Abstract
Objective:
To follow a group of children from primary to early permanent dentition and determine the prevalence, self-correction, and new development of malocclusions; the need for orthodontic treatment; and the possible influences of habits, breathing disturbances, and allergies.
Materials and Methods:
Two hundred and seventy-seven children were followed at 3, 7, and 11.5 years of age. Malocclusions and orthodontic treatment need were determined by clinical examinations. Data on sucking habits, breathing disturbances, allergies, dental trauma, and orthodontic treatments were collected from a questionnaire and dental records.
Results:
Malocclusions were found in 71% of participants at 3 years of age, 56% at 7 years of age, and 71% at 11.5 years of age. Self-correction was noted for anterior open bite, sagittal malocclusions, and posterior crossbite, while deep bite developed. A high number of contact point displacements and spacings contributed to the prevalence of malocclusion rate of 71% at 11.5 years. Severe or extreme orthodontic treatment need was apparent in 22%. Habits, allergies, or breathing disturbances found at 3 years of age had no associations with malocclusions at 11.5 years of age.
Conclusions:
This sample revealed a significant percentage of malocclusions and orthodontic treatment need. A substantial number of self-corrections and establishment of new malocclusions occurred during the transition from primary to early permanent dentition.
Keywords: Malocclusion, Prevalence, Self-correction, Longitudinal study
INTRODUCTION
The prevalence of malocclusion among children has been reported to range from 39% to 93%.1–4 This wide range of prevalence figures may be due to variations in ethnic group, age group, and methods of registration. Even a high prevalence of malocclusion does not indicate that all children or adolescents with malocclusion are in need of orthodontic treatment. Malocclusions can vary from mild to severe, with varying impacts on esthetics and/or function.
The etiology of different malocclusions is complex and varying and includes both hereditary and environmental factors. A relatively high heritability of craniofacial dimensions and low heritability of dental arch variations have been described, but it is still unclear how this relates to the etiologic process of malocclusions that have both skeletal and dental components.5,6 Environmental factors such as sucking habits have been associated with anterior open bite and posterior crossbite.7,8 Mouth breathing as a result of allergic reactions, hypertrophic adenoids, and/or enlarged tonsils has been associated with posterior crossbite.7,9 Snoring and nocturnal breathing disturbances may also have negative effects on the dentition.10–12 Consequently, it is not just hereditary factors, but also environmental components, that have the potential to affect the developing dentition.
In prevalence studies of malocclusions, study samples should be obtained from well-defined populations, should be large enough, and should cover non–orthodontically treated participants of different ages.2 Most previous studies on the prevalence of malocclusions are cross-sectional and, thus, do not allow assessments of stability or change of individual malocclusions. Longitudinal studies would be of great value in increasing our knowledge and understanding of dentition development and in gathering information for effective planning related to orthodontic treatment. Thus, the aim of this study was to follow a group of children to determine the following:
The prevalence of malocclusion from primary to early permanent dentition;
The frequency of self-correction and new development of malocclusions;
The orthodontic treatment need among children in early permanent dentition; and
The possible influence of habits, breathing disturbances, and allergies on the prevalence of malocclusion.
MATERIALS AND METHODS
The study sample was sourced from three Swedish Public Dental Service clinics, each located in a small rural community of about 22,000 inhabitants. Of the 457 children included at baseline (age 3 years), 386 remained at the first follow-up (age 7 years) and 277 remained at the final follow-up (age 11.5 years). Consequently, 277 children (128 boys and 149 girls) constituted the sample in this study. In order to reduce potential confounding factors, such as ethnic differences and environmental conditions, only Scandinavian children were included. Children with syndromes or developmental disorders were excluded. Every child was given at least two opportunities to attend each examination. The ethics committee of the Uppsala Health Care Region, Sweden, approved the study protocol and informed consent form (ref: 2012/273).
Clinical Examination
The examinations at baseline (T0, age 3 years) and first follow-up (T1, age 7 years) were undertaken by one experienced clinician (LD) between 2003 and 2009. At the final follow-up (T2, age 11.5 years), the clinical examination was carried out by two experienced clinicians between 2012 and 2013. The examiners used a mouth mirror and probe and followed a specific protocol. The methods of Björk et al.13 and Foster and Hamilton14 served as guidelines for registration of malocclusion in centric occlusion.
Occlusal Measures
The occlusal measures were stratified as unilateral or bilateral and checked for anterior or lateral shift in the mandibular retruded position. A stainless-steel ruler was used to measure overjet and overbite to an accuracy of 0.5 mm.
Sagittal relations
Sagittal occlusion was determined by the following two measures: (1) The relationship between the primary canines at 3 years of age, as follows:14
Class I (normal occlusion): The tip of the maxillary primary canine tooth is in the same vertical plane as the distal surface of the mandibular primary canine tooth.
Class II (postnormal occlusion): The tip of the maxillary primary canine tooth is in anterior relationship to the distal surface of the mandibular primary canine tooth.
Class III (prenormal occlusion): The tip of the maxillary primary canine tooth is in posterior relationship to the distal surface of the mandibular primary canine tooth.
(2) The relationship between the first maxillary and mandibular permanent molars at 7 and 11.5 years of age, as follows:13
Class I (normal occlusion): Normal, or at most one-half cusp postnormal or prenormal relation;
Class II (postnormal occlusion): More than one-half cusp postnormal relation. Class II (postnormal occlusion) was also subdivided into division 1 (proclined maxillary incisors) and division 2 (retroclined maxillary incisors);
Class III (prenormal occlusion): More than one-half cusp prenormal relation;
Overjet was measured at the most protruding maxillary incisor and classified as normal (0–4 mm), increased (4–6 mm), or excessive (>6 mm). The occurrence of incomplete lip closure was also registered;
Anterior crossbite was registered if one or more maxillary incisors occluded lingual to the mandibular incisors.
Vertical relations
A deep bite was registered when more than two-thirds of the mandibular incisors were covered by the maxillary incisors. Checks were also made for gingival or palatal trauma.
A negative vertical overlap was recorded as an anterior open bite, but lack of overlap due to incomplete eruption of the incisors was not considered to be open bite.
Transverse relations
Posterior crossbite and scissor bite were recorded if at least two teeth were involved.
Anterior space discrepancies
Contact point displacement was registered at T2, with a displacement of 2–4 mm defined as ‘moderate’ and displacement of >4 mm defined as ‘severe.’15 Spacing was also recorded at T2, defined as (1) general spacing and (2) diastema (>2 mm) between the maxillary incisors.
Single tooth anomalies
Impaction and supernumerary and congenitally missing teeth were recorded for permanent teeth.
Orthodontic treatment need
Assessment of treatment need was based on the Dental Health Component of the Index of Orthodontic Treatment Need (IOTN-DHC).15
Questionnaire
Data on sucking habits, breathing disturbances, allergy, dental trauma, and orthodontic treatment were collected via a semistructured interview following a questionnaire that the children and their parents were asked to complete in conjunction with the clinical examinations at T0, T1, and T2. The questionnaire protocol comprised the following “Yes/No” questions (questions 1 and 2 were specifically addressed to the parent and question 6 was only asked at T2):
Does you your child snore while sleeping?
Does your child have breathing interruptions while sleeping?
Do you have any allergies? If yes, what kind of allergies?
Do you have a bite or sucking habit? If yes, what kind of habit?
Have you experienced any dental trauma? If yes, which tooth/teeth?
Have you ever had orthodontic treatment? If yes, what kind of treatment?
Statistical Analysis
Data were analyzed using version 22.0 of the SPSS software package. McNamara's test was used when analyzing dependent data (ie, repeated measurements). Chi-square analysis was used to analyze categorical variables, and odds ratios (ORs) with 95% confidence intervals (95% CI) were calculated to measure the strength of associations. Each sagittal, vertical, and transversal malocclusion was dichotomized in contrast with others and associated with sucking habits, breathing disturbances, allergies, and dental trauma. Differences in probabilities of less than 5% (P < .05) were considered to be statistically significant.
An interexaminer test was performed using kappa statistics; the kappa values ranged from 0.84 to 1.00.
RESULTS
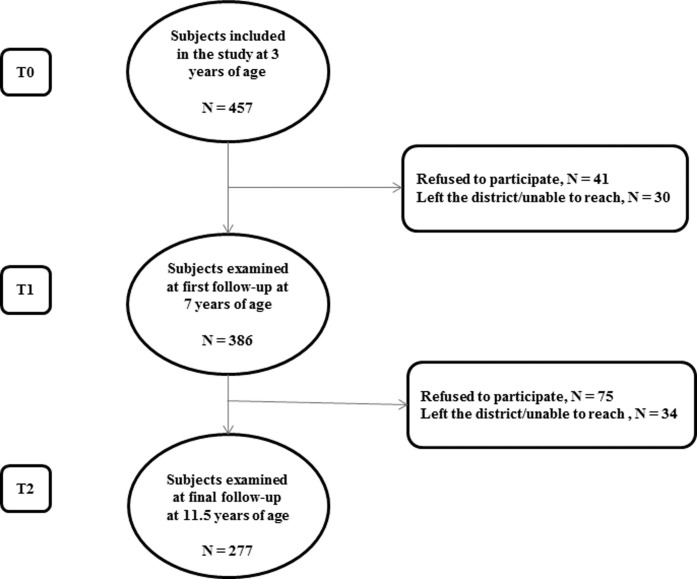
The dropout rate for the whole study period (T0–T2) was 39.4% (Figure 1). There were no differences in gender, clinic, and prevalence of malocclusions or sucking habits at 3 years of age between those who participated in the final follow-up and those who did not. At the time of the examination more than 80% of the children had all the permanent teeth ahead of the first molars in occlusion or under eruption.
Figure 1.
Flowchart of the children in the study at baseline (T0), at the first follow-up (T1), and at the final follow-up (T2).
Orthodontic treatment had been performed in 37 of the 277 children participating in the final follow-up (13%) between T1 and T2. Treatment between T1 and T2 aimed to correct functional disturbances (n = 34), and an additional three children were treated with full fixed appliances.
Prevalence of Malocclusions
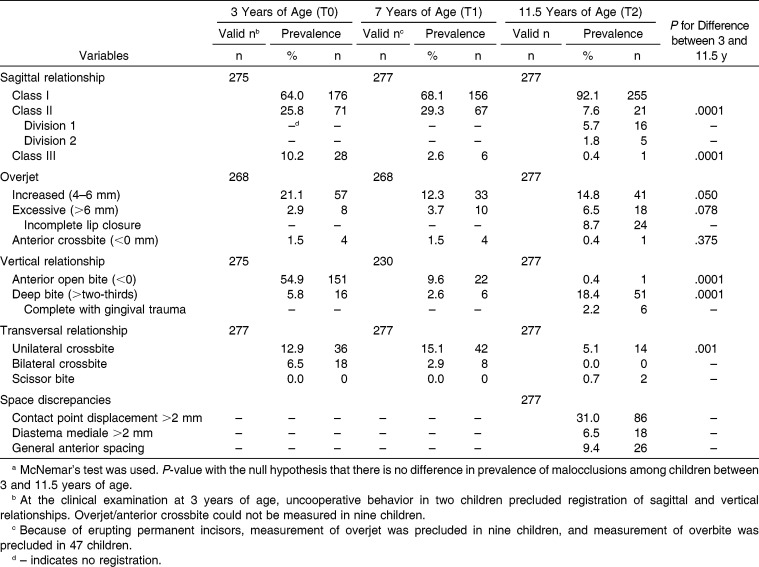
At T0, at least one malocclusion was recorded in 71% of the children. The corresponding figures at T1 and at T2 were 56% and 71%. Two or more malocclusions were recorded in 18% of children at T0, 7% of children at T1, and 37% of children at T2. The most common malocclusion at T0 was open bite, followed by postnormal sagittal relation (Class II), excessive overjet, and unilateral posterior crossbite (Table 1). With the exception of open bite, the picture was similar at T1. At T2, contact point displacement was the most prevalent malocclusion, followed by increased or excessive overjet, deep bite, and spacing (Table 1). Incomplete lip closure was common (41%) among those with an overjet exceeding 4 mm. Of those with a deep bite, 12% showed gingival or palatal trauma (Table 1). Deep bite with gingival contact was more common in children with increased/excessive overjet than in children with normal overjet (67% vs 33%; P < .001; OR = 9.0; 95% CI: 3.2–25.3). At T2, postnormal sagittal relation (Class II malocclusion) was recorded in 7.6% of the children, with the majority classified as division 1 (proclined maxillary incisors); see Table 1. Contact point displacement of more than 2 mm was more common among girls than among boys (40% vs 20%; P = .0001). No other gender differences were seen.
Table 1.
Prevalence of Malocclusions in a Cohort at Three Time Points from Primary to Early Permanent Dentitiona
Single Tooth Anomalies
Hypodontia was diagnosed in 15 children (5.4%) at T2. The most commonly affected tooth was the mandibular second premolar (eight children), followed by the maxillary second premolar (six children) and the maxillary lateral incisor (five children). Four children (1.4%) were diagnosed with ectopic eruption of the maxillary canines. One child had two supernumerary teeth in the midline of the maxilla, and another child showed a germinated tooth (left mandibular lateral incisor). Finally, transposition was found between 23 and 24 in one child.
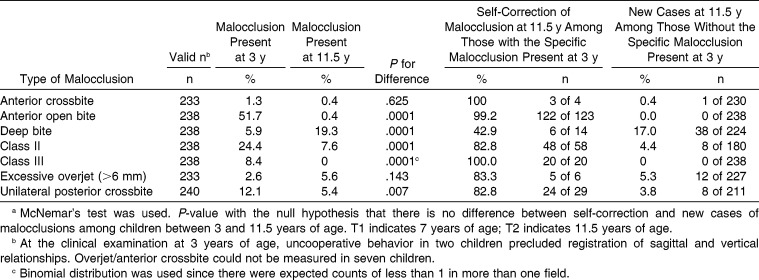
Self-Correction and Development of New Malocclusions
Between T0 and T2, significant self-correction had occurred for open bite, and Class II and III malocclusions had turned into Class I occlusion (Tables 1 and 2). The prevalence of anterior crossbite, anterior open bite, Class II and III malocclusion, excessive overjet, and unilateral posterior crossbite had decreased. On the other hand, the prevalence of deep bite had increased significantly from 5.8% to 18.4% (Table 1). A high number of contact point displacements and spacings had occurred.
Table 2.
Change of Malocclusion in a Cohort of Children from Primary to Early Permanent Dentition; 37 Children Treated Between T1 and T2 Are Excluded (n = 240)a
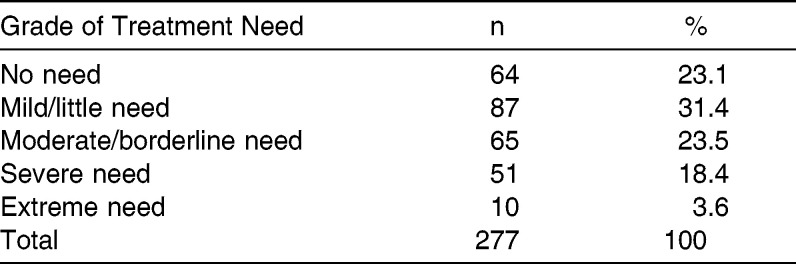
Orthodontic Treatment Need
At T2, 22.0% of the 277 children had severe or extreme treatment need, 23.5% showed moderate or borderline need, and 54.5% showed little or no need (Table 3).
Table 3.
Orthodontic Treatment Need According to the Dental Health Component of the Index of Orthodontic Treatment Need in 11.5-Year-Olds
Habits, Breathing Disturbances, and Allergies
The prevalence of sucking habits decreased from 82% to 0.4% (P < .0001) between T0 and T2; only one child still sucked his/her thumb at T2. The reported prevalence of snoring was 8% at T0 and 20% at T2 (P < .0001). Nocturnal breathing disturbances were reported for 1.4% of children at T2 and 5% of children at T0 (P = .049). The reported prevalence of allergy was 13% at T1 and 32% at T2 (P < .0001). Habits, allergies, or breathing disturbances found at 3 years of age had no associations with malocclusions at 11.5 years of age.
Dental Trauma
Thirty percent of the children had experienced dental trauma. The maxillary primary and permanent incisors were the most commonly affected teeth. At T2, experience of dental trauma was more common if an increased overjet was present (44% vs 26%; P = .008; OR = 2.2; 95% CI: 1.23–4.04). Incomplete lip closure was also more common among those with reported dental trauma (54% vs 28%; P = .007; OR = 3.1; 95% CI: 1.32–7.22).
DISCUSSION
This longitudinal study adds important new knowledge about development of malocclusions from primary to early permanent dentition. The overall prevalence of malocclusions was equal, 71%, at 3 and 11.5 years of age. However, on an individual level changes were clear. Self-correction of open bites was common. In addition, transition of Class II malocclusion to normal occlusion occurred frequently and could be assumed to be a result of mesial movement of the mandibular first molars as the second primary molars exfoliated. The shift from Class III to Class I occlusion was unexpected. However, a similar pattern has been presented in earlier longitudinal studies.16,17 One explanation may be that incorrect sagittal registration was performed at 3 years of age (the 3-year-old child is prone to slide forward with the mandible in occlusion). Another explanation may be the discrepancy in size between maxillary and mandibular deciduous molars, resulting in a flush relationship between the distal surfaces of the maxillary and mandibular second deciduous molars. This favors the normal relationship between permanent molars when deciduous molars are replaced.
Deep bite increased in prevalence between primary and early permanent dentition. In addition, a high number of contact point displacements and spacings that could not be diagnosed at T0 and T1 contributed to the malocclusion prevalence rate at T2. These findings about contact point displacements are parallel with those of earlier studies.17–19
The previously reported strong association between sucking habits and anterior open bite and posterior crossbite at both 3 and 7 years of age1 was not apparent at 11.5 years of age. This implies that sucking habits in the early years have little or no later effect on the permanent dentition. On the other hand, it has been found that presence of a sucking habit until 5 years of age was correlated with morphological malocclusion severity at 12 years of age.20 No association between malocclusion and allergies or snoring was seen in this sample, in contrast to the results of other studies.10,21 One can always question if results from self-reported data are valid, but it has been shown22 that such data have good validity on a population level. However, the validity of the questions about snoring and nocturnal breathing disturbances can be disputed, and the results should be interpreted with caution.
Dental trauma was found in 30% of the sample, and a similar prevalence was found in another population.23 An association was seen between increased overjet and dental trauma at 11.5 years of age, but not at 3 and 7 years of age. This is an interesting and important finding from a clinical point of view, given the discussion about the best time for treatment of excessive overjet. This study supports correction of overjet of greater than 4 mm in combination with incomplete lip closure before 11.5 years of age.
Not all malocclusions need to be treated, but 22% of the participants in this study had, according to the IOTN-DHC, severe or extreme orthodontic treatment need at 11.5 years of age. An additional 23.5% had a borderline need, and it is conceivable that at least half of these will be offered treatment, resulting in a total orthodontic treatment need of about 35% (well in line with reports from other studies).24–26
Longitudinal studies are of great value and are considered to generate a much higher level of evidence than do cross-sectional studies. This type of study is considered the most appropriate for discovering associations between the different factors behind the development or self-correction of malocclusions. Consequently, the strengths of this study were its longitudinal design and the use of a homogeneous sample, one that included only Scandinavian participants. One drawback was the rather high attrition rate, but a certain dropout rate is inevitable in a long-term study. In order to minimize dropouts, an examination at a Public Dental Service clinic in the patient's home area was offered. Although the total attrition rate was 39.6%, the dropout analysis disclosed no differences between the final study sample participants and those who failed to complete the study. It is worth mentioning that the 37 participants who had undergone orthodontic treatment were excluded from the longitudinal analysis. However, these patients had functional disturbances, and from an ethical point of view it was not possible to postpone treatment of features such as functional disturbing posterior crossbite or excessive overjet. Anyhow, the 37 children were included in the presentation of orthodontic treatment need since to receive orthodontic care the children have to have a malocclusion that is at least categorized as “severe treatment need.”
CONCLUSIONS
The prevalence of malocclusions was equal at 3 and 11.5 years of age.
Self-correction of anterior open bite, sagittal malocclusions, and unilateral posterior crossbite in the primary dentition was common.
Deep bite, contact point displacement, and spacing were the malocclusions most commonly emerging from primary to early permanent dentition.
Gingival or palatal trauma was reported in 12% of children with deep bites.
Overjet exceeding 4 mm in combination with incomplete lip closure carried a 3.1 times higher risk for dental trauma in comparison with normal lip closure.
At 11.5 years of age, 22.0% of children had severe or extreme orthodontic treatment need, 23.5% had a moderate or borderline need, and 54.5% had little or no need.
Habits and allergies found at 3 years of age had no associations with malocclusions at 11.5 years of age.
ACKNOWLEDGMENT
The authors would like to thank all patients and their parents for contributing to this study. We also want to thank the staff at the three public dental service clinics and the staff at the Department of Orthodontics at the Postgraduate Dental Education Center for their help in completing this study. This study was supported by grants from the Örebro County Council and from the Swedish Dental Society.
REFERENCES
- 1.Dimberg L, Lennartsson B, Soderfeldt B, Bondemark L. Malocclusions in children at 3 and 7 years of age: a longitudinal study. Eur J Orthod. 2013;35:131–137. doi: 10.1093/ejo/cjr110. [DOI] [PubMed] [Google Scholar]
- 2.Thilander B, Pena L, Infante C, Parada SS, de Mayorga C. Prevalence of malocclusion and orthodontic treatment need in children and adolescents in Bogota, Colombia. An epidemiological study related to different stages of dental development. Eur J Orthod. 2001;23:153–167. doi: 10.1093/ejo/23.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81:12–21. doi: 10.1111/j.1600-0722.1973.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 4.Tschill P, Bacon W, Sonko A. Malocclusion in the deciduous dentition of Caucasian children. Eur J Orthod. 1997;19:361–367. doi: 10.1093/ejo/19.4.361. [DOI] [PubMed] [Google Scholar]
- 5.Mossey PA. The heritability of malocclusion: part 2. The influence of genetics in malocclusion. Br J Orthod. 1999;26:195–203. doi: 10.1093/ortho/26.3.195. [DOI] [PubMed] [Google Scholar]
- 6.Proffit WR, Fields HW, Sarver D, editors. Contemporary Orthodontics 5th ed. St. Louis, MO: Linda Duncan; 2013. [Google Scholar]
- 7.Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1–132. [PubMed] [Google Scholar]
- 8.Larsson E. The effect of dummy-sucking on the occlusion: a review. Eur J Orthod. 1986;8:127–130. doi: 10.1093/ejo/8.2.127. [DOI] [PubMed] [Google Scholar]
- 9.Oulis CJ, Vadiakas GP, Ekonomides J, Dratsa J. The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits. J Clin Pediatr Dent. 1994;18:197–201. [PubMed] [Google Scholar]
- 10.Vazquez-Nava F, Quezada-Castillo JA, Oviedo-Trevino S, et al. Association between allergic rhinitis, bottle feeding, non-nutritive sucking habits, and malocclusion in the primary dentition. Arch Dis Child. 2006;91:836–840. doi: 10.1136/adc.2005.088484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gois EG, Ribeiro-Junior HC, Vale MP, et al. Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008;78:647–654. doi: 10.2319/0003-3219(2008)078[0647:IONSHB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Zicari AM, Albani F, Ntrekou P, et al. Oral breathing and dental malocclusions. Eur J Paediatr Dent. 2009;10:59–64. [PubMed] [Google Scholar]
- 13.Bjoerk A, Krebs A, Solow B. A method for epidemiological registration of malocclusion. Acta Odontol Scand. 1964;22:27–41. doi: 10.3109/00016356408993963. [DOI] [PubMed] [Google Scholar]
- 14.Foster TD, Hamilton MC. Occlusion in the primary dentition. Study of children at 2 and one-half to 3 years of age. Br Dent J. 1969;126:76–79. [PubMed] [Google Scholar]
- 15.Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 16.Leighton BC, Feasby WH. Factors influencing the development of molar occlusion: a longitudinal study. Br J Orthod. 1988;15:99–103. doi: 10.1179/bjo.15.2.99. [DOI] [PubMed] [Google Scholar]
- 17.Foster TD, Grundy MC. Occlusal changes from primary to permanent dentitions. Br J Orthod. 1986;13:187–193. doi: 10.1179/bjo.13.4.187. [DOI] [PubMed] [Google Scholar]
- 18.Legovic M, Mady L. Longitudinal occlusal changes from primary to permanent dentition in children with normal primary occlusion. Angle Orthod. 1999;69:264–266. doi: 10.1043/0003-3219(1999)069<0264:LOCFPT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Jonsson T, Arnlaugsson S, Saemundsson SR, Magnusson TE. Development of occlusal traits and dental arch space from adolescence to adulthood: a 25-year follow-up study of 245 untreated subjects. Angle Orthod. 2009;135:456–462. doi: 10.1016/j.ajodo.2007.04.047. [DOI] [PubMed] [Google Scholar]
- 20.Ovsenik M, Farcnik FM, Korpar M, Verdenik I. Follow-up study of functional and morphological malocclusion trait changes from 3 to 12 years of age. Eur J Orthod. 2007;29:523–529. doi: 10.1093/ejo/cjm065. [DOI] [PubMed] [Google Scholar]
- 21.Luzzi V, Ierardo G, Viscogliosi A, et al. Allergic rhinitis as a possible risk factor for malocclusion: a case-control study in children. Int J Paediatr Dent. 2013;23:274–278. doi: 10.1111/ipd.12003. [DOI] [PubMed] [Google Scholar]
- 22.Kronstrom M, Palmqvist S, Eriksson T, Soderfeldt B, Carlsson GE. Practice profile differences among Swedish dentists. A questionnaire study with special reference to prosthodontics. Acta Odontol Scand. 1997;55:265–269. doi: 10.3109/00016359709114962. [DOI] [PubMed] [Google Scholar]
- 23.Forsberg CM, Tedestam G. Traumatic injuries to teeth in Swedish children living in an urban area. Swed Dent J. 1990;14:115–122. [PubMed] [Google Scholar]
- 24.Josefsson E. Immigrant background and orthodontic treatment need. Quantitative and qualitative studies in Swedish adolescents. Swed Dent J Suppl. 2010:1–92. [PubMed] [Google Scholar]
- 25.Migale D, Barbato E, Bossu M, Ferro R, Ottolenghi L. Oral health and malocclusion in 10-to-11 years-old children in southern Italy. Eur J Paediatr Dent. 2010;207:13–18. [PubMed] [Google Scholar]
- 26.Dias PF, Gleiser R. Orthodontic treatment need in a group of 9-12-year-old Brazilian schoolchildren. Braz Oral Res. 2009;23:182–189. doi: 10.1590/s1806-83242009000200015. [DOI] [PubMed] [Google Scholar]