PRACTICAL IMPLICATIONS
Doxylamine is a widely available first-generation antihistamine used as a sleep aid. Some first-generation antihistamines, such as doxylamine and diphenhydramine, may block voltage-gated sodium channels. Doxylamine toxicity could include ocular flutter in addition to an antihistaminic/antimuscarinic syndrome, causing encephalopathy and mydriasis.
Ocular flutter consists of bursts of high-frequency, low-amplitude, conjugate saccadic oscillations without normal intersaccadic interval and confined to the horizontal plane. Ocular flutter can be present during sleep, eyelid closure, attempted fixation, and volitional eye movements. Cerebellar fastigial nuclei disinhibition and/or inhibition of pontine omnipause cells disturb the excitatory/inhibitory balance of brainstem saccadic burst neurons, ultimately leading to saccadic oscillations including ocular flutter.1 The most common causes of ocular flutter in adults are paraneoplastic and parainfectious. Toxic metabolic etiologies are rare and include medications such as phenytoin and venlafaxine. Cerebellar and brainstem lesions have been reported, but the etiology remains unknown in approximately half of these patients.1,2 We present a case of ocular flutter in the setting of acute doxylamine intoxication. Doxylamine is a first-generation antihistamine widely available over the counter (OTC) as a sedative sleep aid, often combined with antitussives and decongestants.
A 26-year-old man with a history of tobacco and marijuana use acutely developed altered consciousness, abnormal eye movements, and a generalized tonic-clonic seizure after ingestion of large quantities of an unknown OTC substance. Examination revealed encephalopathy, bilateral mydriasis, and ocular flutter (Video1). There were no additional localizing signs or abnormal movements. Laboratory studies revealed elevated venous lactate (16.3 mmol/L, normal = 0.5–2.2), metabolic acidosis (anion gap 41, normal = 7–16; CO2 10 mmol/L, normal = 20–28), hypokalemia (2.9 mmol/L; normal = 3.4–4.7), and acute renal failure (serum creatinine 1.46 mg/dL, normal = 0.67–1.17). ECG showed intermittent supraventricular tachycardia and new-onset right bundle branch block with wide QRS complex (Brugada type-1 pattern). Brain imaging studies were unremarkable. Urine drug panel was positive for doxylamine, tetrahydrocannabinol, and cotinine (nicotine metabolite).
Download Supplementary Video 1 (3.9MB, m4v) via http://dx.doi.org/10.1212/000956_Video_1
The patient was placed on telemetry observation with seizure precautions and supportive therapy. He required 1 mg of intravenous lorazepam for agitation and demonstrated episodes of bradycardia overnight. The following day, ocular flutter had improved and he was more alert. Two days later, ocular flutter completely resolved and he had returned to his baseline mental status (Video 1). Abnormal laboratory values and ECG resolved. He admitted to intentionally overdosing on OTC sleeping pills and was discharged home after psychiatric evaluation and arrangement for follow-up.
The acuity and relatively quick self-resolution of encephalopathy, seizures, intermittent agitation, mydriasis, and supraventricular tachycardia with superimposed cardiac conduction disturbance is consistent with acute antihistamine/anticholinergic overdose. The urine drug assay obtained uses liquid chromatography-tandem mass spectrometry to identify over 250 common pharmaceutical drugs and drugs of abuse, but it does not identify novel psychoactive substances. However, the most likely precipitant in this case was doxylamine overdose. Similar to other first-generation H1-receptor antagonists, doxylamine binds nonselectively to peripheral and central H1 and muscarinic receptors, resulting in widespread antimuscarinic effect. Some first-generation antihistamines, such as diphenhydramine and doxylamine, have a chemical structure similar to phenytoin and can block sodium channels. This could explain the ECG findings seen in this patient, including the wide QRS complex. Similar to phenytoin intoxication, central manifestations of sodium channel blockage could include ataxia and abnormal eye movements.3
Characterization of eye movement abnormalities can help in the differential diagnosis of toxic encephalopathy syndromes. Slow-phase movements (essentially abnormal drift of the eyes) are followed by fast-phase corrective saccades in jerk nystagmus. This type of nystagmus has been reported in multiple intoxications. Interestingly, voltage-gated sodium channel blockage was proposed as the mechanism of vertical jerk nystagmus in a child with antihistamine/anticholinergic intoxication.4 In saccadic intrusions, fast-phase movements initiate and maintain oscillations. Opsoclonus, a multidirectional saccadic oscillation with large amplitude and high frequency, has been reported in toxic encephalopathies because of cefepime (anti-GABAergic), amitriptyline (anticholinergic, noradrenergic, and serotoninergic), phenytoin, and venlafaxine.5,6 Toxic encephalopathy and ocular flutter have been observed in a patient with serotonin syndrome because of venlafaxine.2 Opsoclonus and ocular flutter are considered a spectrum of saccadic oscillations because they have similar pathophysiology and can occur together in the same patient.1
The mechanism of ocular flutter in doxylamine intoxication is unclear. Cerebellar fastigial nuclei disinhibition has been implicated in the pathogenesis of ocular flutter. Purkinje neurons of the dorsal cerebellar vermis, which normally inhibit fastigial nuclei, express voltage-gated sodium channels.1 Similar to phenytoin, large doses of doxylamine and other H1 antagonists could block cerebellar voltage-gated sodium channels, disinhibit fastigial nuclei, and trigger or exacerbate saccadic oscillations.3 Remarkably, venlafaxine-induced sodium channel blockade could have contributed to the saccadic oscillations observed in previously reported patients.2,5,7
In summary, doxylamine and first-generation antihistamine intoxication should be considered in patients who present with encephalopathy, ocular flutter, mydriasis, and other signs of an antihistaminic/antimuscarinic syndrome. Doxylamine is widely available OTC, and intoxication is commonly a result of both intentional and unintentional overdose.
Acknowledgment
We thank the patient for his cooperation. The patient gave written consent to publish the photographs and video included in this article.
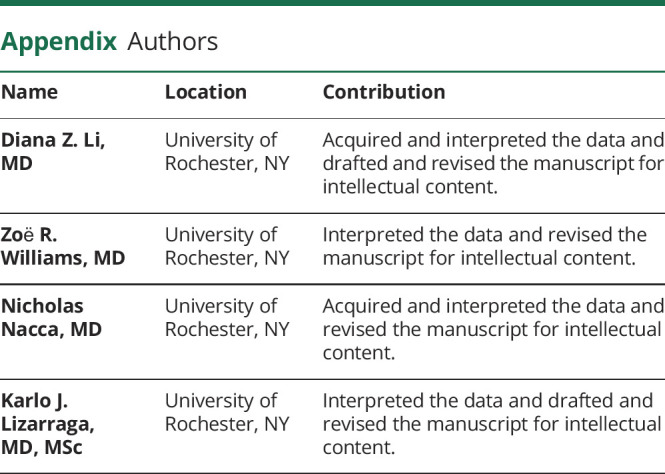
Appendix. Authors
![]()
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Ramat S, Leigh RJ, Zee DS, Optican LM. What clinical disorders tell us about the neural control of saccadic eye movements. Brain 2007;130:10–35. [DOI] [PubMed] [Google Scholar]
- 2.Sim SS, Sun JT. Ocular flutter in the serotonin syndrome. N Engl J Med 2016;375:e38. [DOI] [PubMed] [Google Scholar]
- 3.Kuo CC, Huang RC, Lou BS. Inhibition of Na(+) current by diphenhydramine and other diphenyl compounds: molecular determinants of selective binding to the inactivated channels. Mol Pharmacol 2000;57:135–143. [PubMed] [Google Scholar]
- 4.Alkan G, Emiroglu M, Kartal A. Hydroxyzine-induced vertical nystagmus. Indian Pediatr 2018;55:1094. [PubMed] [Google Scholar]
- 5.Necpál J, Skorvanek M. Opsoclonus-myoclonus ataxia syndrome secondary to venlafaxine intoxication. J Neurol Sci 2017;372:19–20. [DOI] [PubMed] [Google Scholar]
- 6.Lizarraga KJ, Heros DO, Adams D, Lang AE, Kanner AM. Opsoclonus-myoclonus-encephalopathy induced by cefepime. J Neurol Sci 2019;396:33–35. [DOI] [PubMed] [Google Scholar]
- 7.Khalifa M, Daleau P, Turgeon aJ. Mechanism of sodium channel block by venlafaxine in Guinea pig ventricular myocytes. J Pharmacol Exp Ther 1999;291:280–284. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Download Supplementary Video 1 (3.9MB, m4v) via http://dx.doi.org/10.1212/000956_Video_1


