Abstract
Objective
The most important indication for EEGs is the investigation of epileptic and nonepileptic seizures. However, it is unclear whether EEG in the emergency depatment (ED) can be useful in managing other conditions. Our objective was to investigate the usefulness of EEGs in the ED.
Methods
We performed an observational, descriptive, retrospective study based on clinical records between 2018 and 2019. We evaluated patients admitted to our ED or hospital wards who underwent an EEG. We defined the EEG results as useful when they prompted changes in antiepileptic drug (AED) treatment or clinical management.
Results
We gathered information from 236 patients with a mean age of 59.23 years (SD ±22.6), of whom 47.9% were women. In patients with seizures, 18.2% were generalized, 27.1% were focal, and 18.6% were unknown. Overall, 25.8% of the EEGs were abnormal. However, in patients with a history of predisposing conditions for epileptic seizures or encephalopathies, the tracing was abnormal in 47.5%. The most frequent alteration on the abnormal EEGs was generalized slowing (18.2%). The EEG was useful in 76.7% of patients: AEDs changed in 8.4% and clinical management changed in 76.2% of patients. The usefulness of EEGs associated with acute ischemic lesions on CT (p = 0.023) and with the diagnosis of vasovagal syncope (p = 0.022).
Conclusions
Routine EEG is useful in the ED, even in patients with a normal CT or MR brain image, because it helps determine clinical management or AED changes.
Routine EEG in the emergency department (ED) proved to be useful in the ED, especially during the first 24–48 hours.1–3 Nevertheless, EEG in the ED had no clear indication, other than nonconvulsive status epilepticus (NCSE).3–5 EEG is an expensive tool, because of the requirement of highly qualified personal, especially in developing countries, where resources are scarce.
Similarly, routine emergency EEG can help both the ED and hospitalized patients for evaluating diseases other than epilepsy. It can also contribute to the differential diagnosis of seizures. Although the development of neuroimaging has provided more sensitive information in these cases, ordering a routine EEG is useful for ruling out concomitant epileptic seizures (ESs), based on functional analysis, and for proposing treatments that will diminish surrounding morbidity and complementing results.4
Therefore, this study evaluated the usefulness of EEGs in the ED. Usefulness is understood as changes in clinical diagnosis and management, such as changes in the dose or type of antiepileptic drugs (AEDs).
Methods
In this descriptive, observational cross-sectional study, we reviewed the medical records of patients admitted to the ED and hospital wards of an IV level hospital in Bogota during 2018 and 2019. We included patients older than the age of 18 years who underwent an EEG. The treating physician determined an EEG indication. The electrode placement and recording technique were standard. As part of clinical care, follow-up laboratory tests were taken such as a complete blood count (CBC), urinalysis, and electrolytes including potassium, chloride, calcium, magnesium, and sodium that was classified as mild (130–165 mEq/L), moderate (125–129 mEq/L), and severe (<125 mEq/L).6
We included clinical and demographic variables, such as a history of epilepsy or other diseases that would predispose to ESs or encephalopathy, previous AEDs, the reason for the ED visit, type of ES, neurologic examination, and brain CT or MRI results. In addition, we reported the admission electrolyte and CBC results. We categorized the EEG results as follows: normal, generalized interictal epileptiform discharges, focal interictal epileptiform discharges, generalized slowing, focal slowing, and compatible with NCSE. Finally, we evaluated the usefulness of the EEG based on medication changes such as initiation, discontinuation, change, or dose change of AEDs in the ED. Furthermore, we reviewed the clinical management, defined as contributing to the diagnosis (ruling out or confirming a diagnosis), contributing to clinical management (changes in medications not just AEDs), discharge from the ED or hospital wards, and the diagnosis at discharge.
We performed statistical analyses using the SPSS v.22 program. We analyzed qualitative variables using frequency and percentage distributions, and quantitative variables using measures of central tendency such as the average, median and mode, and measures of variability and dispersion such as range, variance, and standard deviation. Subsequently, we used a bivariate analysis to determine the usefulness of the EEG in relationship to the study variables. We used the χ2 test for qualitative variables, whereas normality was assessed for quantitative variables, applying the Mann-Whitney U test if they were not normal. We also calculated the odds ratio (OR) with a 95% confidence interval (CI) for clinical, laboratory, and imaging variables in the study.
Standard Protocol Approvals, Registrations, and Patient Consents
This study was performed according to the Ministry of Health's resolution 008430 of 1993 (“scientific, technical, and administrative norms for health research”); according to local regulations, our study was classified as “no risk”; therefore, patients' consent was not required. The study was approved by the ethics committee from our institution.7 In addition, all patients signed a patient's consent form at hospital admission for data management and research purposes.
Data Availability
Data are available from Dryad (tables 1 and 2, https://datadryad.org/stash/share/x5bf_rm762DrldLmc5VKCSIbg3ue7NNyxGucs-TYrPE). Anonymized data will be shared by request from any qualified investigator.
Results
In this observational study, we included 236 patients with an average age of 59.22 years (±22.61), of whom 47.9% were women. A total of 46.2% had a baseline condition that predisposed them to ESs or encephalopathy (table 1). The most frequent antecedent was epilepsy, which had a structural etiology and an unknown etiology. In patients with a predisposition to encephalopathy, the most frequent antecedent was chronic kidney failure. Altogether, 20.33% of patients diagnosed with epilepsy were receiving AEDs, and the most used AEDs were valproic acid and levetiracetam (table 1).
Table 1.
Sociodemographic Characterization
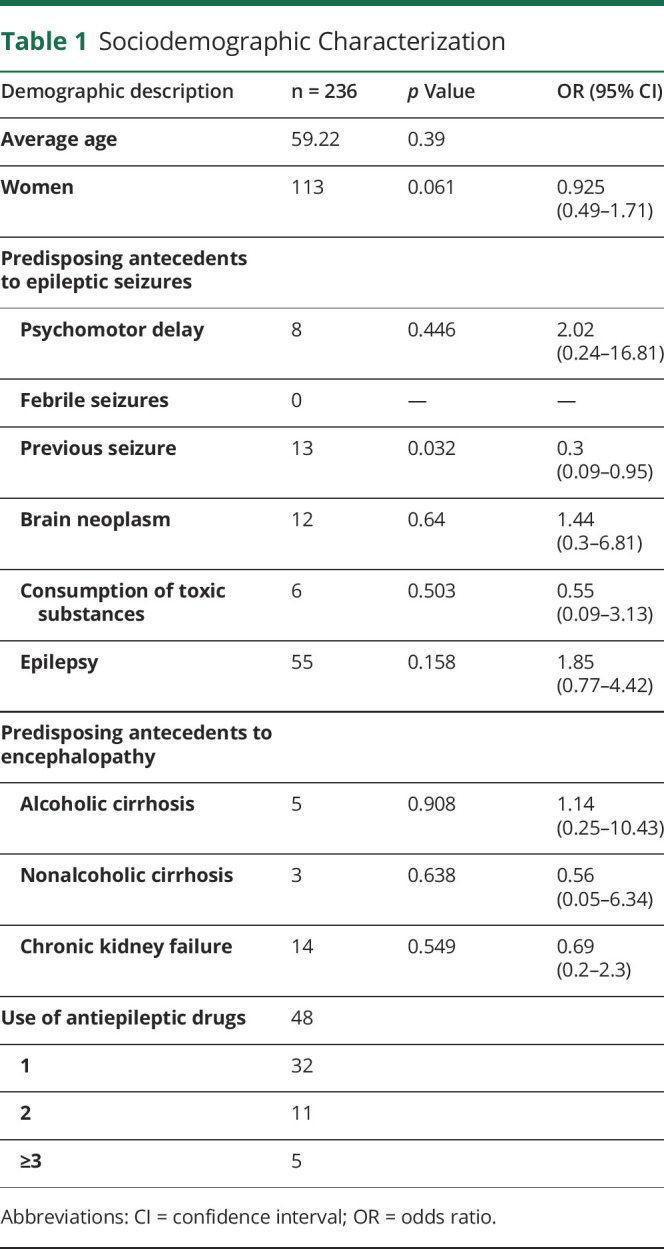
The most frequent admitting diagnoses were altered consciousness, ES, possible non-ESs, and ischemic cerebrovascular accident or transient ischemic attack. Of those with ESs, presented with their first seizure and had recurrent seizures. Furthermore, 18.2% presented with generalized seizures, 27.1% had focal seizures, and the rest were not classified.
The neurologic examination was abnormal in half of the patients. On the laboratory examinations, although the patients had different electrolyte disturbances, the most common was hyponatremia and hypochloremia or hyperchloremia. Hyponatremia was mild in most cases, and of these, 29.6% had an EEG alteration.
A total of 202 CTs were taken, of which more than half were abnormal. The most frequent finding was an old ischemic lesion. Furthermore, 127 MRIs were taken, of which most were abnormal, and the most frequent finding was an old ischemic lesion. The main reason for ordering the EEG was a first ES, followed by a suspected seizure and altered state of consciousness.
The EEGs were abnormal in a quarter of patients. Of these, the most frequent alterations were generalized slowing, focal slowing, and interictal epileptiform discharges. Altogether, half of the abnormal EEGs belonged to patients with some antecedent that predisposed them to ESs or encephalopathies.
The overall usefulness of EEGs was 76.7%. AEDs changed in a reduced group of patients, and most of them received clinical management, such as changing the diagnosis or the hospital management and discharge. Furthermore, despite having a normal EEG, changes in AED treatment were made in 29 cases based on clinical criteria. Accordingly, in patients with a normal EEG, the test was useful in 80% of cases because changes in clinical conduct were made, e.g., patients were discharged (table 2).
Table 2.
EEG Usefulness
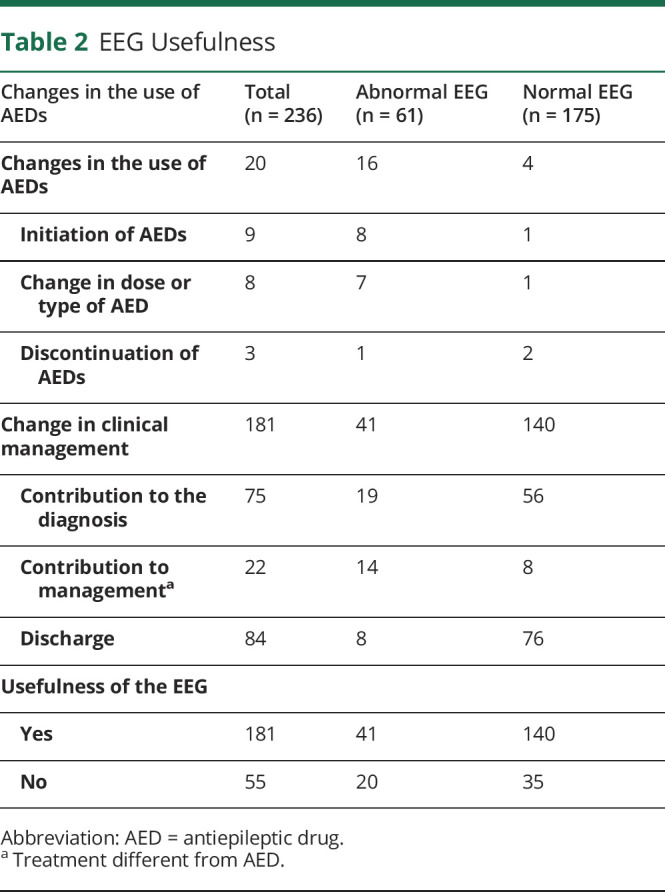
Utility in patients with previous epilepsy was 85.41% (41), meanwhile in patients with predisposing factors to encephalopathy was 72.72% (16) and patients with single seizure presented 90.46% (20) utility.
The variables that achieved statistical significance when evaluating the usefulness of the EEG were patients with an acute ischemic lesion on CT (p = 0.023; OR 0.256; 95% CI 0.085–0.766) or a normal CT (p = 0.02; OR 1.792; 95% CI 0.919–3.494), an admitting diagnosis of syncope (p = 0.022; OR 0.215; 95% CI 0.063–0.737), and a history of epilepsy (p = 0.02; OR 1.85; 95% CI 0.77–4.42).
Discussion
The EEG is very useful for diagnosing epilepsy; however, studies show that this tool is infrequently used in the ED.8 One reason for this is that hospitals face technical difficulties and personnel limitations for performing this test; one multicenter study even showed a 3% order rate for this test. There are various indications for using an EEG in the ED today, such as coma of unknown origin, unexplained focal neurologic disorder, altered state of consciousness after status epilepticus, and suspected psychogenic seizures.2 However, this study showed that the EEG had a usefulness of 77.3% based on the information it provides for making changes in pharmacologic treatment and clinical conduct, in comparison to studies with similar utility classification of EEG showed 60.8% based on diagnosis9 and others evidenced 60.2%.5 This result was more useful in patients with an altered state of consciousness and nonepileptic paroxysmal events.
Various studies have shown the usefulness of this test for indications such as NCES and first seizure.10 Another Spanish observational study (2018)2 found that in 83% of cases, the possibility of NCES was able to be ruled out in patients with an altered state of consciousness, altered behavior, and aphasia. Altogether, 33% of cases were diagnosed with NCES. The EEG performed in the ED to rule out NCES showed a sensitivity of 92.1%, a specificity of 97.2%, a positive predictive value of 94.6%, and a negative predictive value of 96%.2
According to the American Epilepsy Society, an EEG in patients with a first unprovoked seizure should be part of the diagnostic studies, considered the level of evidence B.11 In a large study,12 epileptiform alterations were detected in 51% of patients on whom an EEG was performed within less than 24 hours; another study even found epileptiform abnormalities in 73.5%,1 whereas in our study, these abnormalities presented in only 25.4%.
In various studies, 34%–56% of patients with seizures had abnormal CTs,1 whereas our study reported abnormalities in 31.7%.12 A bivariate analysis between the CT alterations was not statistically significant.
A study similar to ours found that after performing the EEG, changes in AEDs were made in 67.8%, of which 59.8% were chronic or long term and the remaining percentage were acute changes, these being less frequent.13 When compared with this study in which these treatment adjustments were made in 20.7% of patients, this can be correlated with the fact that the EEG abnormalities were less frequent.
Variables that achieved statistical significance based on bivariate analysis when evaluating the usefulness of the EEG were patients with an acute ischemic lesion on CT (p = 0.023; OR 0.256; 95% CI 0.085–0.766) and an admitting diagnosis of syncope (p = 0.022; OR 0.215; 95% CI 0.063–0.737), nevertheless normal CT (p = 0.02; OR 1.792; 95% CI 0.919–3.494) and a history of epilepsy (p = 0.02; OR 1.85; 95% CI 0.77–4.42) were not statistically significant based on their CI.
Limitations
One of the main limitations is that this was a retrospective study. Furthermore, it was carried out at a quaternary-level hospital with highly qualified personnel and greater availability of EEGs than other equivalent institutions in our environment, even for emergency use. Thus, it is hard to extrapolate the results of the study to other hospitals. In addition, more prospective studies are needed.
Conclusion
Routine EEG is useful in the ED, even in patients with syncope or acute ischemic lesions, because it allows clinical management or AED changes to be determined.
Acknowledgment
The authors thank Dr. Fernando Cendes for his help in final drafting and Lic. Diane Lein for help in English translation and grammar.
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ EEG changes the diagnosis and treatment of patients with acute ischemic lesions, syncope, and history of epilepsy.
→ EEG performed in emergency department generate discharges when realized for different indications from status epilepticus.
→ Sometimes EEG present no alterations in patients with clear seizures.
→ Patients with a history of epilepsy presented more alterations in EEG than other patients.
References
- 1.Yigit O, Eray O, Mihci E, Yilmaz D, Arslan S, Eray B. The utility of EEG in the emergency department. Emerg Med J 2012;29:301–305. [DOI] [PubMed] [Google Scholar]
- 2.Máñez Miró JU, Díaz de Terán FJ, Alonso Singer P, Aguilar-Amat Prior MJ. Uso de la electroencefalografía urgente por el neurólogo de guardia: utilidad en el diagnóstico del estatus epiléptico no convulsivo. Neurología 2018;33:71–77. [DOI] [PubMed] [Google Scholar]
- 3.Praline J, Grujic J, Corcia P, et al. Emergent EEG in clinical practice. Clin Neurophysiol 2007;118:2149–2155. [DOI] [PubMed] [Google Scholar]
- 4.Feyissa AM, Tatum WO. Adult EEG. In: Handbook of Clinical Neurology. Amsterdam: Elsevier B.V.; 2019:103–124. [DOI] [PubMed] [Google Scholar]
- 5.Varelas PN, Spanaki MV, Hacein-Bey L, Hether T, Terranova B. Emergent EEG: indications and diagnostic yield. Neurology 2003;61:702–704. [DOI] [PubMed] [Google Scholar]
- 6.Castellanos L, Cárdenas L, Carrillo ML. Revisión hiponatremia. Horiz Me 2016;16:60–71. [Google Scholar]
- 7.MINISTERIO DE SALUD. RESOLUCION NUMERO 8430 DE 1993 [Internet]. 1992:1–19. Available at: minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.PDF. Accessed April 6, 2018. [Google Scholar]
- 8.Pallin DJ, Goldstein JN, Moussally JS, Pelletier AJ, Green AR, Camargo CA. Seizure visits in US emergency departments: epidemiology and potential disparities in care. Int J Emerg Med 2008;1:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Firosh Khan S, Ashalatha R, Thomas SV, Sarma PS. Emergent EEG is helpful in neurology critical care practice. Clin Neurophysiol 2005;116:2454–2459. [DOI] [PubMed] [Google Scholar]
- 10.Paliwal P, Wakerley BR, Yeo LLL, et al. Early electroencephalography in patients with emergency room diagnoses of suspected new-onset seizures: Diagnostic yield and impact on clinical decision-making. Seizure 2015;31:22–26. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz A, Wiebe S, Gronseth GS, et al. Evidence-based guideline: management of an unprovoked first seizure in adults: report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology 2015;84:1705–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King MA, Newton MR, Jackson GD, et al. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. Lancet 1998;352:1007–1011. [DOI] [PubMed] [Google Scholar]
- 13.Viloria Alebesque A, López Bravo A, Bellosta Diago E, Santos Lasaosa S, Mauri Llerda JA. Utilidad del electroencefalograma en el manejo de la epilepsia en el Servicio de Urgencias. Neurología 2020;35:238–244. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from Dryad (tables 1 and 2, https://datadryad.org/stash/share/x5bf_rm762DrldLmc5VKCSIbg3ue7NNyxGucs-TYrPE). Anonymized data will be shared by request from any qualified investigator.


