Abstract
Case Presentation
A 65-year-old male presented to the emergency department with symptoms including fever, abnormal urinalysis, and elevated post-void residual. Point-of-care ultrasound was used to rapidly diagnose a bladder diverticulum. The patient was subsequently seen by urology for outpatient bladder repair.
Discussion
Bladder diverticula, an out-pouching of the bladder, may occur congenitally or as a result of various bladder conditions and/or surgery. Although bladder diverticula are rare and often asymptomatic, severe complications including frequent recurring urinary tract infections may arise depending on the patient.
Keywords: bladder diverticulum, laparoscopy
CASE PRESENTATION
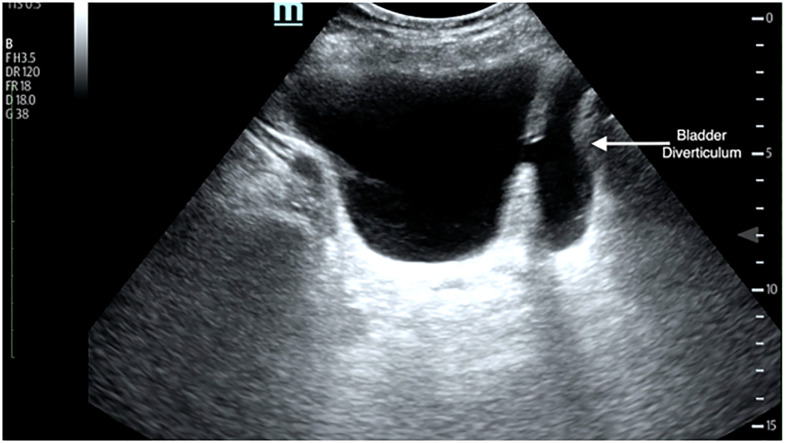
A 65-year-old male with a history of benign prostatic hypertrophy presented to the emergency department with generalized weakness, low-grade fever, and urinary frequency. Point-of-care ultrasound (POCUS) demonstrated a post-void residual greater than 500 milliliters, measured with ultrasound machine calculation software, and a large abnormality of the urinary bladder (Image, Video). No hydronephrosis was seen on renal ultrasound. Chart review showed several prior visits for urinary tract infections (UTI) and one hospitalization for sepsis due to pyelonephritis. Given multiple previous infections and sensation of incomplete emptying, a POCUS was performed and aided in making the diagnosis. The patient was treated with intravenous antibiotics and discharged home. Ultimately, given the symptomatic nature of the bladder diverticula with multiple previous UTIs, urology repaired the defect as an outpatient procedure.
Image.
Ultrasound demonstrating a bladder diverticulum, with the out-pouching (arrow) to the right of the bladder.
DISCUSSION
A bladder diverticulum is an out-pouching of the bladder that occurs when a part of the bladder lining protrudes through a weakness in the bladder wall. These occur either congenitally or as an acquired condition from bladder outlet obstruction, neurogenic bladder conditions, or from prior bladder surgery.1 The prevalence of congenital diverticula is approximately 1.7%.2 The incidence increases with age and is most common in men with benign prostatic hypertrophy at a rate of up to 6%.3 The male to female ratio of 9:1 reflects this finding.4 Because bladder diverticula are typically asymptomatic, they are usually discovered on evaluations for UTIs, hematuria, or lower urethral tract symptoms.
Management of bladder diverticula depends on the complications that arise. Nonoperative, conservative management includes treatment with antibiotics for UTIs and avoidance of medications that cause urinary retention, such as opioids. Malignancy is a feared complication as the diverticula lacks a muscular wall outside the mucosal layer allowing metastatic spread more rapidly. Open or laparoscopic surgical correction options exist and are chosen based on several factors such as malignancy, size, and surgeon experience.1 This diagnosis can be made with POCUS and may explain the etiology of patients with recurrent UTIs. It is important to note that complete imaging of the bladder may be necessary to capture a definitive image of the break in the bladder wall.
CPC-EM Capsule.
What do we already know about this clinical entity?
Bladder diverticulum is an out-pouching of the bladder that may be acquired or congenital.
What is the major impact of the image(s)?
Bladder diverticula, which can be identified using point-of-care ultrasound, should be considered in patients with repeat urinary tract infections (UTI).
How might this improve emergency medicine practice?
Point-of-care ultrasound can help identify bladder diverticula in patients with repeat UTIs.
Supplementary Information
A coronal, or long-axis, view of the bladder with an out-pouching bladder diverticulum on the right side of the screen.
Footnotes
Section Editor: Gentry R. Wilkerson, MD
Full text available through open access at http://escholarship.org/uc/uciem_cpcem
The authors attest that their institution requires neither Institutional Review Board approval nor patient consent for publication of this case report. Documentation on file.
Conflicts of Interest: By the CPC-EM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Pham KN, Jeldres C, Hefty T, et al. Endoscopic management of bladder diverticula. Rev Urol. 2016;18(2):114–7. doi: 10.3909/riu0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blane CE, Zerin JM, Bloom DA. Bladder diverticula in children. Radiology. 1994;190(3):695–7. doi: 10.1148/radiology.190.3.8115613. [DOI] [PubMed] [Google Scholar]
- 3.Burns E. Diverticula of the urinary bladder. Ann Surg. 1944;119(5):656–64. doi: 10.1097/00000658-194405000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Idrees MT, Alexander RE, Kum JB, et al. The spectrum of histopathologic findings in vesical diverticulum: Implications for pathogenesis and staging. Hum Pathol. 2013;44(7):1223–32. doi: 10.1016/j.humpath.2012.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A coronal, or long-axis, view of the bladder with an out-pouching bladder diverticulum on the right side of the screen.