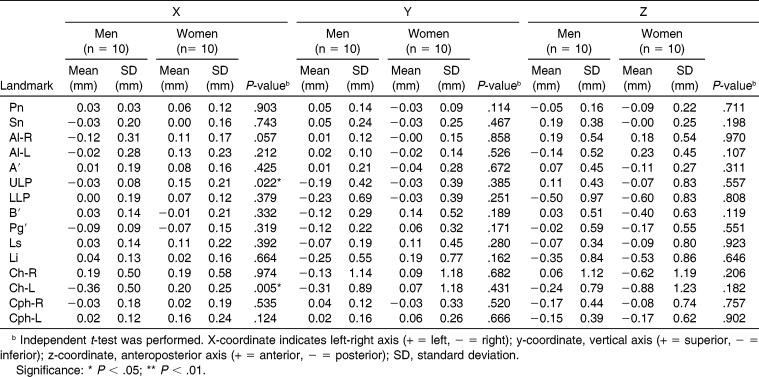
There were significant positional differences in ULP (male, −0.03 mm; female, 0.15 mm, P < .05) and Ch-L (male, −0.36 mm; female, 0.20 mm, P < .01) on the x-axis between the two genders (Table 4).
Table 4.
Mean Differences in 3-D Coordinates Between Each Landmark of Two Images Before and After Removal of Brackets in the Two Genders
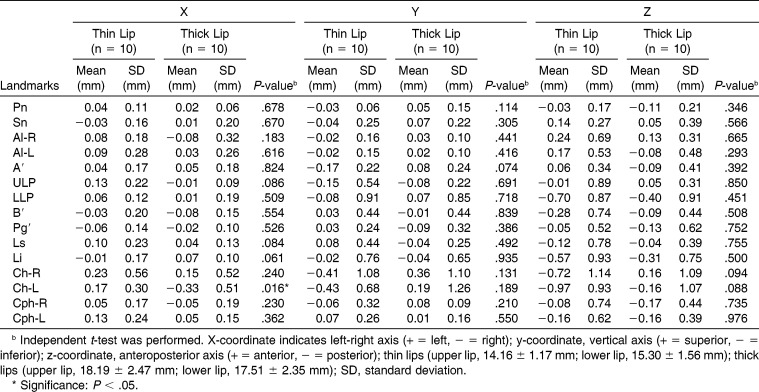
In addition, Ch-L (thin lips, 0.17 mm; thick lips, −0.33 mm; P < .05) on the x-axis showed a significant difference after bracket removal of those having different lip thicknesses (Table 5).
Table 5.
Mean Differences in 3-D Coordinates Between Each Landmark of Two Images Before and After Removal of Brackets in Different Lip Thicknesses
DISCUSSION
With increasing patient demands on the esthetic lip line and facial profile, there has been a need to anticipate the change in soft tissues around the lips after removal of orthodontic brackets. 2-D images have been used to evaluate changes in the facial soft tissue despite its limitations in assessing the parasagittal area. Recently, various methods have been applied to examine soft tissues in 3-D; the most representative method among them is 3-D scanning techniques such as laser scanning and 3-D stereophotogrammetry.4–6 Some researchers have reported that soft tissue analysis using 3-D scanning is reproducible and reliable.7,10,11,15 Similarly, our study has demonstrated that the mean differences in 3-D coordinate values (x, y, and z) of each landmark between two photographs repeated at baseline and after 2 weeks were less than 0.5 mm and that the reproducibility of soft tissue landmarks was high (P > .05; Table 2).7,10 Therefore, soft tissue analysis using 3-D stereophotogrammetry in the field of orthodontics or orthognathic surgery can be an effective method for evaluating and anticipating soft tissue changes without exposure to harmful radiation.
This study used 3-D photographs to examine the changes in soft tissue around the lips after removal of the labial brackets. The coordinate values of each landmark presented no positional changes on either the x- or y-axes. Only LLP, Li, and Ch-L showed significant changes in a posterior direction on the z-axis (−0.55 mm, −0.44 mm, −0.56 mm, respectively; all P < .05; Table 3). These findings suggest that bracket removal may have retrusive effects on the oral commissure and lower lip, but not on the upper lip. Consistent with this study, Eidson et al.5 reported that right and left cheilions and lower lip were significantly retruded (mean range, 0.26 mm to 0.89 mm) immediately after bracket removal. Jeon et al.,16 using 3-D laser scanning, demonstrated that relatively large changes in the perioral soft tissue were recorded immediately after debonding; approximately 1.3 mm (median) in the oral commissures and more than 1 mm in the vermilion border of the upper and lower lips. On 2-D lateral cephalograms, Lee et al.2 reported that the lower lip was significantly retruded immediately after debonding and that the mean retrusion in the lower lip (0.88 mm) was greater than that in the upper lip (0.38 mm). On the contrary, Abed et al.3 reported that there were no statistically significant differences in lip positions after bracket debonding based on 2- D lateral photographs.
Within different genders, there were no significant positional changes in most of perioral landmarks on the x-, y-, or z-axes after bracket removal, with the exception of ULP (P < .05) and Ch-L (P < .01) on the x-axis (Table 4). This indicates that there were no differences in the anteroposterior or vertical positions of the upper or lower lips before or after debonding in the two sexes. Jeon et al.16 reported that males showed more retrusion in the lower lip immediately after debonding. In contrast, Lee et al.2 reported that lip retrusion was greater in females. These differences in lip changes between male and female may be attributed to various factors such as different sample sizes and methods of evaluating soft tissues.
In the present study, most perioral landmarks on the x-, y-, and z-axes before and after bracket removal showed no significant positional changes between lip thicknesses except for Ch-L (P < .05) on the x-axis (Table 5). This corroborates that lip thickness has no prominent effect on left-right, anteroposterior, or vertical lip changes after debonding. However, Jeon et al.16 reported that patients with thinner lips showed more retrusive change immediately after debonding. Additionally, in profile changes associated with orthodontic incisor retraction, Oliver17 and Kokodynski et al.18 reported that greater lip thickness results in less change in the superior labial sulcus. The discrepancy in lip changes among studies may have resulted from the demographic feature of subjects. Because the variation in lip thickness of subjects in this study might have been less than that of subjects from a racially diverse population, lip thickness may have less to do with lip changes after debonding.
Although the amount of change in facial soft tissue after removing or bonding orthodontic brackets differed, most studies showed that changes in the lower lip were more prominent than those in the upper lip.5,16,19 This may be due to low predictability of the upper lip response related to orthodontic treatment, or it may be related to the complex anatomical structure and dynamics of the lip.16,20,21 In addition, Moseling et al.22 reported that the inherent properties and morphology of the soft tissues are the greatest determinants of lip curvature in orthodontic patients.
In the present study, considering that the retrusion in oral commissures and lower lip after removing orthodontic brackets occurred below the level of clinical significance,5 additional treatment may be needed to correct lip posture in cases of lip protrusion remaining before bracket debonding. It is important for clinicians to understand the existence of individual variations of lip retrusion after debonding and the difference in patients' awareness of lip protrusion. Additionally, clinicians should recognize that lip thickness increases during growth and development.23
Although the 3-D stereophotogrammetry used in this study is an effective method of analyzing soft tissue, its reproducibility may diminish due to changes in lip position not recognized by the operator.5 These changes are most likely to be affected by muscle tension and elasticity of the soft tissue around the lips as well as the patient's gender and age.15,24,25 The accuracy between 3-D stereophotogrammetry and laser scanning for soft tissue analysis should also be evaluated. Considering that this study was performed on a small sample, further studies of larger homogeneous samples are needed. Moreover, positional changes of the lip should be examined in terms of different skeletal patterns, the aging process after orthodontic treatment, and differences in lip thickness among diverse races.
CONCLUSIONS
There was a slight retrusion in the oral commissure and lower lip area after removal of the labial brackets, but no changes were found in the upper lip area.
There were no significant changes in the x-, y-, or z-coordinate values of most landmarks in the perioral soft tissues after debonding in different genders and lip thicknesses.
3-D stereophotogrammetry should be useful in evaluating facial soft tissue changes in orthodontic patients.
REFERENCES
- 1.Riedel RA. Esthetics and its relation to orthodontic therapy. Angle Orthod. 1950;20:168–178. doi: 10.1043/0003-3219(1950)020<0168:EAIRTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Lee JS, Choy K, Park YC, Kim KH. Changes in lip and perioral soft tissue after bracket removal. Korean J Orthod. 2007;37:125–136. [Google Scholar]
- 3.Abed Y, Har-Zion G, Redlich M. Lip posture following debonding of labial appliances based on conventional profile photographs. Angle Orthod. 2009;79:235–239. doi: 10.2319/030608-133.1. [DOI] [PubMed] [Google Scholar]
- 4.Kau CH, Richmond S, Incrapera A, English J, Xia JJ. Three-dimensional surface acquisition systems for the study of facial morphology and their application to maxillofacial surgery. Int J Med Robot. 2007;3:97–110. doi: 10.1002/rcs.141. [DOI] [PubMed] [Google Scholar]
- 5.Eidson L, Cevidanes LH, de Paula LK, Hershey HG, Welch G, Rossouw PE. Three-dimensional evaluation of changes in lip position from before to after orthodontic appliance removal. Am J Orthod Dentofacial Orthop. 2012;142:410–418. doi: 10.1016/j.ajodo.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baik HS, Kim SY. Facial soft-tissue changes in skeletal Class III orthognathic surgery patients analyzed with 3-dimensional laser scanning. Am J Orthod Dentofacial Orthop. 2010;138:167–178. doi: 10.1016/j.ajodo.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 7.Aynechi N, Larson BE, Leon-Salazar V, Beiraghi S. Accuracy and precision of a 3D anthropometric facial analysis with and without landmark labeling before image acquisition. Angle Orthod. 2011;81:245–252. doi: 10.2319/041810-210.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim YK, Chu EH, Lee DY, Yang IH, Baek SH. Three-dimensional evaluation of soft tissue change gradients after mandibular setback surgery in skeletal Class III malocclusion. Angle Orthod. 2010;80:896–903. doi: 10.2319/021210-90.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim M, Lee DY, Lim YK, Baek SH. Three-dimensional evaluation of soft tissue changes after mandibular setback surgery in class III malocclusion patients according to extent of mandibular setback, vertical skeletal pattern, and genioplasty. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e20–e32. doi: 10.1016/j.tripleo.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Plooij JM, Swennen GR, Rangel FA, et al. Evaluation of reproducibility and reliability of 3D soft tissue analysis using 3D stereophotogrammetry. Int J Oral Maxillofac Surg. 2009;38:267–273. doi: 10.1016/j.ijom.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 11.de Menezes M, Rosati R, Ferrario VF, Sforza C. Accuracy and reproducibility of a 3-dimensional stereophotogrammetric imaging system. J Oral Maxillofac Surg. 2010;68:2129–2135. doi: 10.1016/j.joms.2009.09.036. [DOI] [PubMed] [Google Scholar]
- 12.Meyer-Marcotty P, Kochel J, Richter U, Richter F, Stellzig-Eisenhauer A. Reaction of facial soft tissues to treatment with a Herbst appliance. J Orofac Orthop. 2012;73:116–125. doi: 10.1007/s00056-011-0068-6. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen T, Cevidanes L, Cornelis MA, Heymann G, de Paula LK, De Clerck H. Three-dimensional assessment of maxillary changes associated with bone anchored maxillary protraction. Am J Orthod Dentofacial Orthop. 2011;140:790–798. doi: 10.1016/j.ajodo.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Besl PJ, McKay ND. A method for registration of 3-D shapes. IEEE Trans. Patt. Anal Machine Intell. 1992;14:239–256. [Google Scholar]
- 15.Toma AM, Zhurov A, Playle R, Ong E, Richmond S. Reproducibility of facial soft tissue landmarks on 3D laser-scanned facial images. Orthod Craniofac Res. 2009;12:33–42. doi: 10.1111/j.1601-6343.2008.01435.x. [DOI] [PubMed] [Google Scholar]
- 16.Jeon H, Lee SJ, Kim TW, Donatelli RE. Three-dimensional analysis of lip and perioral soft tissue changes after debonding of labial brackets. Orthod Craniofac Res. 2013;16:65–67. doi: 10.1111/ocr.12006. [DOI] [PubMed] [Google Scholar]
- 17.Oliver BM. The influence of lip thickness and strain on upper lip response to incisor retraction. Am J Orthod. 1982;82:141–149. doi: 10.1016/0002-9416(82)90492-4. [DOI] [PubMed] [Google Scholar]
- 18.Kokodynski RA, Marshall SD, Ayer W, Weintraub NH, Hoffman DL. Profile changes associated with maxillary incisor retraction in the postadolescent orthodontic patient. Int J Adult Orthod Orthognath Surg. 1997;12:129–134. [PubMed] [Google Scholar]
- 19.Lee WJ, Lee KJ, Yu HS, Baik HS. Lip and perioral soft tissue changes after bracket bonding using 3-D laser scanner. Korean J Orthod. 2011;41:411–422. [Google Scholar]
- 20.Wholley CJ, Woods MG. The effects of commonly prescribed premolar extraction sequences on the curvature of the upper and lower lips. Angle Orthod. 2003;73:386–395. doi: 10.1043/0003-3219(2003)073<0386:TEOCPP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Mirabella D, Bacconi S, Gracco A, Lombardo L, Siciliani G. Upper lip changes correlated with maxillary incisor movement in 65 orthodontically treated adult patients. World J Orthod. 2008;9:337–348. [PubMed] [Google Scholar]
- 22.Moseling KP, Woods MG. Lip curve changes in females with premolar extraction or nonextraction treatment. Angle Orthod. 2004;74:51–62. doi: 10.1043/0003-3219(2004)074<0051:LCCIFW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Bergman RT, Waschak J, Borzabadi-Farahani A, Murphy NC. Longitudinal study of cephalometric soft tissue profile traits between the ages of 6 and 18 years. Angle Orthod. 2014;84:48–55. doi: 10.2319/041513-291.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stephens CK, Boley JC, Behrents RG, Alexander RG, Buschang PH. Long-term profile changes in extraction and nonextraction patients. Am J Orthod Dentofacial Orthop. 2005;128:450–457. doi: 10.1016/j.ajodo.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 25.Schendel SA, Jacobson R, Khalessi S. 3-dimensional facial simulation in orthognathic surgery: is it accurate. J Oral Maxillofac Surg. 2013;71:1406–1414. doi: 10.1016/j.joms.2013.02.010. [DOI] [PubMed] [Google Scholar]



![Figure 3. Soft tissue landmarks and three-dimensional coordinate system: x-axis (left-right axis; left [+], right [−]), y-axis (vertical axis; superior [+], inferior [−]), and z-axis (anteroposterior axis; anterior [+], posterior [−]).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/89eb/8610407/62ec5a5b7834/i0003-3219-85-5-833-f03.jpg)